Abstract
Background
Emergence delirium (ED) is a state of aggressive agitation that can occur temporarily in the process of emerging from anesthesia in children exposed to volatile or intravenous anesthetics. Emergence delirium is typically assessed using the published and validated Pediatric emergence Delirium (PAED) scale. Due to some variation in properties between sevoflurane and desflurane for maintenance of anesthesia after standard sevoflurane induction, we designed a prospective study to examine potential differences in emergence behavior and incidence of ED in children undergoing elective ear-nose-throat surgery.
Methods
Forty-six children aged 12 months-7 years were randomly assigned to receive either sevoflurane (N.=23) or desflurane (N.=23) for maintenance of general anesthesia. All patients were extubated awake in the OR, and upon arrival in the PACU, PAED scores were assessed every 15 minutes until discharged. In addition to PAED scores, time to tracheal extubation, emergence behavior, pain scores, and recovery complications were recorded.
Results
We found no significant difference in incidence of ED or peak PAED scores between sevoflurane and desflurane groups (12 [0-18] versus 12 [0-20]; P=0.79). There were no significant differences between desflurane and sevoflurane with respect to incidence of adverse events, such as nausea, vomiting, laryngospasm, or excessive secretions.
Conclusions
In conclusion, the use of desflurane for maintenance of anesthesia did not significantly affect the incidence or duration of ED when compared to sevoflurane. However, desflurane did not demonstrate any increase in adverse events, which may support its routine use in this patient population.
Keywords: Anesthesia, adverse effects; Child; Prospective studies; Anesthesia recovery period; Postoperative complications; Delirium, diagnosis
Emergence delirium (ED) is a state of aggressive delirium that can occur temporarily in the process of emerging from anesthesia, and occurs most often during the early stages of emergence.1 Also referred to as emergence agitation, emergence delirium occurs in both adults and children, however the incidence is lower in adults when compared to pediatric patients.2 Emergence delirium is a major source of dissatisfaction for parents, physicians, nurses, and others caring for these children. Patients who experience ED may suffer secondary harm due to displacement of surgical dressings, removal of intravenous access/catheters, disruption of surgical closure, and necessity for restraint by nurses. These patients frequently require additional interventions and may have a prolonged length of stay in the post-anesthesia care unit (PACU), even after short surgical procedures.3
The etiology of ED after general anesthesia with volatile anesthetics in children still remains unclear.4, 5 Numerous studies exist in the literature that have attempted to correlate ED with the use of a particular anesthetic agent or technique. Specifically, the newer, volatile anesthetics, sevoflurane and desflurane, have been implicated in a 20-80% 6, 7 increased incidence of adverse emergence effects, including inconsolable crying, restlessness, and delirium unrelated to pain. However, many of these studies did not use a validated scoring system to assess emergence delirium appropriately.8-12 In 2004, the Pediatric anesthesia emergence Delirium (PAED) scale was validated as a measure of emergence delirium.1
Sevoflurane is the preferred volatile anesthetic for mask induction in pediatric patients because of its pleasant scent and lack of irritation to the upper airways. Despite these advantages, there are some concerns with sevoflurane use, as it is known to potentiate seizure activity and, under certain conditions, produces a nephrotoxic degradation byproduct (pentafuoroisopropenyl fuoromethyl ether, PIFE, or Compound a).13 Desflurane neither potentiates seizure activity nor produces PIFE, but it is less widely used in pediatric anesthesia due to its potential for airway irritation, coughing, and laryngospasm.14 Despite the advantages of sevoflurane and desflurane, including rapid induction of anesthesia (sevoflurane), hemodynamic stability, and fast emergence, ED remains a considerable side effect of these anesthetics that demands increased resources in the PACU.15
The literature is equivocal on the incidence of ED associated with the use of desflurane versus sevoflurane and the previous studies concerning ED in children are complicated by a lack of a validated ED scale and the observed time interval after wake-up from anesthesia.8 Given the existence of many confounding factors regarding emergence delirium, it is hard to draw from a single study a definitive answer about whether sevoflurane results in a higher probability of ED in children as compared to desflurane. We, therefore, designed this study with the primary outcome comparing the incidence of ED in pediatric patients undergoing routine ambulatory ear-nose-throat (ENT) surgery under sevoflurane compared to desflurane anesthesia, using a validated and standardized measurement tool, the PAED scale (Table I). Secondary outcomes measured included postoperative pain scores, incidence of delirium indicated by PAED threshold values, adverse events, and time to discharge from the PACU, as well as to better understand if desflurane is a safe and reasonable option for ENT cases given some aspects of its favorable profile when compared to sevoflurane.
Table I.
Pediatric Anesthesia Emergence Delirium (PAED) Scale.
| score | |
|---|---|
| The child makes eye contact with the caregiver The child's actions are purposeful The child is aware of his/her surroundings |
4 = not at all 3 = just a little 2 = quite a bit 1 = very much 0 = extremely |
| The child is restless The child is inconsolable |
0 = not at all 1 = just a little 2 = quite a bit 3 = very much 4 = extremely |
Maximum total score is 20.
Materials and methods
This was an IRB-approved, prospective, randomized, single-blinded clinical trial, with the rater of the PAED scale being blinded to the volatile anesthetic gas the patient received after standardized sevoflurane induction, as well as other perioperative analgesic and anesthesia management. We enrolled 50 patients between the ages of 12 months-7 years who were scheduled for elective ambulatory adenoidectomy and/or tonsillectomy, with or without concomitant bilateral myringotomy and ventilation tube placement. Patients were assigned via block randomization into two groups. Informed consent and child assent, if age 7, were obtained prior to the procedures.
Every patient received sevoflurane induction followed by either sevoflurane or desflurane maintenance of general anesthesia. Children with a history of asthma requiring daily bronchodilator and/or steroid medications, severe sleep apnea defined as Apnea-Hypoxia index >10, ADHD, autism, developmental delay (including Down Syndrome), neurologic or psychological disorders, were excluded. No patients received any premedication (midazolam or others) for sedation. Patients deemed by anesthesiologist to require premedication were excluded from our study.
Induction of anesthesia was accomplished via inhalation of sevoflurane (8 vol%) in nitrous oxide (70%) and oxygen (30%) at a fresh gas flow of 10 Lpm. All patients had one parent present during the induction of anesthesia. Following loss of consciousness, an IV was established and 2 mg/kg of propofol was administered to facilitate endotracheal intubation. After intubation, all patients received 1.5 mcg/kg of fentanyl and 15 mg/kg IV acetaminophen for analgesia. For maintenance of anesthesia, patients were randomized to receive either sevoflurane (maximum of 2.0±0.2 MAC, age adjusted), or desflurane (maximum 2.0±0.2 MAC, age adjusted), with a constant fresh gas flow of 2 L/min (maximum 40% air mixed with oxygen), using a semiclosed circle breathing system. All volatile agents were measured using an intelliVue Anesthetic Gas Module (Philips Inc., Eindhoven, The Netherlands). Ventilation was controlled to maintain normocapnia (ET-CO2 32-38 mmHg). Removal of the mouth gag for adenoidectomy/tonsillectomy was defined as the end of surgery. At this point, inhalational anesthetics were discontinued and fresh gas flow was increased to 8 Lpm, 100% oxygen. Tracheal extubation was performed when normal ventilation was achieved and cough or gag reflex was regained. If the participant awoke agitated in the operating room, a 1 mg/kg of propofol bolus was administered, with the plan that the patient was not included for monitoring and measurement of emergence delirium as per our protocol.
Upon arrival to the PACU, 1 of 2 PACU nurses were assigned to the recovery of these study patients. This PACU nurse, blinded to the anesthetic management, recorded the degree of delirium using the PAED scale upon arrival to the PACU and every 15 minutes for approximately 1 hour after admission, or until discharge from the PACU, whichever came first. Patients were deemed safe for discharge from the PACU using the standardized Post Anesthesia Recovery Score (PARS) and a self-maintained airway. A total PAED score of >12 at any time was considered to be an indicator of ED.
In addition to PAED scores, age at time of surgery, gender, weight, procedure, duration of surgery, volatile agent used, duration of anesthetic exposure, and time from discontinuation of anesthesia to extubation was documented for each patient by study personnel. Time intervals recorded were the duration of surgery (from time of skin incision to end of surgery), duration of anesthesia (from time of induction to extubation) duration of maintenance anesthesia (from time of intubation to extubation), duration of extubation (from end of surgery to extubation) and duration of PACU stay (from time of PACU admission to discharge). All children were also scored using the Face, Legs, Activity, Cry, Consolability (FLACC) Pain Scale (consisting of a five criteria scale with a 0 score indicating no pain and 10 points indicating the worst possible pain), a self-assessment pain tool that has been tested for validity and reliability in children.16 Other secondary outcomes recorded include the incidence of adverse events (nausea, vomiting, excessive secretions, and laryngospasm) and incidence of ED specified by different PAED scale threshold values (≥10 versus >12).
Statistical analysis
The sample size was determined assuming that the probability of sevoflurane agitation was 40%. We calculated that a sample size of 42 children per treatment group would have at least a 90% power (β error=0.1) to detect a difference of 30% in the incidence of emergence agitation. 50 children were enrolled in this study in order to account from patients who deviated from the protocol and were, therefore, excluded from data analysis.
Demographic variables, anesthetics, surgery data, recovery time, PAED and pain scales, were summarized by anesthetic agents (sevoflurane and desflurane). Categorical variables such as gender, surgery, and adverse events, were summarized by number and percentages of patients. Continuous variables such as age, weight, duration of anesthesia, duration of surgery, duration of maintenance anesthesia, time to extubation, duration of PACU stay, and PAED scores, were presented in either mean±SD or median and range, whichever appropriate. Between group comparisons were conducted using a χ2 or Fisher Exact Test for categorical variables, and a two sample t-test or a Mann-Whitney U test for quantitative variables, as appropriate.
Demographic, anesthetic, and surgery data, were examined to check for any imbalances between the two anesthetics, and if substantial differences were found, these variables were used for the adjustment in the analysis of variance to compare the mean recovery time, PAED Scale, and Pain Score. PAED scores were categorized as >12 (considered as incidence of emergence delirium) or ≤12. Univariable as well as multi-variable logistic regressions were used to compare the proportion of patients with delirium at different time points following admission to the PACU. Odds ratio (OR) of patients with PAED scores >12, 95% confidence intervals and P values, were presented for this comparison. Model and test assumptions were checked before the analysis. All tests were two-tailed at the level of significance of 0.05. The statistical software SPSS version 22.0 (IBM, Chicago, IL, USA) was used for sample size estimation and data analysis.
Results
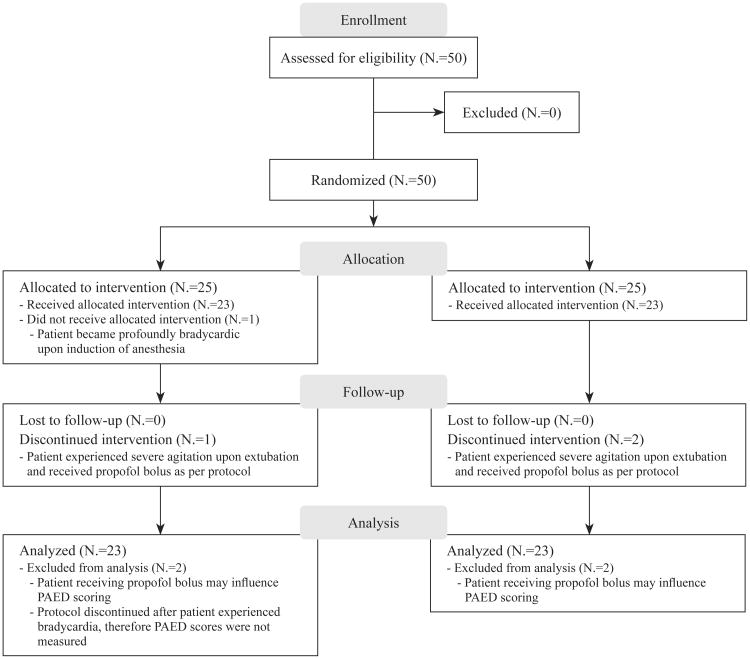
A total of 50 patients were enrolled in the study. One patient in the desflurane group was excluded because of profound bradycardia and was subsequently administered atropine. One patient in the desflurane group and two patients in the sevoflurane group were excluded after experiencing significant delirium upon extubation and received a propofol bolus. Following these exclusions, there were 23 patients analyzed in each group (CONSORT diagram; Figure 1).
Figure 1.
CONSORT trial flow diagram.
Both groups were comparable with respect to age, gender, weight, ASA status, and time from end of surgery to extubation (Table II). There was evidence of a significant difference for duration of maintenance anesthesia, duration of surgery, and total time of anesthesia (Tables II, III). Peak PAED scale scoring in the PACU did not show any significant difference for desflurane (12 [0-20]) as compared to sevoflurane (12 [0-18]). The distribution of PAED scores >12/20 was measured at each of the five time intervals assessed (Table IV). The number of patients with PAED scores >12/20 at least once during the postoperative period was 10/23 (43%) in the sevoflurane group and 8/23 (34%) in the desflurane group (OR=0.69, 95% CI 0.21-2.28; P=0.55). OR of emergence delirium at time of admission to the PACU in desflurane compared to that in sevoflurane was 0.55 (95% CI 0.16-1.92, P=0.35). Time to discharge from PACU initially demonstrated significant advantage for desflurane (31.0±10.8 minutes versus 39.3±14.9; P<0.05), however, after adjusting for duration of anesthesia, time to discharge from the PACU lost its significance (P=0.18). All children in the desflurane group had a PAED score of 0 at time ≤30 minutes following admission to the PACU compared to the sevoflurane group who had one patient with a PAED score of 12 after 1 hour in the PACU (Table IV). There was no significant difference in detecting the incidence of ED using PAED threshold values of ≥10 versus >12 (Table V). No significant differences were found between the study groups with respect to pain or the incidence of adverse events (nausea, vomiting, laryngospasm, excessive secretions).
Table II.
Demographics, anesthetics, and surgery data.
| Sevoflurane (N.=23) | Desflurane (N.=23) | P value (95% CI) a | |
|---|---|---|---|
| ASA status (I/II) | 12/11 | 10/13 | |
| Gender (male/female) | 15/8 | 15/8 | |
| Age (mo) | 55.6±19.7 | 51.1±16.7 | 0.40 |
| Weight (kg) | 17.9±5.3 | 17.9±5.6 | 0.96 |
| Duration of anesthesia (min) | 42.6±13.9 | 35.1±7.9 | 0.03 (0.8-14.2) |
| Surgery time (min) | 20.8±10.5 | 14.2±6.7 | 0.01 (1.4-11.8) |
| End of surgery to extubation (min) | 9.6±3.2 | 8.9±4.4 | 0.54 |
| Surgical procedure | |||
| Tonsillectomy | - | 4 | |
| Adenoidectomy | 7 | 6 | |
| Tonsillectomy and adenoidectomy | 16 | 13 | |
| Myringotomy | 11/23 | 4/23 |
ASA: American Society of Anesthesiologists; CI: confidence interval; Data are presented as mean±SD; Statistical significance was defined as two-tailed P value <0.05.
95% confidence interval of mean difference between sevoflurane and desflurane.
Table III.
Recovery Time, PAED Scale, Pain Score.
| Sevoflurane (N.=23) | Desflurane (N.=23) | P value (95% CI) b | |
|---|---|---|---|
| Duration of maintenance anesthetic (min) | 37.1±14.1 | 28.3±7.1 | 0.01 (2.2-15.1) |
| PAED scale peak in PACU | 12 (0-18) | 12 (0-20) | 0.79 |
| flacc pain score in PACU | 3 (0-9) | 4 (0-10) | 0.63 |
| time to discharge from PACU (min) a | 39.3±14.9 | 31.0±10.8 | 0.18 |
PAED scale: pediatric anesthesia emergence delirium scale; PACU: postanesthesia care unit; FLACC: face, legs, activity, cry, consolability; CI: confidence interval.
Statistical significance was defined as two-tailed P value <0.05; Data are presented as mean±SD or median (range).
Time to discharge from PACU initially demonstrated significant advantage for desflurane (31.0±10.8 minutes versus 39.3±14.9; P=0.03), however, after adjusting for duration of anesthesia, time to discharge from the PACU lost its significance (P=0.18).
95% confidence interval of mean difference between sevoflurane and desflurane.
Table IV.
PAED Scale at admission to PACU, 15 min, 30 min, 45 min, and 1 hour after admission to PACU.
| Group | TA | 15 min | 30 min | 45 mina | 1 hour |
|---|---|---|---|---|---|
| Sevoflurane, N.=23 | |||||
| Median (range) | 12 (0-18) | 5 (0-18) | 3 (0-12) | 1.5 (0-12) | 0 (0-12) |
| Score >12, N. (%) | 9 (39.1) | 3 (13.0) | 1 (4.3) | 0 | 0 |
| Desflurane, N.=23 | |||||
| Median (range) | 12 (0-20) | 5 (0-17) | 0 (0-11) | - | - |
| Score >12, N. (%) | 6 (26.1) | 3 (13.0) | 0 | - | - |
| Odds ratio (95% CI) | 0.55 (0.16-19.2) | 1.0 (0.18-5.60) | - | - | - |
| P value | 0.35 | 1.0 | - | - | - |
PAED scale: pediatric anesthesia emergence delirium scale; PACU: postanesthesia care unit; TA: time of admission to PACU; CI: confidence interval.
All participants who received desflurane for maintenance of general anesthesia had PAED scores: 0 and discharged from the PACU at t≤30 minutes. Odds ratio of delirium in desflurane compared to sevoflurane with 95% CI and P values of odds ratios.
Table V.
Numbers of patients (%) as measured by the PAED Scale.
| Scale used | Numbers of patients with emergence delirium (%) | P value | |
|---|---|---|---|
|
| |||
| Sevoflurane | Desflurane | ||
| PAED≥10 | 16 (69.6) | 17 (73.9) | 0.81 |
| PAED>12 | 10 (43.5) | 8 (34.8) | 0.76 |
PAED: pediatric anesthesia emergence delirium. Statistical significance was defined as two-tailed P value <0.05.
Discussion
Until the utilization of the PAED scale as the measure of emergence delirium in children, there was no valid and/or reliable scale able to accurately characterize the different aspects of ED.1 Despite the validation of the PAED score as a reliable measure to report ED, a threshold value to indicate the presence of ED is still debated.17-19 For example, following the work of Sikich and lerman,1 a PAED Scale of ≥10 was used as a cutoff value to define the presence or absence of ED. More recently, several studies have suggested a PAED score >12 provides a greater sensitivity and specificity than a PAED Score ≥10,17, 20 however this difference was not found to be significant for our study (Table V).
We found that pediatrics patients experienced a peak PAED score within the first 15 minutes of arrival to the PACU, which is consistent with other studies regarding the time of peak emergence delirium following surgery.8, 21 the number of patients with PAED scores >12/20 at least once during the postoperative period was 10/23 (43%) in the sevoflurane group and 8/23 (34%) in the desflurane group. Despite a decreased likelihood (31%) of delirium in the desflurane group compared to sevoflurane, these findings were not found to be statistically significant (Table V). We did, however, find statistically significant differences for duration of maintenance anesthesia, duration of surgery, and total time of anesthesia. These findings can be best explained by chance during the randomization process, which coincidentally led to more patients in the sevoflurane group undergoing concomitant bilateral myringotomy procedures in addition to tonsillectomy and/or adenoidectomy. It was felt that this additional procedure led to the significant increase in surgical time, and thus increased duration of maintenance and total anesthesia for this group.
Initially, our data demonstrated that patients who were assigned desflurane for maintenance of general anesthesia spent a shorter period of time in the PACU as compared to sevoflurane (31.0±10.8 min versus 39.3±14.9; P<0.05). However, after adjusting for duration of anesthesia, time to discharge from the PACU lost its significance (P=0.18). Although adjustment for these variables resulted in a loss of statistical significance, there is still a substantial difference between groups with respect to time to discharge from the PACU. Patients are discharged from the PACU once deemed safe, stable, and have met all discharge criteria. Faster time to discharge from the PACU has several potential advantages. First, given the volume of surgical cases at most busy institutions, faster turnover and discharge from the PACU, once a patient has fulfilled all criteria, minimizes delays for patients to come out of the operative room and into the PACU, which supports overall greater efficiency in perioperative facilities. Although the difference of <10 minutes may not seem clinically important, it should be noted that in our study, 100% of desflurane patients were discharged from the PACU within 30 minutes, while at least three patients who were assigned to sevoflurane for maintenance anesthesia required >45 minutes to be discharged safely from the PACU. The resources required to care for these outliers far outweigh the apparent lesser importance of an average modestly longer length of stay. Second, parents may also experience greater satisfaction not only from not witnessing their child having ED, but also the ability to be discharged earlier, whenever safe and appropriate, after elective ambulatory surgical procedures. Greater safety, efficiency and overall flow of daily work is always a goal for the entire perioperative team and increases staff satisfaction. Safety, efficiency, rapid turnover, as well as greater parental satisfaction, can contribute to a positive financial impact of a hospital. This may be especially beneficial for pediatric hospitals with busy operating rooms that have high patient volumes.
For our study, determining whether sevoflurane or desflurane maintenance anesthesia decreased the incidence of ED in children undergoing ENT surgery has substantial clinical value. Voepel-Lewis et al.3 demonstrated that the prevalence of ED in children undergoing ENT procedures is important, in that patients who underwent ENT surgery experienced emergence delirium significantly more frequently than children undergoing other procedures.3 Our study did not find a significant difference between sevoflurane and desflurane groups in regards peak PAED scores. Studies performed by cohen et al.12 and Demirbilek et al.11 also were unable to identify a difference in delirium between sevoflurane and desflurane for maintenance of general anesthesia. Finally, our study failed to demonstrate a difference in the incidence of adverse events following sevoflurane versus desflurane anesthesia. This finding reinforces other work that has also shown no increased risk of airway complications (coughing, laryngospasm, etc.) following desflurane anesthesia and further dispels the commonly held, but unproven, belief that desflurane should be avoided in pediatric anesthesia because of these issues.
Since the PAED scale has been implemented into clinical practice, research is now focusing on interventions to reduce, with the ultimate goal of eliminating, ED in children. a meta-analysis by Dahmani et al.22 showed that there was a lower incidence and duration of ED in children receiving fentanyl after receiving sevoflurane for general anesthesia. additionally, this study found that postintubation fentanyl may be useful to reduce delirium in PACU even if there is no apparent need of pain control.22 More recent studies have shown that propofol was more effective than fentanyl and associated with lower PAED scores in children who received sevoflurane general anesthesia.23 Specifically, the use of propofol at the end of general anesthesia appears to reduce the incidence of ED and improve the quality of emergence.24 While all of these studies have attempted to reduce the prevalence of ED in children undergoing surgical procedures, there has been no definitive measure in successfully eliminating ED in children.
Limitations of the study
Despite limiting the number of observers measuring PAED scores, one limitation of our study is the subjective variation between the two nurses measuring ED, which may have been reduced with the use of a single individual recording all PAED scores. However, even when using validated scoring methods such as the PAED scale, subjectivity undoubtedly exists between individuals. Variability still exists in regards to the opinions of what defines normal versus abnormal emergence, which also may account for the various definitions of ED found in the literature. Another limitation of our study is the presence of postoperative pain, which makes it exceedingly difficult for medical staff to differentiate between ED and coexisting pain using the PAED and FLACC scores, respectively. In a recent study, somaini et al. emphasized that ED and pain are two distinct entities, which cannot be readily discriminated using PAED and FLACC scores.25 Regardless, the ability to clinically isolate ED from pain is of importance, with the possibility of improving treatment of ED in the future. Another limitation of our study is the measurement of PAED scores at 15-minute intervals. It may have been more precise to have recorded scores at shorter intervals with increased duration of follow-up, however this is uncertain. Finally, because we had found a significant difference in duration of surgery, it may have been more appropriate to limit the surgical procedure to only adenoidectomy and/or tonsillectomy without concomitant bilateral myringotomy, further limiting variability between subjects.
Conclusions
In conclusion, the use of desflurane for maintenance of anesthesia after sevoflurane induction is not associated with a significant difference in incidence or duration of ED following adenoidectomy and/or tonsillectomy in children. Despite this, ED remains a significant obstacle that interferes with a child's recovery in the PACU and challenges doctors, nurses, and other healthcare providers, in terms of assessment and treatment of these patients. While routine ambulatory adenoidectomy and/or adenotonsillectomy are common procedures with relatively short operative times (as short as 10-15 minutes), combined with the volume of cases during a single day, achieving optimal analgesia while minimizing respiratory complications is a major priority concerning pediatric patients. Timely emergence from anesthesia without airway irritation and subsequent laryngospasm are important factors in order to ensure patient safety from the end of the surgical case through recovery in the PACU. Future studies that include additional types of procedures may allow for opportunities to help identify strategies to prevent emergence delirium in children.
Key messages.
— Volatile anesthetics, such as desflurane and sevoflurane, have been implicated in an increased incidence of emergence agitation in children requiring general anesthesia.
— The results show that the use of desflurane for maintenance of general anesthesia is associated with a shorter duration of stay for children in the PACU following ambulatory ENT surgery.
— There was no significant difference in the incidence of emergence delirium when using desflurane as compared to sevoflurane for maintenance of general anesthesia.
— There were no significant differences between desflurane and sevoflurane with respect to incidence of adverse events, such as nausea, vomiting, laryngospasm, or excessive secretions.
— Both desflurane and sevoflurane appear to be safe and reasonable options for maintenance of general anesthesia during ENT surgery in pediatric patients.
Acknowledgments
We would like to thank adam talicska and colleen Mccarthy for their assistance with this study.
Dr. Mychaskiw is a consultant to, has received research funding from and is a member of the professional speakers' bureau of Baxter Healthcare, Inc.
Footnotes
Conflicts of interest. The other authors have no conflicts of interest.
References
- 1.Sikich N, Lerman J. Development and psychometric evaluation of the pediatric anesthesia emergence delirium scale. Anesthesiology. 2004;100:1138–45. doi: 10.1097/00000542-200405000-00015. [DOI] [PubMed] [Google Scholar]
- 2.Kim YS, Chae YK, Choi YS, Min JH, Ahn SW, Yoon JW, et al. A comparative study of emergence agitation between sevoflurane and propofol anesthesia in adults after closed reduction of nasal bone fracture. Korean J anesthesiol. 2012;63:48–53. doi: 10.4097/kjae.2012.63.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Voepel-Lewis T, Malviya S, Tait AR. A prospective cohort study of emergence agitation in the pediatric postanesthesia care unit. Anesth Analg. 2003;96:1625–30. doi: 10.1213/01.ANE.0000062522.21048.61. [DOI] [PubMed] [Google Scholar]
- 4.Lerman J. Inhalational anesthetics. Paediatr Anaesth. 2004;14:380–3. doi: 10.1111/j.1460-9592.2004.01334.x. [DOI] [PubMed] [Google Scholar]
- 5.Welborn LG, Hannallah RS, Norden JM, Ruttimann UE, Callan CM. Comparison of emergence and recovery characteristics of sevoflurane, desflurane, and halothane in pediatric ambulatory patients. Anesth Analg. 1996;83:917–20. doi: 10.1097/00000539-199611000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Davis PJ, Cohen IT, Mcgowan FX, Jr, Latta K. Recovery characteristics of desflurane versus halothane for maintenance of anesthesia in pediatric ambulatory patients. Anesthesiology. 1994;80:298–302. doi: 10.1097/00000542-199402000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Grundmann U, Uth M, Eichner A, Wilhelm W, Larsen R. Total intravenous anaesthesia with propofol and remifentanil in paediatric patients: a comparison with a desflurane-nitrous oxide inhalation anaesthesia. Acta Anaesthesiol Scand. 1998;42:845–50. doi: 10.1111/j.1399-6576.1998.tb05332.x. [DOI] [PubMed] [Google Scholar]
- 8.Cole JW, Murray DJ, Mcallister JD, Hirshberg GE. Emergence behaviour in children: defining the incidence of excitement and agitation following anaesthesia. Paediatr Anaesth. 2002;12:442–7. doi: 10.1046/j.1460-9592.2002.00868.x. [DOI] [PubMed] [Google Scholar]
- 9.Cohen IT, Finkel JC, Hannallah RS, Hummer KA, Patel KM. Rapid emergence does not explain agitation following sevoflurane anaesthesia in infants and children: a comparison with propofol. Paediatr Anaesth. 2003;13:63–7. doi: 10.1046/j.1460-9592.2003.00948.x. [DOI] [PubMed] [Google Scholar]
- 10.Valley RD, Freid EB, Bailey AG, Kopp VJ, Georges LS, Fletcher J, et al. Tracheal extubation of deeply anesthetized pediatric patients: a comparison of desflurane and sevoflurane. Anesth Analg. 2003;96:1320–4. doi: 10.1213/01.ANE.0000058844.77403.16. table of contents. [DOI] [PubMed] [Google Scholar]
- 11.Demirbilek S, Togal T, Cicek M, Aslan U, Sizanli E, Ersoy MO. Effects of fentanyl on the incidence of emergence agitation in children receiving desflurane or sevoflurane anaesthesia. Eur J Anaesthesiol. 2004;21:538–42. doi: 10.1017/s0265021504007069. [DOI] [PubMed] [Google Scholar]
- 12.Cohen IT, Finkel JC, Hannallah RS, Hummer KA, Patel KM. The effect of fentanyl on the emergence characteristics after desflurane or sevoflurane anesthesia in children. Anesth Analg. 2002;94:1178–81. doi: 10.1097/00000539-200205000-00023. [DOI] [PubMed] [Google Scholar]
- 13.Schmidt R, Roeder M, Oeckler O, Simon A, Schurig V. Separation and absolute configuration of the enantiomers of a degradation product of the new inhalation anesthetic sevoflurane. Chirality. 2000;12:751–5. doi: 10.1002/1520-636X(2000)12:10<751::AID-CHIR8>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 14.Murat I. Is there a place for desflurane in paediatric anaesthesia? Paediatr anaesth. 2002;12:663–4. doi: 10.1046/j.1460-9592.2002.00794.x. [DOI] [PubMed] [Google Scholar]
- 15.Uezono S, Goto T, Terui K, Ichinose F, Ishguro Y, Nakata Y, et al. Emergence agitation after sevoflurane versus propofol in pediatric patients. Anesth Analg. 2000;91:563–6. doi: 10.1097/00000539-200009000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Voepel-Lewis T, Zanotti J, Dammeyer JA, Merkel S. Reliability and validity of the face, legs, activity, cry, consolability behavioral tool in assessing acute pain in critically ill patients. Am J Crit Care. 2010;19:55–61. doi: 10.4037/ajcc2010624. [DOI] [PubMed] [Google Scholar]
- 17.Bajwa SA, Costi D, Cyna AM. A comparison of emergence delirium scales following general anesthesia in children. Paediatr Anaesth. 2010;20:704–11. doi: 10.1111/j.1460-9592.2010.03328.x. [DOI] [PubMed] [Google Scholar]
- 18.Pieters BJ, Penn E, Nicklaus P, Bruegger D, Mehta B, Weatherly R. Emergence delirium and postoperative pain in children undergoing adenotonsillectomy: a comparison of propofol vs sevoflurane anesthesia. Paediatr Anaesth. 2010;20:944–50. doi: 10.1111/j.1460-9592.2010.03394.x. [DOI] [PubMed] [Google Scholar]
- 19.Locatelli BG, Ingelmo PM, Emre S, Meroni V, Minardi C, Frawley G, et al. Emergence delirium in children: a comparison of sevoflurane and desflurane anesthesia using the Paediatric anesthesia emergence Delirium scale. Paediatr Anaesth. 2013;23:301–8. doi: 10.1111/pan.12038. [DOI] [PubMed] [Google Scholar]
- 20.Sethi S, Ghai B, Ram J, Wig J. Postoperative emergence delirium in pediatric patients undergoing cataract surgery--a comparison of desflurane and sevoflurane. Paediatr Anaesth. 2013;23:1131–7. doi: 10.1111/pan.12260. [DOI] [PubMed] [Google Scholar]
- 21.Seo IS, Seong CR, Jung G, Park SJ, Kim SY, Kim MM. The effect of sub-Tenon lidocaine injection on emergence agitation after general anaesthesia in paediatric strabismus surgery. Eur J Anaesthesiol. 2011;28:334–9. doi: 10.1097/EJA.0b013e3283426ed6. [DOI] [PubMed] [Google Scholar]
- 22.Dahmani S, Stany I, Brasher C, Lejeune C, Bruneau B, Wood C, et al. Pharmacological prevention of sevoflurane- and desflurane-related emergence agitation in children: a meta-analysis of published studies. Br J Anaesth. 2010;104:216–23. doi: 10.1093/bja/aep376. [DOI] [PubMed] [Google Scholar]
- 23.Kim MS, Moon BE, Kim H, Lee JR. Comparison of propofol and fentanyl administered at the end of anaesthesia for prevention of emergence agitation after sevoflurane anaesthesia in children. Br J Anaesth. 2013;110:274–80. doi: 10.1093/bja/aes382. [DOI] [PubMed] [Google Scholar]
- 24.Costi D, Ellwood J, Wallace A, Ahmed S, Waring L, Cyna A. Transition to propofol after sevoflurane anesthesia to prevent emergence agitation: a randomized controlled trial. Paediatr Anaesth. 2015;25:517–23. doi: 10.1111/pan.12617. [DOI] [PubMed] [Google Scholar]
- 25.Somaini M, Sahillioglu E, Marzorati C, Lovisari F, Engelhardt T, Ingelmo PM. Emergence delirium, pain or both? A challenge for clinicto ians. Paediatr Anaesth. 2015;25:524–9. doi: 10.1111/pan.12580. [DOI] [PubMed] [Google Scholar]