Gene expression during hematopoietic lineage commitment is tightly regulated by a complex network of transcriptional regulators. Growth Factor Independent 1 (GFI1) and GFI1B are recruiters of histone deacetylases, histone methyltransferases, and key transcriptional repressors during hematopoiesis.1,2 These paralogous proteins display 90% amino acid sequence homology in their N-terminal SNAG (Snail/Gfi1) repression domains and C-terminal zinc finger domains, respectively, while the intermediate region is poorly conserved (reviewed in3). The function of GFI1 is most important for maturation of granulocyte-monocyte precursors, whereas homozygous deletion of Gfi1b in mice leads to embryonic lethality due to the failure to produce mature, enucleated erythrocytes.1,2,4 Gfi1b−/− mice display symptoms of severe thrombocytopenia, although megakaryocytic progenitors are present in the bone marrow.1 In humans, alternative splicing of exon 9 leads to the formation of a shorter isoform of GFI1B (p32; NP_001128503). This isoform lacks the first two zinc fingers as compared to the p37 full length protein (NP_004179) and is implicated in erythropoiesis.5 GFI1B germline mutations have been identified which cause autosomal-dominant macrothrombocytopenia with a gray platelet syndrome (GPS)-like phenotype,6–10 now classified as BDPLT17 (MIM 604383) to distinguish them from the classic NBEAL2 mutations (MIM 139090). In the first reported patients, the mutant protein is hypothesized to act in a dominant-negative manner.7,8 Lately, genome-wide association studies (GWAS) revealed a splice-specific GFI1B variant (rs150813342) that possibly disrupts a splice enhancer-binding site in exon 9 with a minor allele frequency of 0.009.11 However, this was associated with a mild phenotype, possibly due to the residual expression of the p37 isoform. Moreover, a recent work described a hypomorphic recessive GFI1B mutation in zinc finger 6 (p.Leu308Pro).12 In this context, functional studies conducted with human cell lines and primary cells have clearly demonstrated the relevance of GFI1b-p37 for megakaryocytic maturation.5,6
We describe a Chechen family from eastern Georgia whose affected members presented with a severe, life-threatening bleeding diathesis. The 36-year-old female index patient (II.3, Figure 1A) had suffered from multiple petechiae and hematoma since childhood. She had a history of several life-threatening hemorrhages following ovarian cyst rupture and had undergone repeated emergency surgeries for intra-abdominal bleeding. At the time of presentation, she was splenectomized and being treated with eltrombopag (according to a working diagnosis of hepatitis C-associated immune thrombocytopenia), but the bleeding phenotype had not improved. Her two children, a 9-year-old girl (III.4) and a 7-year-old boy (III.5), exhibited severe thrombocytopenia (platelet counts: 23–44×109/L) and similar cutaneous bleeding patterns as the index patient (II.3), recurring epistaxis and caries. The index patient’s brother (II.2) had also suffered from a severe bleeding diathesis with thrombocytopenia, and had died at age 33 due to a spontaneous cerebral hemorrhage. In contrast, the index patient’s husband (II.4), her parents (I.1 and I.2) and the children of the deceased brother (III.1, III.2, III.3) were clinically unaffected.
Figure 1.
A recessive mutation in GFI1B causes a grey platelet-like phenotype with ectopic expression of CD34. (A) Pedigree depicting the index patient (red arrow), her two affected children, the affected brother and the heterozygous carriers. Genetic testing was performed in individuals marked by an asterisk(*). (B) Standard blood smears show large platelets with reduced, grayish staining in the index patient (II.3) as compared to platelets from a healthy control (HC; left column), while an analysis of red cell morphology revealed mild anisocytosis, poikilocytosis and hypochromia. (C) Flow cytometric analyses of patients III.4 (blue curves) and III.5 (red curves) compared to a healthy control (green curves), indicating ectopic CD34 expression on platelets and impaired P-selectin (CD62P) exposure upon treatment with 5 μM TRAP-6 in both patients. Gating was performed on a CD41a-positive platelet population. MFI: mean fluorescence intensity. (D) GFI1B was present in most HC megakaryocytes (left column), but absent in the index patient’s megakaryocytes (II.3; right; 400×, insert: 600×). CD34 expression in megakaryocytes (center row) was strongly positive in the index patient as compared to the HC: Bottom row: Expression of CD41 (GPIIb/IIIa) as control megakaryocyte marker (400×; in II.3 and HC).
The blood cell counts, coagulation parameters and platelet markers of the patients showed macrothrombocytopenia with reduced May-Grünwald-Giemsa staining of platelets (Figure 1B and Online Supplementary Figure S1) and decreased immunofluorescence staining for alpha-granule markers von Willebrand factor and P-selectin, suggesting an alpha storage pool deficiency (Online Supplementary Figure S1). Platelet function testing by flow cytometry and aggregometry revealed reduced responses to ADP, collagen, TRAP-6 and arachidonic acid (Figure 1C, Online Supplementary Figure S2, Online Supplementary Table S1). Mepacrine uptake was reduced in two out of three of the affected individuals, and we could not detect mepacrine secretion in any patient upon exposure to various triggers (Online Supplementary Table S1), indicating the presence of a delta-granule defect. This fits well to recent data showing combined alpha-delta granule storage pool deficiency in patients with GFI1B mutations p.Q287* and p.Leu308Pro, respectively.12,13 The white and red blood cell parameters were overall normal in the index patient and both affected children. As a note, the index patient, but not her children, had minor alterations in the red cell lineage that could be attributed to her asplenia, latent iron deficiency and thrombopoietin receptor agonist treatment. These alterations included a slightly increased red cell distribution width, mild anisocytosis, hypochromia, moderate poikilocytosis, and low levels of target cells and Howell-Jolly bodies (Figure 1b, Online Supplementary Figure S1, Online Supplementary Table S1). Notably, both affected children (III.4 and III.5) had normal red blood cell counts and indices, and inconspicuous erythrocyte morphology (Online Supplementary Table S1).
Suspecting autosomal-dominant inheritance, we analyzed DNA from the index patient for 59 genes relevant to platelet biogenesis or function using targeted next-generation sequencing (NGS). We identified a novel, homozygous single nucleotide insertion in GFI1B (NM_004188.5; c.551insG), which was confirmed by Sanger sequencing. The frameshift (p.Ser185Leufs*3) is expected to result in the formation of a premature stop codon. The homozygous variant co-segregated with the phenotype; while both affected children were homozygous for the insertion in GFI1B, the unaffected mother (I.1), husband (II.4) and two nephews (III.1 and III.2) of the index patient were heterozygous, suggesting the existence of a local founder variant and an unexpected autosomal-recessive trait (Figure 1).
To further characterize hematopoietic lineage maturation and platelet activation, peripheral blood cells and bone marrow were subjected to immune phenotyping and flow cytometry, showing an increased proportion of CD34-positive cells without clonal expansion. In addition, platelets from the homozygous patients showed CD34 expression, whereas it was absent on platelets from heterozygous family members (Online Supplementary Table S1, Figure 1C, Online Supplementary Figure S1). Bone marrow from the index patient contained normal erythroid and myeloid progenitors and slightly- to moderately-increased megakaryopoiesis with diffusely dispersed and occasionally locally clustered small to normal-sized megakaryocytes. These megakaryocytes displayed hypolobulated nuclei, frequently showed dense chromatin and a persistent expression of the stem cell marker CD34 (Figure 1C, D; Online Supplementary Figure S3). The megakaryocyte markers CD41, CD42b and CD61 were readily identified in the index patient, whereas GFI1B and CD36 were undetectable (Figure 1D and Online Supplementary Figure S3). The ectopic expression of the hematopoietic stem cell marker CD34 on megakaryocytes, together with their dysplastic appearance, are features that have been described for dominant GFI1B mutations.7 The observed pale, grayish platelet staining pattern might reflect a GPS-like phenotype. However, this term should be used cautiously, as the “grey platelet syndrome” is associated with NBEAL2 mutations.10
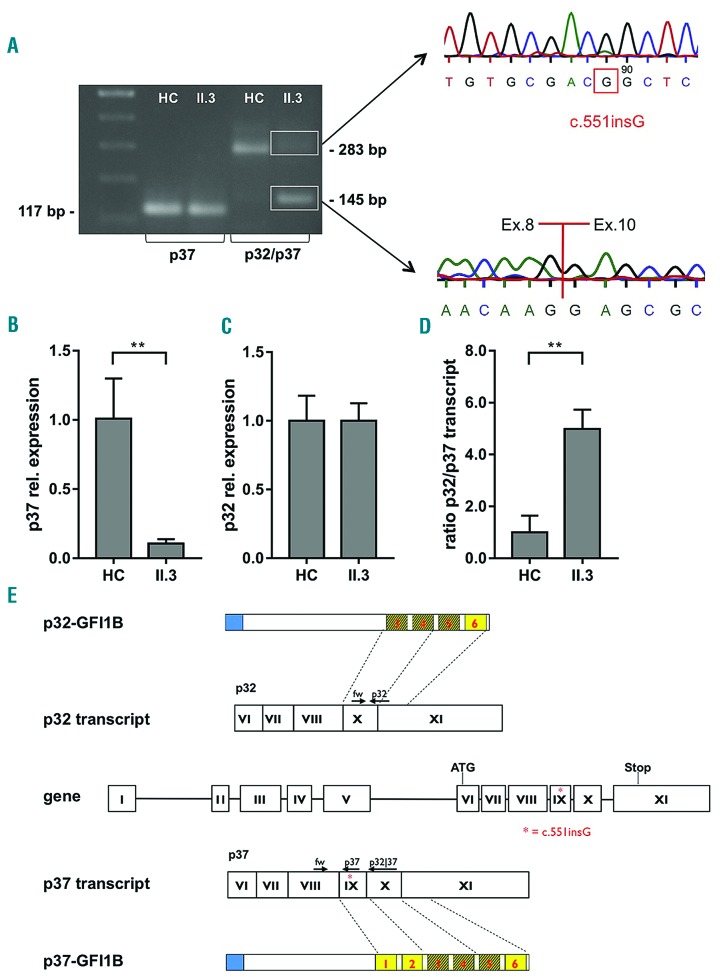
We next sought to determine the presence and quantity of the two GFI1B transcript variants in platelets by using quantitative real-time (q)PCR.5,14 DNA from both qPCR amplicons was gel-purified, and subsequent sequencing confirmed the homozygous c.551_G insertion in p37 at the transcript level as well as the presence of the spliced p32 variant (Figure 2A). In patient II.3, the amount of the GFI1B-p37 transcript was substantially reduced in platelets within context of an increased p32/p37 ratio, since p32 expression was unaffected as compared to healthy controls (Figure 2B–D). These findings indicate that the residual mutated transcript was not completely degraded by nonsense-mediated decay.
Figure 2.
The splice-specific mutation leads to loss of GFI1B-p37 in platelets. (A) Agarose-gel showing the GFI1B-p37 transcript (117 bp; left) and a diverse band pattern for one healthy control (HC) and index-patient II.3 after p32/p37 amplification of both GFI1B transcript variants. p37 (283 bp) and p32 (145 bp) bands from the patient were gel-purified, and PCR products were sequenced. Relative expression of (B) GFI1B-p37 and (C) GFI1B-p32 as well as (D) the ratio of p32/p37 transcripts, each comparing 3 healthy controls (HC) to index patient II.3, were analyzed using qPCR (**P<0.01). (E) Schematic representation of GFI1B gene, transcript and protein structures depicting the splicing variants. Blue: SNAG domain, yellow: zinc finger domains (dashed: predicted DNA-binding Zn-fingers); arrows: primers used to target each specific isoform; red asterisk = c.551insG.
The results of our study clinically confirm that the first two zinc fingers of GFI1B which are encoded by exon 9 are dispensable for human erythropoiesis, but essential for normal megakaryopoiesis and the biogenesis of functional platelets. In contrast to the hitherto reported dominant thrombocytopenia-linked GFI1B mutations that affect both isoforms,2,7,15 the insertion variant identified in this family results in a premature stop codon (p.Ser185Leufs*3) that only affects the longer p37 isoform (Figure 2e). Recent independent evidence by a GWAS analysis supports this finding: in a global genetic screening, a splice-specific recessive GFI1B variant (rs150813342) associated with lower platelet counts was identified.11 The unaffected GFI1B-p32 isoform lacks the first two zinc fingers. These were found not to be essential for DNA binding in vitro, but are relevant during interactions with other zinc fingers and affected the ability of the isoform to bind to DNA-protein complexes.3,16 Thus, while heterozygous mutations that lead to the absence of the terminal zinc fingers (5 and 6) of GFI1B act in a dominant-negative manner and lead to GPS-like macrothrombocytopenia,6–8 abrogating the complete GFI1B-p37 isoform results in autosomal-recessive macrothrombocytopenia with diminished platelet function as seen in the presented trait. Recently, the functional background for Gfi1b-implicated megakaryocytic maturation defects could be addressed in murine lineage-specific knockout models showing the role of Gfi1b in cytoskeletal organization in both early and late stage megakaryopoiesis.17
The context-dependent expression of two paralogous genes (e.g., GFI1 and GFI1B) is generally known to underline hematopoietic lineage breakpoints. However, the splice variant-specific lineage commitment reported here for GFI1B-p37 and GFI1B-p32 defines an important node at the megakaryocytic-erythroid progenitor (MEP) stage.6 GFI1B-p32 was shown to be necessary for human erythropoiesis in vitro.5 Since erythropoiesis appears rather unaffected in presented GFI1B-p37-deficient patients, we clinically confirm that transcriptional regulation of human erythropoiesis is less dependent on GFI1B-p37 than megakaryocyte maturation and platelet production. Conversely, the presence of GFI1B-p32 alone is not sufficient for functional platelet biogenesis in the affected patients.
Chen and colleagues described a case with thrombocytopenia and platelet function defects bearing a homozygous GFI1B variant (Cys168Phe).6 Subsequent functional studies via protein modelling and studying CD34-positive hematopoietic stem cells demonstrated that this respective mutation disturbs proper tertiary structure formation of GFI1B-p37, indicating the crucial relevance of the long GFI1B isoform in human megakaryopoiesis.
Our findings provide support for the non-redundancy of the roles of the two GFI1B isoforms p32 and p37 in vivo. We here report the first GFI1B loss-of-function mutation in alternatively spliced exon 9, which selectively causes macrothrombocytopenia and platelet dysfunction without critically impairing erythropoiesis. Our findings confirm that GFI1B is a crucial transcription factor that regulates megakaryocytic lineage maturation involving alternative splicing, a function that has not previously been identified for any other hematopoietic transcriptional regulator.
Supplementary Material
Acknowledgments
The authors would like to thank C. Khandanpour and B. A. van der Reijden for discussion of the data and methodological advice, A. Raicht and B. Leschnik for technical assistance, S. Crockett for scientific language editing and Dr. E. Haining for the critical review of the manuscript.
Funding: MGS and parts of the study were funded by Steirische Kinderkrebshilfe [Styrian Children’s Cancer Aid].
Footnotes
Funding: this work has been funded with the help of the PIUNA Program of the University of Navarra. L.E.-A. and D.N.-H. have PhD Studentships granted by the Ministry of Education, Culture and Sports of Spain (FPU14/03669 and FPU13/00424 respectively) within the University Faculty Training (FPU) program.
Information on authorship, contributions, and financial & other disclosures was provided by the authors and is available with the online version of this article at www.haematologica.org.
References
- 1.Foudi A, Kramer DJ, Qin J, et al. Distinct, strict requirements for Gfi-1b in adult bone marrow red cell and platelet generation. J Exp Med. 2014;211(5):909–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saleque S, Cameron S, Orkin SH. The zinc-finger proto-oncogene Gfi-1b is essential for development of the erythroid and megakaryocytic lineages. Genes Dev. 2002;16(3):301–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moroy T, Vassen L, Wilkes B, Khandanpour C. From cytopenia to leukemia: the role of Gfi1 and Gfi1b in blood formation. Blood. 2015;126(24):2561–2569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vassen L, Beauchemin H, Lemsaddek W, Krongold J, Trudel M, Moroy T. Growth factor independence 1b (gfi1b) is important for the maturation of erythroid cells and the regulation of embryonic globin expression. PLoS One. 2014;9(5):e96636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Laurent B, Randrianarison-Huetz V, Frisan E, et al. A short Gfi-1B isoform controls erythroid differentiation by recruiting the LSD1-CoREST complex through the dimethylation of its SNAG domain. J Cell Sci. 2012;125(Pt 4):993–1002. [DOI] [PubMed] [Google Scholar]
- 6.Chen L, Kostadima M, Martens JH, et al. Transcriptional diversity during lineage commitment of human blood progenitors. Science. 2014;345(6204):1251033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Monteferrario D, Bolar NA, Marneth AE, et al. A dominant-negative GFI1B mutation in the gray platelet syndrome. N Engl J Med. 2014;370(3):245–253. [DOI] [PubMed] [Google Scholar]
- 8.Stevenson WS, Morel-Kopp MC, Chen Q, et al. GFI1B mutation causes a bleeding disorder with abnormal platelet function. J Thromb Haemost. 2013;11(11):2039–2047. [DOI] [PubMed] [Google Scholar]
- 9.Kitamura K, Okuno Y, Yoshida K, et al. Functional characterization of a novel GFI1B mutation causing congenital macrothrombocytopenia. J Thromb Haemost. 2016;14(7):1462–1469. [DOI] [PubMed] [Google Scholar]
- 10.Nurden AT, Nurden P. Should any Genetic Defect Affecting alpha-Granules in Platelets be Classified as Gray Platelet Syndrome¿ Am J Hematol. 2016;91(7):714–718. [DOI] [PubMed] [Google Scholar]
- 11.Polfus LM, Khajuria RK, Schick UM, et al. Whole-exome sequencing identifies loci associated with blood cell traits and reveals a role for alternative GFI1B splice variants in human hematopoiesis. Am J Hum Genet. 2016;99(3):785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ferreira CR, Chen D, Abraham SM, et al. Combined alpha-delta platelet storage pool deficiency is associated with mutations in GFI1B. Mol Genet Metab. 2017;120(3):288–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marneth AE, van Heerde WL, Hebeda KM, et al. Platelet CD34 expression and alpha/delta-granule abnormalities in GFI1B- and RUNX1-related familial bleeding disorders. Blood. 2017;129(12):1733–1736. [DOI] [PubMed] [Google Scholar]
- 14.Hernandez A, Villegas A, Anguita E. Human promoter mutations unveil Oct-1 and GATA-1 opposite action on Gfi1b regulation. Ann Hematol. 2010;89(8):759–765. [DOI] [PubMed] [Google Scholar]
- 15.Kitamura K, Okuno Y, Yoshida K, et al. Functional characterization of a novel GFI1B mutation causing congenital macrothrombocytopenia. J Thromb Haemost. 2016;14(7):1462–1469 [DOI] [PubMed] [Google Scholar]
- 16.Zweidler-Mckay PA, Grimes HL, Flubacher MM, Tsichlis PN. Gfi-1 encodes a nuclear zinc finger protein that binds DNA and functions as a transcriptional repressor. Mol Cell Biol. 1996;16(8):4024–4034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beauchemin H, Shooshtarizadeh P, Vadnais C, Vassen L, Pastore YD, Moroy T. Gfi1b controls integrin signaling-dependent cytoskeleton dynamics and organization in megakaryocytes. Haematologica. 2017;102(3):484–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.