Abstract
Background
Job stress and cumulative exposure to traumatic events experienced by critical care nurses can lead to psychological distress and the development of burnout syndrome and posttraumatic stress disorder. Resilience can mitigate symptoms associated with these conditions.
Objective
To identify factors that affect resilience and to determine if the factors have direct or indirect effects on resilience in development of posttraumatic stress disorder.
Methods
Data from 744 respondents to a survey mailed to 3500 critical care nurses who were members of the American Association of Critical-Care Nurses were analyzed. Mplus was used to analyze a mediation model.
Results
Nurses who worked in any type of intensive care unit other than the medical unit and had high scores for resilience were 18% to 50% less likely to experience posttraumatic stress disorder than were nurses with low scores. Nurses with a graduate degree in nursing were 18% more likely to experience posttraumatic stress disorder than were nurses with a bachelor’s degree.
Conclusion
Because of their effects on resilience, working in a medical intensive care unit and having a graduate degree may influence the development of posttraumatic stress disorder. Future research is needed to better understand the impact of resilience on health care organizations, development of preventive therapies and treatment of posttraumatic stress disorder for critical care nurses, and the most appropriate mechanism to disseminate and implement strategies to address posttraumatic stress disorder.
The US health care system is experiencing a critical shortage of nurses.1 Among the many reasons for the shortage, an important component is the accelerated departure of nurses from their profession. Across the United States, turnover rates of nurses range from 13% to 20%.1,2 The growing national shortage is a particular concern in the intensive care unit (ICU). Turnover of nurses diminishes nurses’ productivity, staff morale, and quality of care. Turnover also can result in increases in medication errors, patient falls, and other measures of patient morbidity.3–5 Retention of experienced ICU nurses is important because turnover of nurses is costly, affects patient care, and increases job stress while decreasing work satisfaction and group cohesion. Job stress and the cumulative exposure to traumatic events experienced in the work environment can lead to psychological distress and the development of disorders such as burnout syndrome and posttraumatic stress disorder (PTSD).6–8
ICU nurses are repeatedly exposed to work-related stresses, including end-of-life issues, prolongation of life via artificial support measures, provision of postmortem care, and participation in procedures that are painful for patients.6 ICU nurses often experience psychological disorders such as PTSD, anxiety, depression and burnout syndrome,6–8 secondary traumatic stress,9,10 and compassion fatigue11,12 as a result of the work environment. However, some nurses have developed adaptive mechanisms or resilient characteristics that allow them to remain in the difficult work environment for many years.
Resilience is a concept that refers to an individual’s ability to bounce back or positively respond to adversity.13,14 Resilience is also understood to be a psychological mechanism that can thwart PTSD and is recognized as one of the most important factors for a healthy adjustment after trauma.15,16 Although some personality traits promote resilience, resilience can also be learned through cognitive and behavioral interventions.15–18 Psychological characteristics of resilience that can be learned include positive coping skills, engaging the support of others, optimism, humor, and cognitive restructuring.15 The ability to maintain resilience in nursing is influenced by the work environment,13 and the lack of this ability can result in negative psychological outcomes.7 ICU nurses with existing high levels of resilience are significantly less likely than those with low levels to experience PTSD, anxiety, depression, and burnout syndrome,8,17 suggesting that resilience mediates in some manner the potential impact of the traumatic event. In contrast, ICU nurses with symptoms of PTSD have reported problems with relationships, general life satisfaction, and overall functioning in all areas of their life.7
Although some evidence supports the effects of individual resilience on the psychological outcomes of ICU nurses,8 the factors that may significantly contribute to individual resilience and subsequent development of PTSD are relatively unexplored.
Objectives
The purpose of this research was to identify the individual and group characteristics that affect resilience and to determine if the significant individual and group characteristics have a direct or indirect effect on PTSD. We explored nurses’ personal characteristics of resilience because these characteristics are modifiable through cognitive behavioral therapy, whereas resilience traits are inherent. Our results may help in developing interventions to promote resilience and provide valuable information for organizational leaders to determine whether resilience training alone or resilience training in addition to environmental and organizational changes is needed.
Methods
Our study was a secondary analysis of the results from a sample of nurses drawn from an established database.8 Participants completed surveys to measure the prevalence of PTSD, burnout syndrome, anxiety, depression, and resilience. Secondary analysis with the statistical modeling program Mplus gives different and important data than does use of SPSS (IBM Corp) or SAS (SAS Institute Inc) statistical software on resilience as a mediator for the development of PTSD. Testing a mediation model in Mplus allows corrections to deal with dichotomous and continuous variables in the same equation.19 In addition, Mplus allows simultaneous testing of the effects of characteristics that influence resilience in PTSD.
Sample
The sample was drawn from critical care nurses who were members of the American Association of Critical-Care Nurses, which is the largest specialty organization representing the interests of more than 500 000 critical care nurses in the United States. We received a mailing list for 3500 randomly selected critical care nurses who were mailed surveys in a manner to ensure anonymity upon return, as delineated by standard survey principles.20
Measures
The measures used for the study included the posttraumatic diagnostic scale (PDS) and an abbreviated version of the Connor-Davidson Resilience Scale (CD-RISC). The PDS is a validated, self-report tool that yields both a PTSD diagnosis according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), 5th edition,21 and a measure of PTSD symptom severity. Although the gold standard for diagnosing PTSD is the clinician-administered PTSD scale, the PDS is highly correlated (r = 0.01) with the clinician-rated measures for diagnosing PTSD.22–24 The PDS is a well-accepted and validated survey instrument for diagnosis of PTSD7,24 and has high internal consistency reliability (Cronbach α, 0.78–0.92). In addition, test-retest reliability correlation coefficients of the total PDS score have satisfactory reliability: Cronbach α, 0.83 for total symptom severity, 0.77 for reexperiencing, 0.81 for avoidance, and 0.85 for arousal.7,8,24
The CD-RISC25 was used to assess resilience. This instrument is a 25-item self-report scale with a total score from zero to 100. Higher scores reflect greater resilience. Resilience is defined as a score of more than 80 with a mean score of 82. Highly resilient is defined as 1 SD greater than the mean; therefore a score of 92 or greater is considered a positive score for high resilience.25–27 The CD-RISC has excellent reliability (Cronbach α, 0.89) and a test-retest reliability correlation of 0.87.25 For our analysis, the Cronbach α for the instrument was 0.92.8
For the purposes of this study, we used an abbreviated version of the CD-RISC based on previous results of an exploratory factor analysis and confirmatory factor analysis of this sample of ICU nurses.27
Procedures
Approval for this study was obtained from the Colorado Multiple Institutional Review Board. The dataset was complete.
Data Analysis
Descriptive statistics were generated by using IBM SPSS Statistics, version 20, to summarize the demographic variables of the sample, and bivariate correlations were analyzed to determine the individual and group characteristics (Table 1) that significantly affected the 3 subscales of resilience.
Table 1.
Individual and group characteristics
| Type of characteristic | Measurement variable |
|---|---|
| Individual | Children Exercises regularly Highest nursing degree Years practicing Nurse to patient ratio Shift |
| Group | Unit type Generational cohort |
Because potential predictors with more than 2 categories were possible, dummy codes were created. Generational cohort, highest degree earned, nurse to patient ratio, and shift and unit type were recoded. A baseline group was chosen according to predefined hypotheses or the group that represented the majority of the participants in the sample was used as the baseline group or both.28 The baseline group was then compared with the other recoded groups. If any of the dummy grouping categories was significantly associated with the resilience subscales, all of the dummy grouping categories were retained for the mediation model.
Using Mplus, version 7.0, we analyzed a mediation model. This model proposed that each significant characteristic had a direct effect on the development of PTSD and an indirect effect on the development of PTSD through the characteristic’s influence on the 3 subscales of resilience. Beta weights, standard errors, and P values were used to determine which individual and group variables were significant and to model the direct and indirect paths between the significant variables and the development of PTSD. Significance was set at P ≤ .05. Odds ratios and 95% CIs were assessed to determine which of the significant variables had a significant indirect effect. Odds ratios greater than 1.0 indicated that as the predictor variable increased, so did the outcome variable.
Results
Characteristics of the Sample
A total of 1202 nurses completed and returned the survey. Data from 458 nurses were excluded because the respondents were not currently working as ICU nurses. The final sample consisted of 744 critical care nurses.
Table 2 gives the demographics of the final sample. Most of the respondents were women (91%) with a mean age of 43.6 years (SD, 11.0). Race was self-reported as white (83%), Asian (10%), African American (5%), American Indian (1%), and mixed ethnicity or other (1%).
Table 2.
Sample demographics (N=744)
| Characteristic | Valuea |
|---|---|
| Female sex | 674 (91) |
|
| |
| Age, mean (SD), y | 43.6 (11.0) |
|
| |
| Exercise regularly | 458 (62) |
|
| |
| Marital status | |
| Single | 119 (16) |
| Married | 502 (67) |
| Other | 123 (17) |
|
| |
| Type of intensive care unit | |
| Medical | 262 (35) |
| Surgical | 77 (10) |
| Cardiac | 79 (11) |
| Cardiothoracic | 68 (9) |
| Pediatric | 29 (4) |
| Other | 229 (31) |
|
| |
| Highest degree | |
| Associate | 147 (20) |
| Bachelor’s | 421 (57) |
| Other (master’s degree, doctorate of nursing practice, or PhD) | 176 (24) |
|
| |
| Years practiced, mean (SD) | 17.8 (11.7) |
Values are number (percentage) unless indicated otherwise in first column. Because of rounding, not all percentages total 100.
Factors Affecting Resilience
The significant individual characteristics identified after analyzing bivariate correlations included having children (r = 0.01; P= .01), number of years practicing as an ICU nurse (r = 0.09; P= .02), and type of degree earned (DE2; r =0.15; P= .001). All 3 significant individual characteristics were significantly associated with the leadership subscale of resilience. The significant group characteristics that affected resilience included the type of unit that the ICU nurse worked on and generational cohort assignment (Table 3).
Table 3.
Bivariate correlations (Pearson r) of individual and group characteristics with resilience subscales
| Variablea | Variable type | Personal competence | Leadership | Perseverance |
|---|---|---|---|---|
| CH | Individual | 0.02 | 0.01b | 0.02 |
| YP | Individual | 0.04 | 0.09c | 0.03 |
| EX | Individual | 0.05 | 0.01 | 0.07 |
| GC1 | Group | 0.02 | 0.02 | 0.00 |
| GC2 | Group | −0.03 | −0.12b | −0.03 |
| GC3 | Group | −0.02 | 0.01 | −1.01 |
| DE1 | Individual | 0.06 | 0.05 | 0.01 |
| DE2 | Individual | 0.03 | 0.15d | 0.06 |
| RA1 | Individual | −0.04 | 0.03 | 0.02 |
| SH1 | Individual | −0.04 | −0.03 | 0.06 |
| UN1 | Group | −0.08c | −0.03 | −0.06 |
| UN2 | Group | 0.06 | 0.03 | 0.04 |
| UN3 | Group | −0.02 | 0.02 | 0.05 |
| UN4 | Group | −0.03 | 0.02 | 0.01 |
Explanation of variable codes: CH, children; YP, years practicing; EX, exercise; GC1, generation X compared with boomers II; GC2, millennials compared with boomers II; GC3, postwar or boomers I compared with boomers II; DE1, associate degree in nursing or diploma compared with bachelor of science degree in nursing (BSN); DE2, master’s degree or higher compared with BSN; RA1, >2 patients per nurse compared with ≤ 2 patients per nurse; SH1, night shift compared with day shift; UN1, cardiac intensive care unit (ICU) compared with medical ICU; UN2, surgical ICU compared with medical ICU; UN3, cardiothoracic surgery ICU compared with medical ICU; UN4, other ICUs compared with medical ICU.
In 2-tailed test, P ≤ .006.
In 2-tailed test, P ≤ .05.
In 2-tailed test, P = .001.
On the basis of the correlations, 3 dummy grouping variables (generation X, millennial, and boomer I) were chosen for further analysis. All generational cohort dummy variables were coded to allow comparison with the boomer II group. The educational degree variable was recoded into 2 dummy grouping variables (diploma or associate degree and graduate degree); the comparison was with ICU nurses who had a bachelor of science in nursing degree. The nurse to patient ratio variable was recoded into 1 dummy variable (nurse to patient ratio > 2 to 1) that was compared with nurse to patient ratios of 2 to 1 or less. The primary shift variable was recoded into those who worked day shift (7 AM to 7 PM and 7 AM to 3 PM) and those who worked night shift (3 PM to 11 PM and 11 PM to 7 AM). Night shift was compared with day shift. Finally, unit type was recoded into 4 dummy grouping variables (cardiac ICU [CICU], surgical ICU [SICU], cardiothoracic surgery ICU [CTICU], and other type). The medical ICU (MICU) was used as the comparison group (Table 4).
Table 4.
Dummy coding
| Variable | Baseline group | Hypothesis-driven or group majority |
|---|---|---|
| Generational cohort | Boomers II | Group majority |
| Degree | Bachelor of science in nursing | Hypothesis driven |
| Nurse to patient ratio | 1 to 2 | Group majority |
| Shift | Days (7 AM to 3 PM or 7 AM to 7 PM) | Hypothesis driven |
| Unit type | Medical | Hypothesis driven |
The CICU (code UN1) was the only ICU with a significant correlation (r = −0.08; P= .04) through the personal competence subscale of resilience (Table 3). The remaining units were not significantly correlated: SICU (code UN2) r =0.06; P= .12; CTICU (code UN3) r = −0.02; P= .60; and all other units (code UN4) r = −0.03; P=.44. Because the CICU was significantly correlated, all 4 unit types were retained in the final mediation model.
The 3 generational cohorts included generation X (GC1), millennials (GC2), and postwar or boomers II (GC3), which were compared with the boomers II cohort (Table 3). The millennial group was significantly correlated with the leadership subscale of resilience (r =−0.12; P= .001). Generation X (GC1; r = 0.02; P= .51) and postwar or boomers I (GC3; r = 0.01; P= .73) were not significantly correlated but were retained for the final mediation model.
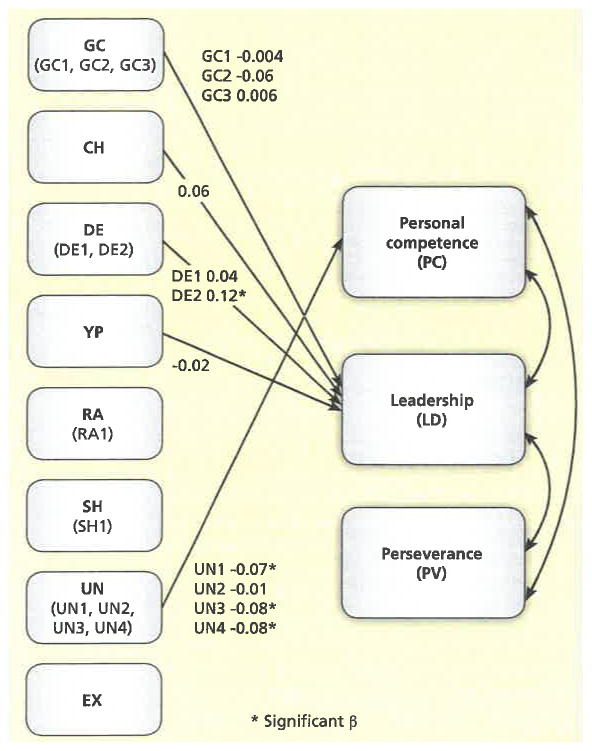
No individual or group characteristics significantly affected the perseverance subscale of resilience, so this subscale was not retained in the final mediation model. Figure 1 is a model of the individual and group factors that significantly affected the resilience subscales. The nonsignificant paths are not included in the figure. Among the unit variables, 3 had significant paths to the personal competence subscale of resilience. The comparison of the CICU with the MICU had a significant β of −0.07 (SE, 0.03; P= .02), as did the CTICU (β =−0.08; SE, 0.03; P=.005) and the ICU category other (β =−0.08; SE, 0.03; P=.01). The SICU and MICU comparison was the only unit type that did not have a significant path (β = −0.01; SE, 0.03; P=.76).
Figure 1.
Significant individual (CH, DE, YP, RA, SH, and EX) and group (GC and UN) characteristics that affect the 3 subscales of resilience.
Explanation of variable codes: GC1, generation X compared with boomers II; GC2, millennial compared with boomers II; GC3, postwar/boomers I compared with boomers II; CH, children; DE1, associate degree in nursing or diploma compared with bachelor of science degree in nursing (BSN); DE2, master’s degree or higher compared with BSN; YP, years practicing; RA1, >2 patients per nurse compared with ≤ 2 patients per nurse; SH1, night shift compared with day shift; UN1, cardiac intensive care unit (ICU) compared with medical ICU; UN2, surgical ICU compared with medical ICU; UN3, cardiothoracic surgery ICU compared with medical ICU; UN4, other ICUs compared with medical ICU; EX, exercise.
Only 1 variable had a significant path to the leadership subscale of resilience. Comparison of respondents with a graduate degree or higher with respondents with a bachelor’s degree in nursing had the following values: β = 0.12; SE, 0.03; P=.001. The remaining variables were not significant and included associate degree or diploma in nursing (DEI; β = 0.04; SE, 0.03; P= .21), having children (β =0.06; SE, 0.03; P= .07), years practicing (β =−0.02; SE, 0.05; P= .67), generation X (GC1; β =−0.004; SE, 0.04; P= .91), millennials (GC2; β = −0.06; SE, 0.05; P= .25), and postwar or boomers I (GC3; β = 0.006; SE, 0.03; P= .85) (see Figure 1).
Direct and Indirect Effects
The 3 subscales of resilience (personal competence, leadership, and perseverance), whether the ICU nurse had children, and the number of years practicing as an ICU nurse had significant inverse direct effects on the development of PTSD (Table 5). On the basis of the odds ratio, ICU nurses with higher levels of personal competence were 28% less likely to experience PTSD than were nurses with lower levels of personal competence. Nurses with higher levels of leadership were 21% more likely to experience PTSD than were nurses with lower levels of leadership, and nurses with higher levels of perseverance were 11% less likely to experience PTSD than were nurses with lower levels of perseverance. ICU nurses with children were 40% less likely to experience PTSD than were nurses who did not have children. Finally, as years of experience increased, ICU nurses were 3% less likely to experience PTSD.
Table 5.
Direct effects of individual and group characteristics on the development of posttraumatic stress disorder
| Variablea | β(SE) | Odds ratio | 95% CI |
|---|---|---|---|
| PC | −0.45 (0.06)b | 0.72 | 0.68–0.79 |
| LD | 0.22 (0.06)c | 1.21 | 1.11–1.34 |
| PV | −0.17(0.06)c | 0.89 | 0.83–0.96 |
| CH | −0.11 (0.05)d | 0.60 | 0.41–0.89 |
| YP | −0.17(0.09)d | 0.97 | 0.94–1.00 |
| GC1 | −0.02 (0.06) | 0.91 | 0.55–1.51 |
| GC2 | −0.11 (0.09) | 0.57 | 0.28–1.14 |
| GC3 | −0.11 (0.06) | 0.48 | 0.24–0.96 |
| DE1 | 0.12(0.05) | 1.10 | 0.74–1.63 |
| DE2 | −0.74 (0.06) | 0.65 | 0.38–1.11 |
| UN1 | −0.002 (0.05) | 0.99 | 0.56–1.73 |
| UN2 | 0.03 (0.05) | 1.24 | 0.70–2.22 |
| UN3 | −0.03 (0.05) | 0.81 | 0.43–1.53 |
| UN4 | 0.07 (0.05) | 1.38 | 0.92–2.03 |
Explanation of variable codes: PC, personal competence, LD, leadership; PV, perseverance; CH, children; YP, years practicing; GC1, generation X compared with boomers II; GC2, millennials compared with boomers II; GC3, postwar or boomers I compared with boomers II; DE1, associate degree in nursing or diploma compared with bachelor of science degree in nursing (BSN); DE2, master’s degree or higher compared with BSN; UN1, cardiac intensive care unit (ICU) compared with medical ICU; UN2, surgical ICU compared with medical ICU; UN3, cardiothoracic surgery ICU compared with medical ICU; UN4, other ICUs compared with medical ICU.
In 2-tailed test, P=.001.
In 2-tailed test, P≤.006.
In 2-tailed test, P≤0.5
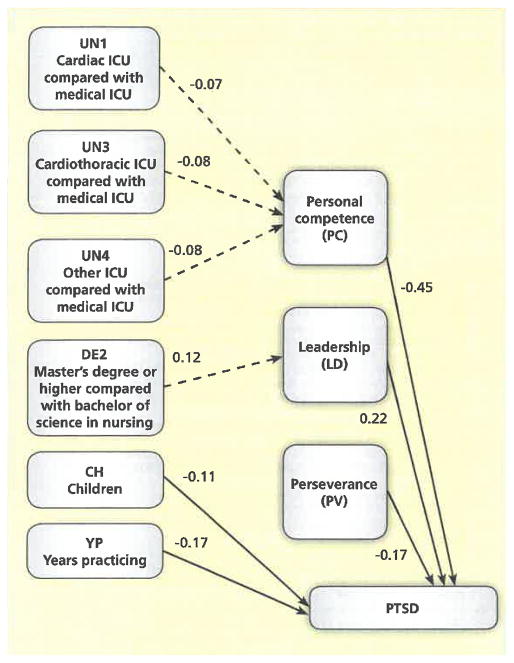
In order to determine whether the significant variables had an indirect effect on the development of PTSD via influence on the resilience subscales, a mediation model was analyzed by using Mplus. Among the unit groupings, 3 variables had significant indirect effects on PTSD via the personal competence subscale of resilience when compared with the MICU (UN1 β=−0.07 with SE, 0.03; UN3 β=−0.08 with SE, 0.03; and UN4 β = −0.08 with SE, 0.03). The odds ratios and the 95% CIs were as follows (Table 6): UNI p=−0.65; 95% CI, −1.1 to −0.12; UN3 (β=−0.82; 95% CI, −1.31 to −0.34) and UN4 (β = −0.50; 95% CI, −0.82 to −0.18. Compared with MICU nurses, the CTICU nurses were 18% less likely, the CICU nurses were 35% less likely, and other ICU nurses were 50% less likely to experience PTSD. The only significant indirect variable for the leadership sub-scale of resilience was graduate degree (DE2): β = 0.12 (SE, 0.03; Table 7). The odds ratio was 0.82 (95% CI, 0.50 to 1.1), indicating that ICU nurses with a graduate degree were 18% more likely to experience PTSD than were nurses with a bachelor of science in nursing degree. Figure 2 shows the full model with the significant direct and indirect effects.
Table 6.
Significant indirect effects on posttraumatic stress disorder through influence on personal competence subscale of resilience
| Personal competence | UN1: CICU vs MICU | UN2: SICU vs MICU | UN3: CTSICU vs MICU | UN4: other vs MICU |
|---|---|---|---|---|
| Estimate, β (SE) | −0.07 (0.03)a | −0.01 (0.03) | −0.08 (0.03)b | −0.08 (0.03)b |
| Odds ratio (95% CI) | −0.65 (−1.1 to−0.12) | NA | −0.82 (−1.3 to−0.34) | −0.50 (−0.82 to−0.18) |
Abbreviations: CICU, cardiac intensive care unit; CTSICU, cardiothoracic surgery intensive care unit; MICU, medical intensive care unit; NA, not applicable; SICU, surgical intensive care unit.
In 2-tailed test, P≤.05.
In 2-tailed test, P≤.01.
Table 7.
Significant indirect effects on posttraumatic stress disorder through influence on leadership subscale of resiliencea
| Leadership | CH | YP | GC1 | GC2 | GC3 | DE1 | DE2 |
|---|---|---|---|---|---|---|---|
| Estimate, β (SE) | 0.06 (0.03) | −0.02 (0.05) | −0.004 (0.04) | −0.06 (0.05) | 0.006 (0.03) | 0.04 (0.03) | 0.12(0.03)b |
| Odds ratio (95% CI) | NA | NA | NA | NA | NA | NA | 0.82(0.50–1.1) |
Abbreviations: CH, children; YP, years practicing; GC1, generation X compared with boomers II; GC2, millennial compared with boomers II; GC3, postwar or boomers I compared with boomers II; DEI, associate degree in nursing or diploma compared with bachelor of science degree in nursing (BSN); DE2, master’s degree or higher compared with BSN; NA, not applicable.
In 2-tailed test, P≤.05.
Figure 2.
Final model with significant direct and indirect effects of individual and group factors on the development of posttraumatic stress disorder (PTSD) through the 3 subscales of resilience.
Discussion
In this secondary analysis of 744 ICU nurses, we identified the individual and group characteristics that significantly affected the 3 subscales of resilience. We further tested a mediation model to determine whether those significant characteristics had a direct or indirect effect on the development of PTSD. ICU nurses who worked in any type of ICU other than the MICU were 18% to 50% less likely to experience PTSD when mediated through resilience. In contrast, ICU nurses with a graduate degree in nursing were 18% more likely to experience PTSD than were nurses with a bachelor’s degree in nursing.
Evidence related to resilience training in nurses is limited. No large randomized clinical trials have been done to determine the effectiveness of resilience interventions on psychological outcomes, nurses’ satisfaction, and nurses’ retention in the ICU. The feasibility and acceptability of a multimodal resilience intervention program that included exercise, written exposure therapy, event-triggered counseling sessions, and mindfulness-based stress reduction exercises were assessed in a small randomized, controlled trial.29 The results suggested that the program was feasible and acceptable, and although the study had insufficient power to detect changes in resilience and psychological disorders, the findings suggested improvements in resilience scores and reduced symptoms of PTSD and depression.
Evidence on characteristics of different types of ICUs is limited. Cimiotti et al30 reported that nurses in MICU and mixed medical-surgical ICUs perceived higher levels of staffing than did nurses in the CICU and SICU. In another study,31 698 ICU nurses from 8 different Magnet hospitals were surveyed to determine which ICUs reported the healthiest work environments. The MICU, mixed medical-surgical ICU, and SICU scored lowest on control of nursing practice, perceived adequacy of staffing, support for education, and clinical competence. These results were consistent with our findings and highlight the need to explore what characteristics are present in the MICU but not in other ICUs. In addition, the results of some studies32,33 have suggested that team support can enhance coping skills in times of stress and can help relieve emotional burden in a stressful environment. However, these studies involved oncology nurses. Future research is needed to explore team support in the ICU. Additionally, research is needed to identify the ICU characteristics to help determine whether resilience interventions can be tailored to modifiable organizational efforts or if additional interventions exist that can be used to mitigate PTSD.
Currently, no research supports the finding that ICU nurses with graduate degrees are more likely to experience PTSD than are nurses with bachelor’s degrees in nursing. Theoretically, nurses who are pursuing graduate degrees may be doing so in an effort to move away from the traumatic experiences common in the ICU setting. Graduate nurses may also experience higher levels of PTSD because of the stress and challenges of working in the ICU environment while pursuing graduate studies. Future research is needed to explore this finding in more depth.
Our study has several limitations. First, secondary analysis of an existing database does not allow the inclusion of all potential variables that may influence resilience. Evidence in the literature supports the notion that system characteristics in nurses’ work environment are beneficial for reducing environment stress. These characteristics include control over nursing practice34,35 managerial support,36 empowerment,37,38 and nurses’ satisfaction.39 Information on these variables was not available in our dataset. However, the sample size was adequate; at least 50 cases per independent variable are recommended for mediation models,40 and the variables that were included in the dataset have been relatively unexplored in relation to resilience and development of PTSD. Second, no information was available on nurses who had left the ICU setting or nursing all together. We found that years in practice had a direct effect on the development of PTSD. As the number of years in practice increased, the risk for PTSD decreased, an assumption that might be false if we are obtaining solely data on resilient nurses who remain at the bedside. Future longitudinal assessments would be needed to fully assess the relationship between years of practice and development of PTSD. Another related limitation is that we used a cross-sectional dataset and temporal precedence was dealt with by applying a theoretical model. Replication of our findings with another dataset or, as mentioned earlier, a longitudinal sample, is needed to solidify our results. Finally, the dataset had no unit-specific or organization-specific information available. Exploring contextual factors specific to an organization or a unit or both in considerations of interventions to increase resilience would be important.
Implications
Our results are important because we found that working in an MICU and having a graduate degree may influence the development of PTSD via the influence of these 2 factors on resilience. Further research is needed to better understand the effect of this influence on resilience in health care organizations, development of preventive therapies and treatment of PTSD for ICU nurses, and the most appropriate mechanism to disseminate and implement strategies to address PTSD. One potential strategy for mitigating symptoms of PTSD or psychological distress is use of resilience training. Results of an earlier study29 indicated that a multimodal resilience training program that included written exposure therapy, exercise, cognitive-behavioral therapy, and mindfulness-based stress reduction exercises significantly improved resilience scores and decreased symptoms of PTSD and depression.
In conclusion, understanding that development of PTSD is influenced by the type of ICU work environment (MICU) and by having a graduate degree generates additional research questions to explore in order to tailor intervention programs and adjunct therapies for nurses at high risk for PTSD.
Footnotes
To purchase electronic or print reprints, contact American Association of Critical-Care Nurses, 101 Columbia, Aliso Viejo, CA 92656. Phone, (800) 899–1712 or (949) 362–2050 (ext 532); fax, (949) 362–2049; reprints@aacn.org.
FINANCIAL DISCLOSURES
None reported
eLetters
Now that you’ve read the article, create or contribute to an online discussion on this topic. Visit www.ajcconline.org and click “Submit a response” in either the full-text or PDF view of the article.
Contributor Information
Meredith Mealer, Assistant professor, Department of Physical Medicine and Rehabilitation, Department of Medicine, University of Colorado School of Medicine, Aurora, Colorado, and Rocky Mountain Mental Illness, Research, Education, and Clinical Center (MIRECC), Denver VA Health, Denver, Colorado.
Jacqueline Jones, Associate professor, College of Nursing, University of Colorado Anschutz Medical Campus, Aurora, Colorado.
Paula Meek, Professor, College of Nursing, University of Colorado Anschutz Medical Campus, Aurora, Colorado.
References
- 1.Chan ZC, Tam WS, Lung MK, Wong WY, Chau CW. A systematic literature review of nurse shortage and the intention to leave. J Nurs Manag. 2013;21(4):605–613. doi: 10.1111/j.1365-2834.2012.01437.x. [DOI] [PubMed] [Google Scholar]
- 2.Hauck A, Quinn Griffin MT, Fitzpatrick JJ. Structural empowerment and anticipated turnover among critical care nurses. J Nurs Manag. 2011;19(2):269–276. doi: 10.1111/j.1365-2834.2011.01205.x. [DOI] [PubMed] [Google Scholar]
- 3.Barlow KM, Zangaro GA. Meta-analysis of the reliability and validity of the Anticipated Turnover Scale across studies of registered nurses in the United States. J Nurs Manag. 2010;18:862–873. doi: 10.1111/j.1365-2834.2010.01171.x. [DOI] [PubMed] [Google Scholar]
- 4.Jones CB. Revisiting nurse turnover costs: adjusting for inflation. J Nurs Adm. 2008;38(1):11–18. doi: 10.1097/01.NNA.0000295636.03216.6f. [DOI] [PubMed] [Google Scholar]
- 5.Waldman JD, Kelly F, Arora S, Smith HL. The shocking cost of turnover in health care. Health Care Manage Rev. 2004;29(1):2–7. doi: 10.1097/00004010-200401000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Mealer ML, Shelton A, Berg B, Rothbaum B, Moss M. Increased prevalence of post-traumatic stress disorder symptoms in critical care nurses. Am J Respir Crit Care Med. 2007;175(7):693–697. doi: 10.1164/rccm.200606-735OC. [DOI] [PubMed] [Google Scholar]
- 7.Mealer M, Burnham EL, Goode CJ, Rothbaum B, Moss M. The prevalence and impact of post traumatic stress disorder and burnout syndrome in nurses. Depress Anxiety. 2009;26(12):1118–1126. doi: 10.1002/da.20631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mealer M, Jones J, Newman J, McFann KK, Rothbaum B, Moss M. The presence of resilience is associated with a healthier psychological profile in intensive care unit (ICU) nurses: results of a national survey. Int J Nurs Stud. 2012;49(3):292–299. doi: 10.1016/j.ijnurstu.2011.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beck CT. Secondary traumatic stress in nurses: a systematic review. Arch Psychiatr Nurs. 2011;25(1):1–10. doi: 10.1016/j.apnu.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 10.Von Rueden KT, Hinderer KA, McQuillan KA, et al. Secondary traumatic stress in trauma nurses: prevalence and exposure, coping, and personal/environmental characteristics. J Trauma Nurs. 2010;17(4):191–200. doi: 10.1097/JTN.0b013e3181ff2607. [DOI] [PubMed] [Google Scholar]
- 11.Maytum JC, Heiman MB, Garwick AW. Compassion fatigue and burnout in nurses who work with children with chronic conditions and their families. J Pediatr Health Care. 2004;18(4):171–179. doi: 10.1016/j.pedhc.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 12.Meadors P, Lamson A. Compassion fatigue and secondary traumatization: provider self care on intensive care units for children. J Pediatr Health Care. 2008;22(1):24–34. doi: 10.1016/j.pedhc.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 13.Turner SB. The resilient nurse: an emerging concept. Nurse Lead. 2014;12(6):71–73. 90. [Google Scholar]
- 14.Earvolino-Ramirez M. Resilience: a concept analysis. Nurs Forum. 2007;42:73–82. doi: 10.1111/j.1744-6198.2007.00070.x. [DOI] [PubMed] [Google Scholar]
- 15.Charney DS. Psychobiological mechanisms of resilience and vulnerability: implications for successful adaptation to extreme stress. Am J Psychiatry. 2004;161(2):195–216. doi: 10.1176/appi.ajp.161.2.195. [DOI] [PubMed] [Google Scholar]
- 16.Davidson JR, Payne VM, Connor KM, et al. Trauma, resilience and saliostasis: effects of treatment in post-traumatic stress disorder. Int Clin Psychopharmacol. 2005;20(1):43–48. doi: 10.1097/00004850-200501000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Hoge EA, Austin ED, Pollack MH. Resilience: research evidence and conceptual considerations for posttraumatic stress disorder. Depress Anxiety. 2007;24(2):139–152. doi: 10.1002/da.20175. [DOI] [PubMed] [Google Scholar]
- 18.Luthar SS, Cicchetti D, Becker B. The construct of resilience: a critical evaluation and guidelines for future work. Child Dev. 2000;71(3):543–562. doi: 10.1111/1467-8624.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Muthen B. [Accessed February 3, 2017];Applications of Causally Defined Direct and Indirect Effects in Mediation Analysis Using SEM in Mplus. https://www.statmodel.com/download/causalmediation.pdf. Published October 28, 2011.
- 20.Dillman D. Mail and Telephone Surveys: The Total Design Method. Hoboken, NJ: John Wiley & Sons; 1978. [Google Scholar]
- 21.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Health Disorders: DSM-5. 5. Washington, DC: American Psychiatric Publishing; 2013. [Google Scholar]
- 22.Foa E, Meadows E. Psychosocial treatments for posttraumatic stress disorder: a critical review. Annu Rev Psychol. 1997;48:449–480. doi: 10.1146/annurev.psych.48.1.449. [DOI] [PubMed] [Google Scholar]
- 23.Mueser KT, Salyers MP, Rosenberg SD, Ford JD, Fox L, Carty P. Psychometric evaluation of trauma and posttraumatic stress disorder assessments in persons with severe mental illness. Psychol Assess. 2001;13(1):110–117. doi: 10.1037//1040-3590.13.1.110. [DOI] [PubMed] [Google Scholar]
- 24.Sheeran T, Zimmerman M. Screening for posttraumatic stress disorder in a general psychiatric outpatient setting. J Consult Clin Psychol. 2002;70(4):961–966. doi: 10.1037//0022-006x.70.4.961. [DOI] [PubMed] [Google Scholar]
- 25.Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC) Depress Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 26.Campbell-Sills L, Forde DR, Stein MB. Demographic and childhood environmental predictors of resilience in a community sample. J Psychiatr Res. 2009;43(12):1007–1012. doi: 10.1016/j.jpsychires.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 27.Mealer M, Schmiege SJ, Meek R. The Connor-Davidson Resilience Scale (CD-RISC) in critical care nurses: a psychometric analysis. J Nurs Meas. 2016;24(1):28–39. doi: 10.1891/1061-3749.24.1.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fields A. Discovering Statistics Using SPSS. 3. Thousand Oaks, CA: Sage Publications Inc; 2009. [Google Scholar]
- 29.Mealer M, Conrad D, Evans J, et al. Feasibility and acceptability of a resilience training program for intensive care unit nurses. Am J Crit Care. 2014;23(6):e97–e105. doi: 10.4037/ajcc2014747. [DOI] [PubMed] [Google Scholar]
- 30.Cimiotti JP, Quinlan PM, Larson EL, Pastor DK, Lin SX, Stone PW. The magnet process and the perceived work environment of nurses. Nurs Res. 2005;54(6):384–390. doi: 10.1097/00006199-200511000-00004. [DOI] [PubMed] [Google Scholar]
- 31.Schmalenberg C, Kramer M. Types of intensive care units with the healthiest, most productive work environments. Am J Crit Care. 2007;16:458–468. [PubMed] [Google Scholar]
- 32.Rohan E, Bausch J. Climbing Everest: oncology work as an expedition in caring. J Psychosoc Oncol. 2009;27:84–118. doi: 10.1080/07347330802616043. [DOI] [PubMed] [Google Scholar]
- 33.Zander M, Hutton A, King L. Coping and resilience factors in pediatric oncology nurses. J Pediatr Oncol Nurs. 2010;27(2):94–108. doi: 10.1177/1043454209350154. [DOI] [PubMed] [Google Scholar]
- 34.Kramer M, Schmalenberg C, Maguire P, et al. Structures and practices enabling staff nurses to control their practice. West J Nurs Res. 2008;30(5):539–559. doi: 10.1177/0193945907310559. [DOI] [PubMed] [Google Scholar]
- 35.Weston M. Defining control over nursing practice and autonomy. J Nurs Adm. 2008;38:404–408. doi: 10.1097/01.NNA.0000323960.29544.e5. [DOI] [PubMed] [Google Scholar]
- 36.Bennett P, Lowe R, Matthews V, Dourali M, Tattersall A. Stress in nurses: coping, managerial support and work demand. Stress Health. 2001;17(1):55–63. [Google Scholar]
- 37.Armstrong K, Laschinger H. Structural empowerment. Magnet hospital characteristics, and patient safety culture: making the link. J Nurs Care Qual. 2006;21(2):124–132. doi: 10.1097/00001786-200604000-00007. [DOI] [PubMed] [Google Scholar]
- 38.Browning A. Moral distress and psychological empowerment in critical care nurses caring for adults at end of life. Am J Crit Care. 2013;22(2):143–151. doi: 10.4037/ajcc2013437. [DOI] [PubMed] [Google Scholar]
- 39.Hayes LJ, O’Brien-Pallas L, Duffield C, et al. Nurse turnover: a literature review. Int J Nurs Stud. 2006;43(2):237–263. doi: 10.1016/j.ijnurstu.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 40.Grimm L, Yarnold P, editors. Reading and Understanding Multivariate Statistics. Washington, DC: American Psychological Association; 2010. [Google Scholar]