Abstract
Purpose of Review
The purpose of this review is to outline the natural history and best clinical practices for nonoperative management of anterior shoulder instability.
Recent Findings
Recent studies continue to demonstrate a role for nonoperative treatment in the successful long-term management of anterior glenohumeral instability. The success of different positions of shoulder immobilization is reviewed as well.
Summary
There are specific patients who may be best treated with nonoperative means after anterior glenohumeral instability. There are also patients who are not good nonoperative candidates based on a number of factors that are outlined in this review. There continues to be no definitive literature regarding the return to play of in-season athletes. Successful management requires a thorough understanding of the epidemiology, pathoanatomy, history, physical examination, diagnostic imaging modalities, and natural history of operative and nonoperative treatment.
Keywords: Anterior glenohumeral instability, Nonoperative instability, Anterior shoulder instability, Natural history
Introduction
Anterior glenohumeral instability is a common problem in young athletic populations. The incidence of anterior shoulder instability in the general United States (US) population is 0.08 per 1000 person-years [1, 2]. Specific at-risk young males have anterior instability at an order of magnitude greater than the general population, with rates as high as 3% per year [2, 3]. Furthermore, collision athletes, such as football and rugby players, have incidence rates as high as 0.51 per 1000 athlete exposures [4]. Ten percent of NFL combine participants reported a history of shoulder instability, and a recent study found a 14.8% rate of shoulder dislocation among 374 high school rugby athletes [5]. The incidence in military personnel, estimated as 1.69 per 1000 person-years, is considerably higher than both the general population and contact athletes [1].
Anatomy and Pathogenesis
Shoulder instability is characterized by the disruption of the native dynamic and static stabilizers of the glenohumeral joint, leading to dislocation, subluxation, or apprehension with associated pain. The articular conformity, negative intra-articular pressure, glenoid labrum, and glenohumeral ligament complex, specifically the anterior and posterior bands of the inferior glenohumeral ligament (IGHL), are critical to maintenance of shoulder stability. Additionally, the rotator cuff and scapular stabilizers are important dynamic sources of restraint [6]. It is well known that osseous defects of the glenoid and humeral head defects contribute significantly to the risk of subsequent instability, and the glenoid track concept [7] has assisted in the identification of engaging, high-risk lesions. Recently, studies have also shown that scapular morphology measurements, such as increased glenoid version and inferior inclination, are associated with anterior shoulder instability [8–10]. In addition, the respective roles of hormonal influence and variable gene expression have also been evaluated. Owens et al. found an association of shoulder instability with elevated serum relaxin concentration [11], whereas reduced local gene expression of COL5A1 in the shoulder capsule may contribute to increased risk in selected patients [12–14].
Commonly known as a Bankart lesion, anterior–inferior labral disruption is the most common pathoanatomic feature of an anterior shoulder instability event that is seen in up to 96% of patients that presents with both subluxation and dislocation events [15]. A combination of plastic deformation and/or compromise of the anterior inferior capsule, IGHL complex, and labrum often contributes to recurrent anterior instability [16], and certain variants may include anterior labral ligamentous periosteal sleeve avulsion (ALPSA) [17], humeral avulsion of the glenohumeral ligament (HAGL), glenolabral articular disruption (GLAD), bony Bankart tear, and Hill–Sachs lesions.
History, Presentation, and Physical Examination
Evaluation of the patient with suspected anterior shoulder instability should begin with a thorough history of the index injury and antecedent shoulder function, including arm dominance and level and type of sporting competition. The mechanism of injury (e.g., high- vs. low-energy, contact-related vs. atraumatic) can also offer useful insights on the extent of injury, while also informing potential workup modalities and strategies for management. It is of paramount importance to comprehensively document the natural history of shoulder instability, including age of first instability event, number of dislocation and/or subluxation, requirement for manual reduction and/or sedation in an emergency room setting, position of instability event, and any prior nonoperative or surgical intervention [18]. Apprehension or instability events in lower degrees of abduction (i.e., below shoulder level) or during sleep may also serve as a harbinger of more complex instability that may involve significant bone loss.
Physical examination should consist of inspection, palpation, and range of motion assessment, with comparison to the contralateral shoulder [19]. Increased external rotation may imply anterior hyperlaxity, and asymmetric hyperabduction greater than 15° difference from the contralateral shoulder (Gagey’s test) with scapular stabilization may indicate incompetency of the IGHL complex. Neurovascular examination is also relevant to exclude the presence of associated injuries, particularly the axillary nerve due to its tethered position in close proximity to the zone of injury. Resting and dynamic scapular position throughout an overhead arc of motion should also be carefully scrutinized, as scapular dyskinesis may unmask underlying shoulder laxity or exacerbate prior history of shoulder instability. Despite the value of these findings, special testing is often considered the most critical portion of the examination. Apprehension and Jobe relocation tests are considered the most diagnostic for identifying anterior shoulder instability, with a positive predictive value of 96% [20]. Additional special tests include the sulcus sign for inferior instability, anterior and posterior load, and shift. The Jerk test, Kim test, and push–pull exam maneuvers will help exclude posterior instability and multidirectional instability, while pathology of the biceps–superior labral complex may also be assessed with O’Brien’s test, Crank test, dynamic labral shear test, and Yergason’s test.
Diagnostic Imaging
Standard orthogonal radiographs should be obtained, consisting of anteroposterior (AP) scapular Y, and axillary lateral (Figs. 1, 2, and 3). Special views may also be obtained prior to magnetic resonance imaging (MRI), potentially with arthrogram (MRA) (Fig. 4) in order to further elucidate any glenoid or humeral head defects. The West Point and Bernageau views assist in identification of anteroinferior bony glenoid injuries, and the Stryker notch view will best show a Hill–Sachs lesion [21]. Computed tomography (CT) and MRAs are indicated to identify concomitant injuries and are useful in assessing the size and morphology of glenoid and humeral head defects (Fig. 5) [22–25]. Specifically, three-dimensional reconstructions with digital humeral head subtraction offers an en-face view of the glenoid (Fig. 6) and allows better characterization of attritional anterior–inferior bone loss using established techniques [26].
Fig. 1.
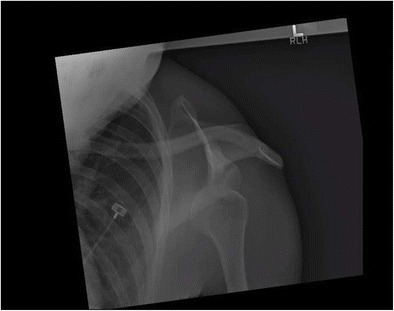
Anteroposterior radiograph of an anteriorly dislocated left glenohumeral joint. Note the oblique angle of the radiograph which is common due to patient discomfort and difficulty with positioning
Fig. 2.
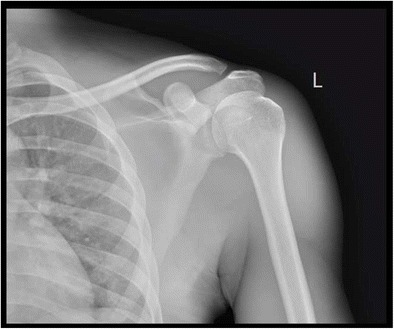
Anteroposterior radiograph of the same patient from Fig. 1 after a successful reduction
Fig. 3.
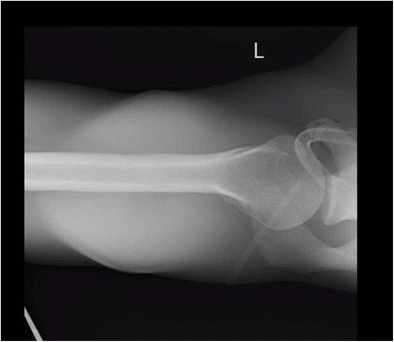
Axillary radiograph of the same patient from Fig. 1 after a successful reduction. This radiograph is essential in confirming a congruent joint after reduction and should not be deferred due to perceived difficulty in obtaining it
Fig. 4.
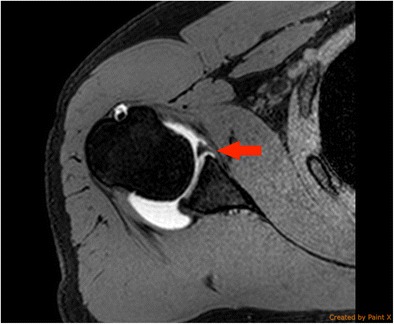
Axial cut of an MR arthrogram of a patient who sustained an anterior glenohumeral dislocation demonstrating a large anterior labral tear with fluid extravasation under the anterior labrum (arrow)
Fig. 5.
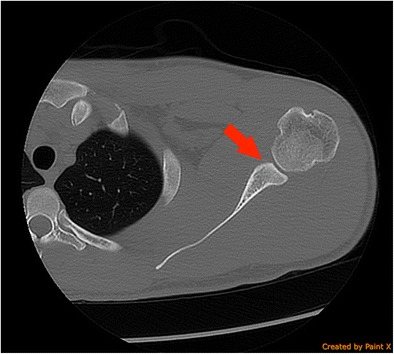
Axial cut of a CT scan of a patient who has sustained multiple anterior glenohumeral dislocations demonstrating the chronic finding of anterior glenoid bone loss (arrow)
Fig. 6.
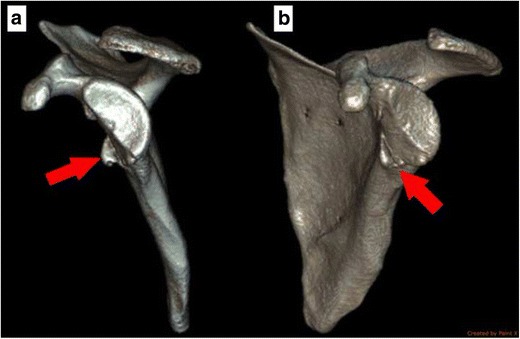
Three-dimensional reconstructions of a CT scan of a patient who has sustained multiple anterior glenohumeral dislocations demonstrating the finding of significant anterior glenoid bone loss. The en-face view (a) demonstrates the anterior bone loss as well as the medialized bone (arrow). A rotated view (b) better demonstrates the medialized anterior bone (arrow)
Natural History of Nonoperative Management
Treatment of anterior shoulder instability requires a thorough understanding of the natural history. The outcomes of nonoperative treatment of anterior shoulder instability are variable and are significantly dependent on patient age. Hovelius and Rahme published a landmark article in which they describe the long-term prognosis in 257 first-time anterior shoulder dislocations in patients less than 40 years old. They found that approximately two thirds of patients had shoulder arthritis at a mean of 25-year follow-up. Additionally, almost half of patients less than 25 years old required surgical stabilization [27]. Robinson et al. prospectively followed 252 patients, less than 35 years old, who sustained an anterior glenohumeral dislocation and were treated with sling immobilization, followed by a physical therapy program. Recurrent instability developed in 55.7% of the shoulders within the first 2 years and increased to 66.8% at 5-year follow-up [28]. Younger male patients were most at risk of recurrent anterior instability. Simonet and Cofield tracked the natural history of nonoperatively treated anterior instability in 116 patients at a mean of 4.6-year follow-up, and they documented an overall 33% rate of recurrent instability. However, patients less than 20 years old had a 66% rate of recurrence, while 82% of athletes sustained a recurrent dislocation versus 30% among patients not involved in athletics [29, 30]. Henry and Genung studied the natural history of 121 young athletes, mean age 19 years old, treated nonoperatively for an acute first-time traumatic anterior shoulder dislocation. One hundred six patients (88%) sustained a recurrent dislocation, and all repeat injuries occurred prior to 18 months after initial instability event [31]. A recent meta-analysis pooled the results of 15 level I and II studies to determine the natural history of nonoperatively treated traumatic anterior shoulder instability. In this investigation, the authors identified an overall 21% recurrence rate, with a rate approaching 80% for males less than 20 years old [32].
Operative Versus Nonoperative Treatment
Operative treatment of anterior shoulder instability has been well studied, especially in young athletic populations. In contrast to nonoperative management, surgical treatment for first-time anterior shoulder dislocations in young patients has often been recommended in order to reduce a risk of recurrent instability and further damage to the glenohumeral joint. There have now been multiple studies examining the long-term success of nonoperative treatment of anterior shoulder instability (Table 1). Initial studies evaluating military cadets demonstrated a high rate of instability recurrence with nonoperative treatment compared to arthroscopic Bankart repair. In a comparative series of first-time anterior shoulder dislocations in West Point cadets, Wheeler et al. found 92% recurrent instability in the nonoperative versus 22% in the operative treatment group [43]. Arciero and colleagues prospectively studied nonoperative management versus arthroscopic Bankart repair for first-time anterior shoulder dislocators at the United States Military Academy (USMA). Eighty (80%) percent of nonoperatively treated patients and 14% of patients who underwent arthroscopic Bankart repair had recurrent instability at an average of 32-month follow-up [44]. Two- to five-year follow-up of this young athletic population showed a continued benefit to operative stabilization over nonoperative treatment [45]. Bottoni et al. performed a prospective randomized controlled trial comparing nonoperative sling management versus early arthroscopic Bankart repair for young athletes with first-time anterior shoulder dislocations. At an average 36-month follow-up, 75% of patients treated nonoperatively had recurrent instability versus 11.1% in the arthroscopic stabilization group [46]. Multiple recent studies have shown a reduction in recurrent anterior shoulder instability in young athletes with operative stabilization versus nonoperative treatment [47–49].
Table 1.
Success of nonoperative treatment of anterior glenohumeral instability
| Study | Level of evidence | No. of patients | Age | Treatment/intervention | Recurrence rate/outcomes | Length of follow-up |
|---|---|---|---|---|---|---|
| Henry and Genung, Am J Sports Med, 1982 | IV | 120 young athletes | 19 years | 62 immobilized with shoulder immobilizer and sling and swath 3–6 weeks; 59 with no immobilization | 90% recurrence in immobilized patients, 85% recurrence when not immobilized | 18 months |
| Simonet et al., Clin Orthop Relat Res, 1984 | IV | 116/124 (93.5% follow-up) | N/A | Nonoperative | 33% overall; 82% in young athletes (< 20 years) | 4.6 years |
| Wheeler et al., Arthroscopy, 1989 | II | 47 | Military cadets | Arthroscopic repair (9) vs. nonoperative (38) treatment | Nonoperative, 92% recurrence Operative, 22% recurrence |
14 months |
| Arciero et al., Am J Sports Med, 1994 | I | 36 | Avg 20 years | Arthroscopic repair and rehabilitation (21); nonoperative, 1 month immobilization, and rehabilitation, full activity at 4 months (15) | Nonoperative, 80% recurrence Operative, 14% recurrence |
Avg 32 months |
| Bottoni et al., Am J Sports Med, 2002 | I | 21/24 (87.5% follow-up) | Avg 22.4 years | Nonoperative: 4 weeks of immobilization followed by rehab Operative: arthroscopic Bankart repair followed by the same rehab |
Nonoperative, 75% recurrence Operative, 11.1% recurrence |
3 years |
| Brophy and Marx, Arthroscopy, 2009 | IV (systematic review) | All studies comparing operative vs. nonoperative treatment | N/A | Nonoperative vs. operative stabilization | Nonoperative, 46% recurrence Operative, 7% recurrence |
2 years |
| Kirkley et al., Arthroscopy, 2005 [33] | II | 31 | Avg 23 years (all patients < 30 years) | Nonoperative: immobilization (3 weeks) and rehabilitation Operative: arthroscopic stabilization |
Nonoperative, 60%; operative, 19% No significant difference in shoulder function by ASES/DASH Minimal significant improvement with WOSI in the operative group |
75 months |
| Robinson et al., J Bone Joint Surg Am, 2006 | III | 252 | 15–35 years | Sling followed by physical therapy | 55.7% had recurrence in first 2 years, and 66.8% by 5 years | 5 years |
| Jakobsen et al., Arthroscopy, 2007 | I | 76 | 15–39 years | Conservative: diagnostic arthroscopy and 1-week sling, followed by therapy Operative: open Bankart repair |
At 2 years, 54% recurrence in the conservative group, 3% in the operative group At 10 years, 74% unsatisfactory results in conservative, 72% good or excellent results in the operative group |
10 years |
| Spiegl et al., BMC Musculoskelet Disord, 2013 [34] | IV | 25 with bony Bankart lesions | 12 nonop, 13 op | Operative if bony Bankart ≥ 5% Nonoperative if bony Bankart < 5% |
Nonoperative: good/excellent Rowe score in 83% with 25% subjective instability Operative: good to excellent Rowe score in 85% with 8% subjective instability |
2 years |
| Dickens et al., Am J Sports Med, 2014 | II | 45, in-season collegiate athletes | Avg 20.7 years | Accelerated rehabilitation without immobilization | 73% return to sport all or some of the season; 67% completed season; 27% completed without recurrence; 64% returned to play but had recurrence | Single season |
| Gigis et al., JPO, 2014 [35] | II | 65 (38 operative and 27 conservative) | 15–18 years | Nonoperative: immobilization and rehabilitation Operative: arthroscopic stabilization |
Nonoperative, 70.3% recurrence Operative, 13.1% recurrence |
36 months |
| Kawasaki et al., J Shoulder Elb Surg, 2014 | III | 378; in-season high school rugby players | 14–18 years | Nonoperative | 14.8% incidence of dislocation with recurrence rate of 54.3% | Single season |
| Khan et al., Bone Joint J, 2014 [36] | IV | 49/80 (61.3% follow-up) | Skeletally immature patients | Conservative treatment vs. Latarjet procedure | 92% operative returned to same level of activity vs. 52% for nonoperative |
N/A |
| Konigshausen, Musculoskelet Surg, 2014 [37] | III | 26/28 (93% follow-up) | 29.3 years | Immobilized in external rotation | 15% recurrence rate | 5 years |
| Leroux et al., Am J Sports Med, 2014 [38] | II | 20,719 | 17–69 years (avg 35 years) | All-comers receiving closed reduction of an anterior shoulder dislocation | 19% incidence of repeat closed reduction Highest in ≤ 20 years Reduction by orthopedist, humeral tuberosity fracture, older age, and more medical comorbidities are protective. Males and low-income areas are risk factors |
2 years |
| Liu et al., Injury, 2014 [39] | I, meta-analysis | 663 | N/A | 338 external immobilization vs. 325 internal immobilization | No difference in recurrence rates between the two types of immobilization | N/A |
| Longo, Arthroscopy, 2014 [40] | IV, systematic review | 2813 | N/A | Compared recurrence in nonoperative vs. operative patients | Recurrence is lower with operative treatment (OR 12.71; 95% CI 5.88–33.1; p < 0.00001) | N/A |
| Olds et al., Br J Sports Med, 2015 | IV, meta-analysis | 1324 | > 18 years with primary anterior shoulder dislocation | Nonoperative | 39% recurrence rate Risk factors are < 40 years, men, and hyperlaxity Protective factors are greater tuberosity fracture |
N/A |
| Riccio et al., Musculoskelet Surg, 2015 | IV | 32 | 20–44 | 3-month conservative treatment protocol | Rowe score for instability improved from 44.5 to 79.8; 78% of patients with good to excellent results with nonoperative treatment | 2 years |
| Roberts et al., Bone Joint J, 2015 | III | 133 | 16.3 years (13–18) | Nonoperative | 76.7% recurrence at mean of 10 months | 95.2 months |
| Leroux et al., Am J Sports Med, 2015 | II | 1937 | 10–16 years (avg 15 years) | All-comers receiving closed reduction of an anterior shoulder dislocation | 38.2% incidence of repeat closed reduction Higher in 14–16 years old Male sex and older age are risk factors for recurrence |
Min of 2 years |
| Hovelius et al., KSSTA, 2016 [41] | III | 257 | 12–40 years | Half of patients immobilized 3–4 weeks and half started with early motion | Recurrence increased up to 10-year follow-up After 25 years, 29% of shoulders with ≥ 2 recurrences stabilized over time. 34% moderate to severe and 27% mild arthropathy at 25 years Age < 25 years and bilateral instability equal to poor prognosis while greater tuberosity fracture equals to a favorable prognosis |
25 years |
| Olds et al., Br J Sports Med, 2016 [42] | IV, meta-analysis | N/A | < 19 years with primary anterior shoulder dislocation | Nonoperative | 73% recurrence Risk factors: older age, male sex, shoulder dominance and injury side, mechanism of injury, state of physis closure, and Hill–Sachs and Bankart lesions |
N/A |
| Wasserstein et al., Arthroscopy, 2016 | II, systematic review | N/A | N/A | Nonoperative | 19–88% recurrence rate with nonoperative treatment Male sex and age < 20 years are risk factors. Greater tuberosity fracture is protective |
2 years |
| Watson et al., Sports Health, 2016 | IV, systematic review | N/A | N/A | In-season athlete return to play considerations | 37–90% | Single season |
| Whalen et al., Am J Sports Med, 2016 [57] | I, meta-analysis | 632 | 30.1 years in ER vs. 30.3 in IR | External vs. internal immobilization | No difference in recurrence (RR 0.69, 95% CI, 0.042–1.14, p = 0.15) | N/A |
Jakobsen et al. evaluated patients (nonspecific athletes) of ages 15–39 presenting after a first-time anterior shoulder dislocation with arthroscopy to characterize the labral damage and then randomized patients to nonoperative treatment versus open Bankart repair [50]. Patients then went through an identical rehabilitation program consisting of a sling for 1 week and then initiation of motion. After an 8-year follow-up, 74% of patients treated without surgical repair had unsatisfactory results, whereas 72% of surgically repaired patients had good or excellent results. Among surgical options, there remains controversy as to the ideal technique to prevent long-term anterior shoulder instability [51, 52].
Post-reduction Immobilization
There is a lack of consensus on the need for immobilization after traumatic anterior shoulder dislocation, and if needed, the optimal type, duration, and position of immobilization. A classic study by Henry and Genung of 121 first-time anterior shoulder dislocators found a 90% rate of recurrence in immobilized shoulders as compared to 85% in those without immobilization [31]. Additionally, evidence has not demonstrated a benefit to sling use longer than 1 week in duration [53].
Selected cadaveric and imaging studies have shown that immobilization of the arm in external rotation (ER) (Fig. 7) may oppose anterior–inferior labral tears to the glenoid rim better than a conventional position of internal rotation [54, 55]. A preliminary prospective clinical study by Itoi et al. showed a significantly reduced recurrence rate after initial anterior shoulder dislocation when treated with ER versus internal rotation sling immobilization [54]. However, the obvious benefit of labral reduction to allow healing must be weighed against the resource implications of bracing, possible discomfort to patients, the potential for a lack of labral reduction, likelihood for patient compliance, and the in vivo clinical results of ER bracing. A recent systematic review of the literature revealed that ER bracing reduced only 35% of Bankart lesions [56]. Furthermore, Paterson et al. conducted a systematic review and meta-analysis of the literature, indicating there is no benefit of conventional sling immobilization for longer than 1 week for the treatment of primary anterior shoulder dislocation in younger patients. Additionally, they found that there was not a significant difference in recurrence rates between ER bracing and traditional sling immobilization [53]. Most recently, Whelan et al. conducted a meta-analysis of six randomized controlled trials comparing internal rotation versus external rotation bracing and found no overall significant difference in rates of recurrence or in patients’ perceptions of their health-related quality of life [57]. Recently, a clinical study found a reduced recurrence rate with ER bracing in not only external rotation (10°) but also abduction (15°), utilizing a customized arm and thoracic shell [58]. Despite the multitude of current studies examining the position of the shoulder with regard to immobilization (Table 2), it remains an individualized decision by the physician and patient.
Fig. 7.

a, b Clinical photographs of a patient wearing an external rotation immobilizer
Table 2.
Studies evaluating outcomes of internal rotation versus external rotation bracing
| Study | Level of evidence | No. of patients | Mean age (years) | Type/duration immobilization | Recurrence rate | Length of follow-up (years) |
|---|---|---|---|---|---|---|
| Whelan et al. (2014) [59] | I | 52 (IR = 25, ER = 27) | 23 (14–35) | IR vs. ER/4 weeks | IR = 40%, ER = 37%; p = 0.41, no significant difference | 2.1 |
| Heidari et al. (2014) [58] | I | 102 (IR = 51, ER = 51) | 35.7 (15–55) | IR vs. 15° Abd 10° ER/3 weeks | IR = 33%, AbdER = 3.9%; p < 0.001, significantly lower recurrence rate in the AbdER group, but more noncooperative patients | 2 |
| Liavaag et al. (2011) [60] | I | 184 (IR = 93, ER = 91) | 26.8 (16–40) | IR vs. 15° ER/3 weeks | IR = 24.7%, ER = 30.8%; p = 0.36, no significant difference | 2 |
| Wang et al. (2011) [61] | II | 93 (IR = 46, ER = 47) | 26 (17–67) | IR vs. ER/3 weeks | IR = 35%, ER = 11%; p < 0.05, significantly lower recurrence rate in the ER group | 2.5 |
| Taskoparan et al. (2010) [62] | III | 33 (IR = 17, ER = 16) | IR = 29, ER = 35 (15–75) | IR vs. ER/3 weeks | IR = 29.4%, ER = 6.3%; significantly lower recurrence rate in the ER group | 1.7 |
| Finestone et al. (2009) [63] | II | 51 (IR = 24, ER = 27) | 20.3 (17–27) | IR vs. 15–20° ER/4 weeks | IR = 41.7%, ER = 37%; p = 0.74, no significant difference | 2.8 |
| Itoi et al. (2007) [64] | II | 159 (IR = 74, ER = 85) | 36 (12–90) | IR vs. 10° ER/3 weeks | IR = 42%, ER = 26%; p = 0.033, significantly lower recurrence rate the in the ER group | 2.1 |
| Itoi et al. (2003) [54] | II | 40 (IR = 20, ER = 20) | 39 (17–84) | IR vs. 10° ER/3 weeks | IR = 30%, ER = 0%; p = 0.08, significantly lower recurrence rate in the ER group | 1.3 |
Physical Therapy
Traditionally, nonoperative intervention with a period of immobilization and physical therapy has been the preferred treatment for patients with a first-time incident of anterior shoulder instability with recurrences rates reported as low as 25% in young active males [65]. While the indications for operative intervention in young, active, males with first-time dislocations are expanding and becoming more common [66, 67], there still remains a significant role for nonoperative treatment in older individuals, noncontact athletes, lower-demand populations, individuals who present with significant losses in range of motion, in-season athletes, patients with ligamentous laxity, and individuals who cannot tolerate general anesthesia.
Physical therapy is critical to shoulder stability through the recruitment and maintenance of dynamic stabilizers and scapulothoracic musculature—subscapularis, supraspinatus, infraspinatus, teres minor, teres major, biceps brachii, trapezius, and deltoid muscles. This is particularly important in patients with anterior shoulder instability who have compromised the integrity of the static stabilizers—glenoid labrum, capsule, anterior/posterior inferior glenohumeral ligaments, and possibly, humeral or glenoid bone stock. Due to this subsequent loss of static restraints, scapular stabilizers inherently adapt to diminish secondary instability. Rajaratnam et al. demonstrated this by using electromyography in 19 young, preoperative anterior instability patients with comparison to 25 age-matched asymptomatic control subjects [68]. They noted that patients with anterior shoulder instability inherently adopt neuromotor control strategies in elevation, both in the sagittal and coronal planes, much earlier than asymptomatic patients, suggesting that the preferential goal is for stability over mobility during shoulder musculature activation. Physical therapy facilitates the development of these dynamic stabilizers, while also maintaining mobilization through controlled exercises and muscle recruitment.
Contemporary data suggests a renewed role for nonoperative treatment with immobilization and subsequent physical therapy in select patient populations with anterior instability. Riccio et al. enrolled 32 patients with an average age of 28 years into a conservative treatment protocol for 3 months after primary anterior shoulder dislocation [69]. At 24 months post injury, 78% of patients had a good or excellent Rowe score for instability. Stratified results were more favorable in patients not involved in sporting activities or those who were not actively employed as overhead workers.
There is no consensus or specific recommendation on the return to play for an in-season athlete with anterior instability, although it is known that physical therapy can play a critical role for the patient desiring an early return to competition. While the emerging data has featured varying recommendations on the ideal treatment of the in-season athlete with anterior shoulder instability, there is generally agreement that certain criteria must be achieved before allowing a full return to sporting activity. At-risk athletes must be pain free and demonstrate symmetric shoulder strength within a functional range of motion that allows safe participation [70]. This typically entails a brief period of immobilization (3–10 days) followed by a progressive physical therapy protocol that focuses on cryotherapy, restoration of normal range of motion, rotator cuff and periscapular strengthening, stabilization drills, and finally, sport-specific drills over a 2–3-week period [71–73]. Dickens et al. demonstrated that a period of immobilization is not necessary, and an accelerated rehabilitation program can be beneficial in a percentage of intercollegiate athletes with in-season anterior shoulder instability [74]. With progressive physical therapy and occasional adjunctive use of shoulder stabilization bracing, the authors found that 33 of 45 (73%) patients were able to return to sport for either all or part of the season, with a median of only 5 days lost from competition. However, only 12 of 45 (27%) were able to complete the season without recurrence, while 11 sustained a recurrent dislocation event and 10 a subluxation event.
Repercussions of Nonoperative Management
It is important to note that while physical therapy is important in the early stages after an anterior shoulder instability event, there are circumstances where it is not recommended as a definitive treatment measure, even among in-season athletes. These circumstances include but are not limited to the following: patients with recurrent instability; inability to adequately and safely perform their job, duties, or sport; and significant humeral or glenoid bone loss where further instability is imminent and/or progressive loss is inevitable [71]. In reviewing the available treatment options, these risks and benefits must be emphasized as a part of shared decision making with the patient, his/her family, and athletic team staff.
While nonoperative management may be prudent for certain patients, the potential sequelae must be fully appreciated and openly discussed. Recurrent instability events may exacerbate the extent of osseous involvement, with repetitive instability displaying greater degrees of attritional glenoid loss alongside individuals involved with contact athletics [75]. Instability recurrence, greater cumulative instability burden, and increased duration of shoulder dislocation likely portend a heightened risk of requiring more advanced surgical intervention at the time of surgery, including remplissage for engaging Hill–Sachs lesions and/or Latarjet for combined attritional glenoid bone loss [76]. Repetitive anterior instability events may also impart detrimental shear stress on the articular chondral surfaces, contributing to worse patient-reported outcome measures and increased risk of developing instability arthropathy [77]. Krych et al. studied the effect of recurrent anterior instability on cartilage injury at the time of arthroscopic repair. Previously documented shoulder dislocation requiring closed reduction and the number of discrete dislocations were both significant for glenoid injury. Also, a greater number of dislocations were associated with higher-grade lesions of the glenohumeral joint (p < 0.001) [78]. Among individuals with over 25-year follow-up after nonoperative treatment of first-time shoulder dislocations, Hovelius and Saeboe indicated that only 44% demonstrated normal radiographic findings and two out of three patients under 25 years old exhibited evidence of arthropathy at long-term assessment [79].
Special Scenarios
Young Patients
With an increase in youth sports participation and a trend toward single sport focus, there has been an increase in youth sport injuries [80]. The incidence of anterior shoulder instability in patients 10 to 16 years old is 164.4 per 100,000 person-years [81], which approaches the high incidence in military personnel. A recent study examined the natural history of nonoperatively treated anterior shoulder dislocations in adolescent patients, mean age 16.3 years (range 13–18 years old). The authors prospectively enrolled 122 adolescent patients after a first-time anterior glenohumeral dislocation. One hundred two patients (76.7%) had a recurrent dislocation. The incidence of recurrent shoulder instability was 59, 38, 21, and 7% at 1-, 2-, 5-, and 10-year follow-up, respectively [82]. The authors advocate for early operative intervention in adolescents due to the high recurrence rates with nonoperative treatment. However, the younger skeletally immature patient, aged 10–13 years old, with open physes is an entirely different instability patient population. Several studies have demonstrated a relatively low rate of recurrent instability in patients 10 to 13 years old after primary dislocation, with one study reporting a 21.4% recurrence rate [83]. Initial management should be conservative, and surgical intervention only considered for skeletally immature patients with recurrent instability [84].
In-season Athletes
There is no consensus regarding return to play for in-season athletes following an anterior shoulder instability event. Recently, several studies have provided good data to guide orthopedic surgeons and team physicians. Dickens et al. prospectively enrolled 45 contact intercollegiate athletes in a multicenter observational study to assess return to play after in-season anterior glenohumeral instability. Thirty-three of 45 (73%) athletes returned to sport for either all or part of the season. Only 12 athletes (27%) completed the season without recurrence. Athletes with a subluxation were 5.3 times more likely to return to sport during the season than those with a dislocation [74]. They found the majority of athletes returned to sport in 10 days. Another review acknowledged that athletes can return to sport within 3 weeks following an initial instability event and felt that motion-restricting bracing may be helpful to prevent recurrence [73].
Bracing of Athletes
The successfulness of bracing to prevent recurrent instability is not well established in the literature. There is a multitude of commercially available braces designed specifically to restrict glenohumeral motion. The ability of an athlete to tolerate this brace is sport- and position-specific. Throwing athletes, overhead athletes, and skill position players in sports such as American football are usually not able to tolerate this type of brace [71, 73]. There are braces that are neoprene sleeves (Fig. 8) that can be utilized which are not specifically motion-limiting which have been found to increase proprioception in subjects with stable and unstable shoulders [85]. There are no studies, however, that show that their use is associated with decreased episodes of instability. Their use can be discussed with patients as a potential method to augment nonoperative care to facilitate return to sports in season after an episode of instability but should not be looked upon as the sole treatment for anterior instability.
Fig. 8.

Clinical photograph of a patient wearing a neoprene shoulder brace designed to decrease subsequent anterior glenohumeral instability events after returning to sport (Courtesy of Brett D. Owens, MD)
Ideal Patients for Nonoperative Management
There are certain patient factors that can lead to an ideal situation for successful nonoperative management of anterior shoulder instability (Fig. 9). As mentioned previously, the biggest indicator for a likely recurrent instability event following an anterior glenohumeral dislocation is age. Competitive or contact sport athletics is another patient factor that carries a high risk of recurrent instability. Therefore, older [28], nonathletic [29, 30] patients are identified as someone who has a successful chance of nonoperative treatment. Increasing age as a positive prognostic factor is not indefinite, as older patients have a higher risk of having a concomitant glenoid rim fracture (bony Bankart) or a rotator cuff tear, which may invalidate a nonoperative plan. Although the high end of the age group that may fare well without surgery is difficult to define, age greater than 25–35 appears to be the low end of this range [27, 28, 86].
Fig. 9.
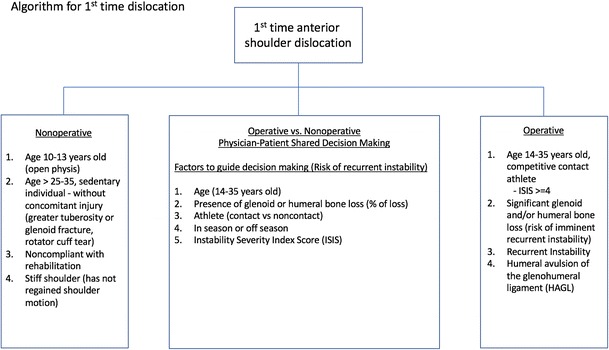
An algorithm to guide the management of first-time dislocators
Patients Who Will Not Likely Be Successful with Nonoperative Management
There is considerable debate in the literature on operative management of certain types of patients who have anterior instability. Although this debate does not always compare the various methods of operative fixation with nonoperative management of anterior instability, it elucidates patient-specific factors that lead to a high rate of recurrent instability even following surgery. It stands to reason that if these factors are present, this would lead to a poor chance at success with nonoperative management. These factors were originally described by Balg and Boileau and consist of age < 20 years, presence of glenoid bone loss, humeral bone loss, degree of sports participation, type of sport, and whether or not shoulder hyperlaxity is present [87]. The Instability Severity Index Score (ISIS) was developed with each of these factors worth 2 points if present with the exception of type of sport and presence of shoulder hyperlaxity which are each worth 1 for a total of 10 points. The authors found that if a patient had a score > 6, they had a 70% chance of recurrent dislocation after a soft tissue repair and advocated a bony stability surgery. This was later studied by Phadnis et al. who found in their series that a score of ≥ 4 was associated with a 70% risk of failure [88]. These studies demonstrate the high rate of recurrent instability even following surgery in young, competitive athletes who have glenoid or humeral bone loss, and thus, these patients should not be routinely treated with nonoperative management.
Conclusion
Despite the continual refinement of surgical techniques for anterior glenohumeral instability, there remains a significant role for nonoperative treatment. History of the patient and information on the type of sport played (contact vs. noncontact) as well as physical examination and imaging are important as they assist the surgeon in determining who will and who will not be a good candidate for nonoperative treatment. There is not sufficient evidence at this time to argue for either immobilization in conventional internal rotation or immobilization with the shoulder in external rotation with ultimately decreased recurrence risk. Risks and benefits must continue to be emphasized as a part of shared decision making with the patient, his/her family, and the athletic team staff, if the patient is an athlete.
Compliance with Ethical Standards
Conflict of Interest
All authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Management of Anterior Shoulder Instability
References
- 1.Owens BD, Dawson L, Burks R, Cameron KL. Incidence of shoulder dislocation in the United States military: demographic considerations from a high-risk population. J Bone Joint Surg Am. 2009;91(4):791–796. doi: 10.2106/JBJS.H.00514. [DOI] [PubMed] [Google Scholar]
- 2.Waterman B, Owens BD, Tokish JM. Anterior shoulder instability in the military athlete. Sports Health. 2016;8(6):514–519. doi: 10.1177/1941738116672161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Owens BD, Duffey ML, Nelson BJ, DeBerardino TM, Taylor DC, Mountcastle SB. The incidence and characteristics of shoulder instability at the United States Military Academy. Am J Sports Med. 2007;35(7):1168–1173. doi: 10.1177/0363546506295179. [DOI] [PubMed] [Google Scholar]
- 4.Gibbs DB, Lynch TS, Nuber ED, Nuber GW. Common shoulder injuries in American football athletes. Curr Sports Med Rep. 2015;14(5):413–419. doi: 10.1249/JSR.0000000000000190. [DOI] [PubMed] [Google Scholar]
- 5.Kawasaki T, Ota C, Urayama S, Maki N, Nagayama M, Kaketa T, et al. Incidence of and risk factors for traumatic anterior shoulder dislocation: an epidemiologic study in high-school rugby players. J Shoulder Elb Surg. 2014;23(11):1624–1630. doi: 10.1016/j.jse.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 6.Itoigawa Y, Itoi E. Anatomy of the capsulolabral complex and rotator interval related to glenohumeral instability. Knee Surg Sports Traumatol Arthrosc. 2016;24(2):343–349. doi: 10.1007/s00167-015-3892-1. [DOI] [PubMed] [Google Scholar]
- 7.Di Giacomo G, de Gasperis N, Scarso P. Bipolar bone defect in the shoulder anterior dislocation. Knee Surg Sports Traumatol Arthrosc. 2016;24(2):479–488. doi: 10.1007/s00167-015-3927-7. [DOI] [PubMed] [Google Scholar]
- 8.Aygun U, Calik Y, Isik C, Sahin H, Sahin R, Aygun DO. The importance of glenoid version in patients with anterior dislocation of the shoulder. J Shoulder Elb Surg. 2016;25(12):1930–1936. doi: 10.1016/j.jse.2016.09.018. [DOI] [PubMed] [Google Scholar]
- 9.Eichinger JK, Massimini DF, Kim J, Higgins LD. Biomechanical evaluation of glenoid version and dislocation direction on the influence of anterior shoulder instability and development of Hill-Sachs lesions. Am J Sports Med. 2016;44(11):2792–2799. doi: 10.1177/0363546516659281. [DOI] [PubMed] [Google Scholar]
- 10.Hohmann E, Tetsworth K. Glenoid version and inclination are risk factors for anterior shoulder dislocation. J Shoulder Elb Surg. 2015;24(8):1268–1273. doi: 10.1016/j.jse.2015.03.032. [DOI] [PubMed] [Google Scholar]
- 11.Owens BD, Cameron KL, Clifton KB, Svoboda SJ, Wolf JM. Association between serum relaxin and subsequent shoulder instability. Orthopedics. 2016;39(4):e724–e728. doi: 10.3928/01477447-20160421-01. [DOI] [PubMed] [Google Scholar]
- 12.Belangero PS, Leal MF, de Castro Pochini A, Andreoli CV, Ejnisman B, Cohen M. Profile of collagen gene expression in the glenohumeral capsule of patients with traumatic anterior instability of the shoulder. Rev Bras Ortop. 2014;49(6):642–646. doi: 10.1016/j.rboe.2014.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Belangero PS, Leal MF, Figueiredo EA, Cohen C, Andreoli CV, Smith MC, et al. Differential expression of extracellular matrix genes in glenohumeral capsule of shoulder instability patients. Connect Tissue Res. 2016;57(4):290–298. doi: 10.3109/03008207.2016.1173034. [DOI] [PubMed] [Google Scholar]
- 14.Belangero PS, Leal MF, Figueiredo EA, Cohen C, Pochini Ade C, Smith MC, et al. Gene expression analysis in patients with traumatic anterior shoulder instability suggests deregulation of collagen genes. J Orthop Res. 2014;32(10):1311–1316. doi: 10.1002/jor.22680. [DOI] [PubMed] [Google Scholar]
- 15.Bankart ASB. The pathology and treatment of recurrent dislocation of the shoulder-joint. Br J Surg. 1938;26:23–29. [Google Scholar]
- 16.Bigliani LU, Pollock RG, Soslowsky LJ, Flatow EL, Pawluk RJ, Mow VC. Tensile properties of the inferior glenohumeral ligament. J Orthop Res. 1992;10(2):187–197. doi: 10.1002/jor.1100100205. [DOI] [PubMed] [Google Scholar]
- 17.Neviaser TJ. The anterior labroligamentous periosteal sleeve avulsion lesion: a cause of anterior instability of the shoulder. Arthroscopy. 1993;9(1):17–21. doi: 10.1016/s0749-8063(05)80338-x. [DOI] [PubMed] [Google Scholar]
- 18.Khiami F, Gerometta A, Loriaut P. Management of recent first-time anterior shoulder dislocations. Orthop Traumatol Surg Res. 2015;101(1 Suppl):S51–S57. doi: 10.1016/j.otsr.2014.06.027. [DOI] [PubMed] [Google Scholar]
- 19.Loh B, Lim JB, Tan AH. Is clinical evaluation alone sufficient for the diagnosis of a Bankart lesion without the use of magnetic resonance imaging? Ann Transl Med. 2016;4(21):419. doi: 10.21037/atm.2016.11.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kumar K, Makandura M, Leong NJ, Gartner L, Lee CH, Ng DZ, et al. Is the apprehension test sufficient for the diagnosis of anterior shoulder instability in young patients without magnetic resonance imaging (MRI)? Ann Acad Med Singap. 2015;44(5):178–184. [PubMed] [Google Scholar]
- 21.Pansard E, Klouche S, Billot N, Rousselin B, Kraus TM, Bauer T, et al. Reliability and validity assessment of a glenoid bone loss measurement using the Bernageau profile view in chronic anterior shoulder instability. J Shoulder Elb Surg. 2013;22(9):1193–1198. doi: 10.1016/j.jse.2012.12.032. [DOI] [PubMed] [Google Scholar]
- 22.Markenstein JE, Jaspars KC, van der Hulst VP, Willems WJ. The quantification of glenoid bone loss in anterior shoulder instability; MR-arthro compared to 3D-CT. Skelet Radiol. 2014;43(4):475–483. doi: 10.1007/s00256-013-1780-7. [DOI] [PubMed] [Google Scholar]
- 23.Ozaki R, Nakagawa S, Mizuno N, Mae T, Yoneda M. Hill-sachs lesions in shoulders with traumatic anterior instability: evaluation using computed tomography with 3-dimensional reconstruction. Am J Sports Med. 2014;42(11):2597–2605. doi: 10.1177/0363546514549543. [DOI] [PubMed] [Google Scholar]
- 24.Saba L, De Filippo M. MR arthrography evaluation in patients with traumatic anterior shoulder instability. J Orthop. 2017;14(1):73–76. doi: 10.1016/j.jor.2016.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van Grinsven S, Nijenhuis TA, Konings PC, van Kampen A, van Loon CJ. Are radiologists superior to orthopaedic surgeons in diagnosing instability-related shoulder lesions on magnetic resonance arthrography? A multicenter reproducibility and accuracy study. J Shoulder Elb Surg. 2015;24(9):1405–1412. doi: 10.1016/j.jse.2015.05.050. [DOI] [PubMed] [Google Scholar]
- 26.Hamamoto JT, Leroux T, Chahla J, Bhatia S, Higgins JD, Romeo AA, et al. Assessment and evaluation of glenoid bone loss. Arthrosc Tech. 2016;5(4):e947–ee51. doi: 10.1016/j.eats.2016.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hovelius L, Rahme H. Primary anterior dislocation of the shoulder: long-term prognosis at the age of 40 years or younger. Knee Surg Sports Traumatol Arthrosc. 2016;24(2):330–342. doi: 10.1007/s00167-015-3980-2. [DOI] [PubMed] [Google Scholar]
- 28.Robinson CM, Howes J, Murdoch H, Will E, Graham C. Functional outcome and risk of recurrent instability after primary traumatic anterior shoulder dislocation in young patients. J Bone Joint Surg Am. 2006;88(11):2326–2336. doi: 10.2106/JBJS.E.01327. [DOI] [PubMed] [Google Scholar]
- 29.Simonet WT, Cofield RH. Prognosis in anterior shoulder dislocation. Am J Sports Med. 1984;12(1):19–24. doi: 10.1177/036354658401200103. [DOI] [PubMed] [Google Scholar]
- 30.Simonet WT, Melton LJ, 3rd, Cofield RH, Ilstrup DM. Incidence of anterior shoulder dislocation in Olmsted County, Minnesota. Clin Orthop Relat Res. 1984;186:186–191. [PubMed] [Google Scholar]
- 31.Henry JH, Genung JA. Natural history of glenohumeral dislocation—revisited. Am J Sports Med. 1982;10(3):135–137. doi: 10.1177/036354658201000301. [DOI] [PubMed] [Google Scholar]
- 32.Wasserstein DN, Sheth U, Colbenson K, Henry PD, Chahal J, Dwyer T, et al. The true recurrence rate and factors predicting recurrent instability after nonsurgical management of traumatic primary anterior shoulder dislocation: a systematic review. Arthroscopy. 2016;32(12):2616–2625. doi: 10.1016/j.arthro.2016.05.039. [DOI] [PubMed] [Google Scholar]
- 33.Kirkley A, Werstine R, Ratjek A, Griffin S. Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder: long-term evaluation. Arthroscopy. 2005;21(1):55–63. doi: 10.1016/j.arthro.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 34.Spiegl UJ, Ryf C, Hepp P, Rillmann P. Evaluation of a treatment algorithm for acute traumatic osseous Bankart lesions resulting from first time dislocation of the shoulder with a two year follow-up. BMC Musculoskelet Disord. 2013;14:305. doi: 10.1186/1471-2474-14-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gigis I, Heikenfeld R, Kapinas A, Listringhaus R, Godolias G. Arthroscopic versus conservative treatment of first anterior dislocation of the shoulder in adolescents. J Pediatr Orthop. 2014;34(4):421–425. doi: 10.1097/BPO.0000000000000108. [DOI] [PubMed] [Google Scholar]
- 36.Khan A, Samba A, Pereira B, Canavese F. Anterior dislocation of the shoulder in skeletally immature patients: comparison between non-operative treatment versus open Latarjet's procedure. Bone Joint J. 2014;96-B(3):354–359. doi: 10.1302/0301-620X.96B3.32167. [DOI] [PubMed] [Google Scholar]
- 37.Konigshausen M, Schliemann B, Schildhauer TA, Seybold D. Evaluation of immobilization in external rotation after primary traumatic anterior shoulder dislocation: 5-year results. Musculoskelet Surg. 2014;98(2):143–151. doi: 10.1007/s12306-013-0276-x. [DOI] [PubMed] [Google Scholar]
- 38.Leroux T, Wasserstein D, Veillette C, Khoshbin A, Henry P, Chahal J, et al. Epidemiology of primary anterior shoulder dislocation requiring closed reduction in Ontario. Canada. Am J Sports Med. 2014;42(2):442–450. doi: 10.1177/0363546513510391. [DOI] [PubMed] [Google Scholar]
- 39.Liu A, Xue X, Chen Y, Bi F, Yan S. The external rotation immobilisation does not reduce recurrence rates or improve quality of life after primary anterior shoulder dislocation: a systematic review and meta-analysis. Injury. 2014;45(12):1842–1847. doi: 10.1016/j.injury.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 40.Longo UG, Loppini M, Rizzello G, Ciuffreda M, Maffulli N, Denaro V. Management of primary acute anterior shoulder dislocation: systematic review and quantitative synthesis of the literature. Arthroscopy. 2014;30(4):506–522. doi: 10.1016/j.arthro.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 41.Olds M, Donaldson K, Ellis R, Kersten P. In children 18 years and under, what promotes recurrent shoulder instability after traumatic anterior shoulder dislocation? A systematic review and meta-analysis of risk factors. Br J Sports Med. 2016;50(18):1135–1141. doi: 10.1136/bjsports-2015-095149. [DOI] [PubMed] [Google Scholar]
- 42.Hovelius L, Rahme H. Primary anterior dislocation of the shoulder: long-term prognosis at the age of 40 years or younger. Knee Surg Sports Traumatol Arthrosc. 2016;24(2):330–342. doi: 10.1007/s00167-015-3980-2. [DOI] [PubMed] [Google Scholar]
- 43.Wheeler JH, Ryan JB, Arciero RA, Molinari RN. Arthroscopic versus nonoperative treatment of acute shoulder dislocations in young athletes. Arthroscopy. 1989;5(3):213–217. doi: 10.1016/0749-8063(89)90174-6. [DOI] [PubMed] [Google Scholar]
- 44.Arciero RA, Wheeler JH, Ryan JB, McBride JT. Arthroscopic Bankart repair versus nonoperative treatment for acute, initial anterior shoulder dislocations. Am J Sports Med. 1994;22(5):589–594. doi: 10.1177/036354659402200504. [DOI] [PubMed] [Google Scholar]
- 45.DeBerardino TM, Arciero RA, Taylor DC, Uhorchak JM. Prospective evaluation of arthroscopic stabilization of acute, initial anterior shoulder dislocations in young athletes. Two- to five-year follow-up. Am J Sports Med. 2001;29(5):586–592. doi: 10.1177/03635465010290051101. [DOI] [PubMed] [Google Scholar]
- 46.Bottoni CR, Wilckens JH, DeBerardino TM, D'Alleyrand JC, Rooney RC, Harpstrite JK, et al. A prospective, randomized evaluation of arthroscopic stabilization versus nonoperative treatment in patients with acute, traumatic, first-time shoulder dislocations. Am J Sports Med. 2002;30(4):576–580. doi: 10.1177/03635465020300041801. [DOI] [PubMed] [Google Scholar]
- 47.Brophy RH, Marx RG. The treatment of traumatic anterior instability of the shoulder: nonoperative and surgical treatment. Arthroscopy. 2009;25(3):298–304. doi: 10.1016/j.arthro.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 48.Chahal J, Marks PH, Macdonald PB, Shah PS, Theodoropoulos J, Ravi B, et al. Anatomic Bankart repair compared with nonoperative treatment and/or arthroscopic lavage for first-time traumatic shoulder dislocation. Arthroscopy. 2012;28(4):565–575. doi: 10.1016/j.arthro.2011.11.012. [DOI] [PubMed] [Google Scholar]
- 49.Godin J, Sekiya JK. Systematic review of rehabilitation versus operative stabilization for the treatment of first-time anterior shoulder dislocations. Sports Health. 2010;2(2):156–165. doi: 10.1177/1941738109359507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jakobsen BW, Johannsen HV, Suder P, Sojbjerg JO. Primary repair versus conservative treatment of first-time traumatic anterior dislocation of the shoulder: a randomized study with 10-year follow-up. Arthroscopy. 2007;23(2):118–123. doi: 10.1016/j.arthro.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 51.An VV, Sivakumar BS, Phan K, Trantalis J. A systematic review and meta-analysis of clinical and patient-reported outcomes following two procedures for recurrent traumatic anterior instability of the shoulder: Latarjet procedure vs. Bankart repair. J Shoulder Elb Surg. 2016;25(5):853–863. doi: 10.1016/j.jse.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 52.Zimmermann SM, Scheyerer MJ, Farshad M, Catanzaro S, Rahm S, Gerber C. Long-term restoration of anterior shoulder stability: a retrospective analysis of arthroscopic Bankart repair versus open Latarjet procedure. J Bone Joint Surg Am. 2016;98(23):1954–1961. doi: 10.2106/JBJS.15.01398. [DOI] [PubMed] [Google Scholar]
- 53.Paterson WH, Throckmorton TW, Koester M, Azar FM, Kuhn JE. Position and duration of immobilization after primary anterior shoulder dislocation: a systematic review and meta-analysis of the literature. J Bone Joint Surg Am. 2010;92(18):2924–2933. doi: 10.2106/JBJS.J.00631. [DOI] [PubMed] [Google Scholar]
- 54.Itoi E, Hatakeyama Y, Kido T, Sato T, Minagawa H, Wakabayashi I, et al. A new method of immobilization after traumatic anterior dislocation of the shoulder: a preliminary study. J Shoulder Elb Surg. 2003;12(5):413–415. doi: 10.1016/s1058-2746(03)00171-x. [DOI] [PubMed] [Google Scholar]
- 55.Itoi E, Sashi R, Minagawa H, Shimizu T, Wakabayashi I, Sato K. Position of immobilization after dislocation of the glenohumeral joint. A study with use of magnetic resonance imaging. J Bone Joint Surg Am. 2001;83-A(5):661–667. doi: 10.2106/00004623-200105000-00003. [DOI] [PubMed] [Google Scholar]
- 56.Jordan RW, Saithna A, Old J, MacDonald P. Does external rotation bracing for anterior shoulder dislocation actually result in reduction of the labrum? A systematic review. Am J Sports Med. 2015;43(9):2328–2333. doi: 10.1177/0363546514555661. [DOI] [PubMed] [Google Scholar]
- 57.Whelan DB, Kletke SN, Schemitsch G, Chahal J. Immobilization in external rotation versus internal rotation after primary anterior shoulder dislocation: a meta-analysis of randomized controlled trials. Am J Sports Med. 2016;44(2):521–532. doi: 10.1177/0363546515585119. [DOI] [PubMed] [Google Scholar]
- 58.Heidari K, Asadollahi S, Vafaee R, Barfehei A, Kamalifar H, Chaboksavar ZA, et al. Immobilization in external rotation combined with abduction reduces the risk of recurrence after primary anterior shoulder dislocation. J Shoulder Elb Surg. 2014;23(6):759–766. doi: 10.1016/j.jse.2014.01.018. [DOI] [PubMed] [Google Scholar]
- 59.Whelan DB, Litchfield R, Wambolt E, Dainty K. External rotation immobilization for primary shoulder dislocation: a randomized controlled trial. Clin Orthop Relat Res. 2014;472(8):2380–2386. doi: 10.1007/s11999-013-3432-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Liavaag S, Brox JI, Pripp AH, Enger M, Soldal LA, Svenningsen S. Immobilization in external rotation after primary shoulder dislocation did not reduce the risk of recurrence: a randomized controlled trial. J Bone Joint Surg Am. 2011;93(10):897–904. doi: 10.2106/JBJS.J.00416. [DOI] [PubMed] [Google Scholar]
- 61.Wang DY, Zhang ZL, Zheng YZ, Rui G. Analysis on the rotation angle and the effect of two immobilization methods after reduction of shoulder dislocation in emergency treatment. New Med. 2011;42:221–224. [Google Scholar]
- 62.Taskoparan H, Kilincoglu V, Tunay S, Bilgic S, Yurttas Y, Komurcu M. Immobilization of the shoulder in external rotation for prevention of recurrence in acute anterior dislocation. Acta Orthop Traumatol Turc. 2010;44(4):278–284. doi: 10.3944/AOTT.2010.2274. [DOI] [PubMed] [Google Scholar]
- 63.Finestone A, Milgrom C, Radeva-Petrova DR. Bracing in external rotation for traumatic anterior dislocation of the shoulder. J Bone Joint Surg Br. 2009;91(7):918–921. doi: 10.1302/0301-620X.91B7.22263. [DOI] [PubMed] [Google Scholar]
- 64.Itoi E, Hatakeyama Y, Sato T. Immobilization in external rotation after shoulder dislocation reduces the risk of recurrence. a randomized controlled trial. J Bone Joint Surg Am. 2007;89(10):2124–2131. doi: 10.2106/JBJS.F.00654. [DOI] [PubMed] [Google Scholar]
- 65.Aronen JG, Regan K. Decreasing the incidence of recurrence of first time anterior shoulder dislocations with rehabilitation. Am J Sports Med. 1984;12(4):283–291. doi: 10.1177/036354658401200408. [DOI] [PubMed] [Google Scholar]
- 66.Balke M, Shafizadeh S, Bouillon B, Banerjee M. Management of shoulder instability: the current state of treatment among German orthopaedic surgeons. Arch Orthop Trauma Surg. 2016;136(12):1717–1721. doi: 10.1007/s00402-016-2553-2. [DOI] [PubMed] [Google Scholar]
- 67.Berendes TD, Pilot P, Nagels J, Vochteloo AJ, Nelissen RG. Survey on the management of acute first-time anterior shoulder dislocation amongst Dutch public hospitals. Arch Orthop Trauma Surg. 2015;135(4):447–454. doi: 10.1007/s00402-015-2156-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rajaratnam BS, Goh J, Kumar PV. Control strategies to re-establish glenohumeral stability after shoulder injury. BMC Sports Sci Med Rehabil. 2013;5(1):26. doi: 10.1186/2052-1847-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Riccio I, de Sire A, Latte C, Pascarella F, Gimigliano F. Conservative treatment of traumatic shoulder instability: a case series study. Musculoskelet Surg. 2015;99(2):133–137. doi: 10.1007/s12306-015-0373-0. [DOI] [PubMed] [Google Scholar]
- 70.Watson S, Allen B, Grant JA. A clinical review of return-to-play considerations after anterior shoulder dislocation. Sports Health. 2016;8(4):336–341. doi: 10.1177/1941738116651956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Burns TC, Owens BD. Management of shoulder instability in in-season athletes. Phys Sportsmed. 2010;38(3):55–60. doi: 10.3810/psm.2010.10.1808. [DOI] [PubMed] [Google Scholar]
- 72.Buss DD, Lynch GP, Meyer CP, Huber SM, Freehill MQ. Nonoperative management for in-season athletes with anterior shoulder instability. Am J Sports Med. 2004;32(6):1430–1433. doi: 10.1177/0363546503262069. [DOI] [PubMed] [Google Scholar]
- 73.Owens BD, Dickens JF, Kilcoyne KG, Rue JP. Management of mid-season traumatic anterior shoulder instability in athletes. J Am Acad Orthop Surg. 2012;20(8):518–526. doi: 10.5435/JAAOS-20-08-518. [DOI] [PubMed] [Google Scholar]
- 74.Dickens JF, Owens BD, Cameron KL, Kilcoyne K, Allred CD, Svoboda SJ, et al. Return to play and recurrent instability after in-season anterior shoulder instability: a prospective multicenter study. Am J Sports Med. 2014;42(12):2842–2850. doi: 10.1177/0363546514553181. [DOI] [PubMed] [Google Scholar]
- 75.Nakagawa S, Ozaki R, Take Y, Mizuno N, Mae T. Enlargement of glenoid defects in traumatic anterior shoulder instability: influence of the number of recurrences and type of sport. Orthop J Sports Med. 2014;2(4):2325967114529920. doi: 10.1177/2325967114529920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Denard PJ, Dai X, Burkhart SS. Increasing preoperative dislocations and total time of dislocation affect surgical management of anterior shoulder instability. Int J Shoulder Surg. 2015;9(1):1–5. doi: 10.4103/0973-6042.150215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Waterman BR, Kilcoyne KG, Parada SA, Eichinger JK. Prevention and management of post-instability glenohumeral arthropathy. World J Orthop. 2017;8(3):229–241. doi: 10.5312/wjo.v8.i3.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Krych AJ, Sousa PL, King AH, Morgan JA, May JH, Dahm DL. The effect of cartilage injury after arthroscopic stabilization for shoulder instability. Orthopedics. 2015;38(11):e965–e969. doi: 10.3928/01477447-20151020-03. [DOI] [PubMed] [Google Scholar]
- 79.Hovelius L, Saeboe M. Neer Award 2008: arthropathy after primary anterior shoulder dislocation—223 shoulders prospectively followed up for twenty-five years. J Shoulder Elb Surg. 2009;18(3):339–347. doi: 10.1016/j.jse.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 80.Smucny M, Kolmodin J, Saluan P. Shoulder and elbow injuries in the adolescent athlete. Sports Med Arthrosc. 2016;24(4):188–194. doi: 10.1097/JSA.0000000000000131. [DOI] [PubMed] [Google Scholar]
- 81.Leroux T, Ogilvie-Harris D, Veillette C, Chahal J, Dwyer T, Khoshbin A, et al. The epidemiology of primary anterior shoulder dislocations in patients aged 10 to 16 years. Am J Sports Med. 2015;43(9):2111–2117. doi: 10.1177/0363546515591996. [DOI] [PubMed] [Google Scholar]
- 82.Roberts SB, Beattie N, McNiven ND, Robinson CM. The natural history of primary anterior dislocation of the glenohumeral joint in adolescence. Bone Joint J. 2015;97-B(4):520–526. doi: 10.1302/0301-620X.97B4.34989. [DOI] [PubMed] [Google Scholar]
- 83.Cordischi K, Li X, Busconi B. Intermediate outcomes after primary traumatic anterior shoulder dislocation in skeletally immature patients aged 10 to 13 years. Orthopedics. 2009;32(9) 10.3928/01477447-20090728-34. [DOI] [PubMed]
- 84.Li X, Ma R, Nielsen NM, Gulotta LV, Dines JS, Owens BD. Management of shoulder instability in the skeletally immature patient. J Am Acad Orthop Surg. 2013;21(9):529–537. doi: 10.5435/JAAOS-21-09-529. [DOI] [PubMed] [Google Scholar]
- 85.Chu JC, Kane EJ, Arnold BL, Gansneder BM. The effect of a neoprene shoulder stabilizer on active joint-reposition sense in subjects with stable and unstable shoulders. J Athl Train. 2002;37(2):141–145. [PMC free article] [PubMed] [Google Scholar]
- 86.Hovelius L, Augustini BG, Fredin H, Johansson O, Norlin R, Thorling J. Primary anterior dislocation of the shoulder in young patients. A ten-year prospective study. J Bone Joint Surg Am. 1996;78(11):1677–1684. doi: 10.2106/00004623-199611000-00006. [DOI] [PubMed] [Google Scholar]
- 87.Balg F, Boileau P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br. 2007;89(11):1470–1477. doi: 10.1302/0301-620X.89B11.18962. [DOI] [PubMed] [Google Scholar]
- 88.Phadnis J, Arnold C, Elmorsy A, Flannery M. Utility of the Instability Severity Index Score in predicting failure after arthroscopic anterior stabilization of the shoulder. Am J Sports Med. 2015;43(8):1983–1988. doi: 10.1177/0363546515587083. [DOI] [PubMed] [Google Scholar]


