Abstract
The incidence of hip fracture in patients with end-stage renal disease (ESRD) is considerably higher than that in the general age- and sex-matched population. Although medical therapy for chronic kidney disease mineral bone disorder (CKD-MBD) has changed considerably over the last decade, rates of hip fracture in the entire ESRD population have not been well-characterized. Herein, we evaluated temporal trends in rates of hip fracture, in-hospital mortality, and costs of associated hospital stay in ESRD. We identified hospitalizations for hip fracture from 2003 to 2011 using the Nationwide Inpatient Sample, a representative national database inclusive of all ages and payers. We incorporated data from the United States Renal Data System and the US Census to calculate population-specific rates. Between 2003 and 2011, we identified 47,510 hip fractures in the ESRD population. The overall rate of hip fracture was 10.04/1000 person-years. The rate was 3.73/1000 person-years in patients aged less than 65 years, and 20.97/1000 person-years in patients aged 65 or older. Age- and sex-standardized rates decreased by 12.6% from 2003 (10.23/1000 person-years; 95% confidence interval (CI), 7.99/1000 to 12.47/1000) to 2011 (8.94/1000 person-years; 95% CI, 7.12/1000 to 10.75/1000). Hip fracture rates over time were virtually identical in patients aged less than 65 years, however, rates decreased by 15.3% among patients aged 65 years or older; rates declined more rapidly in older women compared with older men (p for interaction = 0.047). In-hospital mortality rate after hip fracture operation declined by 26.7% from 2003 (8.6%; 95% CI, 6.8 to 10.4) to 2011 (6.3%; 95% CI, 4.9 to 7.7). In ESRD, age- and sex-standardized hip fracture rates and associated in-hospital mortality have declined substantially over the last decade.
Keywords: Hip fractures, ESRD, Epidemiology, Nationwide Inpatient Sample
INTRODUCTION
Hip fracture is a major public health problem. In the United States (US), there are at least 250,000 persons hospitalized for hip fracture each year,(1) with high rates of mortality and morbidity and an estimated annual cost of $10 billion.(2,3) Specifically, about a half of patients who have experienced a hip fracture are unable to regain their activities of daily living,(4) and one-quarter die within one year.(5) During the past two decades, the incidence of hip fracture has progressively declined in the US.(5,6) The approval of bisphosphonates for osteoporosis (starting in 1996) and subsequent widespread use has been proposed as one possible explanation for the declining trend in hip fracture incidence in the general population.(7)
Hip fracture rates in patients with end-stage renal disease (ESRD) are 4 to 17-fold higher than in the general population.(8–10) With declining kidney function, decreased concentrations of 1,25-hydroxy vitamin D3 and increased concentrations of parathyroid hormone (PTH) and fibroblast growth factor 23 (FGF23) contribute to abnormalities in bone mass and quality.(11,12) Patients with ESRD have other risk factors for hip fracture, including physical inactivity, deconditioning, sensory neuropathy, autonomic neuropathy, orthostatic hypotension, and increased susceptibility to falls.(13–15) In contrast to the general population, little is known regarding temporal trends of hip fracture in the ESRD population. Several,(16–18) but not all(19) studies demonstrated an increase in hip fracture rates until 2004, with inconsistent results thereafter. Previous studies varied with respect to inclusion criteria, definition of hip fracture, and confounding by age, a dominant risk factor for hip fracture. Most previous reports were derived using data from Medicare beneficiaries,(16–19) excluding young patients and those covered by other forms of health insurance, particularly in the first three years of a person’s dialysis experience.
In this study, we sought to determine trends in age- and sex-standardized hip fracture rates among patients with ESRD and associated in-hospital mortality, length of hospital stay, and costs, using data from the Nationwide Inpatient Sample (NIS) during 2003–2011. We hypothesized that age- and sex-standardized rates of hip fracture had declined over that time frame.
MATERIALS AND METHODS
Study Population
The NIS is a nationally representative all-payer inpatient database developed from the Healthcare Cost and Utilization Project by the Agency for Healthcare Research and Quality.(20) Until 2011, NIS data were collected annually as a stratified random sample of about 20% of US hospitals, with the exception of Veterans Affairs hospitals, long-term non-acute care hospitals, and chemical dependence or alcohol treatment facilities. The NIS contains more than 8 million de-identified hospital discharges from about 1000 hospitals. It also has patient demographic information, hospital characteristics, and facility charges related to inpatient stays. Each hospitalization is treated as an individual entry in the database and coded with one principal diagnosis, up to 24 secondary diagnoses, and 15 procedural diagnoses associated with that hospital stay. We selected NIS data from 2003 to 2011 to evaluate the trends of hip fracture hospitalizations.
Case Definition
We used the NIS to estimate the total number of hip fractures that required hospitalization and surgical interventions among adult patients (aged 20 years and older) and then classified such admissions into two distinct groups: ESRD and non-ESRD. We included all admissions with a diagnosis code for hip fracture (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] codes of 820). We excluded open hip fractures or pathologic hip fractures. Furthermore, we limited the inclusion to records with a concurrent ICD-9-CM procedure code for surgical treatment or replacement (Supplemental Table 1), in order to avoid over-counting of hip fracture events that might have occurred before the hospitalization.(21) We then used relevant ICD-9-CM codes to classify each patient as having ESRD or not (Supplemental Table 1); we considered patients to have ESRD if they had either the diagnosis codes for ESRD or kidney transplantation or procedural codes for dialysis. We excluded patients undergoing dialysis who concomitantly had an ICD-9-CM code indicating acute kidney injury (AKI) (Supplemental Table 1). We also excluded patients with missing data for age or sex.
Study Variables and Outcomes
We ascertained basic demographic variables and hospital information, and identified the following comorbidities using ICD-9-CM codes (Supplemental Table 1): chronic pulmonary disease, congestive heart failure, diabetes, and hypertension. We determined the type of fracture in each case: femur neck-, intertrochanteric-, or subtrochanteric fracture and we determined the type of treatment: internal fixation, partial hip replacement, or total hip replacement. We also determined in-hospital mortality, lengths of hospital stay, and total hospital costs. Total hospital charges were converted to costs using cost-to-charge ratio files obtained through the Healthcare Cost and Utilization Project.(22) These files contain a hospital-specific cost-to-charge ratio. We focused our analysis on rates of hip fracture over time and trends of clinical characteristics associated with hip fracture. We calculated rates by categories of age (20–54, 55–64, 65–74, 75–84, 85 years or older) and sex (biological male or female). We compared each of these outcomes in the ESRD group with those in the non-ESRD group.
Statistical Analyses
To calculate annual hospitalization rates, we used multiple databases: we used weighted frequencies of hip fracture as the numerator from the NIS,(23) we used the annual number of patients with ESRD from United States Renal Data System (USRDS) Annual Data Report as the denominator for ESRD group,(24) and annual US Census population estimates as the denominator for non-ESRD group.(25,26) We standardized the rate of hip fracture each year in ESRD and non-ESRD group to the age-sex distribution of USRDS 2003 and US census 2003.(27) We summarized demographic and clinical characteristics according to ESRD or not. For categorical variables, we reported proportions and used chi-square tests to compare the differences between ESRD and non-ESRD groups. For continuous variables, costs and length of stay, which were not normally distributed, we reported medians with 10th, 90th percentile ranges and used Kruskal-Wallis tests to assess inter-group differences. We computed a p-value for the trend in hip fracture rates from 2003 to 2011 using linear regression. We examined interactions among the temporal trend in hip fracture, age, and sex. As there was a significant interaction between age and sex, we examined the temporal trend-sex interaction with age stratification (age 20–64 and age ≥65). We also examined the temporal trend-sex interaction by finer age categories: 65–74, 75–84, and 85 or older. We constructed a multivariable logistic regression model to assess determinants of in-hospital mortality in patients with hip fracture. Numbers of annual discharges were weighted to generate national estimates for each year. We created the cohort using SAS software, version 9.4 (SAS Institute, Cary, NC), and conducted the analyses using SAS and StataMP, version 11 (StataCorp, College Station, TX).
RESULTS
National estimates of hip fractures
We estimated 2,954,393 hospitalizations for hip fracture from 2003 to 2011 in the US (Figure 1). Excluding cases of open fracture, pathologic fracture, no relevant hip fracture-related procedure codes or AKI requiring dialysis, 2,539,902 cases remained. Of these, 47,510 were in the ESRD cohort and 2,492,392 were in the non-ESRD cohort.
Figure 1.
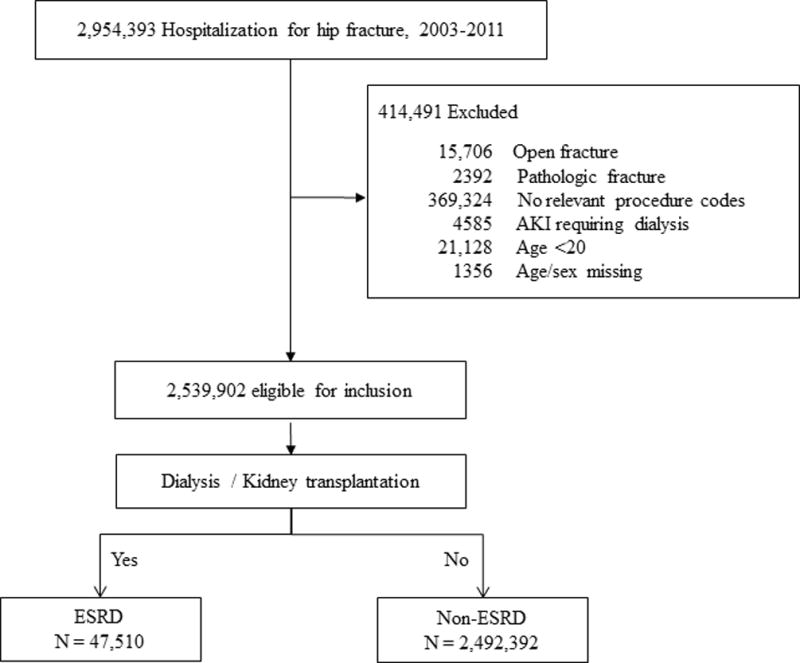
Flow diagram of creating cohorts.
Table 1 describes the demographic characteristics of the study population. The sex distribution differed between ESRD and non-ESRD, with a strong female predominance in non-ESRD that was absent in ESRD. Patients with ESRD and hip fracture were significantly younger than patients without ESRD. There was no detectable difference in the geographic distribution of fractures among patients with and without ESRD, and the geographic distribution in both populations had not materially changed over time. Medicare was the most common primary payer in patients hospitalized for hip fracture (86% in ESRD and 83% in non-ESRD). The proportion of private insurance increased during the study period in ESRD (from 6% in 2003 to 9% in 2011; p for trend = 0.007) and in non-ERSD (from 10% in 2003 to 11% in 2011; p for trend <0.001). More than half of patients with private insurance as primary payer among ESRD were less than 65 years old. Congestive heart failure, diabetes mellitus, and hypertension were more prevalent in ESRD, as expected. The prevalence of diabetes mellitus increased over time in both groups.
Table 1.
Demographic and clinical characteristics of patients with hip fracture operation with and without ESRD
| Year | ESRD
|
non-ESRD
|
||||
|---|---|---|---|---|---|---|
| 2003 | 2007 | 2011 | 2003 | 2007 | 2011 | |
|
|
|
|
||||
| No. of hip fracture | 4597 | 5340 | 5874 | 275,724 | 275,140 | 281,147 |
| Female, N (%) | 2477 (54) | 2746 (51) | 2815 (48) | 199,670 (72) | 194,454 (71) | 198,301 (71) |
| Age, med, (10%–90%), yr | 74 (55–85) | 73 (54–85) | 74 (56–86) | 81 (63–91) | 82 (61–91) | 82 (61–91) |
| Age group, N (%) | ||||||
| 20–54 | 361 (8) | 538 (10) | 455 (8) | 14,864 (5) | 15,505 (6) | 14,482 (5) |
| 55–64 | 596 (13) | 821 (15) | 935 (16) | 15,162 (5) | 18,632 (7) | 22,030 (8) |
| 65–74 | 1287 (28) | 1385 (26) | 1469 (25) | 36,261 (13) | 36,830 (13) | 40,473 (14) |
| 75–84 | 1792 (39) | 1862 (35) | 2083 (35) | 104,560 (38) | 99,138 (36) | 90,625 (32) |
| 85- | 561 (12) | 734 (14) | 933 (16) | 104,878 (38) | 105,035 (38) | 113,537 (40) |
| Region, N (%) | ||||||
| Northeast | 858 (19) | 1000 (19) | 1011 (17) | 53,165 (19) | 50,762 (18) | 50,003 (18) |
| Midwest | 1040 (23) | 1310 (25) | 1413 (24) | 67,825 (25) | 65,533 (24) | 64,564 (23) |
| South | 1726 (38) | 1923 (36) | 2191 (37) | 106,366 (39) | 103,472 (38) | 112,649 (40) |
| West | 974 (21) | 1107 (21) | 1260 (21) | 48,368 (18) | 55,373 (20) | 53,931 (19) |
| Payer, N (%) | ||||||
| Medicare | 4092 (89) | 4659 (87) | 4999 (85) | 233,540 (85) | 226,375 (82) | 232,217 (83) |
| Private | 288 (6) | 369 (7) | 539 (9) | 26,329 (10) | 31,301 (11) | 30,437 (11) |
| All others | 217 (5) | 312 (6) | 336 (6) | 15,855 (6) | 17,464 (6) | 18,492 (7) |
| Hospital teaching, N (%) | ||||||
| Rural | 476 (10) | 451 (8) | 498 (8) | 52,720 (19) | 43,639 (16) | 38,877 (14) |
| Urban-NT | 2089 (45) | 2443 (46) | 2619 (45) | 129,657 (47) | 130,631 (47) | 133,547 (48) |
| Urban-T | 2032 (44) | 2447 (46) | 2758 (47) | 93,347 (34) | 100,869 (37) | 108,723 (39) |
| Bed size, N (%) | ||||||
| Small | 365 (8) | 355 (7) | 565 (10) | 31,087 (11) | 31,766 (12) | 33,679 (12) |
| Medium | 1120 (24) | 1305 (24) | 1218 (21) | 76,433 (28) | 75,237 (27) | 73,175 (26) |
| Large | 3113 (68) | 3680 (69) | 4092 (70) | 168,204 (61) | 168,138 (61) | 174,292 (62) |
| Comorbidity, N (%) | ||||||
| Chronic pulmo disease | 761 (17) | 1003 (19) | 1333 (23) | 55,530 (20) | 59,652 (22) | 60,628 (22) |
| Congestive heart failure | 1309 (28) | 1569 (29) | 1941 (33) | 43,231 (16) | 43,801 (16) | 41,376 (15) |
| Diabetes | 2142 (47) | 2680 (50) | 3127 (53) | 47,748 (17) | 54,418 (20) | 58,213 (21) |
| Hypertension | 3867 (84) | 4772 (89) | 5425 (92) | 148,979 (54) | 170,190 (62) | 193,365 (69) |
Rates of hip fracture
Although the total number of hip fracture hospitalizations among ESRD have increased over time, the unadjusted rate of hospitalization for hip fracture and age- and sex-standardized rate showed a downward trend in ESRD from 2003 to 2011 (Figure 2). Hip fracture rates in patients aged 20–64 were unchanged over time; there was no significant interaction between temporal trend and age. Among older (≥65 years) patients with ESRD, hip fracture rates declined by 15.3% in 2003 to 2011; rates decreased more rapidly in older women relative to older men (p for interaction between temporal trend × sex within older age stratum = 0.047). Among female patients aged 65 years or older, rates declined by 23.9% from 26.50/1000 persons (95% CI, 22.95/1000 to 30.04/1000) in 2003 to 20.17/1000 (95% CI, 17.53/1000 to 22.82/1000) in 2011. When age was stratified into finer groups, a significant interaction was observed only in the 75–84 age group (p for interaction = 0.023). (Supplemental Figure 1). Supplemental Table 2 shows hip fracture rates stratified by age and sex in the ESRD population.
Figure 2.
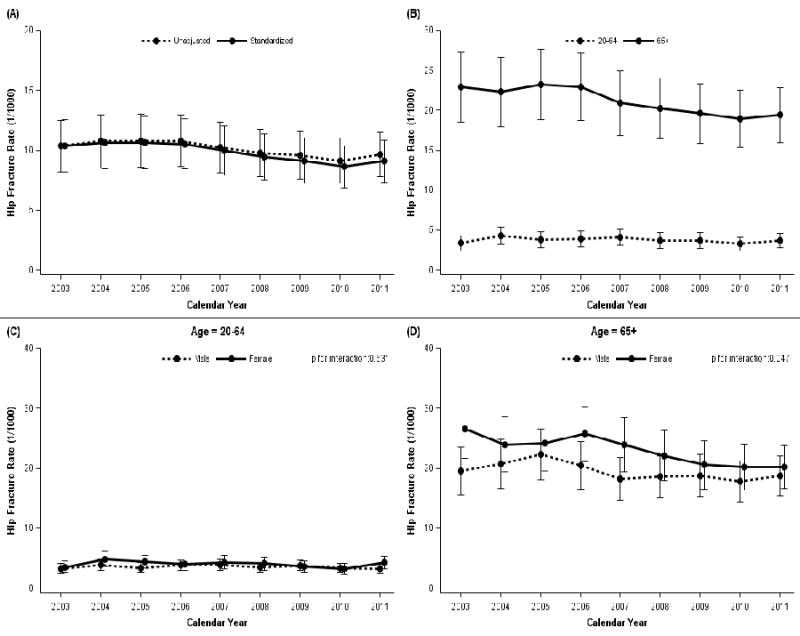
Temporal trends in rate of hip fracture in ESRD population (/1000 persons). (A) Unadjusted and age-sex-standardized rate, (B) by age, (C) by sex (in patients aged 20–64 years old), and (D) by sex (in patients aged 65 or older). Data on hip fracture hospitalization are derived from the NIS, and total ESRD population is estimated from the USRDS.
In patients without ESRD, hip fracture occurred infrequently among patients younger than 65 years, and hip fracture rates were highest among older women (Supplemental Figure 2). Hip fracture rates declined more steeply in older women relative to older men (p for interaction between temporal trends × sex within older age stratum <0.001), particularly in patients aged 85 years or older (Supplemental Figure 3). Supplemental Table 3 shows hip fracture rates stratified by age and sex in the non-ESRD population.
Type of hip fractures
Overall, there were no significant differences over time in terms of type of hip fractures in patients with ESRD. Femur neck fractures (49.2%) and intertrochanteric fractures (44.2%) were two most common types. However, type of hip fractures has changed in patients without ESRD. Femur neck fractures remained major type of fractures, while the proportion of subtrochanteric fractures increased; rates of subtrochanteric hip fracture increased from 2003 (5.7/100,000 persons; 95% CI, 5.1/100,000 to 6.3/100,000) to 2011 (6.5/100,000 persons; 95% CI, 5.8/100,000 to 7.2/100,000) in non-ESRD.
Treatment for hip fractures
Treatment for most patients with hip fracture was internal fixation (65.3% in ESRD), whereas 31.6% of patients underwent a partial hip replacement, and only 2.8% received a total hip replacement. We did not observe any differences between ESRD and non-ESRD. The proportions of each treatment were consistent across the study period in both cohorts.
In-hospital Mortality after hip fracture operation
Overall in-hospital mortality rates were 7.3% in the ESRD group and 2.1% in the non-ESRD group. In ESRD, the hip fracture-associated in-hospital mortality rate steadily declined by 26.7% from 2003 (8.6%; 95% CI, 6.8 to 10.4) to 2011 (6.3%; 95% CI, 4.9 to 7.7). Despite the decreasing trend, in-hospital mortality rates in ESRD were more than 3 times higher than those in non-ESRD in 2011 (6.3% in ESRD versus 1.9% in non-ESRD). After adjusting for age, sex, hospital characteristics, and several comorbid conditions, we observed significantly higher odds of in-hospital mortality after hip fracture operation among patients with ESRD than patients without ESRD (odds ratio 5.90; 95% CI 5.08 to 6.86; Table 2).
Table 2.
Determinants of in-hospital mortality after hip fracture operation
| OR (95% CI) | p value | |
|---|---|---|
| ESRD | 5.90 (5.08–6.86) | <0.001 |
| Male | 1.89 (1.78–2.02) | <0.001 |
| Age | ||
| 20–54 | Reference | N/A |
| 55–64 | 1.66 (1.38–1.98) | <0.001 |
| 65–74 | 2.49 (2.12–2.94) | <0.001 |
| 75–84 | 3.88 (3.32–4.53) | <0.001 |
| 85– | 6.36 (5.46–7.42) | <0.001 |
| Hospital teaching status | ||
| Rural | Reference | N/A |
| Urban non-teaching | 0.93 (0.88–0.99) | 0.033 |
| Urban teaching | 1.03 (0.96–1.10) | 0.455 |
| Chronic pulmonary disease | 1.46 (1.40–1.53) | <0.001 |
| Congestive heart failure | 3.05 (2.85–3.25) | <0.001 |
| Diabetes | 0.79 (0.71–0.87) | <0.001 |
| Hypertension | 0.63 (0.59–0.67) | <0.001 |
Length of Hospital Stay, Hospital Costs, and Disposition
The median (10th, 90th percentile range) duration of hospitalization for hip fracture was 7 (4, 17) days for patients with ESRD, and 5 (3, 10) days for patients without ESRD. Lengths of stay steadily diminished over time in both groups. Median (10th, 90th percentile ranges) hospital costs were $16,219 ($8994, $37,058) in ESRD and $11,991 ($7143, $23,396) in non-ESRD. Costs steadily increased in both ESRD and non-ESRD groups over time. However, costs in patients without ESRD increased more rapidly than those in patients with ESRD (p for interaction <0.001). More than four in five patients were discharged to a nursing facility or intermediate care irrespective of ESRD status.
DISCUSSION
Using a representative national cohort in the US, we observed declining rates of hip fracture in ESRD from 2003 to 2011. Rates declined in older patients, while rates were not materially changed in younger patients. Hip fracture rates declined more rapidly in older women than in older men. Between 2003 and 2011, the proportion of patients with ESRD and hip fracture who were 85 years of age or older increased, as did the burden of comorbidity. Notably, in-hospital mortality and lengths of hospital stay steadily declined.
Several studies have highlighted an increasing trend in hip fracture rates in ESRD between the early 1990s and early 2000s and a decrease after 2004.(16–18) In a study of patients receiving hemodialysis using data from USRDS, hip fracture rates increased steadily from 1993 (11.9/1000 person-years), peaked in 2004 (21.9/1000 person-years), and decreased through 2010 (16.6/1000 person-years).(16) Nair et al. reported on rates of hip fracture in incident patients aged 67 years or older, so that comorbidity could be captured using Medicare claims, and showed similar trends.(17) One study showed a significant temporal increase between 1992 and 2005; thereafter, hip fracture rates decreased in patients treated with hemodialysis but not in patients treated with peritoneal dialysis.(28) The studies cited above demonstrated that hip fracture rates in ESRD in 2009 (2010) were high relative to the 1990s, in contrast to declining rates in the general population in the US. Recently, Hansen et al. reported contradictory findings using a Danish national cohort; in the study by Hansen et al., the authors reported that fracture risk among patients with ESRD had not changed from 2000 to 2011.(29) Possible reasons for the disparate findings include: inclusion of all fractures rather than hip fractures, assessment of trends using 4-year intervals rather than 1-year intervals, and possibly, geographic differences in fracture prevention strategies and/or management of CKD-MBD.
Hip fracture rates in the current study were unchanged in younger patients with ESRD (patients largely excluded from other studies utilizing USRDS data). We previously reported that the relative risk of hip fracture according to kidney function (ESRD versus non-dialysis requiring CKD versus normal or near normal kidney function) was more pronounced in younger age groups.(30) Fractures in older persons are associated with age-related processes including low bone density and strength, decreased functional mobility, impaired neuromuscular function, and an increased risk of falls,(31–33) all of which heighten the risk of hip fracture in older persons with or without ESRD. Younger patients rarely develop osteoporotic hip fractures without kidney disease or other bone and mineral disorders. Among older persons (aged 65 years or older), the downward trend in hip fracture incidence was more pronounced in women relative to men, irrespective of ESRD status. Rates of hip fracture are higher in older women, and hip fracture prevention strategies, including public awareness and fall prevention programs, and the use of calcium + vitamin D and/or anti-resorptive therapy have been directed largely toward post-menopausal women.(34,35) In contrast, the metabolic effects of CKD-MBD occur in both sexes, explaining – at least in part – why there is less female predominance in hip fracture incidence in ESRD.
In general, the type of hip fracture in ESRD was unchanged over time. Fractures of the femoral neck and intertrochanteric fractures were the two most common types of fractures in patients with ESRD, comprising more than 90% of all hip fractures. In contrast, among patients without ESRD, the proportion of subtrochanteric fractures increased, consistent with previous reports.(21) Wang et al. described temporal increases in the incidence of subtrochanteric fracture from 1999 among postmenopausal women, and postulated a relation between subtrochanteric fracture and the increasing use of bisphosphonates.(21) We observed similar trends in patients without ESRD, but not in ESRD; it is noteworthy that bisphosphonates are contraindicated in ESRD. About two-thirds of patients underwent internal fixation, and one third underwent total or partial replacement. This distribution was similar in patients with and without ESRD and did not appear to change materially over time.
Management of CKD-MBD has changed significantly over the past 20 years. In the 1990s, calcium-containing phosphate binders and calcitriol were increasingly used in the management of CKD-MBD. The paradoxical increase in hip fracture rates before 2004 could be explained by the routine use of oral calcium and calcitriol for hyperphosphatemia and secondary hyperparathyroidism, respectively, despite the fact that these agents were used precisely because it was thought that they would reduce fracture rates. It was later recognized that these agents had the potential to over-suppress PTH, which could contribute to bone fragility, especially in patients with undiagnosed osteoporosis and concomitant low bone turnover. With concerns about hypercalcemia and its associated adverse effects, a synthetic vitamin D analog (paricalcitol), a non-calcium containing phosphate binder (sevelamer), and a calcimimetic (cinacalcet) entered the US market in 1998, 2000, and 2004, respectively.(30) other active vitamin D analogs and non-calcium containing phosphate binders were commercially available over the years that followed. Although the lack of medications targeting osteoporosis in ESRD may have contributed to the higher rate of hip fracture relative to patients without ESRD (in whom bisphosphonates have been widely used), differential use of medications for manifestations of CKD-MBD other than osteoporosis (e.g., hyperphosphatemia or secondary hyperparathyroidism) may have contributed to the reduction in hip fracture rates in ESRD over this time frame.(36) Release of clinical practice guidelines and changes in recommended levels of calcium and PTH might also have improved the management of CKD-MBD in more recent years.(11,15)
Strengths of the current study include the large sample size, broad generalizability, inclusion of patients irrespective of age or insurance status, and the availability of multiple diagnosis and procedural codes to adjust for comorbid conditions. Important limitations include the lack of patient-specific follow-up information to determine associations of hip fracture with long-term mortality, cardiovascular events, and other complications. Also, the NIS lacks data on laboratory tests (e.g., serum calcium, phosphorus, PTH, and 25-hydroxy vitamin D) and medications that have been associated with fracture risk in other studies (e.g., glucocorticoids, proton-pump inhibitors, and diuretics). The NIS contains hospital discharge summary data from inpatients only. Therefore, hip fracture events without hospitalization would not be included in this study, although these cases likely represent only a minority of cases overall. Finally, we used multiple data sources to calculate rates of hip fractures among persons with ESRD/non-ESRD (the NIS, the USRDS, and US census). However, considering the broad nature of the NIS sample and the completeness of the USRDS and the US census, estimates from these three databases are likely to be valid.
In summary, using a nationally representative database, we examined rates of hospitalized hip fracture in ESRD over the last decade. We found declining rates of hip fracture; in-hospital mortality rates and lengths of hospital stay also declined. Despite these encouraging trends, hip fracture rates in ESRD remain extremely high, and associated morbidity is considerable. New strategies (pharmacologic and otherwise) are required to further reduce hip fracture rates and rates of associated complications in this high-risk population.
Supplementary Material
Acknowledgments
Dr. Chertow was supported by K24 DK085446.
Authors’ roles:
Study Design: SMK, GMC
Study conduct: NA
Data collection: NA
Data analysis: SMK, SL, JL
Data interpretation: SMK, SL, JL, MEMR, MBL, GMC
Drafting manuscript: SMK, GMC
Revising manuscript content: SMK, SL, JL, MEMR, MBL, GMC
Approving final version of manuscript: SMK, SL, JL, MEMR, MBL, GMC
All authors take responsibility for the integrity of the data analysis.
Dr. Chertow has received research support from Amgen, Inc.
References
- 1.Centers for Disease Control and Prevention. Available at: www.cdc.gov/HomeandRecreationalSafety/Falls/adulthipfx.html. Accessed July 25, 2016.
- 2.Riggs BL, Melton LJ., 3rd The prevention and treatment of osteoporosis. N Engl J Med. 1992;327(9):620–7. doi: 10.1056/NEJM199208273270908. [DOI] [PubMed] [Google Scholar]
- 3.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res. 2007;22(3):465–75. doi: 10.1359/jbmr.061113. [DOI] [PubMed] [Google Scholar]
- 4.Morrison RS, Chassin MR, Siu AL. The medical consultant’s role in caring for patients with hip fracture. Ann Intern Med. 1998;128(12 Pt 1):1010–20. doi: 10.7326/0003-4819-128-12_part_1-199806150-00010. [DOI] [PubMed] [Google Scholar]
- 5.Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302(14):1573–9. doi: 10.1001/jama.2009.1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stevens JA, Anne Rudd R. Declining hip fracture rates in the United States. Age Ageing. 2010;39(4):500–3. doi: 10.1093/ageing/afq044. [DOI] [PubMed] [Google Scholar]
- 7.Stafford RS, Drieling RL, Hersh AL. National trends in osteoporosis visits and osteoporosis treatment, 1988–2003. Arch Intern Med. 2004;164(14):1525–30. doi: 10.1001/archinte.164.14.1525. [DOI] [PubMed] [Google Scholar]
- 8.Alem AM, Sherrard DJ, Gillen DL, et al. Increased risk of hip fracture among patients with end-stage renal disease. Kidney Int. 2000;58(1):396–9. doi: 10.1046/j.1523-1755.2000.00178.x. [DOI] [PubMed] [Google Scholar]
- 9.Coco M, Rush H. Increased incidence of hip fractures in dialysis patients with low serum parathyroid hormone. Am J Kidney Dis. 2000;36(6):1115–21. doi: 10.1053/ajkd.2000.19812. [DOI] [PubMed] [Google Scholar]
- 10.Maravic M, Ostertag A, Torres PU, Cohen-Solal M. Incidence and risk factors for hip fractures in dialysis patients. Osteoporos Int. 2014;25(1):159–65. doi: 10.1007/s00198-013-2435-1. [DOI] [PubMed] [Google Scholar]
- 11.National Kidney F. K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis. 2003;42(4 Suppl 3):S1–201. [PubMed] [Google Scholar]
- 12.Larsson T, Nisbeth U, Ljunggren O, Juppner H, Jonsson KB. Circulating concentration of FGF-23 increases as renal function declines in patients with chronic kidney disease, but does not change in response to variation in phosphate intake in healthy volunteers. Kidney Int. 2003;64(6):2272–9. doi: 10.1046/j.1523-1755.2003.00328.x. [DOI] [PubMed] [Google Scholar]
- 13.Stehman-Breen C. Osteoporosis and chronic kidney disease. Semin Nephrol. 2004;24(1):78–81. doi: 10.1053/j.semnephrol.2003.08.013. [DOI] [PubMed] [Google Scholar]
- 14.Cunningham J, Sprague SM, Cannata-Andia J, et al. Osteoporosis in chronic kidney disease. Am J Kidney Dis. 2004;43(3):566–71. doi: 10.1053/j.ajkd.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 15.Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD) Kidney Int Suppl. 2009;(113):S1–130. doi: 10.1038/ki.2009.188. [DOI] [PubMed] [Google Scholar]
- 16.Arneson TJ, Li S, Liu J, Kilpatrick RD, Newsome BB, St Peter WL. Trends in hip fracture rates in US hemodialysis patients, 1993–2010. Am J Kidney Dis. 2013;62(4):747–54. doi: 10.1053/j.ajkd.2013.02.368. [DOI] [PubMed] [Google Scholar]
- 17.Nair SS, Mitani AA, Goldstein BA, Chertow GM, Lowenberg DW, Winkelmayer WC. Temporal trends in the incidence, treatment, and outcomes of hip fracture in older patients initiating dialysis in the United States. Clin J Am Soc Nephrol. 2013;8(8):1336–42. doi: 10.2215/CJN.10901012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wagner J, Jhaveri KD, Rosen L, Sunday S, Mathew AT, Fishbane S. Increased bone fractures among elderly United States hemodialysis patients. Nephrol Dial Transplant. 2014;29(1):146–51. doi: 10.1093/ndt/gft352. [DOI] [PubMed] [Google Scholar]
- 19.Beaubrun AC, Kilpatrick RD, Freburger JK, Bradbury BD, Wang L, Brookhart MA. Temporal trends in fracture rates and postdischarge outcomes among hemodialysis patients. J Am Soc Nephrol. 2013;24(9):1461–9. doi: 10.1681/ASN.2012090916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project: Introduction to the HCUP nationwide Inpatient Sample (NIS) 2011 Available at: https://www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2011.jsp. Accessed July 10, 2015.
- 21.Wang Z, Bhattacharyya T. Trends in incidence of subtrochanteric fragility fractures and bisphosphonate use among the US elderly, 1996–2007. J Bone Miner Res. 2011;26(3):553–60. doi: 10.1002/jbmr.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Healthcare Cost and Utilization Project (HCUP) Cost-to-charge ratio files. Available at: http://www.hcup-us.ahrq.gov/db/state/costtocharge.jsp Accessed July 24, 2016.
- 23.Agency for Healthcare Research and Quality. The Healthcare cost and utilization project. Introduction to the HCUP nationwide Inpatient Sample (NIS) 2011 Available: https://www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2011.jsp. Accessed October 14, 2015.
- 24.United States Renal Data System. Annual Data Report Reference Tables. Available at: http://www.usrds.org/reference.aspx. Accessed July 26, 2016.
- 25.US Census Bureau. US Census. :2010. Available at: http://www.census.gov/prod/cen2010/briefs/c2010br-03.pdf. Accessed July 26, 2016.
- 26.US Census Bureau. CPS data on Age and Sex. Available at: http://www.census.gov/population/age/data/cps.html. Accessed July 27, 2016.
- 27.Anderson RN, Rosenberg HM. Age standardization of death rates: implementation of the year 2000 standard. Natl Vital Stat Rep. 1998;47(3):1–16, 20. [PubMed] [Google Scholar]
- 28.Mathew AT, Hazzan A, Jhaveri KD, et al. Increasing hip fractures in patients receiving hemodialysis and peritoneal dialysis. Am J Nephrol. 2014;40(5):451–7. doi: 10.1159/000369039. [DOI] [PubMed] [Google Scholar]
- 29.Hansen D, Olesen JB, Gislason GH, Abrahamsen B, Hommel K. Risk of fracture in adults on renal replacement therapy: a Danish national cohort study. Nephrol Dial Transplant. 2016;31(10):1654–62. doi: 10.1093/ndt/gfw073. [DOI] [PubMed] [Google Scholar]
- 30.Kim SM, Long J, Montez-Rath M, Leonard M, Chertow GM. Hip Fracture in Patients With Non-Dialysis-Requiring Chronic Kidney Disease. J Bone Miner Res. 2016;31(10):1803–9. doi: 10.1002/jbmr.2862. [DOI] [PubMed] [Google Scholar]
- 31.Verhaar HJ, Samson MM, Jansen PA, de Vreede PL, Manten JW, Duursma SA. Muscle strength, functional mobility and vitamin D in older women. Aging (Milano) 2000;12(6):455–60. doi: 10.1007/BF03339877. [DOI] [PubMed] [Google Scholar]
- 32.Dhesi JK, Bearne LM, Moniz C, et al. Neuromuscular and psychomotor function in elderly subjects who fall and the relationship with vitamin D status. J Bone Miner Res. 2002;17(5):891–7. doi: 10.1359/jbmr.2002.17.5.891. [DOI] [PubMed] [Google Scholar]
- 33.Yenchek R, Ix JH, Rifkin DE, et al. Association of serum bicarbonate with incident functional limitation in older adults. Clin J Am Soc Nephrol. 2014;9(12):2111–6. doi: 10.2215/CJN.05480614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kiebzak GM, Beinart GA, Perser K, Ambrose CG, Siff SJ, Heggeness MH. Undertreatment of osteoporosis in men with hip fracture. Arch Intern Med. 2002;162(19):2217–22. doi: 10.1001/archinte.162.19.2217. [DOI] [PubMed] [Google Scholar]
- 35.Feldstein A1, Elmer PJ, Orwoll E, Herson M, Hillier T. Bone mineral density measurement and treatment for osteoporosis in older individuals with fractures: a gap in evidence-based practice guideline implementation. Arch Intern Med. 2003;163(18):2165–72. doi: 10.1001/archinte.163.18.2165. [DOI] [PubMed] [Google Scholar]
- 36.Moe SM, Abdalla S, Chertow GM, et al. Effects of Cinacalcet on Fracture Events in Patients Receiving Hemodialysis: The EVOLVE Trial. J Am Soc Nephrol. 2015;26(6):1466–75. doi: 10.1681/ASN.2014040414. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


