Abstract
Gestational diabetes mellitus (GDM) is linked with several acute maternal health risks and long-term development of type 2 diabetes, metabolic syndrome, and cardiovascular disease. Intrauterine exposure to GDM similarly increases offspring risk of early life health complications and later disease. GDM recurrence is common, affecting 40–73% of women, and augments associated maternal/fetal/child health risks. Modifiable and independent risk factors for GDM include maternal excessive gestational weight gain and pre-pregnancy overweight and obesity. Lifestyle interventions that target diet, activity, and behavioral strategies can effectively modify adiposity. Randomized clinical trials testing the effects of lifestyle interventions during pregnancy to reduce excessive gestational weight gain have generally shown mixed effects on reducing GDM incidence. Trials testing the effects of postpartum lifestyle interventions among women with a history of GDM have shown reduced incidence of diabetes and improved cardiovascular disease risk factors. However, the long-term effects of inter-pregnancy or pre-pregnancy lifestyle interventions on subsequent GDM remain unknown. Future adequately powered and well-controlled clinical trials are needed to determine the effects of lifestyle interventions to prevent GDM and identify pathways to effectively reach reproductive-aged women across all levels of society, before, during, and after pregnancy.
Keywords: Lifestyle intervention, gestational diabetes mellitus, postpartum, preconception, inter-pregnancy
INTRODUCTION
Gestational diabetes mellitus (GDM) is rapidly rising in prevalence and could soon impact one in ten women.1 Women with GDM have elevated risk of preeclampsia, cesarean deliveries, induced labor, and preterm birth2,3 and long-term risk of type 2 diabetes, metabolic syndrome, renal disease,4 and cardiovascular disease.5–10 An estimated 15–25% of women with prior GDM will develop type 2 diabetes within 1–2 years after pregnancy,11–14 and 35%–70% will develop type 2 diabetes 10–15 years after pregnancy.7,8,15,16 Moreover, recurrence of GDM in a subsequent pregnancy is common, affecting 40–73% of women overall 17–26 and 66–80% of women with overweight or obesity.18,27,28 Women with additional pregnancies complicated by GDM experience three-fold increases in health risks.4,29,30 Identification and treatment of GDM in women exacts a high cost to the health care system.31–33
Intrauterine exposure to maternal diabetes also conveys high risk of several short and long-term health problems in offspring.34–36 Exposure to GDM has been linked with birth trauma, respiratory distress syndrome, and neonatal death.37,38 GDM increases risk of excess fetal growth in utero,39 higher infant fat mass,40 neonatal macrosomia, and greater childhood prevalence of obesity (> 90th percentile) through adolescence.41,42 Offspring of women with GDM also have increased risk of type 2 diabetes. In a series of longitudinal studies of Pima Indians, most of the increased prevalence of childhood type 2 diabetes occurring over a 30 year time frame was attributable to increasing exposure to maternal diabetes during pregnancy.43 Other long-term, prospective research has shown adolescent offspring of mothers who had diabetes during pregnancy had a significantly higher prevalence of impaired glucose tolerance (19.3 vs. 2.5%, respectively) and obesity (50% vs. 20%, respectively) than the age- and sex-matched controls,44 and females born with obesity had increased risk of later obesity41 and doubled risk for delivering an obese infant themselves.45
Preventing GDM has the potential to reduce the incidence of diabetes and obesity and halt the transgenerational cycle of disease.36 GDM prevention has been identified as a national health priority46,47 Several approaches have been studied for GDM prevention, including effects of metformin,48,49 probiotics50, myoinositol supplementation,51,52 and bariatric surgery.53 This review focuses on the effects of lifestyle interventions targeting maternal weight, eating, and activity.
Obesity: A Modifiable Risk Factor for GDM
Arguably the strongest modifiable risk factor for GDM is pre-pregnancy overweight or obesity.54,55 Obesity affects approximately 36% of adult women overall56 and 20% of women entering pregnancy.57 Kim et al.58 estimated that half of GDM cases could be prevented by reducing pre-pregnancy obesity alone. In epidemiologic studies, the risk of GDM is four to eight times higher in women with overweight or obesity than normal weight women.58 Similarly, a meta-analysis concluded that for every 1 kg increase in pre-pregnancy BMI, the prevalence of GDM was increased by 0.92%.59 Reducing prenatal obesity may also have impacts on offspring health. Honein et al60 estimated that if 10% of women with pre-pregnancy obesity achieved a healthy weight before pregnancy, nearly 300 congenial heart defects and 700 fetal deaths per year could be prevented each year. Independent of GDM, pre-pregnancy obesity is also associated with several adverse maternal/infant outcomes, including preeclampsia, sleep apnea, macrosomia, induction of labor, cesarean delivery, and post-surgical wound infection.61,62 Independent of pre-pregnancy obesity, excessive gestational weight gain during pregnancy is also an independent risk factor for development of GDM.63 Thus, reducing pre-pregnancy obesity and excessive gestational weight gain both have the potential to reduce GDM but also significantly improve other obesity-related complication and risks of disease.
Effective Lifestyle Interventions for Weight Control
Fortunately, there are effective means of promoting healthy weight loss in women. Research in obesity treatment and prevention has identified several dietary, physical activity, and behavioral strategies effective in promoting long-term weight loss (Table 1). Well-controlled randomized trials over the past 30 years have painted a consistent picture of the effective treatment components.64–67 The most effective weight control programs combine calorie restriction, high levels of physical activity, and behavioral strategies, including frequent self-monitoring of diet and body weight. Structured meal plans, partial meal-replacement programs, and ongoing patient-provider contact also appear to improve both short and long-term weight loss outcomes. Moreover, treatment can be delivered over many modalities (in-person, phone-based, internet).68
Table 1.
Variables associated with successful weight control
| Calorie prescription |
| Meal replacements/structured meal plan |
| High physical activity goals (60–90 min/d) |
| Daily self-weighing of body weight |
| Daily monitoring of food intake |
| Behavior therapy |
| Continued patient-provider contact (≥2/mo) |
Clinical trials testing the effects of comprehensive behavioral programs have found weight losses averaging about 10.7 kg (11% of body weight) over 30 weeks.66,69 Nonetheless, even with comprehensive behavioral treatment, gradual weight regain is often observed overtime, resulting in modest (~5%) overall weight losses at 3–4 years.64,70 Even with weight regain, however, improvements in long-term health occur.64 The Diabetes Prevention Program (DPP) Research Group conducted a large, randomized clinical trial involving adults (> 25 y) in the US who had a BMI ≥ 24 and elevated glucose concentrations, making them at high risk for the development of type 2 DM.64,71 The DPP lifestyle intervention produced a 5.6 kg weight loss at 3 years and reduced the risk of developing diabetes by 58%; the intervention also reduced high blood pressure and metabolic syndrome.64 Similarly, other research has shown that lifestyle interventions that promote modest weight loss prevent or delay development of type 2 diabetes in adults with impaired glucose tolerance. 72 In a study of patients with type 2 diabetes, the Look AHEAD trial’s lifestyle intervention produced an 8.6% weight loss at 1 year and a nearly 5% weight loss maintained at 8 years.73 The intervention did not reduce cardiovascular events, such as heart attack and stroke,74 but was associated with improved diabetes control and reduction in cardiovascular disease risk factors and medication use.70,75 Overall, comprehensive lifestyle interventions can promote sustained, modest weight losses that translate into significant health benefits and hold potential for improving the health of women at risk for GDM and its recurrence.
Lifestyle Interventions: Before, During, and/or After pregnancy
During Pregnancy
The National Academy of Science Institute of Medicine (IOM) has formulated specific recommendations based on maternal pre-pregnancy BMI for gestational weight gain ranges that are associated with optimal maternal/child health outcomes.76 However, approximately 35% of normal weight women and 60% of obese women gain more than recommended.77 Excessive gestational weight gain prior to glucose screening is a consistent predictor of GDM, independent of maternal pre-pregnancy BMI.63 Thus, efforts to prevent GDM have focused extensively on testing lifestyle interventions to prevent excessive gestational weight gain and promote healthy eating and activity early during pregnancy.78–84
Randomized clinical trials testing the effects of prenatal interventions to reduce excessive gestational weight gain and incidence of GDM have generally found no significant effects of lifestyle interventions vs. control conditions for the prevention of GDM. 79,81,83,84 Thus, a 2015 Cochrane review concluded no significant differences in the risk of GDM between women receiving prenatal diet and exercise interventions vs. standard care;85 this conclusion has been echoed in other reviews.86,87 A meta-analysis of randomized controlled trials testing prenatal physical activity intervention concluded that physical activity in pregnancy provided only a slight protective effect against the development of GDM.88 GDM prevention interventions that begin during pregnancy may have reduced efficacy due to: 1) low intervention intensity during pregnancy out of concerns over effects on growing fetus; 2) biological changes in pregnancy creating added barriers to adherence (e.g., craving, nausea, edema, weight gain); and, 3) a very short intervention window (2 months) to intervene prior to GDM diagnosis. Notably, the scientific literature to date has been limited by lack of power, variability in interventions, and lack of intervention uptake.86,87
More recently, the RADIEL trial in Finland reported that lifestyle intervention early in pregnancy (< 20 weeks gestation) targeting diet, activity, and weight control significantly reduced gestational weight gain (−0.58 kg) and the incidence of GDM relative to a control group (incidence was 13.9% vs. 21.6%, respectively).89,90 The RADIEL intervention enrolled only women with obesity and was innovative in encouraging no weight gain in the first two trimesters. Ongoing trials are further testing the efficacy of interventions during pregnancy to prevent GDM91,92,90,93 including two US-based studies.94–96 The results of these trials will provide critical information on the efficacy of intervening during pregnancy to prevent GDM.
Postpartum interventions
The time period after pregnancy has also been proposed as an opportune time for intervention to reduce risk of developing type 2 diabetes and related comorbidities in women with a history of GDM. Postpartum diet and exercise interventions specifically for women with prior GDM have shown promise in reducing insulin resistance and diabetes and cardiovascular disease risk factors (Table 2).94,95,97–106 For example, the Tianjin GDM Prevention Program in China enrolled 1180 women (normal and overweight/obese) with prior GDM and randomized participants to a lifestyle intervention targeting diet, activity, and weight control or a control group.100 After 1 year, average weight losses as a percentage of study entry weight were 2.1% in the intervention group vs 0.3% in the control group, and the decrease was more significant among overweight/obese women in the intervention (4.2%) compared with the control group (0.7%). Importantly, the intervention’s modest weight losses significantly reduced diabetes risk factors, including fasting insulin and insulin resistance. Other work from the DPP study found similar - albeit more dramatic - results. The DPP included women with previous histories of GDM,103 and, consistent with the full sample results, the behavioral weight loss intervention significantly reduced the incidence of type 2 diabetes in women with prior GDM by 50% compared with the placebo group.103,64
Table 2.
Randomized controlled trials of lifestyle interventions after gestational diabetes mellitus
| Study reference | Setting & Study duration | Intervention targets | Modality | Impact on weight | Impact on DM biomarkers | |
|---|---|---|---|---|---|---|
|
| ||||||
| Activity | Diet | |||||
| Ratner et al. 2008103 | US 3 y |
Y | Y | In person | Y | Y (T2DM) |
| Hu et al., 2012100 | China 1 y |
Y | Y | In person | Y | Y (insulin) |
| Shyam et al., 2013145 | Malaysia 6 mo |
N | Y | In person/text message/email | Y | N |
| Wein et al., 1999146 | Australia 1–5 y |
N | Y | Telephone/mailing | N/A | Y (T2DM) |
|
| ||||||
| PILOT STUDIES | ||||||
| Reinhardt et al. 2012147 | US 6 mo |
Y | Y | Motivational interviewing/Telephone/mailing | Y | NA |
| Cheung et al., 2011148 | Australia 1 y |
Y | N | In person/telephone/mailing | N | NA |
| Ferrara et al., 201197 | US 1 year |
Y | Y | In person/telephone | N | NA |
| Kim et al., 2012149 | US 3 mo |
Y | N | Web | N | N |
| McIntyre et al., 2012150 | Australia 3 mo |
Y | N | In person/telephone | N | N |
Y=yes; N=no; N/A=non applicable; mo=months; y=years; T2DM= type 2 diabetes mellitus; US= United States. GI= Glycemic index
Interconception or preconceptional interventions
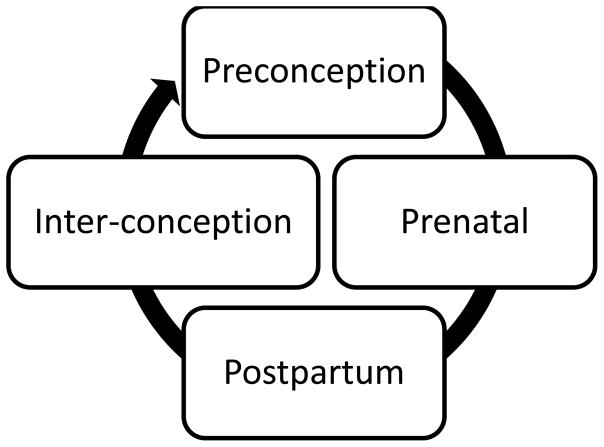
Of course, the postpartum period may also be conceptualized as an interconception or preconceptional period in mothers who are planning (or who will) have additional children (Figure 1). Inter-pregnancy weight gain has been shown to significantly augment risk of GDM and its recurrence. An analysis of 22,351 women in the Kaiser Permanente Northern California Pregnancy Glucose Tolerance Registry found that a gain of 1 to 2 body mass index (BMI) unit between the first and second pregnancy increased risk of GDM by 71%; higher gains doubled and tripled risk of GDM.107 Conversely, a loss of more than 2 BMI units between the first and second pregnancy reduced odds of GDM by 68%. Other epidemiological research suggests that even modest weight losses (> 10 pounds) 108–110 or less weight gain111–113 prior to pregnancy reduces risk of GDM development compared to women who maintain weight or gain >10 pounds. Retrospective data from bariatric surgery populations also suggest that weight loss in obese women prior to pregnancy may reduce the risk of GDM 114–116 and prevent transmission of obesity to children.117 While the findings from observational studies are intriguing, no known clinical trials to date (Table 2) have examined the effect of postpartum weight control interventions on subsequent pregnancy and maternal/child health outcomes among women with prior GDM.
Figure 1.
Continuum of care model for health of mothers
Barriers and Motivators for Lifestyle Change
Several barriers exist in intervening in the postpartum/inter-pregnancy period among women with a history of GDM.118,119 In addition to usual barriers that mothers face after having a baby (fatigue, unpredictable schedules, childcare demands, return to work, financial concerns), women with prior GDM are more likely to also be managing infant health issues, lactation failure, elevated depressive symptoms, and feelings of frustration with healthcare. 118–120 However, timing interventions after pregnancy may also capitalize on a “teachable moment’ for promoting long-term behavior change in women with prior GDM. “Teachable moments” are naturally occurring life transitions or health events thought to augment motivation for adopting risk-reducing health behaviors.121,122 Women with prior GDM report high motivation to change behaviors to protect their health and/or the health of their future child.119,123,124 Data from populations at high-risk of type 2 diabetes, such as Pima Indians125 and Mexican Americans, indicate that some women with a history of GDM may be unaware that GDM poses risks after pregnancy, underscoring another potential motivational target for interventions in the postpartum period.
Future Directions
This is an exciting time for research in prevention of GDM and associated adverse maternal/child health outcomes. The evidence in support of lifestyle interventions after GDM to reduce type 2 diabetes and other disease risk factors is compelling, and some preliminary and ongoing studies suggest the potential for early interventions in pregnancy to reduce incidence of GDM. Several questions merit further investigation.
Can lifestyle interventions during the inter-pregnancy/pre-pregnancy period prevent GDM? As reviewed above, optimizing maternal weight and the intrauterine environment before pregnancy holds promise for preventing GDM recurrence and improving short and long-term maternal/child health outcomes. Postpartum weight loss interventions in women with prior GDM may reduce insulin resistance and diabetes and cardiovascular disease risk factors,94,95,97–106 but effects of postpartum interventions on subsequent maternal/child outcomes have not been investigated. Intervening in the immediate postpartum period may be too distal from subsequent pregnancy to exert a protective effect on GDM recurrence; alternatively, timing interventions soon after a pregnancy complicated by GDM may capitalize on heightened motivation for mothers to reduce GDM recurrence. Although an estimated 45% of pregnancies are unplanned,126 some studies suggest that pre-pregnancy lifestyle weight loss intervention is feasible among women planning pregnancy.127–134 Future research should test whether and how optimizing maternal weight before pregnancy can prevent GDM and its recurrence.
What are the most effective postpartum interventions to reach women after pregnancies complicated by GDM? Postpartum women face several challenges to attending traditional face-to-face weight loss interventions; this may explain the high attrition rates (30–40%) seen in many postpartum weight loss programs.135–138 Delivering weight loss intervention via telephone and/or other modalities (i.e., internet, mobile technology) may offer an alternative to face-to-face interventions68 and may be particularly useful for postpartum women.139 Regardless of modality, sufficient “dose” of treatment and incorporation of evidence-based weight control strategies are likely more important in determining postpartum intervention efficacy.68
Can we envision a future healthcare model that conceptualizes a continuum of care? Most women in the US have access to health care and insurance during pregnancy but may lose coverage postpartum. The expansion of Medicaid in some states and the Affordable Care Act has increased the number of women who have access to insurance coverage for postpartum and preconception healthcare visits. The Affordable Care Act requires insurance coverage of at least one preconception visit without charging a co-payment. Nevertheless, we are far from a model of care that views pre-pregnancy, prenatal, and postpartum care as a continuum of opportunity for disease prevention interventions in mothers and the next generation. Only 48% of women with prior GDM receive postpartum screening for type 2 diabetes mellitus.140 A continuation of services is likely needed to facilitate greater screening for diabetes, weight control counseling, and follow-up of social, behavioral, or physical health problems that may have been identified during pregnancy. Systems are in place that reach reproductive aged women before, during, and after pregnancy. The Maternal, Infant and Early Childhood Home Visiting Program and the Women, Infants, and Children (WIC) Food Supplementation program serves millions of women and young children in the US each month. However, until a larger evidence base shows significant maternal and child health benefit to preconception, prenatal, and postnatal lifestyle interventions, healthcare systems will have little mandate to create an affordable and accessible continuum of care for women and children.
CONCLUSION
More than 200,000 women in the US receive a diagnosis of GDM each year141 and are likely to experience acute pre- and perinatal complications and long-term development of type 2 diabetes, metabolic syndrome, and cardiovascular disease. Children exposed to GDM similarly experience increased risk of early life complications and long-term development of disease. GDM disproportionately impacts women of low socioeconomic status and those of Hispanic, Native-American, Asian, and African-American descent.18,27,28,142–144 Since GDM exerts strong transgenerational effects on obesity and diabetes in offspring, a vicious cycle of social disparities in disease may be promulgated via exposure to GDM. Comprehensive weight loss programs after GDM can reduce diabetes and other disease risk factors. The American College of Obstetrics and Gynecology and the American Diabetes Association both recommend that women with prior GDM be counseled about the benefits of diet, exercise, and weight loss in an effort to prevent the development of type 2 diabetes. However, a critical next step in research is to develop and test innovative methods to reach and improve the health status of reproductive-aged women before pregnancy and across all levels of society.
Acknowledgments
This was funded, in part, by a grant from Eunice Kennedy Shriver National Institute of Child Health and Human Development (1RO1HD084282)
References
- 1.Sacks DA, Hadden DR, Maresh M, et al. Frequency of gestational diabetes mellitus at collaborating centers based on IADPSG consensus panel-recommended criteria: the Hyperglycemia and Adverse Pregnancy Outcome (HAPO) Study. Diabetes Care. 2012;35:526–8. doi: 10.2337/dc11-1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kjos SL, Buchanan TA. Gestational diabetes mellitus. N Engl J Med. 1999;341:1749–56. doi: 10.1056/NEJM199912023412307. [DOI] [PubMed] [Google Scholar]
- 3.Kim C. Gestational diabetes: risks, management, and treatment options. Int J Womens Health. 2010;2:339–51. doi: 10.2147/IJWH.S13333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beharier O, Shoham-Vardi I, Pariente G, et al. Gestational Diabetes Mellitus is a Significant Risk Factor for Long Term Maternal Renal Disease. J Clin Endocrinol Metab. 2015 doi: 10.1210/jc.2014-4474. jc20144474. [DOI] [PubMed] [Google Scholar]
- 5.Vohr BR, Boney CM. Gestational diabetes: the forerunner for the development of maternal and childhood obesity and metabolic syndrome? J Matern Fetal Neonatal Med. 2008;21:149–57. doi: 10.1080/14767050801929430. [DOI] [PubMed] [Google Scholar]
- 6.Kaaja R, Ronnemaa T. Gestational diabetes: pathogenesis and consequences to mother and offspring. The review of diabetic studies. RDS. 2008;5:194–202. doi: 10.1900/RDS.2008.5.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Linne Y, Barkeling B, Rossner S. Natural course of gestational diabetes mellitus: long term follow up of women in the SPAWN study. BJOG. 2002;109:1227–31. doi: 10.1016/s1470-0328(02)01973-0. [DOI] [PubMed] [Google Scholar]
- 8.O’Sullivean JB. Subsequent morbidity among gestational diabetic women. In: Sutherland HWSJ, editor. Carbohydrate Metabolism in Pregnancy and the Newborn. Edingburgh: Churchill Livingstone; 1984. pp. 174–80. [Google Scholar]
- 9.Meigs JB, Larson MG, D’Agostino RB, et al. Coronary artery calcification in type 2 diabetes and insulin resistance: the framingham offspring study. Diabetes Care. 2002;25:1313–9. doi: 10.2337/diacare.25.8.1313. [DOI] [PubMed] [Google Scholar]
- 10.Gunderson EP, Chiang V, Pletcher MJ, et al. History of gestational diabetes mellitus and future risk of atherosclerosis in mid-life: The Coronary Artery Risk Development in Young Adults study. Journal of the American Heart Association. 2014;3:e000490. doi: 10.1161/JAHA.113.000490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Conway DL, Langer O. Effects of new criteria for type 2 diabetes on the rate of postpartum glucose intolerance in women with gestational diabetes. Am J Obstet Gynecol. 1999;181:610–4. doi: 10.1016/s0002-9378(99)70500-4. [DOI] [PubMed] [Google Scholar]
- 12.Ferrara A, Peng T, Kim C. Trends in postpartum diabetes screening and subsequent diabetes and impaired fasting glucose among women with histories of gestational diabetes mellitus: A report from the Translating Research Into Action for Diabetes (TRIAD) Study. Diabetes Care. 2009;32:269–74. doi: 10.2337/dc08-1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schaefer-Graf UM, Buchanan TA, Xiang AH, Peters RK, Kjos SL. Clinical predictors for a high risk for the development of diabetes mellitus in the early puerperium in women with recent gestational diabetes mellitus. Am J Obstet Gynecol. 2002;186:751–6. doi: 10.1067/mob.2002.121895. [DOI] [PubMed] [Google Scholar]
- 14.Kim C, Newton KM, Knopp RH. Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabetes Care. 2002;25:1862–8. doi: 10.2337/diacare.25.10.1862. [DOI] [PubMed] [Google Scholar]
- 15.Bellamy L, Casas JP, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet. 2009;373:1773–9. doi: 10.1016/S0140-6736(09)60731-5. [DOI] [PubMed] [Google Scholar]
- 16.Lauenborg J, Hansen T, Jensen DM, et al. Increasing incidence of diabetes after gestational diabetes: a long-term follow-up in a Danish population. Diabetes Care. 2004;27:1194–9. doi: 10.2337/diacare.27.5.1194. [DOI] [PubMed] [Google Scholar]
- 17.Grant PT, Oats JN, Beischer NA. The long-term follow-up of women with gestational diabetes. Aust N Z J Obstet Gynaecol. 1986;26:17–22. doi: 10.1111/j.1479-828x.1986.tb01521.x. [DOI] [PubMed] [Google Scholar]
- 18.Gaudier FL, Hauth JC, Poist M, Corbett D, Cliver SP. Recurrence of gestational diabetes mellitus. Obstet Gynecol. 1992;80:755–8. [PubMed] [Google Scholar]
- 19.Wein P, Dong ZG, Beischer NA, Sheedy MT. Factors predictive of recurrent gestational diabetes diagnosed before 24 weeks’ gestation. Am J Perinatol. 1995;12:352–6. doi: 10.1055/s-2007-994495. [DOI] [PubMed] [Google Scholar]
- 20.McGuire V, Rauh MJ, Mueller BA, Hickock D. The risk of diabetes in a subsequent pregnancy associated with prior history of gestational diabetes or macrosomic infant. Paediatr Perinat Epidemiol. 1996;10:64–72. doi: 10.1111/j.1365-3016.1996.tb00027.x. [DOI] [PubMed] [Google Scholar]
- 21.Moses RG. The recurrence rate of gestational diabetes in subsequent pregnancies. Diabetes Care. 1996;19:1348–50. doi: 10.2337/diacare.19.12.1348. [DOI] [PubMed] [Google Scholar]
- 22.Spong CY, Guillermo L, Kuboshige J, Cabalum T. Recurrence of gestational diabetes mellitus: identification of risk factors. Am J Perinatol. 1998;15:29–33. doi: 10.1055/s-2007-993894. [DOI] [PubMed] [Google Scholar]
- 23.Major CA, deVeciana M, Weeks J, Morgan MA. Recurrence of gestational diabetes: who is at risk? Am J Obstet Gynecol. 1998;179:1038–42. doi: 10.1016/s0002-9378(98)70211-x. [DOI] [PubMed] [Google Scholar]
- 24.Foster-Powell KA, Cheung NW. Recurrence of gestational diabetes. Aust N Z J Obstet Gynaecol. 1998;38:384–7. doi: 10.1111/j.1479-828x.1998.tb03092.x. [DOI] [PubMed] [Google Scholar]
- 25.MacNeill S, Dodds L, Hamilton DC, Armson BA, VandenHof M. Rates and risk factors for recurrence of gestational diabetes. Diabetes Care. 2001;24:659–62. doi: 10.2337/diacare.24.4.659. [DOI] [PubMed] [Google Scholar]
- 26.Khambalia AZ, Ford JB, Nassar N, Shand AW, McElduff A, Roberts CL. Occurrence and recurrence of diabetes in pregnancy. Diabet Med. 2013;30:452–6. doi: 10.1111/dme.12124. [DOI] [PubMed] [Google Scholar]
- 27.Kim C, Berger DK, Chamany S. Recurrence of gestational diabetes mellitus: a systematic review. Diabetes Care. 2007;30:1314–9. doi: 10.2337/dc06-2517. [DOI] [PubMed] [Google Scholar]
- 28.Philipson EH, Super DM. Gestational diabetes mellitus: does it recur in subsequent pregnancy? Am J Obstet Gynecol. 1989;160:1324–9. doi: 10.1016/0002-9378(89)90851-x. discussion 9–31. [DOI] [PubMed] [Google Scholar]
- 29.Aloba OO, Adewuya AO, Ola BA, Mapayi BM. Validity of the Pittsburgh Sleep Quality Index (PSQI) among Nigerian university students. Sleep Med. 2007;8:266–70. doi: 10.1016/j.sleep.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 30.Beck SL, Schwartz AL, Towsley G, Dudley W, Barsevick A. Psychometric evaluation of the Pittsburgh Sleep Quality Index in cancer patients. J Pain Symptom Manage. 2004;27:140–8. doi: 10.1016/j.jpainsymman.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 31.Committee opinion no. 504: Screening and diagnosis of gestational diabetes mellitus. Obstet Gynecol. 2011;118:751–3. doi: 10.1097/AOG.0b013e3182310cc3. [DOI] [PubMed] [Google Scholar]
- 32.National Institutes of Health consensus development conference statement: diagnosing gestational diabetes mellitus, March 4–6, 2013. Obstet Gynecol. 2013;122:358–69. doi: 10.1097/AOG.0b013e31829c3e64. [DOI] [PubMed] [Google Scholar]
- 33.Chen Y, Quick WW, Yang W, et al. Cost of gestational diabetes mellitus in the United States in 2007. Population health management. 2009;12:165–74. doi: 10.1089/pop.2009.12303. [DOI] [PubMed] [Google Scholar]
- 34.Silverman BL, Rizzo TA, Cho NH, Metzger BE. Long-term effects of the intrauterine environment. The Northwestern University Diabetes in Pregnancy Center. Diabetes Care. 1998;21(Suppl 2):B142–9. [PubMed] [Google Scholar]
- 35.Dabelea D. The predisposition to obesity and diabetes in offspring of diabetic mothers. Diabetes Care. 2007;30(Suppl 2):S169–74. doi: 10.2337/dc07-s211. [DOI] [PubMed] [Google Scholar]
- 36.Barbour LA. Changing perspectives in pre-existing diabetes and obesity in pregnancy: maternal and infant short and long-term outcomes. Current opinion in endocrinology, diabetes, and obesity. 2014 doi: 10.1097/MED.0000000000000079. [DOI] [PubMed] [Google Scholar]
- 37.Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med. 2005;352:2477–86. doi: 10.1056/NEJMoa042973. [DOI] [PubMed] [Google Scholar]
- 38.Macintosh MC, Fleming KM, Bailey JA, et al. Perinatal mortality and congenital anomalies in babies of women with type 1 or type 2 diabetes in England, Wales, and Northern Ireland: population based study. BMJ. 2006;333:177. doi: 10.1136/bmj.38856.692986.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pedersen J. Weight and length at birth of infants of diabetic mothers. Acta Endocrinol (Copenh) 1954;16:330–42. doi: 10.1530/acta.0.0160330. [DOI] [PubMed] [Google Scholar]
- 40.Catalano PM, Thomas A, Huston-Presley L, Amini SB. Increased fetal adiposity: a very sensitive marker of abnormal in utero development. Am J Obstet Gynecol. 2003;189:1698–704. doi: 10.1016/s0002-9378(03)00828-7. [DOI] [PubMed] [Google Scholar]
- 41.Petitt DJ, Bennett PH, Knowler WC, Baird HR, Aleck KA. Gestational diabetes mellitus and impaired glucose tolerance during pregnancy. Long-term effects on obesity and glucose tolerance in the offspring. Diabetes. 1985;34(Suppl 2):119–22. doi: 10.2337/diab.34.2.s119. [DOI] [PubMed] [Google Scholar]
- 42.Philipps LH, Santhakumaran S, Gale C, et al. The diabetic pregnancy and offspring BMI in childhood: a systematic review and meta-analysis. Diabetologia. 2011;54:1957–66. doi: 10.1007/s00125-011-2180-y. [DOI] [PubMed] [Google Scholar]
- 43.Dabelea D, Hanson RL, Bennett PH, Roumain J, Knowler WC, Pettitt DJ. Increasing prevalence of Type II diabetes in American Indian children. Diabetologia. 1998;41:904–10. doi: 10.1007/s001250051006. [DOI] [PubMed] [Google Scholar]
- 44.Silverman BL, Metzger BE, Cho NH, Loeb CA. Impaired glucose tolerance in adolescent offspring of diabetic mothers. Relationship to fetal hyperinsulinism. Diabetes Care. 1995;18:611–7. doi: 10.2337/diacare.18.5.611. [DOI] [PubMed] [Google Scholar]
- 45.Ahlsson F, Gustafsson J, Tuvemo T, Lundgren M. Females born large for gestational age have a doubled risk of giving birth to large for gestational age infants. Acta Paediatr. 2007;96:358–62. doi: 10.1111/j.1651-2227.2006.00141.x. [DOI] [PubMed] [Google Scholar]
- 46.Steps to a Healthier US; Services HaH, editor. Diabetes: A National Plan for Action. Washington, D.C: US Department of Health and Human Services; 2004. [Google Scholar]
- 47.Healthy People. 2020 (Accessed at http://www.healthypeople.gov/2010/document/pdf/volume1/05diabetes.pdf?visit=1.)
- 48.Glueck CJ, Goldenberg N, Wang P, Loftspring M, Sherman A. Metformin during pregnancy reduces insulin, insulin resistance, insulin secretion, weight, testosterone and development of gestational diabetes: prospective longitudinal assessment of women with polycystic ovary syndrome from preconception throughout pregnancy. Hum Reprod. 2004;19:510–21. doi: 10.1093/humrep/deh109. [DOI] [PubMed] [Google Scholar]
- 49.Glueck CJ, Pranikoff J, Aregawi D, Wang P. Prevention of gestational diabetes by metformin plus diet in patients with polycystic ovary syndrome. Fertil Steril. 2008;89:625–34. doi: 10.1016/j.fertnstert.2007.03.036. [DOI] [PubMed] [Google Scholar]
- 50.Luoto R, Laitinen K, Nermes M, Isolauri E. Impact of maternal probiotic-supplemented dietary counselling on pregnancy outcome and prenatal and postnatal growth: a double-blind, placebo-controlled study. Br J Nutr. 2010;103:1792–9. doi: 10.1017/S0007114509993898. [DOI] [PubMed] [Google Scholar]
- 51.Santamaria A, Di Benedetto A, Petrella E, et al. Myo-inositol may prevent gestational diabetes onset in overweight women: a randomized, controlled trial. J Matern Fetal Neonatal Med. 2015:1–4. doi: 10.3109/14767058.2015.1121478. [DOI] [PubMed] [Google Scholar]
- 52.D’Anna R, Di Benedetto A, Scilipoti A, et al. Myo-inositol Supplementation for Prevention of Gestational Diabetes in Obese Pregnant Women: A Randomized Controlled Trial. Obstet Gynecol. 2015;126:310–5. doi: 10.1097/AOG.0000000000000958. [DOI] [PubMed] [Google Scholar]
- 53.Johansson K, Cnattingius S, Naslund I, et al. Outcomes of pregnancy after bariatric surgery. N Engl J Med. 2015;372:814–24. doi: 10.1056/NEJMoa1405789. [DOI] [PubMed] [Google Scholar]
- 54.Nohira T, Kim S, Nakai H, Okabe K, Yoneyama K. Recurrence of gestational diabetes mellitus: rates and risk factors from initial GDM and one abnormal GTT value. Diabetes Res Clin Pract. 2006;71:75–81. doi: 10.1016/j.diabres.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 55.Kaul P, Savu A, Nerenberg KA, et al. Interaction between maternal obesity and gestational diabetes mellitus and long-term development of diabetes, hypertension and cardiovascular disease: a population-level analysis. Canadian journal of diabetes. 2013;37(Suppl 4):S4. [Google Scholar]
- 56.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–14. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Heslehurst N, Ells LJ, Simpson H, Batterham A, Wilkinson J, Summerbell CD. Trends in maternal obesity incidence rates, demographic predictors, and health inequalities in 36,821 women over a 15-year period. BJOG. 2007;114:187–94. doi: 10.1111/j.1471-0528.2006.01180.x. [DOI] [PubMed] [Google Scholar]
- 58.Kim SY, England L, Wilson HG, Bish C, Satten GA, Dietz P. Percentage of gestational diabetes mellitus attributable to overweight and obesity. Am J Public Health. 2010;100:1047–52. doi: 10.2105/AJPH.2009.172890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Torloni MR, Betran AP, Horta BL, et al. Prepregnancy BMI and the risk of gestational diabetes: a systematic review of the literature with meta-analysis. Obes Rev. 2009;10:194–203. doi: 10.1111/j.1467-789X.2008.00541.x. [DOI] [PubMed] [Google Scholar]
- 60.Honein MA, Devine O, Sharma AJ, et al. Modeling the potential public health impact of prepregnancy obesity on adverse fetal and infant outcomes. Obesity (Silver Spring) 2013;21:1276–83. doi: 10.1002/oby.20156. [DOI] [PubMed] [Google Scholar]
- 61.Poston L, Harthoorn LF, Van Der Beek EM Contributors to the IEW. Obesity in pregnancy: implications for the mother and lifelong health of the child. A consensus statement. Pediatr Res. 2011;69:175–80. doi: 10.1203/PDR.0b013e3182055ede. [DOI] [PubMed] [Google Scholar]
- 62.Wahabi HA, Fayed AA, Alzeidan RA, Mandil AA. The independent effects of maternal obesity and gestational diabetes on the pregnancy outcomes. BMC Endocr Disord. 2014;14:47. doi: 10.1186/1472-6823-14-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Brunner S, Stecher L, Ziebarth S, et al. Excessive gestational weight gain prior to glucose screening and the risk of gestational diabetes: a meta-analysis. Diabetologia. 2015;58:2229–37. doi: 10.1007/s00125-015-3686-5. [DOI] [PubMed] [Google Scholar]
- 64.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wadden TA, Butryn ML. Behavioral treatment of obesity. Endocrinol Metab Clin North Am. 2003;32:981–1003. x. doi: 10.1016/s0889-8529(03)00072-0. [DOI] [PubMed] [Google Scholar]
- 66.Wing RR, Phelan S. Behavioral treatment of obesity: strategies to improve outcome and predictors of success. In: Eckel RH, editor. Obesity: An Academic Basis for Clinical Evaluation and Treatment. Williams and Wilkens; 2002. pp. 415–35. [Google Scholar]
- 67.Phelan S, Jankovitz K, Hagobian T, Abrams B. Reducing excessive gestational weight gain: lessons from the weight control literature and avenues for future research. Womens Health (Lond Engl) 2011;7:641–61. doi: 10.2217/whe.11.70. [DOI] [PubMed] [Google Scholar]
- 68.Dutton GR, Laitner MH, Perri MG. Lifestyle interventions for cardiovascular disease risk reduction: a systematic review of the effects of diet composition, food provision, and treatment modality on weight loss. Curr Atheroscler Rep. 2014;16:442. doi: 10.1007/s11883-014-0442-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wadden TA, Butryn ML, Byrne KJ. Efficacy of lifestyle modification for long-term weight control. Obes Res. 2004;12(Suppl):151S–62S. doi: 10.1038/oby.2004.282. [DOI] [PubMed] [Google Scholar]
- 70.Pi-Sunyer X, Blackburn G, Brancati FL, et al. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the look AHEAD trial. Diabetes Care. 2007;30:1374–83. doi: 10.2337/dc07-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.The Diabetes Prevention Program: baseline characteristics of the randomized cohort. The Diabetes Prevention Program Research Group. Diabetes Care. 2000;23:1619–29. doi: 10.2337/diacare.23.11.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wadden TA, Foster GD, Letizia KA. One-year behavioral treatment of obesity: comparison of moderate and severe caloric restriction and the effects of weight maintenance therapy. J Consult Clin Psychol. 1994;62:165–71. doi: 10.1037//0022-006x.62.1.165. [DOI] [PubMed] [Google Scholar]
- 73.Look Ahead Research Group. Eight-year weight losses with an intensive lifestyle intervention: the look AHEAD study. Obesity (Silver Spring) 2014;22:5–13. doi: 10.1002/oby.20662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Look Ahead Research Group. Wing RR, Bolin P, et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med. 2013;369:145–54. doi: 10.1056/NEJMoa1212914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wing RR. Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial. Arch Intern Med. 2010;170:1566–75. doi: 10.1001/archinternmed.2010.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rasmussen KM, Yaktine AL Institute of Medicine (U.S.). Committee to Reexamine IOM Pregnancy Weight Guidelines. Weight gain during pregnancy: reexamining the guidelines. Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- 77.Chu SY, Callaghan WM, Bish CL, D’Angelo D. Gestational weight gain by body mass index among US women delivering live births, 2004–2005: fueling future obesity. Am J Obstet Gynecol. 2009;200:271.e1–7. doi: 10.1016/j.ajog.2008.09.879. [DOI] [PubMed] [Google Scholar]
- 78.Zhou SJ, Yelland L, McPhee AJ, Quinlivan J, Gibson RA, Makrides M. Fish-oil supplementation in pregnancy does not reduce the risk of gestational diabetes or preeclampsia. Am J Clin Nutr. 2012;95:1378–84. doi: 10.3945/ajcn.111.033217. [DOI] [PubMed] [Google Scholar]
- 79.Han S, Middleton P, Crowther CA. Exercise for pregnant women for preventing gestational diabetes mellitus. Cochrane Database Syst Rev. 2012;7:CD009021. doi: 10.1002/14651858.CD009021.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tieu J, Crowther CA, Middleton P. Dietary advice in pregnancy for preventing gestational diabetes mellitus. Cochrane Database Syst Rev. 2008:CD006674. doi: 10.1002/14651858.CD006674.pub2. [DOI] [PubMed] [Google Scholar]
- 81.Luoto R, Kinnunen TI, Aittasalo M, et al. Primary prevention of gestational diabetes mellitus and large-for-gestational-age newborns by lifestyle counseling: a cluster-randomized controlled trial. PLoS Med. 2011;8:e1001036. doi: 10.1371/journal.pmed.1001036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Luoto RM, Kinnunen TI, Aittasalo M, et al. Prevention of gestational diabetes: design of a cluster-randomized controlled trial and one-year follow-up. BMC Pregnancy Childbirth. 2010;10:39. doi: 10.1186/1471-2393-10-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Stafne SN, Salvesen KA, Romundstad PR, Eggebo TM, Carlsen SM, Morkved S. Regular exercise during pregnancy to prevent gestational diabetes: a randomized controlled trial. Obstet Gynecol. 2012;119:29–36. doi: 10.1097/AOG.0b013e3182393f86. [DOI] [PubMed] [Google Scholar]
- 84.Callaway LK, Colditz PB, Byrne NM, et al. Prevention of gestational diabetes: feasibility issues for an exercise intervention in obese pregnant women. Diabetes Care. 2010;33:1457–9. doi: 10.2337/dc09-2336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bain E, Crane M, Tieu J, Han S, Crowther CA, Middleton P. Diet and exercise interventions for preventing gestational diabetes mellitus. Cochrane Database Syst Rev. 2015;4:CD010443. doi: 10.1002/14651858.CD010443.pub2. [DOI] [PubMed] [Google Scholar]
- 86.Halperin IJ, Feig DS. The role of lifestyle interventions in the prevention of gestational diabetes. Curr Diab Rep. 2014;14:452. doi: 10.1007/s11892-013-0452-2. [DOI] [PubMed] [Google Scholar]
- 87.Skouteris H, Morris H, Nagle C, Nankervis A. Behavior modification techniques used to prevent gestational diabetes: a systematic review of the literature. Curr Diab Rep. 2014;14:480. doi: 10.1007/s11892-014-0480-6. [DOI] [PubMed] [Google Scholar]
- 88.Russo LM, Nobles C, Ertel KA, Chasan-Taber L, Whitcomb BW. Physical activity interventions in pregnancy and risk of gestational diabetes mellitus: a systematic review and meta-analysis. Obstet Gynecol. 2015;125:576–82. doi: 10.1097/AOG.0000000000000691. [DOI] [PubMed] [Google Scholar]
- 89.Koivusalo SB, Rono K, Klemetti MM, et al. Gestational Diabetes Mellitus Can Be Prevented by Lifestyle Intervention: The Finnish Gestational Diabetes Prevention Study (RADIEL): A Randomized Controlled Trial. Diabetes Care. 2016;39:24–30. doi: 10.2337/dc15-0511. [DOI] [PubMed] [Google Scholar]
- 90.Rono K, Stach-Lempinen B, Klemetti MM, et al. Prevention of gestational diabetes through lifestyle intervention: study design and methods of a Finnish randomized controlled multicenter trial (RADIEL) BMC Pregnancy Childbirth. 2014;14:70. doi: 10.1186/1471-2393-14-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Nitert MD, Barrett HL, Foxcroft K, et al. SPRING: an RCT study of probiotics in the prevention of gestational diabetes mellitus in overweight and obese women. BMC Pregnancy Childbirth. 2013;13:50. doi: 10.1186/1471-2393-13-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Crowther CA, Hague WM, Middleton PF, et al. The IDEAL study: investigation of dietary advice and lifestyle for women with borderline gestational diabetes: a randomised controlled trial - study protocol. BMC Pregnancy Childbirth. 2012;12:106. doi: 10.1186/1471-2393-12-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Jelsma JG, van Poppel MN, Galjaard S, et al. DALI: Vitamin D and lifestyle intervention for gestational diabetes mellitus (GDM) prevention: an European multicentre, randomised trial - study protocol. BMC Pregnancy Childbirth. 2013;13:142. doi: 10.1186/1471-2393-13-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ferrara A, Hedderson MM, Albright CL, et al. A pragmatic cluster randomized clinical trial of diabetes prevention strategies for women with gestational diabetes: design and rationale of the Gestational Diabetes’ Effects on Moms (GEM) study. BMC Pregnancy Childbirth. 2014;14:21. doi: 10.1186/1471-2393-14-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Chasan-Taber L, Marcus BH, Rosal MC, et al. Estudio Parto: postpartum diabetes prevention program for hispanic women with abnormal glucose tolerance in pregnancy: a randomised controlled trial - study protocol. BMC Pregnancy Childbirth. 2014;14:100. doi: 10.1186/1471-2393-14-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Chasan-Taber L, Marcus BH, Stanek E, 3rd, et al. A randomized controlled trial of prenatal physical activity to prevent gestational diabetes: design and methods. J Womens Health (Larchmt) 2009;18:851–9. doi: 10.1089/jwh.2008.1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ferrara A, Hedderson MM, Albright CL, et al. A pregnancy and postpartum lifestyle intervention in women with gestational diabetes mellitus reduces diabetes risk factors: a feasibility randomized control trial. Diabetes Care. 2011;34:1519–25. doi: 10.2337/dc10-2221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Infanti JJ, Dunne FP, AOD, et al. An evaluation of Croi MyAction community lifestyle modification programme compared to standard care to reduce progression to diabetes/pre-diabetes in women with prior gestational diabetes mellitus (GDM): study protocol for a randomised controlled trial. Trials. 2013;14:121. doi: 10.1186/1745-6215-14-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Rautio N, Jokelainen J, Korpi-Hyovalti E, et al. Lifestyle Intervention in Prevention of Type 2 Diabetes in Women With a History of Gestational Diabetes Mellitus: One-Year Results of the FIN-D2D Project. J Womens Health (Larchmt) 2014;23:506–12. doi: 10.1089/jwh.2013.4520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hu G, Tian H, Zhang F, et al. Tianjin Gestational Diabetes Mellitus Prevention Program: study design, methods, and 1-year interim report on the feasibility of lifestyle intervention program. Diabetes Res Clin Pract. 2012;98:508–17. doi: 10.1016/j.diabres.2012.09.015. [DOI] [PubMed] [Google Scholar]
- 101.Shih ST, Davis-Lameloise N, Janus ED, et al. Mothers After Gestational Diabetes in Australia Diabetes Prevention Program (MAGDA-DPP) post-natal intervention: study protocol for a randomized controlled trial. Trials. 2013;14:339. doi: 10.1186/1745-6215-14-339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Buchanan TA, Xiang AH, Peters RK, et al. Preservation of pancreatic beta-cell function and prevention of type 2 diabetes by pharmacological treatment of insulin resistance in high-risk hispanic women. Diabetes. 2002;51:2796–803. doi: 10.2337/diabetes.51.9.2796. [DOI] [PubMed] [Google Scholar]
- 103.Ratner RE, Christophi CA, Metzger BE, et al. Prevention of diabetes in women with a history of gestational diabetes: effects of metformin and lifestyle interventions. J Clin Endocrinol Metab. 2008;93:4774–9. doi: 10.1210/jc.2008-0772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Zeng YC, Li MJ, Chen Y, et al. The use of glyburide in the management of gestational diabetes mellitus: a meta-analysis. Advances in medical sciences. 2014;59:95–101. doi: 10.1016/j.advms.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 105.Clark HD, van Walraven C, Code C, Karovitch A, Keely E. Did publication of a clinical practice guideline recommendation to screen for type 2 diabetes in women with gestational diabetes change practice? Diabetes Care. 2003;26:265–8. doi: 10.2337/diacare.26.2.265. [DOI] [PubMed] [Google Scholar]
- 106.Clark HD, Graham ID, Karovitch A, Keely EJ. Do postal reminders increase postpartum screening of diabetes mellitus in women with gestational diabetes mellitus? A randomized controlled trial. Am J Obstet Gynecol. 2009;200:634e1–7. doi: 10.1016/j.ajog.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 107.Ehrlich SF, Hedderson MM, Feng J, Davenport ER, Gunderson EP, Ferrara A. Change in body mass index between pregnancies and the risk of gestational diabetes in a second pregnancy. Obstet Gynecol. 2011;117:1323–30. doi: 10.1097/AOG.0b013e31821aa358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Pole JD, Dodds LA. Maternal outcomes associated with weight change between pregnancies. Can J Public Health. 1999;90:233–6. doi: 10.1007/BF03404122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Villamor E, Cnattingius S. Interpregnancy weight change and risk of adverse pregnancy outcomes: a population-based study. Lancet. 2006;368:1164–70. doi: 10.1016/S0140-6736(06)69473-7. [DOI] [PubMed] [Google Scholar]
- 110.Glazer NL, Hendrickson AF, Schellenbaum GD, Mueller BA. Weight change and the risk of gestational diabetes in obese women. Epidemiology. 2004;15:733–7. doi: 10.1097/01.ede.0000142151.16880.03. [DOI] [PubMed] [Google Scholar]
- 111.Solomon CG, Willett WC, Carey VJ, et al. A prospective study of pregravid determinants of gestational diabetes mellitus. JAMA. 1997;278:1078–83. [PubMed] [Google Scholar]
- 112.Rudra CB, Sorensen TK, Leisenring WM, Dashow E, Williams MA. Weight characteristics and height in relation to risk of gestational diabetes mellitus. Am J Epidemiol. 2007;165:302–8. doi: 10.1093/aje/kwk007. [DOI] [PubMed] [Google Scholar]
- 113.Hedderson MM, Williams MA, Holt VL, Weiss NS, Ferrara A. Body mass index and weight gain prior to pregnancy and risk of gestational diabetes mellitus. Am J Obstet Gynecol. 2008;198:409e1–7. doi: 10.1016/j.ajog.2007.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Wittgrove AC, Jester L, Wittgrove P, Clark GW. Pregnancy following gastric bypass for morbid obesity. Obes Surg. 1998;8:461–4. doi: 10.1381/096089298765554368. discussion 5–6. [DOI] [PubMed] [Google Scholar]
- 115.Ducarme G, Revaux A, Rodrigues A, Aissaoui F, Pharisien I, Uzan M. Obstetric outcome following laparoscopic adjustable gastric banding. Int J Gynaecol Obstet. 2007;98:244–7. doi: 10.1016/j.ijgo.2007.02.020. [DOI] [PubMed] [Google Scholar]
- 116.Dixon JB, Dixon ME, O’Brien PE. Birth outcomes in obese women after laparoscopic adjustable gastric banding. Obstet Gynecol. 2005;106:965–72. doi: 10.1097/01.AOG.0000181821.82022.82. [DOI] [PubMed] [Google Scholar]
- 117.Kral JG, Biron S, Simard S, et al. Large maternal weight loss from obesity surgery prevents transmission of obesity to children who were followed for 2 to 18 years. Pediatrics. 2006;118:e1644–9. doi: 10.1542/peds.2006-1379. [DOI] [PubMed] [Google Scholar]
- 118.Bentley-Lewis R, Levkoff S, Stuebe A, Seely EW. Gestational diabetes mellitus: postpartum opportunities for the diagnosis and prevention of type 2 diabetes mellitus. Nat Clin Pract Endocrinol Metab. 2008;4:552–8. doi: 10.1038/ncpendmet0965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Nicklas JM, Zera CA, Seely EW, Abdul-Rahim ZS, Rudloff ND, Levkoff SE. Identifying postpartum intervention approaches to prevent type 2 diabetes in women with a history of gestational diabetes. BMC Pregnancy Childbirth. 2011;11:23. doi: 10.1186/1471-2393-11-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Dalfra MG, Nicolucci A, Bisson T, Bonsembiante B, Lapolla A, Qlisg Quality of life in pregnancy and post-partum: a study in diabetic patients. Qual Life Res. 2012;21:291–8. doi: 10.1007/s11136-011-9940-5. [DOI] [PubMed] [Google Scholar]
- 121.Phelan S. Pregnancy: a “teachable moment” for weight control and obesity prevention. Am J Obstet Gynecol. 2010;202:135e1–8. doi: 10.1016/j.ajog.2009.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.McBride CM, Emmons KM, Lipkus IM. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ Res. 2003;18:156–70. doi: 10.1093/her/18.2.156. [DOI] [PubMed] [Google Scholar]
- 123.Swan WE, Liaw ST, Dunning T, Pallant JF, Kilmartin G. Diabetes risk reduction behaviours of rural postpartum women with a recent history of gestational diabetes. Rural Remote Health. 2010;10:1461. [PubMed] [Google Scholar]
- 124.Dasgupta K, Da Costa D, Pillay S, et al. Strategies to optimize participation in diabetes prevention programs following gestational diabetes: a focus group study. PLoS ONE. 2013;8:e67878. doi: 10.1371/journal.pone.0067878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Kieffer EC, Willis SK, Arellano N, Guzman R. Perspectives of pregnant and postpartum latino women on diabetes, physical activity, and health. Health Educ Behav. 2002;29:542–56. doi: 10.1177/109019802237023. [DOI] [PubMed] [Google Scholar]
- 126.Gipson JD, Santelli JS. Unplanned and assisted conception pregnancies. BMJ. 2010;343:d4996. doi: 10.1136/bmj.d4996. [DOI] [PubMed] [Google Scholar]
- 127.Zielinski R, Ackerson K, Misiunas RB, Miller JM. Feasibility of a longitudinal study of women anticipating first pregnancy and assessed by multiple pelvic exams: recruitment and retention challenges. Contemp Clin Trials. 2010;31:544–8. doi: 10.1016/j.cct.2010.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Jack BW, Culpepper L, Babcock J, Kogan MD, Weismiller D. Addressing preconception risks identified at the time of a negative pregnancy test. A randomized trial. J Fam Pract. 1998;47:33–8. [PubMed] [Google Scholar]
- 129.de Jong-Potjer LC, Elsinga J, le Cessie S, et al. GP-initiated preconception counselling in a randomised controlled trial does not induce anxiety. BMC Fam Pract. 2006;7:66. doi: 10.1186/1471-2296-7-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Elsinga J, van der Pal-de Bruin K, le Cessie S, de Jong-Potjer L, Verloove-Vanhorick S, Assendelft W. Preconception counselling initiated by general practitioners in the Netherlands: reaching couples contemplating pregnancy [ISRCTN53942912] BMC Fam Pract. 2006;7:41. doi: 10.1186/1471-2296-7-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Floyd RL, Sobell M, Velasquez MM, et al. Preventing alcohol-exposed pregnancies: a randomized controlled trial. Am J Prev Med. 2007;32:1–10. doi: 10.1016/j.amepre.2006.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Lumley J, Donohue L. Aiming to increase birth weight: a randomised trial of pre-pregnancy information, advice and counselling in inner-urban Melbourne. BMC Public Health. 2006;6:299. doi: 10.1186/1471-2458-6-299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Velott DL, Baker SA, Hillemeier MM, Weisman CS. Participant recruitment to a randomized trial of a community-based behavioral intervention for pre- and interconceptional women findings from the Central Pennsylvania Women’s Health Study. Womens Health Issues. 2008;18:217–24. doi: 10.1016/j.whi.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 134.Phelan S, Hagobian T, Brannen A, Stewart A, Schmid BA, Cedars L. Promoting weight loss before pregnancy: Feasible or Futile? Calif J Health Prom. 2013;11:86–92. [Google Scholar]
- 135.Lovelady CA, Garner KE, Moreno KL, Williams JP. The effect of weight loss in overweight, lactating women on the growth of their infants. N Engl J Med. 2000;342:449–53. doi: 10.1056/NEJM200002173420701. [DOI] [PubMed] [Google Scholar]
- 136.Leermakers EA, Anglin K, Wing RR. Reducing postpartum weight retention through a correspondence intervention. Int J Obes. 1998;22:1103–9. doi: 10.1038/sj.ijo.0800734. [DOI] [PubMed] [Google Scholar]
- 137.O’Toole ML, Sawicki MA, Artal R. Structured diet and physical activity prevent postpartum weight retention. J Womens Health (Larchmt) 2003;12:991–8. doi: 10.1089/154099903322643910. [DOI] [PubMed] [Google Scholar]
- 138.Kinnunen TI, Pasanen M, Aittasalo M, Fogelholm M, Weiderpass E, Luoto R. Reducing postpartum weight retention--a pilot trial in primary health care. Nutr J. 2007;6:21. doi: 10.1186/1475-2891-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Phelan S, Brannen A, Erickson K, et al. ‘Fit Moms/Mamas Activas’ internet-based weight control program with group support to reduce postpartum weight retention in low-income women: study protocol for a randomized controlled trial. Trials. 2015;16:59. doi: 10.1186/s13063-015-0573-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Tovar A, Chasan-Taber L, Eggleston E, Oken E. Postpartum screening for diabetes among women with a history of gestational diabetes mellitus. Prev Chronic Dis. 2011;8:A124. [PMC free article] [PubMed] [Google Scholar]
- 141.American Diabetes Association. Gestational Diabetes Mellitus. Diabetes Care. 2004;27:S88–S90. doi: 10.2337/diacare.27.2007.s88. [DOI] [PubMed] [Google Scholar]
- 142.Berkowitz GS, Lapinski RH, Wein R, Lee D. Race/ethnicity and other risk factors for gestational diabetes. Am J Epidemiol. 1992;135:965–73. doi: 10.1093/oxfordjournals.aje.a116408. [DOI] [PubMed] [Google Scholar]
- 143.Di Cianni G, Volpe L, Lencioni C, et al. Prevalence and risk factors for gestational diabetes assessed by universal screening. Diabetes Res Clin Pract. 2003;62:131–7. doi: 10.1016/j.diabres.2003.07.004. [DOI] [PubMed] [Google Scholar]
- 144.Anna V, van der Ploeg HP, Cheung NW, Huxley RR, Bauman AE. Sociodemographic correlates of the increasing trend in prevalence of gestational diabetes mellitus in a large population of women between 1995 and 2005. Diabetes Care. 2008;31:2288–93. doi: 10.2337/dc08-1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Shyam S, Arshad F, Abdul Ghani R, et al. Low glycaemic index diets improve glucose tolerance and body weight in women with previous history of gestational diabetes: a six months randomized trial. Nutr J. 2013;12:68. doi: 10.1186/1475-2891-12-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Wein P, Beischer N, Harris C, Permezel M. A trial of simple versus intensified dietary modification for prevention of progression to diabetes mellitus in women with impaired glucose tolerance. Aust N Z J Obstet Gynaecol. 1999;39:162–6. doi: 10.1111/j.1479-828x.1999.tb03363.x. [DOI] [PubMed] [Google Scholar]
- 147.Reinhardt JA, van der Ploeg HP, Grzegrzulka R, Timperley JG. Implementing lifestyle change through phone-based motivational interviewing in rural-based women with previous gestational diabetes mellitus. Health Promot J Austr. 2012;23:5–9. doi: 10.1071/he12005. [DOI] [PubMed] [Google Scholar]
- 148.Cheung NW, Smith BJ, van der Ploeg HP, Cinnadaio N, Bauman A. A pilot structured behavioural intervention trial to increase physical activity among women with recent gestational diabetes. Diabetes Res Clin Pract. 2011;92:e27–9. doi: 10.1016/j.diabres.2011.01.013. [DOI] [PubMed] [Google Scholar]
- 149.Kim C, Draska M, Hess ML, Wilson EJ, Richardson CR. A web-based pedometer programme in women with a recent history of gestational diabetes. Diabet Med. 2012;29:278–83. doi: 10.1111/j.1464-5491.2011.03415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.McIntyre HD, Peacock A, Miller YD, Koh D, Marshall AL. Pilot study of an individualised early postpartum intervention to increase physical activity in women with previous gestational diabetes. International journal of endocrinology. 2012;2012:892019. doi: 10.1155/2012/892019. [DOI] [PMC free article] [PubMed] [Google Scholar]