Abstract
Background: Collagenase Clostridium histolyticum (CCH) injection and manipulation is a relatively new method for treating Dupuytren contracture that is growing in popularity. Although side effects such as swelling and ecchymosis are common, they are typically mild and self-limited. Major complications are rare but have included flexor tendon rupture and complex regional pain syndrome. Methods: This study describes a case report of 2 patients seen at our institution. Results: Here, we report 2 patients seen at our institution each with different, yet serious complications after CCH injection and manipulation. One patient had extensive skin loss and chose amputation over reconstruction. The other patient had loss of perfusion and required finger amputation. Conclusions: Although it is unclear how directly the administration of CCH is connected to the observed complications, physicians should recognize the potential for serious rare complications in any treatment of Dupuytren contracture.
Keywords: collagenase, Dupuytren, Xiaflex, epinephrine, amputation
Introduction
Surgical release of Dupuytren cords, whether by fasciotomy or fasciectomy, has been the mainstay of treatment for Dupuytren contracture since the early 19th century. Enzymatic division of Dupuytren cords using collagenase derived from the bacterium Clostridium histolyticum, first described in 1996 by Hurst et al, is a minimally invasive treatment for Dupuytren contracture.7 Since the Food and Drug Administration (FDA) approval of collagenase Clostridium histolyticum (CCH; Xiaflex; Auxilium Pharmaceuticals, Chesterbrook, Pennsylvania) in 2010, the treatment has rapidly gained popularity. The CCH is injected into the Dupuytren cord, and after approximately 24 hours according to the manufacturer’s recommendations, the patient returns to the clinic where the cords are lysed by manipulating the fingers into extension. Five-year follow-up data have shown efficacy comparable with surgical intervention with 70% of patients showing complete or nearly complete release of their metacarpophalangeal (MP) joint contractures and 39% showing recurrent contractures within the follow-up period.3 Collagenase treatment of Dupuytren contracture affecting the proximal interphalangeal (PIP) joint, like surgical intervention, is less successful with only 40% showing complete or near complete release, and a higher recurrence rate of 66% at 5 years.3 Overall, the treatment of Dupuytren contracture with CCH appears to have short-term efficacy similar to palmar fasciectomy with a shorter recovery period and without the attendant risks of general anesthesia.3
The most common complications noted following CCH injection are edema (75%), ecchymosis (23%), and skin lacerations (9.2%), with rare reports of flexor tendon rupture (0.3%) and complex regional pain (0.1%).10 Overall, the rate of major complications is similar to or lower than the rates associated with surgical intervention.3,10
Here, we report 2 patients seen at our institution each with different, yet catastrophic complications after CCH injection and manipulation.
Case Report
Patient 1
An 81-year-old ambidextrous male with a 2-year history of Dupuytren contracture involving the left ring and small fingers and the first web space was evaluated. The patient’s medical history was significant only for Raynaud’s phenomenon affecting both hands. His MP joint contractures were 12° at the ring finger and 30° at the small finger. The small finger also had a 6° PIP joint contracture. The first web space contracture limited full palmar abduction of the thumb. After a discussion of treatment options, he chose to undergo CCH injections to pretendinous cords of the ring and small fingers and a first web space cord. The small finger pretendinous cord extended to the mid-proximal phalanx. A volume of 9.5 mL of lidocaine with epinephrine (1:100 000) with 0.5 mL of bicarbonate was injected as local anesthesia, and 0.9 mg of CCH was used on the hand and was split among the 3 cords. When he returned to the clinic the following day, the hand had typical bruising and swelling, was not painful, and was well perfused. He received local anesthesia of 9.5 mL of lidocaine with epinephrine (1:100 000) with 0.5 mL of bicarbonate and then underwent manipulation. Full finger extension of small and ring fingers was achieved, and the web space contracture was fully corrected with no skin lacerations noted.
The patient developed swelling, ecchymosis, and increased pain within 4 hours after the manipulation and presented to the emergency department at about 8 hours post manipulation. The patient had blistering on the ring and small fingers, reduced but not absent sensation, and sluggish capillary refill at the fingertips with a small area of blanching on the radial ring and small fingers at the distal phalanx (Figures 1 and 2). Based on his clinical appearance, there was concern for eventual tissue loss distally at the pad of the small finger. The examiner concluded during his hospital stay that both pain and vasospasm symptoms were resolving, and aspirin was given to prevent thrombosis at discharge.
Figure 1.

Ecchymosis and swelling in the palmar hand after collagenase Clostridium histolyticum injection and manipulation, which are commonly seen after treatment.
Figure 2.

Blistering of the ring and small fingers present after collagenase Clostridium histolyticum injection and manipulation, not typically seen after treatment and concerning for vascular insufficiency.
He was referred to our institution 2 weeks following his CCH injection, and there were lines of demarcation at the mid-proximal phalanges of both the ring and small fingers with no dopplerable signal distally. Recommendation was made for amputation of the necrotic fingers, and he subsequently underwent amputation of the ring and small fingers at the level of the mid-proximal phalanges (Figure 3). His postoperative course was uncomplicated. Arteriosclerosis was noted in the pathology specimens.
Figure 3.
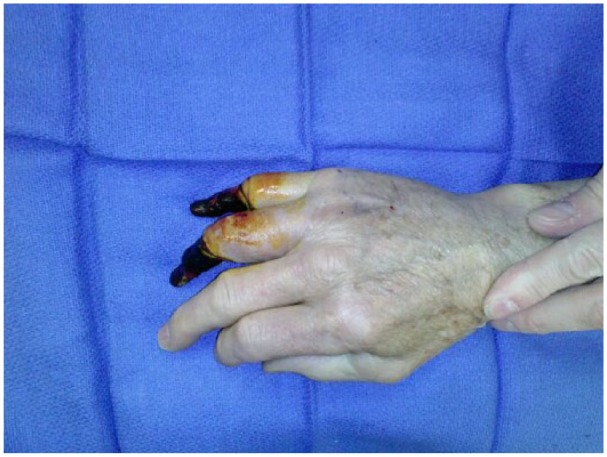
Hand appearance just prior to amputation weeks after initial treatment.
Patient 2
A 64-year-old male with rheumatoid arthritis presented to his rheumatologist with Dupuytren contracture of the right small finger primarily affecting the PIP joint. He had undergone surgical release twice previously, but the quality and location of scarring from these procedures was not noted by the referring provider. At the time of treatment, recurrent contractures were estimated at 60° of the PIP and 80° at the distal interphalangeal (DIP) joint based on available imaging. The initial 0.58 mg of CCH, which was diluted per manufacturer’s recommendations, was injected just distal to the distal palmar crease. He returned the following day for manipulation which resulted in no improvement in his small finger range of motion and did not significantly change in appearance of the small finger cord extending from the palm to the PIP joint. He returned 4 weeks later, for a repeat 0.58 mg injection of CCH again just distal to the distal palmar crease. He returned the following day and was noted to have a large hemorrhagic blister circumferentially on the finger. Finger manipulation was performed following an injection of 1% plain lidocaine. The blood blister ruptured during the manipulation attempt, and the PIP joint retained its flexion contracture with no improvements in extension. The finger retained normal distal capillary refill, but there was significant skin loss over the proximal phalanx with exposed flexor tendon.
The patient was then referred to our hand surgeon for treatment of his full-thickness skin loss with exposed tendon. Following debridement, the patient had a 3 × 3-cm circumferential area of full-thickness skin loss with exposed flexor and extensor tendons. The wound was covered with Integra dermal regeneration template. The patient sought further treatment outside our institution, and after discussion with his local orthopedist, he chose to proceed with amputation because of predicted poor outcome of function presented by his provider. He underwent MP joint level amputation of the small finger 3 weeks later after the initial injection treatment.
Discussion
CCH injection and manipulation is being used more commonly for the treatment of Dupuytren contracture as longer term data on its safety and efficacy become available. Adverse events such as edema, skin lacerations, and ecchymosis are typically mild and self-limited, although there have been rare reports of more serious complications like flexor tendon rupture.3,10 Minor bleeding-related complications such as injection site ecchymosis (23%), blood blisters (7%), or hematoma (6%) have also known to occur.10 The cases that we present show 2 different, but serious complications that ultimately were treated with finger amputation.
Our first patient, whose pathology report identified underlying peripheral vascular disease, sustained vascular injury after injection and manipulation. The loss of circulation after manipulation under anesthesia was multifactorial. Arterial injury may have occurred due to traction injury, enzymatic damage, vascular injection, direct puncture, or a combination of these factors. One likely possibility is that forcible extension of the digit led to digital vessel thrombosis or rupture as can occur during open fasciectomy. CCH is least active against the type IV collagen found in the basement membrane of blood vessels,5,7,9 and it is unclear in this case whether it was a factor in the loss of finger perfusion. Digital vessel injury after CCH injection has previously been reported in the case of a 71-year-old patient who experienced loss of ulnar digital artery perfusion distal to the injection site.6 Bluish discoloration of the treated finger was noted by the patient, and the diagnosis was confirmed by angiogram, but no further intervention was required as the radial digital artery flow was sufficient. Spiers et al hypothesized that if the arterial vessel walls were exposed to a significant amount of collagenase, structural damage could occur; however, the authors also gave several other plausible reasons for the vascular disruption including injury from the needle, the manipulation, splinting of a damaged vessel, or a subclinical vasospastic disease.6
Other possible causes include direct injury to the digital vessels from the injection of local anesthetic prior to manipulation or vasospasm and thrombosis of the digital arteries from the epinephrine contained in the local anesthetic. The use of local anesthetic with epinephrine in the digits is generally considered to be safe,1 yet many are reluctant to use epinephrine in digits with known vascular injury or vascular disease.8 However, vasospasm did not occur on the initial treatment day when both lidocaine and epinephrine and CCH were first administered which makes a multifactorial cause likely.
The second patient’s complication involved significant skin loss related to CCH treatment, and the patient had no documented vascular insufficiency. Skin damage, in the form of ecchymosis, blistering, and skin tears, is common following treatment with CCH.2,10 Skin tears that require skin grafting after CCH treatment have been reported in the literature.4 Although these side effects are presumed to be related to reactivity of the CCH with collagen within the skin and skin vasculature, the exact mechanism is unknown and could result from a local inflammatory response. As with lesser skin losses, it is possible that our second patient’s finger could have been salvaged with further treatment. Nevertheless, the patient chose to abandon further reconstruction and opted for amputation.
For patients with Dupuytren contracture, the desirability of a treatment that can be administered as an in-office injection and that has an effectiveness similar to surgery is a reasonable option. It is important to emphasize that it is unclear how directly the administration of CCH is connected to the observed complications, yet physicians should recognize the potential for serious rare complications in any treatment of Dupuytren contracture.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: Informed consent was obtained for all patients and for those whose identifying information is included in this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Denkler K. Dupuytren’s fasciectomies in 60 consecutive digits using lidocaine with epinephrine and no tourniquet. Plast Reconstr Surg. 2005;115(3):802-810. [DOI] [PubMed] [Google Scholar]
- 2. Manning CJ, Delaney R, Hayton MJ. Efficacy and tolerability of day 2 manipulation and local anaesthesia after collagenase injection in patients with Dupuytren’s contracture. J Hand Surg Eur Vol. 2014;39(5):466-471. doi: 10.1177/1753193413490899. [DOI] [PubMed] [Google Scholar]
- 3. Peimer CA, Blazar P, Coleman S, Kaplan FT, Smith T, Lindau T. Dupuytren contracture recurrence following treatment with collagenase Clostridium histolyticum (CORDLESS [collagenase option for reduction of Dupuytren long-term evaluation of safety study]): 5-year data. J Hand Surg Am. 2015;40(8):1597-1605. doi: 10.1016/j.jhsa.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 4. Peimer CA, McGoldrick CA, Fiore GJ. Nonsurgical treatment of Dupuytren’s contracture: 1-year US post-marketing safety data for collagenase Clostridium histolyticum. Hand (N Y). 2012;7(2):143-146. doi: 10.1007/s11552-012-9407-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rydevik B, Ehira T, Linder L, Olmarker K, Romanus M, Branemark PI. Microvascular response to locally injected collagenase. An experimental investigation in hamsters and rabbits. Scand J Plast Reconstr Surg Hand Surg. 1989;23(1):17-21. [DOI] [PubMed] [Google Scholar]
- 6. Spiers JD, Ullah A, Dias JJ. Vascular complication after collagenase injection and manipulation for Dupuytren’s contracture. J Hand Surg Eur Vol. 2014;39(5):554-556. doi: 10.1177/1753193413517075. [DOI] [PubMed] [Google Scholar]
- 7. Starkweather KD, Lattuga S, Hurst LC, et al. Collagenase in the treatment of Dupuytren’s disease: an in vitro study. J Hand Surg Am. 1996;21(3):490-495. doi:S0363-5023(96)80368-6. [DOI] [PubMed] [Google Scholar]
- 8. Thomson CJ, Lalonde DH, Denkler KA, Feicht AJ. A critical look at the evidence for and against elective epinephrine use in the finger. Plast Reconstr Surg. 2007;119(1):260-266. doi: 10.1097/01.prs.0000237039.71227.11. [DOI] [PubMed] [Google Scholar]
- 9. Toyoshima T, Matsushita O, Minami J, Nishi N, Okabe A, Itano T. Collagen-binding domain of a Clostridium histolyticum collagenase exhibits a broad substrate spectrum both in vitro and in vivo. Connect Tissue Res. 2001;42(4): 281-290. [DOI] [PubMed] [Google Scholar]
- 10. United States FDA Report. Briefing document for collagenase Clostridium histolyticum (AA4500) in the treatment of advanced Dupuytren’s disease. Arthritis Advisory Committee Meeting, September 16, 2009 https://www.fda.gov/downloads/AdvisoryCommittees/committeesmeetingmaterials/drugs/arthritisadvisorycommittee/ucm182015.pdf [Google Scholar]


