Abstract
Pain is the most common manifestation of both acute and chronic inflammation that often challenges patients with rheumatic disease. Simply, we attribute this to local joint changes of pH in joints, the formation of radicals, enhanced joint pressure, or cytokine release acting on local nerves to produce pain. However, there is a more complex interplay of interactions between cytokines, mediators of inflammation, and ion channels that influence the final immune response and our perception of pain. Endocannabinoids, a group of less well-known endogenous bioactive lipids, have such manifold immunomodulatory effects able to influence both inflammation and pain. In this review, we overview the endocannabinoid system, its role in pain, inflammation, and immune regulation, and highlight the emerging challenges and therapeutic hopes.
Keywords: Endocannabinoids, pain, inflammation, arthritis
The Endocannabinoid System
Since the identification of endocannabinoid receptors, the potential of cannabinoid pharmacotherapy in clinical pain conditions has received much attention (1, 2). The three fundamental constituents of the endocannabinoid system include the endocannabinoid signaling molecules, G-protein-coupled cannabinoid receptors, and enzymes involved in ligand biosynthesis and inactivation. All these components have since been mapped throughout the peripheral nerve terminals and extend up to the supraspinal centers, which constitute the pain (nociceptive) pathway (3). Anti-nociception refers to the act or process of blocking the detection of painful or harmful stimuli by sensory neurons, thereby reducing ones sensitivity to pain. Preclinical studies of systemically administered cannabinoids have noted anti-nociception as a prominent feature in various models of pain (4). It is well accepted that endocannabinoids have anti-nociceptive effects (5–7). Under physiological conditions, potentially harmful stimuli are integrated by the nociceptors of primary afferent fibers and relayed for final processing in the supraspinal centers. In pathological states, the relaying of noxious input by the nervous system is corrupted, resulting in abnormal nociceptive signaling and an aberration in pain responses (8). The analgesic effects of cannabinoids and their ligands are primarily mediated by the cannabinoid receptor 1 (CB1) via inhibition of presynaptic gamma-aminobutyric acid (GABA) and glutamatergic transmission. Within the nervous system, GABA transmission suppresses neuronal excitability (4, 9). Despite the endocannabinoids therapeutic appeal, its clinical application is marred by a plethora of psychoactive side effects, necessitating a cautious and critical evaluation as well as a search for an alternate cannabinoid-based approach or analogs to analgesia (10). In this review, the analgesic properties mediated by the endocannabinoid system is discussed and their potential use as novel pharmacotherapies in the treatment of arthritic pain is evaluated.
Endocannabinoid Ligands
The endocannabinoid system is regulated by a series of lipid signaling molecules known as “endocannabinoids,” belonging to the N-acylethanolamines. Of these, the two most widely investigated are anandamide (arachidonoyl ethanolamine [AEA]), initially isolated from porcine brain, and 2-arachidonoylglycerol (2-AG), initially isolated from canine intestines (11, 12). AEA is responsible for maintaining basal endocannabinoid signalling, binding to both the CB1 and CB2 receptors (13). At elevated concentrations, AEA also functions as a full agonist for the transient receptor potential vanilloid 1 (TRPV1), an ionotropic receptor responsible for the integration of noxious stimuli that cause pain (14, 15). In contrast to AEA, 2-AG functions as a full agonist for both CB1 and CB2 (16). In addition to these compounds, a series of other biochemically similar endocannabinoids such as 2-AG ether, virodhamine and N-arachidonoyl dopamine have been discovered. Knowledge of their function and regulatory role remains in its infancy.
Endocannabinoid Synthesis and Degradation
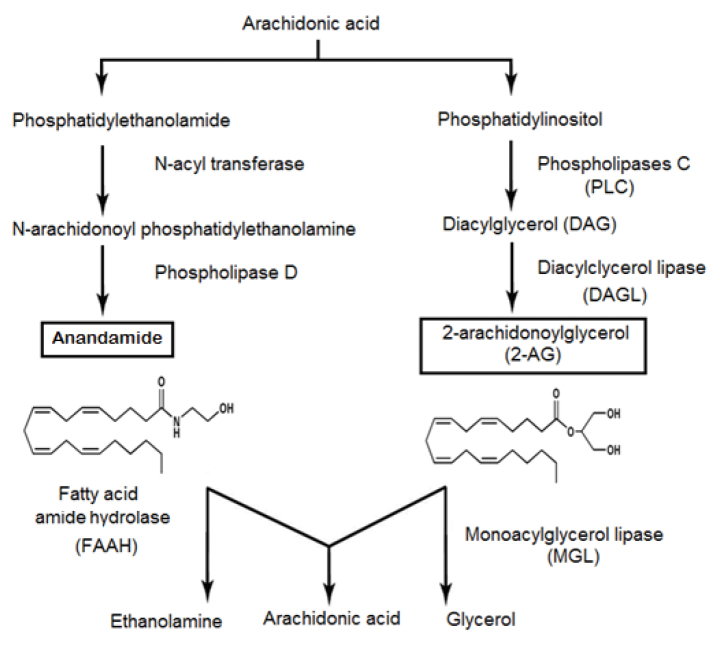
While the predominant endocannabinoids AEA and 2-AG are both lipid molecules generated from the breakdown of arachidonic acid, they share very few similarities in their biosynthetic pathways, as shown in Figure 1 (17). Endocannabinoid synthesis is a result of enzymatic cleavage of phospholipids within the cell membrane. Once released, the endocannabinoid ligands diffuse, acting locally as retrograde messengers to regulate the release of multiple presynaptic messengers. Following cellular uptake, the endocannabinoid ligands are quickly transported from the synaptic space and inactivated through subsequent catabolism via specific enzymes within the intracellular environment (18). This in-activation is catalyzed by intracellular enzymes which are unique to each endocannabinoid, and include fatty acid amide hydrolase (FAAH), the principal enzyme for AEA, and monoacyl glycerol lipase (MAGL) for the breakdown of 2-AG, as shown in Figure 2 (19). Enzymatic degradation of these endocannabinoids yields arachidonic acid and ethanolamine from AEA and glycerol from 2-AG, respectively (20).
Figure 1.
Main pathways for the biosynthesis and degradation of the two main endocannabinoids: anandamide and 2-AG (17)
Figure 2.
The inactivation of endocannabinoids
FAAH: fatty acid amide hydrolase; MAGL: monoacylglycerol lipase; AMT: anandamide membrane transport (19)
Endocannabinoid Receptors
Various inhibition studies of the cannabinoid receptors have shown that endocannabinoids attenuate and suppress the perception of pain (21). The anti-nociceptive potency of cannabinoid agonists is strongly correlated with their ability to displace binding ligands from the cannabinoid receptor, obstructing their signaling. Localization studies using receptor binding immunohistochemistry and in-situ hybridization have mapped the distribution of the cannabinoid receptors along all levels of the pain nexus, providing a neuroanatomical framework befitting to the function of the cannabinoid system in sensory processing. The widespread expression of the cannabinoid receptors along the principal pain processing sites offer boundless opportunities for the development of analgesics for various pain conditions.
Cannabinoid receptor 1
Cannabinoid receptor 1 is the principal receptor of the central nervous system (CNS) and is densely expressed in several areas of the brain and supraspinal regions involved with nociceptive transmission. These areas include the cortex, basal ganglia, hippocampus, dorsal root ganglion (DRG), spinal cord, thalamus, periaqueductal gray (PAG), and amygdala (22). More recently, CB1 was shown to be densely cumulated within the frontal-limbic brain circuits that are key in both the affective and emotional manifestations of human pain. CB1 inhibition of ascending nociceptive transmission, mainly at the thalamus level, has been shown to modify the emotional pain component acting at the limbic system and cortical areas. At the supraspinal level, CB1 activates the descending inhibitory pathway by suppressing GABA release in the PAG and rostral ventral medulla, intercepting descending input to the spinal cord nociceptive system through CB1 function (22, 23). At the level of the spinal cord, CB1 is densely expressed at the presynaptic terminals of primary afferents and excitatory neurons and regulate the transmission of noxious stimuli to the brain by inhibiting neurotransmitter release (24). As well as these central effects, CB1 receptors localize on sensory terminals in the periphery, gating the propagation of pain signals, contributing to peripheral analgesia (25). Indeed, inhibition of peripheral CB1 receptor expression suppressed the analgesic effects of administered cannabinoids in a neuropathic pain model, demonstrating the importance of peripheral CB1 function in cannabinoid-mediated analgesia (26).
Cannabinoid Receptor 2
In the periphery, CB2 receptors are widely located on immune cells and therefore represent a target for influencing inflammatory pain processing. Direct evidence of CB2-mediated anti-nociceptive effects was first reported in 1999 using the selective CB2 agonist, HU-308, which markedly decreased nociceptive behavior in the hind paw model of formalin treated rats (27). CB2 receptor agonists contributed to anti-nociception in other models of both inflammatory and nociceptive pain by suppressing the local secretion of pro-inflammatory factors by non-neural cells, which sensitize neighboring nociceptive neuron terminals. Stimulation of peripheral CB2 receptors therefore mediate anti-nociceptive responses in settings of neuropathic pain or inflammatory hyperalgesia by acting locally on immune cells in the periphery and microglia in the CNS (28). Although originally described as being restricted to immune cells, evidence for CB2 receptor expression in neural cells involved in pain perception and modulation has emerged (29). In vitro studies show CB2 receptor expression in human DRG sensory neurons and nerve fibers within the synovium and digit skin (30). Recently, CB2 receptors were detected on β-endorphin-containing keratinocytes on the epidermis of rat hind paws. This expression supports the notion that CB2-mediated effects may be regulated by a functional interplay between the endocannabinoid and μ-opioid systems, resulting in an indirect activation of opioid receptors expressed in primary afferent pathways (31). Thus, cannabinoid compounds may modulate pain by a number of pathways and a number of different mechanisms.
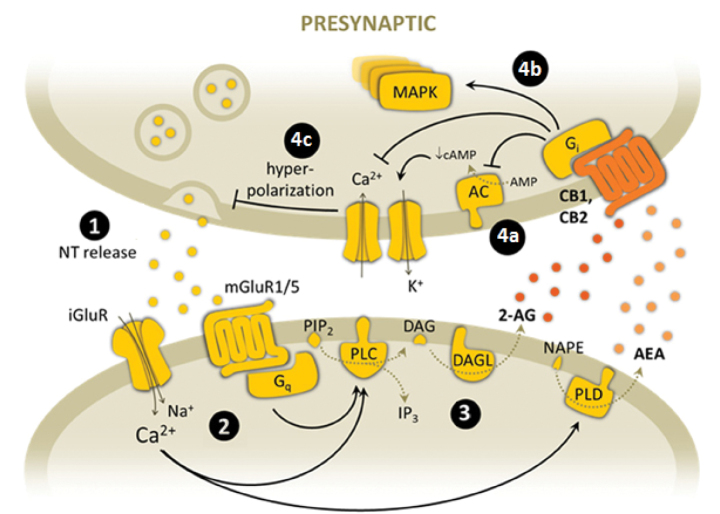
Intracellular Endocannabinoid Signaling
Cannabinoid receptors located on the presynaptic neurons regulate the synthesis and secretion of neurotransmitters to the synapse, as shown in Figure 3 (32). Action potentials in the presynaptic neuron cause the release of neurotransmitters within vesicles. Binding of the neurotransmitters to their postsynaptic receptors causes a depolarization of the postsynaptic membrane and the accumulation of Ca2+ in the cytoplasm, stimulating the activation of the calcium-dependent enzymes (phospholipase [PL] and diacylglycerol lipase [DAGL]) in charge of the biosynthesis of endocannabinoids. After synthesis, the endocannabinoid ligands are released and diffuse within the synapse, acting locally as retrograde messengers to regulate the release of multiple presynaptic messengers. Binding of the endocannabinoid ligands to the CB receptors induces a G-protein-dependent inhibition of presynaptic Ca2+ influx through voltage-gated Ca2+ channels. In addition to the pathway mentioned above, endocannabinoid binding may also cause the activation of enzymes PI3 kinase, sphingomye-linase, and phospholipase. As a result, hyperpolarization of the presynaptic membrane occurs, modulating the release of neurotransmitter and thus synaptic transmission. CB1 receptor stimulation regulates the intensity and duration of synaptic transmission (22). Similarly, in immune cells, CB2 activation has been shown to mediate an inhibitory effect on activation, cell motility and secretion of inflammatory mediators (28). Endocannabinoids are internalized by a selective transporter and degraded by specific enzymes (FAAH, MAGL) (32).
Figure 3.
Overview of the endocannabinoid-mediated synaptic signaling. (1) Action potential generated and cytoplasmic vesicles fuse with presynaptic membrane to release neurotransmitters (NT). (2) Binding of neurotransmitter on postsynaptic membrane receptors causes Ca2+ accumulation, depolarization of the membrane, and activation of calcium-dependent enzymes responsible for the biosynthesis of endocannabinoids (PL, DAGL). (3) Endocannabinoid retrograde transport and CB receptor activation. (4) Target signaling pathways reduce neurotransmitter release: (4a) suppression of adenyl cyclase (AC) activity, (4b) activation of protein kinase cascades, (4c) modulation of Ca2+ and K+ ion channels and membrane hyperpolarization and inhibition of NT release.
NT: neurotransmitter; iGluR: ionotropic glutamate receptor; mGluR: metabotropic glutamate receptor; PIP2: phosphatidylinositol bisphosphate; DAG: diacylglicerol; 2-AG: 2-arachidonoylglycerol; NAPE: N-arachidonoyl-phosphatidylethanolamine; AEA: anandamide; PLC: phospholipase C; DAGL: diacylglycerol lipase; PLD: phospholipase D; AC: adenyl cyclase; cAMP: cyclic AMP; MAPK: mitogen-activated protein kinase; PKC: protein kinase C; X+: unspecific cation32
Endocannabinoids and Arthritic Pain
Arthritic pain is both nociceptive, resulting from the irritation of sensory nociceptors responsible for the detection of potentially noxious stimuli, and neuropathic, resulting from a malfunction in the somatosensory nervous system (33). Extensive innervation within the joint helps facilitate the sensation of pain in inflammatory joint conditions (34). Under normal physiological conditions, joint nociceptors are localized within the articular structure of the joint. Under inflammatory conditions, these silent nociceptors expand to adjacent tissues and function to propagate and amplify the sensation of pain (33, 34). The altered neuronal activity, also known as neuronal plasticity, is collectively believed to constitute the foundation of rheumatic pain and is characterized by hyperalgesia, an elevated noxious response to painful stimuli, and allodynia, a painful response to a normally mild and harmless stimulus. The primary components of the endocannabinoid signaling system (CB1, CB2, and FAAH) are characteristically expressed in the synovium of both osteoarthritic (OA) and rheumatoid arthritic (RA) patients, with compelling evidence to demonstrate an active participation in the pathophysiology of joint pain (35). Preclinical and clinical studies support the therapeutic application of cannabinoids in the treatment of chronic pain, and to date, patients suffering from chronic arthritic and musculoskeletal pain represent the most prevalent users of medicinal cannabis (36). Despite this optimism, hesitation in clinical application is prevalent with extensive guidelines published in different countries (37–39).
Changes in CB Receptor Expression
In chronic pain states, central sensitization results in the reorganization of the spinal nociceptive circuitry through a localized up-regulation of CB1 and CB2 receptor expression along the pain nexus. As a result, hypersensitivity manifests as both hyperalgesia and allodynia occurs, for which standard analgesic treatments are unsuccessful. In neuropathic settings, both the up-regulation of spinal CB2 receptors (29, 40) and a greater effect of intrathecally administered cannabinoid CB2 agonists have been noted (40).
The functional importance of CB2 up-regulation in the integration and sensitization of OA pain has been demonstrated through the use of genetically modified mice (41). In pain experiments, mechanical induced allodynia was suppressed in transgenic mice overexpressing CB2 in the CNS41. By contrast, no significant changes in pain responses were observed in CB1 knockout mice, suggesting that the centrally controlled mechanisms of these nociceptive responses are primarily regulated via CB2, with minor input via CB1 (41). This is consistent with previous studies showing increased levels of AEA, 2-AG, and their synthesizing enzymes within the spinal cord of rat monoiodoacetic acid (MIA) models of OA (42). The tonic release of spinal endocannabinoid levels counteract peripheral sensitization through enhanced endocannabinoid signaling within the spinal cord (42). In a rat model of OA pain, systemic administration of CB2 agonist, JWH-133, suppressed pain behavior, while acute administration to the spine inhibited mechanically stimulated noxious neurotransmission (43).
More recently, an increased expression of CB1 accompanied by OA development has been demonstrated (36). CB1 receptors are located on peripheral sympathetic nerve terminals as well as on nociceptive nerve fibers, where they modulate adrenergic signaling to influence cytokine production (44). Stimulation of CB1 receptors desensitize neurons by modulating ion channels of the Transient receptor potentials (TRP), suppressing action potentials and reducing pain. Externally administered AEA and CB1 agonist, arachidonyl-2-chloroethylamide (ACEA), have been shown to significantly reduce the firing rate of afferent nerve fibers in OA joints, but not in the control joints, suggesting a tonic release of endocannabinoids at the joint level in OA. Considering the close positioning of transient receptor potentials type 1 (TRPV1) and CB1 receptors in relation to nociceptive transmission both have drawn interest in the development of novel therapies of OA pain and is discussed in more detail below (3, 9).
Changes in TRP Stimulation
TRP channels, also known as capsaicin receptors, are a group of ligand-gated ion channels responsible for the detection and integration of noxious stimuli (14, 44). Primarily found in the nociceptive neurons of the peripheral nervous system, stimulation of the transient receptor potential vanilloid receptor type 1 (TRPV1) results in a cation influx and the production of an action potential that consequently results in the sensation of pain. As such, the TRPV1 channels represent a prime focus for the development of novel analgesics. Modulators of TRPV1 function include agonists such as capsaicin, used clinically as creams or patches, to desensitize TRPV1 activity and reduce pain. Indeed, it has been well-documented that heavy capsaicin dosing depletes neuropeptides levels, with a resultant suppression in the severity of adjuvant-induced joint disease (45). Other antagonists that block TRPV1 activity (capsazepine, ruthenium red) as well as clinical trial compounds (AMG517, GRC6211, NGD 8243) have also been shown to be effective in reducing pain but have not progressed in development due to undesirable side effect levels of hyperthermia.
In arthritis, TRPV1 receptors are located on peripheral cells and sensory neurons abundantly expressed in arthritic synovial tissue. The importance of these receptors in arthritis is highlighted in TRPV1−/− knockout animals that demonstrate elevations in pain threshold and an associated reduction in joint inflammation (46). In addition to enhanced neurotransmitter release, stimulation of TRPV1 is associated with increases in inflammatory mediators contributing to joint inflammation (47). A recent study found that tumor necrosis factor-alpha (TNF-α)-induced mechanical hyperalgesia in an arthritic model could be blocked by a central, but not peripheral, injection of a TRPV1 antagonist (48). Similarly, interleukin-1 beta (IL-1β) can upregulate TRPV1 expression in arthritic rat DRG neurons, as well as sensitize articular C-fibers (48). Together, these findings indicate a novel link between TRP channels and cytokines in the generation of joint pain through central sensitization (44). Similar to cytokines, endocannabinoid’s AEA, OEA, and palmitoylethanolamide (PEA) can activate the TRPV1 receptors (49, 50). AEA is believed to modulate synaptic plasticity, a key component in arthritic pain, through actions at both the pre and postsynaptic TRPV1 channels (15). On exposure, the TRPV1 channels are rapidly desensitized, resulting in reduced calcium influx and increased pain thresholds. In a recent study, TRPV1 activation via AEA produced nociceptive behavior through the excitation of C-fibers (51). Additionally, cross-talk between CB1 and TRPV1 co-expressed on sensory nerves, modulate pain and inflammation in arthritis (52). When co-expressed, CB1 agonists suppressed TRPV1 activation through dephosphorylation, increasing the threshold level for agonists (47). Pharmacological elevations of AEA in an arthritic rat were shown to suppress hypersensitivity of afferent nociceptors and elevated pain thresholds by a process containing CB1 and TRPV1 channels (15). This mechanism was confirmed through the use of joint blood flow experiments, which demonstrated that the vasomotor effects of a CB1 agonist in rat knees could be inhibited by TRPV1 antagonism (53). Similarly, in a model of OA pain, local administration of CB1 agonist ACEA reduced mechanosensitivity of afferent nerve fibers, suppressing nociceptive transmission in OA and healthy rat knee joints. Inhibition of both the TRPV1 and CB1 receptors suppressed ACEA responses, indicating the dual involvement of both channels in ACEA-mediated nociception. At present, TRPV1 has been shown to co-localize with CB1 in sensory DRG and the spinal cord, and brain neurons and with CB2 receptors in sensory neurons and osteoclasts (30).
More recently, the transient receptor potential canonical 5 (TRPC5) expressed on fibroblast like synoviocytes cells within the joint has been shown to protect against pain and inflammation in arthritic mice (54). Inhibition of TRPC5 using knockouts or pharmacological agents is correlated well with the propagation of joint inflammation and hyperalgesia, providing evidence that TRCP5 is a negative regulator of inflammation. The proposed mechanism of action suggested by Alawi et al. (54) is that TRPC5 acts to suppress inflammation by influencing the early cytokine-immunity axis discussed below (54). These exciting results highlight how TRP receptors protect against pain and vascular joint inflammation in arthritis.
Endocannabinoids and Inflammation
There is increasing and exciting evidence showing that endocannabinoids regulate the immune response at both the innate (monocytes, macrophages, neutrophils, NK cells, eosinophils, basophils, mast cells) and adaptive immune level (55). Immune cells are not only able to be influenced, but are also able to generate and secrete endocannabinoids that lead to changes in immune-cell behavior as well as the production of other inflammatory factors that subsequently influence tissue inflammation (56, 57).
The Role of Endocannabinoids in Joint Inflammation
Chinese healers, who have known about the healing properties of endocannabinoids since 2000 BC, have claimed that cannabis “undoes rheumatism” (58). Evidence supporting the anti-inflammatory effects of endocannabinoids come from preclinical studies that have shown that all classes of cannabinoids including phytocannabinoids (tetrahydrocannabinol, cannabidiol) and synthetic analogs such as Ajulemic acid, “Nabilone,” and elmiric acid possess anti-inflammatory effects (18). These anti-inflammatory effects may be due to direct action on participating immune cells, or by changes in the local endocannabinoid concentrations that then carry out anti-inflammatory actions. In arthritis, persistent inflammation results in the infiltration of immune cells and the subsequent development of hypersensitivity. Synovial serum samples from patients with RA consistently express elevated cytokine levels such as TNF-α, interleukin-6 (IL-6), and IL-1β, which act directly to sensitize joint nociceptors and stimulate the release of prostaglandins (59, 60). In an elegant study by Sancho et al. it was shown that AEA can inhibit TNF-α-induced NF-κβ activation by direct inhibition of the IκB kinase (60). The protective effects of endocannabinoids have been noted in other inflammatory conditions such as multiple sclerosis, celiac disease, and periodontitis (18).
Malfait et al. (61) have shown that endocannabinoids can block progression of joint inflammation in rodent models of arthritis. The anti-inflammatory potential of CB2 has been confirmed in mouse models of arthritis (61, 62). The protective CB2 effects include the suppression of pro-inflammatory cytokine and damaging proteinases secretion; as well as regulating immune cell adhesion and migration to the inflamed joint. Together, this helps slow the perpetuation of disease and alleviate associated arthritic pain primarily derived from localized inflammation (36). Further to this, elevated levels AEA and 2-AG are detected in the synovial fluid of RA and OA patients, but absent in healthy controls, suggest that local endocannabinoid secretion may assist in minimising inflammation in the arthritic joints (4, 60). With both cannabinoid receptors and endogenous ligands present in inflamed human joints, targeting this system may hold therapeutic promise for both inflammatory, as well as degenerative arthritis (60). Administration of cannabinoid agonists, WIN55212 and CP55940, have shown the ability to reduce inflammatory IL-6 and interleukin-8 (IL-8) cytokine production by fibroblast like synoviocytes cells, ameliorating acute inflammation and associated pain in arthritic joints (2, 63). Similarly, systemic administration of the CB2 agonist, JWH133, suppressed pain and corrected deviation in circulating pro- and anti-inflammatory cytokines in the rat MIA model (43). These anti-inflammatory effects are limited by the rapid cellular uptake and degradation of endocannabinoid metabolites but can be overcome through the inhibition of the catabolic enzyme FAAH allowing longer physiological effects (35). In-vivo studies by Krustev et al. (64) reported that FAAH inhibition with compound URB597 can elevate tissue concentrations of AEA by inhibiting local endocannabinoid degradation and dampen inflammatory pain in rodent models of OA. In a similar study, URB597 suppressed inflammatory hyperemia in a mouse model of acute arthritis (64). In the periphery, FAAH inhibition mediates anti-inflammatory effects by down regulating cytokine production and the desensitization of TRPV1, resulting in analgesia (15). Inhibition of AEA catabolism is said to have promising effects in the management of OA pain mediated by both anti-inflammatory (65) and anti-hyperalgesia actions (62). Therapeutic intervention in peripherally restricted CB1 antagonist and FAAH inhibition are promising strategies to ameliorate chronic inflammation and pain in RA.
Neurogenic Inflammation
In neurogenic inflammation, local afferent neurons secrete inflammatory mediators such as neurokinin A, substance P (SP), and calcitonin gene-related peptide which perpetuate inflammation. Once these neuropeptides are secreted, they act on adjacent mast cells to release histamine, which in turn evoke the release of SP and calcitonin gene-related peptide creating a positive feedback loop which amplifies the inflammatory response. In arthritic joints, the subsequent release of immunomodulatory molecules from the peripheral terminals of Aδ and C-fibers result in the development of local neurogenic inflammation (65). These neuropeptides sensitize local articular afferents in the inflamed joint and stimulate the increases in TRPV1 expression, sustaining nociceptive signaling and the maintenance of neuropathic pain (43, 66). In RA, enhanced levels of nerve growth factor, prostaglandins and bradykinins within the synovium sensitize TRPV1 to the inflammatory stimuli and aggravate pain (67).
Neural-immune Circuits in Inflammation
In RA, sustained stimulation of the sympathetic nervous system propagate inflammation through norepinephrine signaling. The influence of adrenergic signaling and the loss of sympathetic nerve fibers in the inflamed tissue in RA has been demonstrated in several animal models of arthritis (68). Sympathectomy in the early phase of the disease has been shown to ameliorate experimental arthritis, indicating the pro-inflammatory influence of adrenergic signaling (69). During arthritic inflammation, nerve repulsion factors released by macrophages result in the withdrawal of sympathetic neurons from the synovial tissue and the subsequent depletion of synovial norepinephrine concentrations (68). As a result, inadequate norepinephrine levels causes a shift from previously stimulated anti-inflammatory α-adrenergic to β-adrenergic signaling, favoring pro-inflammatory cascades (70). Peripheral norepinephrine release from the sympathetic terminals is regulated through the CB1 receptors and can be stimulated by respective CB1 endocannabinoid agonists such as AEA and 2-AG. In adjuvant arthritis, β2 receptor stimulation suppresses levels of TNF-α, increases anti-inflammatory interleukin-10 (IL-10), shifts the T-cell profile, and enhances T-regulatory immune responses potentiating a widespread reduction in joint destruction, inflammation, and pain (71). Similarly, it has been demonstrated that antagonism of CB1 at splenic sympathetic terminals mediates strong anti-inflammatory effects and improves collagen-induced arthritis in an in-vivo mouse model, which was reversed by β2 adrenergic antagonism (72). Recent research using CB1 knockout mice showed impaired neurogenesis when compared to wild type, suggesting endogenous CB1 signaling may promote basal levels of neurogenesis (73, 74). While further studies are required, this possible application to sympathetic nerves may promote the extension of nerves previously lost from the synovial space during arthritic inflammation (68, 70).
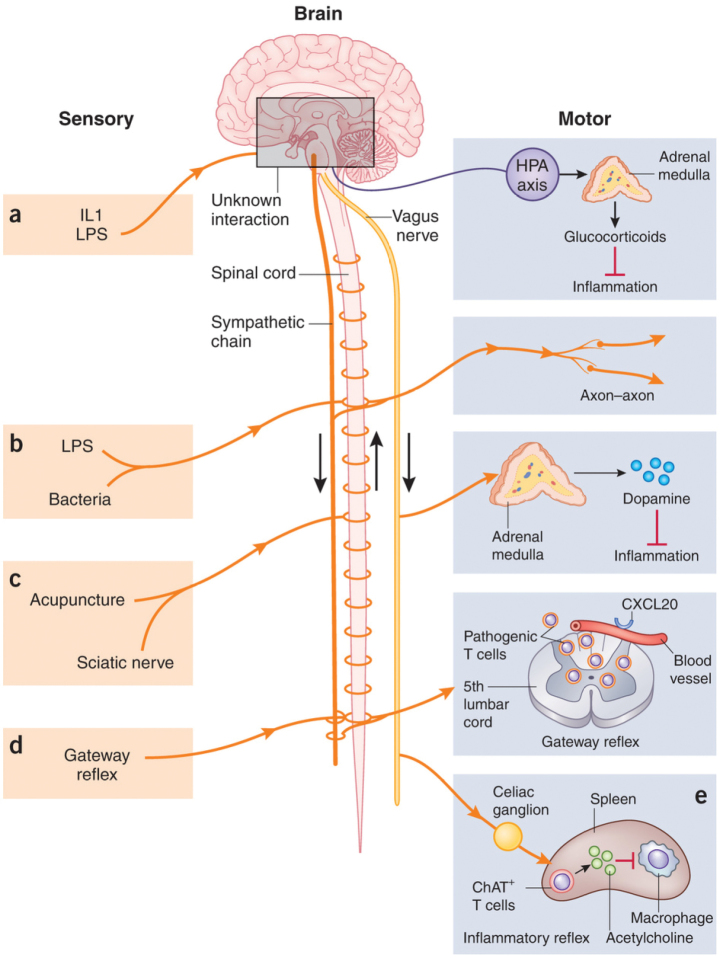
As discussed above, neural circuits can modulate immune responses by secreting compounds that influence cell function or through the detection of inflammatory mediators, which in turn causes the nerves to relay signals or release immunomodulatory peptides back to the immune system. The release of IL-1 following inflammation, for instance, act on the hypothalamic-pituitary adrenal axis via neuronal input to release glucocorticoids that then influence the peripheral immune response outcome. Such neural-immune reflex circuits that regulate innate immunity are well understood. Other neural-immune reflexes such as dopamine and electro-acupuncture based circuits also exist but are less-well defined, as shown in Figure 4 (75). The effects of acupuncture stimulation on neural reflex immunity circuits provides important and exciting insights into the regulation of innate immunity and the discovery of new targets as anti-inflammatory therapeutics (76).
Figure 4.
Neural reflex immunity circuits. Various stimuli such as (a) inflammatory (e.g., IL1), (b) bacterial, (c) acupuncture, or (d) pressure/acupuncture are detected by sensory afferent nerves and relayed to interneurons located in the spinal cord/brainstem. The generated efferent signals work to dampen the innate immune responses signaling through (a) efferent neurons of the hypothalamic-pituitary adrenal (HPA) axis, (c) via the release of dopamine via the adrenal medulla, or (b) via the local axon-axon reflex which suppress the innate immune responses by cytokine release and immune cell activation. Efferent signals sent via the sympathetic system (d) or vagus nerve (e), release neurotransmitters that influence the immune response (75)
Current Work and Future Direction of Research
In this review, we have focused on the basic sciences of endocannabinoids and overviewed their role in inflammation and pain. While compelling evidence suggests the therapeutic potential of endocannabinoids therapy in arthritis and chronic musculoskeletal pain syndromes, barriers to research include insufficient legally registered marijuana manufacturers and a limited number of clinical trials. In the study by Blake et al. (77), the effect of cannabis spray, “Nabiximols,” improved pain scores and disease activity when compared with placebo in 28 joints observed. Treatment took place over a 5-week period in a randomized, double-blinded trial group of 58 RA patients. Although adverse events in the active treatment group were not serious, they were common (77). In studies examining the endocannabinoid-based drug “Nabilone” on pain outcomes in fibromyalgia, the statistically significant effects were outweighed when side effects were taken into consideration (78–80). In a separate review of cannabinoid-based therapies in chronic pain conditions, three of which were rheumatic pain (2 fibromyalgia, 1 RA), concluded that while the majority demonstrated improvements in pain, no direct evidence on effects of herbal marijuana in rheumatic pain (78).
The FAAH inhibitor, PF-04457845, showed both analgesic and anti-inflammatory effects in animal studies comparable to naproxen (79). However, when compared to naproxen, PF-04457845 was ineffective for OA pain when compared to placebo-control in a randomized phase II clinical trial (79). As endocannabinoids do not solely mediate their effects via the CB1/CB2 receptors, it is thought activity mediated via the TRPV channels hampered analgesic potential (80). Also interesting and worth mentioning is the relationship between cyclooxygenase enzyme (COX) inhibitors and endocannabinoids. COX enzyme is involved in the generation of prostaglandins from arachidonic acid that mediates inflammation. What is less well appreciated is that COX enzyme also metabolizes endocannabinoids to prostaglandin-glycerol esters for 2-AG and prostaglandin ethanolamines for AEA, as shown in Figure 2. These bioactive lipids may have a role in inflammation (81). What is also not known is the functional consequences between cyclooxygenase-2 (COX-2) inhibition and endocannabinoid effects. More recently, focus has been drawn to dual-acting compounds such as OMDM-198. OMDM-198 works to increase FAAH substrate concentrations while simultaneously inhibiting TRPV1 receptors. In an MIA rat model of OA, OMDM-198 exhibited a meaningful reversal of hypersensitivity in joint pain, representing a promising avenue in endocannabinoid pain management.
While the benefits of pharmaceutically prepared cannabinoid treatments have been inconsistent with large variations between species and population groups, they appear to have clinical benefits warranting the need for further investigation. Comprehensive evaluations through well-controlled randomized trials are also required to clarify the true clinical efficacy and long-term risks associated with cannabinoid therapy. Advancements in our understanding of the endocannabinoid system and cannabinoid pharmacology, has raised the hope of exciting new pharmacological entities. Cannabis-based medications which enhance endocannabinoid function may represent a novel therapeutic solution to disorders associated with chronic pain and remains a promising avenue of contemporary importance.
Footnotes
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - N.M., N.B.; Design - N.M., N.B.; Supervision - N.M.; Resources - N.M.; Materials - N.M.; Data Collection and/or Processing - N.B.; Analysis and/or Interpretation - N.B., N.M.; Literature Search - N.B.; Writing Manuscript - N.B., N.M.; Critical Review - N.B., N.M.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Mechoulam R, Devane WA, Breuer A, Zahalka J. A random walk through a cannabis field. Pharmacol Biochem Behav. 1991;40:461–4. doi: 10.1016/0091-3057(91)90347-5. https://doi.org/10.1016/0091-3057(91)90347-75. [DOI] [PubMed] [Google Scholar]
- 2.Russo EB. History of cannabis and its preparations in saga, science, and sobriquet. Chem Biodivers. 2007;4:1614–48. doi: 10.1002/cbdv.200790144. https://doi.org/10.1002/cbdv.200790144. [DOI] [PubMed] [Google Scholar]
- 3.Hohmann AG. Spinal and peripheral mechanisms of cannabinoid antinociception: behavioural, neurophysiological and neuroanatomical perspectives. Chem Phys Lipids. 2002;121:173–90. doi: 10.1016/s0009-3084(02)00154-8. https://doi.org/10.1016/S0009-3084(02)00154-8. [DOI] [PubMed] [Google Scholar]
- 4.Walker JM, Huang SM. Endocannabinoids in pain modulation. Prostaglandins Leukot Essent Fatty Acids. 2002;66:235–42. doi: 10.1054/plef.2001.0361. https://doi.org/10.1054/plef.2001.0361. [DOI] [PubMed] [Google Scholar]
- 5.Richardson JD, Aanonsen L, Hargreaves KM. Antihyperalgesic effects of spinal cannabinoids. Eur J Pharmacol. 1998;345:145–53. doi: 10.1016/s0014-2999(97)01621-x. https://doi.org/10.1016/S0014-2999(97)01621-X. [DOI] [PubMed] [Google Scholar]
- 6.Calignano A, La Rana G, Giuffrida A, Piomelli D. Control of pain initiation by endogenous cannabinoids. Nature. 1998;394:277–81. doi: 10.1038/28393. https://doi.org/10.1038/28393. [DOI] [PubMed] [Google Scholar]
- 7.Strangman NM, Patrick SL, Hohmann AG, Tsou K, Walker JM. Evidence for a role of endogenous cannabinoids in the modulation of acute and tonic pain sensitivity. Brain Research. 1998;813:323–8. doi: 10.1016/s0006-8993(98)01031-2. https://doi.org/10.1016/S0006-8993(98)01031-2. [DOI] [PubMed] [Google Scholar]
- 8.Heinricher MM, Tavares I, Leith JL, Lumb BM. Descending control of nociception: specificity, recruitment and plasticity. Brain Res Rev. 2009;60:214–25. doi: 10.1016/j.brainresrev.2008.12.009. https://doi.org/10.1016/j.brainresrev.2008.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pertwee RG. Cannabinoid receptors and pain. Prog Neurobiol. 2001;63:569–611. doi: 10.1016/s0301-0082(00)00031-9. https://doi.org/10.1016/S0301-0082(00)00031-9. [DOI] [PubMed] [Google Scholar]
- 10.Fitzcharles MA, McDougall J, Ste-Marie PA, Padjen I. Clinical implications for cannabinoid use in the rheumatic diseases: potential for help or harm? Arthritis Rheum. 2012;64:2417–25. doi: 10.1002/art.34522. https://doi.org/10.1002/art.34522. [DOI] [PubMed] [Google Scholar]
- 11.Devane WA, Hanus L, Breuer A, Pertwee RG, Stevenson LA, Griffin G, et al. Isolation and structure of a brain constituent that binds to the cannabinoid receptor. Science. 1992;258:1946–9. doi: 10.1126/science.1470919. https://doi.org/10.1126/science.1470919. [DOI] [PubMed] [Google Scholar]
- 12.Mechoulam R, Ben-Shabat S, Hanus L, Ligumsky M, Kaminski NE, Schatz AR, et al. Identification of an endogenous 2-monoglyceride, present in canine gut, that binds to cannabinoid receptors. Biochem Pharmacol. 1995;50:83–90. doi: 10.1016/0006-2952(95)00109-d. https://doi.org/10.1016/0006-2952(95)00109-D. [DOI] [PubMed] [Google Scholar]
- 13.Gonsiorek W, Lunn C, Fan X, Narula S, Lundell D, Hipkin RW. Endocannabinoid 2-arachidonyl glycerol is a full agonist through human type 2 cannabinoid receptor: antagonism by anandamide. Mol Pharmacol. 2000;57:1045–50. [PubMed] [Google Scholar]
- 14.Schaible HG, Von Banchet GS, Boettger MK, Brauer R, Gajda M, Richter F, et al. The role of proinflammatory cytokines in the generation and maintenance of joint pain. Ann N Y Acad Sci. 2010;1193:60–9. doi: 10.1111/j.1749-6632.2009.05301.x. https://doi.org/10.1111/j.1749-6632.2009.05301.x. [DOI] [PubMed] [Google Scholar]
- 15.Starowicz K, Przewlocka B. Modulation of neuropathic-pain-related behaviour by the spinal endocannabinoid/endovanilloid system. Philos Trans R Soc Lond B Biol Sci. 2012;367:3286–99. doi: 10.1098/rstb.2011.0392. https://doi.org/10.1098/rstb.2011.0392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sugiura T, Kondo S, Kishimoto S, Miyashita T, Nakane S, Kodaka T, et al. Evidence that 2-arachid-onylglycerol but not N-palmitpylethanolamine or anandamide is the physiological ligand for the cannabinoid CB2 receptor. J Biol Chem. 2000;275:605–12. doi: 10.1074/jbc.275.1.605. https://doi.org/10.1074/jbc.275.1.605. [DOI] [PubMed] [Google Scholar]
- 17.Castillo PE, Younts TJ, Chávez AE, Hashimotodani Y. Endocannabinoid signaling and synaptic function. Neuron. 2012;76:70–81. doi: 10.1016/j.neuron.2012.09.020. https://doi.org/10.1016/j.neuron.2012.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burstein SH, Zurier RB. Cannabinoids, endocannabinoids, and related analogs in inflammation. AAPS J. 2009;11:109–19. doi: 10.1208/s12248-009-9084-5. https://doi.org/10.1208/s12248-009-9084-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bisogno T, Ligresti A, Di Marzo V. The endocannabinoid signalling system: Biochemical aspects. Pharmacol Biochem Behav. 2005;81:224–38. doi: 10.1016/j.pbb.2005.01.027. https://doi.org/10.1016/j.pbb.2005.01.027. [DOI] [PubMed] [Google Scholar]
- 20.Wang J, Ueda N. Biology of endocannabinoid synthesis system. Prostaglandins Other Lipid Mediat. 2009;89:112–9. doi: 10.1016/j.prostaglandins.2008.12.002. https://doi.org/10.1016/j.prostaglandins.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 21.Ledent C, Valverde O, Cossu G, Petitet F, Aubert JF, Beslot F, et al. Unresponsiveness to cannabinoids and reduced addictive effects of opiates in CB1 receptor knockout mice. Science. 1999;283:401–4. doi: 10.1126/science.283.5400.401. https://doi.org/10.1126/science.283.5400.401. [DOI] [PubMed] [Google Scholar]
- 22.Martin WJ, Patrick SL, Coffin PO, Tsou K, Walker JM. An examination of the central sites of action of cannabinoid-induced antinociception in the rat. Life Sci. 1995;56:2103–9. doi: 10.1016/0024-3205(95)00195-c. https://doi.org/10.1016/0024-3205(95)00195-C. [DOI] [PubMed] [Google Scholar]
- 23.Lee MC, Ploner M, Wiech K, Bingel U, Wanigasekera V, Brooks J, et al. Amygdala activity contributes to the dissociative effect of cannabis on pain perception. Pain. 2013;154:124–34. doi: 10.1016/j.pain.2012.09.017. https://doi.org/10.1016/j.pain.2012.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pernia-Andrade AJ, Kato A, Witschi R, Nyilas R, Katona I, Freund TF, et al. Spinal endocannabinoids and CB1 receptors mediate C-fiber-induced heterosynaptic pain sensitization. Science. 2009;325:760–4. doi: 10.1126/science.1171870. https://doi.org/10.1126/science.1171870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ständer S, Schmelz M, Metze D, Luger T, Rukwied R. Distribution of cannabinoid receptor 1 (CB1) and 2 (CB2) on sensory nerve fibers and adnexal structures in human skin. J Dermatol Sci. 2005;38:177–88. doi: 10.1016/j.jdermsci.2005.01.007. https://doi.org/10.1016/j.jdermsci.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 26.Agarwal N, Pacher P, Tegeder I, Amaya F, Constantin CE, Brenner GJ, et al. Cannabinoids mediate analgesia largely via peripheral type 1 cannabinoid receptors in nociceptors. Nat Neurosci. 2007;10:870–9. doi: 10.1038/nn1916. https://doi.org/10.1038/nn1916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hanus L, Breuer A, Tchilibon S, Shiloah S, Goldenberg D, Horowitz M, et al. HU-308: a specific agonist for CB2, a peripheral cannabinoid receptor. Proc Natl Acad Sci. 1999;96:14228–33. doi: 10.1073/pnas.96.25.14228. https://doi.org/10.1073/pnas.96.25.14228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ibrahim MM, Deng H, Zvonok A, Cockayne DA, Kwan J, Mata HP, et al. Activation of CB2 cannabinoid receptors by AM1241 inhibits experimental neuropathic pain: pain inhibition by receptors not present in the CNS. Proc Natl Acad Sci U S A. 2003;100:10529–33. doi: 10.1073/pnas.1834309100. https://doi.org/10.1073/pnas.1834309100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wotherspoon G, Fox A, McIntyre P, Colley S, Bevan S, Winter J. Peripheral nerve injury induces cannabinoid receptor 2 protein expression in rat sensory neurons. Neurosci. 2005;135:235–45. doi: 10.1016/j.neuroscience.2005.06.009. https://doi.org/10.1016/j.neuroscience.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 30.Anand P, Whiteside G, Fowler CJ, Hohmann AG. Targeting CB2 receptors and the endocannabinoid system for the treatment of pain. Brain Res Rev. 2009;60:255–66. doi: 10.1016/j.brainresrev.2008.12.003. https://doi.org/10.1016/j.brainresrev.2008.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ibrahim MM, Porreca J, Lai J, Albrecht PJ, Rice FL, Khodorova A, et al. CB2 cannabinoid receptor activation produces antinociception by stimulating peripheral release of endogenous opioids. Proc Natl Acad Sci. 2005;102:3093–98. doi: 10.1073/pnas.0409888102. https://doi.org/10.1073/pnas.0409888102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Benarroch E. Endocannabinoids in basal ganglia circuits: implications for Parkinson disease. Neurology. 2007;69:306–9. doi: 10.1212/01.wnl.0000267407.79757.75. https://doi.org/10.1212/01.wnl.0000267407.79757.75. [DOI] [PubMed] [Google Scholar]
- 33.McDougall JJ. Arthritis and pain. Neurogenic origin of joint pain. Arthritis Res Ther. 2006;8:220. doi: 10.1186/ar2069. https://doi.org/10.1186/ar2069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hunter DJ, McDougall JJ, Keefe FJ. The symptoms of osteoarthritis and the genesis of pain. Med Clin North Am. 2009;93:83–100. doi: 10.1016/j.mcna.2008.08.008. https://doi.org/10.1016/j.mcna.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 35.Richardson D, Pearson RG, Kurian N, Latif ML, Garle MJ, Barrett DA, et al. Characterisation of the cannabinoid receptor system in synovial tissue and fluid in patients with osteoarthritis and rheumatoid arthritis. Arthritis Res Ther. 2008;10:43–57. doi: 10.1186/ar2401. https://doi.org/10.1186/ar2401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ware MA, Adams H, Guy GW. The medicinal use of cannabis in the UK: results of a nationwide survey. Int J Clin Pract. 2005;59:291–5. doi: 10.1111/j.1742-1241.2004.00271.x. https://doi.org/10.1111/j.1742-1241.2004.00271.x. [DOI] [PubMed] [Google Scholar]
- 37.California Medical Association. Physician Recommendation of Medical Cannabis. Guidelines of the Council on Scientific Affairs Subcommittee on Medical Marijuana Practice Advisory. 2011. available at http://www.mbc.ca.gov/Licensees/Prescribing/medical_marijuana_cma-recommend.pdf.
- 38.College of Family Physicians of Canada. Authorizing dried cannabis for chronic pain or anxiety: preliminary guidance from the college of family physicians of Canada. Mississauga, ON: College of Family Physicians of Canada; 2014. [Google Scholar]
- 39.Hawaii Department of Public Safety. Physician’s guideline&patient information for completing hawaii’s written certification/registry identification forms for the medical use of marijuana. available at http://dps.hawaii.gov/wp-content/uploads/2012/09/Physian-Information-Med-Marijuana-rev113011.pdf.
- 40.Romero-Sandoval A, Nutile-McMenemy N, De-Leo JA. Spinal microglia and perivascular cell cannabinoid receptor type 2 activation reduces behavioral hypersensitivity without tolerance after peripheral nerve injury. Anesthesiology. 2008;108:722–34. doi: 10.1097/ALN.0b013e318167af74. https://doi.org/10.1097/ALN.0b013e318167af74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.La Porta C, Bura SA, Aracil-Fernandez AM, Nanzanares J, Maldonado R. Role of CB1 and CB2 cannabinoid receptors in the development of joint pain induced by monosodium iodoacetate. Pain. 2013;154:160–74. doi: 10.1016/j.pain.2012.10.009. https://doi.org/10.1016/j.pain.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 42.Sagar DR, Staniaszek LE, Okine BN, Woodhams S, Norris LM, Pearson RG, et al. Tonic modulation of spinal hyperexcitability by the endocannabinoid receptor system in a rat model of osteoarthritis pain. Arthritis Rheum. 2010;62:3666–76. doi: 10.1002/art.27698. https://doi.org/10.1002/art.27698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Burston JJ, Sagar DR, Shao P, Bai M, King E, Brailsford L, et al. Cannabinoid CB2 receptors regulate central sensitization and pain responses associated with osteoarthritis of the knee joint. PloS One. 2013;8:e80440. doi: 10.1371/journal.pone.0080440. https://doi.org/10.1371/journal.pone.0080440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Murai M, Tsuji F, Nose M, Seki I, Oki K, Setoguchi C, et al. SA13353 (1-[2-(1-Adamantyl)ethyl]-1-pentyl-3-[3-(4-pyridyl)propyl]urea) inhibits TNF-alpha production through the activation of capsaicin-sensitive afferent neurons mediated via transient receptor potential vanilloid 1 in vivo. Eur J Pharmacol. 2008;588:309–15. doi: 10.1016/j.ejphar.2008.04.037. https://doi.org/10.1016/j.ejphar.2008.04.037. [DOI] [PubMed] [Google Scholar]
- 45.Colpaert FC, Donnerer J, Lembeck F. Effects of capsaicin on inflammation and on the substance P content of nervous tissues in rats with adjuvant arthritis. Life Sci. 1983;32:1827–34. doi: 10.1016/0024-3205(83)90060-7. https://doi.org/10.1016/0024-3205(83)90060-7. [DOI] [PubMed] [Google Scholar]
- 46.Szabo A, Helyes Z, Sandor K, Bite A, Pinter E, Nemeth J, et al. Role of transient receptor potential vanilloid 1 receptors in adjuvant-induced chronic arthritis: in vivo study using gene-deficient mice. J Pharmacol Exp Ther. 2005;314:111–9. doi: 10.1124/jpet.104.082487. https://doi.org/10.1124/jpet.104.082487. [DOI] [PubMed] [Google Scholar]
- 47.Yang Y, Yang H, Wang Z, Varadaraj K, Kumari SS, Mergler S, et al. Cannabinoid receptor 1 suppresses transient receptor potential vanilloid 1-induced inflammatory responses to corneal injury. Cell Signal. 2013;25:501–11. doi: 10.1016/j.cellsig.2012.10.015. https://doi.org/10.1016/j.cellsig.2012.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fernandes ES, Russell FA, Spina D, McDougall JJ, Graepel R, Gentry C, et al. A distinct role for transient receptor potential ankyrin 1, in addition to transient receptor potential vanilloid 1, in tumor necrosis factor α-induced inflammatory hyperalgesia and Freund’s complete adjuvant-induced monarthritis. Arthritis Rheum. 2011;63:819–29. doi: 10.1002/art.30150. https://doi.org/10.1002/art.30150. [DOI] [PubMed] [Google Scholar]
- 49.Ebbinghaus M, Uhlig B, Richter F, Segond von Banchet G, Gajda M, Bräuer R, et al. The role of interleukin-1β in arthritic pain: main involvement in thermal but not in mechanical hyperalgesia in rat antigen-induced arthritis. Ann Rheum Dis. 2012;71:253–61. doi: 10.1002/art.34675. https://doi.org/10.1136/ard.2011.150318. [DOI] [PubMed] [Google Scholar]
- 50.Ambrosino P, Soldovieri MV, Russo C, Taglialatela M. Activation and desensitization of TRPV1 channels in sensory neurons by the PPARalpha agonist palmitoylethanolamide. Br J Pharmacol. 2013;168:1430–44. doi: 10.1111/bph.12029. https://doi.org/10.1111/bph.12029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Redmond WJ, Gu L, Camo M, McIntyre P, Connor M. Ligand determinants of fatty acid activation of the pronociceptive ion channel TRPA1. PeerJ. 2014;2:e248. doi: 10.7717/peerj.248. https://doi.org/10.7717/peerj.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wang ZY, McDowell T, Wang P, Alvarez R, Gomez T, Bjorling DE. Activation of CB1 inhibits NGF-induced sensitization of TRPV1 in adult mouse afferent neurons. Neuroscience. 2014;277:679–89. doi: 10.1016/j.neuroscience.2014.07.041. https://doi.org/10.1016/j.neuroscience.2014.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Baker CL, McDougall JJ. The cannabinomimetic arachidonyl-2-chloroethylamide (ACEA) acts on capsaicin-sensitive TRPV1 receptors but not cannabinoid receptors in rat joints. Br J Pharmacol. 2004;142:1361–7. doi: 10.1038/sj.bjp.0705902. https://doi.org/10.1038/sj.bjp.0705902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Alawi M, Russell FA, Aubdool AA, Srivastava S, Riffo-Vasquez Y, Baldissera L, et al. Transient receptor potential canonical 5 (TRPC5) protects against pain and vascular inflammation in arthritis and joint inflammation. Ann Rheum Dis. 2017;76:252–60. doi: 10.1136/annrheumdis-2015-208886. https://doi.org/10.1136/annrheumdis-2015-208886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chiurchi V, Battistini L, Maccarrone M. Endocannabinoid signalling in innate and adaptive immunity. Immunology. 2015;144:352–64. doi: 10.1111/imm.12441. https://doi.org/10.1111/imm.12441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Maccarrone M, Bab I, Bíró T, Cabral GA, Dey SK, Di Marzo V, et al. Endocannabinoid signaling at the periphery: 50 years after THC. Trends Pharmacol Sci. 2015;36:277–96. doi: 10.1016/j.tips.2015.02.008. https://doi.org/10.1016/j.tips.2015.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Katchan V, David P, Shoenfeld Y. Cannabinoids and autoimmune diseases: A systematic review. Autoimmunity Rev. 2016;15:513–28. doi: 10.1016/j.autrev.2016.02.008. https://doi.org/10.1016/j.autrev.2016.02.008. [DOI] [PubMed] [Google Scholar]
- 58.Rubin V, Hui-Lin L. Cannabis and Culture. In: Rubin V, editor. Mouton; The Hague: 1975. pp. 51–62. https://doi.org/10.1515/9783110812060. [Google Scholar]
- 59.Kidd BL, Urban LA. Mechanisms of inflammatory pain. Br J Anaesth. 2001;87:3–11. doi: 10.1093/bja/87.1.3. https://doi.org/10.1093/bja/87.1.3. [DOI] [PubMed] [Google Scholar]
- 60.Sancho R, Calzado MA, Di Marzo V, Appendino G, Mu-oz E. Anandamide inhibits nuclear factor-kappaB activation through a cannabinoid receptor-independent pathway. Mol Pharmacol. 2003;63:429–38. doi: 10.1124/mol.63.2.429. https://doi.org/10.1124/mol.63.2.429. [DOI] [PubMed] [Google Scholar]
- 61.Malfait A, Sumariwalla P, Malik A, Andreakos E, Mechoulam R, Feldmann M. The nonpsychoactive cannabis constituent cannabidiol is an oral anti-arthritic therapeutic in murine collagen-induced arthritis. Proc Natl Acad Sci. 2000;97:9561–6. doi: 10.1073/pnas.160105897. https://doi.org/10.1073/pnas.160105897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kinsey SG, Mahadevan A, Zhao B, Sun H, Naidu PS, Razdan RK, et al. The CB2 cannabinoid receptor-selective agonist O-3223 reduces pain and inflammation without apparent cannabinoid behavioral effects. Neuropharmacology. 2011;60:244–51. doi: 10.1016/j.neuropharm.2010.09.004. https://doi.org/10.1016/j.neuropharm.2010.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fukuda S, Kohsaka H, Takayasu A, Yokoyama W, Miyabe C, Miyabe Y, et al. Cannabinoid receptor 2 as a potential therapeutic target in rheumatoid arthritis. BMC Musculoskelet Disord. 2014;15:275. doi: 10.1186/1471-2474-15-275. https://doi.org/10.1186/1471-2474-15-275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Krustev E, Reid A, McDougall JJ. Tapping into the endocannabinoid system to ameliorate acute inflammatory flares and associated pain in mouse knee joints. Arthritis Res Ther. 2014;16:437. doi: 10.1186/s13075-014-0437-9. https://doi.org/10.1186/s13075-014-0437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bánvölgyi A, Pozsgai G, Brain SD, Helyes ZS, Szolcsányi J, Ghosh M, et al. Mustard oil induces a transient receptor potential vanilloid 1 receptor-independent neurogenic inflammation and a non-neurogenic cellular inflammatory component in mice. Neuroscience. 2004;125:449–59. doi: 10.1016/j.neuroscience.2004.01.009. https://doi.org/10.1016/j.neuroscience.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 66.Heppelmann B, Pawlwak M. Sensitisation of articular afferents in normal and inflamed knee joints by substance P in the rat. Neurosci Lett. 1997;223:97–100. doi: 10.1016/s0304-3940(97)13408-5. https://doi.org/10.1016/S0304-3940(97)13408-5. [DOI] [PubMed] [Google Scholar]
- 67.Raychaudhuri SP, Raychaudhuri SK, Atkuri KR, Herzenberg LA, Herzenberg LA. Nerve growth factor: a key local regulator in the pathogenesis of inflammatory arthritis. Arthritis Rheum. 2011;63:3243–52. doi: 10.1002/art.30564. https://doi.org/10.1002/art.30564. [DOI] [PubMed] [Google Scholar]
- 68.Fassold A, Falk W, Anders S, Hirsch T, Mirsky VM, Straub Soluble RH. Neuropilin-2, a nerve repellent receptor, is increased in rheumatoid arthritis synovium and aggravates sympathetic fiber repulsion and arthritis. Arthr Rheum. 2009;60:2892–901. doi: 10.1002/art.24860. https://doi.org/10.1002/art.24860. [DOI] [PubMed] [Google Scholar]
- 69.Härle P, Pongratz G, Albrecht J, Tarner IH, Straub RH. An early sympathetic nervous system influence exacerbates collagen-induced arthritis via CD4 + CD25+ cells. Arthritis Rheum. 2008;58:2347–55. doi: 10.1002/art.23628. https://doi.org/10.1002/art.23628. [DOI] [PubMed] [Google Scholar]
- 70.Pongratz G, Straub RH. Role of peripheral nerve fibres in acute and chronic inflammation in arthritis. Nat Rev Rheumatol. 2013;9:117–26. doi: 10.1038/nrrheum.2012.181. https://doi.org/10.1038/nrrheum.2012.181. [DOI] [PubMed] [Google Scholar]
- 71.Russell FA, Fernandes ES, Courade JP, Keeble JE, Brain SD. Tumour necrosis factor alpha mediates transient receptor potential vanilloid 1-dependent bilateral thermal hyperalgesia with distinct peripheral roles of interleukin-1beta, protein kinase C and cyclooxygenase-2 signalling. Pain. 2009;142:264–74. doi: 10.1016/j.pain.2009.01.021. https://doi.org/10.1016/j.pain.2009.01.021. [DOI] [PubMed] [Google Scholar]
- 72.Mnich SJ, Hiebsch RR, Huff RM, Muthian S. Anti-inflammatory properties of CB1-receptor antagonist involves beta2 adrenoceptors. J Pharmacol Exp Ther. 2010;333:445–53. doi: 10.1124/jpet.109.163998. https://doi.org/10.1124/jpet.109.163998. [DOI] [PubMed] [Google Scholar]
- 73.Takahashi HK, Mori S, Liu K, Wake H, Zhang J, Liu R, et al. Beta2-adrenoceptor stimulation inhibits advanced glycation end products-induced adhesion molecule expression and cytokine production in human peripheral blood mononuclear cells. Eur J Pharmacol. 2010;627:313–7. doi: 10.1016/j.ejphar.2009.10.034. https://doi.org/10.1016/j.ejphar.2009.10.034. [DOI] [PubMed] [Google Scholar]
- 74.Jin K, Xie L, Kim SH, Parmentier-Batteur S, Sun Y, Mao XO, et al. Defective adult neurogenesis in CB1 cannabinoid receptor knockout mice. Mol Pharmacol. 2004;66:204–8. doi: 10.1124/mol.66.2.204. https://doi.org/10.1124/mol.66.2.204. [DOI] [PubMed] [Google Scholar]
- 75.Chavan SS, Tracey KJ. Regulating innate immunity with dopamine and electroacupuncture. Nat Med. 2014;20:239–41. doi: 10.1038/nm.3501. https://doi.org/10.1038/nm.3501. [DOI] [PubMed] [Google Scholar]
- 76.Torres-Rosas R, Yehia G, Pena G, Mishra P, del Rocio Thompson-Bonilla M, Moreno-Eutimio MA, et al. Dopamine mediates vagal modulation of the immune system by electroacupuncture. Nat Med. 2014;20:291–5. doi: 10.1038/nm.3479. https://doi.org/10.1038/nm.3479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Blake DR, Robson P, Ho M, Jubb RW, McCabe CS. Preliminary assessment of the efficacy, tolerability and safety of a cannabis-based medicine (Sativex) in the treatment of pain caused by rheumatoid arthritis. Rheum. 2006;45:50–52. doi: 10.1093/rheumatology/kei183. https://doi.org/10.1093/rheumatology/kei183. [DOI] [PubMed] [Google Scholar]
- 78.Ware MA, Fitzcharles MA, Joseph L, Shir Y. The effects of nabilone on sleep in fibromyalgia: results of a randomized controlled trial. Anesth Analg. 2010;110:604–10. doi: 10.1213/ANE.0b013e3181c76f70. https://doi.org/10.1213/ANE.0b013e3181c76f70. [DOI] [PubMed] [Google Scholar]
- 79.Huggins JP, Smart TS, Langman S, Taylor L, Young T. An efficient randomised, placebo-controlled clinical trial with the irreversible fatty acid amide hydrolase-1 inhibitor PF-04457845, which modulates endocannabinoids but fails to induce effective analgesia in patients with pain due to osteoarthritis of the knee. Pain. 2012;153:1837–46. doi: 10.1016/j.pain.2012.04.020. https://doi.org/10.1016/j.pain.2012.04.020. [DOI] [PubMed] [Google Scholar]
- 80.Piscitelli F, Di Marzo V. “Redundancy” of endocannabinoid inactivation: new challenges and opportunities for pain control”. ACS Chem Neurosci. 2012;3:356–63. doi: 10.1021/cn300015x. https://doi.org/10.1021/cn300015x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Alhouayek M, Masquelier J, Cani PD, Lambert DM, Muccioli GG. Implication of the anti-inflammatory bioactive lipid prostaglandin D2-glycerol ester in the control of macrophage activation and inflammation by ABHD6. Proc Natl Acad Sci U S A. 2013;110:17558–63. doi: 10.1073/pnas.1314017110. https://doi.org/10.1073/pnas.1314017110. [DOI] [PMC free article] [PubMed] [Google Scholar]