Abstract
Global budget payment is one of the most effective strategies for cost containment, but its impacts on provider behavior have not been explored in detail. This study examines the theoretical and empirical role of global budget payment on provider behavior. The study proposes that global budget payment with price adjustment is a form of common-pool resources. A two-product game theoretic model is derived, and simulations demonstrate that hospitals are expected to expand service volumes, with an emphasis on products with higher price–marginal cost ratios. Next, the study examines the early effects of Taiwan’s global budget payment system using a difference-in-difference strategy and finds that Taiwanese hospitals exhibited such behavior, where the pursuit of individual interests led to an increase in treatment intensities. Furthermore, hospitals significantly increased inpatient service volume for regional hospitals and medical centers. In contrast, local hospitals, particularly for those without teaching status designation, faced a negative impact on service volume, as larger hospitals were better positioned to induce demand and pulled volume away from their smaller counterparts through more profitable services and products such as radiology and pharmaceuticals.
Keywords: global budget payment, provider behavior, noncooperative competition, hospital, common-pool resources
1. INTRODUCTION
In recent decades, countries around the world have witnessed a rapid and inexorable increase in health care costs (Fan and Savedoff, 2014). Such continuously escalating health spending not only absorbs part or all of real-income increases but also threatens to crowd out public programs in education and other social services (Chernew et al., 2009). Therefore, cost control is one of the most prominent features in almost all health reform efforts, and among the strategies for cost control, global budget payment, defined as the setting of all-inclusive operating budget in advance, has been successful (Benstetter and Wambach, 2006; Schwartz, Glennerster and Saltman, 1996; U.S. General Accounting Office, 1991; Wolfe and Moran, 1993; Yakoboski et al., 1994). Some have also argued that a global budget payment system can control costs without infringing on professional autonomy; under a sector-wide budget, providers are free to decide how best to deliver services to their patients (Roberts et al., 2004; Chen, 2009).
Yet despite the accumulated experiences with global budget payment systems in the past three decades in Canada and in advanced economies in Europe, we only have limited theoretical and empirical knowledge of the impact of such payment schemes on provider behavior and on dimensions of health system performance other than cost control. Indeed, a Mathematica study commissioned by the Massachusetts State Government concluded, ‘because the effect of global budget caps on health care spending and outcomes has not been studied, there is no general agreement about their impact’ (Mathematica, 2009).
In the theoretical literature, only a few studies have presented analyses of global budget payment (Benstetter and Wambach, 2006; Mougeot and Naegelen, 2005). In the empirical literature, except on the effect on cost containment, studies have not reached much agreement on other impacts of global budget payment. Hurley et al. (1997) found a rapid increase in the total service volume after the introduction of global physician expenditure caps in two provinces of Canada. Similar phenomena were also noted in the German (Benstetter and Wambach, 2006) and Taiwanese global budget payment systems (Chen et al., 2007; Cheng et al., 2009). In contrast, Detsky et al. (1983) asserted that global budgeting had led to lower real inputs per admission and per patient-day in Ontario and in US hospitals. Redmon and Yakoboski (1995) also argued that sectoral budgeting helped to control service utilization in French hospitals from 1960 to 1990. Furthermore, most of these earlier writings are descriptive or do not take into account the counterfactuals in their effect estimation. Consequently, it is rather difficult to validate those findings and reach a definitive conclusion on the impacts of global budget payment.
This paper contributes to both the theoretical and empirical literature. This study extends current theory by presenting a two-product model, which in turn generates intuitions about a provider’s product mix under global budget payment or fee-for-service (FFS). Second, this study assesses the changes in hospital behavior as a consequence of a global budget payment system in Taiwan implemented in 2002. We begin by defining the various types of global budget payment and describing the Taiwanese system. Section 3 presents the theoretical model and accompanying simulations. Section 4 presents methods and data for the empirical analyses using Taiwanese hospital claims data, followed by corresponding results in Section 5. Section 6 concludes.
2. BACKGROUND ON GLOBAL BUDGET PAYMENT AND THE TAIWANESE SYSTEM
2.1. Global budget payment
One source of confusion about the impact of ‘global budget payment’ is that the term has been used to refer to a wide variety of schemes used in different contexts. Typically, global budget payment means the allocation of a fixed amount of resources to health at the sector or system level, not at the individual or organizational level. Major differences, however, exist in the way the system-wide expenditure cap is enforced. There are three enforcement mechanisms, entailing different incentives for providers: price adjustment, capitated payments to the health plans, and limiting a provider’s budget (Long and Marquis, 1994). The first mechanism holds expenditure fixed by adjusting the prices of services in accordance with volume change. To our knowledge, only a limited number of systems, that is, German ambulatory sector, Taiwanese, and few Canadian provinces, apply such a price adjustment. This paper focuses exclusively on the first mechanism. The second and third mechanisms allocate fixed amounts of money to health plans and providers, respectively, and the difference between the allocated budget and actual spending can be retained as profits or suffered as losses. For example, in the USA, ‘global budget payment’ often implicitly refers to the latter two mechanisms (e.g., Congressional Budget Office, 2008; Griner, 1994; Mathematica, 2009; Sack 2009).
2.2. Taiwanese global budget payment system
In 1995, Taiwan established its universal National Health Insurance (NHI) system, which is a compulsory insurance scheme with generous benefits including inpatient care, outpatient care, drugs, dental care, and Chinese medicine. Under the NHI, the enrollment rapidly expanded: by the end of 1996, 96% of the population had already been insured (Lu and Hsiao, 2003). As insurance coverage expanded and the payment system remained largely FFS, NHI expenditures grew at a faster rate than its revenues since its inception: the average annual growth rate in spending was 6.26%, compared with 4.26% in revenue over 1995–2001 (Cheng, 2003). To control the expenditure growth, a global budget payment system with price adjustment was implemented in 2001 and 2002 for the clinic and the hospital sectors, respectively, to replace the previous FFS scheme. This paper is concerned with the global budget payment scheme with price adjustment for the hospital sector.
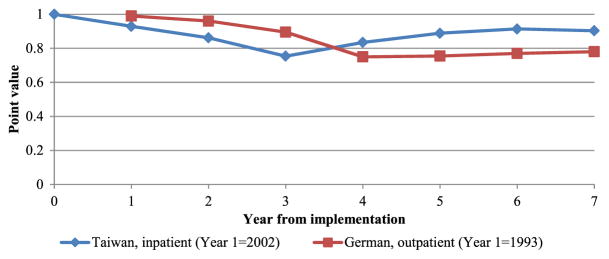
In the Taiwanese global budget system, each treatment and intervention are assigned a certain amount of points reflecting relative values in a point schedule (similar to a fee schedule). To allocate the budget to providers, the total budget is divided by the point sum of all services rendered by all hospitals, generating a point value (PV). Whereas the relative prices of treatments are fixed, the actual values are determined ex post on the basis of the PV—that is, the ‘price adjustment’. Consequently, even though the total sectoral budget is set prospectively, the actual reimbursement for each hospital is determined retrospectively, contingent on the volumes of others in the market. This contrasts to the practices in countries using other types of global budgeting, for example, for hospitals, in which an individual hospital budget and the absolute prices of each intervention are both known prospectively. Such as the German system for outpatient care, the Taiwanese system creates uncertainty that drives the behavioral response of the providers. Figure 1 presents the trend of national average PV over time in the Taiwanese system for inpatient care, compared with the German system for outpatient care. After Taiwan implemented its global budget payment system for inpatient care in 2002, the PV dropped by 25% by year 3 (2004) compared with the baseline year of 2001, indicating an increase in service volume in terms of total number of points. Similarly, after Germany implemented an ex post floating point-value mechanism, the PV also reduced by 25% by year 4 (1996) (Benstetter and Wambach, 2006).
Figure 1.
Trends in point value in Taiwanese and German global budget payment systems
Notes: Data for Taiwan are from Bureau of National Health Insurance (2013) and for Germany from Benstetter and Wambach (2006). After falling, the point values in both Taiwan and Germany increased but for different reasons. In Germany the point value stabilized after a limit on the number of points per practice was imposed (Benstetter and Wambach, 2006). By contrast, in Taiwan, after learning from early experiences of the global budget payment, providers began to act cooperatively to overcome their collective action dilemma after 2004 (see Chen, 2011 for detailed discussion), and thus the post-2004 reversal was not a consequence of any policy change during global budget payment early implementation, the focus of this study.
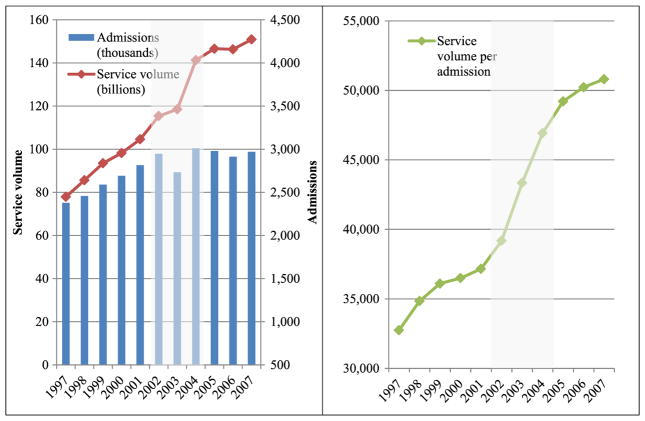
In Taiwan, the total point volume of provided services has increased since policy implementation, even as the number of admissions has been stable (or even declined slightly after 2004) (Figure 2, left), indicating that hospitals expanded service volume through higher intensity of treatment per admission (Figure 2, right). Moreover, the service intensity expanded rapidly during the early period (2002–2004) but stabilized in the later period (2005–2007). The next section of this paper will present a theoretical model of why treatment intensities increase and the PVs drop in the early stage of global budget payment.
Figure 2.
Admission number and total service volume for inpatient care, Taiwan, 1997–2007
Note: The drop in case number in 2003 was potentially related to an exogenous and temporary system shock (SARS epidemic outbreak), and hence data for 2003 are not used in the study.
3. THEORETICAL ANALYSIS OF THE GLOBAL BUDGET PAYMENT SYSTEM
3.1. Common-pool resources and collective action
In global budget payment with price adjustment, providers are faced with the following dilemma: as a group, providers are better off with a lower service volume as the budget is fixed. Nevertheless, from the individual’s perspective, regardless of what others do, the dominant strategy to secure a higher share of the budget is always producing larger quantities of services. Meanwhile, any simultaneous increase in service volume by providers automatically results in a lower PV and lower de facto prices for all. In other words, the pursuit of individual interests by rational individuals could lead to a collective failure.
This dilemma however is by no means unique. The funds in this type of global budget payment system are in essence a type of common-pool resource (CPR) (Ostrom et al., 1994). Unlike pure public goods with low subtractability and excludability, CPR often faces issues of over-crowding or overuse (Hardin, 1968; Olson, 1965). Many researchers have attempted to investigate the social dilemma in CPR using game theory—the simplest presentation of which is the Prisoner’s Dilemma in noncooperative games. This analysis predicts that if nonexcludable goods are involved, individuals will not act to achieve their common interest. The failure of cooperation predicted by game theory has also been repeatedly reinforced by laboratory experiments (Gardner and Ostrom, 1991) and empirical studies (e.g. Moran and Ostrom, 2005; Myers and Worm, 2003; and Pauly et al., 2002). Applying such reasoning to the global budget payment, hospitals will always pursue the dominant strategy of ‘defecting’ to increase service volume in the Nash equilibrium (NE).
Although predictions from early noncooperative game studies about the prospect of collective action are pessimistic, other studies argued for some optimism (Axelrod, 1984; Fudenberg and Maskin, 1986). These optimistic studies, however, typically assume a critical precondition that there already exist at least a small yet critical number of people who adopt a strategy to cooperate first and punish later if other players defect. Yet if everyone had similar decision-making processes and objective functions, there would be no reason to believe that any one player should suddenly decide to change to a strategy that is different from others. Therefore, when players are mostly driven by self-interest and engage in noncooperative competition under a constraining global budget, the application of noncooperative game theory is still warranted in understanding provider strategic behavior.
3.2. A model of provider behavior under global budget payment
In this section, a formal model of hospital behavior under global budget payment is presented in which the NE strategy in the global budget payment is derived. Assume n homogenous hospitals in the market with a global budget B. Hospital managers set the target total service volume in terms of k points, which determines the share of the budget each hospital receives. Assume that two services are provided, with the relative prices indicated by points, p1 and p2. Hospital managers decide the optimal quantities of each services, q1 and q2. Further assume that there is no complementarity in the production of the two services. This two-product setup extends the theoretical models in the literature, which are mostly based on a homogenous single product; this two-product setup reflects the fact that in reality, hospitals provide a mix of different products. Further, assume that the absolute and relative demands for the different services are driven by the providers in this model, given that patients are protected against financial costs in the Taiwanese system.
Let the cost function for an individual hospital take the following form:
Then the optimization problem is essentially an exercise in cost-minimization:
Taking the first-order conditions, one can derive the cost function as a function of p1, p2, and k (Supporting Information A).
In this system, the real prices of items are set by a joint function of the point (fee) schedule and PV, which are derived by dividing the total budget by the total point sum of all services by all hospitals. Hence, the profit (π) for hospital x is:
The hospital competition here is a Cournot competition where firms compete on output quantity and set them independently and simultaneously. Consider the NE outcome, in which each hospital chooses its best production strategy, taking into consideration the behavior of others without any effective communication or coordination. The output volume (k*) at NE can then be derived (Supporting Information B), and its comparative statics can be studied:
Once the total service output at equilibrium (k*) is set, the managers need to decide the best service mix. The quantity of product 1 at equilibrium should equal
Service output for product 1 at equilibrium is affected by its price. The direction of the relationship is shaped by the term ( ) in the comparative statics. This implies that if the price/marginal cost ratio of product 1 is relatively high than that of product 2, hospitals will devote much more of their delivery to product 1 as p1 increases. The reaction to price change will be much less if the price/marginal cost ratio is relatively smaller, compared to the other product. The model demonstrates that product profitability for the hospitals is determined by the price/marginal cost ratio of the product and that not only do hospitals produce more under global budget payment, the increase in service volume is higher when the price/marginal cost is higher.
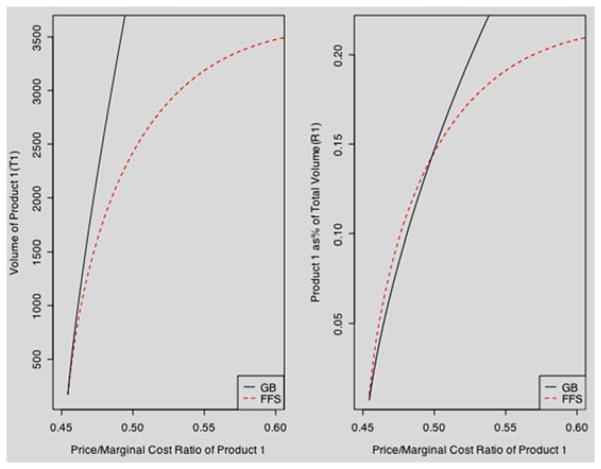
Figure 3 presents the results of a simulation of the service volume and service mix as a function of the price–marginal cost ratio of product 1, showing that the increase in service volume is higher when the price/marginal cost is higher under global budget compared with FFS (left graph). In terms of the importance of the product as the revenue source, or the relative role in the service mix, indicated by the share of total service volume devoted to the product (right graph), when the price/marginal cost ratio is low and hence relatively less profitable, the relative share in the global budget could even become lower than in FFS. Yet, when the profitability of product 1 becomes larger, the service mix also shifts toward product 1. In short, the simulation results indicate that hospitals do not simply expand the service volume with the same mix but strategically increase more of the products that give higher profit intensities (Supporting Information C).
Figure 3.
Product 1 service volume (T1) and its share of total volume (R1) under fee-for-service (FFS) and global budget payment (GB)
This derivation and simulation demonstrate that what constitutes higher profitability in global budget system differs from that in FFS, even though the price/cost (p/c) ratio and the price-cost (p-c) difference are correlated. Under FFS, providers are mainly concerned with the p-c difference rather than the p/c ratio. By contrast, under global budget, an indicator of profitability is the p/c ratio or, more accurately, the price/marginal cost ratio. The intuition behind this phenomenon is that because of the fixed cap of the global budget, for every unit of additional production cost, the hospitals seek out services with higher profits, hence the attention to p/c ratio.
As an example, take two different products, one with a 10% margin service of $10,000 has a lower p/c ratio (1.1) and another with a 50% margin service of $1000 with a p/c ratio of 2. Under an FFS regime and to maximize profits regardless of the budget constraint, a provider would choose the first product as it has higher profits, although it has a lower p/c ratio. In contrast, under a global budget payment regime, the total budget and total volume of services determine the additional value or profit per point of service, and a provider seeking higher profits would focus on p/c ratio. Further supporting this argument is related literature found from cost-benefit analysis in weighing whether to use the cost-benefit difference or the cost-benefit ratio as the criterion to rank the value of a program. In the case of limited resources, it is generally agreed that the ratio, not the difference, should be used for ranking purpose (Dompere, 2004 and Drummond et al., 2005).
To identify services with high p/c ratios, without access to a detailed costing study, one must resort to the literature. One common feature of medical services with high p/c ratios is that they usually require relatively more capital than labor inputs. This is because prices of the capital-intensive services are typically set at their average cost to account for the large fixed costs required to acquire machines or equipment, and marginal costs further reduce with the advances in technology (Ginsburg and Grossman, 2005). Moreover, physician’s time is often the scarcest resource of all in a health care production process and may even have increasing marginal costs (Mattke, 2001). One type of services, for instance, that is of the aforementioned characteristics and often reported to have high p/c ratios, is radiologic imaging services, such as CT and MRI (Evens and Evens, 1991; Ginsburg and Berenson, 2007; Hsiao et al., 1988; McGuire and Pauly, 1991). In related work by Chen (2011), the profitability of services was assessed through qualitative interviews of 17 private hospital managers and CEOs (local or regional hospitals with a capacity ranging from approximately 80 to 800 beds), who have access to their own cost data and make decisions regarding the response of the hospitals to payment change and allocation of resources across a wide spectrum of health services. Both the literature and the qualitative study provided a consistent indication of the relative profitability of different services.
The aforementioned arguments are under the assumptions that there is no change in incentives on the demand side and that health services utilization is largely driven by the supply side. Both assumptions hold true in the Taiwanese NHI. First, except for an increase in the copayment of less than $5 for hospital ambulatory services in 2005, there has been no change in the benefit package since 2002. Second, although providers are constrained by legal rules and medical ethics and cannot freely induce any and everything, in reality, there are numerous circumstances where clinical uncertainties allow for, and indeed require, professional judgment. Given the large latitude by providers to affect the consumption of health services, which is commonly observed empirically, the assumption remains valid.
4. EMPIRICAL ANALYSIS OF HOSPITAL BEHAVIOR IN TAIWAN
4.1. Methods
In practice, policy interventions are usually implemented nationwide at the same time without an apparent control group. Thus, one common deficiency in past research on the effects of global budget payment has been the lack of use of a valid counterfactual (Chen et al., 2007; Cheng et al., 2009; Hurley et al., 1997). If a simple difference of the outcome is taken before and after the policy change, this single difference would contain both the causal impact and the time trend. This study identifies the effects of Taiwan’s global budget system by difference-in-difference analysis using data from hospital claims.
In this difference-in-difference analysis, the regression is specified as follows:
where Yit indicates the outcome of interest, that is, total point volume or service mix, of provider i in year t. Et is a dummy variable equal to 1 if the observation belongs to the treatment group (year 2001/2004). Postt is a time dummy, indicating that the observation is in the later year of its group (year 2000/2004). δ is the DID estimator of the global budget payment impact; X is a range of different time-varying hospital characteristics such as accreditation level, ownership, and teaching status; and ηi are hospital fixed effects (FEs). The error term εit is clustered by a hospital. A key assumption is that without the global budget payment, the rate of change in the provision of services would not have been systematically different in pre-policy and post-policy period. Nevertheless, the control group used here cannot account for other nonlinear trends occurring at the same time.
Several robustness checks are performed. First, the DID is applied using a ‘placebo treatment group’, where the policy intervention in fact did not take place. If the time trend is linear, the DID estimate using the placebo treatment group should be insignificantly different from zero. Second, as most hospitals compete locally and their behavior is affected by interactions with other hospitals in the same geographic area, separate analyses are performed using county rather than hospital FEs to account for county-specific effects affecting treatment pattern heterogeneity, with robust standard errors clustered by counties. Third, frontier matching methods are applied with difference-in-differences (Iacus et al., 2011). Hence ‘treated’ and ‘control’ hospitals are matched by different hospital and regional characteristics and the post-period. Fourth, a difference-in-difference analysis using cross-country time-series data estimates the effect of Taiwan’s global budget payment after 2002 on inpatient service volume. This analysis uses as counterfactuals different sets of countries with universal health insurance but lacking global budget payment (Supporting Information D).
4.2. Data
The analyses use National Health Research Institute databases assembled from electronic inpatient claims submitted by all hospitals from 1997 to 2004. The National Health Research Institute claims database covers 99% of the population and all hospitals in the country, and analyses based on these data are hence free from selection bias. The claims data contain information on services provided to the patients: age and sex of the beneficiary; hospital and physician id; type of treatment; date and duration of treatment; diagnosis (ICD-9 code); name, quantity, and price of the drugs prescribed; and total charge and its breakdown. Given that the research question is to examine the behavior of hospitals, the unit of observation is the hospital.
The outcomes of interest expressed in PVs are annual inpatient service volume and annual volume of services in different categories, that is, diagnosis, examinations, radiological studies, therapy, and surgery expressed as a proportion of the total service volume in the respective hospital. The diagnosis category includes fees to reimburse providers’ decision-making efforts to diagnose and prescribe medication, examinations, and interventions. The examination category includes all types of nonradiological examinations, such as biochemical and microbiological tests, physiological function examinations, sonography, ophthalmic tests, and endoscopy. The therapy category includes a wide variety of nonsurgical treatments, such as wound treatments, local anesthesia and nerve block, local incision and drainage, and endoscopic treatments.
The database also contains provider registration files with hospital characteristics information, including level of accreditation, ownership, whether it is a teaching hospital, volume of admission, and geographical location. Taiwanese hospitals are generally accredited and categorized into three levels (medical centers, regional hospitals, and local hospitals) on the basis of their bed capacity, medical specialties, and staff densities (e.g., regional hospitals and medical centers are required to have certain number of anesthesiologists and radiologists per respective bed sizes). Separately, hospitals are also accredited with teaching status if they meet the requirements for performing educational and research activities.
Descriptive statistics are presented in Table I, showing that the number of hospitals decreased from 649 in 1997 to 557 in 2004, with the reduction more among local hospitals. The majority of hospitals (85%) are privately owned. The average service volume, measured by the sum of points of all services, varied substantially across different levels of accreditation, with the volumes in medical centers on average more than 50 times that in local hospitals.
Table I.
Descriptive statistics of claims data
| 1997 | 2000 | 2001 | 2004 | |
|---|---|---|---|---|
| N | 649 | 628 | 588 | 557 |
| % Medical centers | 2.16 | 3.03 | 3.06 | 3.23 |
| % Regional hospitals | 10.02 | 11.15 | 12.24 | 13.82 |
| % Private | 85.67 | 85.03 | 84.52 | 83.84 |
| Mean volume (millions of points) | ||||
| Medical center | 2481.15 | 2453.63 | 2777.33 | 3333.27 |
| Regional hospitals | 404.19 | 477.35 | 495.10 | 708.15 |
| Local hospitals | 32.48 | 36.18 | 46.76 | 64.51 |
5. RESULTS OF EMPIRICAL ANALYSIS
5.1. Difference-in-difference analyses
Table II presents the results of the DID estimator. The first column shows that the Taiwanese global budget payment had differential effects by hospital characteristics. For example, among nonteaching public hospitals, on average, global budget resulted in an overall increase in annual inpatient service volume of 133 million points for regional hospitals, 750 million points for medical centers, and a decrease of 37 million points for local hospitals. As reference, the average annual inpatient service volume in 2001 was 2.78 billion points for medical centers, 495.1 million points for regional hospitals, and 41.8 million points for local hospitals. Accordingly, the impact of global budget translated into a volume increase, measured by number of points, of approximately 27% of the service volume in 2001 for nonteaching public regional hospitals and medical centers. In contrast, there was on average a sharp reduction of 88% in service volume among local hospitals. Teaching hospitals, compared with their counterparts without teaching status, also had an increase of 57 million points as a result of global budget. There was no statistically significant difference between the private and public hospitals in service volume change.
Table II.
Difference-in-difference estimation of Taiwan’s global budget payment effect on volume and service mix
| Control variables | Total volume | Services of specific category (% of total volume) | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Diagnosis | Examination | Radiology | Therapy | Surgery | Drug | ||
|
|
|||||||
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | |
| Treatment | 48.3*** (7.5) | 0.00675*** (0.00101) | −0.01550*** (0.00160) | −0.00393*** (0.00093) | 0.04465*** (0.00588) | 0.00396 (0.00392) | −0.02660*** (0.00219) |
| Post | 32.4*** (6.7) | 0.00783*** (0.00093) | −0.01235*** (0.00146) | −0.00315*** (0.00083) | 0.03087*** (0.00512) | 0.00479 (0.00346) | −0.01463*** (0.00202) |
| DID | 132.9*** (31.3) | −0.01631*** (0.00408) | −0.00406 (0.00422) | 0.00521** (0.00249) | 0.01217 (0.01477) | −0.02528*** (0.00837) | 0.01113* (0.00635) |
| DID* center | 616.6*** (117.0) | −0.00222 (0.00172) | 0.00091 (0.00208) | 0.00347 (0.00223) | −0.01818*** (0.00556) | 0.00957*** (0.00353) | 0.01044** (0.00422) |
| DID* local | −169.7*** (33.1) | −0.00624** (0.00253) | −0.00288 (0.00293) | −0.01228*** (0.00207) | 0.01397* (0.00825) | 0.00120 (0.00488) | −0.01074** (0.00450) |
| DID* teaching | 57.2*** (14.8) | 0.00944*** (0.00273) | 0.01936*** (0.00358) | 0.00646*** (0.00191) | −0.06965*** (0.01158) | −0.00045 (0.00631) | 0.01138** (0.00448) |
| DID* private | 10.8 (26.1) | 0.00777** (0.00379) | 0.00110 (0.00282) | 0.00224 (0.00154) | 0.03247*** (0.01232) | −0.00906* (0.00541) | −0.00602 (0.00428) |
| Medical center | −141.6 (87.5) | −0.00000 (0.00120) | 0.00260 (0.00232) | −0.00150 (0.00397) | −0.02517*** (0.00946) | −0.00471 (0.00440) | 0.01725*** (0.00395) |
| Local hospital | −59.5 (37.3) | −0.00147 (0.00164) | 0.00227 (0.00296) | 0.00130 (0.00187) | −0.00484 (0.00897) | 0.00731 (0.00564) | 0.00929 (0.00647) |
| Teaching hospital | 39.6** (17.1) | −0.01057*** (0.00299) | −0.00474 (0.00403) | −0.00098 (0.00143) | 0.02171* (0.01235) | −0.00592 (0.00770) | 0.00493 (0.00657) |
| R2 | 0.49 | 0.09 | 0.18 | 0.11 | 0.21 | 0.06 | 0.25 |
| Control experiment | |||||||
| DID | 7.6 (18.3) | −0.00849*** (0.00300) | 0.00239 (0.00367) | 0.00287 (0.00230) | 0.00262 (0.01179) | −0.00645 (0.00800) | −0.00778 (0.00687) |
Robust standard errors clustered by hospitals in parentheses. Controlled for accreditation level, ownership, and teaching status of hospitals. Total volume in millions of points.
Significance levels:
p<0.10;
p<0.05;
p<0.01.
To investigate shifts in the service mix within a hospital, columns 2–7 present estimates of the impact on the hospital share of a service category by hospital characteristics. The results show that global budget led to an increase in the relative shares of radiological imaging studies and of pharmaceuticals among regional hospitals and medical centers, especially teaching hospitals. In contrast, the volume of shares of surgical and diagnosis fees reduced. Global budget also decreased the share of nonsurgical therapies among medical centers, especially, again, in teaching hospitals. Additionally, for teaching hospitals, global budget also resulted in an increase of share for examination fees. The change in service mix in response to global budget was similar among private and public hospitals, except that private hospitals had a smaller reduction in share of diagnosis fees, a larger decline in share of surgical treatments, and an increase in share of nonsurgical treatments for nonteaching hospitals.
5.2. Robustness checks
To check the robustness of the results, a similar specification is estimated using the change in outcome over 1999–2001 as the ‘placebo’ and the change over 1997–1999 as the control. The placebo test uses a 2-year period rather than a 1-year period difference; this placebo test is closer to a 3-year period difference used in the main results and less susceptible to year-to-year fluctuations if one used a 1-year difference. The DID estimates of the ‘control experiments’ or falsification tests do not indicate a statistically significant impact of the placebo treatment, supporting the linear time assumption, except for the shares of diagnosis fees (Table II). Another set of specifications are carried out using county FEs and robust standard errors clustered by county, and the two results are mostly consistent with each other in terms of sign (Table III and Supporting Information E). The results indicate that the share of radiological services and drugs each increased, whereas surgery and diagnosis fees each decreased. In the robustness check using coarsened exact matching, the results are highly consistent with the DID results using hospital FEs (Table III). In the cross-country time-series analysis, the results indicate that after 2002, there was a significant increase in per capita service volume in Taiwan relative to comparable countries (Supporting Information D).
Table III.
Robustness checks on difference-in-difference estimates
| DID estimate | Total volume | Services of specific category (% of total volume) | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Diagnosis | Examination | Radiology | Therapy | Surgery | Drug | ||
|
|
|
|
|
|
|
|
|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | |
| A. DID, hospital FEs | 132.9*** (31.3) | −0.01631*** (0.00408) | −0.00406 (0.00422) | 0.00521** (0.00249) | 0.01217 (0.01477) | −0.02528*** (0.00837) | 0.01113* (0.00635) |
| B. DID, county FEs | 237.8*** (37.25) | −0.000299 (0.00280) | 0.0230*** (0.00352) | 0.0161*** (0.00226) | −0.0893*** (0.0118) | −0.0227*** (0.00874) | 0.0363*** (0.00497) |
| C. CEM+ DID | 190.5*** (43.9) | −0.01841*** (0.00435) | 0.00793 (0.00618) | 0.00945** (0.00368) | −0.00019 (0.01760) | −0.03160** (0.01319) | 0.02800*** (0.00791) |
Robust standard errors clustered by hospital in parentheses except for (B). Total volume in millions of points. A. Controlled for hospital fixed effects, accreditation level, ownership, and teaching status of hospitals and region.
B. Controlled for county fixed effects, accreditation level, ownership, and teaching status of hospitals and region; robust standard errors clustered by county in parentheses.
C. Hospitals matched using CEM (Iacus et al., 2011) on accreditation level, ownership, and teaching status of hospitals and region.
Significance levels:
p<0.10;
p<0.05;
p<0.01.
6. DISCUSSION
This study makes two main contributions. First, it extends the theory on global budget payment through a two product noncooperative game theoretic model and simulation. The simulation demonstrates that the increase in treatment intensities under global budget and the importance of p/c ratios on service volume and mix are even greater than under FFS. Second, using the case of Taiwan’s global budget payment, the study finds that during the first few years after the replacement of FFS by global budget payment, the behavior of hospitals was consistent with strategic actions undertaken by players in a noncooperative competition game. Hospitals expanded their service volume and also exhibited a shift toward services, which generally have higher p/c ratios in their outputs—hospitals proportionally increased services such as radiological imaging studies and drugs but reduced physician-labor-intensive surgical interventions and, to a lesser extent, decision-making efforts of diagnosis. These analyses were robust to a variety of specifications and falsification tests.
The findings indicate that global budget payment may have resulted in a differential response by hospital characteristics, that is, across local hospitals, regional hospitals, and medical centers, as well as between teaching and nonteaching hospitals. While there was an increase of close to 30% of the service volume in both regional hospitals and medical centers, nonteaching local hospitals faced a serious negative impact in service volume. As hospitals attempted to drive up their service volume through increased provision of capital-intensive services such as radiological imaging, medical centers and regional hospitals are much better equipped to do so. Local hospitals are constrained by capital requirements to acquire new equipment, which contributes to patients’ preferences or biases toward larger hospitals for such imaging services. Consequently, as regional hospital and medical centers raced to increase their service volume, the relative volume from local hospitals declined. This is consistent with the finding that the number of local hospitals in Taiwan decreased, as the reduction in volume and the inability to drive high marginal p/c services led to consolidation.
Similarly, teaching hospitals, which are more likely to have imaging or lab test equipment for educational and research purposes, are also better positioned to increase service volume through capital-intensive and high p/c ratio services. In fact, among local hospitals, those with teaching status, although comprising a relatively small portion, could drive up service volume by almost 50% (20 million points out of an average of 42 million-point 2001 baseline) under global budget payment, as opposed to the volume reduction experienced by others without such accreditation.
The obvious question following the findings of shifts toward high p/c ratio services is its impact on quality of care. The inducement of unnecessary services could impose higher morbidity and even mortality risk onto patients. We began to explore this question through a subgroup analysis on a specific procedure—cardiac catheterization (Supporting Information F). Results suggest that global budgeting may have incentivized providers to favor marginally more profitable yet more harmful procedures. It would be important to investigate further in future studies, given the grave implications not only on long-term healthcare cost but also, more importantly, population health.
The findings presented here should be generalized with caution. The method is based on the assumption of a linear time trend in service provision without the global budget payment. The robustness checks employed provide some assurance of this strategy, but they do not guarantee the validity of such strategy in every context. The empirical analysis cannot exclude the potential of other trends happening simultaneously such as the consolidation of the hospital industry and selection effects among surviving hospitals. Furthermore, the profitability profiles of specific services heavily depend on the specific rates, costs, and relevant regulations in the health sector examined. Therefore, one should exercise caution in inferring from the results here any direct predictions on exact volume change of specific services if global budget payment were to be introduced in other countries.
Another limitation of this paper is the lack of more direct evidence of health-service costs obtained through a detailed costing study—which in turn could permit systematic examination of the changes in service mix by profitability by p-c ratios and differences. Nevertheless, this study provides evidence of an indication that global budget payment shifts service mix towards categories, which are known to have high p/c ratios in both the literature and through qualitative research (Chen, 2011).
A third limitation of this paper is that it is focused on the early years of the global budget payment system. A related study by Chen (2011) examines the longer-term effects of the global budget payment system and finds that the post-2004 increase in PV is a consequence of hospital managers learning from their early experiences in the global budget payment system and acting cooperatively to overcome the collective action dilemma, albeit with varied levels of success in different regions. The most critical determinant of effective coordination across regions has been the level of trust and reciprocity among hospitals. This in turn could be affected by a number of factors including heterogeneity, communication, and linkages among hospital managers.
In countries such as Germany, Canada, and Taiwan, global budget payment has been employed to reduce health care cost inflation, whereas other countries and even states in the USA have also been considering the adoption of similar schemes. Taiwanese global budget payment was intended as a cost containment strategy without too much interference into the professional autonomy. It was hoped that through peer pressure, providers would deliver appropriate care and improve the efficiency and quality of the health system. This study has found that, on the contrary, the policy may have fallen short. If the hospitals are driven by financial incentives, pursuit of profits in a noncooperative competition can lead to volume race with allocative inefficiency and even compromise in quality of care. By simply putting an expenditure cap on top of a FFS-like system—and in this case using a floating point-value mechanism—will not alleviate distorted incentives existing in the fee or point schedule. Unless the payment rate is revised to reflect the marginal costs, hospitals will still concentrate on services such as imaging services that would not necessarily yield many health benefits. Ultimately, when reimbursement is tied to quantity and profits, hospitals respond in quantity, not by efforts to improve health outcomes. Policy makers intending to employ global budgeting to curb health expenditure growth but at the same time attempting to maintain or improve quality of care would need to consider complementing point-based global budget payment with other strategies, such as performance-based payment, or an increased emphasis on the use of evidence-based medicine and clinical pathways to minimize its unintended consequences.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge Ajay Mahal, Marc Roberts, Winnie Yip, Thomas McGuire, and two anonymous reviewers for their comments.
Footnotes
The work was completed in part with the financial support from CCK Foundation for International Scholarly Exchange.
Supporting information may be found in the online version for this article.
CONFLICT OF INTEREST
The authors have no conflict of interest.
References
- Axelrod RM. The Evolution of Cooperation. Basic Books; New York: 1984. [Google Scholar]
- Benstetter F, Wambach A. The treadmill effect in a fixed budget system. Journal of Health Economics. 2006;25(1):146–169. doi: 10.1016/j.jhealeco.2005.04.004. [DOI] [PubMed] [Google Scholar]
- Bureau of National Health Insurance (BNHI) The national health insurance statistics report, 2010. National Health Insurance Administration, Ministry of Health and Welfare; 2013. [Google Scholar]
- Chen S-H. Master thesis. National Taiwan University; Taipei, Taiwan: 2009. The political analysis of global budgeting for the national health insurance. [Google Scholar]
- Chen F-J, Laditka JN, Laditka SB, Xirasagar S. Providers’ response to global budgeting in Taiwan: what were the initial effects? Health Services Management Research. 2007;20(2):113–120. doi: 10.1258/095148407780744624. [DOI] [PubMed] [Google Scholar]
- Chen YTB. Dissertation. Harvard School of Public Health; Boston, MA: 2011. Strategic Provider Behavior Under Global Budget Payment. [Google Scholar]
- Cheng T-M. Taiwan’s new national health insurance program: genesis and experience so far. Health Affairs. 2003;22(3):61–76. doi: 10.1377/hlthaff.22.3.61. [DOI] [PubMed] [Google Scholar]
- Cheng S-H, Chen C-C, Chang W-L. Hospital response to a global budget program under universal health insurance in Taiwan. Health Policy. 2009;92(2–3):158–164. doi: 10.1016/j.healthpol.2009.03.008. [DOI] [PubMed] [Google Scholar]
- Chernew ME, Hirth RA, Cutler DM. Increased spending on health care: long term implications for the nation. Health Affairs. 2009;28(5):1253–1255. doi: 10.1377/hlthaff.28.5.1253. [DOI] [PubMed] [Google Scholar]
- Congressional Budget Office. Key Issues in Analyzing Major Health Insurance Proposals. The Congress of the United States; Washington D.C: 2008. [accessed December 7, 2010]. http://www.cbo.gov/ftpdocs/99xx/doc9924/toc.shtml. [Google Scholar]
- Detsky AS, Stacey SR, Bombardier C. The effectiveness of a regulatory strategy in containing hospital costs—the Ontario experience, 1967–1981. New England Journal of Medicine. 1983;309:151–159. doi: 10.1056/NEJM198307213090306. [DOI] [PubMed] [Google Scholar]
- Dompere KK. Cost-Benefit Analysis and the Theory of Fuzzy Decisions: Fuzzy Value Theory. Springer; New York: 2004. [Google Scholar]
- Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the Economic Evaluation of Health Care Programmes. 3. Oxford University Press; New York: 2005. [Google Scholar]
- Evens RG, Evens RG., Jr Analysis of economics and use of MR imaging units in the United States in 1990. American Journal of Roentgenology. 1991;157(2):603–607. doi: 10.2214/ajr.157.3.1872246. [DOI] [PubMed] [Google Scholar]
- Fan VY, Savedoff WD. The health financing transition: a conceptual framework and empirical evidence. Social Science and Medicine. 2014 doi: 10.1016/j.socscimed.2014.01.014. Forthcoming. [DOI] [PubMed] [Google Scholar]
- Fudenberg D, Maskin E. The folk theorem in repeated games with discounting or with incomplete information. Econometrica. 1986;54(3):533–554. [Google Scholar]
- Gardner R, Ostrom E. Rule and games. Public Choice. 1991;70(2):121–149. [Google Scholar]
- Ginsburg PB, Grossman JM. When the price isn’t right: how inadvertent payment incentives drive medical care. Health Affairs. 2005;W5:376–384. doi: 10.1377/hlthaff.w5.376. [DOI] [PubMed] [Google Scholar]
- Ginsburg PB, Berenson RA. Revising Medicare’s Physician Fee Schedule–Much Activity, Little Change. New England Journal of Medicine. 2007;356:1201–1203. doi: 10.1056/NEJMp068272. [DOI] [PubMed] [Google Scholar]
- Griner PF. Changing the Health Care System: Models from Here and Abroad. Institute of Medicine; Washington D.C: 1994. The Rochester, New York experience; pp. 82–85. [Google Scholar]
- Hardin G. The tragedy of the commons. Science. 1968;162(5364):1243–1248. [PubMed] [Google Scholar]
- Hsiao WC, Braun P, Dunn D, Becker ER, DeNicola M, Ketcham TR. Results and policy implications of the resource-based relative value study. New England Journal of Medicine. 1988;319:881–888. doi: 10.1056/NEJM198809293191330. [DOI] [PubMed] [Google Scholar]
- Hurley J, Lomas J, Goldsmith LJ. Physician responses to global physician expenditure budgets in Canada: a common property perspective. Milbank Quarterly. 1997;75(3):343–364. doi: 10.1111/1468-0009.00059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iacus SM, King G, Porro G. Multivariate matching methods that are monotonic imbalance bounding. Journal of the American Statistical Association. 2011;106:345–361. [Google Scholar]
- Long SH, Marquis MS. Toward a global budget for the U.S. health system: implementation issues and information needs. [accessed December 7, 2010];RAND Issue Paper IP-143. 1994 http://www.rand.org/pubs/issue_papers/IP143.html.
- Lu JFR, Hsiao WC. Does universal health insurance make health care unaffordable? Lessons from Taiwan. Health Affairs. 2003;22(3):77–88. doi: 10.1377/hlthaff.22.3.77. [DOI] [PubMed] [Google Scholar]
- Mathematica. [accessed August 16, 2010];Global budgets for health care. 2009 http://www.mass.gov/Eeohhs2/docs/dhcfp/pc/2009_03_13_Global_Budgets_final-C5.pdf.
- Mattke S. Doctoral thesis. Harvard University; 2001. The effect of financial incentives and institutional arrangements on provider behavior. [Google Scholar]
- McGuire TG, Pauly MV. Physician response to fee changes with multiple payers. Journal of Health Economics. 1991;10(4):385–410. doi: 10.1016/0167-6296(91)90022-f. [DOI] [PubMed] [Google Scholar]
- Moran EF, Ostrom E. Seeing the Forest and the Trees: Human–Environment Interactions in Forest Ecosystems. MIT Press; Cambridge: 2005. [Google Scholar]
- Mougeot M, Naegelen F. Hospital price regulation and expenditure cap policy. Journal of Health Economics. 2005;24(1):55–72. doi: 10.1016/j.jhealeco.2004.04.007. [DOI] [PubMed] [Google Scholar]
- Myers RA, Worm B. Rapid worldwide depletion of predatory fish communities. Nature. 2003;423:280–283. doi: 10.1038/nature01610. [DOI] [PubMed] [Google Scholar]
- Olson M. The Logic of Collective Action: Public Goods and the Theory of Groups. Harvard University Press; Cambridge: 1965. [Google Scholar]
- Ostrom E, Gardner R, Walker J. Rules, Games, and Common-Pool Resources. University of Michigan Press; Ann Arbor: 1994. [Google Scholar]
- Pauly D, Christensen V, Guenette S, Pitcher TJ, Sumalia UR, Walters CJ, Watson R, Zeller D. Towards sustainability in world fisheries. Nature. 2002;418:689–695. doi: 10.1038/nature01017. [DOI] [PubMed] [Google Scholar]
- Redmon DP, Yakoboski PJ. The nominal and real effects of hospital budgets in France. Inquiry. 1995;32:174–183. [PubMed] [Google Scholar]
- Roberts MJ, Hsiao W, Berman P, Reich MR. Getting Health Reform Right: A Guide to Improving Performance and Equity. Oxford University Press; Oxford: 2004. [Google Scholar]
- Sack K. Mass. Panel backs radical shift in health payment. [accessed February 18, 2011];New York Times. 2009 Jul 16; http://www.nytimes.com/2009/07/17/health/policy/17masshealth.html.
- Schwartz FW, Glennerster H, Saltman RB, editors. Fixing Health Budgets: Experience from Europe and North America. John Wiley & Sons Ltd; Chichester: 1996. [Google Scholar]
- U.S. General Accounting Office. Health care spending control: the experience of France, Germany, and Japan. [accessed February 18, 2011];Report to Congressional Requesters. HRD-92-9. 1991 http://archive.gao.gov/d31t10/145301.pdf.
- Wolfe PR, Moran DW. Global budgeting in the OECD countries. Health Care Financing Review. 1993;14(3):55–76. [PMC free article] [PubMed] [Google Scholar]
- Yakoboski PJ, Ratner J, Gross DJ. The effectiveness of budget targets and capsin the German ambulatory care sector. Benefits Quarterly. 1994;10(3):31–37. [PubMed] [Google Scholar]
- Fukawa T, Izumida N. Japanese healthcare expenditure in a comparative context. The Japanese Journal of Social Security Policy. 2004;3(2):51–61. [Google Scholar]
- Newhouse JP. Pricing the Priceless: A Health Care Conundrum. MIT Press; Cambridge: 2002. [Google Scholar]
- Rosenberg SN, Allen DR, Handte JS, Jackson TC, Leto L, Rodstein BM, Stratton SD, Westfall G, Yasser R. Effect of utilization review in a fee-for-service health insurance plan. The New England Journal of Medicine. 1995;333(20):1326–1330. doi: 10.1056/NEJM199511163332006. [DOI] [PubMed] [Google Scholar]
- Wagstaff A, Barnum H. Policy Research Working Papers #WPS1044. The World Bank; Washington D.C: 1992. Hospital cost functions for developing countries. [Google Scholar]
- Agency for Healthcare Research and Quality (AHRQ) Guide to inpatient quality indicators: quality of care in hospitals—volume, mortality, and utilization. Version 3.1. Department of Health and Human Services; Rockville: 2007. [accessed September 8, 2010]. http://qualityindicators.ahrq.gov/downloads/iqi/iqi_guide_v31.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.