Abstract
Coronary artery calcification is a part of atherosclerosis process associated with coronary heart disease. Recently, coronary artery calcification assessment using computed tomography (CT) is still the best noninvasive imaging with high sensitivity and specificity. Osteoprotegerin (OPG) is one of vascular calcification marker that through its role to bind receptor activator of nuclear factor-κβ ligand and inhibit osteoclastogenesis is suspected of playing a role for coronary calcification in atherosclerosis process. The objective of this study was to prove a positive correlation between OPG serum level and coronary calcification using coronary artery calcium (CAC) score in patient with moderate–severe cardiovascular (CV) risk factor. This is a cross-sectional study with purposive sampling technique. Thirty-three subjects participate in this research and each subject underwent a multislice computed tomography (MSCT) examination to assess coronary calcification and their blood samples were collected for OPG measurement. This study is analyzed with Spearman's correlation test. The mean of OPG serum level in this study was 5.89 ± 2.1 pmol/L for moderate-risk Framingham risk score (FRS) and the mean of OPG serum level for high-risk FRS was 7.27 ± 3.4. There was a positive, moderate, and significant correlation between OPG serum level and coronary calcification using CAC score in patient with moderate–severe CV risk factor ( r = 0.694; p < 0.001).
Keywords: coronary artery, calcium score, osteoprotegerin, Framingham risk score, moderate–severe cardiovascular risk factor, atherosclerosis, coronary calcification
Atherosclerotic cardiovascular disease (ASCVD) is a chronic disorder developing insidiously throughout life and usually progressing to an advanced stage by the time symptoms occur. It remains the major cause of premature death in Europe, even though CVD mortality has fallen considerably over recent decades in many European countries. It is estimated that > 80% of all CVD mortality now occurs in developing countries. 1 2 3
The high cardiovascular (CV) mortality and morbidity need preventive strategy to decrease future CV events. One of them is CV risk stratification by Framingham Heart Study 2008. This risk stratification classified subjects become low, moderate, and high CV risk by several parameters (age, sex, hypertension history, low-density lipoprotein value, and smoking history). 4 5
Coronary artery calcification is a part of atherosclerosis development, exclusively happening in coronary artery and there is no such calcification in other normal wall vessels. 6 7 The presence of calcium in coronary artery lumen is diagnostic tools for coronary artherosclerosis. 8 9 10 Computed tomography (CT) is the only one noninvasive method with high sensitivity and specificity for detecting calcium deposit and calculating calcification level in coronary artery, then results coronary artery calcium (CAC) score and plaque burden level. The American College of Cardiology/American Heart Association 2013 recommended CAC scoring for moderate CV risk to reclassify the CV risk. 10
Recently, osteoprotegerin (OPG) is discovered as a subclinical atherosclerosis biomarker through several mechanisms. OPG is a soluble glycoprotein member of the tumor necrosis factor (TNF) receptor superfamily, originally discovered as an inhibitor osteoclastogenesis through the mechanism of RANK–RANKL (receptor activator of nuclear factor-κβ–receptor activator of nuclear factor-κβ ligand ) interaction in bone metabolism. OPG competes with RANK to bind RANKL. OPG also upregulates endothelial cell (EC) adhesion molecules in atherosclerosis development. 11 12
Therefore, we evaluated the correlation between the serum OPG level and CAC in those patients with moderate–severe CV risk based on Framingham risk score (FRS), by assessing CAC with CAC score.
Subject and Methods
From March 2016 to July 2016, we recruited 33 patients who met inclusion and exclusion criteria. Inclusion criteria were men or women, age between 35 and 65 years, having moderate–severe CV risk factors based on FRS (10–19 and ≥20% 10-year risk) with normal electrocardiogram (ECG) results. Exclusion criteria were ASCVD, pregnancy, patient with malignancy, presence of percutaneous coronary intervention or coronary artery bypass grafting history, patient with chronic inflammation disease, patient with immunosuppressant therapy, patient with ongoing heparin therapy, and presence of chronic kidney disease. This study was approved by our institutional review committee; the subjects were informed of the investigative nature of the study and a written consent was obtained before study entry.
Evaluation of Target Lesion Calcium Using Computed Tomography Scan and Coronary Artery Calcium Score
Evaluation of target lesion calcium was using GE Company MSCT scan machine having 128 slices. No special preparation for CAC scoring is required, other than abstinence from caffeine and cigarette 4 hours before scan to ensure optimized heart rate of 80 bpm. ECG electrodes were applied, scan preparation was completed, and the acquisition scan was performed requiring only a 20-second breath hold. The 45 to 65 images obtained were analyzed, then yielded total calcium score using Agatston–Janowitz's score. This total score is based on the scores of the five interrogated coronary arteries (left main, left anterior descending, left circumflex, right coronary, and posterior descending) which in turn represent the total number of calcified plaques in each artery. Each plaque is scored based on the lesion area and density.
Serum OPG Measurement
Blood samples were collected and stored at 20°C until the laboratory examination. The serum OPG levels were determined by using BioVendor's human OPG enzyme-linked immunosorbent assay (ELISA). First, 100 µL of diluted calibrators, quality controls, dilution buffer, and samples were incubated in a plate at room temperature (25°C), then was shaken in an orbital microplate shaker and washed in the well three times with wash solution. Next, 100 µL of biotin labeled anti-OPG antibody solution were added, then incubated at room temperature and shaken them, then washed again. Then 100 µL conjugate solution were added and met the same before treats. Then 100 µL of substrate solution were added and incubated the plate for 10 minutes at room temperature and stopped the color development by adding 100 µL of stop solution. The final process was determining the absorbance by reading the plate at 450 nm.
The mean value study with serum samples from young healthy donors that has been established with the human OPG ELISA was 4.1 ± 0.33 pmol/L. 13
Statistical Analysis
The results were expressed as means ± standard deviations or as medians, according to the variables. The normality data distribution test and Kolmogorov–Smirnov's test were done before evaluating correlation between OPG serum level and CAC score. Since abnormal data distribution, correlation analysis was done using Spearman's rank correlation test ( Table 1 ; Fig. 1 ).
Table 1. The plaque complexity level and cardiovascular risk according to CAC score.
| Calcium score | Plaque and cardiovascular disease risk |
|---|---|
| 0 | No identifiable plaque Very low cardiovascular disease risk |
| 1–10 | Minimal plaque burden Low cardiovascular disesase risk |
| 11–100 | Mild plaque burden Moderate cardiovascular disease risk |
| 101–400 | Moderate plaque burden Moderately high cardiovascular disease risk |
| > 400 | Extensive plaque burden High cardiovascular disease risk |
Abbreviation: CAC, coronary artery calcium.
Fig. 1.
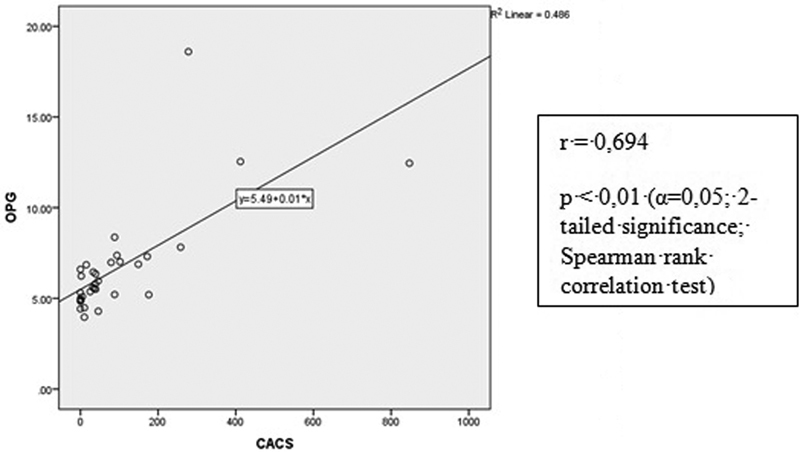
Correlational OPG serum level and CAC score. CAC, coronary artery calcium; OPG, osteoprotegerin.
Results
The study group included 17 men and 16 women, and their ages ranged from 35 to 65 years (mean age, 53.73 ± 6.90). The mean value of the body mass index was 25.48 ± 2.7. Dyslipidemia is the most common risk factor in this study group, 27 subjects (81.8%). There were 15 subjects (45.5%) with moderate CV risk and 18 subjects (54.5%) with severe CV risk. The characteristics of the subjects are given in Table 2 .
Table 2. Patients' characteristics of study group.
| Variable | n (%) or mean ± SD |
|---|---|
| Age (y) | 53.73 ± 6.90 |
| Sex | |
| Male | 17 (51.5) |
| Female | 16 (48.5) |
| Height (m) | 1.62 ± 0.08 |
| Weight (kg) | 66.85 ± 7.5 |
| Body mass index (kg/m 2 ) | 25.48 ± 2.7 |
| LDL value (mg/dL) | 137.52 ± 33.2 |
| Hypertension | 22 (66.7%) |
| DM | 17 (54.5%) |
| With DM therapy | 16 (94.1%) |
| Dyslipidemia | 27 (81.8%) |
| With dyslipidemia therapy | 22 (81.5%) |
| Smoking | 8 (24.2%) |
| Framingham risk score | |
| Moderate | 15 (45.5%) |
| Severe | 18 (54.5%) |
Abbreviations: DM, diabetes mellitus; LDL, low-density lipoprotein; SD, standard deviation.
The median CAC score was 38. The mean CAC score was higher at severe CV risk group than moderate CV risk group (126.56 ± 198.1 vs. 56.13 ± 108.7). The highest OPG serum level was 18.6 pmol/L and the median was 5.8 pmol/L. The mean OPG serum level was higher at severe CV risk group than moderate CV risk group (7.27 ± 3.4 vs. 5.89 ± 2.1) ( Tables 3 and 4 ).
Table 3. Descriptive analysis between FRS and CAC score.
| Variable |
Moderate FRS
n
(%)
Mean ± SD |
Severe FRS
n
(%)
Mean ± SD |
|---|---|---|
| CAC score (HU) | 56.13 ± 108.7 | 126.56 ± 198.1 |
| No plaque burden | 3 (20%) | 3 (16.7%) |
| Minimal | 4 (26.7%) | 2 (11.1%) |
| Mild | 6 (40.0%) | 7 (38.9%) |
| Moderate | 1 (6.7%) | 5 (27.8%) |
| Extensive | 1 (6.7%) | 1 (5.6%) |
Abbreviations: CAC, coronary artery calcium; FRS, Framingham risk score; SD, standard deviation.
Table 4. Descriptive analysis between OPG serum level and FRS.
| Variable |
Moderate FRS (
n
= 15)
Mean ± SD |
Severe FRS ( n = 18) Mean ± SD |
Median |
|---|---|---|---|
| OPG serum level (pmol/L) | 5.89 ± 2.1 | 7.27 ± 3.4 | 5.8 |
Abbreviations: FRS, Framingham risk score; OPG, osteoprotegerin; SD, standard deviation.
Note : The OPG serum levels were significantly positively correlated with CAC score ( p < 0.001; r = 0.694).
Discussion
Calcification is a frequent finding in advanced atherosclerosis with the process having similarities to bone remodeling. Several bone remodeling cytokines, in particular OPG, have been identified adjacent to areas of atheroma calcification. 12
OPG is expressed in vivo by ECs, vascular smooth muscle cells, and osteoblasts. OPG acts as a decoy substrate to RANKL and competes with RANK, inhibiting RANK–RANKL interactions. Binding of OPG to RANKL prevents the proliferation and differentiation of osteoclasts and consequently bone resorption even vascular calcification. 11
Inflammation plays an important role in the progression and complication of atherosclerosis and TNF-α is one of cytokine inflammation marker. Recent study demonstrated that OPG upregulates the expression of several adhesion molecule-1, vascular cells adhesion molecule-1, and E-selectin by ECs in TNF-α activated human umbilical vein ECs. 12
Recent study shows that OPG circulating levels are increased in patients with metabolic syndrome. In this study, we included subject with moderate–severe CV risk based on FRS and also showed that OPG serum level was higher in severe FRS group than in moderate FRS group.
Shaw et al, in their cohort study, showed CAC scoring was superior to FRS to estimate CV risk. 14 Greenland et al informed that CAC score exceed 100 was related with increasing CV risk (high CV risk) for patients with 10 to 15% or more group based on FRS. The 10 to 15% FRS group with CAC score exceed 300 have CV risk equal with > 20% FRS group with CAC score > 300. 5
In this study, there was three subjects with moderate FRS; no plaque and four subjects with moderate FRS; minimal plaque (CAC score 11–100); therefore, these subjects could be reclassified to be subjects with low CV risk. There was also one subject with moderate FRS; moderate plaque (CAC score 101–400) and one subject with moderate FRS; extensive plaque; therefore, these subjects could be reclassified to be subjects with high CV risk.
Thereby, this study was in accordance with the prior study, Anand et al explained that OPG serum level was correlated significantly with CAC score and carotid intima-media thickness in subjects with diabetes mellitus as one of risk factor for atherosclerosis. 15 Pérez de Ciriza et al concluded that OPG serum level was increased significantly in subjects with coronary artery calcification than subjects without coronary artery calcification. 16
In conclusion, OPG serum level was correlated significantly with CAC score in subjects with moderate–severe CV risk ( r = 0.694; p < 0.001). Our study also have some limitations, first, no limitation for ASCVD therapy (statin, oral antihypetension drugs, oral antidiabetic drugs) for subjects with that comorbid condition; second, this study included small number of participants. These data suggest that more research is needed to validate OPG as a CV damage or risk biomarker.
References
- 1.Laslett L J, Alagona P, Jr, Clark B A, IIIet al. The worldwide environment of cardiovascular disease: prevalence, diagnosis, therapy, and policy issues: a report from the American College of Cardiology J Am Coll Cardiol 201260(25, Suppl):S1–S49. [DOI] [PubMed] [Google Scholar]
- 2.Perk J, De Backer G, Gohlke H et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts) Eur Heart J. 2012;33(13):1635–1701. doi: 10.1093/eurheartj/ehs092. [DOI] [PubMed] [Google Scholar]
- 3.Kohli P, Whelton S P, Hsu S et al. Clinician's guide to the updated ABCs of cardiovascular disease prevention. J Am Heart Assoc. 2014;3(05):e001098. doi: 10.1161/JAHA.114.001098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharma R K, Sharma R K, Voelker D J et al. Cardiac risk stratification: role of the coronary calcium score. Vasc Health Risk Manag. 2010;6:603–611. doi: 10.2147/vhrm.s8753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Greenland P et al. ACCF/AHA Clinical Expert Consensus Document on Coronary Artery Calcium Score by Computed Tomography in Global Cardiovascular Risk Assessment and in Evaluation of Patients With Chest Pain. Circulation. 2007;115:402–426. doi: 10.1161/CIRCULATIONAHA..107.181425. [DOI] [PubMed] [Google Scholar]
- 6.Budoff M J, Gul K M. Expert review on coronary calcium. Vasc Health Risk Manag. 2008;4(02):315–324. doi: 10.2147/vhrm.s1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gerber T C.Diagnostic and Prognostic Implications of Coronary Artery Calcification Detected by Computed Tomography. 2014Available at:www.uptodate.com. Accessed on January 13, 2017
- 8.Mollet N R, Cademartiri F, de feyter P J. Non-invasive multislice CT coronary imaging. Heart. 2005;91:401–407. doi: 10.1136/hrt.2004.034009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Romanens M J, Bergerb D C, Battegay E J. Predictive value of clinical risk assessment tools and guidelines for 10-year coronary heart disease risk in practice-based primary care. Kardiovaskuläre Medizin. 2005;8:180–186. [Google Scholar]
- 10.Madhavan M V, Tarigopula M, Mintz G S, Maehara A, Stone G W, Généreux P. Coronary artery calcification: pathogenesis and prognostic implications. J Am Coll Cardiol. 2014;63(17):1703–1714. doi: 10.1016/j.jacc.2014.01.017. [DOI] [PubMed] [Google Scholar]
- 11.Venuraju S M, Yerramasu A, Corder R, Lahiri A. Osteoprotegerin as a predictor of coronary artery disease and cardiovascular mortality and morbidity. J Am Coll Cardiol. 2010;55(19):2049–2061. doi: 10.1016/j.jacc.2010.03.013. [DOI] [PubMed] [Google Scholar]
- 12.Mangan S H, Van Campenhout A, Rush C, Golledge J. Osteoprotegerin upregulates endothelial cell adhesion molecule response to tumor necrosis factor-α associated with induction of angiopoietin-2. Cardiovasc Res. 2007;76(03):494–505. doi: 10.1016/j.cardiores.2007.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Naylor K E, Rogers A, Fraser R B, Hall V, Eastell R, Blumsohn A. Serum osteoprotegerin as a determinant of bone metabolism in a longitudinal study of human pregnancy and lactation. J Clin Endocrinol Metab. 2003;88(11):5361–5365. doi: 10.1210/jc.2003-030486. [DOI] [PubMed] [Google Scholar]
- 14.Shaw L J, Raggi P, Schisterman E, Berman D S, Callister T Q. Prognostic value of cardiac risk factors and coronary artery calcium screening for all-cause mortality. Radiology. 2003;228:826–833. doi: 10.1148/radiol.2283021006. [DOI] [PubMed] [Google Scholar]
- 15.Anand D V, Lahiri A, Lim E et al. The relationship between plasma osteoprotegerin levels and coronary artery calcification in uncomplicated type 2 diabetic subjects. J Am Coll Cardiol. 2006;47(09) doi: 10.1016/j.jacc.2005.12.054. [DOI] [PubMed] [Google Scholar]
- 16.Pérez de Ciriza C, Moreno M, Restituto P et al. Circulating osteoprotegerin is increased in the metabolic syndrome and associates with subclinical atherosclerosis and coronary arterial calcification. Clin Biochem. 2014;47(18):272–278. doi: 10.1016/j.clinbiochem.2014.09.004. [DOI] [PubMed] [Google Scholar]


