Abstract
Ankle impingement syndromes encompass a broad spectrum of post-traumatic and chronic degenerative changes that present with pain on specific movements about the ankle joint. Both amateur and professional athletes are disproportionately affected by these conditions, and while conservative measures can potentially treat an impingement syndrome, definitive therapy is often alleviated surgically. Imaging (including conventional radiography, ultrasound, CT and MRI) plays an invaluable role in the diagnosis and pre-surgical work-up. An anatomically based classification system is useful in these syndromes, as the aetiology, sites of pathology and preferred treatment methods are similarly based on anatomic locations about the ankle. This review focuses on the anatomic locations, pathophysiology, imaging considerations and brief discussion of therapies for each of the major anatomic ankle impingement syndromes.
INTRODUCTION
Ankle impingement syndromes are common and important post-traumatic causes of morbidity in athletes, both professional and amateur.1–3 An ankle impingement syndrome is characterized by a limited range of motion and pain when performing specific movements about the joint and often in a load-bearing position. The aetiology and pathogenesis can be quite varied. In general, the diagnosis of ankle impingement is clinical, with supporting information provided by radiographs and more advanced imaging (CT, MRI and ultrasound),3–6 which can help further elucidate the anatomic mechanism of impingement, localize pathology to guide diagnostic and therapeutic injections and assist with pre-surgical planning.
Given the breadth of causative mechanisms and preferred treatment, the ankle joint can be subsegmented into anatomic regions: anteromedial, anterior, anterolateral, posteromedial and posterior. Another less common impingement syndrome about the ankle is the extra-articular lateral hindfoot or subfibular impingement syndrome. In general, the aetiology of impingement can be due to post-traumatic synovitis, malunion of fracture, scarring, recurrent sprains or other osseous causes.2 Depending on the morbidity and imaging findings, treatment is initially accomplished conservatively, but open surgical and/or arthroscopic approaches have proven to have a safe and efficacious role.7–9
The goal of this article was to review the relevant anatomy of the different compartments, describe the mechanisms of injury with common imaging findings, differential diagnoses when applicable and to review the different treatments options for ankle impingement syndromes.
ANTEROLATERAL IMPINGEMENT
Anatomic region
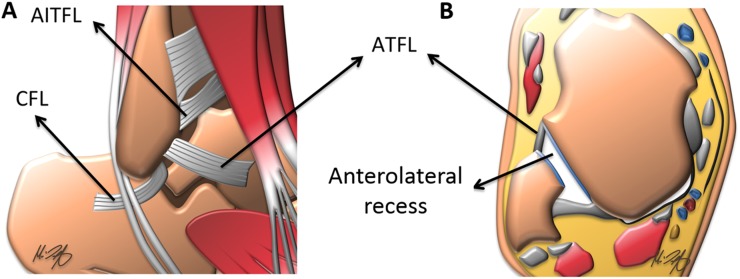
The anterolateral impingement syndrome is caused by obstruction of the so-called anterolateral gutter (ALG) or recess. This pyramidal space is formed medially by the tibia, laterally by the fibula, superiorly by the anteroinferior tibiofibular ligament (AITFL), inferiorly by the calcaneofibular ligament and anteriorly by the anterior talofibular ligament (ATFL) and joint capsule (Figure 1).
Figure 1.
Anatomic illustrations describing normal ligaments and the anterolateral recess: (a) an illustration as seen from a lateral view; (b) an illustration in the axial plane. AITFL, anteroinferior tibiofibular ligament; ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament.
This potential space may contain some joint fluid in asymptomatic individuals; however, a synovial reaction or debris can indicate pathology.10 During normal dorsiflexion, the anterolateral border of the talus extends into the anterolateral recess and its obstruction by abnormal bony or soft-tissue structures in this recess is responsible for the clinical finding of limited dorsiflexion.
Pathogenesis of anterolateral ankle impingement
The anterolateral impingement syndrome is characterized by localized pain during internal/external rotation with limited dorsiflexion. Clinical examination has been reported with 95% sensitivity and 75% specificity in detecting impingement.11 The most common ankle injury is a sprain of the ATFL, which typically results from a plantar flexion/inversion mechanism,12,13 and impingement is an uncommon sequela (occurring in approximately 2% of cases).14 A robust haemarthrosis and resultant synovitis can occur after injury. Over time, this can coalesce into a triangular or meniscoid hyalinized fibroid mass within the ALG.15
A less common cause of anterolateral ankle impingement is thickening of a portion of the inferior aspect of the AITFL.16 Although initially described as an “accessory” ligament, this band was recognized by Bassett et al1 in 1990 to be part of the AITFL proper. Although not truly its own ligament, this distinct band carries the name “Bassett's ligament” in the literature.17 In subsequent cadaver studies, this band was seen in nearly the entire population.16,18
Other causes of impingement are small ganglia, anterolateral tibial plafond spurs/ossicles, avulsed osseous fragments and syndesmotic ligament complex injury. Osteochondral injury to the anterolateral talar dome may be present, reported to occur in 17% of cases.19 Important differential considerations that may present similarly include: sinus tarsi syndrome, peroneal tendon subluxation or injury, tarsal coalition and osteoarthrosis.20
Imaging characteristics
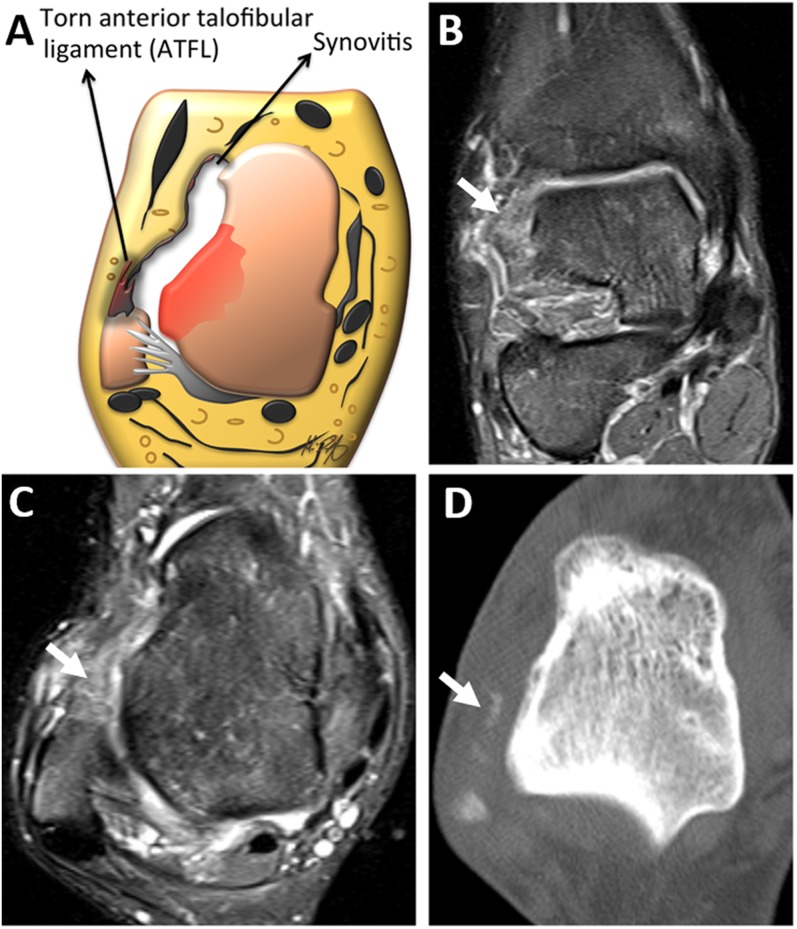
Often times, the initial imaging study is the conventional weight-bearing set of ankle radiographs. While limited in sensitivity and specificity for impingement, radiographs can be useful to demonstrate osseous bodies/fragments or osteophytes projecting over the ALG or the anterolateral tibial plafond.21 CT can also be utilized for the evaluation of bony intra-articular fragments or osteophytes, but with limited evaluation of the associated soft tissues (Figure 2). Ultrasonography has additionally been evaluated with possible utility in directing diagnostic and therapeutic corticosteroid injection.5 In addition, ultrasound has the ability to add assistance in diagnosis by utilizing dynamic techniques.
Figure 2.
Anterolateral impingement: (a) an illustration in the axial plane of an injured anterior talofibular ligament (ATFL) with associated synovitis. (b) Coronal and (c) axial fluid-sensitive MR images are showing a distinct hyperintense soft-tissue mass in the anterolateral recess (arrows), which is corresponding to an early meniscoid lesion in the setting of a chronically injured ATFL. (d) An axial CT image in the same patient is showing small calcified bodies embedded in the synovial hypertrophy within the anterolateral recess (arrow).
The main workhorse in imaging the ALG remains MRI. With exquisite soft-tissue contrast, MRI is capable of not only identifying a space-occupying lesion, it can often further evaluate the nature of the lesion. Early reports showed limited utility of MRI in the absence of a joint effusion.11 However, recent reports have shown a sensitivity of 83%, specificity of 78.6% and accuracy of 78.9% for the diagnosis of anterolateral impingement.22 MRI is capable of identifying small avulsed fragments and ligamentous abnormalities (notably the ATFL and AITFL) (Figures 2 and 3). The use of i.v. gadolinium-based contrast agents has been studied with enhancement of the surrounding synovial reaction.23 In that study, use of i.v. gadolinium with a fat-suppressed three-dimensional fast spoiled gradient-echo sequence resulted in a sensitivity of 76.5%, specificity of 96.9% and accuracy of 94.4% for the diagnosis of soft-tissue impingement. In addition, intra-articular injection of a gadolinium agent has also been shown to be the most specific; but, given its invasive nature, it is not commonly acquired.2,24
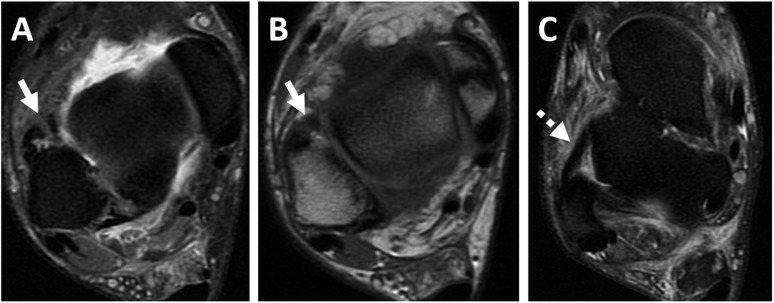
Figure 3.
Anterolateral impingement symptoms in a male with a previous syndesmotic ligament complex injury: (a) axial fluid-sensitive and (b) axial T1 weighted MR images are showing a thickened and irregular anteroinferior tibiofibular ligament (arrows). (c) An axial fluid-sensitive MR image is showing a thickened but intact anterior talofibular ligament (dashed arrow).
Anterolateral impingement syndrome treatment
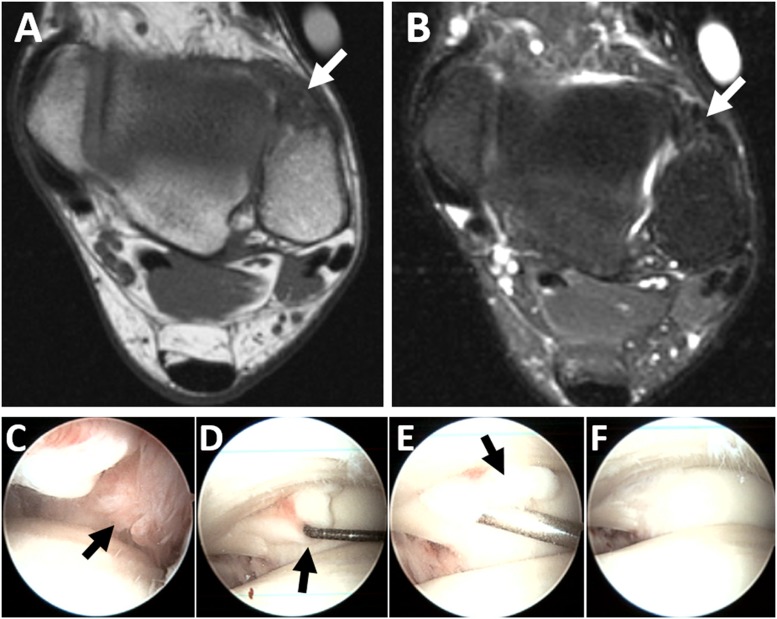
The initial treatment of choice for anterolateral impingement is generally conservative.11 Potential options include rest, physical therapy, ankle bracing or taping, shoe modification and local corticosteroid injection. Frequently, conservative treatment fails and surgery is recommended. Current guidelines consider arthroscopy as the gold standard surgical approach with its high safety and low complication rates (approximately 4%) (Figure 4).25 A recent meta-analysis of arthroscopic treatment for anterolateral impingement showed patient satisfaction ranging from 76% to 100%.26
Figure 4.
A 43-year-old male with a history of injury 2 years ago, now with anterolateral ankle pain limiting ankle movement consistent with anterolateral impingement: (a) axial T1 weighted and (b) fluid-sensitive MR images are showing a heterogeneous, predominantly hypointense mass at the anterior portion of the distal tibiofibular joint (white arrows). (c) Arthroscopic images are showing an incisural tissue in the syndesmosis that is being pulled on by the probe in (d) and shaved in (e) (black arrows). (f) After resection, a clean incisura is demonstrated.
ANTERIOR IMPINGEMENT SYNDROME
Anatomic region
Anatomically, the anterior aspect of the ankle is defined as the central portion of the ankle recess between the anterior tibial plafond and talar dome (Figure 5). Anterior impingement syndrome was first described in soccer players in 1943 by Morris27 and later by McMurray28 and named “athlete's ankle” and “footballers' ankle”. The prototypical patient who presents with anterior ankle impingement is a ballet dancer or soccer player who has anterior joint pain and limited dorsiflexion.
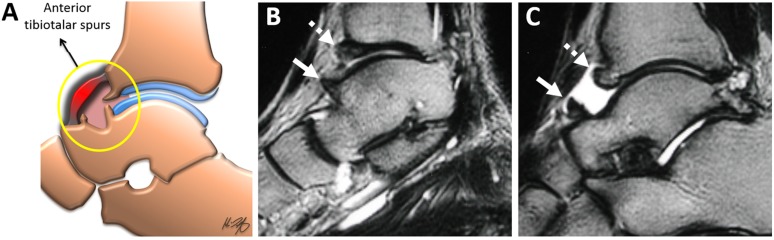
Figure 5.
Anterior ankle impingement: (a) an illustration in the mid-sagittal plane is demonstrating the involved anterior joint capsule (circle) with associated osteophytes from the anterior tibial plafond and anterior talar neck. (b, c) Sagittal fluid-sensitive MR images are showing a superior talar neck (arrows) and anterior tibial osteophytes (dashed arrows) in a male with anterior ankle impingement symptoms.
Pathogenesis of anterior ankle impingement
Initially, it was thought that the anterior ankle impingement was caused by plantar flexion of the tibiotalar joint with repetitive traction to the anterior joint capsule forming anterior tibiotalar osteophytes (traction spurs).29 However, cadaveric and arthroscopic evaluations suggest direct microtrauma to the talus and tibia as the aetiology.17,29,30 The natural course of this repetitive microtrauma is to form osseous spurs (Figure 5).29,31 These spurs can cause impingement through a Cam-type mechanism.32 However, it should also be noted that osteophyte formation is common in asymptomatic ballet dancers and soccer players.33,34
Much like the anterolateral impingement syndrome, this reactive process can cause irritation of the capsule and lead to a synovial inflammatory response, which in itself can cause pain and can also lead to the formation of fibrous bands.29,35 These bands can further limit dorsiflexion. A differential diagnosis may include tendon sheath rupture, tenosynovitis, synovial cyst rupture or a ganglion cyst.
Imaging characteristics
While anterior impingement syndrome remains chiefly a clinical diagnosis, radiography can have an important role. Initial evaluation typically begins with ankle radiographs, which may demonstrate anterior tibial and talar neck osteophytes. CT may further be able to localize the osteophytes and assist in pre-surgical planning.
Further evaluation can be performed with MRI, which can help localize the bone spurs and further characterize the synovial thickening.36 MRI can also be particularly useful to visualize intra-articular fibrous bands and identify soft-tissue pathology, if present. A prospective study evaluating MRI in the setting of chronic ankle pain noted only modest sensitivity and specificity for anterior tibial osteophytes (67% and 78%, respectively), although it had high a sensitivity (89%) for synovitis, capsular thickening, scar and granulation tissue.36 Generally, indirect arthrography (i.v. gadolinium-based contrast material injection followed by 10 min of physical activity) has a marginal additional benefit, except in specific situations, such as poor distention of the joint with fluid. Finally, in approximately 57% of patients, extra-articular causes of pain were discovered, which eliminated the need for arthroscopy.36
Treatment for anterior ankle impingement syndrome
As with anterolateral ankle impingement, conservative measures are employed initially. Unfortunately, these measures frequently fail to relieve symptoms.26 Open surgical techniques have been used with moderate success.37,38 More recently, there has been a move to the arthroscopic technique (Figure 6).39
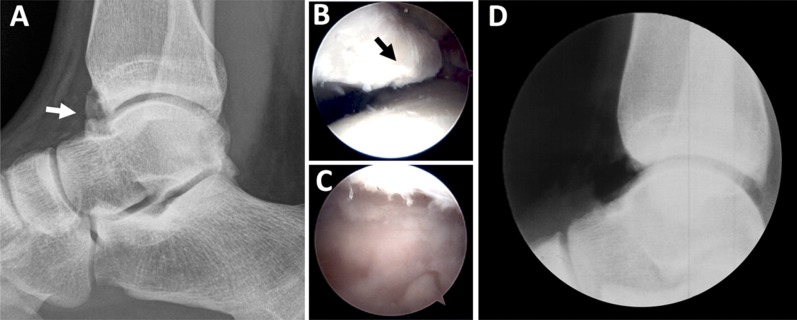
Figure 6.
An 18-year-old college football player with pain on dorsiflexion consistent with anterior impingement: (a) a pre-operative lateral radiograph is showing large anterior osteophytes at the tibiotalar joint (white arrow); arthroscopic images (b) before and (c) after debridement of the large anterior osteophyte (black arrow). (d) An intraoperative fluoroscopic image is confirming the removal of large osteophytes.
Multiple studies evaluating the early and late outcomes from arthroscopic management showed excellent responses with decreased post-surgical pain scores, faster return to sport/full activity, increased range of motion and high willingness to undergo surgery again if needed.26 Curiously, osteophyte regrowth is a common delayed outcome after surgery, but no correlation with recurrence of pain has been noted.35
ANTEROMEDIAL IMPINGEMENT SYNDROME
Anatomic region
The anteromedial gutter or recess is formed superficially by the anteromedial joint capsule, laterally by the talar dome, body and neck, medially by the medial malleolus and inferiorly by the anterior tibiotalar fascicle of the deltoid ligament (anterior tibiotalar ligament) (Figure 7).
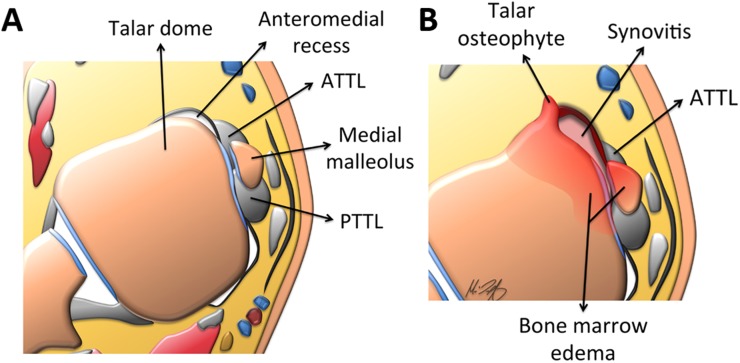
Figure 7.
Axial illustrations through the level of the talus: (a) the normal appearance of the anteromedial ankle recess is shown, which is formed by the talus, anteromedial joint capsule, medial malleolus and the anterior tibiotalar ligament (ATTL). Also shown is the posterior tibiotalar ligament (PTTL), which forms the posterior border. (b) Possible aetiologies of anteromedial impingement syndrome are shown, including but not limited to: a talar osteophyte from chronic repetitive microtrauma, thickening of the ATTL, synovial inflammatory response and associated bone marrow oedema.
Pathogenesis of anteromedial ankle impingement syndrome
Clinically, the anteromedial ankle impingement syndrome presents with pain associated with dorsiflexion and inversion and can be seen in soccer players, dancers and cross-country runners.40 This can result as the sequela of a prior plantar flexion/inversion injury.1 The condition was first described by Egol and Parisien in 1997 in a case report and subsequently by Mosier-La Clair et al in 2000 with a case series of 11 patients.41,42
During the acute injury, there is damage to the anterior tibiotalar ligament, which subsequently thickens.41 In addition to ligament thickening, osteophytes, synovitis and fractures have been described as other possible causative factors.41 Lastly, recurrent microtrauma over time can form bony spurs along the talar neck, anterior margin of the medial malleolus or anteromedial tibial plafond, which can impair the range of motion, similar to anterior ankle impingement.40
Imaging characteristics
Conventional radiography including frontal and exaggerated oblique projections can visualize medial talar, tibial plafond and medial malleolar osteophytes/enthesophytes (Figure 8).43 CT has an additional role by better localizing bone spurs and osteochondral lesions and assisting in the pre-operative planning.3 MRI can be used to better evaluate the medial ligaments, articular cartilage and associated soft tissues. There is sparse literature evaluating the effectiveness of MR arthrography.
Figure 8.
A 20-year-old female with a history of ankle sprain, progressively worsening anteromedial pain and limited dorsiflexion, consistent with anteromedial impingement: (a, b) oblique radiographs at 8 and 24 months post-injury are demonstrating progressively enlarging bone proliferation at the anterior colliculus of the medial malleolus (arrows). (c) Sagittal fluid-sensitive and (d) sagittal T1 weighted sequences are showing synovitis in the anteromedial recess (arrowhead) and adjacent osteophyte (dashed arrow).
Treatment for anteromedial ankle impingement syndrome
Conservative treatment remains a controversial first step in management. Positive results have been seen with ultrasound guidance for anteromedial meniscoid lesion steroid injections. However, outcomes from such injections have not been well studied.44 Given the high rates of failure, it has been suggested that surgery, saving 6 weeks of morbidity, be considered as a first-line treatment.11,25,40 In a retrospective cohort of 41 patients, 93% of patients were satisfied with the results of arthroscopy and all but 1 patient returned to their previous level of activity.40 This places it on par with surgical treatment of anterior and anterolateral ankle impingement.
POSTEROMEDIAL IMPINGEMENT SYNDROME
Anatomic region
The anterior boundaries of the posteromedial recess are the medial malleolus and posterior tibiotalar ligament (PTTL). The lateral side is formed by the talar dome and posterior process of the talus. Peripherally, the recess is demarcated by the posteromedial joint capsule, neurovascular bundle and flexor hallucis longus tendon (Figure 9).
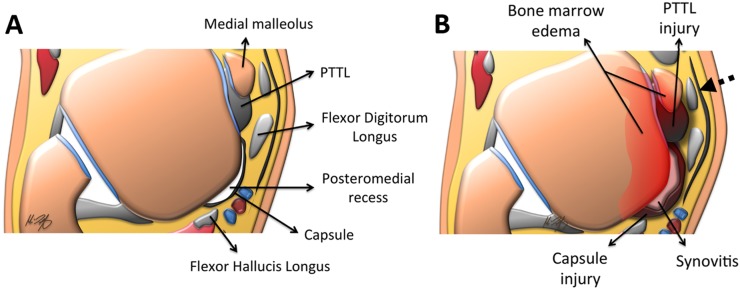
Figure 9.
Axial illustrations through the level of the talus: (a) the boundaries of the posteromedial recess are the medial malleolus and posterior tibiotalar ligament (PTTL) anteriorly, the talar dome and posterior process of the talus laterally and the posteromedial joint capsule, neurovascular bundle and flexor hallucis longus tendon peripherally. (b) In posteromedial impingement, a constellation of findings can be seen including an injured and thickened PTTL, associated synovitis, posteromedial joint capsule injury and bone marrow oedema. The close proximity of the enlarged posteromedial recess to the flexor tendons, especially the tibialis posterior (dashed arrow), which is affected in approximately 40% of cases, can be noted.
Pathogenesis of posteromedial ankle impingement syndrome
The common precipitating injury for posteromedial ankle impingement is a plantar flexion, inversion and internal rotation trauma. This can lead to damage to the PTTL and associated synovitis, which can partially encase the posterior tibialis tendon (PTT) (40% of cases), the flexor hallucis longus tendon (16% of cases) or the flexor digitorum longus tendon (8% of cases).45
It was first described by Liu and Mirzayan46 in 1993 and remains one of the least common ankle impingement syndromes.17 Commonly, the patient presents with pain over the posteromedial aspect of the ankle with both passive and active movement.47,48 Owing to the strong nature of the deltoid ligament, injury occurs in 15% of ligamentous traumas of the ankle and leads to an impingement syndrome only in a fraction of those cases.49 Also, given the high-energy nature of an injury that could lead to deltoid ligament rupture, a high percentage of patients will have concomitant osteochondral injuries or other ligamentous injury.47
Imaging characteristics
Ankle radiography is usually initially performed, but is often of little utility, as the usual pathophysiology is ligamentous or soft tissue in nature in contradistinction to anterior impingement. Recent reports have demonstrated the possible utility of ultrasonography for evaluation of the PTTL, which may be thickened and hypoechoic, denoting increased fibrous tissue formation and oedema.50
Given the high-energy nature injury to the deep deltoid ligament with likely concomitant lateral ligamentous injury, MRI is frequently performed. On MRI, the normal deep portion of the deltoid ligament appears as a fan-shaped tendon with insertions onto the calcaneus, talus and navicular bones. Pathology to the deltoid ligament, particularly the PTTL, presents with intermediate intensity on fluid-sensitive sequences and with thickening and loss of the normal fibrillar pattern. Additional fluid collections or synovitis may be seen posteriorly.50 Irregular soft tissues may also be seen within the posteromedial recess (Figure 10).
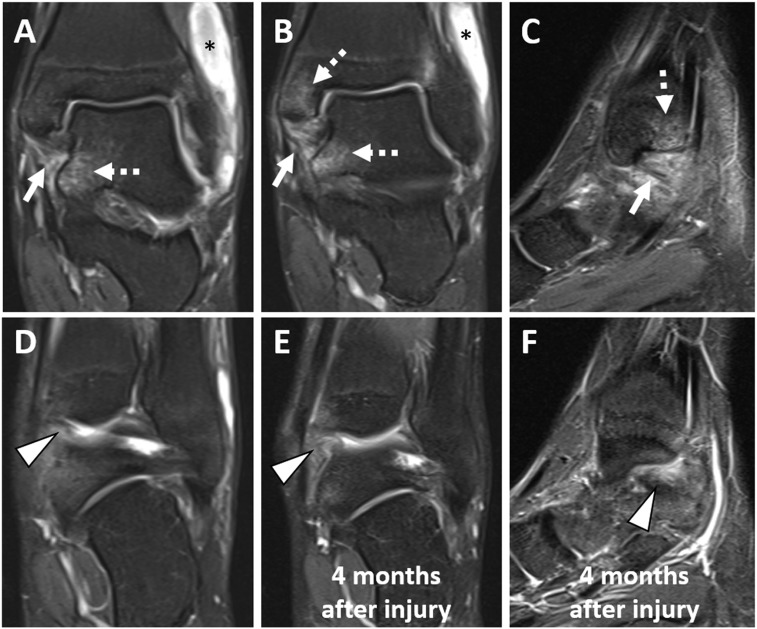
Figure 10.
A 23-year-old male with an ankle inversion injury and subsequent posteromedial impingement imaged (a–d) immediately and 4 months after injury. (a, b) Coronal and (c) sagittal fluid-sensitive images are showing partial tearing of the posterior tibiotalar ligament due to compression (arrows). Bone contusions in the medial malleolus and medial talus are shown (dashed arrows). A haematoma is also seen superficial to the lateral malleolus (asterisk). (d) A coronal fluid-sensitive image is showing the normal joint capsule at the posteromedial recess (arrowhead). (e) Coronal and (f) sagittal fluid-sensitive images obtained 4 months after injury are showing thickening and fibrosis in the posteromedial recess (arrowheads), which were not present on the initial examination.
Treatment for anteromedial ankle impingement syndrome
The identification of medial ankle pain after a severe inversion injury is usually delayed owing to the presenting symptom mainly centred around the lateral ligamentous disruption.48 Treatment is usually started conservatively, but surgical treatment can also be safely performed with quite promising results. Complete or near complete relief of symptoms was seen after surgery in all six patients in a case series.48 Unfortunately, owing to the relative rarity of this condition, and other concomitant ankle injuries, large case series or trials have been lacking.
POSTERIOR IMPINGEMENT SYNDROME
Relevant anatomy
The majority of the posterior impingement syndromes are related to the posterior talus. The secondary ossification centre of the posterolateral talus forms around 8–13 years of age and then subsequently fuses within 1 year of that.51 Occasionally (approximately 7%), there may be non-fusion with a resultant os trigonum.51,52 In addition, this ossification centre may remain prominent with the so-called “Stieda's53 process” (Figure 11).
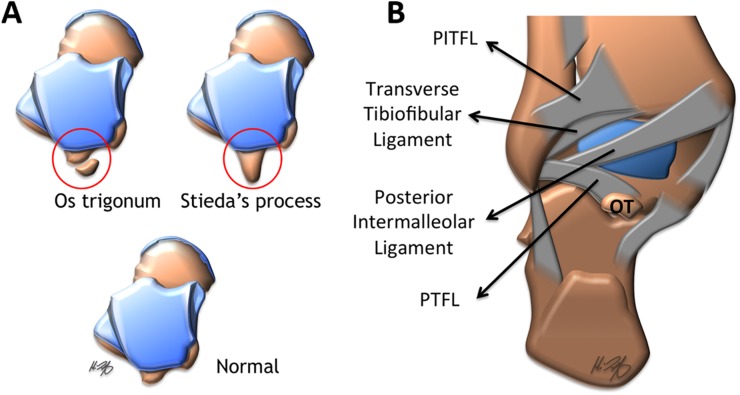
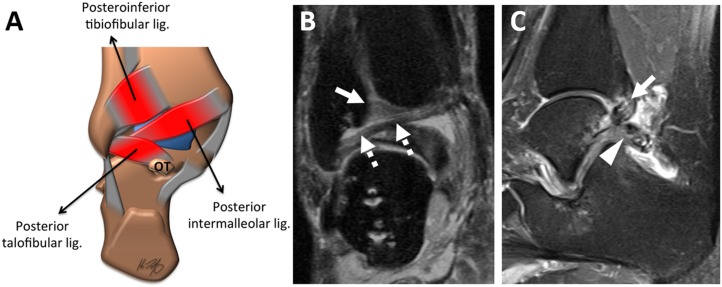
Figure 11.
(a) Illustrations as seen from a superior view demonstrating the normal posterior process of the talus, os trigonum (OT) and Stieda's process variants; (b) an illustration as seen from a posterior view of the ankle demonstrating the ligamentous anatomy of the posterolateral ankle. PITFL, posteroinferior tibiofibular ligament; PTFL, posterior talofibular ligament. Adapted from Ngai et al69 with permission from Elsevier.
In addition to the osseous posterolateral talus, the ligamentous anatomy includes (from superior to inferior): (1) the posteroinferior talofibular ligament, which extends from the lateral malleolus to the posterolateral tibia; (2) the transverse tibiofibular ligament extending from the fibula to the posterior tibia and medial malleolus; (3) the tibial slip, also called the posterior intermalleolar ligament, originating from the posterior tibia and inserts at the posterior talofibular ligament; and (4) the posterior talofibular ligament extending from the lateral malleolus to the posterolateral talus (Figure 11).
Pathophysiology of the posterior ankle impingement
Clinically, the posterior impingement syndrome presents with chronic pain and swelling within the posterior ankle. Classically, this is seen with activities that cause extreme plantar flexion, such as ballet, soccer, football and downhill running.51
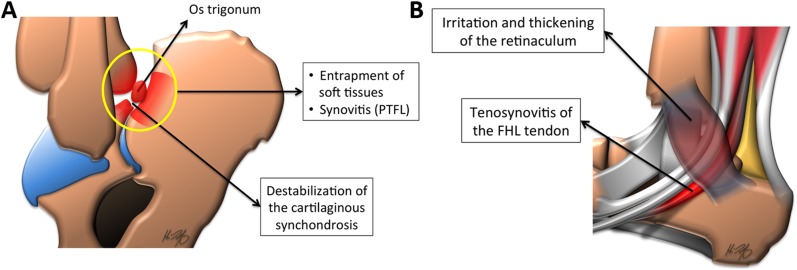
The two main proposed mechanisms of posterior impingement are: (1) an acute plantar hyperflexion injury and (2) chronic repetitive microtrauma.54,55 The similarity between the two mechanisms revolves around the posterior soft tissues, which may become secondarily hypertrophied and compressed between the posterior talus and the calcaneus. The presence of an osseous body (os trigonum or prominent Stieda's process) can further narrow this space, which has led to its other name of “os trigonum syndrome”(Figure 12).51 This increased compression leads to damage to the regional tendons and ligaments. Flexor hallucis longus tenosynovitis is commonly involved (Figure 12).56 Important differentials include Achilles tendinosis/tear, arthrosis, acute posterior talar process fractures, flexor hallucis longus tenosynovitis, Haglund's syndrome, osteochondral lesions and retrocalcaneal bursitis.20
Figure 12.
Sagittal illustrations as seen from a lateral view in posterior ankle impingement: (a) in the plantar flexed ankle with an associated os trigonum, there is an entrapment of the posterior soft tissues, including the posterior talofibular ligament (PTFL) and associated synovitis. (b) An irritated and thickened flexor retinaculum can cause flexor hallucis longus (FHL) tendon irritation and tenosynovitis owing to their intimate relationship.
Imaging characteristics
Initial evaluation with conventional radiography may demonstrate a normal appearance, but special attention should be placed on the lateral radiograph for the presence of a Stieda's process or an os trigonum. As these are seen commonly in patients without symptoms of posterior impingement syndrome, they are not sufficient to cause an impingement syndrome; but, in the appropriate clinical context, they may contribute to symptomatology.57
Further evaluation with CT can visualize osseous variants, additional osseous bodies and osteochondral abnormalities and can be performed to assist with pre-operative management.54 Ultrasound may be used for injections of a local anaesthetic or corticosteroids, which may help in the diagnosis and palliation of posterior impingement syndrome.58
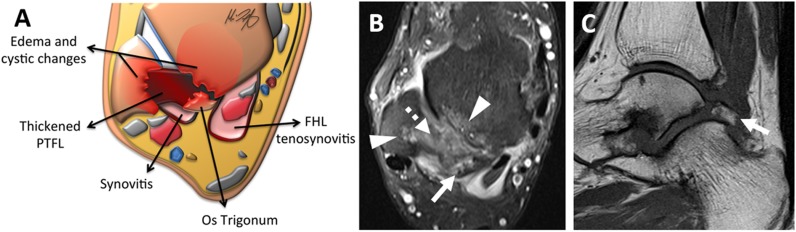
MRI, with its superior soft-tissue contrast, plays an invaluable role in the evaluation of posterior ankle pain. One key feature is bone marrow oedema (low T1 and high T2 signal) within the talus, calcaneus or an os trigonum (Figure 13).51,59 Other features include increased signal at the synchondrosis, associated synovitis and thickening of the posterior ligaments (Figure 14), as well as the possibility of a posterior subtalar or tibiotalar ganglia being present.
Figure 13.
A 47-year-old male with chronic ankle pain that worsens during plantar flexion, consistent with posterior impingement: (a) an axial illustration, (b) an axial fluid-sensitive image and (c) sagittal T1 weighted images are showing a degenerated os trigonum (arrows) with a thickened posterior talofibular ligament (PTFL) (dashed arrow) and oedema/cystic changes of the talus and fibula (arrowheads).
Figure 14.
Posterior impingement: (a) an illustration as seen from a posterior view is showing thickened and degenerated posterior ligaments. In a 40-year-old male with pain during plantar flexion, (b) coronal and (c) sagittal fluid-sensitive images are showing a thick and hyperintense posteroinferior tibiofibular ligament (arrows), intermalleolar ligament (dashed arrows) and posterior talofibular ligament (arrowhead), consistent with the clinical diagnosis of posterior impingement. OT, os trigonum.
Treatment for posterior ankle impingement syndrome
As with other impingement syndromes, the first-line treatment is conservative measures.60 If those fail, then surgery remains a viable option (Figure 15). A recent meta-analysis comparing open to arthroscopic treatment found no change in patient satisfaction. However, it should be noted that patients with arthroscopic treatment had fewer complications (15.9% vs 7.3%) and in particular, fewer major complications (13.8% vs 5.4%).60 Most patients returned to full activity on an average within 8 or 16 weeks with arthroscopic and open surgical technique, respectively.60
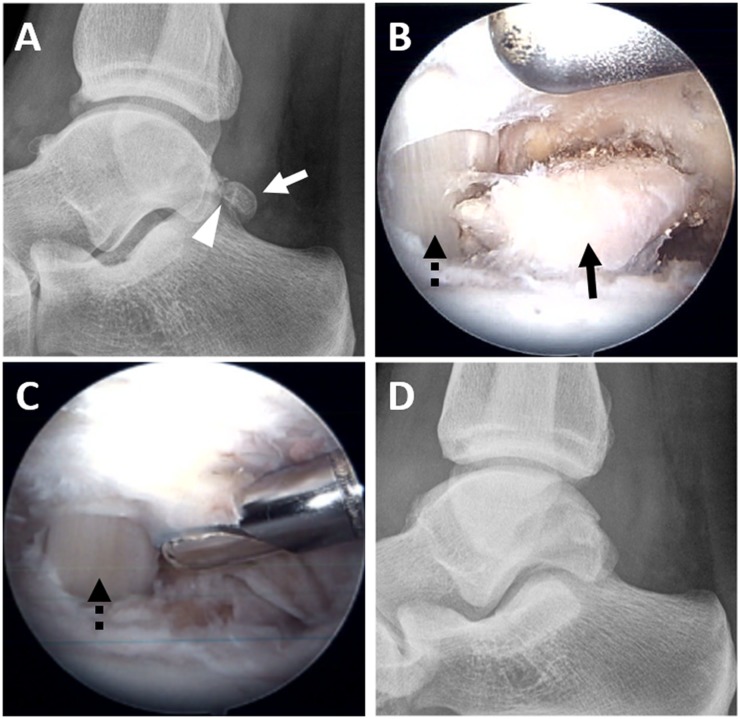
Figure 15.
A 25-year-old professional lacrosse player with posterior impingement: (a) a pre-operative lateral radiograph is showing an os trigonum (white arrow) with degeneration at the synchondrosis (arrowhead). (b) An arthroscopic image after debridement of the soft tissues is showing an exposed os trigonum (black arrow) with the flexor hallucis longus tendon (FHL) seen medially (black dashed arrow). (c) An arthroscopic image after removal of the os trigonum with FHL seen medially (black dashed arrow). (d) A post-operative lateral radiograph is confirming successful os trigonum removal.
EXTRA-ARTICULAR LATERAL HINDFOOT IMPINGEMENT SYNDROME
Relevant anatomy
The extra-articular lateral hindfoot impingement syndrome (ELHIS) is a non-traumatic cause of impingement and presents as the sequela of a pathologic PTT, which causes a flatfoot and hindfoot valgus deformity.61 While patients present similarly, the exact site of pathology varies. Common sites for impingement are between the lateral talus and calcaneus (talocalcaneal impingement) and between the calcaneus and fibula (subfibular impingement). Other sites involved in PTT pathology include the sinus tarsi and distal fibula (e.g. stress fracture) and are important causes of non-impingement lateral hindfoot pain to consider.61
In addition to PTT pathology, Martus et al62 described a case series of patients who presented with an ELHIS, which improved after resection of an accessory anterolateral talar facet. This accessory anterolateral talar facet was first described in 1904 and is found in 10.2% of Egyptian tali.63 This was further evaluated in 1993, and large accessory facets were found in 4% of patients and with variable sizes seen in 34% of all patients.64
Pathogenesis of extra-articular lateral hindfoot impingement syndrome
It has been suggested that there are likely two aetiologies of ELHIS. The first, primary lateral hindfoot impingement, is due to the accessory anterolateral talar facet. This relatively common accessory articulation may become pathologic with a flatfoot/hindfoot valgus deformity causing abnormal mechanics during subtalar eversion. Interestingly, this has a propensity to effect patients who are young and obese.62,65
With the second, or acquired, aetiology of ELHIS, the normal change in joint space calibre within the sinus tarsi on subtalar eversion is exaggerated owing to hindfoot valgus and subsequently, abnormal contact between the lateral talus and calcaneus (talocalcaneal impingement) may occur. If the degree of hindfoot valgus is great enough, there can be contact between the calcaneus and the fibula (subfibular impingement).61 Over time, this abnormal contact can lead to early arthrosis of the involved joints or distal fibular erosions and presents with classic symptoms of pain over the lateral sinus tarsi.66 Talocalcaneal impingement and calcaneofibular impingement affects almost exclusively patients with flatfoot/hindfoot valgus.66
Imaging characteristics
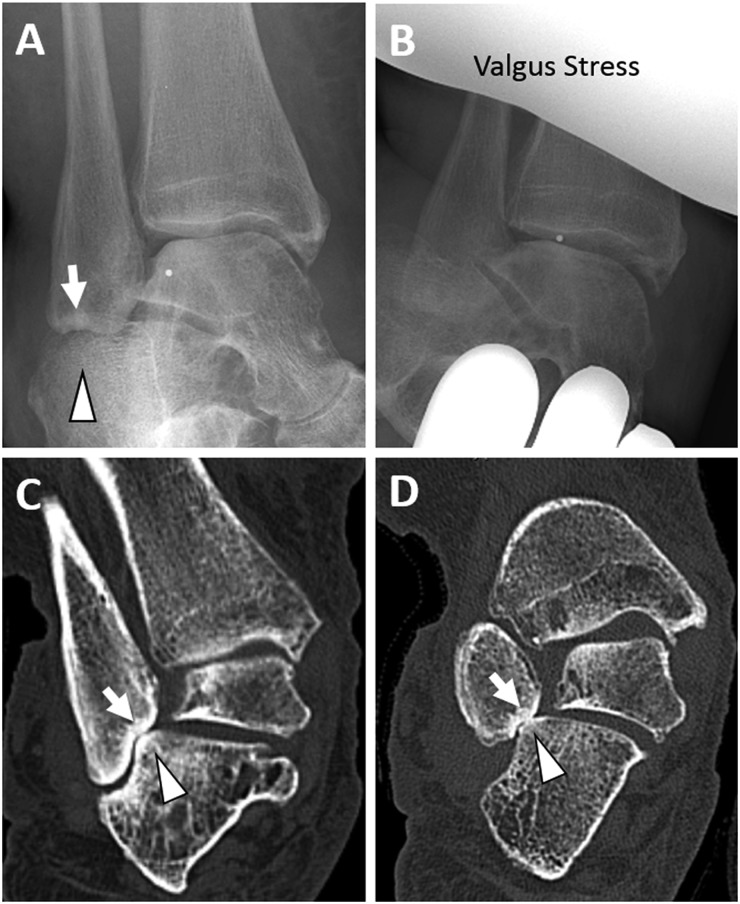
The imaging evaluation usually starts with conventional radiography. Given its planar nature and extensive overlying structures, it may be difficult to see the osseous contact, especially with neutral foot posture. However, secondary signs such as cystic degeneration or subchondral sclerosis may be seen.66,67 In addition, dorsal talar “beaking” can be an informative secondary sign.62
CT has also been used for both diagnosis and to assist surgical planning with its increased ability to resolve degenerative subtalar and subfibular changes (Figure 16). In addition, CT has the ability to evaluate for additional causes of lateral hindfoot pain, particularly tarsal coalitions (cartilaginous or fibrous).62 Simulated weight-bearing CT examinations have been shown to be useful in evaluating the degree of sinus tarsi narrowing.67
Figure 16.
A 67-year-old female with severe pes planovalgus and lateral sided pain: (a) an oblique radiograph is showing sclerosis and irregularity of the inferior fibula (arrow), which is closely apposed to the calcaneus (arrowhead). (b) Significant pain was reported when minimal valgus stress was applied. (c, d) Coronal oblique CT images are showing valgus tilting of the talus with contact between the fibula (arrows) and calcaneus (arrowheads), consistent with clinically suspected subfibular impingement.
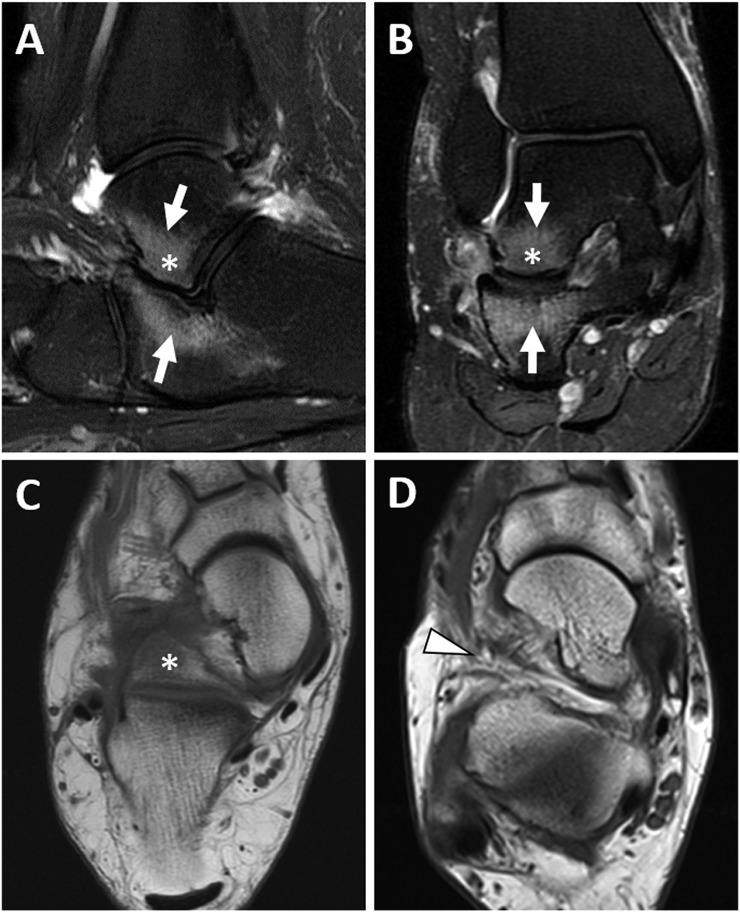
Along with CT, MRI has the ability to calculate the hindfoot valgus angle and evaluate for accessory anterolateral talar facet. MRI has a superior advantage when evaluating the degree of PTT pathology, which has the potential to correlate to clinical grading systems.61 The most common MRI findings are cystic changes and bone marrow oedema within the lateral talus (Figure 17). Additional soft-tissue thickening between the fibula and the calcaneus may be seen, which has been associated with entrapment of fat or the calcaneofibular ligament.61 In addition, there may be fibular tip oedema and a calcaneofibular neofacet demonstrated.61
Figure 17.
A 20-year-old female weighing 420 pounds, who presents with severe, chronic, posterolateral ankle pain and swelling for 8 months: (a) sagittal and (b) coronal fluid-sensitive images are showing a large accessory anterolateral talar facet (asterisks), which is abutting the calcaneus with extensive marrow oedema (arrows), consistent with talocalcaneal impingement. (c) An axial T1 weighted image is showing the large accessory facet (asterisk) extending into the sinus tarsi. (d) An axial T1 weighted image in another patient without an accessory talar facet is showing the normal appearance of the sinus tarsi (arrowhead).
Treatment for extra-articular lateral hindfoot impingement syndrome
A conservative approach including rest and non-steroidal anti-inflammatory drugs is the usual first-line treatment. If this fails, subtalar arthrodesis can be safely performed.68 For patients with an accessory anterolateral talar joint, results have been promising for a subtalar-sparing operative strategy, which may save early-onset ankle degenerative changes seen with subtalar arthrodesis, especially given the young age of patients with primary extra-articular lateral hindfoot impingement.62
CONCLUSION
Ankle impingement syndromes encompass a broad spectrum of chronic ankle conditions. They have different pathogenesis and, depending on the location/causative factor, different preferred treatments. Imaging, including radiographs through advanced modalities such as MRI, has a valuable role in assisting the clinician with confirming the clinical diagnosis, highlighting secondary relevant soft tissues and osseous abnormalities, which at times may not be visible on arthroscopy, or palliating pain by guiding intra-articular injections.
FUNDING
Eric Y Chang, MD gratefully acknowledges support from the VA Clinical Science Research and Development (1IK2CX000749 and 1I01CX001388).
Contributor Information
Zachary Berman, Email: zberman@ucsd.edu.
Monica Tafur, Email: motafur@gmail.com.
Sonya S Ahmed, Email: ssa003@ucsd.edu.
Brady K Huang, Email: bradyhuang@gmail.com.
Eric Y Chang, Email: ericchangmd@gmail.com.
REFERENCES
- 1.Bassett FH, 3rd, Gates HS, 3rd, Billys JB, Morris HB, Nikolaou PK. Talar impingement by the anteroinferior tibiofibular ligament. A cause of chronic pain in the ankle after inversion sprain. J Bone Joint Surg Am 1990; 72: 55–9. doi: https://doi.org/10.2106/00004623-199072010-00009 [PubMed] [Google Scholar]
- 2.Robinson P, White LM. Soft-tissue and osseous impingement syndromes of the ankle: role of imaging in diagnosis and management. Radiographics 2002; 22: 1457–69; discussion 1470–1. doi: https://doi.org/10.1148/rg.226025034 [DOI] [PubMed] [Google Scholar]
- 3.Russo A, Zappia M, Reginelli A, Carfora M, D'Agosto GF, La Porta M, et al. Ankle impingement: a review of multimodality imaging approach. Musculoskelet Surg 2013; 97(Suppl. 2): S161–8. doi: https://doi.org/10.1007/s12306-013-0286-8 [DOI] [PubMed] [Google Scholar]
- 4.McCarthy CL, Wilson DJ, Coltman TP. Anterolateral ankle impingement: findings and diagnostic accuracy with ultrasound imaging. Skeletal Radiol 2008; 37: 209–16. doi: https://doi.org/10.1007/s00256-007-0411-6 [DOI] [PubMed] [Google Scholar]
- 5.Yablon CM. Ultrasound-guided interventions of the foot and ankle. Semin Musculoskelet Radiol 2013; 17: 60–8. doi: https://doi.org/10.1055/s-0033-1333916 [DOI] [PubMed] [Google Scholar]
- 6.Hauger O, Moinard M, Lasalarie JC, Chauveaux D, Diard F. Anterolateral compartment of the ankle in the lateral impingement syndrome: appearance on CT arthrography. AJR Am J Roentgenol 1999; 173: 685–90. doi: https://doi.org/10.2214/ajr.173.3.10470904 [DOI] [PubMed] [Google Scholar]
- 7.Dinato MC, Luques IU, Freitas Mde F, Pereira Filho MV, Ninomiya AF, Pagnano RG, et al. Endoscopic treatment of the posterior ankle impingement syndrome on amateur and professional athletes. Knee Surg Sports Traumatol Arthrosc 2016; 24: 1396–401. doi: https://doi.org/10.1007/s00167-015-3747-9 [DOI] [PubMed] [Google Scholar]
- 8.Nihal A, Rose DJ, Trepman E. Arthroscopic treatment of anterior ankle impingement syndrome in dancers. Foot Ankle Int 2005; 26: 908–12. [DOI] [PubMed] [Google Scholar]
- 9.van Dijk CN, Tol JL, Verheyen CC. A prospective study of prognostic factors concerning the outcome of arthroscopic surgery for anterior ankle impingement. Am J Sports Med 1997; 25: 737–45. doi: https://doi.org/10.1177/036354659702500603 [DOI] [PubMed] [Google Scholar]
- 10.Dimmick S, Linklater J. Ankle impingement syndromes. Radiol Clin North Am 2013; 51: 479–510. doi: https://doi.org/10.1016/j.rcl.2012.11.005 [DOI] [PubMed] [Google Scholar]
- 11.Liu SH, Nuccion SL, Finerman G. Diagnosis of anterolateral ankle impingement. Comparison between magnetic resonance imaging and clinical examination. Am J Sports Med 1997; 25: 389–93. doi: https://doi.org/10.1177/036354659702500320 [DOI] [PubMed] [Google Scholar]
- 12.van den Bekerom MP, Raven EE. The distal fascicle of the anterior inferior tibiofibular ligament as a cause of tibiotalar impingement syndrome: a current concepts review. Knee Surg Sports Traumatol Arthrosc 2007; 15: 465–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cass JR, Morrey BF. Ankle instability: current concepts, diagnosis, and treatment. Mayo Clin Proc 1984; 59: 165–70. doi: https://doi.org/10.1016/S0025-6196(12)60769-1 [DOI] [PubMed] [Google Scholar]
- 14.Ferkel RD, Karzel RP, Del Pizzo W, Friedman MJ, Fischer SP. Arthroscopic treatment of anterolateral impingement of the ankle. Am J Sports Med 1991; 19: 440–6. doi: https://doi.org/10.1177/036354659101900504 [DOI] [PubMed] [Google Scholar]
- 15.McCarroll JR, Schrader JW, Shelbourne KD, Rettig AC, Bisesi MA. Meniscoid lesions of the ankle in soccer players. Am J Sports Med 1987; 15: 255–7. doi: https://doi.org/10.1177/036354658701500311 [DOI] [PubMed] [Google Scholar]
- 16.Subhas N, Vinson EN, Cothran RL, Santangelo JR, Nunley JA, 2nd, Helms CA. MRI appearance of surgically proven abnormal accessory anterior-inferior tibiofibular ligament (Bassett's ligament). Skeletal Radiol 2008; 37: 27–33. doi: https://doi.org/10.1007/s00256-007-0390-7 [DOI] [PubMed] [Google Scholar]
- 17.Cerezal L, Abascal F, Canga A, Pereda T, Garcia-Valtuille R, Perez-Carro L, et al. MR imaging of ankle impingement syndromes. AJR Am J Roentgenol 2003; 181: 551–9. doi: https://doi.org/10.2214/ajr.181.2.1810551 [DOI] [PubMed] [Google Scholar]
- 18.Akseki D, Pinar H, Yaldiz K, Akseki NG, Arman C. The anterior inferior tibiofibular ligament and talar impingement: a cadaveric study. Knee Surg Sports Traumatol Arthrosc 2002; 10: 321–6. [DOI] [PubMed] [Google Scholar]
- 19.Odak S, Ahluwalia R, Shivarathre DG, Mahmood A, Blucher N, Hennessy M, et al. Arthroscopic evaluation of impingement and osteochondral lesions in chronic lateral ankle instability. Foot Ankle Int 2015; 36: 1045–9. doi: https://doi.org/10.1177/1071100715585525 [DOI] [PubMed] [Google Scholar]
- 20.Jordan LK, 3rd, Helms CA, Cooperman AE, Speer KP. Magnetic resonance imaging findings in anterolateral impingement of the ankle. Skeletal Radiol 2000; 29: 34–9. [DOI] [PubMed] [Google Scholar]
- 21.Rubin DA, Tishkoff NW, Britton CA, Conti SF, Towers JD. Anterolateral soft-tissue impingement in the ankle: diagnosis using MR imaging. AJR Am J Roentgenol 1997; 169: 829–35. doi: https://doi.org/10.2214/ajr.169.3.9275907 [DOI] [PubMed] [Google Scholar]
- 22.Ferkel RD, Tyorkin M, Applegate GR, Heinen GT. MRI evaluation of anterolateral soft tissue impingement of the ankle. Foot Ankle Int 2010; 31: 655–61. doi: https://doi.org/10.3113/FAI.2010.0655 [DOI] [PubMed] [Google Scholar]
- 23.Huh YM, Suh JS, Lee JW, Song HT. Synovitis and soft tissue impingement of the ankle: assessment with enhanced three-dimensional FSPGR MR imaging. J Magn Reson Imaging 2004; 19: 108–16. doi: https://doi.org/10.1002/jmri.10438 [DOI] [PubMed] [Google Scholar]
- 24.Robinson P, White LM, Salonen DC, Daniels TR, Ogilvie-Harris D. Anterolateral ankle impingement: MR arthrographic assessment of the anterolateral recess. Radiology 2001; 221: 186–90. doi: https://doi.org/10.1148/radiol.2211001666 [DOI] [PubMed] [Google Scholar]
- 25.Simonson DC, Roukis TS. Safety of ankle arthroscopy for the treatment of anterolateral soft-tissue impingement. Arthroscopy 2014; 30: 256–9. doi: https://doi.org/10.1016/j.arthro.2013.10.014 [DOI] [PubMed] [Google Scholar]
- 26.Zwiers R, Wiegerinck JI, Murawski CD, Fraser EJ, Kennedy JG, van Dijk CN. Arthroscopic treatment for anterior ankle impingement: a systematic review of the current literature. Arthroscopy 2015; 31: 1585–96. doi: https://doi.org/10.1016/j.arthro.2015.01.023 [DOI] [PubMed] [Google Scholar]
- 27.Morris LH. Athlete's ankle. J Bone Joint Surg Am 1943; 25: 220. [Google Scholar]
- 28.McMurray TP. Footballer's ankle. J Bone Joint Surg Am 1950; 32: 68–9. [Google Scholar]
- 29.Tol JL, van Dijk CN. Etiology of the anterior ankle impingement syndrome: a descriptive anatomical study. Foot Ankle Int 2004; 25: 382–6. [DOI] [PubMed] [Google Scholar]
- 30.Tol JL, Slim E, van Soest AJ, van Dijk CN. The relationship of the kicking action in soccer and anterior ankle impingement syndrome. A biomechanical analysis. Am J Sports Med 2002; 30: 45–50. [DOI] [PubMed] [Google Scholar]
- 31.Biedert R. Anterior ankle pain in sports medicine: aetiology and indications for arthroscopy. Arch Orthop Trauma Surg 1991; 110: 293–7. doi: https://doi.org/10.1007/BF00443461 [DOI] [PubMed] [Google Scholar]
- 32.Amendola N, Drew N, Vaseenon T, Femino J, Tochigi Y, Phisitkul P. CAM-type impingement in the ankle. Iowa Orthop J 2012; 32: 1–8. [PMC free article] [PubMed] [Google Scholar]
- 33.Stoller SM, Hekmat F, Kleiger B. A comparative study of the frequency of anterior impingement exostoses of the ankle in dancers and nondancers. Foot Ankle 1984; 4: 201–3. doi: https://doi.org/10.1177/107110078400400409 [DOI] [PubMed] [Google Scholar]
- 34.Massada JL. Ankle overuse injuries in soccer players. Morphological adaptation of the talus in the anterior impingement. J Sports Med Phys Fitness 1991; 31: 447–51. [PubMed] [Google Scholar]
- 35.Tol JL, Verheyen CP, van Dijk CN. Arthroscopic treatment of anterior impingement in the ankle. J Bone Joint Surg Br 2001; 83: 9–13. doi: https://doi.org/10.1302/0301-620X.83B1.10571 [DOI] [PubMed] [Google Scholar]
- 36.Haller J, Bernt R, Seeger T, Weissenback A, Tuchler H, Resnick D. MR-imaging of anterior tibiotalar impingement syndrome: agreement, sensitivity and specificity of MR-imaging and indirect MR-arthrography. Eur J Radiol 2006; 58: 450–60. doi: https://doi.org/10.1016/j.ejrad.2006.03.008 [DOI] [PubMed] [Google Scholar]
- 37.Coull R, Raffiq T, James LE, Stephens MM. Open treatment of anterior impingement of the ankle. J Bone Joint Surg Br 2003; 85: 550–3. doi: https://doi.org/10.1302/0301-620x.85b4.13871 [DOI] [PubMed] [Google Scholar]
- 38.Hensley JP, Saltrick K, Le T. Anterior ankle arthroplasty: a retrospective study. J Foot Surg 1990; 29: 169–72. [PubMed] [Google Scholar]
- 39.Glazebrook MA, Ganapathy V, Bridge MA, Stone JW, Allard JP. Evidence-based indications for ankle arthroscopy. Arthroscopy 2009; 25: 1478–90. doi: https://doi.org/10.1016/j.arthro.2009.05.001 [DOI] [PubMed] [Google Scholar]
- 40.Murawski CD, Kennedy JG. Anteromedial impingement in the ankle joint: outcomes following arthroscopy. Am J Sports Med 2010; 38: 2017–24. doi: https://doi.org/10.1177/0363546510369335 [DOI] [PubMed] [Google Scholar]
- 41.Mosier-La Clair SM, Monroe MT, Manoli A. Medial impingement syndrome of the anterior tibiotalar fascicle of the deltoid ligament on the talus. Foot Ankle Int 2000; 21: 385–91. [DOI] [PubMed] [Google Scholar]
- 42.Egol KA, Parisien JS. Impingement syndrome of the ankle caused by a medial meniscoid lesion. Arthroscopy 1997; 13: 522–5. doi: https://doi.org/10.1016/s0749-8063(97)90136-5 [DOI] [PubMed] [Google Scholar]
- 43.van Dijk CN, Wessel RN, Tol JL, Maas M. Oblique radiograph for the detection of bone spurs in anterior ankle impingement. Skeletal Radiol 2002; 31: 214–21. doi: https://doi.org/10.1007/s00256-002-0477-0 [DOI] [PubMed] [Google Scholar]
- 44.Jose J, Mirpuri T, Lesniak B, Kaplan L. Sonographically guided therapeutic injections in the meniscoid lesion in patients with anteromedial ankle impingement syndrome. Foot Ankle Spec 2014; 7: 409–13. doi: https://doi.org/10.1177/1938640014543363 [DOI] [PubMed] [Google Scholar]
- 45.Giannini S, Buda R, Mosca M, Parma A, Di Caprio F. Posterior ankle impingement. Foot Ankle Int 2013; 34: 459–65. doi: https://doi.org/10.1177/1071100713477609 [DOI] [PubMed] [Google Scholar]
- 46.Liu SH, Mirzayan R. Posteromedial ankle impingement. Arthroscopy 1993; 9: 709–11. doi: https://doi.org/10.1016/s0749-8063(05)80514-6 [DOI] [PubMed] [Google Scholar]
- 47.van Dijk CN, Bossuyt PM, Marti RK. Medial ankle pain after lateral ligament rupture. J Bone Joint Surg Br 1996; 78: 562–7. [PubMed] [Google Scholar]
- 48.Paterson RS, Brown JN. The posteromedial impingement lesion of the ankle. A series of six cases. Am J Sports Med 2001; 29: 550–7. [DOI] [PubMed] [Google Scholar]
- 49.Cetti R. Conservative treatment of injury to the fibular ligaments of the ankle. Br J Sports Med 1982; 16: 47–52. doi: https://doi.org/10.1136/bjsm.16.1.47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Koulouris G, Connell D, Schneider T, Edwards W. Posterior tibiotalar ligament injury resulting in posteromedial impingement. Foot Ankle Int 2003; 24: 575–83. [DOI] [PubMed] [Google Scholar]
- 51.Karasick D, Schweitzer ME. The os trigonum syndrome: imaging features. AJR Am J Roentgenol 1996; 166: 125–9. doi: https://doi.org/10.2214/ajr.166.1.8571860 [DOI] [PubMed] [Google Scholar]
- 52.O'Rahilly R. A survey of carpal and tarsal anomalies. J Bone Joint Surg Am 1953; 35: 626–42. [PubMed] [Google Scholar]
- 53.Stieda L. Ueber secundäre fusswurzelknochen. Arch Phys Wiss Med 1869: 108–11. [Google Scholar]
- 54.Hayashi D, Roemer FW, D'Hooghe P, Guermazi A. Posterior ankle impingement in athletes: pathogenesis, imaging features and differential diagnoses. Eur J Radiol 2015; 84: 2231–41. doi: https://doi.org/10.1016/j.ejrad.2015.07.017 [DOI] [PubMed] [Google Scholar]
- 55.Hamilton WG, Geppert MJ, Thompson FM. Pain in the posterior aspect of the ankle in dancers. Differential diagnosis and operative treatment. J Bone Joint Surg Am 1996; 78: 1491–500. doi: https://doi.org/10.2106/00004623-199610000-00006 [DOI] [PubMed] [Google Scholar]
- 56.Hedrick MR, McBryde AM. Posterior ankle impingement. Foot Ankle Int 1994; 15: 2–8. doi: https://doi.org/10.1177/107110079401500102 [DOI] [PubMed] [Google Scholar]
- 57.van Dijk CN, Lim LS, Poortman A, Strubbe EH, Marti RK. Degenerative joint disease in female ballet dancers. Am J Sports Med 1995; 23: 295–300. [DOI] [PubMed] [Google Scholar]
- 58.Robinson P, Bollen SR. Posterior ankle impingement in professional soccer players: effectiveness of sonographically guided therapy. AJR Am J Roentgenol 2006; 187: W53–8. doi: https://doi.org/10.2214/AJR.05.0614 [DOI] [PubMed] [Google Scholar]
- 59.Bureau NJ, Cardinal E, Hobden R, Aubin B. Posterior ankle impingement syndrome: MR imaging findings in seven patients. Radiology 2000; 215: 497–503. doi: https://doi.org/10.1148/radiology.215.2.r00ma01497 [DOI] [PubMed] [Google Scholar]
- 60.Zwiers R, Wiegerinck JI, Murawski CD, Smyth NA, Kennedy JG, van Dijk CN. Surgical treatment for posterior ankle impingement. Arthroscopy 2013; 29: 1263–70. doi: https://doi.org/10.1016/j.arthro.2013.01.029 [DOI] [PubMed] [Google Scholar]
- 61.Donovan A, Rosenberg ZS. Extraarticular lateral hindfoot impingement with posterior tibial tendon tear: MRI correlation. AJR Am J Roentgenol 2009; 193: 672–8. doi: https://doi.org/10.2214/AJR.08.2215 [DOI] [PubMed] [Google Scholar]
- 62.Martus JE, Femino JE, Caird MS, Kuhns LR, Craig CL, Farley FA. Accessory anterolateral talar facet as an etiology of painful talocalcaneal impingement in the rigid flatfoot: a new diagnosis. Iowa Orthop J 2008; 28: 1–8. [PMC free article] [PubMed] [Google Scholar]
- 63.Sewell RB. A study of the astragalus. J Anat Physiol 1904; 39(Pt 1): 74–88. [PMC free article] [PubMed] [Google Scholar]
- 64.Sarrafian SK. Biomechanics of the subtalar joint complex. Clin Orthop Relat Res 1993; 290: 17–26. doi: https://doi.org/10.1097/00003086-199305000-00003 [PubMed] [Google Scholar]
- 65.Luhmann SJ, Rich MM, Schoenecker PL. Painful idiopathic rigid flatfoot in children and adolescents. Foot Ankle Int 2000; 21: 59–66. [DOI] [PubMed] [Google Scholar]
- 66.Malicky ES, Crary JL, Houghton MJ, Agel J, Hansen ST, Jr, Sangeorzan BJ. Talocalcaneal and subfibular impingement in symptomatic flatfoot in adults. J Bone Joint Surg Am 2002; 84: 2005–9. doi: https://doi.org/10.2106/00004623-200211000-00015 [DOI] [PubMed] [Google Scholar]
- 67.Ellis SJ, Deyer T, Williams BR, Yu JC, Lehto S, Maderazo A, et al. Assessment of lateral hindfoot pain in acquired flatfoot deformity using weightbearing multiplanar imaging. Foot Ankle Int 2010; 31: 361–71. doi: https://doi.org/10.3113/fai.2010.0361 [DOI] [PubMed] [Google Scholar]
- 68.Metcalfe SA, Bowling FL, Reeves ND. Subtalar joint arthroereisis in the management of pediatric flexible flatfoot: a critical review of the literature. Foot Ankle Int 2011; 32: 1127–39. doi: https://doi.org/10.3113/FAI.2011.1127 [DOI] [PubMed] [Google Scholar]
- 69.Ngai SS, Tafur M, Chang EY, Chung CB. Magnetic resonance imaging of ankle ligaments. Can Assoc Radiol J 2016; 67: 60–8. doi: https://doi.org/10.1016/j.carj.2015.09.002 [DOI] [PubMed] [Google Scholar]