Abstract
Purpose of Review
Arthroscopic Bankart repair is commonly utilized for shoulder stabilization in patients with anterior shoulder instability with minimum glenoid bone loss. The purpose of this review is to provide the indications, surgical technique, complications, and recent outcomes in arthroscopic Bankart repair for shoulder instability.
Recent Findings
Improvements in arthroscopic techniques have led to better patient outcomes, as well as an improved understanding of the pathoanatomy of instability. More recent studies have shown that one of the potential failures of primary arthroscopic repair may be due to unaddressed bone loss. This underscores the importance of evaluating glenoid bone loss and proper patient selection for this procedure to ensure successful outcome.
Summary
When indicated, arthroscopic stabilization is the treatment of choice for many surgeons due to its lower morbidity and low overall complication rate. Future work must focus on longer-term outcomes in patients undergoing arthroscopic Bankart repair, as well as the clinical outcomes of new fixation techniques, augmentation techniques, and the effect of glenoid bone loss in outcome.
Keywords: Shoulder instability, Arthroscopy, Bankart, Hill-Sachs, Bone loss, Outcomes
Introduction
Arthroscopic Bankart repair is currently the most utilized technique in the surgical management of symptomatic shoulder instability. Arthroscopic Bankart repair was first described in 1993, with its popularity rapidly increasing over the past several decades as arthroscopic instrumentation and techniques have improved [1]. An investigation of the American Board of Orthopaedic Surgery (ABOS) for surgical trends in Bankart repair revealed a stark increase in the percentage of the Bankart repairs done arthroscopically compared to open [2]. From 2003 to 2005, 71.2% of repairs were performed arthroscopically, compared with 87.7% from 2006 to 2008 [2]. With an increase in literature revealing similar clinical outcomes between patients undergoing open versus arthroscopic repair [3–10], there has been a recent shift towards arthroscopic stabilization as the first-line in surgical management of shoulder instability.
Indications/Contraindications
Arthroscopic Bankart repair is most appropriate in the setting of a “simple” Bankart lesion without significant glenoid bone loss (GBL). Balg and Boileau proposed the Instability Severity Index Score (ISIS) as a pre-operative means of assessing a patient’s likelihood of recurrent instability following arthroscopic repair (Table 1) [11]. They reported that patients who score 7 or higher on this index have a 70% recurrence risk, while those who score 6 or less have only a 10% recurrence risk [11]. While overly simplified, the ISIS represents a quick way to further risk-stratify patients and aids in the selection of the appropriate treatment course. The authors also recommend considering open stabilization or Latarjet procedure in individuals with exceptionally high ISIS scores [11]. Phadnis et al. reported on the utility of the ISIS in predicting failure of arthroscopic Bankart repair. Out of 141 patients, 19 (13.5%) experienced recurrence, with their mean ISI score being significantly higher than those who did not recur (5.1 versus 1.7) [12]. GBL carried the highest risk of failure (70%). Also, patients with an ISIS ≥ 4 had a 70% change of failures as opposed to a 4% risk of recurrence with a score < 4 [12]. Rouleau et al. assessed the multicenter reliability of the ISS and found that it was very reliable, with an interclass coefficient of 0.933. Despite this, it is important to note that it did not correlate with quality of life questionnaires in patients [12].
Table 1.
Instability Severity Index Score (adapted from [11])
| Criteria | # points |
|---|---|
| 20 years old or younger | 2 |
| Participation in competitive sports | 2 |
| Hill-Sachs lesion in external rotation on AP radiograph | 2 |
| Loss of glenoid contour on AP radiograph | 2 |
| Participation in contact sport or overhead sport | 1 |
| Shoulder hyperlaxity anteriorly or inferiorly | 1 |
While non-surgical management with physical therapy can be a viable treatment strategy in low-demand patients following first-time instability events, younger, more active patients have a high rate of recurrent instability [13, 14]. Re-dislocation rates in this high-risk patient population have been reported as high as 90% after non-operative treatment [3]. Robinson et al. reported that out of 252 patients aged 15–35 years old, 53.2% experienced a repeat dislocation (134 patients), or recurrent subluxation (16 (6.5%) patients), after a mean of 13.3 months [15]. Some studies have reported even lower rates of recurrence in young populations. One review article reported that recurrence rates can range anywhere from 0 to 100% in skeletally immature patients [3]. Cordishi et al. also reported on recurrence rates following traumatic dislocation in 14 patients who were skeletally immature. They found that 21.4% of patients experienced recurrent dislocation and required surgery [3].
In patients with a high risk of recurrent instability or who have failed non-operative management, arthroscopic Bankart repair is the stabilization technique of choice. When indicating patients for arthroscopic Bankart repair, it is essential to evaluate both the glenoid and humeral bone loss. Arthroscopic repair alone is contraindicated when GBL exceeds 25%, or in the presence of a large, engaging Hill-Sachs (HS) lesion [16]. Burkhart first classified significant glenoid bone lose as having an “inverted-pear” glenoid, in which enough anterior-inferior bone is lost for the glenoid to assume the shape of a pear [3]. In a study of 194 patients who underwent arthroscopic Bankart repair, 11 of 18 (61.1%) with inverted pear-shaped glenoids experienced recurrent instability [3]. These lesions may lead to chronic instability if not addressed during the index surgery. So-called subcritical bone loss, bone loss below 15%, is an area of controversy. Shaha et al. investigated the clinical outcomes of four subsets of patients with varying degrees of GBL treated solely with arthroscopic Bankart repair. The study found that GBL (13.5%) was predictive of outcome assessed via WOSI score, even in the absence of recurrent dislocation. Patients who had greater than 13.5% GBL experienced significantly higher WOSI scores than would be considered clinically unacceptable with regard to their outcome even in the setting of no recurrence of instability. This led the authors to conclude that the threshold for bone loss should be redefined as a value less than 15%, especially in highly active patients [17]. Similarly Dickens et al. investigated subcritical bone loss in American football players undergoing arthroscopic anterior shoulder stabilization. Their investigation of 50 athletes found a rate of 5.31 cases of recurrent instability per 1000 athlete exposures for subjects with greater than 13.5% GBL. There were no episodes of recurrence in athletes with < 13.5% GBL in 72,000 athlete exposures [18]. The authors concluded that arthroscopic Bankart repair was a reliable procedure in American football players with up to 13.5% GBL. Shin et al. recently evaluated values of critical bone loss in a study of 169 patients. Their statistical analysis defined critical bone loss as 17.3% (sensitivity 75%, specificity 86.6%) [3]. In their study, 42.9% (15 of 35) patients with critical bone loss experienced failure of their surgery compared to 3.7% (5 of 134) in the non-critical group [3]. These two recent studies demonstrate that a gray zone exists between 13.5 to 17.3% GBL, thus indications for arthroscopic Bankart repair versus open glenoid bone grafting should be individualized based on patient’s activity level, goals, and expectations.
The presence of an engaging HS lesion should also be considered when indicating a patient for arthroscopic Bankart repair. Wolf et al. investigated the repair of engaging HS lesions in patients with < 25% GBL. HS engagement was confirmed arthroscopically and managed via lesion filing arthroscopic remplissage. At mean patient follow-up of 58 months, only 2/45 experienced re-dislocation, both following new traumatic events [19]. Itoi et al. examined the effect of HS lesions and their relationship to GBL by examining the glenoid track [20]. The glenoid track is defined as a distance 84% the width of the glenoid, with the track becoming smaller in the setting of GBL. If a HS lesion extends medial to the margin of the glenoid track, it is defined as an “off-track” lesion and can be expected to engage on the glenoid rim during motion causing recurrent dislocation [20]. GBL further reduces the distance the humeral head needs to travel in order for the HS to engage, thus decreasing the size of the glenoid track. The authors concluded that in the setting of such lesions, Bankart repair alone is unlikely to be successful [20]. This concept of “bi-polar” bone loss has emerged as a central area in understanding instability of the shoulder. Locher et al. investigated the recurrence rate in patients with off versus on track HS lesions in 100 patients [3]. In this patient population, 33% (4 of 12) patients with off-track lesions required revision surgery for recurrent instability compared with 6% (5 of 88) in patients with on track injuries.
Fabricant et al. suggested an algorithm that summarizes their preferred treatment methods [21]. In patients presenting with an initial instability event and who are at low risk for recurrence, conservative treatment is preferred. In all other cases, surgery is recommended. Non-contact athletes with less than 10% GBL are treated arthroscopically with single row capsulolabral stabilization. Contact athletes with up to 20% GBL are recommended arthroscopic repair with double row stabilization. Lastly, patients with greater than 20% GBL are recommended open repair with glenoid augmentation and bone fragment fixation [21]. Owens et al. proposed an algorithm for the management of instability in the in-season athlete [22]. Athletes with GBL greater than 13.5 to 17.3%, a large (engaging) HS lesion, or recurrent instability events are recommended to have immediate season ending surgery [23–25]. Patients with an initial instability event at the beginning of the season may attempt return to play following 2–3 weeks of immobilization and physical therapy, if they are able to perform sport specific activities without pain and instability. Athletes who remain symptomatic or those who are injured near the end of the season are recommended to undergo surgical intervention [22].
Regardless of the indications used, surgical intervention is more effective when performed early after injury, with a greater number of instability events prior to surgery portending a worse outcome due to continued damage to the capsulolabral junction with each event [26]. Recurrent instability has also been shown to lead to erosive changes in the glenoid [27]. Krych et al. found that patients with increased number of shoulder dislocations were both more likely to have injury to their glenoid cartilage and more frequently had high-grade glenoid lesions [28]. A decision regarding surgical intervention should be made following a discussion of the goals of surgery as well as the potential risks of delaying repair (Fig. 1). Surgical intervention should be completed as quickly as practical once decided upon as the proper course of treatment. Benefits of using an arthroscopic Bankart repair technique include a lower complication rate, smaller incisions, less blood loss, shorter operative times, greater range of shoulder motion postoperatively, less postoperative pain, better cosmesis, less postoperative shoulder stiffness, and fewer wound infections [4, 29].
Fig. 1.
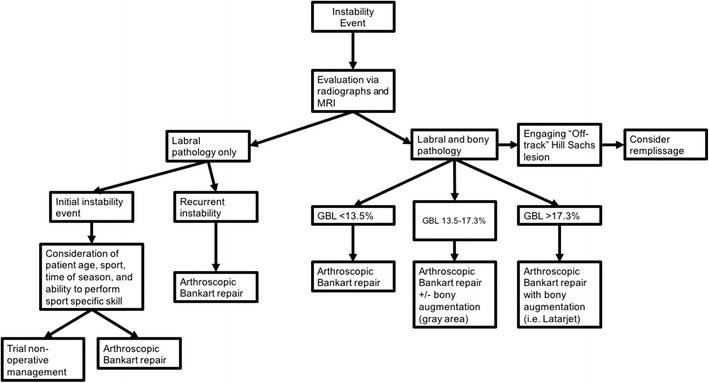
Proposed algorithm for the management of anterior instability based on patient pathology
Surgical Techniques
The goal of Bankart repair is to appropriately release, mobilize, and tension the capsulolabral complex at the antero-inferior aspect of the glenoid. Arthroscopic Bankart repair is performed with standard arthroscopic positioning in either the beach chair (Fig. 2) or lateral decubitus position, based on surgeon experience and familiarity. A discussion of the advantages and disadvantages of beach chair versus lateral decubitus is beyond the scope of this review but has been well-described in the literature [30]. Following patient positioning, the anatomic landmarks of the shoulder are identified including the borders of the acromion, coracoid process, AC joint, and distal clavicle (Fig. 3).
Fig. 2.

Patient in beach chair position, the operative arm is held by a pneumatic arm holder
Fig. 3.

a Anterior landmarks of the shoulder, coracoid (blue arrow), antero-inferior portal, and antero-superior portal (green arrows). b Posterior portal (green arrow), an accessory 5 o’clock portal (blue arrow) can be made inline with the posterior border of the clavicle (dotted line) if posterior pathology is present. c Antero-lateral (white arrow) and posteriolateral (green arrow) corner of the acromion
A posterior portal is created for camera insertion approximately 2 cm distal and 1 cm medial to the postero-lateral border of the acromion. A diagnostic arthroscopy should then be performed to confirm the presence of a Bankart lesion and any associated pathology. Diagnostic arthroscopy should include evaluation of the labrum, capsular tissue, rotator cuff and biceps tendons, humeral head, and assessment and measurement of any HS lesion. An arthroscopic “load-shift” test can be performed to measure anterior and posterior translation. In order to communicate the location of a Bankart lesion, the glenoid can be described as a clock face, with 6 o’clock representing the inferior most aspect of the glenoid and 12 o’clock being the superior most aspect [31]. Following diagnostic arthroscopy, a low antero-inferior portal within the area of the deltopectorial interval should be created. Needle localization is used to enter the joint just above the subscapularis tendon for improved glenoid instrumentation in the axillary pouch and at the 6 o’clock position of the glenoid [31]. Next, an antero-superior portal is created distal to the antero-superior border of the acromion. Needle localization is used to create the portal immediately lateral to the biceps tendon within the rotator interval. Once portals have been established, the lesion should be aggressively mobilized with an arthroscopic elevator or covator. The donor glenoid area is then debrided and decorticated with an arthroscopic shaver to allow for improved soft tissue healing (Fig. 4). The mobility of the capsulolabral lesion should be addressed with a soft tissue grasper, ensuring adequate superior excursion to properly restore the labral bumper. It is essential that the muscle belly of the subscapularis is visualized at this step of the case to ensure adequate mobilization of the capsulolabral complex prior to the repair. The Bankart lesion should be completely free anteriorly before proceeding with fixation (Fig. 5).
Fig. 4.
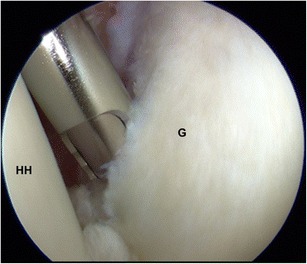
The arthroscopic shaver is used to debride the zone of injury, assist in mobilization of the Bankart lesion, and decorticate bone on the glenoid for improved healing prior to repair. Glenoid (G), humeral head (HH)
Fig. 5.
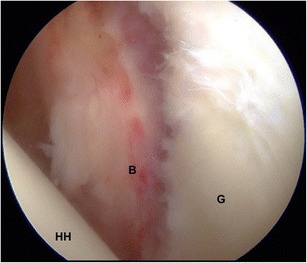
Fully mobilized Bankart lesion (B), glenoid (G), humeral head (HH)
There are numerous techniques available for fixation of Bankart lesions but most involve the use of suture anchors to repair the labral tissue back to the glenoid. Nho et al. examined the differences in the biomechanics between repairs with simple stitch, suture anchor with horizontal mattress stitch, double-loaded suture anchor with simple stich, and knotless suture anchors [32]. This study found that all four constructs displayed less than 2-mm displacement when 25 N of cyclical load was applied; however, the knotless device exhibited significantly less force to ultimate failure while the other three constructs performed similarly [32]. While performance under cyclic loading is clinically important when considering daily tasks, ultimate load to failure may be important to consider when performing repair on contact athletes. Additionally, with regardless to knotless fixation versus tied knots, biomechanical studies have shown that modes and rates of failure have been found to be equivalent [33]. Regardless of construct, it is important to consider the number of suture anchors when performing Bankart repair. Shibata et al. found that repairs using less than four anchors were significantly more likely to fail [34]. Boileau et al. also found that patients who underwent repair with three or less suture anchors were at a higher risk of failure [35].
When repairing the capsulolabral complex to the glenoid, many authors advocate for single row repair of the labrum 1 to 2 mm onto the articular surface, or at the articular edge, following full release and mobilization from the glenoid neck [36]. Other authors argue that repair to the articular surface does not facilitate healing and alters the native anatomy of the capsulolabral complex and instead support double row repair [31, 37, 38]. Moran et al. recommend double row repair in the case of recurrent instability, for a first-time dislocation who are high risk for recurrence, males under age 25, patients who have had more than three dislocations requiring reduction, or contact athletes [21, 31]. It is important to note that these studies have mostly been performed in a laboratory setting and that there are no randomized clinical studies evaluating the differences in clinical outcomes between singe versus double row fixation. For this reason, fixation should be individualized based on patient pathology, with single row fixation being the current accepted standard for repair.
The authors preferred technique is a single row repair performed in the beach chair position. Positioning in beach chair allows for ease of orientation for both the surgical team as well as trainees; ease of treatment of concomitant shoulder pathology; ease of conversion to open surgery such as Latarjet procedure, or humeral avulsion of the glenohumeral ligament (HAGL) repair; and the improved ability to assess the glenohumeral joint through a complete range of motion (range of motion). A suture passer, typically a 45 or 90° angled to the ipsilateral side, is introduced through the low anterior portal and is used to shuttle suture through the avulsed capsulolabral tissue, with care being taken to capture at least 1 cm of capsular tissue in addition to the labrum. The antero-superior portal allows for the usage of instrumentation such as an arthroscopic grasper to reduce the labral tissue, as well as for suture retrieval. Anchors are placed from inferior to superior on the glenoid rim, allowing for reduction of the Bankart lesion, with the first suture being passed as inferior as possible at approximately the 5:30 or 6:30 position [39]. If visualization is difficult, the 30° scope can be inserted into the antero-lateral portal or alternatively, a 70° scope can be used in the posterior viewing portal to improve the visualization for repair.
Complications
Arthroscopic Bankart repair is considered a safe and effective procedure, with a lower complication rate compared to open repair [2]. Implant selection plays an important role in potential complications. Anchor usage can lead to significant pain, decreased ROM, and failure if they are not positioned properly during the initial procedure [40]. Degenerative joint conditions, such as chondrolysis and osteoarthritis (OA), have also been reported as long-term complications of arthroscopic Bankart repair, primarily due to intra-articular pain pumps, which have since fallen out of favor. Postoperative OA in arthroscopic Bankart repairs has not been as extensively studied; however, the few long-term studies published have reported rates of postoperative OA to be as high as 26% [41]. Development of OA, however, is likely due to the initial instability event itself. Hovelius et al. reported an 11% rate of mild and a 9% rate of moderate OA 10 years following primary dislocation [42]. One study found mild to severe OA in 50 out of 74 shoulders [43]. In an 8-year follow-up study by Francheschi et al., the most common risk factors for OA after arthroscopic Bankart repairs were older age at first dislocation, increased length of time from first injury to surgery, increased number of anchors used, and the degenerative state of the labrum at time of surgery, indicating that factors other than quality of repair likely contribute to development of OA [44].
As with most arthroscopic shoulder surgeries, there is always the potential for infection and nerve injury. Data from the American Board of Orthopedic Surgery has shown that the infection rate in arthroscopic Bankart repair is 0.22% [2]. Despite this low rate, it is important to evaluate patient risk factors for infection as a preventative measure. Nerve injury occurs more frequently than infection (0.3%) and most often affects the axillary nerve [2, 45]. Anatomically, the axillary nerve courses around the inferior aspect of the glenoid from anterior-to-posterior and is at risk during aggressive mobilization of the Bankart lesion as well as during anchor placement. Hill et al. reviewed 15,000 patients undergoing shoulder arthroscopy for any reason and found a 30-day readmission rate of only 0.98%. The most common causes for readmission was pulmonary embolism (0.09%), with surgery > 1.5 h, age 40–65, ASA class 3 or greater, and chronic steroid use being predictors for readmission [46].
Outcomes
Following arthroscopic Bankart repair, clinical outcomes may be assessed by several clinical metrics including recurrence of shoulder instability, ROM, return to work or sport, complication rate including reoperation, and various patient reported outcome measures (PROMs) (Table 2).
Table 2.
Recent clinical studies and outcomes on arthroscopy instability repair
| Authors | Journal (year) | N | Mean follow-up in months | Outcomes | Recurrence rate |
|---|---|---|---|---|---|
| Castagna et al. [47] | Am J Sports Med (2010) | 31 | 130.8 | Rowe score, 80.1 UCLA score, 32.1 71% returned to activity |
19.4% |
| Voos et al. [48] | Am J Sports Med (2010) | 73 | 33 | ASES score, 94.9 | 9.6% |
| Cho et al. [49] | Clin Orthop Surgery (2010) | 62 | 15 | ASES score, 91.8 Rowe, 94.1 |
NA |
| Zhu et al. [50] | Am J Sports Med (2011) | 49 | 29 | ASES score, 96 Rowe score, 89.8 Constant score, 97.8 |
8.2% |
| Millett et al. [51] | Am J Sports Med (2013) | 15 | 32.4 | ASES score, 98 quickDASH, 2.8 |
7% |
| Jiang et al. [52] | Am J Sports Med (2013) | 50 | 32.5 | ASES score, 95.7 Rowe score, 91.4 |
8% |
| Maiotti et al. [53] | J Shoulder Elbow Surg (2016) | 89 | 31.5 | ASES score, 95.5 Rowe score, 94.1 |
3.3& |
| Milchteim et al. [54] | Arthroscopy (2016) | 94 | 60 | ASES score, 91.5 Rowe score, 84.3 Satisfaction, 8.8/10 |
6.4% |
| Maiotti et al. [55] | Arthroscopy (2016) | 110 | 40.5 | ASES score, 96.5 Rowe score, 95.3 VAS score, 0.5 |
2.7% |
| Bionna et al. [5] | Am J Sports Med (2016) | 60 | 63.6 | SPORTS score, 8 | 10% |
| Aboalata et al. [3] | Am J Sports Med (2017) | 180 | 156 | Satisfied, 92.3% Return to sport, 49.5% |
18.2% |
| Nakagawa et al. [56] | Am J Sports Med (2017) | 172 | 24 | NA | 29.4% |
Recurrence of Shoulder Instability
While a large number of studies have looked at recurrence of shoulder instability following arthroscopic Bankart repair, a large degree of variability exists ranging from 3.4 to 33.3% lifetime recurrence rate, with an average rate of 13.1% when pooling 12 high-quality trials [8, 57–64]. The reported recurrence rate after arthroscopic Bankart repair ranges from 4 to 19% [65]; in newer literature, the risk is increased by participation in contact sports [66]. Additionally, the average amount of time prior to another instability event is less with arthroscopic than open Bankart repair (12.6 versus 34.2 months, respectively) [9]. Patients who desire to return to contact sports should be counseled on the higher recurrent instability rate after arthroscopic repair and weigh this risk against the benefits of this technique, including a faster return to activity, as well as a greater likelihood that they will be able to do so [5]. With regard to open versus arthroscopic repair, Fabbriciani et al. concluded that open Bankart repair does not offer significantly better 2-year results in terms of stability than arthroscopic repair and may negatively affect the recovery of full range of motion [67]. Kim et al. reported that 95% of a 167 patient cohort who underwent arthroscopic Bankart repair for traumatic recurrent instability of the anterior shoulder scored good (17%) to excellent (78%) on the Rowe score scale at a mean follow-up of 44 months [68]. One study found that recurrent dislocation rates of shoulders repaired arthroscopically versus open procedure were comparable at 13-year follow-up [3].
Range of Motion (ROM)
Following arthroscopic Bankart repair, average external rotation is commonly decreased, both with the arm at the side (ranging between 3.5 and 9°) and with the arm abducted to 90° (ranging between 3.5 and 7°) [8, 57–59, 68]. Similarly, a small degree of average loss of forward flexion is to be expected, ranging 1–3° [57]. Despite this, some studies have suggested that arthroscopic repair has a lower rate of postoperative stiffness compared to open repair [10, 65]. A meta-analysis by Wang et al. analyzed four studies with ROM outcomes after open and arthroscopic Bankart repairs. Patients surgically treated by arthroscopic repair had significantly better range of motion than those treated by open repair [10]. Stiffness can be due to excess immobilization after surgery and can often be treated conservatively with physical therapy and corticosteroid injections into the glenohumeral joint. In extreme cases, arthroscopic capsular release can be performed after conservative approaches have been exhausted [45].
Return to Work/Sport
Return to previous level of work ranges from 46 to 97% following arthroscopic Bankart repair with an average rate of 70.7% when pooling data from six high-quality studies [57, 58, 61, 62, 64, 69]. Recent long-term data have shown that return to previous athletic level is possible in as few as 49.5% of patients, although return to play has been shown to be as high as 90% in other studies [3, 70].
Functional Outcomes
In a study of 180 patients seen at average follow-up of 13 years following arthroscopic Bankart repair, overall long-term patient satisfaction was 92.3% [11]. With regard to patient recorded outcomes scales, the ASES (American Shoulder and Elbow Surgeons) shoulder score and the Rowe score are frequently used methods of assessment following arthroscopy Bankart repair. While the ASES score focuses on pain level and functional ability both at work and leisure activity, the Rowe score is based stability, motion, and function. ASES scores following arthroscopic Bankart repair have ranged from 87 to 98 while Rowe scores generally range from 77 to 97 at a minimum follow-up of 2 years, indicating a high level of motion and function following arthroscopic repair (Table 1) [5, 47–56].
Future Directions
Future increased understanding of the effects of new repair techniques, bi-polar bone loss, and adjuvant procedures should help improve outcomes when managing shoulder instability. Studies investigating the consequences of humeral bone loss, such as those by Itoi et al. [20], have led to innovation in arthroscopic stabilization by identifying a potential cause of failure following “simple” Bankart repair. Hartzler et al. further explored this theory by performing a biomechanical analysis of the glenoid track concept following Bankart repair with and without remplissage of the HS lesion [71]. The authors found that the addition of remplissage prevented HS engagement in all shoulders with large lesions which were not otherwise stabilized with Bankart repair alone [71]. Ko et al. examined the clinical outcomes of concomitant remplissage in patients with engaging HS lesions undergoing Bankart repair [72]. Forty-eight patients with engaging HS lesions underwent surgical stabilization, 24 with Bankart repair alone, and 24 with Bankart combined with remplissage. Five patients in the Bankart group experienced recurrent dislocation compared to zero in the combined group. ASES and Rowe score were also significantly better in the combined procedure group [72]. Also, the remplissage group experienced less loss of motion in external rotation and abduction than the isolated Bankart repair group, potentially alleviated concerns of over constraint when addressing engaging HS lesions [72]. As the understanding of bi-polar bone loss continues to evolve, future studies are required to determine the long-term clinical outcomes of patients treated with Bankart repair combined with remplissage. Additionally, arthroscopic Bankart repair in patients with less than 13.5% bone loss will result in successful outcome and in patients with more than 17.3% bone loss, addressing the anterior glenoid with bone grafting is essential to ensure success [3]. The gray zone is between 13.5 to 17.3% and in these patients, indications for arthroscopic Bankart repair vs. open glenoid bone grafting (Latarjet, etc.) should be individualized based on patient’s activity level, goals, and expectations.
Conclusion
Arthroscopic Bankart repair is currently the preferred method for surgical management of anterior shoulder instability in a majority of patients with minimum GBL based its growth in popularity due to its relative lack of invasiveness and low overall complication rate. Arthroscopic Bankart repair is an ideal method of stabilization in patients with an injury to the inferior labrum without significant osseous injury (large bony Bankart or HS lesion). Overall, when performed for the correct indications, arthroscopic repair results in a low risk for recurrent instability and a high return to sport or work. Future work must focus on longer-term outcomes and rate of glenohumeral arthritis in patients undergoing arthroscopic Bankart repair. Additionally, further work is needed to investigate the clinical outcomes in patients with larger bony defects and those undergoing concomitant stabilization procedures such as arthroscopic remplissage.
Compliance with Ethical Standards
Conflict of Interest
Brett D. Owens reports non-financial support from MTF/CONMED and Mitek, outside the submitted work. The rest of the authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Management of Anterior Shoulder Instability
References
- 1.el Akad AM, Winge S, Molinari M, Eriksson E. Arthroscopic Bankart procedures for anterior shoulder instability. A review of the literature. Knee Surg Sports Traumatol Arthrosc. 1993;1(2):113–122. doi: 10.1007/BF01565465. [DOI] [PubMed] [Google Scholar]
- 2.Owens BD, Harrast JJ, Hurwitz SR, Thompson TL, Wolf JM. Surgical trends in Bankart repair: an analysis of data from the American Board of Orthopaedic Surgery certification examination. Am J Sports Med. 2011;39(9):1865–1869. doi: 10.1177/0363546511406869. [DOI] [PubMed] [Google Scholar]
- 3.Aboalata M, Plath JE, Seppel G, Juretzko J, Vogt S, Imhoff AB. Results of arthroscopic Bankart repair for anterior-inferior shoulder instability at 13-year follow-up. Am J Sports Med. 2016:1–6. [DOI] [PubMed]
- 4.Alkaduhimi H, van der Linde JA, Willigenburg NW, Paulino Pereira NR, van Deurzen DFP, van den Bekerom MPJ. Redislocation risk after an arthroscopic Bankart procedure in collision athletes: a systematic review. J Shoulder Elb Surg Elsevier Inc. 2016;25(9):1549–1558. doi: 10.1016/j.jse.2016.05.002. [DOI] [PubMed] [Google Scholar]
- 5.Blonna D, Bellato E, Caranzano F, Assom M, Rossi R, Castoldi F. Arthroscopic Bankart repair versus open Bristow-Latarjet for shoulder instability: a matched-pair multicenter study focused on return to sport. Am J Sports Med. 2016;44(12):3198–3205. doi: 10.1177/0363546516658037. [DOI] [PubMed] [Google Scholar]
- 6.Carreira DS, Mazzocca AD, Oryhon J, Brown FM, Hayden JK, Romeo AA. A prospective outcome evaluation of arthroscopic Bankart repairs: minimum 2-year follow-up. Am J Sports Med. 2006;34(5):771–777. doi: 10.1177/0363546505283259. [DOI] [PubMed] [Google Scholar]
- 7.Green MR, Christensen KP. Arthroscopic versus open Bankart procedures: a comparison of early morbidity and complications. Arthroscopy. 1993;9(4):371–374. doi: 10.1016/S0749-8063(05)80308-1. [DOI] [PubMed] [Google Scholar]
- 8.Guanche CA, Quick DC, Sodergren KM, Buss DD. Arthroscopic versus open reconstruction of the shoulder in patients with isolated Bankart lesions. Am J Sports Med. 1996;24(2):144–148. doi: 10.1177/036354659602400204. [DOI] [PubMed] [Google Scholar]
- 9.Virk MS, Manzo RL, Cote M, Ware JK, Mazzocca AD, Nissen CW, et al. Comparison of time to recurrence of instability after open and arthroscopic Bankart repair techniques. Orthop J Sport Med. 2016;4(6):2325967116654114. doi: 10.1177/2325967116654114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang L, Liu Y, Su X, Liu S. A meta-analysis of arthroscopic versus open repair for treatment of Bankart lesions in the shoulder. Med Sci Monit. 2015;21:3028–3035. doi: 10.12659/MSM.894346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Balg F, Boileau P. The instability severity index score. J Bone Jt Surg - Br. 2007;89–B(11):1470–1477. doi: 10.1302/0301-620X.89B11.18962. [DOI] [PubMed] [Google Scholar]
- 12.Phadnis J, Arnold C, Elmorsy A, Flannery M. Utility of the instability severity index score in predicting failure after arthroscopic anterior stabilization of the shoulder. Am J Sports Med. 2015;43(8):1983–1988. doi: 10.1177/0363546515587083. [DOI] [PubMed] [Google Scholar]
- 13.Owens BD, Duffey ML, Nelson BJ, DeBerardino TM, Taylor DC, Mountcastle SB. The incidence and characteristics of shoulder instability at the United States Military Academy. Am J Sports Med. 2007;35(7):1168–1173. doi: 10.1177/0363546506295179. [DOI] [PubMed] [Google Scholar]
- 14.Owens LCBD, Nelson BJ, Duffey ML, Mountcastle SB, Taylor C, Ret DC, Cameron KL, et al. Pathoanatomy of first-time, traumatic, anterior glenohumeral subluxation events. J Bone Jt Surgery-American Vol. 2010;92(7):1605–1611. doi: 10.2106/JBJS.I.00851. [DOI] [PubMed] [Google Scholar]
- 15.Robinson CM, Howes J, Murdoch H, Will E, Graham C. Functional outcome and risk of recurrent instability after primary traumatic anterior shoulder dislocation in young patients. J Bone Jt Surg. 2006;88–A(11):2326–2336. doi: 10.2106/JBJS.E.01327. [DOI] [PubMed] [Google Scholar]
- 16.Di Giacomo G, De Vita A, Costantini A, de Gasperis N, Scarso P. Management of humeral head deficiencies and glenoid track. Curr Rev Musculoskelet Med [Internet] Springer. 2014;7(1):6–11. doi: 10.1007/s12178-013-9194-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shaha JS, Cook JB, Song DJ, Rowles DJ, Bottoni CR, Shaha SH, et al. Redefining “critical” bone loss in shoulder instability. Am J Sports Med. 2015;43(7):1719–1725. doi: 10.1177/0363546515578250. [DOI] [PubMed] [Google Scholar]
- 18.Dickens JF, Owens BD, Cameron KL, DeBerardino TM, Masini BD, Peck KY, et al. The effect of subcritical bone loss and exposure on recurrent instability after arthroscopic bankart repair in intercollegiate American football. Am J Sports Med. SAGE PublicationsSage CA: Los Angeles, CA; 2017 5 [cited 2017 May 7];36354651770418 Available from: http://journals.sagepub.com/doi/10.1177/0363546517704184 [DOI] [PubMed]
- 19.Wolf EM, Arianjam A. Hill-Sachs remplissage, an arthroscopic solution for the engaging Hill-Sachs lesion: 2- to 10-year follow-up and incidence of recurrence. J Shoulder Elb Surg. 2014;23(6):814–820. doi: 10.1016/j.jse.2013.09.009. [DOI] [PubMed] [Google Scholar]
- 20.Yamamoto N, Itoi E, Abe H, Minagawa H, Seki N, Shimada Y, et al. Contact between the glenoid and the humeral head in abduction, external rotation, and horizontal extension: a new concept of glenoid track. J Shoulder Elb Surg. 2007;16(5):649–656. doi: 10.1016/j.jse.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 21.Fabricant PD, Taylor SA, McCarthy MM, Gausden EB, Moran CJ, Kang RW, et al. Open and arthroscopic anterior shoulder stabilization. JBJS Rev. 2015;3(2) [DOI] [PubMed]
- 22.Owens BD, Dickens JF, Kilcoyne KG, Rue J-PH. Management of mid-season traumatic anterior shoulder instability in athletes. J Am Acad Orthop Surg. 2012;20(8):518–526. doi: 10.5435/JAAOS-20-08-518. [DOI] [PubMed] [Google Scholar]
- 23.Donohue MA, Owens BD, Dickens JF. Return to play following anterior shoulder dislocation and stabilization surgery. Clin Sports Med. 2016;35:545–61. [DOI] [PubMed]
- 24.Locher J, Wilken F, Beitzel K, Buchmann S, Longo UG, Denaro V, et al. Hill-Sachs off-track lesions as risk factor for recurrence of instability after arthroscopic Bankart repair. Arthroscopy. 2016;32(10):1993–1999. doi: 10.1016/j.arthro.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 25.Shin S-J, Kim RG, Jeon YS, Kwon TH. Critical value of anterior glenoid bone loss that leads to recurrent glenohumeral instability after arthroscopic Bankart repair. Am J Sports Med. SAGE PublicationsSage CA: Los Angeles, CA; 2017 Jul 23 [cited 2017 Jul 28];45(9):1975–81 Available from: http://journals.sagepub.com/doi/10.1177/0363546517697963 [DOI] [PubMed]
- 26.Dumont GD, Russell RD, Robertson WJ. Anterior shoulder instability: a review of pathoanatomy, diagnosis and treatment. Curr Rev Musculoskelet Med. 2011;4(4):200–207. doi: 10.1007/s12178-011-9092-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sugaya H, Moriishi J, Dohi M, Kon Y, Tsuchiya A. Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Joint Surg Am. 2003;85–A(5):878–884. doi: 10.2106/00004623-200305000-00016. [DOI] [PubMed] [Google Scholar]
- 28.Krych AJ, Sousa PL, King AH, Morgan JA, May JH, Dahm DL. The effect of cartilage injury after arthroscopic stabilization for shoulder instability. Orthopedics. 2015;38(11):e965–e969. doi: 10.3928/01477447-20151020-03. [DOI] [PubMed] [Google Scholar]
- 29.Virk MS, Manzo RL, Cote M, Ware JK, Mazzocca AD, Nissen CW, et al. Comparison of time to recurrence of instability after open and arthroscopic Bankart repair techniques. Orthop J Sport Med. 2016;4(6):2325967116654114. doi: 10.1177/2325967116654114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Peruto CM, Ciccotti MG, Cohen SB. Shoulder arthroscopy positioning: lateral decubitus versus beach chair. Arthrosc J Arthrosc Relat Surg. 2009;25(8):891–896. doi: 10.1016/j.arthro.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 31.Moran CJ, Fabricant PD, Kang R, Cordasco FA. Arthroscopic double-row anterior stabilization and Bankart repair for the “high-risk” athlete. Arthrosc Tech. 2014;3(1):e65–e71. doi: 10.1016/j.eats.2013.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nho SJ, Frank RM, Van Thiel GS, Wang FC, Wang VM, Provencher MT, et al. A biomechanical analysis of anterior Bankart repair using suture anchors. Am J Sports Med. 2010;38(7):1405–1412. doi: 10.1177/0363546509359069. [DOI] [PubMed] [Google Scholar]
- 33.Ranawat AS, Golish SR, Miller MD, Caldwell PE, Singanamala N, Treme G, et al. Modes of failure of knotted and knotless suture anchors in an arthroscopic Bankart repair model with the capsulolabral tissues intact. Am J Orthop (Belle Mead NJ) 2011;40(3):134–138. [PubMed] [Google Scholar]
- 34.Shibata H, Gotoh M, Mitsui Y, Kai Y, Nakamura H, Kanazawa T, et al. Risk factors for shoulder re-dislocation after arthroscopic Bankart repair. J Orthop Surg Res. 2014;9(1):53. doi: 10.1186/s13018-014-0053-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Boileau P, Villalba M, Héry J-Y, Balg F, Ahrens P, Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Jt Surg. 2006;88(8):1755. doi: 10.2106/JBJS.E.00817. [DOI] [PubMed] [Google Scholar]
- 36.Magit DP, Tibone JE, Lee TQ. In vivo comparison of changes in glenohumeral translation after arthroscopic capsulolabral reconstructions. Am J Sports Med. 2008;36(7):1389–1396. doi: 10.1177/0363546508315199. [DOI] [PubMed] [Google Scholar]
- 37.Lafosse L, Baier GP, Jost B. Footprint fixation for arthroscopic reconstruction in anterior shoulder instability: the Cassiopeia double-row technique. Arthroscopy. 2006;22(2):231.e1–231.e6. doi: 10.1016/j.arthro.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 38.Ahmad CS, Galano GJ, Vorys GC, Covey AS, Gardner TR, Levine WN. Evaluation of glenoid capsulolabral complex insertional anatomy and restoration with single- and double-row capsulolabral repairs. J Shoulder Elb Surg. 2009;18(6):948–954. doi: 10.1016/j.jse.2009.03.022. [DOI] [PubMed] [Google Scholar]
- 39.Owens BDGE. Uncomplicated anterior instability: the “simple” arthroscopic Bankart reconstruction. In: Abrams J, TJ BR, editors. Advanced reconstruction: shoulder 2. Chicago, IL: AAOS.
- 40.Dhawan A, Ghodadra N, Karas V, Salata MJ, Cole BJ. Complications of bioabsorbable suture anchors in the shoulder. Am J Sports Med. 2012;40(6):1424–1430. doi: 10.1177/0363546511417573. [DOI] [PubMed] [Google Scholar]
- 41.Harris JD, Gupta AK, Mall NA, Abrams GD, McCormick FM, Cole BJ, et al. Long-term outcomes after Bankart shoulder stabilization. Arthrosc J Arthrosc Relat Surg. 2013;29(5):920–933. doi: 10.1016/j.arthro.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 42.Hovelius L, Augustini BG, Fredin H, Johansson O, Norlin R, Thorling J. Primary anterior dislocation of the shoulder in young patients. A ten-year prospective study. J Bone Joint Surg Am. 1996;78(11):1677–1684. doi: 10.2106/00004623-199611000-00006. [DOI] [PubMed] [Google Scholar]
- 43.Kavaja L, Pajarinen J, Sinisaari I, Savolainen V, Björkenheim J-M, Haapamäki V, et al. Arthrosis of glenohumeral joint after arthroscopic Bankart repair: a long-term follow-up of 13 years. J Shoulder Elb Surg. 2012;21(3):350–355. doi: 10.1016/j.jse.2011.04.023. [DOI] [PubMed] [Google Scholar]
- 44.Franceschi F, Papalia R, Del Buono A, Vasta S, Maffulli N, Denaro V. Glenohumeral osteoarthritis after arthroscopic Bankart repair for anterior instability. Am J Sports Med. 2011;39(8):1653–1659. doi: 10.1177/0363546511404207. [DOI] [PubMed] [Google Scholar]
- 45.Petrera M, Dwyer T, Tsuji MRS, Theodoropoulos JS. Outcomes of arthroscopic Bankart repair in collision versus noncollision athletes. Orthopedics. 2013;36(5):e621–e626. doi: 10.3928/01477447-20130426-25. [DOI] [PubMed] [Google Scholar]
- 46.Hill JR, McKnight B, Pannell WC, Heckmann N, Sivasundaram L, Mostofi A, et al. Risk factors for 30-day readmission following shoulder arthroscopy. Arthroscopy. 2017;33(1):55–61. doi: 10.1016/j.arthro.2016.06.048. [DOI] [PubMed] [Google Scholar]
- 47.Castagna A, Markopoulos N, Conti M, Rose GD, Papadakou E, Garofalo R. Arthroscopic Bankart suture-anchor repair: radiological and clinical outcome at minimum 10 years of follow-up. Am J Sports Med. 2010;38(10):2012–2016. doi: 10.1177/0363546510372614. [DOI] [PubMed] [Google Scholar]
- 48.Voos JE, Livermore RW, Feeley BT, Altchek DW, Williams RJ, Warren RF, et al. Prospective evaluation of arthroscopic Bankart repairs for anterior instability. Am J Sports Med. 2010;38(2):302–307. doi: 10.1177/0363546509348049. [DOI] [PubMed] [Google Scholar]
- 49.Cho HL, Lee CK, Hwang TH, Suh KT, Park JW. Arthroscopic repair of combined Bankart and SLAP lesions: operative techniques and clinical results. Clin Orthop Surg. 2010;2(1):39. doi: 10.4055/cios.2010.2.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhu Y-M, Lu Y, Zhang J, Shen J-W, Jiang C-Y. Arthroscopic Bankart repair combined with remplissage technique for the treatment of anterior shoulder instability with engaging Hill-Sachs lesion: a report of 49 cases with a minimum 2-year follow-up. Am J Sports Med. 2011;39(8):1640–1647. doi: 10.1177/0363546511400018. [DOI] [PubMed] [Google Scholar]
- 51.Millett PJ, Horan MP, Martetschläger F. The “bony Bankart bridge” technique for restoration of anterior shoulder stability. Am J Sports Med [Internet]. SAGE Publications Sage CA: Los Angeles, CA; 2013 Mar [cited 2017 Apr 1];41(3):608–14 Available from: http://journals.sagepub.com/doi/10.1177/0363546512472880 [DOI] [PubMed]
- 52.Jiang C-Y, Zhu Y-M, Liu X, Li F-L, Lu Y, Wu G. Do reduction and healing of the bony fragment really matter in arthroscopic bony Bankart reconstruction?: a prospective study with clinical and computed tomography evaluations. Am J Sports Med. 2013;41(11):2617–2623. doi: 10.1177/0363546513499304. [DOI] [PubMed] [Google Scholar]
- 53.Maiotti M, Russo R, Zanini A, Schröter S, Massoni C, Bianchedi D. Arthroscopic Bankart repair and subscapularis augmentation: an alternative technique treating anterior shoulder instability with bone loss. J Shoulder Elb Surg. 2016;25(6):898–906. doi: 10.1016/j.jse.2015.09.025. [DOI] [PubMed] [Google Scholar]
- 54.Milchteim C, Tucker SA, Nye DD, Lamour RJ, Liu W, Andrews JR, et al. Outcomes of Bankart repairs using modern arthroscopic technique in an athletic population. Arthroscopy. 2016;32(7):1263–1270. doi: 10.1016/j.arthro.2016.01.025. [DOI] [PubMed] [Google Scholar]
- 55.Maiotti M, Massoni C, Russo R, Schroter S, Zanini A, Bianchedi D. Arthroscopic subscapularis augmentation of Bankart repair in chronic anterior shoulder instability with bone loss less than 25% and capsular deficiency: clinical multicenter study. Arthrosc J Arthrosc Relat Surg Arthroscopy Association of North America. 2016:1–8. [DOI] [PubMed]
- 56.Nakagawa S, Iuchi R, Mae T, Mizuno N, Take Y. Clinical outcome of arthroscopic Bankart repair combined with simultaneous capsular repair. Am J Sports Med [Internet]. SAGE PublicationsSage CA: Los Angeles, CA; 2017 30 [cited 2017 Apr 1]; 36354651668775 Available from: http://journals.sagepub.com/doi/10.1177/0363546516687752 [DOI] [PubMed]
- 57.Cole BJ, L’Insalata J, Irrgang J, Warner JJ. Comparison of arthroscopic and open anterior shoulder stabilization. A two to six-year follow-up study. J Bone Joint Surg Am. 2000;82–A(8):1108–1114. doi: 10.2106/00004623-200008000-00007. [DOI] [PubMed] [Google Scholar]
- 58.Kim S-H, Ha K-I, Kim S-H. Bankart repair in traumatic anterior shoulder instability: open versus arthroscopic technique. Arthroscopy. 2002;18(7):755–763. doi: 10.1053/jars.2002.31701. [DOI] [PubMed] [Google Scholar]
- 59.Mahiroğulları M, Ozkan H, Akyüz M, Uğraş AA, Güney A, Kuşkucu M. Comparison between the results of open and arthroscopic repair of isolated traumatic anterior instability of the shoulder. Acta Orthop Traumatol Turc. 2010;44(3):180–185. doi: 10.3944/AOTT.2010.2289. [DOI] [PubMed] [Google Scholar]
- 60.Netto NA, Tamaoki MJS, Lenza M, dos Santos JBG, Matsumoto MH, Faloppa F, et al. Treatment of Bankart lesions in traumatic anterior instability of the shoulder: a randomized controlled trial comparing arthroscopy and open techniques. Arthrosc J Arthrosc Relat Surg. 2012;28(7):900–908. doi: 10.1016/j.arthro.2011.11.032. [DOI] [PubMed] [Google Scholar]
- 61.Geiger DF, Hurley JA, Tovey JA, Rao JP. Results of arthroscopic versus open Bankart suture repair. Clin Orthop Relat Res. 1997 Apr [cited 2017 Feb 21];(337):111–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9137182. [DOI] [PubMed]
- 62.Sandow MJ, David HG, Misan D. Bankart repair using a suture anchor: a comparison between an arthroscopic and open technique. J Shoulder Elb Surg [Internet]. Elsevier; 1996 Mar [cited 2017 Feb 21];5(2):S88. Available from: http://linkinghub.elsevier.com/retrieve/pii/S1058274696803946
- 63.Sperber A, Hamberg P, Karlsson J, Swärd L, Wredmark T. Comparison of an arthroscopic and an open procedure for posttraumatic instability of the shoulder: a prospective, randomized multicenter study. J Shoulder Elb Surg. 2001;10(2):105–108. doi: 10.1067/mse.2001.112019. [DOI] [PubMed] [Google Scholar]
- 64.Steinbeck J, Jerosch J. Arthroscopic transglenoid stabilization versus open anchor suturing in traumatic anterior instability of the shoulder. Am J Sports Med. 1998;26(3):373–378. doi: 10.1177/03635465980260030501. [DOI] [PubMed] [Google Scholar]
- 65.Ahmed I, Ashton F, Robinson CM. Arthroscopic Bankart repair and capsular shift for recurrent anterior shoulder instability. J Bone Jt Surg. 2012;94(14):1308–1315. doi: 10.2106/JBJS.J.01983. [DOI] [PubMed] [Google Scholar]
- 66.Cho NS, Hwang JC, Rhee YG. Arthroscopic stabilization in anterior shoulder instability: collision athletes versus noncollision athletes. Arthrosc - J Arthrosc Relat Surg. 2006;22(9):947–953. doi: 10.1016/j.arthro.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 67.Fabbriciani C, Milano G, Demontis A, Fadda S, Ziranu F, Mulas PD. Arthroscopic versus open treatment of Bankart lesion of the shoulder: a prospective randomized study. Arthrosc - J Arthrosc Relat Surg. 2004;20(5):456–462. doi: 10.1016/j.arthro.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 68.Kim S-H, Ha K-I, Cho Y-B, Ryu B-D, Oh I. Arthroscopic anterior stabilization of the shoulder: two to six-year follow-up. J Bone Joint Surg Am. 2003;85–A(8):1511–1518. doi: 10.2106/00004623-200308000-00012. [DOI] [PubMed] [Google Scholar]
- 69.Sperling JW, Duncan SFM, Torchia ME, O’Driscoll SW, Cofield RH. Bankart repair in patients aged fifty years or greater: results of arthroscopic and open repairs. J Shoulder Elb Surg. 2005;14(2):111–113. doi: 10.1016/j.jse.2004.06.011. [DOI] [PubMed] [Google Scholar]
- 70.Donohue MA, Owens BD, Dickens JF. Return to play following anterior shoulder dislocation and stabilization surgery. Clin Sports Med. 2016;35(4):545–561. doi: 10.1016/j.csm.2016.05.002. [DOI] [PubMed] [Google Scholar]
- 71.Hartzler RU, Bui CNH, Jeong WK, Akeda M, Peterson A, McGarry M, et al. Remplissage of an off-track Hill-Sachs lesion is necessary to restore biomechanical glenohumeral joint stability in a bipolar bone loss model. Arthrosc J Arthrosc Relat Surg. 2016;32(12):2466–2476. doi: 10.1016/j.arthro.2016.04.030. [DOI] [PubMed] [Google Scholar]
- 72.Ko S-H, Cha J-R, Lee C-C, Hwang I-Y, Choe C-G, Kim M-S. The influence of arthroscopic remplissage for engaging Hill-Sachs lesions combined with Bankart repair on redislocation and shoulder function compared with Bankart repair alone. Clin Orthop Surg. 2016;8(4):428. doi: 10.4055/cios.2016.8.4.428. [DOI] [PMC free article] [PubMed] [Google Scholar]


