Abstract
Objective
To determine the proportion of patients receiving statins for primary or secondary prevention of cardiovascular disease (CVD), as well as to describe lipid-screening trends.
Design
Retrospective chart review using the Manitoba Primary Care Research Network repository.
Setting
Manitoba.
Participants
A total of 149 262 patients.
Main outcome measures
Proportion of patients who were taking statins for primary or secondary prevention of cardiovascular disease (CVD), who did not have evidence of CVD recorded in their charts, and who underwent lipid screening; distribution of statins among age groups; and the proportion of patients eligible for lipid screening when the age cutoffs of the 2012 and 2016 Canadian Cardiovascular Society guidelines were applied.
Results
Of the 149 262 patients, 139 025 (93%) did not have CVD recorded in their electronic medical records and made up the primary prevention group; of these 139 025 patients, 5955 (4%) were taking statins. Also in the primary prevention group, 14 814 (11%) patients were 75 years of age and older; of these patients, 1374 (9%) were taking statins. A total of 10 237 of the 149 262 (7%) patients had CVD recorded in their charts (secondary prevention group); 3013 (29%) of these patients were taking statins. When the 2016 Canadian Cardiovascular Society guidelines age cutoffs were applied, 56% of patients (83 119 of 149 262) were eligible for lipid screening, and 31% (26 024 of 83 119) of them had evidence of screening in the past 5 years. Of the total population of those aged 75 and older, 28% (5597 of 20 188) had undergone lipid screening. Of the total population taking statins, 28% (2481 of 8968) had undergone lipid testing while taking statins.
Conclusion
In Manitoba, less than 5% of the primary prevention population and less than 30% of the secondary prevention population had received repeat statin prescriptions from their primary care providers. This represents a possible practice gap that warrants future research, as statins offer considerable morbidity and mortality benefits in these patients.
Résumé
Objectif
Déterminer la proportion des patients qui prennent des statines en prévention primaire ou secondaire des maladies cardiovasculaires (MCV) et décrire les tendances actuelles relatives au dosage des lipides sanguins.
Type d’étude
Revue rétrospective à l’aide des dossiers du Réseau de recherche en santé primaire du Manitoba.
Contexte
Le Manitoba.
Participants
Un total de 149 262 patients.
Principaux paramètres à l’étude
La proportion des patients qui reçoivent des statines en prévention primaire ou secondaire des MCV et dont les dossiers ne mentionnent pas de MCV, et de ceux qui ont eu un dosage des lipides sanguins; la distribution des groupes d’âge chez les patients qui prennent des statines; et la proportion des patients admissibles au dosage des lipides selon les directives émises en 2012 et en 2016 par la Société canadienne de cardiologie.
Résultats
Sur les 149 262 patients, 139 025 (93 %) n’avaient aucune mention de MCV dans leurs dossiers électroniques : ils constituent le groupe en prévention primaire. Dans ce dernier groupe, 5955 (4 %) prenaient des statines. Également dans ce groupe, 14 814 patients (11 %) avaient 75 ans ou plus et 1374 (9 %) de ces derniers prenaient des statines. Sur les 149 262 patients, 10 237 (7 %) avaient une mention de MCV dans leur dossier (le groupe en prévention secondaire); de ce groupe, 3013 (29 %) prenaient des statines. Selon les directives émises en 2016 par la Société canadienne de cardiologie, 56 % des patients (83 119 sur 149 262) auraient pu avoir un dosage des lipides et 31 % (26 024 sur 83 119) avaient des preuves d’un tel dosage au cours des 5 dernière années. Sur l’ensemble des patients de 75 ans et plus, 28 % (5597 sur 20 188) avaient eu un dosage des lipides. Parmi tous les patients qui prenaient des statines, 28 % (2481 sur 8968) avaient eu un dosage des lipides pendant qu’ils prenaient des statines.
Conclusion
Au Manitoba, moins de 5 % des patients en prévention primaire et moins de 30 % de ceux en prévention secondaire avaient eu des prescriptions répétées de statines de la part de leur principal soignant de première ligne. Ce faible taux de prescription mériterait probablement une étude additionnelle étant donné que les statines confèrent aux patients une protection appréciable sur le plan de la morbidité et de la mortalité.
Canadians spend more money each year on statins than any other drug with the exception of anti–tumor necrosis factor inhibitors.1 The 2012 Canadian Cardiovascular Society (CCS) guidelines recommend lipid screening in men between the ages of 40 and 75 and in women between the ages 50 and 75 every 1 to 5 years; and the 2016 CCS guidelines recommend screening for everyone between the ages of 40 and 75.2,3 The 2012 and 2016 CCS guidelines recommend that a Framingham risk score (FRS) be calculated for all primary prevention patients to determine their eligibility for statin therapy, and that all secondary prevention patients (those with clinical evidence of atherosclerosis) be started on statins regardless of score.2,3 The FRS is used to calculate each individual’s 10-year risk of cardiovascular disease (CVD).2,3 Statin therapy is recommended for those with a risk score of 20% or higher, as per both guidelines, should be considered in those with an intermediate risk of 10% to 20%, and for those outside of specific lipid targets depending on other factors such as diabetes or current smoking status.2,3
Cardiovascular disease is the leading cause of death in North America, accounting for 27% of deaths in Canada, and statins have shown a relative risk reduction for major vascular events (ie, myocardial infarction, stroke, or coronary revascularization) of approximately 25% regardless of age, sex, baseline low-density lipoprotein (LDL) cholesterol levels, or previous vascular disease.4–9
The use of statins in secondary prevention heralds a relative risk reduction in all-cause mortality of 12% to 16%, which has not been demonstrated in the primary prevention population.10,11 However, there still exists a considerable relative risk reduction for cardiovascular morbidity in these patients.6,12–14 Moderate- and high-risk primary prevention patients make up a substantial proportion of the disease burden, with many patients dying from their initial cardiovascular event.14–16 Thus, much of the research on statin prescribing has focused on primary prevention in an effort to prevent the development of CVD in those who have not yet been diagnosed.2,3,14 Because the incidence of CVD is so high in the primary care population, statin intervention even in low-risk populations should result in considerable CVD reductions.14
There has been a trend toward becoming more liberal with statin prescribing for primary prevention of CVD during the past decade. In the United States, for example, the 2013 American Heart Association and the American College of Cardiology guidelines for the treatment of cholesterol now advocate for consideration of statin therapy in individuals who have a 10-year risk of CVD that is 7.5% or higher, which is lower than the 10% cutoff quoted in the 2001 and 2004 guidelines published by the National Heart, Lung, and Blood Institute.17–19 Similarly, in Canada, guideline changes in the 2012 CCS guidelines resulted in a 2- to 3-fold increase in the number of patients receiving statin therapy compared with the 2006 recommendations, with approximately one-third of the primary prevention population now being eligible for statins.20–22 The more recent 2016 CCS guidelines3 recommend statin prescribing regardless of lipid levels in all patients with abdominal aortic aneurysms, those with chronic kidney disease, and those with diabetes mellitus who are 40 years of age or older, whereas the 2012 guidelines recommended just earlier screening in these groups.22
The counterargument to statin prescribing in primary prevention is that it promotes overmedicalization of otherwise healthy patients.23,24 Whereas modest decreases in CVD risk are considerable on a population scale, they might not be so on an individual basis, and therefore the benefits should be weighed against the risks.25,26 Commonly reported adverse effects related to statins include increased risk of diabetes, myopathy, elevated liver enzymes, cataracts, fatigue, and decreased sexual function.27–31 Statins are costly, ranging from $12 to $50 per month.32 However, the adverse effect rates for statins are small and are lower than those for acetylsalicylic acid, another medication used for primary prevention of CVD.31,33 In some studies, statins have adverse effect rates similar to placebo.31,33
Despite the ample discussion regarding the efficacy of statins in primary prevention, there is a paucity of data regarding the prevalence of statin prescribing in this population. We sought to better clarify the breakdown of statin prescribing for primary and secondary prevention of CVD in a large primary care sample. We also aimed to describe lipid-screening trends and adherence to the 2016 CCS guidelines among primary care practitioners. To our knowledge no similar studies have been performed in North America to date.
METHODS
A retrospective chart review was completed using the Manitoba Primary Care Research Network (MaPCReN) repository. The MaPCReN is part of the Canadian Primary Care Sentinel Surveillance Network (CPCSSN), the largest multisystem database in Canada that collects and processes de-identified information derived from electronic medical records (EMRs) from consenting primary care practices.
All patients who had at least 1 visit with a primary care provider captured in the MaPCReN repository within a 5-year period from July 1, 2010, to June 30, 2015, were included in the study. Patients with no recorded birth date or sex, and any patients younger than 20 years of age or older than 100, were excluded.
All medications within the CPCSSN database are assigned an ATC (Anatomic Therapeutic Chemical) code derived either from the EMR or assigned by an algorithm based on the medication name. We queried the medication table that captures prescription records by employing the ATC code C10AA (HMG-CoA [β-hydroxy-β-methylglutarylcoenzyme A] reductase inhibitors or statins). To eliminate those who were prescribed statins in error or who never initiated their medication, we included only those who had at least 1 refill prescription in their EMR.
In order to determine whether patients were taking statins for primary or secondary prevention of CVD, ICD-9 (International Classification of Diseases) diagnosis codes used for billing and health conditions (problem list or cumulative patient profile diagnoses) were searched for evidence of CVD. We defined CVD as any diagnoses related to atherosclerosis in the form of cerebrovascular, cardiovascular, aortic, or peripheral vascular disease. For a full list of ICD-9 codes queried, please contact the corresponding author. Patients who had 1 or more of the ICD-9 codes listed in their charts on 1 or more occasions were considered to have a past medical history of CVD and thus were considered as secondary prevention patients in this study.
Adherence to the CCS guidelines was determined by considering how many patients had evidence of lipid screening within and outside of the age-screening recommendations (the age ranges in the 2012 CCS guidelines were ages 40 to 75 for men and ages 50 to 75 for women; the 2016 CCS guidelines included everyone aged 40 to 75). Laboratory results were queried for all records in laboratory tables containing LDL or cholesterol.
Ethics approval was obtained from the Health Research Ethics Board of the University of Manitoba in Winnipeg before commencing the study, as was application for data access usage from the MaPCReN. All data collected were de-identified based on CPCSSN protocols and stored on a secure computer on the Bannatyne campus at the University of Manitoba, which was securely connected to the High Performance Computing Virtual Laboratory at Queen’s University in Kingston, Ont. Data were analyzed using Microsoft Excel.
RESULTS
Study sample
The MaPCReN repository contained 149 262 records from primary care practices in Manitoba that met our inclusion criteria between the years 2010 and 2015.
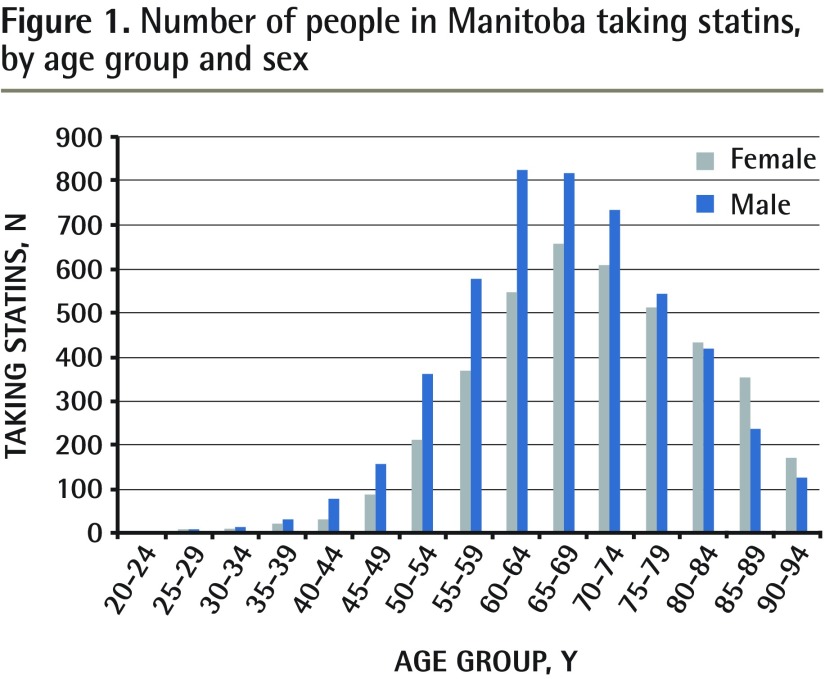
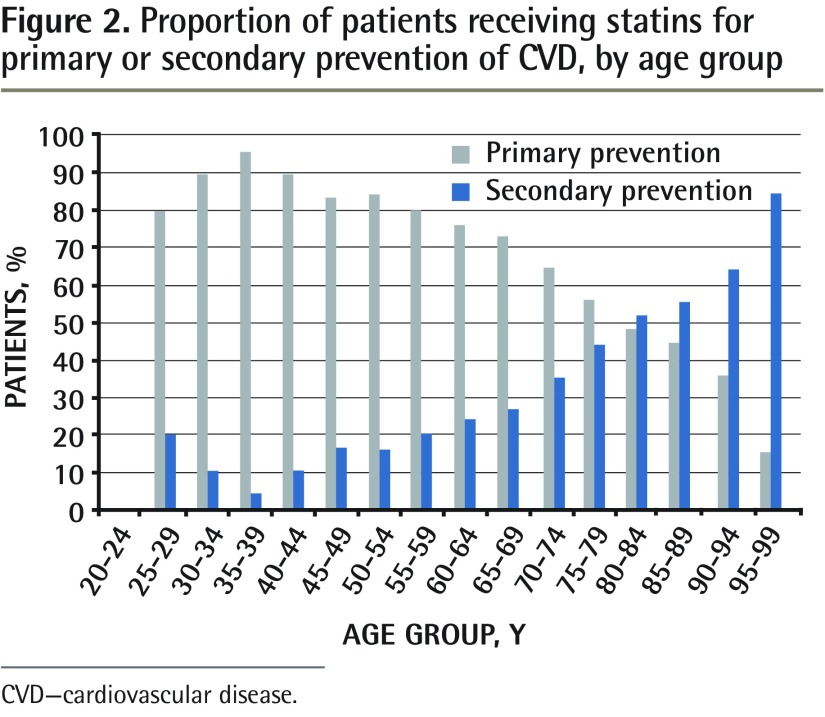
Of these, 44% were men and 56% were women. The mean (SD) age was 51.6 (19.3) years for all enrolled patients; 49.9 (18.5) years for patients eligible for primary prevention; and 74.2 (14.0) years for those eligible for secondary prevention. The mean (SD) age of patients taking statins was 68.8 (11.9) years and 50.5 (19.1) years for those not taking statins. Table 1 presents the statin use and lipid-screening characteristics of the study sample for the primary and secondary prevention groups.3 Figure 1 shows the number of those in the study sample taking statins, by age group and sex. Figure 2 presents the proportion of patients receiving statins for primary and secondary prevention of CVD, by age group.
Table 1.
Characteristics of the total patient sample (N = 149 262 [n = 65 620 men; n = 83 642 women]): A) Primary prevention group; B) secondary prevention group.
| A) CHARACTERISTICS | PRIMARY PREVENTION GROUP* | ||
|---|---|---|---|
|
| |||
| TOTAL NO. OF PATIENTS (N = 139 025), N (%) | MALE (N = 60 013), N (%) | FEMALE (N = 79 012), N (%) | |
| Taking statins | 5955 (4) | 3111 (5) | 2844 (4) |
| Not taking statins | 133 070 (96) | 56 902 (95) | 76 168 (96) |
| Age ≥ 75 y | 14 814 (11) | 6120 (10) | 8694 (11) |
| Taking statins and aged ≥ 75 y | 1374 (1) | 577 (1) | 797 (1) |
| Lipid testing in past 5 y | 32 950 (24) | 14 155 (24) | 18 435 (23) |
| Lipid testing inside age ranges | 23 736 (17) | 10 461 (17) | 13 275 (17) |
| Lipid testing and ≥ 75 y | 3528 (3) | 1299 (2) | 2229 (3) |
| Lipid testing while taking statins | 1596 (1) | 813 (1) | 756 (0) |
| B) CHARACTERISTICS | SECONDARY PREVENTION GROUP* | ||
|---|---|---|---|
|
| |||
| TOTAL NO. OF PATIENTS (N = 10 237), N (%) | MALE (N = 5607), N (%) | FEMALE (N = 4630), N (%) | |
| Taking statins | 3013 (29) | 1832 (32) | 1181 (26) |
| Not taking statins | 7224 (71) | 3775 (67) | 3449 (75) |
| Age ≥ 75 y | 5374 (52) | 2547 (45) | 2827 (61) |
| Taking statins and aged ≥ 75 y | 1472 (14) | 775 (14) | 697 (15) |
| Lipid testing in past 5 y | 4387 (43) | 2534 (45) | 1853 (40) |
| Lipid testing inside age ranges | 2288 (22) | 1477 (26) | 811 (18) |
| Lipid testing and aged ≥ 75 y | 2069 (20) | 1041 (19) | 1028 (22) |
| Lipid testing while taking statins | 911 (9) | 561 (10) | 350 (7) |
The 2016 Canadian Cardiovascular Society guidelines3 were followed for age cutoffs.
Figure 1.
Number of people in Manitoba taking statins, by age group and sex
Figure 2.
Proportion of patients receiving statins for primary or secondary prevention of CVD, by age group
CVD—cardiovascular disease.
Primary prevention
A total of 139 025 of 149 262 (93%) patients had no evidence of CVD recorded in their charts and thus were included in the primary prevention group. Of these patients, 5955 (4%) were taking statins.
A total of 14 814 (11%) patients in the primary prevention group were aged 75 and older and 1374 (9%) of them were taking statins. We were unable to determine whether these patients received new or refilled statin prescriptions.
Table 2 shows statin use according to age groups. There is a trend toward more elderly patients receiving statin therapy for primary prevention; this is demonstrated by the 70-to-74 and 75-to-79 age groups, which comprise the highest amount of statin use for primary prevention (13% in both groups).
Table 2.
Proportion of patients in the primary and secondary prevention groups taking statins and undergoing lipid testing, by age group
| AGE GROUP | PRIMARY PREVENTION GROUP | SECONDARY PREVENTION GROUP | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| TOTAL NO. OF PATIENTS | NO. TAKING STATINS (%) | NO. UNDERGOING LIPID TESTING (%) | TOTAL NO. OF PATIENTS | NO. TAKING STATINS (%) | NO. UNDERGOING LIPID TESTING (%) | |
| 20–24 | 11 654 | 0 (0) | 903 (8) | 25 | 0 (0) | 2 (8) |
| 25–29 | 11 530 | 4 (0) | 1165 (10) | 33 | 1 (3) | 4 (12) |
| 30–34 | 11 271 | 17 (0) | 1399 (12) | 54 | 2 (4) | 21 (39) |
| 35–39 | 11 341 | 45 (0) | 1859 (16) | 47 | 2 (4) | 3 (6.4) |
| 40–44 | 11 813 | 94 (1) | 2519 (21) | 111 | 11 (10) | 49 (44) |
| 45–49 | 12 420 | 200 (2) | 3135 (25) | 195 | 40 (21) | 97 (50) |
| 50–54 | 13 792 | 479 (4) | 4315 (31) | 398 | 90 (23) | 197 (50) |
| 55–59 | 12 961 | 752 (6) | 4358 (34) | 627 | 193 (31) | 316 (50) |
| 60–64 | 11 465 | 1042 (9) | 3897 (34) | 959 | 329 (34) | 475 (50) |
| 65–69 | 9510 | 1078 (11) | 3246 (34) | 1177 | 399 (34) | 569 (48) |
| 70–74 | 6454 | 870 (13) | 2266 (35) | 1237 | 474 (38) | 585 (47) |
| 75–79 | 4612 | 590 (13) | 1509 (33) | 1264 | 464 (37) | 608 (48) |
| 80–84 | 3767 | 408 (11) | 1046 (28) | 1359 | 440 (32) | 610 (45) |
| 85–89 | 3024 | 261 (9) | 632 (21) | 1279 | 325 (25) | 468 (37) |
| 90–94 | 2157 | 105 (5) | 255 (12) | 1036 | 188 (18) | 288 (28) |
| 95–99 | 1254 | 10 (1) | 86 (7) | 436 | 55 (13) | 95 (22) |
Secondary prevention
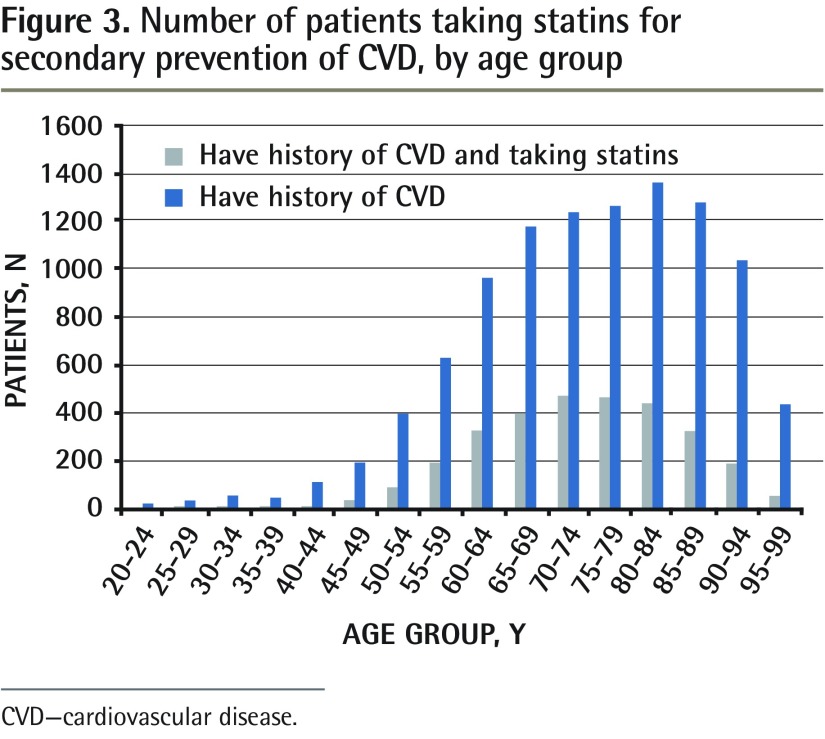
A total of 10 237 of 149 262 (7%) patients had a history of CVD recorded in their charts; of these patients, 3013 (29%) were taking statins. More than half of those (52%) in the secondary prevention group were aged 75 and older; of these 5374 patients, 1472 (27%) were taking statins (Table 1). Within the secondary prevention group, there was once again a trend toward increased statin prescribing in older age groups, with the 70-to-74 and 75-to-79 age groups having the highest percentages of statin use (38% and 37%, respectively) (Table 2). Figure 3 shows the number of patients taking statins for secondary prevention of CVD by age group.
Figure 3.
Number of patients taking statins for secondary prevention of CVD, by age group
CVD—cardiovascular disease.
Lipid screening
Patients in the secondary prevention group (ie, with a history of CVD) were more likely to have undergone lipid testing within the past 5 years than those in the primary prevention group (ie, without a history of CVD) were. In the secondary prevention group, 43% (4387 of 10 237) of patients had undergone lipid testing compared with 24% (32 950 of 139 025) in the primary prevention group.
A substantial proportion of patients aged 75 and older had undergone lipid testing. A total of 20 188 of 149 262 (14%) patients were aged 75 and older, and 5597 (28%) of them had had lipid testing in the past 5 years. Patients aged 75 years and older in the secondary prevention group were more likely to have had lipid testing done than those aged 75 years and older in the primary prevention group were (39% vs 24%, respectively).
For those patients taking statins, similar proportions in the secondary and primary prevention groups underwent lipid testing (30% [911 of 3013] vs 27% [1596 of 5955], respectively).
When the different age cutoffs of the 2012 and 2016 CCS guidelines were applied to the total sample, there was a 10% increase in the number of patients eligible for screening (Table 3). When the age cutoffs of the 2012 CCS guidelines were applied (ages 40 to 75 for men and ages 50 to 75 for women), 46% of patients (69 212 of 149 262) were eligible for screening compared with 56% (83 119 of 149 262) when the 2016 guidelines were applied (everyone aged 40 to 75). Figure 4 presents the total number of patients who were eligible for lipid screening and those who had evidence of receiving screening in the past 5 years using the age cutoffs in the 2016 CCS guidelines.
Table 3.
Comparison of the lipid-screening trends when the differing age cutoffs between the 2012 CCS guidelines and the 2016 CCS guidelines are applied: Eligibility for screening was based on age cutoffs alone.
| SAMPLE SIZE AND SCREENING TRENDS | USING 2012 CCS GUIDELINE CUTOFFS | USING 2016 CCS GUIDELINE CUTOFFS |
|---|---|---|
| Study sample, N | 149 262 | 149 262 |
| Eligible for screening, n (%) | 69 212 (46) | 83 119 (56) |
| Screening inside age ranges, n (%) | 22 783 (33) | 26 024 (31) |
| Screening outside age ranges, n (%) | 14 194 (18)* | 10 997 (17)† |
CCS—Canadian Cardiovascular Society.
The total number of patients outside the recommended age range was 80 050.
The total number of patients outside the recommended age range was 66 143.
Figure 4.
Number of patients who were eligible for lipid screening and those who had screening in the past 5 years, using the age cutoffs in the 2016 CCS guidelines
CCS—Canadian Cardiovascular Society.
Applying these age cutoffs resulted in a small decrease in the number of patients who had undergone screening (ie, had LDL levels recorded in their charts) within the recommended age ranges when comparing the 2012 and 2016 guidelines (33% vs 31%, respectively) (Table 3).
DISCUSSION
Our data suggest that less than 5% of the population that is eligible for primary prevention of CVD with statins is receiving repeat statin prescriptions from their primary care providers. Unfortunately, these data do not provide information regarding individual FRS results to help us determine what proportion of high- and intermediate-risk patients are receiving statin therapy, and therefore we cannot comment on whether high-risk patients who are eligible for primary prevention are left untreated. However, previous research has estimated that high-risk primary prevention patients (those with an FRS of ≥ 20%) comprise 5% to 26% of the population, and we found the total prescribing rate of statin use in primary prevention to be 4%.34,35 Our findings are lower than research in other jurisdictions, which found a statin-prescribing rate of 6.3% in primary prevention.36 These data bring to attention a possible practice gap that requires further exploration, as statin prescribing in this population has shown statistically significant reductions in cardiovascular morbidity.12,37,38
We found that 29% of patients with a history of CVD (ie, secondary prevention group) received repeat prescriptions from their family doctors in Manitoba, where the 2012 and 2016 CCS guidelines would advocate that all of these patients be taking statins.2,3 These data are in keeping with those reported in the literature, which describe rates ranging from 20% to 50%.39–45 If these patients are not receiving their prescriptions elsewhere (such as from their cardiologists), these figures might identify another important practice gap that emphasizes the need for further efforts to promote statin prescribing in secondary prevention, because according to the 2012 and 2016 CCS guidelines, 100% of these patients should be taking statins, as this is the population in which statins effect the most benefit.2,3,46,47
The evidence for statin use for primary prevention in patients aged 75 and older is particularly weak.48–50 We found that 9% of patients aged 75 and older in the primary prevention group were taking statins. Evidence for whether or not to stop taking statins in primary prevention once a patient has turned the age of 75 is lacking.51 It would have been useful to know what proportion of patients aged 75 and older received new prescriptions versus refills, but unfortunately our data do not provide this information. Given that elderly populations are typically at greater risk of morbidity and mortality due to polypharmacy, further research in this population is warranted.52
The 2016 CCS guidelines recommend lipid screening at minimum every 1 to 5 years. In our sample, 31% of patients within the recommended age ranges for screening were screened by their primary care providers in the past 5 years. We did not include the number of visits for each patient, and thus it is possible that a large proportion of this could be explained by lack of consistent patient-provider relationships.
There is little evidence to support routine lipid screening in patients aged 75 and older or for those already taking statins. Yet, 28% of patients aged 75 and older had evidence of screening in this study. Similarly, of patients already taking statins, 28% had lipid screening despite taking statins. It is possible that for some of these instances screening might have been ordered for alternate reasons, which the data do not tell us. However, it is also possible that some of these tests might be unnecessary according to the simplified lipid guidelines published by Allan et al.53 Eliminating this excess could help to reduce health care costs without affecting patient outcomes.
We used the CCS guidelines for this study instead of the primary care guidelines recently published by Allan et al because the CCS guidelines were the standard for the time period when most of this study was conducted (through the past 5 years). However, the simplified lipid guidelines warrant mention here, as they are written by family physicians and are better focused on primary care.53
To determine whether our results were representative of all Manitobans and Canadians, we were able to compare some of our findings with published provincial and national data that report the prevalence of CVD and statin prescribing. The 7% of patients in this sample with CVD is consistent with that reported by the 2013 Manitoba Centre for Health Policy study (7.9%) and Statistics Canada in 2009 (5.9%).8,54 However, the proportion of those taking statins in our sample is lower than that reported by Statistics Canada in 2016 (6% vs 10%, respectively).55 This discrepancy could be explained by the fact that we could not capture prescriptions written by other specialists, and that the Statistics Canada study used a more liberal definition of statin use than we did (only 1 prescription on file vs evidence of a refill).55 The CPCSSN database has previously been criticized for not employing enough nonacademic practices and community clinics, and its generalizability to the Canadian population is an area that warrants further study.56
Limitations
As with any retrospective study that uses primary care EMR data, there are weaknesses that are inherent to this approach. These data are less comprehensive than administrative or hospital data, and therefore care provided by specialists (such as cardiologists), or while admitted as an inpatient, might not be captured in this data set.57
In our study history of CVD was based on a single recording in the chart and this has unknown reliability. It is possible that some or many of these recordings were made in error or were misdiagnoses, or that a substantial proportion of patients with CVD did not have their conditions properly recorded in their EMRs. Unfortunately, with this study methodology, there is little else to rely upon to try and identify patients eligible for secondary prevention. Research to determine the accuracy and reliability of EMR data is ongoing, and this also speaks to the need for physicians employing EMRs in their practices to use stringent recording practices.
Primary prevention was considered the default condition in this study. If none of the ICD-9 billing codes we used were found in billing, problem lists, or cumulative patient profiles, patients in this study were automatically presumed to be eligible for the primary prevention group. Therefore, it is possible that there is some degree of overreporting of the primary prevention population in our data and, subsequently, underreporting of the secondary prevention population.
However, this might in part have been balanced by using a very broad definition of CVD, which might have led to overcapturing of the secondary prevention population. Although the evidence for statins in some of the conditions we employed as part of our definition of CVD might be weaker than in others (eg, heart failure or valvulopathies), we chose to emphasize capturing as many patients with CVD as possible, assuming that if a patient had evidence of one of these conditions, there was a high likelihood that they had others that might not have been documented.
It is likely that we have undercaptured lipid screening. Adoption of EMRs in Canada is relatively recent, and therefore suboptimal use of all of EMR capabilities (eg, laboratory interface) and lack of integration noted in previous studies might also have reduced data capture.58 We unfortunately were limited in our ability to determine any pre-existing conditions, such as diabetes or chronic kidney disease, which would have been an indication for earlier or more frequent lipid screening.
Conclusion
Less than 30% of patients eligible for secondary prevention received repeat statin prescriptions from their primary care providers, as did less than 5% of those eligible for primary prevention. This represents a possible practice gap that warrants future research, as statins offer considerable morbidity and mortality benefits in these patients.
EDITOR’S KEY POINTS
Using the Manitoba Primary Care Research Network repository, this study determined the statin-prescribing trends for primary and secondary prevention of cardiovascular disease (CVD) within a large primary care sample. A total of 149 262 patient charts were categorized as either not having CVD recorded (ie, primary prevention group) or having a history of CVD recorded (secondary prevention group).
Four percent of patients in the primary prevention group were taking statins, and 29% were taking statins in the secondary prevention group. Both groups showed a trend of more elderly patients receiving statin therapy, as in both groups the 70-to-74 and 75-to-79 age ranges had the highest percentages of statin use.
Patients in the secondary prevention group were more likely to have undergone lipid testing within the past 5 years than those in the primary prevention group were (43% vs 23%, respectively). When the age cutoffs of 2012 Canadian Cardiovascular Society guidelines were applied (men aged 40 to 75 and women aged 50 to 75), 46% of patients were eligible for screening compared with 56% when the 2016 guidelines were applied (everyone aged 40 to 75).
POINTS DE REPÈRE DU RÉDACTEUR
Dans cette recherche, on a utilisé les très nombreuses données du Réseau de recherche en soins primaires du Manitoba pour examiner les tendances actuelles dans la façon de prescrire les statines en prévention primaire et secondaire des maladies cardiovasculaires (MCV). Les dossiers de 149 262 patients ont été classés selon qu’ils ne souffraient pas d’une MCV (groupe en prévention primaire) ou qu’ils avaient une histoire de MCV inscrite au dossier (groupe en prévention secondaire).
Dans le groupe en prévention primaire, 4 % des patients prenaient des statines contre 29 % dans le groupe en prévention secondaire. Dans les deux groupes, ce sont les 70 à 74 ans et les 7 à 79 ans qui prenaient le plus de statines, ce qui indique que ce sont surtout les plus âgés qui en prennent.
Les patients du groupe en prévention secondaire étaient plus susceptibles que ceux du groupe en prévention primaire d’avoir eu une mesure des lipides sanguins au cours des 5 dernières années (43 % c. 23 %, respectivement). Si on tient compte des directives concernant l’âge émises en 2012 par la Société canadienne de cardiologie, 46 % des patients (entre 40 et 75 ans pour les hommes et entre 50 et 75 ans pour les femmes) étaient admissibles pour un dépistage par rapport à 56 % lorsqu’on utilise les directives de 2016 (tous ceux qui ont entre 40 et 75 ans).
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Contributors
All authors contributed to the concept and design of the study; data gathering, analysis, and interpretation; and preparing the manuscript for submission.
Competing interests
None declared
References
- 1.Canadian Institute of Health Information . Prescribed drug spending in Canada, 2013: a focus on public drug programs. North York, ON: Canadian Institute of Health Information; 2015. Available from: https://secure.cihi.ca/estore/productFamily.htm?locale=en&pf=PFC2896&lang=en. Accessed 2015 Dec 10. [Google Scholar]
- 2.Anderson TJ, Grégoire J, Hegele RA, Couture P, Mancini GB, McPherson R, et al. 2012 Update of the Canadian Cardiovascular Society guidelines for the diagnosis and treatment of dyslipidemia for the prevention of cardiovascular disease in the adult. Can J Cardiol. 2013;29(2):151–67. doi: 10.1016/j.cjca.2012.11.032. [DOI] [PubMed] [Google Scholar]
- 3.Anderson TJ, Grégoire J, Pearson GJ, Barry AR, Couture P, Dawes M, et al. 2016 Canadian Cardiovascular Society guidelines for the management of dyslipidemia for the prevention of cardiovascular disease in the adult. Can J Cardiol. 2016;32(11):1263–82. doi: 10.1016/j.cjca.2016.07.510. [DOI] [PubMed] [Google Scholar]
- 4.Cholesterol Treatment Trialists’ (CTT) Collaborators. Mihaylova B, Emberson J, Blackwell L, Keech A, Simes J, et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380(9841):581–90. doi: 10.1016/S0140-6736(12)60367-5. Epub 2012 May 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thavendiranathan P, Bagai A, Brookhart MA, Choudhry NK. Primary prevention of cardiovascular diseases with statin therapy: a meta-analysis of randomized controlled trials. Arch Intern Med. 2006;166(21):2307–13. doi: 10.1001/archinte.166.21.2307. [DOI] [PubMed] [Google Scholar]
- 6.Brugts JJ, Yetgin T, Hoeks SE, Gotto AM, Shepherd J, Westendorp RG, et al. The benefits of statins in people without established cardiovascular disease but with cardiovascular risk factors: meta-analysis of randomised controlled trials. BMJ. 2009;338:b2376. doi: 10.1136/bmj.b2376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Petretta M, Costanzo P, Perrone-Filardi P, Chiariello M. Impact of gender in primary prevention of coronary heart disease with statin therapy: a meta-analysis. Int J Cardiol. 2010;138(1):25–31. doi: 10.1016/j.ijcard.2008.08.001. Epub 2008 Sep 14. [DOI] [PubMed] [Google Scholar]
- 8.Public Health Agency of Canada. Canadian Institute for Health Information. Canadian Stroke Network. Heart and Stroke Foundation of Canada. Statistics Canada . Tracking heart disease and stroke in Canada. Ottawa, ON: Public Health Agency of Canada; 2009. Available from: www.phac-aspc.gc.ca/publicat/2009/cvd-avc/pdf/cvd-avs-2009-eng.pdf. Accessed 2017 Sep 27. [Google Scholar]
- 9.Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366(9493):1267–78. doi: 10.1016/S0140-6736(05)67394-1. Epub 2005 Sep 27. [DOI] [PubMed] [Google Scholar]
- 10.Naci H, Brugts J, Ades T. Comparative tolerability and harms of individual statins: a study-level network meta-analysis of 246 955 participants from 135 randomized, controlled trials. Circ Cardiovasc Qual Outcomes. 2013;6(4):390–9. doi: 10.1161/CIRCOUTCOMES.111.000071. Epub 2013 Jul 9. [DOI] [PubMed] [Google Scholar]
- 11.Wilt TJ, Bloomfield HE, MacDonald R, Nelson D, Rutks I, Ho M, et al. Effectiveness of statin therapy in adults with coronary heart disease. Arch Intern Med. 2004;164(13):1427–36. doi: 10.1001/archinte.164.13.1427. [DOI] [PubMed] [Google Scholar]
- 12.Mills EJ, Rachlis B, Wu P, Devereaux PJ, Arora P, Perri D. Primary prevention of cardiovascular mortality and events with statin treatments: a network meta-analysis involving more than 65,000 patients. J Am Coll Cardiol. 2008;52(22):1769–81. doi: 10.1016/j.jacc.2008.08.039. [DOI] [PubMed] [Google Scholar]
- 13.Ray KK, Seshasai SR, Erqou S, Sever P, Jukema JW, Ford I, et al. Statins and all-cause mortality in high-risk primary prevention: a meta-analysis of 11 randomized controlled trials involving 65,229 participants. Arch Intern Med. 2010;170(12):1024–31. doi: 10.1001/archinternmed.2010.182. [DOI] [PubMed] [Google Scholar]
- 14.Rashid S, Francis GA. Statins and primary prevention: is all the evidence in? Can J Cardiol. 2008;24(4):301–3. doi: 10.1016/s0828-282x(08)70180-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McPherson R, Frohlich J, Fodor G, Genest J, Canadian Cardiovascular Society Canadian Cardiovascular Society position statement—recommendations for the diagnosis and treatment of dyslipidemia and prevention of cardiovascular disease. Can J Cardiol. 2006;22(11):913–27. doi: 10.1016/s0828-282x(06)70310-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Unal B, Critchley JA, Capewell S. Modelling the decline in coronary heart disease deaths in England and Wales, 1981–2000: comparing contributions from primary prevention and secondary prevention. BMJ. 2005;331(7517):614. doi: 10.1136/bmj.38561.633345.8F. Epub 2005 Aug 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S1–45. doi: 10.1161/01.cir.0000437738.63853.7a. Erratum in: Circulation 2014;129(25 Suppl 2):S46–8. [DOI] [PubMed] [Google Scholar]
- 18.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285(19):2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 19.Kavousi M, Leening MJ, Nanchen D, Greenland P, Graham IM, Steyerberg EW, et al. Comparison of application of the ACC/AHA guidelines, Adult Treatment Panel III guidelines, and European Society of Cardiology guidelines for cardiovascular disease prevention in a European cohort. JAMA. 2014;311(14):1416–23. doi: 10.1001/jama.2014.2632. [DOI] [PubMed] [Google Scholar]
- 20.Armstrong DW, Brouillard D, Matangi MF. The effect of the change in the Framingham Risk Score calculator between the 2006 and 2009 Canadian lipid guidelines. Can J Cardiol. 2011;27(2):167–70. doi: 10.1016/j.cjca.2010.12.025. [DOI] [PubMed] [Google Scholar]
- 21.Genest J, McPherson R, Frohlich J, Anderson T, Campbell N, Carpentier A, et al. 2009 Canadian Cardiovascular Society/Canadian guidelines for the diagnosis and treatment of dyslipidemia and prevention of cardiovascular disease in the adult—2009 recommendations. Can J Cardiol. 2009;25(10):567–79. doi: 10.1016/s0828-282x(09)70715-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hennessy DA, Bushnik T, Manuel DG, Anderson TJ. Comparing guidelines for statin treatment in Canada and the United States. J Am Heart Assoc. 2015;4(7):e001758. doi: 10.1161/JAHA.114.001758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abramson JD, Rosenberg HG, Jewell N, Wright JM. Should people at low risk of cardiovascular disease take a statin? BMJ. 2013;347:f6123. doi: 10.1136/bmj.f6123. Erratum in: BMJ 2014;348:g3329. [DOI] [PubMed] [Google Scholar]
- 24.Do statins have a role in primary prevention? An update. Ther Lett. 2010 Oct 18; Available from: www.ti.ubc.ca/wordpress/wp-content/uploads/2011/07/77.pdf. Accessed 2017 Sep 27. [PubMed] [Google Scholar]
- 25.Abramson JD, Rosenberg HG, Jewell N, Wright JM. Should people at low risk of cardiovascular disease take a statin? BMJ. 2013;347:f6123. doi: 10.1136/bmj.f6123. [DOI] [PubMed] [Google Scholar]
- 26.Ballantyne CM, Corsini A, Davidson MH, Holdaas H, Jacobson TA, Leitersdorf E, et al. Risk for myopathy with statin therapy in high-risk patients. Arch Intern Med. 2003;163(5):553–64. doi: 10.1001/archinte.163.5.553. [DOI] [PubMed] [Google Scholar]
- 27.Bellosta S, Paoletti R, Corsini A. Safety of statins. Focus on clinical pharmacokinetics and drug interactions. Circulation. 2004;109(23 Suppl 1):III-50–7. doi: 10.1161/01.CIR.0000131519.15067.1f. [DOI] [PubMed] [Google Scholar]
- 28.Hippisley-Cox J, Coupland C. Unintended effects of statins in men and women in England and Wales: population based cohort study using the QResearch database. BMJ. 2010;340:c2197. doi: 10.1136/bmj.c2197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Beltowski J, Wójcicka G, Jamroz-Wiśniewska A. Adverse effects of statins—mechanisms and consequences. Curr Drug Saf. 2009;4(3):209–28. doi: 10.2174/157488609789006949. Epub 2009 Sep 1. [DOI] [PubMed] [Google Scholar]
- 30.Ridker PM. The JUPITER trial: results, controversies, and implications for prevention. Circ Cardiovasc Qual Outcomes. 2009;2(3):279–85. doi: 10.1161/CIRCOUTCOMES.109.868299. [DOI] [PubMed] [Google Scholar]
- 31.Silva MA, Swanson AC, Gandhi PJ, Tataronis GR. Statin-related adverse events: a meta-analysis. Clin Ther. 2006;28(1):26–35. doi: 10.1016/j.clinthera.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 32.Are you taking the right treatment for your high cholesterol? Our analysis and new guidelines could change your choice. Consum Rep. 2014 Mar; Available from: www.consumerreports.org/cro/2014/03/treating-high-cholesterol-with-statins/index.htm. Accessed 2015 Dec 31. [Google Scholar]
- 33.Karmali KN, Lloyd-Jones DM, Berendsen MA, Goff DC, Jr, Sanghavi DM, Brown NC, et al. Drugs for primary prevention of atherosclerotic cardiovascular disease: an overview of systematic reviews. JAMA Cardiol. 2016;1(3):341–9. doi: 10.1001/jamacardio.2016.0218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Emberson J, Whincup P, Morris R, Walker M, Ebrahim S. Evaluating the impact of population and high-risk strategies for the primary prevention of cardiovascular disease. Eur Heart J. 2004;25(6):484–91. doi: 10.1016/j.ehj.2003.11.012. [DOI] [PubMed] [Google Scholar]
- 35.Hippisley-Cox J, Coupland C, Vinogradova Y, Robson J, Minhas R, Sheikh A, et al. Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ. 2008;336(7659):1475–82. doi: 10.1136/bmj.39609.449676.25. Epub 2008 Jun 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fleetcroft R, Schofield P, Ashworth M. Variations in statin prescribing for primary cardiovascular disease prevention: cross-sectional analysis. BMC Health Serv Res. 2014;14(1):414. doi: 10.1186/1472-6963-14-414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Colhoun HM, Betteridge DJ, Durrington PN, Hitman GA, Neil HA, Livingstone SJ, et al. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): multicentre randomised placebo-controlled trial. Lancet. 2004;364(9435):685–96. doi: 10.1016/S0140-6736(04)16895-5. [DOI] [PubMed] [Google Scholar]
- 38.Taylor F, Huffman MD, Macedo AF, Moore TH, Burke M, Davey Smith G, et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2013;(1):CD004816. doi: 10.1002/14651858.CD004816.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reid FD, Cook DG, Whincup PH. Use of statins in the secondary prevention of coronary heart disease: is treatment equitable? Heart. 2002;88(1):15–9. doi: 10.1136/heart.88.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Austin PC, Mamdani MM, Juurlink DN, Alter DA, Tu JV. Missed opportunities in the secondary prevention of myocardial infarction: an assessment of the effects of statin underprescribing on mortality. Am Heart J. 2006;151(5):969–75. doi: 10.1016/j.ahj.2005.06.034. [DOI] [PubMed] [Google Scholar]
- 41.Wei L, Ebrahim S, Bartlett C, Davey PD, Sullivan FM, MacDonald TM. Statin use in the secondary prevention of coronary heart disease in primary care: cohort study and comparison of inclusion and outcome with patients in randomised trials. BMJ. 2005;330(7495):821. doi: 10.1136/bmj.38398.408032.8F. Epub 2005 Mar 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gnavi R, Migliardi A, Demaria M, Petrelli A, Caprioglio A, Costa G. Statins prescribing for the secondary prevention of ischaemic heart disease in Torino, Italy. A case of ageism and social inequalities. Eur J Public Health. 2007;17(5):492–6. doi: 10.1093/eurpub/ckm005. Epub 2007 Feb 15. [DOI] [PubMed] [Google Scholar]
- 43.Choudhry NK, Setoguchi S, Levin R, Winkelmayer WC, Shrank WH. Trends in adherence to secondary prevention medications in elderly post-myocardial infarction patients. Pharmacoepidemiol Drug Saf. 2008;17(12):1189–96. doi: 10.1002/pds.1671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ko DT, Mamdani M, Alter DA. Lipid-lowering therapy with statins in high-risk elderly patients: the treatment-risk paradox. JAMA. 2004;291(15):1864–70. doi: 10.1001/jama.291.15.1864. [DOI] [PubMed] [Google Scholar]
- 45.University of Manitoba [website] Manitoba population research data repository. Winnipeg, MB: University of Manitoba; 2017. Available from: http://umanitoba.ca/faculties/health_sciences/medicine/units/chs/departmental_units/mchp/resources/repository/index.html. Accessed 2017 Sep 27. [Google Scholar]
- 46.Schwartz GG, Olsson AG, Ezekowitz MD, Ganz P, Oliver MF, Waters D, et al. Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes. The MIRACL study: a randomized controlled trial. JAMA. 2001;285(13):1711–8. doi: 10.1001/jama.285.13.1711. [DOI] [PubMed] [Google Scholar]
- 47.Scandinavian Simvastatin Survival Study Group Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S) Lancet. 1994;344(8934):1383–9. [PubMed] [Google Scholar]
- 48.Joseph JP, Afonso M, Berdaï D, Salles N, Bénard A, Gay B, et al. Benefits and risks for primary prevention with statins in the elderly [article in French] Presse Med. 2015;44(12 Pt 1):1219–25. doi: 10.1016/j.lpm.2015.09.015. Epub 2015 Nov 14. [DOI] [PubMed] [Google Scholar]
- 49.Shepherd J, Blauw GJ, Murphy MB, Bollen EL, Buckley BM, Cobbe SM, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet. 2002;360(9346):1623–30. doi: 10.1016/s0140-6736(02)11600-x. [DOI] [PubMed] [Google Scholar]
- 50.Choosing Wisely . Cholesterol drugs for people 75 and older. When you need them—and when you don’t. Philadelphia, PA: ABIM Foundation; 2014. Available from: www.choosingwisely.org/wp-content/uploads/2017/06/ChoosingWiselyCholesterolDrugsAMDA-ER.pdf. Accessed 2017 Sep 27. [Google Scholar]
- 51.Toward Optimized Practice . Prevention and management of cardiovascular disease risk in primary care. Clinical practice guideline. Edmonton, AB: Toward Optimized Practice; 2015. Available from: www.topalbertadoctors.org/download/1655/Lipid%20Pathway%20CPG.pdf?_20160325221151. Accessed 2017 Sep 27. [Google Scholar]
- 52.Hajjar ER, Cafiero AC, Hanlon JT. Polypharmacy in elderly patients. Am J Geriatr Pharmacother. 2007;5(4):345–51. doi: 10.1016/j.amjopharm.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 53.Allan GM, Lindblad AJ, Comeau A, Coppola J, Hudson B, Mannarino M, et al. Simplified lipid guidelines. Prevention and management of cardiovascular disease in primary care. Can Fam Physician. 2015;61(10):857–67. (Eng), e439–50 (Fr). [PMC free article] [PubMed] [Google Scholar]
- 54.Zierler A. Tracking health and healthcare in Manitoba. Winnipeg, MB: University of Manitoba; 2013. Available from: http://mchp-appserv.cpe.umanitoba.ca/reference/RHA_2013_4_pager_web_version.pdf. Accessed 2017 Oct 12. [Google Scholar]
- 55.Hennessy DA, Tanuseputro P, Tuna M, Bennett C, Perez R, Shields M, et al. Population health impact of statin treatment in Canada. Catalogue no. 82-003-X. Ottawa, ON: Statistics Canada; 2016. [PubMed] [Google Scholar]
- 56.Queenan JA, Williamson T, Khan S, Drummond N, Garies S, Morkem R, et al. Representativeness of patients and providers in the Canadian Primary Care Sentinel Surveillance Network: a cross-sectional study. CMAJ Open. 2016;4(1):E28–32. doi: 10.9778/cmajo.20140128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Singer A, Yakubovich S, Kroeker AL, Dufault B, Duarte R, Katz A. Data quality of electronic medical records in Manitoba: do problem lists accurately reflect chronic disease billing diagnoses? J Am Med Inform Assoc. 2016;23(6):1107–12. doi: 10.1093/jamia/ocw013. Epub 2016 Apr 23. [DOI] [PubMed] [Google Scholar]
- 58.Price M, Singer A, Kim J. Adopting electronic medical records. Are they just electronic paper records? Can Fam Physician. 2013;59(7):e322–9. Available from: www.cfp.ca/content/cfp/59/7/e322.full.pdf. Accessed 2017 Sep 27. [PMC free article] [PubMed] [Google Scholar]