Abstract
Background: Reconstruction of malunited diaphyseal fractures of the forearm is one of the most difficult treatments due to its complicated structure. Widespread usage of Digital Imaging and Communications in Medicine (DICOM) data of 3-dimensional (3D) computed tomography (CT) and 3D printing can make estimating the true plane of the deformity easy. Methods: A 21-year-old man with limited supination due to left forearm nonunion deformity initially treated by locking plate fixation was referred to our hospital. We evaluated the deformity by superimposing the mirror image bone model of the contralateral normal bone onto a model of the affected bone and 3D real full-scale bone model. Results: The patient underwent a manual corrective osteotomy according to our planning. He had satisfactory improvement of his symptoms with no complications. Conclusions: We postulated that our simple preoperative simulation and manual osteotomy with the aid of 3D CT reconstruction and 3D real full-scale bone model fit in the clinical practice as a recent trend.
Keywords: malunited diaphyseal fractures of forearm, corrective osteotomy, simple surgical planning, 3-dimensional CT data, full-scale model
Introduction
In the correction of malunited fractures, diaphysis of the forearm is one of the most difficult and challenging areas due to its complicated structure. Jayakumar and Jupiter described this complicated estimation, planning, and treatment in detail with their review article.1 Deformity of the long bones consists of angular deformation and rotation deformation. Determining the true plane of the deformity is very complicated. Murase et al reported a custom-made osteotomy guide4; however, its widespread acceptance is difficult in clinical practice, and surgical correction to the original form is not always suitable for all patients’ demands. Wide-spread acceptance of the usage of Digital Imaging and Communications in Medicine (DICOM) data of 3-dimensional (3D) computed tomography (CT) by commercially available software and 3D printing can make calculating or estimating the true plane of the deformity easy and familiar.2-4 Here we report its utility and our simple strategy on planning the corrective osteotomy of frequently observed malunited diaphyseal fractures of the forearm. The real-scale bone model made by the 3D printer was utilized for preoperative planning and navigation during operation.
Case Presentation and Our Surgical Strategy
A 21-year-old man with limited supination due to left forearm nonunion deformity was introduced to our hospital. He had received open reduction and internal fixation (ORIF) of the diaphysis of both radius and ulna by locking plate after trauma, and had been followed up for 1 year due to a nonunion with progressing deformity of the radius.
Examination revealed a severe limitation of supination, which was concomitant with his chief complaint that he could not catch a ground ball when playing baseball. The flexion-extension arc was 15 (0)° to 125 (130)°, with 65 (65)° pronation and 0 (85)° supination (nonaffected right side) (Figure 1). The radiograph at initial examination revealed a hypertrophic nonunion with gradual deformity in the central one-third region of the radial diaphysis and complete union in the central region of the ulnar diaphysis (Figure 2).
Figure 1.
The photograph of the patient at supination and pronation before surgery.
Figure 2.
The radiograph and 3-dimensional computed tomography of the patient before surgery.
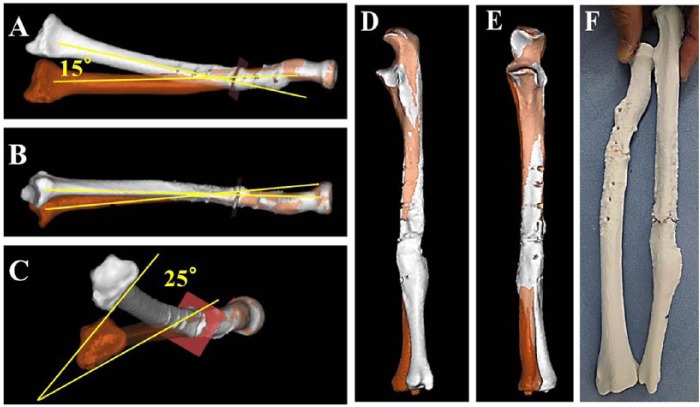
The preoperative 3D CT data sets were exported in DICOM format. After constructing a surface model of the bone, we evaluated deformity by superimposing the mirror-image bone model of the contralateral normal bone onto a model of the affected bone using the commercially available computer software (Magics; Materialise, Leuven, Belgium). As shown in Figure 3, the deformities of the radius and ulna were evaluated, and a real-sized bone model made of acrylonitrile butadiene styrene (ABS) resin was manufactured by 3D printer for simulation of the corrective osteotomy. The model was sterilized by ethylene oxide and used during the surgery for navigation.
Figure 3.
Superimposing the mirror-image bone model of the contralateral normal bone onto a model of the affected bone. (a) to (c) show the radius. (d) and (e) show the ulna. (f) shows the real-sized plastic model of the affected forearm.
Our simple strategy is described as follows. The order of the correction of radius or ulna is the severe side first. The angle of deformity of the 3 parameters (radial-ulnar angular, volar-dorsal angular, and rotational) are measured with an aid of superimposing the mirror-image bone model as shown in Figure 3a-c. We select the severe 2 parameters according to the severity of deformity (usually >10°).
In clinical practice, as a recent trend, the following condition is frequently observed in treating malunited forearm diaphyseal fractures that had been treated by ORIF. The standard treatment of forearm diaphyseal fractures in adults involves anatomic reduction and stable plate fixation. Most of the malunion occurs due to the delayed union during fracture healing. Anatomically, the radius rotates but the ulna does not rotate. The radius is exposed rotational mechanical strength during activities of daily use. Therefore, the rotational as well as angulation deformity seemed to be observed in the radius rather than ulna. In addition, as the locking plate is conventionally fixed on volar or dorsal surface, angulation deformity in frontal plane rather than sagittal plane as well as rotational deformity was frequently observed. In this case also, the deformity of radius but not ulna was evident, and the 2 parameters with severe deformity (varus 15° and pronation 25° but not extension <10°) were selected as a target of the correction as shown in Figure 3.
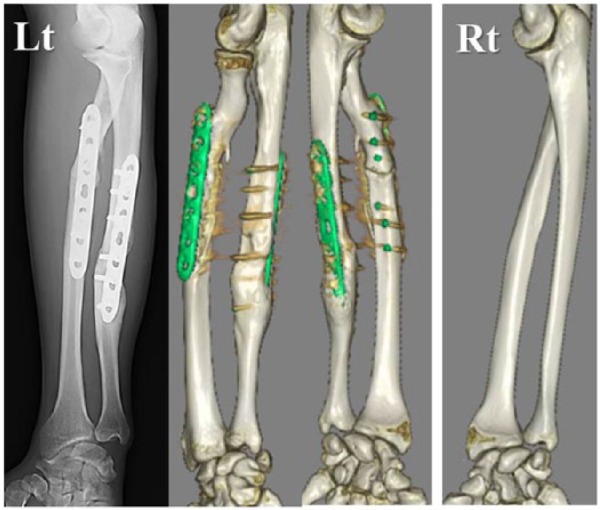
The patient underwent the surgery 1.2 years after the initial ORIF. A straight incision was made over the previous incision on the radius, and the nonunion site was explored after removal of the locking plate. To know the current position during correction procedure, 2 parallel Kirschner wires (K-wires) were fixed at proximal and distal fragment perpendicular to the bone axis, as a marker of correction. The fibrous tissue mixed with osteocartilaginous mass at the nonunion site was removed. The distal fragment was manually corrected 15° in radial deviation and 25° in supination with an aid of the previously introduced 2 parallel K-wires as a reference. At this point, supination was improved; however, pronation was severely limited due to eccentric movement of the radial head. After addition of the correction of nearly 10° in extension, an acceptable improvement of rotational arc was obtained. In this corrected position, the proximal and distal fragments were fixed by a guide wire of cannulated headless screw. After checking the improvement of rotational arc and supination, a cannulated headless screw was inserted through the guide wire as a lag screw, and the radius was rigidly fixed by a locking neutralization plate. After partial release of the interosseous membrane (IOM) on the exposed radius, chip bone was packed in the nonunion site. The improved good congruity through 40° of pronation and 50° of supination motion was confirmed during the surgery. The surgical/tourniquet times were 80/65 minutes. The elbow was immobilized in 90° of flexion and neutral rotation for 3 weeks with a cast. After permitted active pronation-supination, passive pronation-supination exercise was started using a splint at 6 weeks after surgery. Six months later, bone union was achieved (Figure 4), and the forearm was stable and had complete mobility, except for 5° loss in pronation and supination compared with the nonaffected side. The man remained asymptomatic with improved range of motion (ROM) as an active baseball player for 2 years after surgery. The flexion-extension arc was 5 (0)° to 130 (130)°, with 60 (65)° pronation and 80 (85)° supination (nonaffected right side) (Figure 5).
Figure 4.

The anteroposterior and lateral radiographs 6 months after surgery.
Figure 5.
The photograph of the patient at supination and pronation at 12 months after surgery.
Discussion
Review of the literature revealed the utility of the 3D CT or a real-sized bone model prepared by preoperative computer simulation.2-4 However, these simulations and surgery necessitate special equipment and take time. In our study, we used the widely spreading computer simulation by 3D CT data and bone model by 3D printer. Therefore, our simple strategy fits in clinical practice. The commercially available computer software to analyze DICOM data has been widely used, and its cost acceptable. The price varies according to its performance (ie, estimated rough price is from $10 000: http://biomedical.materialise.com/mimics, http://analyzedirect.com/analyze-12-0/, http://www.miyuki-net.co.jp/jp/product/researchEquipment/MriRelation/Analyze.shtml, https://www.zio.co.jp/products/ziostation2/index.html). The cost of a real-sized bone model manufactured by 3D printer was about $100 in this study.
Adult malunited diaphyseal fractures of the forearm after ORIF seemed to be observed frequently in radius rather than ulna. Furthermore, its deformity seemed to be caused by coronal angulation and rotation but not sagittal angulation, due to the position of plate, which is usually on the dorsal or volar surface of the radius. This case was simply treated by valgus and supination with additional extension osteotomy manually using K-wires as a reference. During the surgery, manual correction of more than 2 parameters at the same setting is difficult in clinical practice; therefore, we selected severe 2 parameters at first. Complete release of the IOM may not be necessary, because the final rotational arc overcomes the arc obtained during the surgery in this case.
Although our strategy is not precise compared with the previous reports,2-4 our treatment process shows the most frequently observed type of deformity and employs technology that will be viable for wide usage even in community hospitals in the near future. Our simple strategy will fit in clinical practice as a relatively easy method without usage of any special equipment.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation 140 (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: Identifying information, including patients’ names, initials, or hospital numbers, were not published in written descriptions, photographs, and pedigrees.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Jayakumar P, Jupiter JB. Reconstruction of malunited diaphyseal fractures of the forearm. Hand (N Y). 2014;9:265-273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kataoka T, Oka K, Miyake J, Omori S, Tanaka H, Murase T. 3-dimensional prebent plate fixation in corrective osteotomy of malunited upper extremity fractures using a real-sized plastic bone model prepared by preoperative computer simulation. J Hand Surg Am. 2013;38:909-919. [DOI] [PubMed] [Google Scholar]
- 3. Miyake J, Oka K, Kataoka T, Moritomo H, Sugamoto K, Murase T. 3-dimensional deformity analysis of malunited forearm diaphyseal fractures. J Hand Surg Am. 2013;38:1356-1365. [DOI] [PubMed] [Google Scholar]
- 4. Murase T, Oka K, Moritomo H, Goto A, Yoshikawa H, Sugamoto K. Three-dimensional corrective osteotomy of malunited fractures of the upper extremity with use of a computer simulation system. J Bone Joint Surg Am. 2008;90:2375-2389. [DOI] [PubMed] [Google Scholar]