Abstract
Emotional reactivity is theorized to contribute to both eating disorders (ED) and nonsuicidal self-injury (NSSI). Although EDs and NSSI frequently co-occur, no study has examined emotional reactivity in individuals with both conditions. This study examined the following hypotheses in a large clinical sample (N=648): (1) patients with co-occurring ED and NSSI would report higher emotional reactivity and more severe clinical characteristics; (2) among those with EDs, patients with bulimia nervosa (BN) would be more likely to report NSSI and evidence the highest emotional reactivity; and (3) higher emotional reactivity would be associated with worse treatment outcomes. Data were collected at admission and discharge from inpatient, partial hospitalization, and intensive outpatient treatment programs for ED or NSSI. The NSSI-only and co-occurring groups reported significantly higher emotional reactivity than the ED-only group. Among those with EDs, individuals with BN reported higher emotional reactivity and were more likely to engage in NSSI compared to those with anorexia nervosa. Emotional reactivity was inconsistently related to treatment outcomes among the co-occurring and ED-only groups. Results highlight the importance of emotional reactivity in clinical presentation, particularly when NSSI is present.
Keywords: Emotional reactivity, Eating disorders, Nonsuicidal self-injury, Treatment outcome
1. Introduction
Eating disorders (EDs) and nonsuicidal self-injury (NSSI) are two maladaptive behaviors with substantial co-occurrence that represent significant mental and physical health concerns (Cucchi et al., 2016; Kostro et al., 2014). Among those with EDs, a recent meta-analysis reported a lifetime history of NSSI of 32.7% among those with bulimia nervosa (BN) and 27.3% among those with anorexia nervosa (AN) (Cucchi et al., 2016). Among those with NSSI, one study found 19.4% of participants with a history of NSSI also experience ED symptoms (Muehlenkamp et al., 2012), while another study found 29.9% of people being treated for NSSI engaged in binging, purging, or food restriction (Washburn et al., 2015).
The co-occurrence of these disorders has led to attempts to identify shared risk factors. Both EDs and NSSI are associated with a range of emotion regulation deficits (e.g., Klonsky, 2007; Lavender et al., 2015). Similarly, Muehlenkamp et al. (2012) found that emotion regulation deficits were associated with both ED and NSSI behaviors, and levels of emotion dysregulation and depression were highest among those who reported both behaviors. Thus far, however, it remains unclear if there are predisposing factors underlying emotion regulation deficits and the co-occurrence of EDs and NSSI (Claes and Muehlenkamp, 2013).
Emotional reactivity has recently been theorized as a risk factor for the development and maintenance of co-occurring ED and NSSI (Claes and Muehlenkamp, 2013). Emotional reactivity refers to the strength and duration with which positive and negative emotions are experienced (Davidson, 2000; Nock et al., 2008; Rothbart and Derryberry, 1981). Heightened emotional reactivity may contribute to the development and maintenance of behavioral problems, such as EDs and NSSI, that are associated with broader emotional regulation deficits (Claes, 2014; Chapman, 2012; Nock et al., 2008). That is, individuals who are predisposed to experience emotions as more aversive and intolerable may resort to more extreme, maladaptive coping responses to regulate emotions.
Emotional reactivity is distinct from related emotional regulation constructs such as impulsivity, inhibitory control, and negative urgency. Whereas emotional reactivity refers to a subjective experience of emotions, impulsivity refers a range of cognitive and behavioral responses to stimuli without forethought or regard for consequences (Evenden, 1999). Negative urgency specifically refers to the tendency to act impulsively while experiencing extreme negative emotions (Cyders and Smith, 2008). In contrast to impulsivity and negative urgency, inhibitory control reflects the capacity to override prepotent cognitive or behavioral responses that are inconsistent with goal-directed behavior (Diamond, 2013). Thus, individuals who are prone to elevated emotional reactivity may also exhibit elevations in impulsivity and negative urgency, and decreased inhibitory control, ultimately contributing to maladaptive coping responses to seek immediate relief from emotional distress. Previous research supports this conceptualization, finding emotional reactivity positively associated with behavioral inhibition but negatively associated with attentional and behavioral control (Carol et al., 2014; Claes et al., 2014; Klonsky et al., 2003; Nock et al., 2008).
1.1.Emotional reactivity in NSSI and EDs
Emotional reactivity has been implicated in both EDs and NSSI. Several studies have found that emotional reactivity is elevated among people who engage in NSSI (e.g., Franklin et al., 2012; Klonsky et al., 2003; Glenn et al., 2011). With respect to EDs, few studies have specifically examined emotional reactivity. For example, two studies examined emotional reactivity with ED samples using the Emotion Reactivity Scale (ERS; Nock et al., 2008). The initial validation study of the ERS found emotional reactivity elevated across psychiatric diagnoses; however, scores were highest among the small subsample (n=6) of patients with EDs (Nock et al., 2008). Claes et al. (2014) also found higher ERS scores among high school students with ED symptoms compared to those without these symptoms. In contrast to Nock et al. (2008), students with symptoms of NSSI had higher rates of ERS total scores than those with ED symptoms. In addition, a recent study found emotional reactivity, as measured through an experimental procedure, to be higher in BN than AN (Tapajoz et al., 2015).
1.2.The present study
Despite recent interest in both emotional reactivity (Lannoy et al., 2014) and the co-occurrence of ED and NSSI (Claes and Muehlenkamp, 2013), little is known about emotional reactivity in co-occurring ED and NSSI. While a theoretical model has identified emotional reactivity as a risk factor for co-occurring ED and NSSI (Claes and Muehlenkamp, 2013), and prior studies demonstrated that individuals with co-occurring ED and NSSI experience maladaptive emotion regulation (Claes et al., 2014), it is unclear if emotional reactivity differs between individuals with only ED, those with only NSSI, and those with co-occurring ED and NSSI. Indeed, emotional reactivity may be additive in co-occurring ED and NSSI; alternatively, emotional reactivity may be similarly elevated across these groups, which could suggest it is a more general than specific risk factor. To date, however, no study has compared levels of emotional reactivity between these groups or assessed how emotional reactivity influences treatment. If heightened reactivity is related to a worse prognosis, this may indicate a need to more specifically target emotion regulation skills during treatment (Wonderlich et al., 2014).
The primary aim of the present study was to address these gaps by examining emotional reactivity and other relevant domains in a large clinical sample of patients categorized into ED-only, NSSI-only, and co-occurring ED and NSSI groups. First, we compared emotional reactivity between these groups, hypothesizing that patients with co-occurring NSSI and ED would evidence higher emotional reactivity than those with ED-only or NSSI-only. Second, we examined whether these groups differed in condition-specific psychopathology (i.e., overall ED psychopathology and NSSI frequency) and quality of life. While worse quality of life is associated with EDs and NSSI (e.g., Agh et al., 2016; Ammerman, et al., 2017) and may convey a more severe clinical presentation, quality of life has not been investigated among those with both ED and NSSI. Based on an additive model of psychopathology, we expected that the co-occurring group would exhibit greatest severity condition-specific psychopathology and impairment in quality of life. Third, we assessed whether emotional reactivity is associated with treatment outcomes (i.e., changes in ED or NSSI frequency) in these groups. We predicted higher emotional reactivity at admission would be associated with worse treatment outcomes, and that diagnostic grouping would moderate this association such that those with co-occurring ED and NSSI would evidence worse outcomes.
As a secondary aim, we examined differences in ERS scores and NSSI frequency among those with EDs. We hypothesized that among individuals with EDs, those with BN would exhibit greater NSSI frequency and emotional reactivity compared to those with AN (Tapajoz et al., 2015).
2. Methods
2.1. Procedures
Data for this study were obtained from databases developed for clinical and organizational improvement purposes at a large non-profit hospital providing inpatient, partial hospitalization, and intensive outpatient treatment specifically for ED and/or NSSI. Patients completed measures at admission and discharge as part of routine clinical outcome assessment. Age, sex, and ethnicity were obtained from electronic medical records. Clinical diagnoses were provided at admission and confirmed at discharge by attending psychiatrists who specialize in ED and NSSI. All data were de-identified prior to analysis, and all study protocols were reviewed and found exempt by the hospital’s Institutional Review Board.
2.2. Participants
The initial sample consisted of 660 patients from inpatient, partial hospitalization, and intensive outpatient programs for ED and NSSI. Participants were grouped into three categories: ED-only, NSSI-only, or co-occurring ED and NSSI based on a combination of patients’ admission program (i.e., ED or NSSI) and data from clinical assessments administered at the time of admission. Specifically, “ED-only” included patients admitted to the ED program with a primary ED who denied ever engaging in NSSI; “NSSI-only” included patients admitted to the NSSI program with primary NSSI without a diagnosis of ED (i.e., AN, BN, Eating Disorder NOS [EDNOS], Binge Eating Disorder [BED]); and “co-occurring ED and NSSI” included patients admitted to the ED program with primary ED who also endorsed engaging in NSSI at least once in their lifetime, as well as patients admitted to the NSSI program with primary NSSI and diagnosed with an ED. Three patients were missing admission data, and were grouped according to their discharge program and discharge assessments. If patients had multiple episodes of care, they were grouped based on the data from their first admission and the earliest admission data (i.e., first episode of care) and latest discharge data (i.e., last episode of care) were used in all subsequent analyses. One patient was missing admission data but was identified as having a subsequent episode of care; for this patient the second admission data were used to establish group membership and for subsequent analyses. Additionally, eight patients were transferred between programs; of these, four were transferred between programs during a single episode of care (one of whom also had multiple episodes of care), and four patients had multiple distinct episodes of care in both ED and NSSI programs; all of these patients were classified as “co-occurring ED and NSSI.” Twelve patients in the ED program were missing NSSI data and were excluded from the sample.
The final sample (N=648) was 85.8% female, with 28 individuals (4.3%) missing sex data. The sample included 172 participants identified as ED-only, 319 participants identified as NSSI only, and 157 participants identified as co-occurring ED and NSSI (79 with primary ED; 78 with primary NSI). The ED-only and co-occurring ED and NSSI groups included patients with AN (n=63), BN (n=58), BED (n=17), and EDNOS (n=191). Of the 648 patients, 60.9% completed discharge assessments.
Pearson Chi-square analysis (χ2[2]=14.90, p=0.001) indicated a significant association between group membership and sex, such that the proportion of males was significantly higher in the NSSI-only group (14.7% male) compared to the co-occurring group (3.3% male). Age ranged from 12 to 67 years (M=21.04; SD=10.39). An ANOVA indicated age differed significantly by group (F[2, 617]=36.66, p<0.001); post-hoc analyses indicated the mean age of the ED-only group (M=26.43, SD=13.63) was significantly greater than the co-occurring group (M=20.85, SD=8.98), both of which were significantly older than the NSSI-only group (M=18.26, SD=7.59). Of those who reported their ethnicity (n=515; 79.5%), the majority (70.1% of total sample) identified as non-Hispanic white, while the remaining identified as Hispanic (5.9%), Asian (0.8%), African American (1.4%), American Indian (0.6%), “other” (0.6%), or “multiple” (0.2%). A chi-square analysis assessed group membership among non-Hispanic white participants and participants who identified as ethnicities other than non-Hispanic white; results found no significant association between group membership and ethnicity, χ2(2)=1.21, p=0.547.
2.3. Measures
2.3.1 Emotion Reactivity Scale (ERS)
The ERS is a self-report measure of emotion sensitivity, intensity, and persistence. Exploratory and confirmatory factor analyses have found support for single- and three factor models (Claes et al., 2014; Lannoy et al., 2014; Nock et al., 2008). The ERS has demonstrated good convergent, divergent, and criterion-related validity (Nock et al., 2008). For this study, the internal consistency was excellent for the ERS total scale (α=0.96).
2.3.2 Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q), Short Form
The Q-LES-Q-SF is a 16-item measure of quality of life in populations with mental disorders with good internal consistency (α=0.90), test-retest reliability (κ=0.93), and validity (Stevanovic, 2011). The raw score of the Q-LES-Q-SF was converted to a percentage of the maximum total score possible, with a range from 0 to 100, with higher scores indicating greater quality of life. For this study, the internal consistency of the percent maximum total score was sufficient (α=.0.87).
2.3.3 NSSI Frequency
NSSI frequency was assessed by the Alexian Brothers Weekly Treatment Monitoring Form (ABWTM), which is an eight-question measure that includes an assessment of the frequency of NSSI in the last week, measured through the question, “How many times did you intentionally (on purpose) injure or hurt yourself in the last week?” with a 5-point ordinal response scale (i.e., no NSSI; 1–3 times; 3–5 times; 5–10 time; and >10 times).
2.3.4 Eating Disorder Examination Questionnaire (EDE-Q) version 6.0
The EDE-Q is the self-report version of the Eating Disorder Examination interview, yielding four subscale scores (i.e., eating concerns, shape concerns, weight concerns, and restraint) and a global score of ED symptom severity. The present study included the global score, which had a Cronbach’s alpha of 0.94.
All participants completed measures of emotional reactivity (ERS), quality of life (QLES), and condition-specific psychopathology (i.e., NSSI frequency, EDE-Q global) upon admission. At discharge, all participants completed the QLES; participants with primary NSSI completed the NSSI frequency assessment, and participants with primary ED completed the EDE-Q.
2.4. Statistical analyses
2.4.1. Primary aims
We examined differences between the ED-only, NSSI-only, and co-occurring groups in emotional reactivity (i.e., ERS total score) and quality of life assessed at admission using Generalized Linear Models (GLM). GLMs were also conducted for condition-specific dependent measures (i.e, EDE-Q global score and NSSI frequency) within condition-specific groups, such that EDE-Q global scores were compared between the ED-only and co-occurring groups, and NSSI frequency was compared between the NSSI-only and co-occurring groups. GLMs for NSSI frequency were conducted with negative binomial distributions, which accounted for non-normal distributions of these dependent variables. Age and sex were included as covariates in each GLM given that groups differed on these variables. Main effects of group were assessed with Wald chi-square tests; significant effects were followed up with pairwise comparisons using LSD adjustments.
Treatment outcomes were operationalized as quality of life (QLES), ED severity (i.e., EDE-Q global score), and NSSI frequency. GLMs were conducted determine if continuous outcomes (i.e., discharge levels of QLES, EDE-Q global scores, NSSI frequency1) could be predicted as a function of admission ERS scores, group membership, and their possible interaction. For dependent variables with non-normal distributions (i.e., NSSI frequency), GLMs with a gamma link function were used. Missing data at discharge were imputed using the expectation maximization (EM) algorithm. Each GLM equations estimated co-varied for length of stay (i.e., total treatment days), sex, age, and admission scores of the outcome variable. Admission ERS scores, group membership (i.e., ED-only, NSSI-only, co-occurring), and the interaction of ERS and group were entered as independent predictors of each outcome variable.
2.4.2. Secondary aims
Among those with EDs, a GLM was conducted to examine differences in ERS total scores between ED diagnoses (i.e., AN, BN, BED, and EDNOS), group (i.e., ED-only and co-occurring groups), and their possible interaction. A Pearson Chi-square test also compared the proportion of participants in each ED diagnostic category who reported engaging in NSSI.
Statistical analyses were performed using SPSS version 22.0.
3. Results
3.1. Descriptive information
One-way ANOVAs compared the number and duration of episodes of care per person between each group. Results indicated that the total number of episodes of care per person (M=1.78, SD=.75) did not differ significantly between groups, F(2, 645)=2.22, p=0.11. The total length of stay (days) was significantly higher among individuals in the ED-only group (M=18.78, SD=12.47) compared to the co-occurring group (M=16.19, SD=12.02), both of which had longer lengths of stay compared to the NSSI-only group (M=12.88, SD=9.04), F(2, 562)=15.06, p<0.001. The proportion of patients who had discharge data did not differ between by group, or by specific ED diagnoses. No significant differences were found between patients who did and did not have discharge data for sex, age, race/ethnicity, length of stay, or number of episodes of care.
3.2. Primary aims
3.2.1. Group differences in emotional reactivity at admission
Table 1 displays descriptive statistics and GLM results for comparisons among the ED-only, NSSI-only, and co-occurring groups at admission. The GLM comparing ERS-total scores demonstrated a significant effect of group, such that pairwise comparisons indicated that the means of the co-occurring (M=2.26, SD=0.94) and NSSI-only groups (M=2.21, SD=0.94) were significantly higher than the ED-only group (M=1.80, SD=1.04); ERS means for the co-occurring and NSSI-only groups did not differ significantly from each other.
Table 1.
Admission descriptive statistics and Generalized Linear Model (GLM) results
|
|
|
||||||
|---|---|---|---|---|---|---|---|
| ED-only1 | NSSI- only2 |
Co- occurring 3 |
GLM group effects | ||||
|
|
|||||||
| Measure | M (SD) | M (SD) | M (SD) | N | Wald χ2 |
p | Pairwise comparison |
|
|
|
||||||
| ERS-total | 1.80 | 2.19 | 2.26 | 620 | 26.20 | <0.001 | 2,3>1 |
| (1.04) | (0.94) | (0.94) | |||||
| QLES | 53.41 | 51.97 | 47.15 | 609 | 15.30 | <0.001 | 1>2,3 |
| (20.31) | (16.81) | (17.90) | |||||
| EDE-Q | 3.68 | --- | 4.22 | 239 | 6.75 | 0.009 | 3>1 |
| (1.46) | (1.20) | ||||||
| NSSI frequency | --- | 2.17 | 2.28 | 377 | 0.69 | 0.407 | |
| (1.19) | (1.10) | ||||||
Note. Each GLM included age and gender as covariates. Pairwise comparisons were made with LSD adjustments. ERS= Emotion Reactivity Scale; QLES=Quality of Life Enjoyment and Satisfaction Scale; EDE-Q=Eating Disorder Examination-Questionnaire; NSSI=Nonsuicidal self-injury.
3.2.2. Group differences in condition-specific psychopathology and quality of life at admission
GLM results indicated significant effects of group for QLES scores in the total sample. Pairwise comparisons indicated that the co-occurring and NSSI-only groups reported lower QLES scores than the ED-only group, although the NSSI-only group did not differ significantly from the co-occurring group.
Among participants with primary ED, GLM results also showed an effect of group for EDE-Q global scores, such that the co-occurring group reported higher overall ED psychopathology than the ED-only group. With respect to participants with primary NSSI, there were no significant differences in NSSI frequency between the co-occurring and NSSI-only groups.
3.2.3. Associations between emotional reactivity, group, and treatment outcomes
Results of separate GLM models predicting discharge QLES, NSSI frequency, and EDE-Q global scores from admission ERS scores, group membership, and their interaction are shown in Table 2. Across the total sample, a significant group effect was observed for QLES scores at discharge, in that the ED-only group evidenced higher scores compared to the co-occurring and NSSI-only groups, which did not differ significantly from each other in QLES scores at discharge; however neither admission ERS scores nor the interaction of group and ERS scores were significant predictors of discharge QLES scores after adjusting for covariates (i.e., age, sex, length of stay, and admission level of QLES). In addition, main effects of age and treatment days indicated that younger participants and those with shorter lengths of stay evidenced higher QLES at discharge.
Table 2.
Generalized Linear Models (GLM) predicting treatment outcomes from admission ERS scores and group membership
|
|
||||||||
|---|---|---|---|---|---|---|---|---|
| 95% Confidence interval |
||||||||
| Outcome (model) |
Program (n) |
B | SE | Lower | Upper | χ2 (1) | p | |
| QLES (GLM) | ED and NSSI | Intercept | 56.05 | 4.43 | 47.37 | 64.73 | 160.10 | <0.001 |
| (n=556) | Age | −0.17 | 0.06 | −0.29 | −0.06 | 8.38 | 0.004 | |
| Sex (male) | 2.39 | 1.94 | −1.40 | 6.19 | 1.53 | 0.217 | ||
| Treatment days | −0.11 | 0.05 | −0.22 | −0.01 | 4.75 | 0.029 | ||
| Admission QLES | 0.22 | 0.03 | 0.16 | 0.29 | 42.45 | <0.001 | ||
| Admission ERS-total | 0.61 | 1.24 | −1.81 | 3.03 | 0.25 | 0.620 | ||
| Group: ED-only | 7.79 | 3.69 | 0.56 | 15.01 | 4.46 | 0.035 | ||
| Group: NSSI-only | 0.69 | 3.66 | −6.48 | 7.86 | 0.04 | 0.850 | ||
| Admission ERS × ED-only group | −1.67 | 1.60 | −4.80 | 1.47 | 1.09 | 0.297 | ||
| Admission ERS × NSSI-only group | −0.01 | 1.50 | −2.94 | 2.92 | <0.001 | 0.994 | ||
| NSSI | NSSI | Intercept | 0.56 | 0.08 | 0.41 | 0.72 | 48.70 | <0.001 |
| frequency (GLM) | (n=340) | Age | 0.01 | <0.001 | <0.001 | 0.01 | 13.97 | <0.001 |
| Sex (male) | −0.02 | 0.03 | −0.08 | 0.04 | 0.34 | 0.562 | ||
| Treatment days | <0.001 | <0.001 | <0.001 | 0.01 | 13.38 | <0.001 | ||
| Admission NSSI frequency | 0.03 | 0.01 | 0.01 | 0.04 | 9.60 | 0.002 | ||
| Admission ERS-total | 0.02 | 0.03 | −0.03 | 0.07 | 0.61 | 0.434 | ||
| Group: NSSI-only | −0.01 | 0.07 | −0.15 | 0.13 | 0.02 | 0.896 | ||
| Admission ERS × NSSI-only group | <0.001 | 0.03 | −0.06 | 0.06 | <0.001 | 0.977 | ||
| EDE-Q global (GLM) | ED | Intercept | 1.39 | 0.45 | 0.52 | 2.26 | 9.71 | 0.002 |
| (n=221) | Age | 0.01 | 0.01 | <0.001 | 0.02 | 2.58 | 0.108 | |
| Sex (male) | 0.69 | 0.28 | 0.14 | 1.24 | 5.96 | 0.015 | ||
| Treatment days | −0.02 | 0.01 | −0.03 | −0.01 | 8.55 | 0.003 | ||
| Admission EDE-Q global | 0.35 | 0.06 | 0.24 | 0.46 | 40.80 | <0.001 | ||
| Admission ERS-total | −0.29 | 0.12 | −0.53 | −0.06 | 5.87 | 0.015 | ||
| Group: ED-only | −0.98 | 0.33 | −1.62 | −0.33 | 8.82 | 0.003 | ||
| Admission ERS × ED-only group | 0.34 | 0.14 | 0.06 | 0.62 | 5.74 | 0.017 | ||
Note. ERS=Emotional Reactivity Scale (ERS) total score; QLES=Quality of Life Enjoyment and Satisfaction Scale; EDEQ-G=Eating Disorder Examination Questionnaire (EDEQ) global score; NSI=nonsuicidal self-injury; ED=eating disorder. Reference groups for sex and group were coded as females and co-occurring groups, respectively.
For participants with primary NSSI, the GLM estimating discharge NSSI frequency indicated that older participants and those with longer treatment evidenced higher NSSI frequency at discharge; however no other effects were significant.
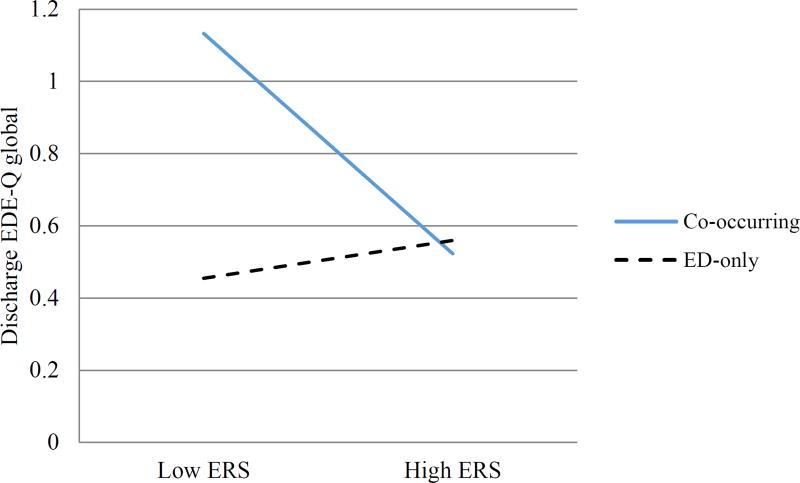
With respect to EDE-Q global scores among participants with primary ED, GLM results demonstrated significant effects of admission ERS scores, group, and their interaction. As depicted in Figure 1, among those with co-occurring ED and NSSI, lower ERS scores at admission were associated with higher discharge EDE-Q global scores after controlling for other covariates; however, this relationship was not observed among those in the ED-only group. Additionally, main effects of sex and treatment days indicated older participants and those with shorter lengths of stay reported higher overall ED psychopathology at discharge.
Figure 1.
EDE-Q global scores at discharge based on levels of emotional reactivity and group membership. Note. EDE-Q=Eating Disorder Examination-Questionnaire; ERS=Emotional Reactivity Scale; co-occurring=co-occurring ED and NSSI group; ED-only=ED-only group. Analyses co-varied for admission EDE-Q global scores, age, sex, and treatment duration.
3.3. Secondary aims
3.3.1. Differences in emotional reactivity between ED diagnoses
The ERS total score means for specific ED diagnoses (AN, BN, BED, and EDNOS) in the ED-only and co-occurring groups are shown in Table 3. GLM results (Table 4) showed significant effects for ED diagnosis and group, but not the interactions of ED diagnosis and group. Pairwise comparisons indicated that across the ED-only and co-occurring groups, participants with BN evidenced higher ERS scores than those with AN. Across all ED diagnoses, those with co-occurring NSSI reported higher ERS scores than those with only ED.
Table 3.
Descriptive statistics and pairwise comparisons of ERS total scores by eating disorder diagnosis and group status
| Group | Diagnosis | n | M | SD | Pairwise comparisons |
|---|---|---|---|---|---|
| ED-only | AN | 48 | 1.50 | 0.96 | BN>AN |
| BN | 33 | 2.30 | 1.09 | Co-occurring>ED-only | |
| BED | 16 | 1.76 | 1.06 | ||
| EDNOS | 73 | 1.79 | 0.99 | ||
|
|
|||||
| Co-occurring | AN | 15 | 2.07 | 1.10 | |
| BN | 25 | 2.34 | 0.88 | ||
| BED | 1 | 2.95 | --- | ||
| EDNOS | 116 | 2.27 | 0.94 | ||
Note. ERS= Emotion Reactivity Scale; ED=eating disorder; AN=anorexia nervosa; BN=bulimia nervosa; BED=binge eating disorder; EDNOS=eating disorder not otherwise specified.
Table 4.
Generalized Linear Models (GLM) estimating admission ERS scores from ED diagnosis and group membership
|
|
||||||||
|---|---|---|---|---|---|---|---|---|
| 95% Confidence interval |
||||||||
| Outcome | Program (n) | B | SE | Lower | Upper | χ2 (1) | p | |
| ERS | ED and NSSI | Intercept | 1.56 | 0.27 | 1.03 | 2.09 | 33.58 | <0.001 |
| (n=314) | Age | 0.00 | 0.00 | −0.01 | 0.01 | 0.11 | 0.742 | |
| Sex (male) | 0.20 | 0.23 | −0.25 | 0.66 | 0.77 | 0.382 | ||
| Group: Co-occurring | 0.48 | 0.15 | 0.18 | 0.77 | 10.20 | 0.001 | ||
| ED diagnosis: BED | 0.05 | 0.29 | −0.52 | 0.61 | 0.03 | 0.871 | ||
| ED diagnosis: BN | 0.52 | 0.20 | 0.12 | 0.92 | 6.47 | 0.011 | ||
| ED diagnosis: AN | −0.32 | 0.18 | −0.68 | 0.04 | 3.06 | 0.080 | ||
| Co-occurring group X BED | 0.62 | 1.00 | −1.35 | 2.58 | 0.38 | 0.540 | ||
| Co-occurring group X BN | −0.47 | 0.30 | −1.05 | 0.11 | 2.50 | 0.114 | ||
| Co-occurring group X AN | 0.12 | 0.32 | −0.51 | 0.75 | 0.13 | 0.714 | ||
Note. ERS= Emotion Reactivity Scale; ED=eating disorder; AN=anorexia nervosa; BN=bulimia nervosa; BED=binge eating disorder. Co-occurring group=ED and NSSI group. Reference groups for sex, co-occurring group, and ED diagnosis were coded as females, ED-only group, and eating disorder not otherwise (EDNOS), respectively.
3.3.2. Differences in NSSI between ED diagnoses
Results of a chi-square test demonstrated that the proportion of individuals who endorsed NSSI differed significantly between ED diagnostic groups, χ2(3)=11.47, p=0.009; the proportions of individuals who endorsed NSSI within the EDNOS, BN, AN, and BED groups were 56.0%, 26.2%, 16.7% and 1.2%, respectively.
4. Discussion
A growing body of literature has highlighted the co-occurrence of ED and NSSI, with emotional reactivity implicated as one of the shared vulnerabilities underlying both conditions (Claes et al., 2014; Nock et al., 2008). No study, however, has examined emotional reactivity in samples with co-occurring ED and NSSI. The present study addressed gaps in the literature by using a large sample of patients treated for ED or NSSI to examine the following primary hypotheses: (1) participants with co-occurring ED and NSSI would exhibit higher emotional reactivity than those with ED-only or NSSI-only, (2) those with co-occurring ED and NSSI would evidence more severe psychopathology and worse quality of life than those with ED-only or NSSI-only, and (3) higher emotional reactivity and the co-occurrence of ED and NSSI would be related to worse treatment outcomes. In addition, we expected that among individuals with EDs, those with BN would be more likely to engage in NSSI and evidence higher reactivity than those with AN.
4.1. Group differences in emotional reactivity
Results partially supported the first hypothesis. The co-occurring group and the NSSI-only groups evidenced significantly higher emotional reactivity than the ED-only group; however, there was no significant difference between the co-occurring and NSSI-only groups. Greater emotional reactivity among those with NSSI, when compared to those with only EDs, is consistent with Claes et al. (2014) but contrary to Nock et al. (2008); however, neither study directly compared emotional reactivity between the two groups nor examined co-occurring conditions. These findings underscore the clinical severity associated with the presence of NSSI, regardless of the presence of an ED, highlighting the relative importance of emotional reactivity in understanding NSSI.
4.2. Group differences in condition-specific psychopathology and quality of life
Among participants with primary ED, the co-occurring group reported greater overall ED psychopathology than the ED-only group. Among participants with primary NSSI, however, there were not significant differences in NSSI frequency between co-occurring and NSSI-only groups. These findings suggest that the presence of co-occurring NSSI has an additive influence of ED symptom severity, whereas the presence of co-occurring ED may not exacerbate severity of NSSI. A similar pattern was found when examining quality of life. Both the NSSI-only and co-occurring groups reported worse quality of life than the ED-only group. Taken together, the findings for condition-specific psychopathology and quality of life suggest that NSSI may be an indicator of greater severity more broadly when compared to ED without co-occurring NSSI.
4.3. Associations between emotional reactivity, group, and treatment outcomes
Results indicate that participants in the ED-only group evidenced better quality of life at the end of treatment compared to NSSI-only and co-occurring groups, even after adjusting for group differences in quality of life at admission. This finding suggests that the presence of NSSI, regardless of being primary or secondary to ED, impedes improvement in functional impairments during treatment. Although ED is a challenging condition to treat, demonstrating some of the lowest response rates of any conditions (Hofmann et al., 2012), very little is known about the response of NSSI to treatment. This study suggests that NSSI may be even especially challenging treat as a primary condition, as well as complicating treatment for other co-occurring conditions.
Contrary to our hypothesis, lower emotional reactivity was related to higher levels of ED psychopathology at discharge among those in the co-occurring group. At higher levels of emotional reactivity, the presence of NSSI was associated with more improvement in overall ED symptoms; however, for those with only ED, relative levels of emotional reactivity do not appear to be associated with changes in ED symptoms. Additionally, for the ED-only group but not the co-occurring group, higher emotional reactivity at admission was associated with decreased treatment response with respect to the frequency of bulimic episodes, in that this group evidenced higher frequencies at discharge relative to the co-occurring group.
While the reasons for these findings are unclear, one possible explanation is that those high in emotional reactivity who also engaged in NSSI responded better to a treatment approach that specifically targets emotion regulation deficits. These skills may have been particularly effective and well-matched to address ED-related psychopathology in those in the co-occurring group who evidenced higher reactivity. Additional research is necessary to replicate these findings, and if replicated, to better understand their implications.
Neither emotional reactivity, diagnostic group, nor their interaction predicted response to treatment with respect to NSSI frequency. Factors other than emotional reactivity likely played a more significant role in response to treatment for this outcome. For example, learning and using emotion regulation skills, which provide healthier alternatives for coping with negative emotions than NSSI behaviors, may be valuable targets for future studies examining moderators of NSSI symptom change.
4.4. Differences in emotional reactivity and NSSI between ED diagnoses
Consistent with hypotheses, emotional reactivity was significantly greater for the BN group compared to the AN group, and those with BN were more likely to report NSSI than those with other diagnoses. While Lavender and colleagues (2015) concluded that AN and BN do not appear to differ in behavioral control when distressed, our results are consistent with findings that BN is associated with higher emotional reactivity compared to AN (Tapajoz et al., 2015), that negative urgency is greater among people with binge eating behavior (Kelly et al., 2014; Manjrekar et al., 2015), and that NSSI is particularly salient among those reporting binge and purge behaviors (Kostro et al., 2014). Taken together, these findings suggest that emotional reactivity may be a useful factor to specifically examine the development and maintenance of BN, and that reactivity may be most relevant to the co-occurrence of NSSI and BN specifically, as opposed to other EDs.
4.5. Limitations
This study has several limitations. The sample was predominantly Caucasian females, which limits generalizability to males and other ethnicities. While the large sample size is a strength of this study, less than two-thirds completed both admission and discharge assessments. The use of a self-report instrument to assess emotional reactivity introduces the possibility of recall bias and raises questions regarding ecological validity. Thus, it would be beneficial for future research to examine emotional reactivity using multiple assessment methods, such as ecological momentary assessment, behavioral observation, experimental procedures, and physiological measurement. Additionally, the lack of a control group makes it difficult to understand if, and to what extent, emotional reactivity is elevated in these populations. The study also relied on clinical diagnoses rather than structured interviews to create the diagnostic groups. Finally, this study did not examine factors that may explain vulnerability to emotional reactivity. Further research is needed to understand common and specific risk factors for emotional reactivity among people with ED, NSSI, and co-occurring ED and NSSI.
4.6. Conclusions
In summary, emotional reactivity appears particularly elevated in individuals with NSSI and BN. Results highlight the importance of both emotional reactivity and NSSI in understanding clinical severity. Although emotional reactivity appears to be higher among those with NSSI and BN, it was not found to be consistently associated with treatment outcomes in an acute treatment setting. Thus, more studies that employ multiple forms of assessment of emotional reactivity are needed to understand the mechanisms by which emotional reactivity could directly and/or indirectly influence outcomes in a wider variety of clinical settings, as well as with more diverse samples.
Highlights.
Research suggests EDs and NSSI are associated with elevated emotional reactivity.
We assessed emotional reactivity in ED-only, NSSI-only, and co-occurring groups.
Emotional reactivity was highest in the co-occurring and NSSI-only groups.
Those with bulimia reported higher emotional reactivity than those with anorexia.
Emotional reactivity was not consistently related to treatment outcomes.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
NSSI frequency was treated as a continuous variable given that it was assessed using a Likert-type scale.
References
- Agh T, Kovacs G, Supina D, Pawaskar M, Herman BK, Voko Z, et al. A systematic review of the health-related quality of life and economic burdens of anorexia nervosa, bulimia nervosa, and binge eating disorder. Eat. Weight. Disord. 2016;21(3):353–364. doi: 10.1007/s40519-016-0264-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman BA, Jacobucci R, Kleiman EM, Muehlenkamp JJ, McCloskey MS. Development and validation of empirically derived frequency criteria for NSSI disorder using exploratory data mining. Psychol. Assess. 2017;29(2):221–231. doi: 10.1037/pas0000334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron IM, Cunningham L, Crawford JR, Eagles JM, Eisen SV, Lawton K, et al. Psychometric properties of the BASIS-24(c) (behaviour and symptom identification scale-revised) mental health outcome measure. Int. J. Psychiatry Clin. Pract. 2007;11(1):36–43. doi: 10.1080/13651500600885531. [DOI] [PubMed] [Google Scholar]
- Carol JR, Fairholme CP, Gallagher MW, Thompson-Hollands J, Barlow DH. The effects of anxiety and depressive symptoms on daily positive emotion regulation. J Psychopathol. Behav. Assess. 2014;36(2):224–236. [Google Scholar]
- Chapman AL, Dixon-Gordon KL, Walters KN. Borderline personality features moderate emotion reactivity and emotion regulation in response to a fear stressor. J. Exp. Psychopathol. 2013;4(5):451–470. [Google Scholar]
- Claes L, Muehlenkamp J. Non-Suicidal Self-Injury in Eating Disorders: Advancements in Etiology and Treatment. Springer; Berlin: 2013. [Google Scholar]
- Claes L, Smits D, Bijttebier P. The Dutch version of the Emotion Reactivity Scale: validation and relation with various behaviors in a sample of high school students. Eur. J. Psychol. Assess. 2014;30(1):73–79. [Google Scholar]
- Cucchi A, Ryan D, Konstantakopoulos G, Stroumpa S, Kaçar AS, Renshaw S, et al. Lifetime prevalence of non-suicidal self-injury in patients with eating disorders: a systematic review and meta-analysis. Psychol. Med. 2016;46(7):1345–1358. doi: 10.1017/S0033291716000027. [DOI] [PubMed] [Google Scholar]
- Cyders MA, Smith GT. Emotion-based dispositions to rash action: positive and negative urgency. Psychol. Bull. 2008;134(6):807. doi: 10.1037/a0013341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond A. Executive functions. Annu Rev. Psychol. 2013;64:135–168. doi: 10.1146/annurev-psych-113011-143750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evenden JL. Varieties of impulsivity. Psychopharmacology. 1999;146(4):348–361. doi: 10.1007/pl00005481. [DOI] [PubMed] [Google Scholar]
- Franklin JC, Aaron RV, Arthur MS, Shorkey SP, Prinstein MJ. Nonsuicidal self-injury and diminished pain perception: the role of emotion dysregulation. Compr. Psychiatry. 2012;53(6):691–700. doi: 10.1016/j.comppsych.2011.11.008. [DOI] [PubMed] [Google Scholar]
- Glenn CR, Blumenthal TD, Klonsky ED, Hajcak G. Emotional reactivity in nonsuicidal self-injury: divergence between self-report and startle measures. Int. J. Psychophysiol. 2011;80(2):166–170. doi: 10.1016/j.ijpsycho.2011.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoek HW. The incidence and prevalence of anorexia and bulimia nervosa in primary care. Psychol. Med. 1991;21(2):455–460. doi: 10.1017/s0033291700020560. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Asnaani A, Vonk IJ, Sawyer AT, Fang A. The efficacy of cognitive behavioral therapy: a review of meta-analyses. Cognit. Ther. Res. 2012;36(5):427–440. doi: 10.1007/s10608-012-9476-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joiner TE, Ribeiro JD, Silva C. Nonsuicidal self-injury, suicidal behavior, and their co-occurrence as viewed through the lens of the interpersonal theory of suicide. Curr. Dir. Psychol. Sci. 2012;21(5):342–347. doi: 10.1177/0963721412454873. [DOI] [Google Scholar]
- Kelly NR, Cotter EW, Mazzeo SE. Examining the role of distress tolerance and negative urgency in binge eating behavior among women. Eat. Behav. 2014;15(3):483–489. doi: 10.1016/j.eatbeh.2014.06.012. [DOI] [PubMed] [Google Scholar]
- Klonsky ED. The functions of deliberate self-injury: a review of the evidence. Clin. Psychol. Rev. 2007;27(2):226–239. doi: 10.1016/j.cpr.2006.08.002. [DOI] [PubMed] [Google Scholar]
- Klonsky ED, Oltmanns TF, Turkheimer E. Deliberate self-harm in a nonclinical population: prevalence and psychosocial correlates. Am. J. Psychiatry. 2003;160(8):1501–1508. doi: 10.1176/appi.ajp.160.8.1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kostro K, Lerman JB, Attia E. The current status of suicide and self-injury in eating disorders: a narrative review. J. Eat. Disord. 2014;2(19):1–9. doi: 10.1186/s40337-014-0019-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lannoy S, Heeren A, Rochat L, Rossignol M, Van der Linden M, Billieux J. Is there an all-embracing construct of emotion reactivity? adaptation and validation of the emotion reactivity scale among a French-speaking community sample. Compr. Psychiatry. 2014;55(8):1960–1967. doi: 10.1016/j.comppsych.2014.07.023. [DOI] [PubMed] [Google Scholar]
- Lavender JM, Wonderlich SA, Engel SG, Gordon KH, Kaye WH, Mitchell JE. Dimensions of emotion dysregulation in anorexia nervosa and bulimia nervosa: a conceptual review of the empirical literature. Clin. Psychol. Rev. 2015;40:111–122. doi: 10.1016/j.cpr.2015.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manjrekar E, Berenbaum H, Bhayani N. Investigating the moderating role of emotional awareness in the association between urgency and binge eating. Eat. Behav. 2015;17:99–102. doi: 10.1016/j.eatbeh.2015.01.010. [DOI] [PubMed] [Google Scholar]
- Muehlenkamp JJ, Peat CM, Claes L, Smits D. Self-injury and disordered eating: expressing emotion dysregulation through the body. Suicide Life Threat. Behav. 2012;42(4):416–425. doi: 10.1111/j.1943-278X.2012.00100.x. [DOI] [PubMed] [Google Scholar]
- Nock MK, Wedig MM, Holmberg EB, Hooley JM. The emotion reactivity scale: development, evaluation, and relation to self-injurious thoughts and behaviors. Behav. Ther. 2008;39(2):107–116. doi: 10.1016/j.beth.2007.05.005. [DOI] [PubMed] [Google Scholar]
- Stevanovic D. Quality of life enjoyment and satisfaction questionnaire- short form for quality of life assessments in clinical practice: a psychometric study. J. Psychiatr. Ment. Health Nurs. 2011;18(8):744–750. doi: 10.1111/j.1365-2850.2011.01735.x. [DOI] [PubMed] [Google Scholar]
- Tapajoz PdSF, Soneira S, Aulicino A, Harris P, Allegri RF. Emotional reactivity to social stimuli in patients with eating disorders. Psychiatry Res. 2015;229(3):887–894. doi: 10.1016/j.psychres.2015.07.049. [DOI] [PubMed] [Google Scholar]
- Washburn JJ, Potthoff LM, Juzwin KR, Styer D. Assessing DSM-5 nonsuicidal self-injury disorder in a clinical sample. Psychol. Assess. 2015;27(1):31–41. doi: 10.1037/pas0000021. [DOI] [PubMed] [Google Scholar]
- Wonderlich SA, Peterson CB, Crosby RD, Smith TL, Klein MH, Mitchell JE, et al. A randomized controlled comparison of integrative cognitive-affective therapy (ICAT) and enhanced cognitive-behavioral therapy (CBT-E) for bulimia nervosa. Psychol. Med. 2014;44(3):543–553. doi: 10.1017/S0033291713001098. [DOI] [PMC free article] [PubMed] [Google Scholar]