Abstract
Background
Special insoles and shoes designed to prevent foot ulcers caused by repetitive high pressures are recommended for patients with diabetes who have any of the following risk factors: neuropathy; peripheral vascular disease; foot deformities; previous ulcers; amputation; and skin pathologies. However, there is a need for increased knowledge regarding: a) differences in the peak pressure (PP) and pressure time integral (PTI) for different types of insoles; and b) the properties of the pressure distribution for insoles used over a period of several months. We present the results of a randomized trial to compare the plantar pressures of three commonly used insoles.
Objectives
The primary objective was to compare the PP and PTI between three types of insoles. The secondary objective was to explore the long-term pattern of peak plantar pressure distribution and variations in specific regions of interest (ROI). The tertiary objective was to investigate the impacts of insole adjustments, how much the insoles were used, and the levels of patient satisfaction.
Methods
In a 2-year trial, 114 patients with type 1 (N = 31) or type 2 (N = 83) diabetes (62 men and 52 women; mean age, 57.7 ± 15.4 years; duration of diabetes, 12.3 ± 11.2 years; neuropathy, 38%), were randomized to be supplied with one of three different insoles. The ethylene vinyl acetate (EVA) insoles were used in outdoor walking shoes. The 35 EVA group (N = 39) received soft custom-made insoles composed of EVA of 35 shore A hardness, the 55 EVA group (N = 37) received custom-made insoles composed of EVA of 55 shore hardness, and the control group (N = 38) received prefabricated insoles composed of a hard core with a top layer of soft 12 shore hardness microfiber. Using F-Scan®, the in-shoe plantar pressures were measured at seven ROI (hallux, metatarsal head 1, metatarsal head 2, metatarsal head 4, metatarsal head 5, lateral aspect of the mid-foot, heel) on five occasions during the study period. The plantar-pressure variables used were PP (main outcome) and PTI. The plantar patterns of load were explored, satisfaction and usage of the insoles were rated by the participants, and insole adjustments were recorded.
Results
A mixed model analysis estimated lower PP values in the heel regions for the 35 EVA and 55 EVA insoles (171 ± 13 and 161 ± 13 kPa, respectively) than for the prefabricated insoles (234 ± 10 kPa) (p < 0.001). Also for some of the other six ROI indications of difference in PP or PTI could be observed. The redistribution of peak plantar pressure for all of the insoles, was stable at the mid-foot, while the proportion of load on the distal area changed during the study period According to the self-reported answers (scale, 0–100), the average usage of the insoles was rated as 79 and satisfaction was rated as 85 (N = 75). Thirty-two percent of the subjects had not received foot care. Fourteen adjustments to insoles were made during the study period, and 86 pairs of insoles were exchanged due to wear, with 49% being exchanged in the 35 EVA group.
Conclusions
Custom-made insoles used in combination with stable walking shoes gave lower pressures at the heel region. The variation makes it difficult to detect a systematic difference in plantar pressure for the 6 ROI, if such a difference indeed exists. The levels of satisfaction and usage for all the insoles tested were high. The insoles maintained their pressure redistribution properties over long periods, and few adjustments were needed.
Keywords: Diabetes, Foot ulcer, Prevention, Insoles, Offloading, Clinical trial
Abbreviations: EVA, ethylene vinyl acetate; 35 EVA, 35 shore EVA insoles; 55 EVA, 55 shore EVA insoles; ROI, region of interest; MTH1, metatarsal head 1; MTH2, metatarsal head 2; MTH4, metatarsal head 4; MTH5, metatarsal head 5; PP, peak pressure; PTI, pressure time integral
Introduction
The effective prevention of foot ulcers in the 347 million people around the world who are diagnosed with diabetes can be achieved with appropriate footwear [1]. Overall, 50%–86% of lower limb amputations in patients with diabetes are preceded by foot ulcers 2, 3, 4, which are often caused by ill-fitting footwear 5, 6. The prevalence of foot ulcers is 3%–10% 7, 8, 9, and neuropathy, peripheral vascular disease, previous ulcers or amputation, skin pathology, and high plantar pressure due to foot deformities have been identified as risk factors for the onset of foot ulcers 10, 11, 12, 13, 14, 15. The international recommendations for preventing diabetic foot ulcers includes the prescription of appropriate footwear (insoles and shoes), foot care, regular foot checks, and education [5]. These preventive steps have been proven to have positive effects on patient quality of life and in reducing healthcare expenditure 16, 17, 18. However, there is a need for long-term studies in which the pressure redistribution capacities of different types of insoles are compared 19, 20, 21. There is also a need for a global consensus on how to interpret the results from in-shoe pressure measurement devices [22].
Previous research has shown that high plantar pressure can be reduced through the use of custom-made or contoured insoles, in combination with special footwear 23, 24, 25, 26. It is widely debated among clinicians whether or not: (i) all patients with diabetes should have custom-made insoles; and (ii) custom-made insoles constructed from softer material are more effective in reducing the pressures in areas where there is a high risk of an ulcer development. Using an in-shoe pressure measurement technique, new insights may be obtained as to plantar pressure distribution, which will enable the formulation of recommendations related to the optimal prescription of insoles. This paper presents the results of a study in which patients with diabetes were given different types of insoles and the impacts on plantar pressure were evaluated. The patients were followed for 2 years with regard to differences in the peak pressure (PP) and pressure time integral (PTI) for different types of insoles, and additional information, e.g., levels of patient satisfaction with the insoles, was recorded at the end of the study.
Several studies on this topic have been performed in recent years. The first randomized trial, which was conducted by Paton and colleagues in 2012, included 119 patients with diabetes (96% with type 1) and neuropathy [27] and compared custom-made insoles with prefabricated insoles. The material used for both types of insoles consisted of a 3-mm-thick EVA base (medium density), with a top cover of 6-mm-thick Poron®. Their results showed no significant differences in peak plantar pressure between the different types of insoles, as measured with the F-Scan in-shoe measurement system. However, the PTI values during walking were lower for the custom-made insoles than for the prefabricated in the forefoot area.
Bus et al. [28] and Owings et al. [29] measured plantar pressure in cross-sectional studies using the Pedar® shoe-pressure measuring system. Bus et al. [28] studied 20 patients with diabetic neuropathy and foot deformities and showed that custom-made CAD-CAM manufactured insoles (composed of urethane foam over a 2-mm base with a 0.7-mm top cover) significantly reduced the PP and force-time integrals at the heel and first metatarsal head, as compared with a flat insole made of open-cell polyurethane 0.95 mm. These two types of insoles were tested in super-depth shoes.
Owing et al. [29] established a threshold value (207 kPa) for plantar pressure, and they recommended this value as the upper limit that should not be exceeded if ulcer recurrence was to be avoided. These results were obtained from a group of 49 patients with diabetes and neuropathy who used their own shoes during the study period. In the same study, the mean barefoot plantar peak pressure measured with the Emed® platform was 566 kPa.
The primary objective of the present study was to compare the peak pressures (PP), maximal peak pressures (maxPP) and pressure time integrals (PTI) for three types of commonly used insoles in a cohort of diabetic patients with or without neuropathy. The plantar pressure variables were studied for seven regions of interest (ROI). The secondary objective involved exploring the redistribution patterns of the average peak plantar pressures between the ROI, by studying the different sources of variations in the data and describing the insoles, adjustments, the frequencies of insole use, and the levels of patient satisfaction.
Subjects and methods
We performed a randomized, controlled trial that comprised patients with type 1 or type 2 diabetes who were referred to the Department of Prosthetics and Orthotics at Sahlgrenska University Hospital, Gothenburg, Sweden. The patients were supplied with insoles and shoes. Data collection and pressure measurements were performed in collaboration with the Gait Laboratory, Lundberg Laboratory for Orthopaedic Research, located at the same hospital. Recruitment took place between January 2008 and September 2009, and the patients were followed for 2 years, with examinations at approximately 6-month intervals. In line with regional guidelines and prevention strategies, the patients who were referred to be supplied with insoles and shoes were those who showed clinical signs of distal neuropathy or angiopathy, had a history of a previous ulcers or amputation, and had foot deformities or foot pathologies [30]. A total of 235 participants met the primary criteria for study eligibility, which were: ≥18 years of age; diagnosis of diabetes; ability to walk unaided; ability to understand the Swedish language; no present foot ulcers and being first-time visitors. Patients who were included in the study were randomly allocated to one of the following three interventions: (i) custom-made insoles composed of ethylene vinyl acetate (EVA) with a hardness of 35 shore A (35 EVA group; N = 39); (ii) custom-made insoles composed of EVA of 55 shore A hardness (55 EVA group; N = 37); and (iii) prefabricated insoles (control group; N = 38). The 35 shore A EVA is softer than the 55 shore EVA. A randomization with sealed envelopes (38 in each group) was performed prior study start prepared by the researchers at Lundberg Laboratory for Orthopaedic Research. The allocation was concealed until assignment occurred and the technician was informed of the assigned intervention. A mistake at the Department of Prosthetics and Orthotics at study start resulted that one participant extra got insoles of 35 shore hardness and the 55 EVA group got one less.
Custom-made insoles were fabricated using individual positive plaster molds, based on a negative plaster cast. Casting of the foot was performed with the patient in a prone position. The heating and vacuum formation of the 14-mm-thick EVA material followed the distributor's recommendations (E603442, E603402; Össur Nordic, Uppsala, Sweden). Patients in the control group received prefabricated insoles (GloboTec® Comfort 312750501400; GloboTec, Bauerfeind, Germany) (Figure 1). One technician fabricated all the individual insoles with a standardized metatarsal bar proximal to metatarsal heads II–IV. The insoles were adjusted to fit into the participant's shoes, which were designed to be used outdoors. All the shoes had a semi-rigid outer sole or stiff rocker bottom, a stable heel counter, and adjustable laces or Velcro straps (Figure 1). Upon manufacturing, the shoes were checked, to ensure that they met all the set criteria. In addition, at each follow-up, it was confirmed that the shoes still met the criteria. Photographs were taken of the shoes and the plantar surfaces of the feet of the subjects. All adjustments to the insoles during the study period were registered in the categories of: higher or lower metatarsal bar; more lateral or medial support; and more material under the heel. New insoles were supplied when any cracks or breakdown areas in the insoles were detected at follow-up (Figure 1). At baseline, the self-reported status was recorded, which included the duration of diabetes, type of diabetes, glycated hemoglobin (HbA1c) level, use of medication, use of nicotine, and ability to walk normally (yes/no).
Figure 1.
Insoles and shoes. A) The contours of the custom-made insoles composed of ethylene vinyl acetate (EVA) with a standardized metatarsal bar. B) Prefabricated insole GloboTec® Comfort 312750501400 (GloboTec, Bauerfeind, Germany), with support of the medial arch and a metatarsal pad in the forefoot in a material with a core (reinforcement element) that consists of a mixture of thermoplastic, polyurethane, polyester, and polycarbonate. The cushioning material is foam that belongs to the chemical family of urethane polymers with a shore density of about 12 shore A. The cover is a 2-mm layer of microfiber, consisting of polyester and polyurethane. C) Photograph of a representative walking shoe used in the study (Opara Deluxe men 809159, ladies 8807159; Erimed, Stockholm, Sweden). The shoe has a semi-rigid outer sole, a stable heel counter, and adjustable lacing. The maximum height of the toe box is 40 mm vs. 43 mm for EUR size 38/Women last vs 45/Men last. D) An example of a custom-made insole that is ready to be exchanged due to the presence of cracks and breakdown areas.
At baseline and at each follow-up, the loss of protective sensation in the feet, defined as a positive response to one of the following tests, was assessed by measuring responses to: a) the 10-g Semmes-Weinstein monofilament; b) the C128-Hz tuning fork; c) positioning of the big toe in extension and flexion; and d) a slight touch of a pencil [31].
At the Month-24 follow-up, all the participants filled in a questionnaire that contained questions as to how often they had used the insoles, how satisfied they were with the insoles, and whether they had received foot care during the study period. The answers to the first two questions were recorded on a visual analogue scale (0–100), wherein a higher value represents more frequent use and greater satisfaction. Participants who developed plantar ulcers discontinued the study and received appropriate treatment. The Gothenburg regional Ethics Review Board approved the study (diary number 299-07), and all the participants gave their written informed consent. The complete trial protocol is available upon request from the first author.
Pressure measurements
After the subjects were fitted with the insoles, dynamic in-shoe pressure measurements were made with the F-Scan® 6.10 (Tekscan, Boston, MA, USA) at the Gait Laboratory. The ultra-thin pressure sensor was trimmed to fit into the participant's shoes before the assessment. The foot sensors had a spatial density of four pressure sensors per cm2 and recorded the data for 400 frames in 8 s at a sampling rate of 50 Hz. The participants walked 10 m at a self-selected speed 6 times, and walking calibration was performed for each individual according to the manufacturer's recommendations and the protocol of Hsiao et al. [32]. These authors recommend a calibration procedure with the sensors loaded with similar pressure as in the trial, giving a reasonable measurement error (1.3 ± 5.8%). In the current study, each record was controlled for saturation before the record was saved. The investigator looked at the screen and confirmed that the saturation level of the pressure sensor was not reached. The sensors used had a durability that allowed each to be used several times, and they were discarded when signs of measurement error appeared on the screen at the time of recording.
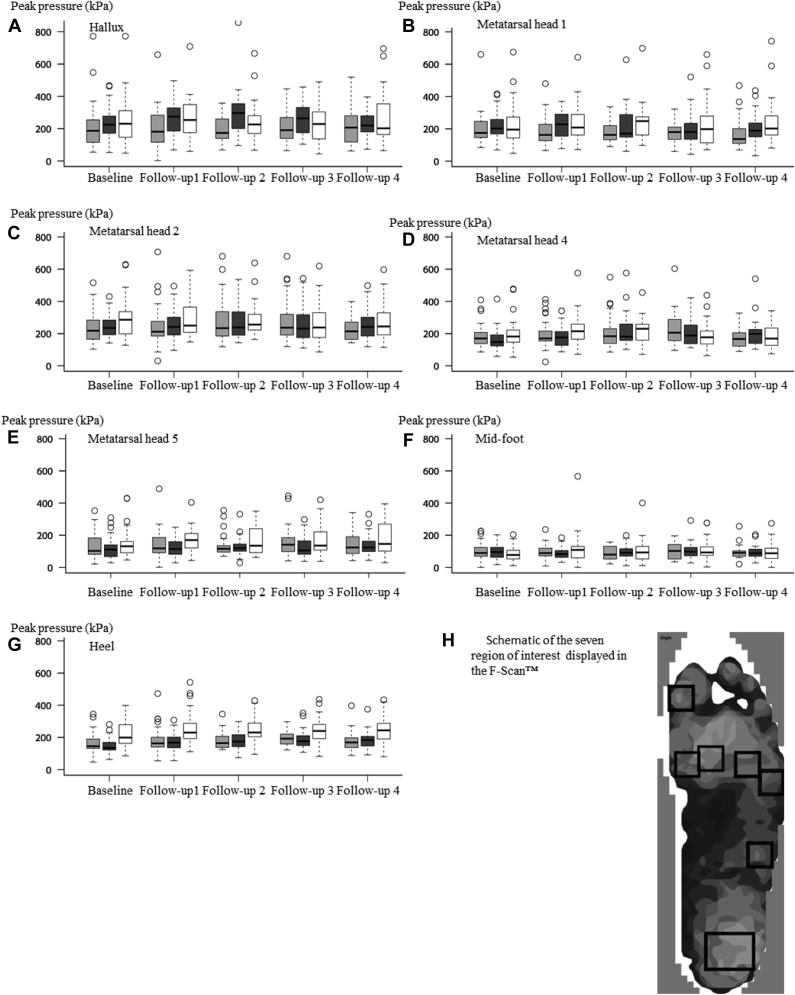
The F-Scan® 6.62 software has predefined boxes with analysis tools for seven regions of interest (ROI), which correspond to regions that are exposed to high levels of pressure during walking, i.e., the heel, lateral aspect of the mid-foot, metatarsal head 5 (MTH5), MTH4, MTH2, MTH1, and the hallux. The predefined boxes (3 × 4 cm at the heel region and 2 × 2 cm at all the other ROI) were manually positioned to cover the seven anatomic regions (Figure 3).
Figure 3.
Peak pressure in seven regions of interests A-G. For each region of interest, the peak pressures for three types of insoles are presented as a box plot. Gray boxes represent the 35 EVA insoles, black boxes the 55 EVA insoles, and white boxes the prefabricated insoles. The outliers (circles) represent high pressure levels and give evidence as to the significant inter-individual variation. For the heels, the pressures in the prefabricated insoles are higher than those in the custom-made 35 EVA and 55 EVA insoles at each follow-up (p < 0.001) H. Schematic of the seven regions of interests displayed in the F-Scan.
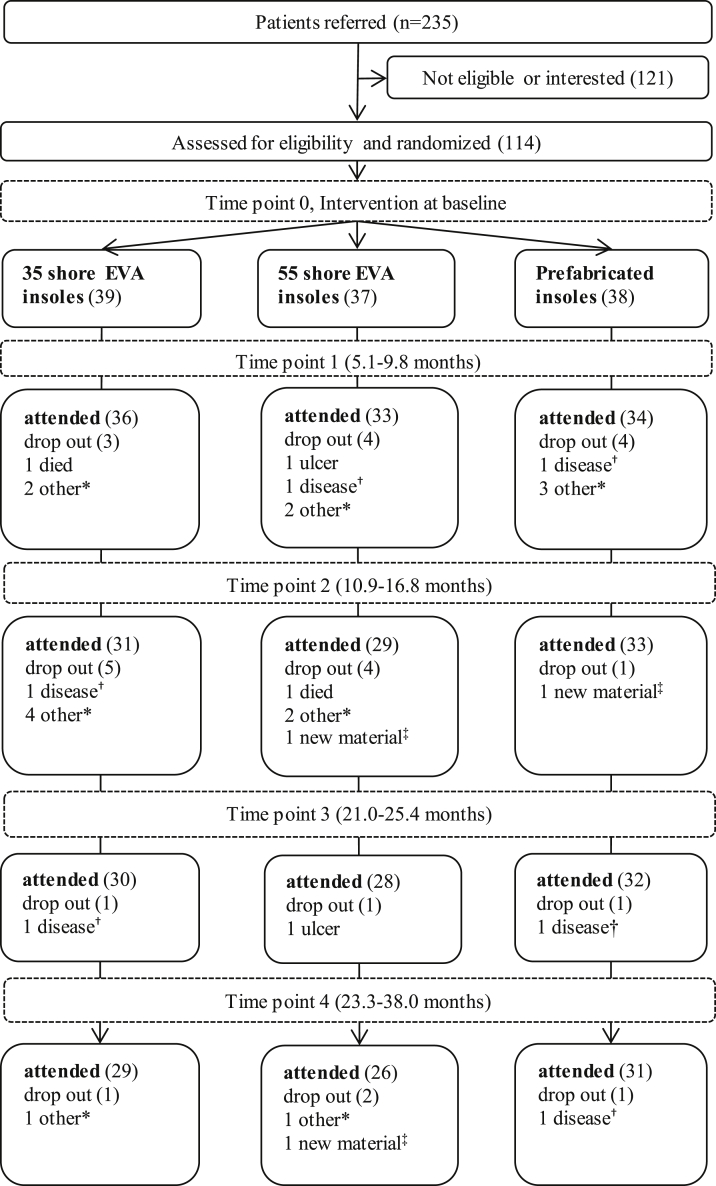
Five time-points were planned for the pressure measurements (baseline and four follow-ups at 6-month intervals). However, in reality, this interval varied between the patients, so the term “measurement time point” was used to reflect the time interval (Figure 2).
Figure 2.
Flow chart for the participants in the study and the reasons for study drop-outs. The “measurement time point” reflects the time interval and is reported as a range (minimum to maximum). The numbers of participants are presented in parentheses. Reasons for dropping out are explained as follows: *participant drop-out for personal reasons; †other disease made participation impossible; ‡ participant wanted to change material of the insoles or the participant was prescribed another insole material.
At each time-point, six walking trials, consisting of four to eight steps, were performed. One of the six trials was randomly selected for analysis. The first and last steps were excluded in the calculation of the average peak pressure for the trial. Three different variables describing different aspects of plantar pressure distribution were analyzed [1]: peak pressure (PP) [2]; maximum peak pressure (maxPP); and [3] pressure time integral (PTI). Peak pressure was defined as the maximum peak plantar pressure sensed for each cm2 in the positioned boxes per footstep, averaged over five to seven footsteps. The maxPP is the highest pressure sensed within each of the seven ROI over the same number of footsteps. The calculation PTI followed the equation: PTI = P1 × T1 + P2 × T2 + … PN × TN, where P1 is the total pressure present in the first frame of the stance, T1 is the duration (time) of the first frame of the stance, PN is the total pressure present in the last frame of the stance, and TN is the duration of the final frame of the stance (from F-Scan User Manual 6.62, Rev H). Stance number 3 was selected for the analysis of PTI, as measured in kiloPascals × second.
Participants
In total, 86 (75%) of the participants assessed at baseline completed the four follow-ups. At baseline, 31 (27%) were diagnosed with type 1 diabetes and 83 (73%) were diagnosed with type 2 diabetes, 62 (54%) were male and 52 (46%) were female, and the mean HbA1c (N = 106) was 6.4% ± 1.8 (46 mmol/mol).
At baseline, 43 (38%) of the participants had a loss of protective sensation, defined as a positive response to any of following tests: monofilament (18%); vibration (37%); proprioception (11%); or superficial (6%). Smoking was reported by 18% of the participants, and 6% used tobacco snuff. Overall, 65% of the participants were being treated for high blood pressure or heart disease. More than 70% of the participants in each group reported normal walking ability (79% in the 35 EVA insoles group; 76% in the 55 EVA insoles group; and 71% in the prefabricated insoles group). Most of the participants (97%; N = 111) used walking shoes with a semi-rigid outer sole. One participant in each group used shoes with a stiff rocker bottom sole. The baseline characteristics of the participants are presented in Table 1A, Table 1B.
Table 1A.
Baseline characteristics of the patients. Values shown for continuous variables are mean (SD)
| N | Age (years) | Female (%) | Diabetes type 1 (%) | Duration of diabetes (years) | BMI (kg/m2) | HbA1c (mol/mmol) | Neuropathy (%, N) | |
|---|---|---|---|---|---|---|---|---|
| 35 EVA | 39 | 58 (16.8) | 44 | 39 | 13 (13) | 28 (5) | 6.3 (0.9) | 38.5 (15) |
| 55 EVA | 37 | 57 (15) | 41 | 16 | 9 (7) | 28 (4) | 6.5 (2.6) | 35.1 (13) |
| Prefab | 38 | 59 (15) | 53 | 29 | 15 (12) | 28 (5) | 6.4 (1.7) | 37.5 (12) |
| Total | 114 | 58 (15) | 46 | 28 | 12 (11) | 28 (5) | 6.4 (1.8) | 37.7 (43) |
Table 1B.
Baseline peak pressures, maximal peak pressures, pressure time integrals and areas of seven regions of interests in the feet of the subjects
| Patients (N) | Hallux | Metatarsal head 1 | Metatarsal head 2 | Metatarsal head 4 | Metatarsal head 5 | Mid-foot | Heel | Area (cm2) | |
|---|---|---|---|---|---|---|---|---|---|
| Peak pressure in kPa | |||||||||
| 35 EVA | 39 | 200 (99) | 195 (95) | 255 (84) | 168 (70) | 141 (74) | 128 (69) | 175 (58) | 182 (22) |
| 55 EVA | 37 | 232 (130) | 211 (103) | 294 (83) | 155 (69) | 136 (102) | 109 (53) | 159 (57) | 177 (22) |
| Prefab | 38 | 206 (122) | 237 (145) | 292 (110) | 180 (75) | 151 (89) | 82 (49) | 237 (94) | 170 (19) |
| Total | 114 | 212 (118) | 214 (112) | 280 (94) | 168 (72) | 143 (88) | 107 (60) | 191 (79) | 176 (21) |
| Maximal peak pressure in kPa | |||||||||
| 35 EVA | 39 | 235 (109) | 255 (127) | 281 (95) | 197 (76) | 187 (92) | 176 (92) | 191 (61) | 182 (22) |
| 55 EVA | 37 | 284 (142) | 269 (142) | 322 (93) | 193 (84) | 179 (120) | 145 (66) | 176 (62) | 177 (22) |
| Prefab | 38 | 249 (153) | 301 (172) | 327 (127) | 213 (83) | 203 (122) | 120 (62) | 261 (98) | 170 (19) |
| Total | 114 | 256 (136) | 275 (148) | 310 (107) | 201 (81) | 190 (111) | 147 (78) | 209 (84) | 176 (21) |
| Pressure time integral in kPa × sec | |||||||||
| 35 EVA | 39 | 34 (19) | 39 (22) | 55 (24) | 46 (22) | 38 (19) | 43 (24) | 37 (14) | 180 (22) |
| 55 EVA | 37 | 36 (23) | 40 (24) | 61 (22) | 37 (16) | 33 (23) | 37 (22) | 32 (15) | 174 (22) |
| Prefab | 38 | 30 (14) | 46 (26) | 57 (21) | 50 (25) | 44 (25) | 31 (24) | 53 (28) | 167 (22) |
| Total | 114 | 33 (19) | 42 (24) | 58 (22) | 44 (22) | 38 (23) | 37 (24) | 41 (22) | 174 (22) |
Values shown for continuous variables are mean (SD).
BMI, body mass index; 35 EVA, 35 shore ethylene vinyl acetate-containing custom-made insoles; 55 EVA, 55 shore ethylene vinyl acetate-containing custom-made insoles; Prefab, prefabricated insoles.
While 570 pressure measurements were planned (five separate occasions for the 114 participants), 131 (23%) were lost due to patient drop-out (N = 90), patients not attending follow-ups (N = 38), and technical errors (N = 3). In the 35 EVA group, 52 measurements (27%) were missing, whereas in the 55 EVA group, 43 (23%) were missing and 36 (20%) were missing in the prefabricated group.
Two participants developed foot ulcers during the study and were excluded. The sites of these ulcers were the plantar aspect of MTH3 and digit three. Both of these participants were men who had been assigned to the 55 EVA group (Figure 2).
The patients who were not included in the study due to ineligibility or lack of interest (N = 121, 56% male, 44% female) were aged 60 ± 14 years (Figure 2).
The sample size (N = 114) was based on a pilot study that compared the differences in forefoot PP, measured with the F-Scan® in-shoe pressure measurement device, between custom-made insoles of the 35 EVA and 55 EVA types [33]. The calculation of sample size was based on an effect size in PP of 30 kPa, α = 0.05, power of 80%, and a dropout rate of 15%.
Statistical methods
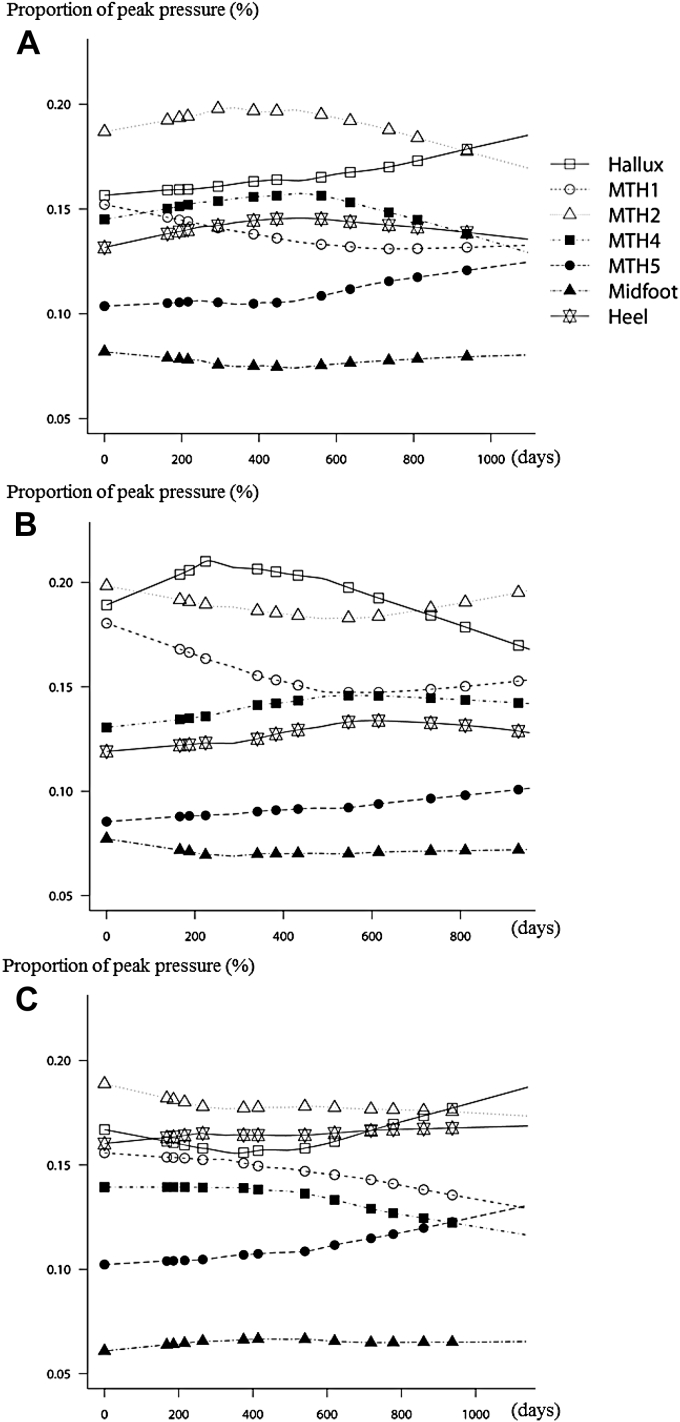
Several statistical analyzes of the data, using both explorative methods, such as graphs, and more formal approaches, such as tests and modeling, were performed. To avoid additional complications arising from the dependence upon measurements for the left and right foot, only the data for the right foot were used in all the analyses. An exploratory overview of the pressure data was made for each type of insole using the raw data for PP, maxPP, and PTI and the results are presented as mean (SD) for the seven ROI in Table 2. The raw date included the values obtained from all the follow-ups for each participant. To illustrate the distribution of PP values, we also created boxplots for the three types of insoles for each of individual time-points from baseline to the fourth follow-up (Figure 3). The proportions of load for the different ROI are shown in separate figures for each type of insole (Figure 4). The proportion of and change in load, during the study, were calculated for each ROI in relation to the sum of the peak pressures for all seven ROI. In a final exploratory analysis, a mean value for each type of insole was calculated.
Table 2.
Results of plantar pressure measurements recorderd in patients with diabetes including those with and without neuropathy
| Region of interest | 35 shore EVA insoles (N = 143) |
55 shore EVA insoles (N = 142) |
prefabricated insoles (N = 154) |
|||
|---|---|---|---|---|---|---|
| Mean (SD) | ±2SD | Mean (SD) | ±2SD | Mean (SD) | ±2SD | |
| Peak pressure in kPa | ||||||
| Hallux | 206 (118) | 187–226 | 259 (114) | 240-278 | 250 (137) | 229-272 |
| MTH1 | 189 (85) | 175–203 | 217 (95) | 201–232 | 238 (130) | 217–259 |
| MTH2 | 251 (118) | 231–270 | 259 (95) | 242–275 | 283 (119) | 264–302 |
| MTH4 | 197 (89) | 182–212 | 193 (86) | 179–207 | 202 (85) | 189–216 |
| MTH5 | 144 (83) | 130–157 | 127 (65) | 116–128 | 163 (88) | 149–177 |
| Mid-foot | 98 (47) | 91–106 | 95 (44) | 88–102 | 99 (69) | 88–110 |
| Heel | 178 (64) | 168–189 | 171 (57) | 162–181 | 242 (88) | 228–256 |
| Maximum peak pressure in kPa | ||||||
| Hallux | 257 (144) | 233–281 | 314 (133) | 292–336 | 316 (171) | 288–343 |
| MTH1 | 244 (109) | 227–262 | 270 (123) | 249–290 | 303 (161) | 277–328 |
| MTH2 | 288 (136) | 265–310 | 291 (103) | 274–309 | 327 (139) | 304–349 |
| MTH4 | 234 (103) | 217–251 | 230 (96) | 214–246 | 246 (103) | 230–263 |
| MTH5 | 190 (103) | 173–207 | 171 (81) | 158–185 | 225 (120) | 206–244 |
| Mid-foot | 137 (62) | 127–148 | 135 (62) | 125–145 | 145 (95) | 130–160 |
| Heel | 202 (76) | 189–215 | 193 (67) | 181–204 | 276 (102) | 260–293 |
| Pressure time integral in kPa × sec | ||||||
| Hallux | 36 (20) | 33–40 | 39 (21) | 36–43 | 37 (21) | 33–40 |
| MTH1 | 40 (20) | 37–43 | 42 (21) | 38–45 | 49 (28) | 45–54 |
| MTH2 | 54 (23) | 50–58 | 55 (23) | 51–59 | 59 (29) | 54–63 |
| MTH4 | 49 (21) | 46–53 | 46 (19) | 43–49 | 48 (19) | 45–51 |
| MTH5 | 39 (21) | 35–42 | 36 (20) | 33–39 | 45 (26) | 41–49 |
| Mid-foot | 32 (18) | 29–35 | 33 (19) | 30–36 | 29 (18) | 26–32 |
| Heel | 41 (19) | 38–44 | 35 (13) | 33–37 | 54 (23) | 50–58 |
The three variables of pressure, measured at time points 0–4, are grouped for each type of insole and presented as the means (SD) for the seven regions of interest. MTH1, metatarsal head 1; MTH2, metatarsal head 2; MTH4, metatarsal head 4; MTH5, metatarsal head 5. N, number of valid measurements.
Figure 4.
Proportion of peak pressure during the study period Patients with diabetes who were at risk of developing foot ulcers (N = 114) took part in an intervention with three types of insole: A, 35 shore EVA insoles; B, 55 shore EVA insoles; C, prefabricated insoles. The distributions and changes over time of the plantar peak pressures are presented as the proportion of load for each region of interests. The proportional loads are highest at metatarsal head 2 and the hallux. MTH1, metatarsal head 1; MTH2, metatarsal head 2; MTH4, metatarsal head 4; MTH5, metatarsal head 5.
After performing the exploratory part, we proceeded to compare the PP and PTI values for the 35 EVA and 55 EVA with the corresponding values for the prefabricated insoles using a mixed model. This model explicitly takes into account the dependence structure of the data (Table 3). The model had only one random effect, namely an intercept, with patients considered as the grouping factor. The “intercept” factor denotes a baseline, i.e., the estimated mean pressure for new prefabricated insoles. It included two main effects: type of insoles and time since the last change of insoles. This essentially means that we assume that there is a certain effect that different types of insoles have on pressure, although this effect may change in a linear fashion as the insoles get older and wear out. The resulting estimates of the main effects, as well as the corresponding standard deviations are presented in Table 3. The “Diff. 35 EVA” and “Diff. 55 EVA” parameters give the estimated difference in pressure between new custom-made and new prefabricated insoles. Finally, the term “Age of insoles” factor accommodates the possibility that the effect of insoles on plantar pressure may change as the insoles become worn-out.
Table 3.
Summary of the model with random intercepts. The response variables are plantar peak pressure and pressure time integral and the model includes two main effects: the type of insoles and ‘Age of insoles’ (days)
| Peak plantar pressure (kPa) |
Pressure time integral (kPa × sec) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Value | Std. Err. | DF | t-value | p-value | Value | Std. Err. | DF | t-value | p-value | |
| Hallux | ||||||||||
| (Intercept) | 248.84 | 16.66 | 323 | 14.94 | 0 | 35.91 | 2.67 | 323 | 13.43 | 0.00 |
| Diff. 35 EVA | −39.40 | 22.40 | 111 | −1.76 | 0.08 | −0.25 | 3.55 | 111 | −0.07 | 0.94 |
| Diff. 55 EVA | 9.92 | 22.68 | 111 | 0.44 | 0.66 | 2.75 | 3.59 | 111 | 0.77 | 0.44 |
| Age of insoles | 0.00 | 0.02 | 323 | −0.09 | 0.93 | 0.00 | 0.00 | 323 | 1.01 | 0.31 |
| Metatarsal head 1 | ||||||||||
| (Intercept) | 241.52 | 14.70 | 323 | 16.43 | 0.00 | 50.51 | 3.22 | 323 | 15.68 | 0.00 |
| Diff. 35 EVA | −40.32 | 19.96 | 111 | −2.02 | 0.05* | −7.55 | 4.37 | 111 | −1.73 | 0.09 |
| Diff. 55 EVA | −15.45 | 20.21 | 111 | −0.76 | 0.45 | −6.76 | 4.42 | 111 | −1.53 | 0.13 |
| Age of insoles | −0.02 | 0.01 | 323 | −1.82 | 0.07 | −0.01 | 0.00 | 323 | −1.78 | 0.08 |
| Metatarsal head 2 | ||||||||||
| (Intercept) | 291.11 | 15.05 | 323 | 19.34 | 0.00 | 58.57 | 3.29 | 323 | 17.82 | 0.00 |
| Diff. 35 EVA | −41.92 | 20.23 | 111 | −2.07 | 0.04* | −5.63 | 4.39 | 111 | −1.28 | 0.20 |
| Diff. 55 EVA | −29.26 | 20.48 | 111 | −1.43 | 0.16 | −5.16 | 4.44 | 111 | −1.16 | 0.25 |
| Age of insoles | −0.01 | 0.02 | 323 | −0.56 | 0.58 | 0.00 | 0.00 | 323 | 1.06 | 0.29 |
| Metatarsal head 4 | ||||||||||
| (Intercept) | 202.49 | 11.29 | 323 | 17.94 | 0.00 | 46.54 | 2.63 | 323 | 17.70 | 0.00 |
| Diff. 35 EVA | −10.28 | 15.17 | 111 | −0.68 | 0.50 | −0.09 | 3.53 | 111 | −0.02 | 0.98 |
| Diff. 55 EVA | −10.69 | 15.36 | 111 | −0.70 | 0.49 | −2.51 | 3.57 | 111 | −0.70 | 0.48 |
| Age of insoles | 0.00 | 0.01 | 323 | 0.26 | 0.80 | 0.01 | 0.00 | 323 | 2.61 | 0.01* |
| Metatarsal head 5 | ||||||||||
| (Intercept) | 156.00 | 10.97 | 323 | 14.22 | 0.00 | 41.95 | 3.01 | 323 | 13.95 | 0.00 |
| Diff. 35 EVA | −21.33 | 14.93 | 111 | −1.43 | 0.16 | −6.22 | 4.07 | 111 | −1.53 | 0.13 |
| Diff. 55 EVA | −35.07 | 15.12 | 111 | −2.32 | 0.02* | −9.14 | 4.12 | 111 | −2.22 | 0.03* |
| Age of insoles | 0.02 | 0.01 | 323 | 1.91 | 0.06 | 0.01 | 0.00 | 323 | 3.06 | 0.00** |
| Mid-foot | ||||||||||
| (Intercept) | 96.09 | 7.31 | 323 | 13.14 | 0.00 | 28.68 | 2.42 | 323 | 11.85 | 0.00 |
| Diff. 35 EVA | −0.55 | 9.87 | 111 | −0.06 | 0.96 | 3.06 | 3.25 | 111 | 0.94 | 0.35 |
| Diff. 55 EVA | −5.63 | 9.99 | 111 | −0.56 | 0.57 | 2.52 | 3.29 | 111 | 0.77 | 0.45 |
| Age of insoles | 0.01 | 0.01 | 323 | 1.27 | 0.20 | 0.00 | 0.00 | 323 | 0.70 | 0.48 |
| Heel | ||||||||||
| (Intercept) | 234.12 | 9.52 | 323 | 24.60 | 0.00 | 52.15 | 2.59 | 323 | 20.14 | 0.00 |
| Diff. 35 EVA | −63.59 | 12.80 | 111 | −4.97 | 0.00*** | −13.98 | 3.52 | 111 | −3.97 | 0.00*** |
| Diff. 55 EVA | −72.56 | 12.96 | 111 | −5.60 | 0.00*** | −20.10 | 3.56 | 111 | −5.64 | 0.00*** |
| Age of insoles | 0.02 | 0.01 | 323 | 2.50 | 0.01* | 0.01 | 0.00 | 323 | 3.61 | 0.00*** |
Intercept, the estimated mean pressure for new prefabricated insoles.
Diff. 35 EVA, the differences between the custom-made 35 EVA insoles and the prefabricated insoles. Diff. 55 EVA, the differences between the custom-made 55 EVA insoles and the prefabricated insoles. Std. Err, standard error; DF, degree of freedom.
*p < 0.05, **p < 0.005, ***p < 0.001.
Several sub-analyzes of the data were also made. In the first sub-analysis, the differences in total loaded plantar surface area (cm2) between the different insoles were evaluated. This evaluation was performed first using ANOVA, and then proceeding to pair-wise comparisons with t-tests. To account for multiplicity, Dunnett's multiplicity correction procedure was used. As the areas for different time-points for the same patient were expected to be dependent, this analysis was performed not on the raw data, but rather on the average of the loaded area (averaging for each patient over time). Thus, an additional response variable, termed “AVERAGE area,” was introduced.
In the second sub-analysis, differences in PP values for the participants with and without neuropathy were evaluated with a t-test. Following the reasoning outlined above, the response variable analyzed was “AVERAGE peak pressure” (averaging the PP for each patient over time). The calculation was done for all seven ROI.
The third sub-analysis was a further examination of the distribution of the data, made by examining measurement variations in five randomly selected participants. For these five participants, the pressure measurements for all 30 separate walks were available. Thus, the within-subject variation, “measurement error,” for each ROI at time-points 0–4 was compared with the between-subject variation, “population diversity.”
Finally, the participants with values of peak pressure that exceeded 500 kPa were examined separately.
The Microsoft Excel 2010, SPSS version 19, and R software packages were used for the statistical calculations.
Results
The results of the exploratory analysis for PP, maxPP, and PTI at baseline for the three types of insoles are presented in Table 1A, Table 1BA and B. The graphical presentation (Figure 3) shows that all three insoles produced a median pressure of approximately 200 kPa throughout the study.
The distributions of the proportion of peak pressure during the study for each ROI and for each type of insole are presented in the Figure 4. The highest peak pressures were at MTH2 and the hallux, while the lowest peak pressure was at the mid-foot for all the insole types. The redistribution properties over the PP over the 2 years were stable at the mid-foot, while the proportion of load on the distal area changed during the study period. The overall peak pressures for the custom-made 35 EVA and 55 EVA insoles were lower than those for the prefabricated insoles (35 EVA, 180 kPa (15% lower); 55 EVA, 189 kPa (10% lower); prefabricated, 211 kPa), as we ignored the differences in the seven ROI.
From the mixed models analysis (Table 3), a clear difference is evident only for the heel region between the two custom-made insoles and the prefabricated insoles. The estimated difference in PP between the EVA 35 insoles and the prefabricated insoles was 63 kPa, and the estimated difference between the 55 EVA insoles and the prefabricated insoles was 72 kPa (p < 0.001 for both comparisons). The estimated difference in PTI between the 35 EVA insoles and the prefabricated insoles was 14 kPa × sec, and the estimated difference between the 55 EVA insoles and the prefabricated insoles was 20 kPa × sec (p < 0.001). For such small p-values, the statistical significance would remain even if a multiplicity correction procedure (e.g. Bonferroni) would be performed.
The mixed model analysis also indicated possible differences in PP values between the prefabricated insoles and the EVA 35 insoles for MTH1 (p = 0.046) and MTH2 (p = 0.041), and a possible difference between the prefabricated insoles and EVA 55 insoles for MTH5 (p = 0.02). However, it should be borne in mind that these p-values are calculated without taking into account the issue of multiple hypotheses testing, and thus, although they indicate a difference, this cannot be seen as a confirmation of its existence.
Several of the mixed effects models (PP and PTI for the heel region, PTI for MTH4 and MTH5) also detected a possible effect of the “Age of insoles.” For all of these, the estimate of the effect was positive, supporting the intuitive belief that the pressures at some ROI should increase as the soles become older.
In the first sub-analysis of the total loaded plantar surface using ANOVA, the null hypothesis of no difference between the insoles could be rejected with a p-value of 0.028. The subsequent Dunnett's test gave p < 0.015 with an estimated difference of 12 cm2 when comparing EVA 35 insoles with the prefabricated insoles, and p = 0.174 (estimated difference of 8 cm2) when comparing EVA 55 insoles with the prefabricated insoles. Therefore, we conclude that the total loaded area differs between the EVA 35 and prefabricated insoles. The second sub-analysis showed no statistically significant differences between participants with and without neuropathy. The AVERAGE peak pressure was lower at the hallux region and higher at the heel for those participants with neuropathy (for the hallux, 215 kPa vs. 250 kPa, p < 0.063; for the heel, 202 kPa vs. 191 kPa, p = 0.399; values for ‘with neuropathy’ versus ‘without neuropathy’).
The third sub-analysis of the variation (within-subject variation divided by between-subject variation, which we refer to as the “relative variance”) in PP values for the five participants' measurements (seven ROI at five time-points) showed variance of <20% in 74% (n = 26) of the measurements. Relative variance levels of >20% and <30% appeared in 20% (n = 7) and relative variance of >30% appeared in 6% (n = 2) of the measurements.
Finally, the subjects with extremely high PP levels under the sole of the foot (>500 kPa) were examined separately. Such high pressures were observed in six participants. By analyzing images of the plantar surface in these cases, calluses, thin fat pads, and foot deformities were identified and found to correspond to the areas with PP values >500 kPa.
Patient compliance with the insoles was reported, with a mean score of 79 on the 0–100 analogue scale (N = 75) at the final follow-up (for the 35 EVA, 55 EVA, and prefabricated insoles groups: 73, 81, and 84, respectively). The satisfaction level was 85 (for the 35 EVA, 55 EVA, and prefabricated insoles groups: 86, 87, and 81, respectively). Forty-nine (66%) of the participants reported having had access to foot care.
In total, 86 pairs of insoles were exchanged due to wear (49% of the replacements occurred in the 35 EVA group, 20% in 55 EVA group, and 31% in the control group). Forty-three percent (N = 49) of the participants used the original pair of assigned insoles throughout the study. The average life-time of the insoles per group, calculated as the mean number of days (SD), was 260 (252) days for the 35 EVA group, 327 (284) for the 55 EVA group, and 318 (278) days for the prefabricated insoles group. In all, 14 adjustments to insoles were made during the study. Ten adjustments were made in the 55 EVA group and two in each of the other groups. The adjustments made to insoles in the 55 EVA group were: lowering of the metatarsal bar (n = 5); addition of material beneath the insoles (n = 2); offloading a bony prominence at digit three (n = 1); and unspecified (n = 2). One insole had both an adjustment of a lower metatarsal bar and added lateral support. The adjustments made to insoles in the 35 EVA group involved the addition of material under the heel (n = 2). The adjustments made to the prefabricated insoles were: the addition material under the heel (n = 1); and unspecified (n = 1).
Discussion
The most important finding of the present study is the significantly lower pressure at the heel observed in the comparisons of the custom-made insoles with the prefabricated insoles. Both the PP and PTI analyzes of the heel confirmed this finding. Aging of the insoles also had an effect on the PP and PTI at this ROI.
The pressure redistribution capacities of custom-made insoles in the heel region assessed in the present study are in accordance with the previously described results of Bus et al. [28]. Pressure reduction in the heel region is probably due to the casting procedure, which entails tight molding that follows the contour of the heel. A three-dimensional view of a custom-made insole (Figure 1) shows a narrow heel width together with high edges, which retain the heel pad under the bony prominences of the calcaneus, thereby providing cushioning. Thus adjusting the prefabricated insoles with higher edges that are positioned tight to the heel can be assumed to improve the pressure reduction properties.
The overall peak pressures on the foot soles of the patients who wore custom-made insoles in our study were 180 kPa and 189 kPa. These pressures are comparable to the overall peak pressures reported by Ledoux et al. [34], who studied patients with diabetes with or without foot ulcers. They also used the F-Scan® in-shoe pressure measurement system and reported overall mean peak pressures of 194 kPa for patients without ulcers (N = 274) and 219 kPa for patients with foot ulcers (N = 47). In that study, 81% of the patients the ulcerated group had neuropathy, whereas 48% of the non-ulcer group had neuropathy. The patients with foot ulcers in the study of Ledoux et al. [34] had an overall peak pressure that was higher than the patients in the current study (none of whom had foot ulcers) who were provided with prefabricated insoles (211 kPa). However, the results of the overall peak pressure measurements might not be fully comparable, as definition of the total area analyzed was different than current study.
The clinically relevant reference value to avoid diabetic foot ulcers recurrence has been variously reported as 207 kPa (measured using the Pedar® system) and 291 kPa (measured with the Pliance® system) [29]. These values are similar to the peak pressures obtained for all three insoles in the present study (Table 2). However, comparisons of threshold values should be interpreted with care, due to differences between ROI and differences in applied technologies (e.g., spatial resolution, pressure range, sampling calibration procedure, and raw data pre-processing) between the Pedar®, Pliance®, and F-Scan® systems. The implication is that all three types of insoles possibly might reduce the pressure at the heel to a degree that prevents stress on the soft tissue. The issue as to whether or not differences in pressure distribution properties exist for the remaining six ROI analyzed here is not resolved in the present study.
Based on the results of the present study, we recommend that patients with diabetes should be given custom-made insoles when reduction of the peak pressure in the heel region is the primary goal. The current results can be generalized and are clinically applicable to patients with diabetes with or without neuropathy and without ulcers. It is assumed that walking shoes are used together with the insoles.
The second aim of the study was to explore the patterns of plantar pressure redistribution in the patients who wore the shoes with the different insoles. The proportion of the load shown in Figure 3 indicates that small changes occur over time in the seven ROI for all of the different insoles. The load on the forefoot is larger than that on the mid-foot. The main differences are in the heel region, with higher relative pressures for the prefabricated insoles than for the custom-made insoles. Differences between the insoles can be seen in the hallux region and the metatarsal heads. The reasons to the variation of pressure over time in these distal regions are not fully understood.
Three different pressure measurement outcomes were used in the present study, due to the lack of international consensus, to evaluate the different aspects of plantar pressure distribution. The PP variable and PTI are commonly applied in studies that use F-Scan® in-shoe pressure-measuring devices 27, 34. The maxPP parameter was added for descriptive purposes (Tables 1A and B and Table 2), although is omitted in the subsequent analyzes. The sub-analyzes of total loaded plantar area are presented for the reader to evaluate further the differences in contact between the foot and insoles for the different types of insoles.
Twenty-eight (25%) of the participants were lost to the final follow-up. They left the study due to personal reasons (N = 15), disease (N = 6), change of insoles (N = 3), death (N = 2), and the development of foot ulcers (N = 2). The missing pressure measurements (n = 90) are mainly due to drop-outs (69%). The high dropout rates (25%–50%) observed for patients with diabetes at risk of developing ulcers must be considered when designing future trials. Bus et al. [35], who followed patients with diabetes and a healed foot ulcers over 18 months, reported a drop-out rate of 47%.
The annual incidence of foot ulcers in the present study (0.9%) is low compared with previously those in published population-based studies from the UK (2%), and USA (3%) 36, 37. To evaluate the outcome of the yearly incidence of foot ulcers, a higher number of participants needs to be included in future studies.
In total, 14 adjustments to the insoles were made during the study. The 55 EVA insoles accounted for most (71%) of these adjustments. Overall, 43% of the participants did not change their shoe insoles during the entire study period. This result includes the participants who left the study before the last follow-up. It is noteworthy that the prefabricated and 35 EVA insoles had to be exchanged more frequently due to material fatigue. Surprisingly, the prefabricated insole had a longer life-span than the custom-made insoles. The life-span data show a large standard deviation, which is attributable to the extensive inter-subject variability; some participants exchanged their insoles frequently, while others used the originally assigned insoles for the entire duration of the study. The patient-reported outcomes reveal extensive use of the insoles and a high level of satisfaction among the participants, which are of importance for the prevention of diabetic foot ulcers [38], 39. At the point in time when the present study initiated objective estimates of compliance were not available, therefore we used a visual analogue scale. To our knowledge, the first report of an objective instrument for adherence to footwear was presented in Year 2012 [40].
Prevention strategies to avoid foot ulcers recommend that foot care be included. In the present study, one-third of the patients had not received any foot care. Based on our result it is advisable to combine insole use with routine foot care.
Limitations
The study showed a high level of variation for the PP, maxPP, and PTI values (Table 1A, Table 1BA and B and Table 2). These variations are similar to those reported in other studies 23, 24, 25, 29, although the reasons for the variations are not fully understood. The current analysis of five randomly selected participants confirms the large variations, even though the measurements were recorded under stable and similar conditions for all the participants. All the participants walked on a level floor and used the same type of shoe during the assessments. The variability observed in the present study may be related to the complicated, dynamic nature of walking and the physiologic factors associated with diabetes 41, 42. The variations in the pressure values can be attributed to a combination of the participant's adjustment and co-ordination in order to maintain balance, some technical error, and a wrinkled sock or sensor. The sensors used at each time-point were not assigned to a specific individual, possibly adding to the within-subject variation. The sensor had the following technical properties: linearity, ≤3%, according to the end-point linearity of the transducer; hysteresis, <4.5% of full-scale output; and repeatability, ≤3.5%, giving reasonable accuracy. To achieve a high level of accuracy, equilibration is recommended before calibration is performed [43]. However, at the time that this study started, this was not a recommended procedure, and walking calibration was used to ensure appropriate accuracy.
In the sub-analysis of the six participants, who had PP values >500 kPa, some explanations for the large variation were found. During analysis of the photographs of the plantar surfaces of the feet of these participants, we noted the presence of atrophied fat pads, foot deformities, and calluses. Correlations between foot deformities, a thin fat pad, and gait deviation have previously been detected, although this remains a topic for further investigation 15, 44. Only one of the five walking trials performed at each follow-up was analyzed due to the time-consuming manual procedure required to translate the data into numerical form. The availability of appropriate software, including the possibility to run the analysis automatically, would allow processing of all the data on plantar pressures and would decrease the variation. This would facilitate the detection of differences in the pressure redistribution properties in regions other than the heel. A limitation of the present study is that in-shoe pressure measurements were not performed when the patients walked with their assigned shoes without any insoles. Finally, barefoot measurements were not included in the present study. This was because the participants were recommended not to walk barefoot, as this might entail a risk for trauma. Nevertheless, it is true that barefoot measurements are essential for evaluation of the effectiveness of the intervention.
Measurement errors
Attempts to capture dynamic walking and the properties of three-dimensional insoles in a longitudinal study have inherent limitations, which might lead to measurement errors. First, the in-shoe pressure measurement only registers two-dimensional forces between the foot sole and the shaped insoles; shear forces are not recorded [45]. Second, equilibration and calibration procedures might affect the accuracy of subsequent measurements and is a topic for further investigation. The intra- or inter-subject variations in gait velocity, as well as the types of hosiery used were not strictly controlled during the study.
Conclusions
We conclude that for patients with diabetes who are at risk for foot ulcers, custom-made insoles used in combination with stable walking shoes result in lower pressure levels at the heel region (one of the seven regions of interest investigated), as compared with walking shoes with the type of prefabricated insoles that were tested in the present study. The observed variability of the measurements makes it difficult to define systematic differences in plantar pressure for the other six regions of interest of the foot. The levels of self-reported satisfaction and usage of the insoles were high, and the insoles retained their pressure redistribution properties over a long time, so few adjustments were needed.
Acknowledgments
No potential conflicts of interest relevant to this article are reported. The authors thank all co-workers at the Department of Prosthetics and Orthotics, Sahlgrenska University Hospital, Gothenburg for all help and assistance during this study.
Ulla Hellstrand Tang (U.H.T) is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analyzes. U.H.T. designed the study, researched the data, contributed to discussions, and wrote the manuscript. R.Z and R.T designed the study, researched the data, contributed to discussions, and reviewed and edited the manuscript. V.L carried out statistical analyzes, contributed to discussions, and wrote the manuscript. K.H and J.K. contributed to discussions and reviewed and edited the manuscript.
The preliminary results of this study were presented in abstract form at the 6th Diabetic Foot Conference, Noordwijkerhout, The Netherlands, on May 11–14, 2011, the Nordisk Ortopedteknisk Konferens, Lilleström, Norway, on October 25–27, 2012, and the International Conference of Prosthetics & Orthotics, Hyderabad, India, on February 4–7, 2013. Funding for the study was obtained: the Promobilia Foundation; Skobranschens Utvecklingsfond Foundation; the Local Research and Development Board for Gothenburg and Södra Bohuslän grant number VGFOUGSB-9725; the Felix Neubergh Foundation; the Gunnar Holmgrens Minne Foundation, the Fund for Rehabilitering och Medicinsk Forskning, and the IngaBritt and Arne Lundbergs Research Foundation.
Footnotes
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/3.0/).
References
- 1.Danaei G., Stevens G.A., Rao M., Ali M.K., Riley L.M., Robinson C.A. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2·7 million participants. The Lancet. 2011;378(9785):31–40. doi: 10.1016/S0140-6736(11)60679-X. [DOI] [PubMed] [Google Scholar]
- 2.Adler A.I., Boyko E.J., Ahroni J.H., Smith D.G. Lower-extremity amputation in diabetes. The independent effects of peripheral vascular disease, sensory neuropathy, and foot ulcers. Diabetes Care. 1999;22(7):1029–1035. doi: 10.2337/diacare.22.7.1029. [DOI] [PubMed] [Google Scholar]
- 3.Pecoraro R.E., Reiber G.E., Burgess E.M. Pathways to diabetic limb amputation: basis for prevention. Diabetes Care. 1990;13(5):513–521. doi: 10.2337/diacare.13.5.513. [DOI] [PubMed] [Google Scholar]
- 4.Larsson J., Apelqvist J. Towards less amputations in diabetic patients: Incidence, causes, cost, treatment, and prevention—a review. Acta Orthop Scand. 1995;66(2):181–192. doi: 10.3109/17453679508995520. [DOI] [PubMed] [Google Scholar]
- 5.Bakker K., Apelqvist J., Schaper N.C. Practical guidelines on the management and prevention of the diabetic foot 2011. Diabetes Metab Res Rev. 2012;28:225–231. doi: 10.1002/dmrr.2253. [DOI] [PubMed] [Google Scholar]
- 6.Apelqvist J., Larsson J., Agardh C.-D. The influence of external precipitating factors and peripheral neuropathy on the development and outcome of diabetic foot ulcers. J Diabet Complications. 1990;4(1):21–25. doi: 10.1016/0891-6632(90)90060-i. [DOI] [PubMed] [Google Scholar]
- 7.Apelqvist J., Larsson J. What is the most effective way to reduce incidence of amputation in the diabetic foot. Diabetes Metab Res Rev. 2000;16(Suppl. 1):S75–S83. doi: 10.1002/1520-7560(200009/10)16:1+<::aid-dmrr139>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 8.Abbott C.A., Vileikyte L., Williamson S., Carrington A.L., Boulton A.J. Multicenter study of the incidence of and predictive risk factors for diabetic neuropathic foot ulceration. Diabetes Care. 1998;21(7):1071–1075. doi: 10.2337/diacare.21.7.1071. [DOI] [PubMed] [Google Scholar]
- 9.Kärvestedt L., Mårtensson E., Grill V., Elofsson S., von Wendt G., Hamsten A. The prevalence of peripheral neuropathy in a population-based study of patients with type 2 diabetes in Sweden. J Diabet Complications. 2011;25(2):97–106. doi: 10.1016/j.jdiacomp.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 10.Lavery L.A., Armstrong D.G., Wunderlich R.P., Tredwell J., Boulton A.J. Predictive value of foot pressure assessment as part of a population-based diabetes disease management program. Diabetes Care. 2003;26(4):1069–1073. doi: 10.2337/diacare.26.4.1069. [DOI] [PubMed] [Google Scholar]
- 11.Abbott C.A., Garrow A.P., Carrington A.L., Morris J., Van Ross E.R., Boulton A.J. Foot ulcer risk is lower in South-Asian and african-Caribbean compared with European diabetic patients in the U.K.: the North-West diabetes foot care study. Diabetes Care. 2005;28(8):1869–1875. doi: 10.2337/diacare.28.8.1869. [DOI] [PubMed] [Google Scholar]
- 12.Lavery L.A., Armstrong D.G., Vela S.A., Quebedeaux T.L., Fleischli J.G. Practical criteria for screening patients at high risk for diabetic foot ulceration. Arch Intern Med. 1998;158(2):157–162. doi: 10.1001/archinte.158.2.157. [DOI] [PubMed] [Google Scholar]
- 13.Crawford F., Inkster M., Kleijnen J., Fahey T. Predicting foot ulcers in patients with diabetes: a systematic review and meta-analysis. QJM. 2007;100:65–86. doi: 10.1093/qjmed/hcl140. [DOI] [PubMed] [Google Scholar]
- 14.Cavanagh P., Bus S. Off-loading the diabetic foot for ulcer prevention and healing. J Vasc Surg. 2010;52(3 Suppl.):37S–43S. doi: 10.1016/j.jvs.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 15.Ahroni J.H., Boyko E.J., Forsberg R.C. Clinical correlates of plantar pressure among diabetic veterans. Diabetes Care. 1999;22(6):965–972. doi: 10.2337/diacare.22.6.965. [DOI] [PubMed] [Google Scholar]
- 16.Boulton A.J., Vileikyte L., Ragnarson-Tennvall G., Apelqvist J. The global burden of diabetic foot disease. Lancet. 2005;366(9498):1719–1724. doi: 10.1016/S0140-6736(05)67698-2. [DOI] [PubMed] [Google Scholar]
- 17.Ragnarson Tennvall G., Apelqvist J. Health-related quality of life in patients with diabetes mellitus and foot ulcers. J Diabetes Complications. 2000;14(5):235–241. doi: 10.1016/s1056-8727(00)00133-1. [DOI] [PubMed] [Google Scholar]
- 18.Ragnarson Tennvall G., Apelqvist J. Health-Economic Consequences of Diabetic Foot Lesions. Clin Infect Dis. 2004;39(S2):132–139. doi: 10.1086/383275. [DOI] [PubMed] [Google Scholar]
- 19.Bus S.A. Priorities in offloading the diabetic foot. Diabetes Metab Res Rev. 2012;28(Suppl. 1):54–59. doi: 10.1002/dmrr.2240. [DOI] [PubMed] [Google Scholar]
- 20.Paton J., Bruce G., Jones R., Stenhouse E. Effectiveness of insoles used for the prevention of ulceration in the neuropathic diabetic foot: a systematic review. J Diabet Complications. 2009;25(1):52–62. doi: 10.1016/j.jdiacomp.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 21.Healy A., Naemi R., Chockalingam N. The effectiveness of footwear as an intervention to prevent or to reduce biomechanical risk factors associated with diabetic foot ulceration: a systematic review. J Diabetes Complications. 2013;27(4):391–400. doi: 10.1016/j.jdiacomp.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 22.Giacomozzi C., Keijsers N., Pataky T., Rosenbaum D. International scientific consensus on medical plantar pressure measurement devices: technical requirements and performance. Ann Ist Super Sanita. 2012;48(3):259–271. doi: 10.4415/ANN_12_03_06. [DOI] [PubMed] [Google Scholar]
- 23.Arts M.L.J., Waaijman R., de Haart M., Keukenkamp R., Nollet F., Bus S.A. Offloading effect of therapeutic footwear in patients with diabetic neuropathy at high risk for plantar foot ulceration. Diabet Med. 2012;29(12):1534–1541. doi: 10.1111/j.1464-5491.2012.03770.x. [DOI] [PubMed] [Google Scholar]
- 24.Owings T.M., Woerner J.L., Frampton J.D., Cavanagh P.R., Botek G. Custom therapeutic insoles based on both foot shape and plantar pressure measurement provide enhanced pressure relief. Diabetes care. 2008;31(5):839–844. doi: 10.2337/dc07-2288. [DOI] [PubMed] [Google Scholar]
- 25.Guldemond N.A., Leffers P., Schaper N.C., Sanders A.P., Nieman F., Willems P. The effects of insole configurations on forefoot plantar pressure and walking convenience in diabetic patients with neuropathic feet. Clin Biomech (Bristol Avon) 2007;22(1):81–87. doi: 10.1016/j.clinbiomech.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 26.Viswanathan V., Madhavan S., Gnanasundaram S., Gopalakrishna G., Das B.N., Rajasekar S. Effectiveness of different types of footwear insoles for the diabetic neuropathic foot: a follow-up study. Diabetes Care. 2004;27(2):474–477. doi: 10.2337/diacare.27.2.474. [DOI] [PubMed] [Google Scholar]
- 27.Paton J.S., Stenhouse E.A., Bruce G., Zahra D., Jones R.B. A comparison of customised and prefabricated insoles to reduce risk factors for neuropathic diabetic foot ulceration: a participant-blinded randomised controlled trial. J Foot Ankle Res. 2012;5(1):1–11. doi: 10.1186/1757-1146-5-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bus S.A., Ulbrecht J.S., Cavanagh P.R. Pressure relief and load redistribution by custom-made insoles in diabetic patients with neuropathy and foot deformity. Clin Biomech (Bristol, Avon) 2004;19(6):629–638. doi: 10.1016/j.clinbiomech.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 29.Owings T.M., Apelqvist J., Stenström A., Becker M., Bus S.A., Kalpen A. Plantar pressures in diabetic patients with foot ulcers which have remained healed. Diabet Med. 2009;26(11):1141–1146. doi: 10.1111/j.1464-5491.2009.02835.x. [DOI] [PubMed] [Google Scholar]
- 30.Västra Götalandsregionen . 2008. Regionalt vårdprogram/riklinjer. Diabetesfoten.https://alfresco.vgregion.se/alfresco/service/vgr/storage/node/content/3132?a=false&guest=true&native=true Available from: [Google Scholar]
- 31.Boulton A.J.M., Armstrong D.G., Albert S.F., Frykberg R.G., Hellman R., Kirkman M.S. Comprehensive Foot Examination and Risk Assessment: a report of the Task Force of the Foot Care Interest Group of the American Diabetes Association, with endorsement by the American Association of Clinical Endocrinologists. Diabetes Care. 2008;31(8):1679–1685. doi: 10.2337/dc08-9021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hsiao H., Guan J., Weatherly M. Accuracy and precision of two in-shoe pressure measurement systems. Ergonomics. 2002;45(8):537–555. doi: 10.1080/00140130210136963. [DOI] [PubMed] [Google Scholar]
- 33.Zügner R., Tranberg R., Wensby L., Millesten B., Kärrholm J. How does two custom moulded insoles influence the diabetic patient? A comparison between insoles in different stiffness. International Conference Society of Prosthetics and Orthotics Vancouver. Canada. 2007 [Google Scholar]
- 34.Ledoux W.R., Shofer J.B., Cowley M.S., Ahroni J.H., Cohen V., Boyko E.J. Diabetic foot ulcer incidence in relation to plantar pressure magnitude and measurement location. J Diabetes Complications. 2013;27(6):621–626. doi: 10.1016/j.jdiacomp.2013.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bus S.A., Waaijman R., Arts M., de Haart M., Busch-Westbroek T., van Baal J. Effect of custom-made footwear on foot ulcer recurrence in Diabetes: a multicenter randomized controlled trial. Diabetes Care. 2013;36(12):4109–4116. doi: 10.2337/dc13-0996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Abbott C.A., Johnson K.E., Ryder C.H., Torkington R., Van Ross E.R.E., Whalley A.M. The North-West Diabetes Foot Care Study: incidence of, and risk factors for, new diabetic foot ulceration in a community-based patient cohort. Diabet Med. 2002;19(5):377. doi: 10.1046/j.1464-5491.2002.00698.x. [DOI] [PubMed] [Google Scholar]
- 37.Boyko E.J., Ahroni J.H., Stensel V., Forsberg R.C., Davignon D.R., Smith D.G. A prospective study of risk factors for diabetic foot ulcer. The Seattle Diabetic Foot Study. Diabetes Care. 1999;22(7):1036–1042. doi: 10.2337/diacare.22.7.1036. [DOI] [PubMed] [Google Scholar]
- 38.Waaijman R, Keukenkamp R, de Haart M, Polomski WP, Nollet F, Bus SA. Adherence to wearing prescription custom-made footwear in patients with diabetes at high risk for plantar foot ulceration. Diabetes Care 13:1613–1618 [DOI] [PMC free article] [PubMed]
- 39.Chantelau E., Haage P. An audit of cushioned diabetic footwear - relation to patient compliance. Diabet Med. 1994;11(1):114–116. doi: 10.1111/j.1464-5491.1994.tb00240.x. [DOI] [PubMed] [Google Scholar]
- 40.Bus S.A., Waaijman R., Nollet F. New monitoring technology to objectively assess adherence to prescribed footwear and assistive devices during ambulatory activity. Arch Phys Med Rehabil. 2012;93(11):2075–2079. doi: 10.1016/j.apmr.2012.06.019. [DOI] [PubMed] [Google Scholar]
- 41.Cavanagh P.R., Morag E., Boulton A.J.M., Young M.J., Deffner K.T., Pammer S.E. The relationship of static foot structure to dynamic foot function. J Biomech. 1997;30(3):243–250. doi: 10.1016/s0021-9290(96)00136-4. [DOI] [PubMed] [Google Scholar]
- 42.Ko M., Hughes L., Lewis H. Walking speed and peak plantar pressure distribution during barefoot walking in persons with diabetes. Physiother Res Int. 2012;17(1):29–35. doi: 10.1002/pri.509. [DOI] [PubMed] [Google Scholar]
- 43.Giacomozzi C. Appropriateness of plantar pressure measurement devices: a comparative technical assessment. Gait Posture. 2010;32(1):141–144. doi: 10.1016/j.gaitpost.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 44.Bus S.A., Maas M., de Lange A., Michels R.P., Levi M. Elevated plantar pressures in neuropathic diabetic patients with claw/hammer toe deformity. J Biomech. 2005;38(9):1918–1925. doi: 10.1016/j.jbiomech.2004.07.034. [DOI] [PubMed] [Google Scholar]
- 45.Spooner S.K., Smith D.K., Kirby K.A. In-shoe pressure measurement and foot orthosis research: a giant leap forward or a step too far? J Am Podiatr Med Assoc. 2010;100(6):518–529. doi: 10.7547/1000518. [DOI] [PubMed] [Google Scholar]