Although neutrophils are a histologic hallmark of psoriasis, it is unclear whether neutrophils are simply effector cells or drive pathogenesis. A recent psoriasis study with murine models evaluated various chemokines, lipids, and cytokines proposing that neutrophils are key players in positive feedback loops perpetuating the disease.1 Additionally, when neutrophils are depleted in pustular psoriasis, the disease drastically improves.2 There is mounting evidence supporting the use of neutrophil to lymphocyte ratio (NLR) as a marker of inflammation in active psoriasis. While absolute neutrophil counts (ANC) varies significantly amongst individuals, NLR may serve as an individually-normalized measure of relative neutrophil counts in psoriasis patients, and has been shown to be elevated in psoriasis patients with severe disease.3–5
To better understand the relationship between psoriasis area severity index (PASI) and NLR, we evaluated how the NLR changed as psoriasis is effectively treated and PASI declines. We conducted a retrospective chart review of plaque psoriasis patients from the Mount Sinai (MS) Medical Center, New York, NY who had completed unblinded clinical trials with therapeutic antibodies, brodalumab and ustekinumab. The improvement threshold was a PASI decrease over 50% at week 12, which is a clinically significant endpoint to stratify treatment response and meaningful change in quality of life6. No patients treated with placebo had a PASI decrease over 50%. The experimental groups consisted of 18 patients on brodalumab and 12 patients on ustekinumab who responded to treatment, as well as 7 placebo patients. A total of 5 treatment non-responders (patients on brodalumab or ustekinumab who did not achieve PASI50) were also included in further analysis. The absolute neutrophil count and the absolute lymphocyte value from each patient’s laboratory blood test (units x 103/μL) and PASI scores at week 0 and 12 were documented. The NLR was calculated by dividing the absolute neutrophil count by the absolute lymphocyte count. The reviewers who recorded the PASI were blinded. Statistical analyses were performed using GraphPad Prism 6.0. To compare the NLR for each group at weeks 0 and 12, multiple unpaired t-tests were used and statistical significance (P<0.05) was determined using the Holm-Sidak method. A Pearson correlation was also calculated for initial PASI score and the NLR.
Our findings showed that after 12 weeks there was no significant change in the NLR of placebo patients whereas a significant reduction was observed in NLR of antibody-treated patients (P<0.05) (Fig. 1). Contrary to an earlier study by Kim et al. 2015, we did not find a correlation between the baseline PASI and NLR, which confirms previous results by Ataseven et al. 2014, since our calculated Pearson correlation was 0.013 (P=0.938).4,5
Figure 1.
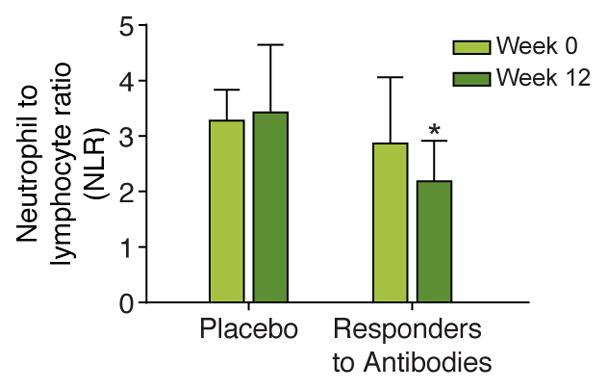
Neutrophil to lymphocyte ratio (NLR) measured in psoriasis patients 12 weeks after placebo or antibody treatment. Bars denote the average for each experimental condition, and error bars indicate standard deviations. P value significance (*, P < 0.05) was calculated by multiple unpaired t-tests and adjusted by use of the Holm-Sidak method.
As treatment with therapeutic antibodies may modulate neutrophil function and may directly affect NLR, we also examined the difference in NLR between treatment responders and non-responders. We found that treatment responders had a significant reduction in NLR (P=0.005) whereas treatment non-responders did not (P=0.092) (Fig. 2).
Figure 2.

Neutrophil to lymphocyte ratio (NLR) comparing responders versus non-responders after 12 weeks of antibody treatment in psoriasis patients. Bars denote the average for each experimental condition, and error bars indicate standard deviations. Responders show a significant decrease in NLR (p=0.005), and non-responders do not show any significant change in NLR (p= 0.092). P value significance (*, P < 0.05) was calculated by multiple unpaired t-tests and adjusted by use of the Holm-Sidak method.
Our results suggest that as psoriasis patients respond to treatment with therapeutic antibodies, their NLR decreases concurrently with decrease in PASI. Only patients who improved on treatment had a decreased NLR, suggesting a key role for neutrophils in the pathogenesis of psoriasis. This critically shows that decrease in NLR is reflective of underlying disease activity and not simply a treatment effect. Thus, NLR may serve as a corollary blood value in psoriasis patients for response to treatment, which can be easily calculated from a routine blood test.
Future investigation of mechanisms underlying this change in systemic NLR may be helpful to understand the pathophysiology of psoriasis, with the potential to develop novel diagnostic and therapeutic options.
Acknowledgments
Statement of Funding: L.R.M. was supported by the National Institute of General Medical Sciences of the US NIH under award number R15GM117501.
Footnotes
Disclosure Statement: None of the authors have any conflicts of interest to disclose.
IRB Approval: This study was approved by the Icahn School of Medicine at Mount Sinai institutional review board (HS#: 15-01051).
References
- 1.Sumida H, Yanagida K, Kita Y, et al. Interplay between CXCR2 and BLT1 Facilitates Neutrophil Infiltration and Resultant Keratinocyte Activation in a Murine Model of Imiquimod-Induced Psoriasis. J Immunol. 2014;192(9):4361–9. doi: 10.4049/jimmunol.1302959. [DOI] [PubMed] [Google Scholar]
- 2.Ikeda S, Takahashi H, Suga Y, et al. Therapeutic Depletion of Myeloid Lineage Leukocytes in Patients with Generalized Pustular Psoriasis Indicates a Major Role for Neutrophils in the Immunopathogenesis of Psoriasis. J Am Acad Dermatol. 2013;68(4):609–17. doi: 10.1016/j.jaad.2012.09.037. [DOI] [PubMed] [Google Scholar]
- 3.Yamanaka K, Umezawa Y, Yamagiwa A, et al. Biologic Therapy Improves Psoriasis by Decreasing the Activity of Monocytes and Neutrophils. J Dermatol. 2014;41(8):679–85. doi: 10.1111/1346-8138.12560. [DOI] [PubMed] [Google Scholar]
- 4.Kim DS, Shin D, Lee MS, et al. Assessments of Neutrophil to Lymphocyte Ratio and Platelet to Lymphocyte Ratio in Korean Patients with Psoriasis Vulgaris and Psoriatic Arthritis. J Dermatol. 2015;43(3):305–10. doi: 10.1111/1346-8138.13061. [DOI] [PubMed] [Google Scholar]
- 5.Ataseven A, Bilgin AU, Kurtipek GS, et al. The Importance of Neutrophil Lymphocyte Ratio in Patients with Psoriasis. Mater Sociomed. 2014;26(4):231–3. doi: 10.5455/msm.2014.231-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carlin CS, Feldman SR, Kreuger JG, Menter A, Kreuger GG. A 50% reduction in the Psoriasis Area and Severity Index (PASI 50) is a clinically significant endpoint in the assessment of psoriasis. J Am Acad Dermatol. 2004;50(6):859–66. doi: 10.1016/j.jaad.2003.09.014. [DOI] [PubMed] [Google Scholar]


