Abstract
Aims
Research has shown that the ongoing rate of diabetes-related amputations remains significant despite the existence of prevention methods and that amputation in most cases can be prevented. The purpose of the study was to assess the relationship between the level of self-efficacy and performance of foot self-care in those with diabetes as they relate to the prevention of lower extremity amputation (LEA).
Methods
A descriptive correlational study was conducted using the theoretical framework of Bandura's social cognitive theory. The Foot Care Confidence Scale (FCCS) and the Nottingham Assessment of Functional Footcare (NAFF) survey instruments were distributed to individuals over 18 years old with diabetes Type 1 and 2 in the lower peninsula of Michigan (N = 223).
Results
No significant correlation was identified between the level of self-efficacy and performance of foot self-care behaviors. Statistical significance was found between foot self-care behaviors and gender with males scoring higher than females.
Conclusions
This study adds to the body of knowledge regarding self-efficacy and diabetic foot self-care behaviors. Further research is needed to explore the relationship of gender, diabetes education attendance, and foot self-care behaviors as influencing factors in LEA prevention.
Keywords: Diabetes, Self-care, Self-efficacy, Foot, Amputation, Nurse practitioner
Highlights
-
•
Diabetes is the leading cause of nontraumatic lower extremity amputations (LEA).
-
•
The majority of LEA's are preventable with appropriate foot self-care.
-
•
Self-efficacy is a preeminent factor in performance of self-care behaviors.
-
•
Dual instrumentation including the FCCS and NAFF surveys was used for correlation.
-
•
Further research and possibly alternative methodology are needed.
Introduction
Diabetes affects 25.8 million people in the U.S. with a presumed seven million of those being undiagnosed in 2010, and is on the rise [8]. Diabetes has been noted to be a “complex and potentially devastating chronic illness” [29]; p. 312). Due to the body's inability to properly regulate blood glucose and insulin levels, this chronic illness can cause complications in many areas of the body including the lower extremities and remains the “leading cause of nontraumatic lower-limb amputations” [8]; p. 1–10).
Study aim
The aim of this study was to assess the relationship between the level of self-efficacy and reported performance of daily foot self-care practices in diabetics using a cross-sectional descriptive correlational design via survey questionnaires. The levels of self-efficacy and foot self-care behavior have been assessed in individuals with and without prior history of diabetic foot complications (ulceration, amputation) to determine the impact of these added variables. The results of the study have been analyzed in order to draw conclusions for directing patient care interventions of nurses in the role of family nurse practitioner whom care for patients with diabetes and at risk foot conditions.
Placing higher emphasis on educating patients and equipping them with the tools they need to play an active role in self-care practices has been the recent trend of health care delivery for people with diabetes and other chronic illnesses. In collaboration with the health care team, optimal disease related outcomes, improved quality of life, and greater satisfaction with treatment are attainable for individuals who are empowered to take an active role in the management of their health 7, 9, 14, 16, 22. Self-efficacy has been described as behavior specific and dynamic, and identifying a person's perception of their capability in a certain setting or with a certain behavior has often been noted as a preeminent indicator of self-care behavior performance [26]. Nurses at all levels are considered promoters of health maintenance, managers of acute/chronic illnesses, consumers of nursing theory and evidenced-based practice, health counselors and most of all patient advocates [17]. With responsibilities such as these encompassed by the scope and standards of the profession, advanced practice nurses are an intricate part of the health promotion and patient care equation, including self-efficacy enhancement and foot self-care teaching to individuals with diabetes.
The World Health Organization [30] estimated the incidence of diabetes as 347 million worldwide, and this finding has doubled since 2005. Foot care practices and prevention of wounds among the diabetic population is a prominent role for the nursing professional. Boulton et al. [6] identified that approximately 50% of all non-traumatic lower limb amputations in the US were related to diabetes and/or complications of diabetes. The WHO [31] identified that 80% of all diabetic foot complications could be prevented with basic diabetes management and care. Health education and promotion are key components of nursing care.
Background and significance
Druss et al. [13] noted how one's self-care of a chronic illness when they are not under direct medical supervision can greatly affect their quality of life and their health, as well as influence their collaboration with health care providers. As health care has gradually shifted over time toward prevention rather than cure, society's value in “nursing care that resolves problems or manages health promoting behaviors” [3] has remained steadfast. Self-efficacy advancement is a nursing health promotion intervention which has been linked with positive results. In a randomized control trial (RCT) using self-efficacy as an intervention to improve the outcome of diabetic patients [32], identified improved outcomes in self-care activities, reduced hospitalizations and reduced emergency visits.
Research has shown that the ongoing rate of diabetes-related amputations remains significant despite the existence of prevention methods and the known fact that amputations in most cases, can be prevented [1]. Statistics continue to indicate that “more than 60% of non-traumatic lower-limb amputations occur in people with diabetes” [8]; p. 8). The efforts of podiatrists, primary care providers, as well as many other professionals and organizations have been unable to stem the ongoing expense of billions of medical care dollars spent annually on diabetes care related to lower extremity amputations (LEA) [8]. Cook and Simonson [10] reported an average cost of $26,000–88,000 health care dollars per patient in 2010 varying with the severity of the amputation, highlighting a need for an alternate approach to this issue. These figures are on top of the emotional and physical cost of such an event for each individual in which more frequent hospitalizations and longer lengths of stay are necessitated 10, 12. As a primary care provider, there is a clear need for the nurse practitioner to initiate preventive action early on in order to slow the natural progression of the diabetic foot [1].
According to Stockl et al. [28]; of the diabetic patients who undergo LEA, 28–51% will “require a second leg amputation” (p. 2129) within five years. The risk of ulcers and amputations increases “two to four fold with both age and duration of diabetes,” [15]; p. 2161) and is often compounded by a history of previous ulceration 14, 25, 28. This significant burden to patients as well as to the healthcare system elucidates the need for concentrated preventive interventions and early treatment of diabetic foot ulcers.
In a recent study, McCleary-Jones [16] identified that only self-efficacy was associated with foot self-care. The study revealed that those with higher self-efficacy also were more likely to perform regular foot self-care behaviors. The cost and time required for implementing strategies to prevent LEA in those with diabetes was said to be negligible when compared to the alternative of neglecting such practices; frequently offsetting the cost of expensive surgical amputations and care 12, 15. Therefore, a focus on improved self-efficacy in regard to diabetic foot self-care for those at risk of complications has been proposed to represent an avenue toward prevention of unnecessary LEA.
Primary care providers are in a position to frequently encounter patients with diabetes and therefore are in strategic position in the assessment of overall diabetes health, risk of ulceration, and other factors that may indicate advancing disease. As part of a multidisciplinary team, the primary care provider is capable of providing effective foot care to patients with diabetes, indicating that proper care is not solely derived from specialty care providers (i.e. podiatrists). As a competent coordinator of care, once foot health issues are identified, the primary care provider is then able to work closely with the patient to implement prevention modalities and initiate treatment of the diabetic foot in order to preserve limbs and lives of those with diabetes [23].
Preventive foot self-care
Considered a psychologically as well as behaviorally demanding chronic illness, diabetes greatly impacts one's daily routine as the illness necessitates constant self-care [11]. As part of a comprehensive approach to diabetes management, daily foot self-care can contribute to an overall reduction of health risks and complications from the disease 8, 14. Therefore, one's daily self-care is a key factor in prevention of lower extremity amputations in those with diabetes since it is up to the patient to make personal decisions regarding the actions they will take. These facts draw attention to the importance of foot self-care for those with diabetes and demand employment of innovative preventive care approaches by health care providers, including consideration of the impact of self-efficacy on such practices.
Organizations such as the National Institute of Diabetes, Digestive and Kidney Diseases [18] and the American Diabetes Association [2] maintain a focus on prevention of lower extremity amputations (LEA) in people with diabetes and strongly advocate for the practice of daily foot self-care as the main prevention strategy. Using the definition of self-care provided by Richard and Shea [22] as “performance of activities necessary to achieve, maintain, or promote optimal health,” (p. 256) the connection to preventive foot self-care practices in those with diabetes is evident as well as consistent with the definition. The NDIC [18] and ADA [2] have recommended simple daily practices to monitor the condition of feet and provide appropriate preventive foot self-care. Such practices generally consist of maintaining proper control of blood glucose levels, checking feet daily, and protecting feet from potential sources of injury and skin breakdown.
The general lack of current research to support an up to date evidence-based approach to diabetes self-care and barriers to its practice have indicated a need for more nursing research on the topic of self-efficacy to determine its continued relevance in improving self-care behaviors of those with diabetes rather than simply educating them on the disease and related complications. Furthermore, the relatively limited expanse of studies specific to foot self-care has demanded more research and more attention in order to promote the use of evidence-based care in the prevention of lower extremity complications in those with diabetes.
Theoretical framework
The primary constructs of social cognitive theory: knowledge, perceived self-efficacy, outcome expectations, goals, and perceived facilitators & impediments, interact to formulate the control a person has over their illness, influencing “human motivation and action” ([5]; p. 144). The theory proposes that without adequate confidence in one's self to accomplish required activities and reach desired goals, self-care actions will not be performed [5]. This notion has been reiterated numerous times by many researchers and can be applied to diabetic foot self-care in the sense that one can know it is necessary to care for their feet, but if they are not confident they can care for their feet, they are less likely to perform self-care activities.
Beginning assumptions of this study centered on the point that those who regularly practice foot self-care have higher levels of self-efficacy compared to those who do not participate in regular foot self-care. In comparing participants who have had previous ulceration to those who have not, an attempt was made to identify the relationship between the level of self-efficacy, frequency of foot self-care practices and their influence on actually preventing ulceration and amputation. This understanding would allow practitioners to more specifically target intervention strategies to prevent a first and/or subsequent occurrence of diabetic foot ulceration based on educational/supportive needs revealed from the study.
Material and methods
The use of dual instrumentation including the Nottingham Assessment of Functional Footcare [24] and modified Foot Care Confidence Scale 19, 27 was employed in an effort to obtain well rounded responses regarding foot self-care practices (behaviors) and confidence (self-efficacy) levels from participants for correlation. Permission was obtained from the creating authors for usage of both scales. No participant names/identifiers (birthdate, address, personal information, etc.) were collected and therefore participants were anonymous.
Data collection
A convenience sample of adults with diabetes attending each of the following settings was used to gather data: primary care offices, podiatry offices, diabetes education and/or support groups, diabetic organization walks, health fairs and wound clinics in and around the lower peninsula of Michigan. Facility staff were directed to offer the surveys to all adult (age > 18 years) individuals with either Type 1 or Type 2 diabetes, with or without previous foot ulceration whom were willing and able (can read/write/make own decisions) to participate in the study. Survey packets were also offered to community partners at the National Kidney Foundation of Michigan, Flint's monthly coalition meeting for disbursement to their clients. Participants were offered the opportunity to participate in the study when they presented to these given locations or events. This method has been used by similar research studies in other locales 19, 20, 27 and allows for easy access to a representative sample of the population although it is weaker than randomized collection methods which are beyond the scope of this study. Commencement of survey distribution began once University IRB approval was received.
The researchers delivered up to 50 survey packets (consisting of an introductory cover letter which served as the consent, the chosen survey instruments, a demographic sheet, and a diabetic foot self-care information page) to each of the 55 distribution locations in the Lower Peninsula of Michigan from July to December 2013. Stamped envelopes addressed to the research advisor were attached to each set of questionnaires to permit them to be returned by mail at no cost to participants. The researchers placed the survey packets in the waiting area of the facilities with a poster notifying diabetic patients of the study and requesting their voluntary participation. Completion and return of the surveys and demographic data indicated and implied consent to participate in the study.
A minimum of 500 distributed questionnaire packets was deemed necessary to obtain a sample size of at least 100 participants as determined by power analysis correlation coefficient of .20 [21]. A total of at least 100 participant responses were also desired for the purpose of surmounting the 96 participants in the study by Perrin et al. [20] which the researchers deemed as possibly being a small and biased representation of the population. With the opportunity to attend the Diabetes Walk and Diabetes Day Expo and funding from a university mini grant, the researchers were able to greatly expand the number of survey packets distributed to approximately 1800.
Results
The statistical software system SPSS was used to evaluate study findings. There were 229 participants who completed the survey forms. Six participant responses were disqualified based on their identification of not having Type 1 or Type 2 diabetes, leaving a final study population of 223 participants. The study population consisted of 40.4% over age 65 years, 60.5% female and most with Type 2 diabetes mellitus (78.3%). A preponderance of the study population had lived with diabetes for greater than 10 years (53.2%). Regarding the current health state of their feet, 66.8% denied having peripheral vascular disease and 50.5% denied having peripheral neuropathy, although 53.6% reported having sensations of pain, tingling or loss of feeling in their feet. With regard to history of ulceration and/or amputation of toes, foot or leg, 87.5% indicated they never had a foot ulcer and 95.1% indicated they had never had an amputation of a lower extremity. The level of diabetes education was split among this group with 10.9% never having attended diabetes education, 37.3% attending once, 19.1% attending twice and 32.7% having identified themselves as having diabetes attended education three or more times. The majority of the population (61.1%) reported that they perform their own foot care and 89.7% saw their doctor every three to six months for diabetes related care.
The Foot Care Confidence Scale (FCCS) [27] was used to determine the individual's level of self-efficacy in relation to performing foot self-care. According to the author/creator of the instrument, there is a total possible score of 60 but a near perfect score would be 40 indicating a perceived high level of self-efficacy. The mean score of this population was 39.29 with a standard deviation (SD) ±7.317, indicating a rather high level of confidence (self-efficacy).
The Nottingham Assessment of Functional Footcare (NAFF) [24], scale was used to determine the actual foot self-care behaviors performed by the population surveyed. The authors/creators of the tool have suggested a cutoff score of 50 as indication of the need for further evaluation of foot self-care behaviors. Study results revealed a mean NAFF score of 75.34 with an SD, ±9.096; indicating an overall performance of protective (versus potentially unsafe) foot self-care behaviors in the study population. Analyses of the data reveal that the FCCS and NAFF scores are both high in this population.
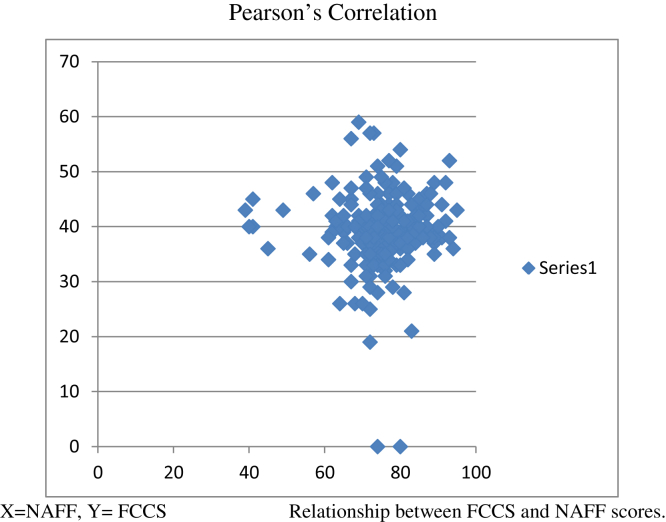
The research addressed the question “Is there a relationship between self-efficacy and diabetic foot self-care?” utilizing the Pearson's correlation coefficient to establish the presence or lack of a relationship in the findings of the FCCS and NAFF scores. There was no significant correlation between the level of confidence (self-efficacy) identified by the FCCS scores and performance of foot self-care behaviors identified by the NAFF scores (r = .026, p = .704) (Fig. 1).
Figure 1.
Pearson correlation.
Further Pearson's correlations were performed to analyze the participant's age, number of years with diabetes and possible relationship to their individual FCCS and NAFF scores.
Pearson's correlation results
| Age | Years of diabetes | |
|---|---|---|
| FCCS | r = .066, p = .333 | r = .036, p = . 596 |
| NAFF | r = .098, p = .150 | r = .040, p = .559 |
No significant correlations were further identified.
Further data analyses utilizing T-test statistical measures were performed to determine the existence of a causal effect of type of diabetes (1 or 2), history of foot ulceration/amputation (yes/no), or an individual's gender (male/female) on both the resultant level of self-efficacy and foot self-care behaviors among individual participants. In analyzing the data there was no identified statistical significance that would indicate the above mentioned variables had impacted self-efficacy levels or foot self-care behaviors in comparison to the given FCCS and NAFF scores with the exception of participant's gender and the NAFF score. The data did reveal a statistically significant difference between gender and foot care behaviors with males (mean = 77.22; SD, ±8.192) scoring higher than females (mean = 74.11; SD, ±9.469).
ANOVA testing was employed to determine any possible effect of who cares for the individual's feet, diabetes education attendance, and the frequency of visits with providers may have had on the participant's level of self-efficacy and foot self-care behaviors. The person responsible for performing each participant's foot care (self, family, or provider) was significantly linked with the level of individual self-efficacy (F = 4.066, df = 7/207, p = .000); revealing that those who performed their own self-care generally had a greater level of self-efficacy. Likewise, attendance in diabetes education (once, twice, or three times) was significantly related to the level of foot self-care behaviors as identified by the NAFF scores (F = 5.235, df = 3/216, p = .002); indicating that attending diabetes education at least once was an influencing factor in performance of foot self-care behaviors. No significant findings among the frequency of visits with the provider (every 3–6 months, yearly, or when there is a problem) were found. Regression analysis was performed with diabetes education (once, twice, three or more times) and foot self-care behaviors (NAFF) (R1 = .061, R2 = .004, B = 76.832, p = .000), revealing that diabetes education, even if it is minimal (once), is a positive predictor of foot self-care behavior performance.
Discussion
In summary, it was determined that no significant correlation existed between self-efficacy and foot self-care performance in the diabetic population studied. This determination is a surprising finding due to the fact that the level of self-efficacy is indeed predictive of most other diabetes related self-care behaviors. The application of these findings is one of support for previous research by adding strength to the evidence regarding diabetic foot self-care practices. Diabetes education is a predictor of foot self-care behaviors and the clinician is in a pivotal role not only to educate but to inspire self-efficacy in the diabetic individual. The findings of the study advocate for the use of screening instruments such as the FCCS and NAFF within the office setting to equip the clinician in promoting the patient's self-efficacy and foot self-care behaviors based upon individual needs highlighted by the results of the screening.
In this study the NAFF scores were relatively similar between the varying amounts of diabetes education received (once, twice, three times or more), although the impact of attending at least once outweighed that of further attendance. With health care dollars shrinking, further research is needed to understand and identify the depth of diabetes education needed to impact foot self-care behaviors.
The identification that gender makes a statistically significant difference in performance of foot self-care behaviors needs further exploration. Research is needed to understand the complexity of this issue as it relates not only to foot self-care practices but also to potential predictive variables.
Finally, further research is needed as it relates to self-efficacy and diabetic foot self-care as this study's population was rather healthy and therefore scored high on both scales, leaving the population with significant foot health issues unexamined. A longitudinal research study using the FCCS and NAFF tools in a population with a history of foot ulceration and/or amputation may provide significant insight, as well as further research to explore motivational factors associated with the prevention of the progressive deficits of diabetes.
Conclusions
The current findings have contributed to the small yet growing body of inquiry regarding self-efficacy and self-care promotion in the diabetic population, particularly as it relates to care of the lower extremities. This research has supported the findings of previous studies in not finding a correlation between self-efficacy and diabetic foot self-care behaviors despite examination of greater sample size.
Further investigative efforts should be done using qualitative interview or an observational approach, similarly recommended by Perrin and Snow [19]. It may be beneficial to perform correlational studies of the FCCS and NAFF instruments within a population who are unable to care for their own feet. Confidence is not the only component of self-efficacy and thus behavioral change, but consideration must also be given to motivation. Bandura [4] reflected that expectancy outcomes or the capacity to represent future outcomes provides current motivation. Further investigation is needed on motivating factors that influence an individual's decision to participate in foot self-care behaviors as well as alternate evidence based means of preventing lower extremity amputation in the diabetic population.
Conflict of interest statement
The authors deny any conflict of interest in association with this research project or the funds granted. They are students at the University and have completed this study as a requisite for graduation. The authors have no financial or professional obligation to any entity related to this study.
Acknowledgments
We would like to thank the Student Research and Creativity Institute of SVSU for supporting our research project with grant funding for additional supplies and travel expenses of the researchers. We would also like to thank all of our participating survey sites, especially the American Diabetes Association and University of Michigan for allowing us to attend the annual diabetes walk and World Diabetes Day expo. Lastly, we give our sincerest appreciation to research advisory committee members Dr. Karen Brown-Fackler, EdD, RN, CNE, and Barbara Hoag Ilkka, MSN, FNP-BC, CWCN, for helping us to refine the content and configuration of our research manuscript and encouraging us to pursue publication.
References
- 1.Abu-Qamar M. Diabetic foot screening: why is it neglected? Int Wound J. 2006;3(3):203–213. doi: 10.1111/j.1742-481X.2006.00232.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Diabetes Association (ADA) 2013. Living with diabetes: foot complications.http://www.diabetes.org/living-with-diabetes/complications/foot-complications/ [Google Scholar]
- 3.American Nurses Association (ANA) 2nd ed. American Nurses Publishing; Silver Spring, MD: 2003. Nursing's social policy statement. [Google Scholar]
- 4.Bandura A. Self-efficacy: toward a unifying theory of behavior change. Psychol Rev. 1977;2:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 5.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 6.Boulton A., Meneses P., Ennis W. Diabetic foot ulcers: a framework for prevention and care. Wound Repair Regen. 1999;7(1):7–16. doi: 10.1046/j.1524-475x.1999.00007.x. [DOI] [PubMed] [Google Scholar]
- 7.Boren S.A., Gunlock T.L., Schaefer J., Albright A. Reducing risks in diabetes self-management: a systematic review of the literature. Diabetes Educ. 2007;33(6):1053. doi: 10.1177/0145721707309809. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention . US Department of Health and Human Services, Centers for Disease Control and Prevention; Atlanta, GA: 2011. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. [Google Scholar]
- 9.Clark M.L., Utz S.W., Hollen P. Use of diabetes self-management instruments among rural African American populations. South Online J Nurs Res. 2011;11(1) [PMC free article] [PubMed] [Google Scholar]
- 10.Cook J.J., Simonson D.C. Epidemiology and health care cost of diabetic foot problems. In: Veves A., editor. The diabetic foot: medical and surgical management. Springer Science+Business Media; USA: 2012. pp. 17–32. [Google Scholar]
- 11.Cox D.J., Gonder-Frederick L. Major development in diabetes research. J Consult Clin Psychol. 1992;60(4):310–321. doi: 10.1037//0022-006x.60.4.628. [DOI] [PubMed] [Google Scholar]
- 12.Driver V., Fabbi M., Lavery L., Gibbons G. The costs of diabetic foot: the economic case for the limb salvage team. J Am Podiatr Med Assoc. 2010;100(5):335–341. doi: 10.7547/1000335. [DOI] [PubMed] [Google Scholar]
- 13.Druss B.G., Lorig K., Sterling E.W. Chronic disease self-management programs in psychiatry: helping patients help themselves. Psychiatr Times. 2012;29(1):40. [Google Scholar]
- 14.Iversen M., Ostbye T., Clipp E., Midthjell K., Uhlving S., Graue M. Regularity of preventive foot care in persons with diabetes: results from the Nord-Trøndelag Health Study. Res Nurs Health. 2008;31(3):226–237. doi: 10.1002/nur.20255. [DOI] [PubMed] [Google Scholar]
- 15.Mayfield J., Reiber G., Sanders L., Janisse D., Pogach L. Preventive foot care in people with diabetes. Diabetes Care. 1998;21(12):2161–2177. doi: 10.2337/diacare.21.12.2161. [DOI] [PubMed] [Google Scholar]
- 16.McCleary-Jones V. Health literacy and its association with diabetes knowledge, self-efficacy and disease self-management among African Americans with diabetes mellitus. ABNF J. 2011;22(2):25–32. [PubMed] [Google Scholar]
- 17.Michigan Nurses Association . 2010. Nurse practitioner FAQs.www.minurses.org [Google Scholar]
- 18.National Diabetes Information Clearinghouse . 2008. A service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Institutes of Health (NIH). Prevent diabetes problems: keep your feet and skin healthy.http://diabetes.niddk.nih.gov/dm/pubs/complications_feet/index.aspx Retrieved from: [Google Scholar]
- 19.Perrin B., Snow P. Foot care confidence in people with diabetes. Australas J Podiatr Med. 2006;40(1):3–8. [Google Scholar]
- 20.Perrin B.M., Swerissen H., Payne1 C. The association between foot-care self-efficacy beliefs and actual foot-care behaviour in people with peripheral neuropathy: a cross-sectional study. J Foot Ankle Res. 2009;2(3) doi: 10.1186/1757-1146-2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Polit D.F., Beck C.T. 9th ed. Lippincott Williams & Wilkins; Philadelphia, PA: 2012. Nursing research: generating and assessing evidence for nursing practice. [Google Scholar]
- 22.Richard A., Shea K. Delineation of self-care and associated concepts. J Nurs Scholarsh. 2011;43(3):255–264. doi: 10.1111/j.1547-5069.2011.01404.x. [DOI] [PubMed] [Google Scholar]
- 23.Seeman S. The role of the nurse specialist in the care of patients with diabetic foot ulcers. Foot Ankle Int. 2005;26(1):19–26. doi: 10.1177/107110070502600104. [DOI] [PubMed] [Google Scholar]
- 24.Senussi M., Lincoln N., Jeffcoate W., Thomas D. Psychometric properties of the Nottingham Assessment of Functional Footcare (NAFF) including commentary by Thomas D. Int J Ther Rehabil. 2011;18(6):330–334. [Google Scholar]
- 25.Shaya F., Onwudiwe N., Samant N., Winston R., Johnson W., Laird A. Foot self-check and diabetes awareness. P T. 2007;32(11):614. [Google Scholar]
- 26.Shi Q., Ostwald S., Wang S. Improving glycaemic control self-efficacy and glycaemic control behaviour in Chinese patients with Type 2 diabetes mellitus. J Clin Nurs. 2010;19(3–4):398–404. doi: 10.1111/j.1365-2702.2009.03040.x. http://dx.doi.org.library.svsu.edu/10.1111/j.1365-2702.2009.03040.x [DOI] [PubMed] [Google Scholar]
- 27.Sloan H. Louisiana State University Health Sciences Center School of Nursing; 2002. Developing and testing the Foot Care Confidence Scale to measure self-efficacy in foot care. [Google Scholar]
- 28.Stockl K., Vanderplas A., Tafesse E., Chang E. Costs of lower-extremity ulcers among patients with diabetes. Diabetes Care. 2004;27(9):2129–2134. doi: 10.2337/diacare.27.9.2129. Retrieved from: http://dx.doi.org/10.2337/diacare.27.9.2129. [DOI] [PubMed] [Google Scholar]
- 29.Whittemore R., Roy C., Sr. Adapting to diabetes mellitus: a theory synthesis. Nurs Sci Q. 2002;15(4):311–316. doi: 10.1177/089431802236796. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization . 2013. Fact sheet.http://www.who.int/mediacentre/factsheets Retrieved from: [Google Scholar]
- 31.World Health Organization . 2005. World diabetes day: too many people are losing lower limbs unnecessarily to diabetes, lower limbs unnecessarily to diabetes.http://www.who.int/mediacentre/news/releases/2005 Retrieved from: [Google Scholar]
- 32.Wu S., Lee M., Liang S., Lu Y., Wang T., Tung H. Effectiveness of a self-efficacy program for persons with diabetes: a randomized controlled trial. Nurs Health Sci. 2011;13(3):335–343. doi: 10.1111/j.1442-2018.2011.00625.x. [DOI] [PubMed] [Google Scholar]