Abstract
In cases of acute stroke, differentiation between an occluded and a patent internal carotid artery (ICA) is crucial for diagnosis and management. Although CT angiography (CTA) can be highly accurate in defining high-grade stenosis and ICA occlusions, misleading ICA occlusion patterns are not rare in patients with acute stroke. We investigated the underlying causes of ICA pseudo-occlusions with CTA with respect to digital subtraction angiography. 11 out of 72 patients had pseudo-occlusion on CTA. Of these, there were three cases of tandem occlusions accompanying high-grade ICA stenosis, five cases of Distal ICA bifurcation occlusion as a result of atrial fibrillation, two cases of cervical ICA dissection and one acute thrombosis of the stent. Consideration of the aforementioned aetiologies by interventionists is warranted, as it may change the planning of endovascular intervention and treatment of acute stroke.
INTRODUCTION
The prevalence of internal internal carotid artery (ICA) occlusion in patients with acute stroke is approximately 24%.1 The diagnosis is mainly based on clinical findings, which are supported by cross-sectional imaging methods.
CT angiography (CTA) is usually used to locate the vascular occlusion level with a high accuracy because the procedure is easily accessible and rapid; furthermore, it also provides the anatomical knowledge for planning the endovascular procedure.2 However, reports using CTA have identified cases of incorrect ICA occlusion compared with digital subtraction angiography (DSA) referred to as carotid artery pseudo-occlusion.3–5
CTA pseudo-occlusion is diagnosed when no visible contrast is detected in the cervical segment or orifice of the ICA and the vessel is found to be patent at the occlusion level by DSA. These are thought to occur because occlusion at different segments of the ICA results in arrested blood flow that inhibits contrast propagation and lumen filling in CTA imaging.6
The aetiologic reasons for pseudo-occlusion defined on CTA can be classified as atherosclerosis and ulcerated plaque at the ICA orifice, cervical ICA dissection, atrial fibrillation (AF) and acute thrombosis of the stent.
We identified 11 (15%) cases of ICA pseudo-occlusions out of 72 patients. This exceeds the rate found by Marquering et al1 of 11%. In contrast, Desole et al6 reported a carotid pseudo-occlusion rate of 2.3%. This difference may have emerged because they studied patients who are chronically occluded, while we only included cases with acute stroke. All DSA images showed a patent extracranial ICA on the side where an occlusion was diagnosed based on CTA.
The mean age in this group was 59 years (23–74 years) and the median National Institutes of Health Stroke Scale score was 20 (11–25) (Table 1).
Table 1.
Age, National Institutes of Health Stroke Scale (NIHSS), CT angiography (CTA) and digital subtraction angiography (DSA) findings and aetiologies of the study group
| Case | Age (years) | NIHSS | CTA | DSA | Aetiology |
|---|---|---|---|---|---|
| 1 (Figure 4a,b) | 74 | 20 | Left CCA distal–ICA occlusion | Carotid T occlusion | AF |
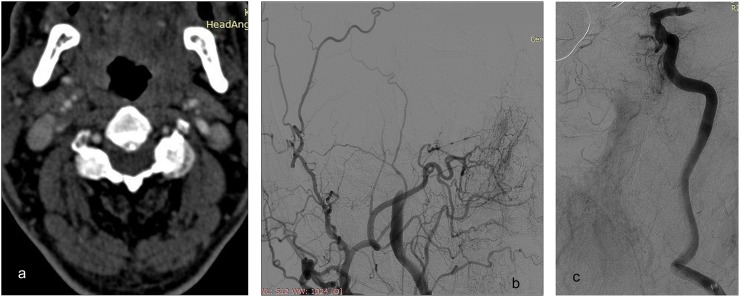
| 2 (Figures 5a,b and c) | 68 | 22 | Right ICA occlusion | ACA orifice and mid-M1 segment of MCA | AF |
| 3 | 65 | 19 | Right ICA proximal occlusion | Carotid T occlusion | AF |
| 4 | 60 | 15 | Right ICA occlusion | ICA orifice right MCA | AF, atherosclerosis |
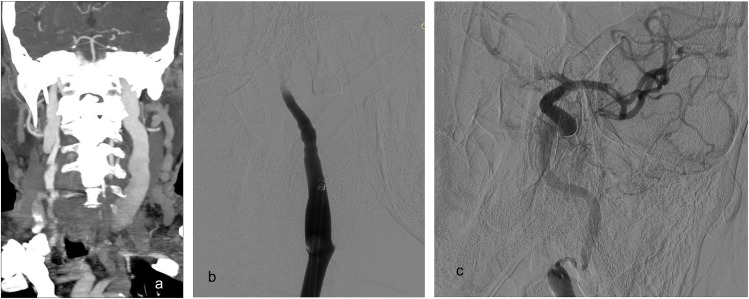
| 5 (Figure 6a–c) | 74 | 25 | Left ICA and ECA proximal occlusion | Carotid T occlusion and ECA occlusion | AF |
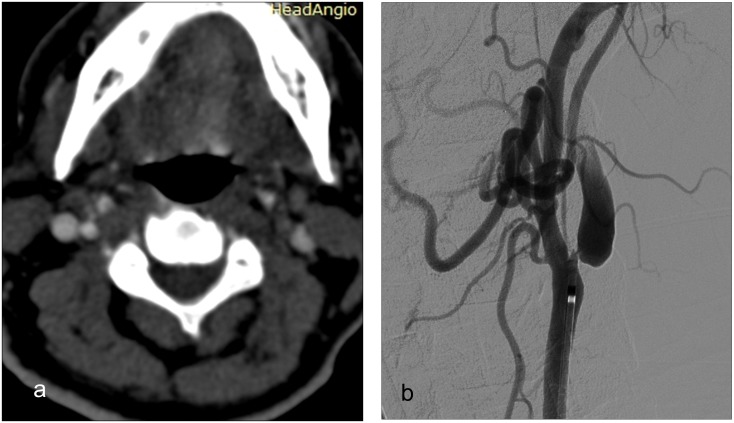
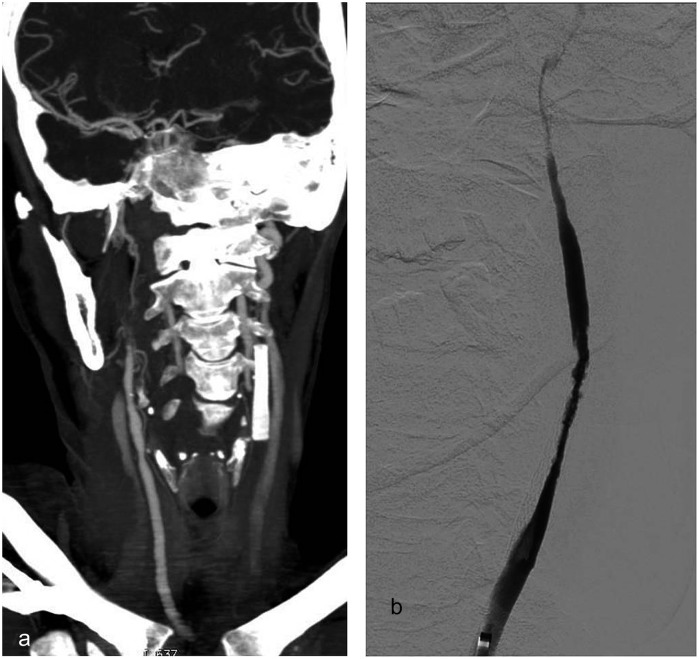
| 6 (Figure 1a,b) | 56 | 21 | Left ICA orifice occlusion | High-grade extracranial ICA stenosis | Atherosclerosis |
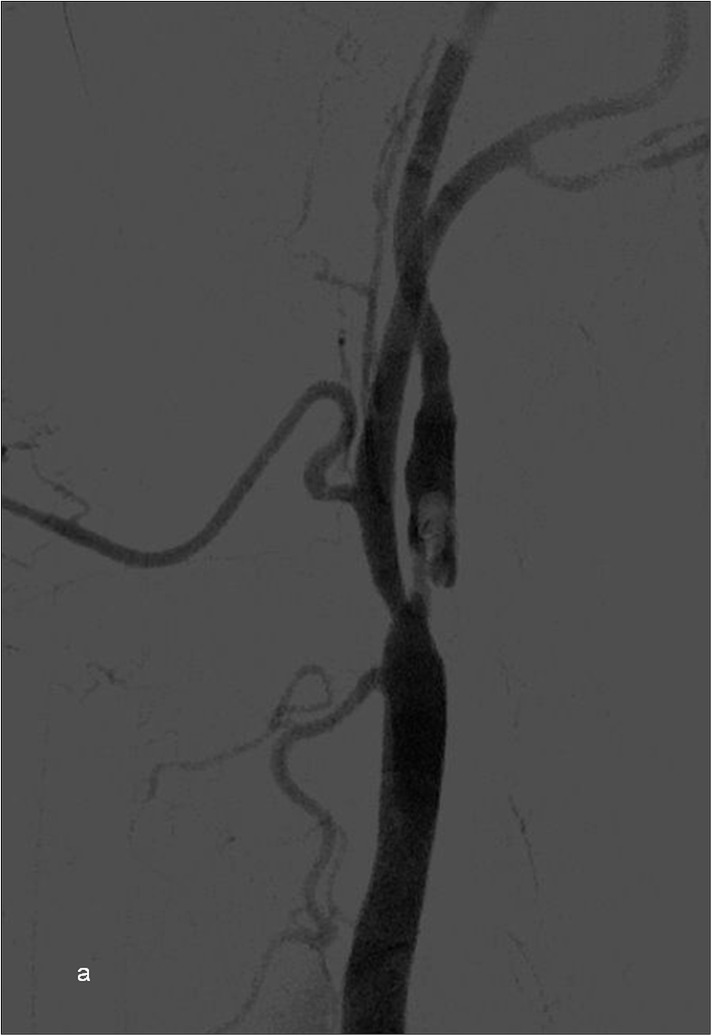
| 7 (Figure 2) | 58 | 24 | Left ICA orifice occlusion | High-grade extracranial ICA stenosis | Atherosclerosis |
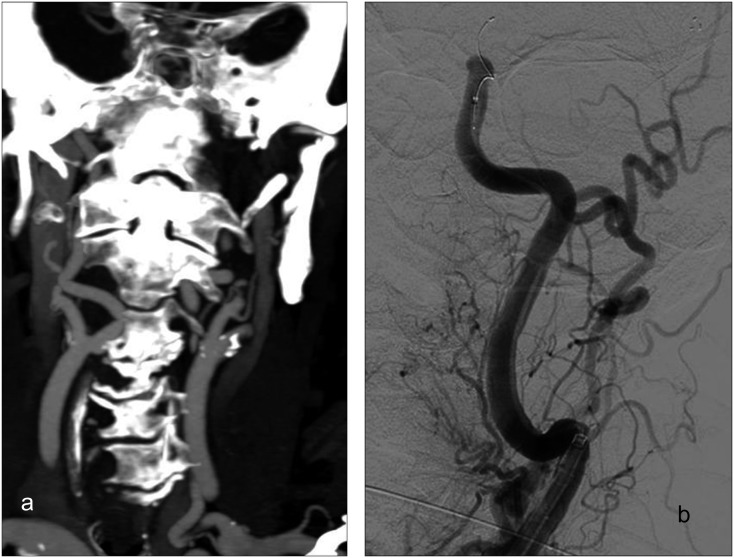
| 8 (Figure 3a,b) | 66 | 14 | ICA orifice occlusion | High-grade extracranial ICA stenosis | Atherosclerosis |
| 9 (Figure 8) | 23 | 11 | Partial contrast enhancement of right ICA orifice | Proximal ICA dissection with thrombus on the wall, left MCA M2 occlusion | Cervical dissection |
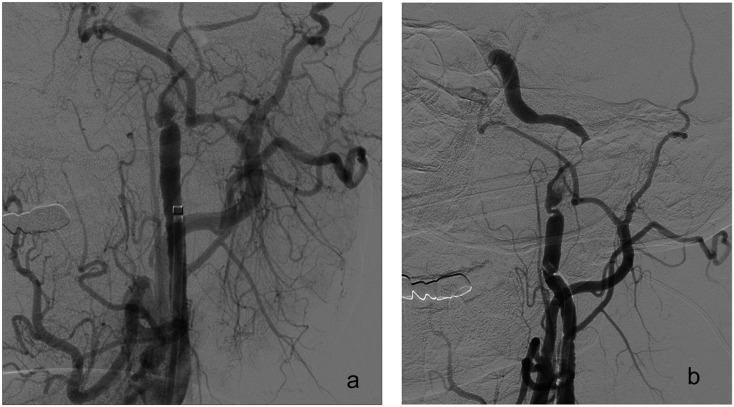
| 10 (Figure 7a,b) | 53 | 19 | Left ICA orifice occlusion | Petrosal ICA dissection with narrowing of the lumen and MCA occlusion | Cervical dissection |
| 11 (Figure 9a,b) | 56 | 21 | Left mid-CCA occlusion | CCA occlusion and high-grade stenosis of CCA–ICA stent lumen | Reocclusion of the stent |
ACA, anterior cerebral artery; AF, atrial fibrillation; CCA, common carotid artery; ECA, external carotid artery; ICA, internal carotid artery; MCA, middle cerebral artery.
Of the 11 patients, 3 patients had tandem occlusions accompanying high-grade proximal ICA stenosis (Figures 1–3). Five cases had an Distal ICA bifurcation (ICA-T) occlusion without proximal occlusion, as a result of AF (Figures 4–6). Two patients had a cervical ICA dissection (Figures 7 and 8) and one patient had an acute reocclusion of the stent, giving rise to a common carotid artery ICA occlusion appearance on CTA (Figure 9). 10 patients underwent recanalization with Thrombolysis in cerebral infarction ≥2b.
Figure 1.
(a) A coronal CT angiography maximum intensity projection image of a 56-year-old female patient with right-sided hemiparesis is showing bilateral internal carotid artery (ICA) orifice occlusion and pseudo-occlusion on the left (black arrow). (b) Digital subtraction angiography of the same patient is showing a high-grade left ICA stenosis with irregular plaques within the ICA orifice and proximal segment (white arrow) exposed after stent-assisted thrombectomy was performed.
Figure 3.
(a) An axial CT angiography section of a 66-year-old male patient is showing loss of contrast enhancement at the left proximal internal carotid artery (ICA). (b) Digital subtraction angiography of the same patient is showing high-grade stenosis of the left ICA orifice resulting in a very slow flow, where we performed ICA stenting to stabilize the ICA access and reach the distal segments of ICA for endovascular stroke treatment.
Figure 4.
(a) Coronal CTA MIP images showing left ICA occlusion of a 74-year-old patient with AF and right-sided hemiplegic (b) A DSA scan showing sluggish flow at the proximal ICA with ICA-T occlusion at the distal tip, which was observed causing a pseudo-occlusion by CTA.
Figure 6.
(a) A left-sided external carotid artery (ECA)–internal carotid artery (ICA) occlusion can be observed in the coronal CT angiography (CTA) maximum intensity projection images of a 74-year-old patient with bilateral internal jugular vein contrast staining clarifying that it is not an early arterial phase CTA. (b) Pseudo-occlusion can be observed in the left ICA with total occlusion in the left ECA following consecutive digital subtraction angiography scans. (c) A tandem occlusion can also be observed in the left anterior cerebral artery A1 segment and small thrombus in the left middle cerebral artery M1 segment in accordance with the proximal ICA dissection flap. SAT was performed to tandem occlusion sites.
Figure 7.
(a) A digital subtraction angiography image of a 53-year-old male patient with left internal carotid artery (ICA) pseudo-occlusion is showing retarded flow at the left ICA proximal segment. (b) Left proximal ICA dissection can be observed at the left cervical ICA, while an Distal ICA bifurcation occlusion can also be spotted at the distal tip. SAT was performed to middle cerebral artery (MCA) occlusion after distal access through the dissected segment. But, the dissection caused repetitive occlusion at the ICA lumen without MCA reocclusion. Control runs from the right-side ICA showed arterial supply to the left MCA by the anterior communicating artery without delay. As a result, stenting was not performed to ICA occlusion.
Figure 8.

A digital subtraction angiography image of a 23-year-old patient who attended the emergency department with progressive left-sided hemiparesis is showing a proximal internal carotid artery (ICA) dissection causing slow flow at the right ICA with tandem middle cerebral artery occlusion. The patient was stented to prevent distal migration.
Figure 9.
(a) A coronal CT angiography maximum intensity projection image of a patient is showing occlusion of the left common carotid artery–internal carotid artery 2 hours after stent replacement. (b) Digital subtraction angiography of the same patient is demonstrating pseudo-occlusion due to acute reocclusion of the stent with central sluggish flow, which was restored after the second SAT was performed (These figures were used in the article: Akpınar et al. Periprocedural complications in endovascular stroke treatment, Br J Radiol 2016; 89: 20150267.
TECHNIQUE
We retrospectively analyzed 72 patients with acute stroke with 85 occlusions. All of the patients underwent neurointerventional treatment under the guidance of DSA (AlluraXper FD20; Philips Medical Systems, Best, Netherlands) after undergoing non-contrast CT and CTA (Somatom Sensation 16; Siemens Medical Solutions, Forchheim, Germany).
An iodinated non-ionic contrast was injected with an automatic injector at 3 ml s−1. CT imaging was initiated from the aortic arcus when arterial contrast staining reached 80-HU density. Contrast injection was initiated before reaching this Hounsfield unit level with a following 3-s delay. At the time, when ICA bifurcation sections were taken, venous staining was also present at cervical and cerebral vessels. The CTA scan encompassed the craniocervical region and maximum intensity projection images were generated in three planes.
General anaesthesia was often used in such cases of ICA occlusions causing severe neurological symptoms. An 8-Fr introducer was usually placed into the puncture site for an anterior circulation stroke, followed by a Simmons 2 catheter (Stryker Neurovascular, Fremont, CA) or vertebral catheter 100/125 cm (Cook, Bloomington, IN) to engage the supra-aortic arteries. A Terumo stiff guidewire (Terumo, Tokyo, Japan) was used to launch the 8-Fr Corail balloon-guiding catheter (Balt, Montmorency, France) to the main arteries.
Ethical approval
All human and animal studies were approved by the ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All patients gave informed consent prior to inclusion in this study.
The aetiologic reasons for pseudo-occlusion defined on CT angiography
Atherosclerosis and ulcerated plaque
Tandem occlusion due to the migration of the plaques from the ulcerated plaque surface of atherosclerotic stenosis is one of the main reasons of ICA pseudo-occlusion. In these cases, the sluggish flow at the high-grade stenotic site may result in a pseudo-occlusion appearance at CTA and may be misdiagnosed as chronic occlusion with the underlying atherosclerotic findings.1,7 Selective DSA runs at the site of occlusion clarify whether the cause is a chronic total occlusion or as a result of the severe stenosis causing this pseudo-occlusion. In our study group, four patients had these appearances owing to atherosclerotic stenosis. Two pathogenic mechanisms could explain this appearance in our patients. The first was an ulcerated plaque causing an acute near-occlusive stenosis at the ICA bifurcation which was recurring, despite recanalization by thrombectomy (Figure 1). The second mechanism was due to repetitive thrombus formation causing distal embolism and focal thrombus extension from the atherosclerotic plaque in the ICA orifice (Figures 2 and 3). Although instant endovascular angioplasty or carotid endarterectomy after stroke treatment could be an option in atherosclerotic ICA stenosis, both cases were treated with wall stent placement owing to the repeated emboli and slow flow even after stent assisted thrombectomy (SAT). Nowadays, in most centres, i.v aspirin is advised promptly and double antiplatelet treatment on the following days in patient wall stents is applied.8,9
Figure 2.
Digital subtraction angiography of a 58-year-old female patient is showing high-grade stenosis and endoluminal elongated thrombus causing pseudo-occlusion appearance at the left proximal internal carotid artery (ICA) and sluggish flow, which was diagnosed as ICA occlusion on CT angiography. Proximal ICA stenting was performed to trap the thrombus elongating from the stenosis site and SAT was applied to distal occlusion.
Atrial fibrillation
The most frequent reason resulting in an ICA pseudo-occlusion appearance in our study group was AF, which was observed in five patients. We realized that different locations of occlusion may give rise to the pseudo-occlusion appearance in the AF group. The main cause was the arrested flow at the long segment of ICA giving rise to pseudo-occlusion appearance on CTA. This was noticed mainly in two groups of patients. In the first group, the pseudo-occlusion appearance was due to both proximal anterior cerebral artery and middle cerebral artery (MCA) occlusion on DSA (Figure 4). In the second group, the reason was Distal ICA bifurcation occlusion, which could only be identified at late phase of DSA run (Figure 5). Other than these groups, both Distal ICA bifurcation occlusion and external carotid artery orifice occlusion were identified in one patient, which resulted in the arrested flow at the occlusion site (Figure 6). All of the cases were treated with SAT using a 40 × 6 mm Solitaire stent (Figures 4–6).
Figure 5.
(a) A right ICA proximal segment occlusion was observed in axial CTA section showing no contrast enhancement at the petrosal and terminal segments (b) DSA of the same patient showed very slow flow at the proximal ICA (c) Occlusions at the ACA orifice and the left MCA M1 segment were also present.
Cervical internal carotid artery dissection
The cervical ICA spontaneous dissection is a common cause of ischaemic stroke in patients younger than 50 years and it accounts for as many as 25% of ischaemic strokes in patients who are young and middle-aged with no gender-based difference.10 Imaging the flame appearance on CTA or DSA is the hallmark of the ICA dissection. The dissection may stay silent on the involved ICA segment, but could also cause a pseudo-occlusion appearance, which could be exposed only by selective DSA runs at the site of occlusion. Pseudo-occlusion in cases of dissections may be due to distal embolization from the site of dissection or as a result of the movement of the dissected vascular flap. Spontaneous dissection-related pseudo-occlusion was noted in two patients in our group. In the first case, ICA occlusion was revealed with proximal ICA DSA runs, which exposed the dissection flap accompanying left MCA occlusion. Although MCA was recanalized by SAT, progressive occlusion was identified at the left ICA runs. Right ICA runs showed the blood flow without delay to the right MCA through the patent anterior communicating artery to the left MCA (Figure 7). The second case was a patient who was young who had irregularity of ICA orifice lumen accompanying MCA occlusion. Dissection was observed in the proximal ICA with tandem MCA partial occlusion (Figure 8). The first case was followed with anticoagulant treatment. Carotid artery stenting was applied to the second case after thrombectomy following the restored flow.
Acute thrombosis of the stent
Whatever the reason for stenosis or occlusion of the ICA was, either the dissection or ulcerated plaques that caused repeated emboli, or sluggish flow in spite of SAT, stenting was prompted as the treatment method to prevent the recurrence of the stroke. Although carotid endarterectomy could be a choice in non-complicating high-grade stenosis, the main concern in patients with acute stroke is the hazard that may complicate the anticoagulation treatment after stenting. If stenting is to be performed for the proximal ICA, dual antiaggregant treatment is advised after stenting to prevent reocclusion, although some centres use i.v. aspirin for the initial treatment followed by a double antiplatelet regime.8,9 In all these applications, although haemorrhage is the most feared outcome, acute thrombosis of the stent could occur. Acute thrombosis of stents, generating a high-grade stenosis, can give rise to tandem occlusions and present as a CT pseudo-occlusion. In one of our cases, although aspirin 300 mg and 300-mg clopidogrel was loaded (via nasogastric tube) in addition to 5000 IU heparin injection after ICA stent deployment, ICA stent thrombosis caused common carotid artery–ICA pseudo-occlusion appearance on CTA which was exposed on DSA runs (Figure 9). If prompt DSA is performed, the true occlusion level or the stenosis grade can be identified that may occur owing to in-stent thrombosis.
CONCLUSION
CTA pseudo-occlusion of the ICA was identified at a rate of 15% in our patient group. The appearance of ICA occlusions in patients with acute stroke who undergo interventions may be a false finding and aetiologies that might be underlying this should be carefully evaluated by both the interventionist and neurologist.
Contributor Information
Süha Akpınar, Email: akpinarsuha@hotmail.com.
Pınar Gelener, Email: drpinargelener@gmail.com.
Güliz Yilmaz, Email: glz.yilmaz@hotmail.com.
REFERENCES
- 1.Marquering HA, Nederkoorn PJ, Beenen LF, Lycklama à Nijeholt GJ, van den Berg R, Roos YB, et al. Carotid pseudo-occlusion on CTA in patients with acute ischemic stroke: a concerning observation. Clin Neurol Neurosurg 2013; 115: 1591–4. doi: https://doi.org/10.1016/j.clineuro.2013.02.008 [DOI] [PubMed] [Google Scholar]
- 2.Koelemay MJ, Nederkoorn PJ, Reitsma JB, Majoie CB. Systematic review of computed tomographic angiography for assessment of carotid artery disease. Stroke 2004; 35: 2306–12. doi: https://doi.org/10.1161/01.STR.0000141426.63959.cc [DOI] [PubMed] [Google Scholar]
- 3.Malhotra AK, Camacho M, Ivatury RR, Davis IC, Komorowski DJ, Leung DA, et al. Computed tomographic angiography for the diagnosis of blunt carotid/vertebral artery injury: a note of caution. Ann Surg 2007; 246: 632–42; discussion 642–3. doi: https://doi.org/10.1097/sla.0b013e3181568cab [DOI] [PubMed] [Google Scholar]
- 4.Kim JJ, Dillon WP, Glastonbury CM, Provenzale JM, Wintermark M. Sixty-four-section multidetector CT angiography of carotid arteries: a systematic analysis of image quality and artifacts. AJNR Am J Neuroradiol 2010; 31: 91–9. doi: https://doi.org/10.3174/ajnr.A1768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Röhrer C, Ertl M, Altmann M, Kasprzak P, Bogdahn U, Schuierer G, et al. Internal carotid artery pseudo occlusion with embolic cerebral ischemia and low flow in the central retinal artery: a diagnostic challenge. Clin Pract 2011; 1: e62. doi: https://doi.org/10.4081/cp.2011.e62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Desole A, Campanile F, Tosato F, Milite D, Surgical treatment for pseudo-occlusion of the internal carotid artery. Interact Cardiovasc Thorac Surg 2015; 20: 636–40. doi: https://doi.org/10.1093/icvts/ivv016 [DOI] [PubMed] [Google Scholar]
- 7.Delgado Almandoz JE, Romero JM, Pomerantz SR, Lev MH. Computed tomography angiography of the carotid and cerebral circulation. Radiol Clin North Am 2010; 48: 265–81. doi: https://doi.org/10.1016/j.rcl.2010.02.007 [DOI] [PubMed] [Google Scholar]
- 8.Lescher S, Czeppan K, Porto L, Singer OC, Berkefeld J. Acute stroke and obstruction of the extracranial carotid artery combined with intracranial tandem occlusion: results of interventional revascularization. Cardiovasc Intervent Radiol 2015; 38: 304–13. doi: https://doi.org/10.1007/s00270-014-1047-2 [DOI] [PubMed] [Google Scholar]
- 9.Chýlová M, Mot'ovská Z, Osmančík P, Procházka B, Kalvach P. The effect of different doses and different routes of acetylsalicylic acid administration on platelet aggregation in healthy volunteers and ischemic stroke patients. Transl Stroke Res 2015; 6: 160–5. doi: https://doi.org/10.1007/s12975-014-0382-6 [DOI] [PubMed] [Google Scholar]
- 10.Blum CA, Yaghi S. Cervical artery dissection: a review of the epidemiology, pathophysiology, treatment, and outcome. Arch Neurosci 2015; 2: 4. doi: https://doi.org/10.5812/archneurosci.26670 [DOI] [PMC free article] [PubMed] [Google Scholar]