Abstract
Purpose of Review
Glenoid Bone Loss is a commonly encountered problem in anterior shoulder instability. In this article, we review current techniques for diagnosis, indications and management of glenoid bone loss.
Recent Findings
Multiple bone grafting techniques are available depending on the glenoid defect size including the coracoid, distal clavicle, iliac crest, and allograft distal tibia. Advancement in imaging methods allows for more accurate quantification of bone loss. Indications and techniques are continuing to evolve, and emerging evidence suggests that smaller degrees of bone loss “subcritical” may be best treated with bone grafting.
Summary
Future directions for innovation and investigation include improved arthroscopic techniques and a refinement of indications for the type of bone grafts and when to indicate a patient of arthroscopic repair versus glenoid bone grafting for smaller degrees of bone loss to ensure successful outcome.
Keywords: Glenoid bone loss, Shoulder instability, Latarjet, Distal tibia allograft
Introduction
Anterior shoulder instability is a commonly diagnosed and treated shoulder disorder [1]. The most common underlying pathology is an injury to the anterior glenoid labrum or Bankart lesion; however, there is often an associated osseous defect in the glenoid and/or humeral head [2]. Following an initial shoulder dislocation, an osseous defect is present in up to 22% of patients, and up to 88% of patients with recurrent instability [3, 4]. Glenoid bone deficiency leads to recurrent glenohumeral instability by altering its function as a static restraint of the shoulder [5]. Historically, research in anterior shoulder instability was focused on the importance of the soft tissue envelope surrounding the glenohumeral joint. Glenoid bone loss is now a recognized cause of recurrent shoulder dislocations or poorer functional outcomes following an arthroscopic or open soft tissue repair for glenohumeral instability [6–9]. In the past 10–15 years, more attention is being paid to the role of glenoid bone deficiency and its management for patients with recurrent anterior shoulder instability. Advances in imaging, quantification of bone loss and evolution in bone grafting techniques continue to emerge. This article reviews new and established techniques for imaging and calculating glenoid bone loss, as well as evolving indications for intervention and current options available for surgical management.
Diagnosis of Glenoid Bone Loss
History and Physical Exam
An accurate and detailed history is helpful for making the diagnosis of glenoid bone deficiency. Acute bone loss in the primary dislocator’s initial dislocation event often involves a high energy injury with an axial load placed on the glenoid [7]. Patients with bone loss experience subsequent instability episodes with increasing frequency even with lower energy episodes. A comprehensive shoulder exam should be performed taking note of axillary nerve dysfunction and distal arm paresthesias. Axillary nerve dysfunction can manifest as sensory alterations, deltoid weakness, and atrophy. Following a dislocation event, axillary nerve palsy is present in up to 48% of patients (range 13.5–48%) [10–12]. However, even complete axillary nerve injuries should receive surgery as reasonable function can be attained in the setting of a permanent injury [13•]. Instability apprehension is apparent with early to midrange abduction and external rotation and worsens with increasing severity of glenoid bone deficiency [14–16]. Patients who describe instability and apprehension with daily activities coupled with night-time instability will frequently have substantial glenoid and humeral bone loss. Risk factors for recurrent instability such as younger age, athletes (particularly those participating in contact and overhead sports), and generalized ligamentous laxity lower the threshold at which bone loss is tolerated [16].
Imaging
Standard AP, axillary lateral, and scapular Y radiographs of the shoulder should initially be obtained. In addition, specific projections with the beam angled obliquely to the glenoid face may provide more detail, including the Bernageau profile view (Fig. 1), Didiee, West Point, and apical oblique views [17–20]. Radiography, while helpful in identifying bone loss, is not as accurate as computed tomography (CT) and magnetic resonance imaging (MRI) for quantifying bone loss [21•].
Fig. 1.
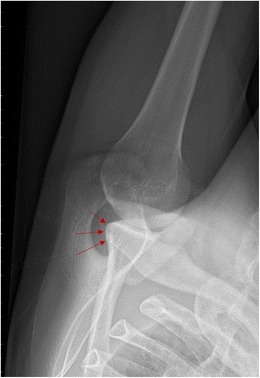
Bernageau view of the left shoulder. The anterior glenoid, indicated with red arrows, is easily visualized in profile
CT imaging is helpful to understand bone loss; however, standard 2-dimensional (2D) CT imaging of the glenoid can over or underestimate glenoid bone loss if the patient is not accurately oriented in the CT gantry [22•]. Three-dimensional (3D) CT is the current gold standard imaging modality for accurately demonstrating glenoid bone loss [23]. It removes the effect of gantry angles and allows the user to orient the glenohumeral joint with the scapula plane [22•]. It provides the ability to subtract the humeral head from the image of the glenohumeral joint, leaving an en face view of the glenoid surface (Fig. 2) [23–25]. The isolated view of the glenoid surface gives a more precise image to accurately quantify the amount of glenoid bone loss and its location. Similarly, 3D CT allows for accurate quantification of humeral head bone loss with scapular subtraction [26]. While CT is generally considered to be superior to radiography for measuring glenoid bone loss, one study found no statistical difference in measurements taken from the radiographic Bernageau profile view and 3D CT in a small sample of patients with glenoid bone loss [27]. It is unknown if the Bernageau view can accurately distinguish between critical and subcritical bone loss, so 3D CT is still the gold standard for evaluating glenoid bone loss.
Fig. 2.
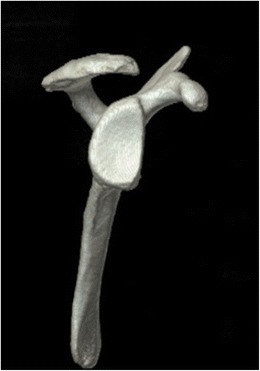
CT-generated scapula, en face view of glenoid
MRI is the gold standard imaging modality for assessing soft tissue shoulder pathology with the addition of contrast arthrography for further soft tissue assessment [28]. As a result, MRIs are frequently obtained for patients with shoulder instability; however, similar to 2D CT scans, quantification of glenoid bone loss can potentially be misleading. A recent cadaveric study comparing bone loss measurements revealed that 3D CT is more accurate than 2D CT, 2D MRI, and plain radiography for quantifying glenoid bone loss [25]. Recently, interest has developed in the use of three-dimensional magnetic resonance imaging (3D-MRI) for the assessment of glenoid bone loss as a potential alternative to 3D CT [28, 29•, 30•]. Gyftopoulos et al. performed a clinical study to evaluate the accuracy of 3D-MRI for measuring glenoid bone loss using arthroscopy as the gold standard. Glenoid bone loss was quantified using the best-fit circle method for 3D-MRI reconstructions and the bare spot method for intraoperative measurements. The findings show that 3D-MRI reconstructions may be used to accurately quantify glenoid bone loss [29•]. Stillwater et al. conducted a prospective study comparing the use of 3D-MRI to 3D-CT for the quantification of glenoid and/or humeral head bone loss in patients with glenohumeral instability [30•]. A total of 11 patients (mean age 29) with glenohumeral instability or recurrent shoulder dislocations were included in the study. Each patient underwent CT and MRI imaging of their shoulder (3-T MRI scanner and 64-multidetector row CT scanner). The images were post processed to create 3D reconstructions, and measurements were taken of the glenoid and humeral head. There was no statistically significant difference between measurements taken from the 3D-MRI or 3D-CT reconstructions, and percent bone loss was equivalent. Advantages of 3D-MRI include elimination of the radiation dose associated with a CT scan and the need for only one examination (Fig. 3) [30•].
Fig. 3.

3D-MRI of glenoid, en face view, demonstrating the best-fit circle method of quantifying glenoid bone loss. (Reproduced, with permission, from Gyftopoulos S, Beltran LS, et al. use of 3D MR reconstructions in the evaluation of glenoid bone loss: a clinical study. Skeletal Radiol. 2014 Feb;43(2):213–8)
Quantification of Glenoid Bone Loss
It is clear that 3D imaging is required to more accurately quantify bone loss, but the optimal method for doing so has not been identified [21•, 31]. There are multiple described methods for quantifying glenoid bone deficiency; however, there is no universally accepted method for measuring defects. The most accurate methods utilize a CT-generated en face view of the glenoid to make either linear or surface area measurements of the inferior glenoid. Commonly used linear and ratio measurements include the Glenoid Index method (Fig. 4a) and Gerber x-ratio, while the most common surface area measurement studied is the Pico method (Fig. 4b) [29•, 32–34]. A recent review of imaging methods for quantifying bone loss found the Glenoid Index and Pico methods to be the most accurate and reliable forms of measurement [21•]. Automated computer-generated calculation software is now being used at some centers. While this software provides an accurate measurement of bone loss, it is not widely available for use by most surgeons.
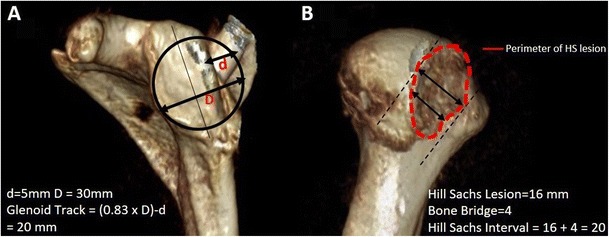
Fig. 4.
(a) Glenoid index method for quantifying glenoid bone deficiency, linear measurements. (b) PICO method for quantifying bone loss, surface area measurements
There is recent evidence suggesting that attritional loss of the bone fragment displaced from the glenoid may play an important role in management. McNeil et al. performed a study which analyzed the degree of attritional bone loss and found that duration of shoulder instability was significantly associated with percentage of attrition of the displaced fragment [35•]. It is important to consider the duration of symptoms during surgical planning, because small bony Bankart lesions when repaired may not reconstitute the glenoid.
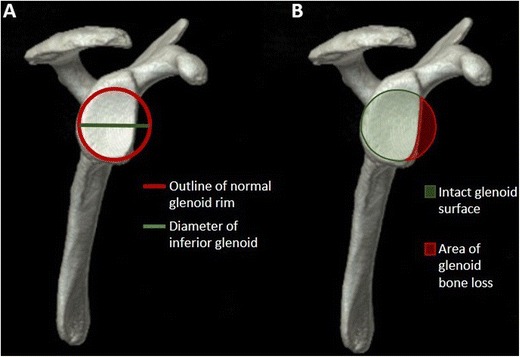
The glenoid track concept was developed to account for the dynamic relationship of glenoid and humeral bone defects in shoulder instability [36]. It is recognized that both humeral bone loss and glenoid bone loss must be accounted for when assessing shoulder instability, as increasing size of the Hill-Sachs lesion is an independent risk factor for recurrent instability and potentiates the severity of glenoid bone loss [16]. Di Giacomo et al. further defined calculation based on the degree of humeral and glenoid bone loss to determine whether the interaction is “on-track” or “off-track” [37•]. Independent 3D CT of the humeral head and scapula are required to perform the measurements and calculations if the width of the Hill-Sachs lesions matches that of the glenoid lesion then the Hill-Sachs glenoid loss combined lesion is considered “off-track” and warrants consideration for bony augmentation of the glenoid (Fig. 5). Shaha et al. evaluated patients undergoing arthroscopic Bankart reconstructions and found a significant increase in recurrent postoperative shoulder instability in “off-track” patients [38•].
Fig. 5.
(a) Glenoid track (GT) formula where D = diameter of the inferior glenoid and d = the width of the anterior glenoid bone loss. (b) Hill-Sachs interval (HSI) formula, the sum of the width of the HS lesion and the width of the bone bridge between the rotator cuff attachments and the lateral aspect of the HS lesion. If HSI > GT, the HS is off-track or engaging. If HSI < GT, the HS is on track, or non-engaging
Management
Non-operative
Non-surgical management for recurrent anterior shoulder instability in the setting of glenoid bone loss is not a recommended treatment option for young, active patients, as recurrent instability will result in further damage to the soft tissue or cartilage within the glenohumeral joint that may end up progressing to symptomatic glenohumeral arthritis. Treatment is limited to physiotherapy and is based on the important role that the periscapular and rotator cuff musculature plays in dynamic shoulder stabilization. This principle is used to create a protocol focused on strengthening these muscle groups. However, non-surgical management is limited to lower demand older patients with minor glenoid deficiencies [5].
Operative
There are several strategies for the surgical management of glenoid bone loss, including the Latarjet or coracoid transfer as well as other osseous and osteoarticular autografts and allografts (Fig. 6) [39•]. Common grafts used for reconstruction of glenoid bone deficiency include iliac crest and distal tibia [40•, 41]. All of the currently described techniques share the same goal: to restore the osseous defect in a manner that most closely resembles the native glenoid. Traditionally, bone loss of greater than 20–25% is considered a contraindication for soft tissue repairs alone due to the poor biomechanical environment and high clinical failure [7, 42].
Fig. 6.
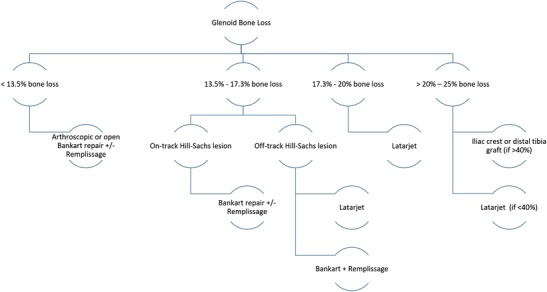
Flowchart demonstrating surgical treatment options based on percent of glenoid bone loss
Recent research has identified the concept of “subcritical” bone loss, in which a lower percentage of bone loss after arthroscopic Bankart repair does not necessarily result in a recurrence of dislocation events, but results in poorer patient reported clinical outcomes (WOSI scores) when comparing a soft tissue repair to those patients treated with bone augmentation [38•, 43•]. Shin et al. identified 17.3% glenoid bone loss as the critical value that leads to recurrent instability following arthroscopic Bankart repair. In their study, 43% of patients with greater than 17.3% bone loss had surgical failure, which was defined as need for revision surgery or subjective feelings of instability, compared to 3.7% of patients with less than 17.3% glenoid bone loss [44•]. This research suggests that, particularly for higher demand individuals, such as contact athletes, bone augmentation may result in better outcomes and lower failure rates for patients with this subcritical bone loss between 13.5 and 17.3%.
Some authors suggest that shoulder instability should be treated with a primary Latarjet procedure independent of glenoid bone loss [45•, 46•]. Conversely, however, DiGiacomo et al. showed a coracoid graft resorption of 39.6% at 1 year follow-up in patients with less than 15% glenoid bone loss [47•], which suggests that an unloaded graft will ultimately resorb according to Wolff’s law. The high rate of graft osteolysis may be a risk factor for recurrent instability and subsequent development of early glenohumeral arthritis [48].
Latarjet
The Latarjet procedure was originally described by Michael Latarjet in 1954 and later modified to the Latarjet-Bristow procedure by Arthur Helfet in 1958 [49, 50]. There are multiple described variations of the procedure, but the general technique involves transecting the coracoid at its base and transferring the graft intra-articular to the glenoid neck (Fig. 7) with one or two screw fixation. The pectoralis minor is detached from the coracoid, and a portion of the coracoacromial ligament is maintained for capsular repair.
Fig. 7.
General technique for Latarjet, graft of coracoid intra-articularly transferred to the glenoid neck
There are currently two commonly used techniques for a coracoid transfer: traditional Latarjet and congruent arc. The traditional Latarjet involves fixation of the inferior surface of the coracoid to the anterior surface of the glenoid [51•]. This technique provides a large surface area for fixation and bone healing, but leaves less anterior to posterior distance to fill the glenoid defect and restore glenoid width [51•]. The congruent arc technique involves fixation of the medial aspect of the coracoid to the glenoid and is accomplished by rotating the coracoid 90°. This creates a congruent surface between the inferior surface of the coracoid and the articular surface of the glenoid [52]. The congruent arc technique provides more anterior to posterior distance to restore glenoid width and can be used to fill larger glenoid defects [51•]. Furthermore, it more closely matches the radius of curvature of the native glenoid [39•]. However, this comes at the cost of less surface area for fixation between the glenoid and coracoid [51•, 53].
The Latarjet procedure remains the gold standard technique for addressing anterior glenoid bone loss, and its success is evidenced by its low long-term failure rate [54–56]. Several studies show excellent outcomes for both traditional and congruent arc techniques; however, there have been no clinical studies comparing the two methods [52, 54, 57•].
Cowling et al. recently published a systematic review of the described techniques and outcomes of the Latarjet procedure [58•]. In the review, the authors discuss variations for the coracoid osteotomy site, subscapularis approach, fixation site of the coracoid, orientation of the coracoid graft, and fixation method. There were several described methods for determining the osteotomy site, including 1–2 cm of coracoid length, junction between the horizontal and vertical parts of the coracoid, junction between the superior two-thirds and inferior one-third, immediately distal to the pectoralis minor or just anterior to the coracoclavicular ligaments, but rate of recurrent dislocation and nonunion did not differ. The subscapularis approach was mainly performed through a horizontal split in line with muscle fibers or a vertical tenotomy. Five of the seven studies performing a vertical tenotomy split only two-thirds of the tendon and reflected the upper half into an L-shape. Although a statistical analysis was not performed, the subscapularis split seems to preserve postoperative external rotation compared with a vertical tenotomy. The coracoid graft was most commonly placed flush with glenoid rim and less commonly placed medial to the glenoid rim. Unfortunately, a comparative analysis of recurrent dislocations based on fixation site could not be accurately completed due to biased study results. Only a few studies reported on graft position and orientation, making analysis difficult.
Iliac crest
Iliac crest autograft is usually reserved for patients with significant glenoid bone loss greater than 25 to 30%. Warner et al. described the technique in a case series of 11 patients in which a tri cortical iliac crest autograft is used to reconstruct large glenoid defects in patients with recurrent anterior shoulder instability. The authors use the inner table of the iliac due to its ability to closely match the concave articular surface of the glenoid. At a mean follow-up of 33 months, there were no episodes of recurrent instability, and at 4–6 months after surgery, there was no evidence of graft osteolysis [41]. Auffarth et al. described a variation of this procedure in which an autologous bicortical iliac crest graft is fashioned into a J-shape and secured to the glenoid in a press fit method with the keel of the graft impacted into a preformed crevice medial to the glenoid rim. In their series of 46 patients, there were no episodes of recurrent instability at a mean follow-up of 7.5 years [59]. The lack of hardware in the J-bone technique offers a theoretical benefit by eliminating the risk of prominent hardware and the need for additional surgery in the event of graft resorption.
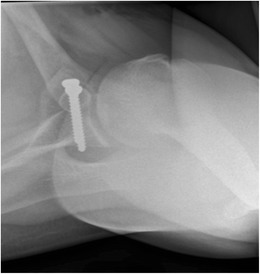
Distal Tibia Allograft
The use of a fresh osteochondral distal tibia allograft (DTA) is a relatively new approach for the reconstruction of anterior glenoid bone deficiency (Fig. 8). Provencher et al. originally described the technique in a small case series in which the lateral aspect of the distal tibia was used to reconstruct the glenoid in patients with greater than 30% glenoid bone loss [60]. The lateral aspect of the distal tibia is used, because its curvature is similar to the curvature of the native glenoid, thus providing a more anatomical reconstruction. Further, the graft contains a cartilaginous service with a radius of curvature that is highly congruent with the area of glenoid bone loss. The DTA can accommodate large glenoid defects that are unable to be reconstructed using the Latarjet technique. A recent case series of 27 patients who underwent reconstruction with a DTA for recurrent anterior shoulder instability in the setting of greater than 15% glenoid bone loss found significantly improved clinical outcome scores and no episodes of recurrent instability at an average follow-up of 45 months. There was an average allograft healing rate of 89% and average allograft osteolysis of 3% seen on CT scans 1.4 years post operatively. This early data is promising, although more studies and long-term data are needed.
Fig. 8.
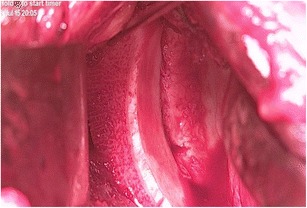
Intraoperative photograph of a distal tibia allograft secured to the glenoid rim
Distal Clavicle Autograft
The distal clavicle osteochondral autograft is a new arthroscopic technique for addressing glenohumeral instability secondary to glenoid bone loss. The technique was originally described by Tokish et al., and it is performed by harvesting the distal 6 to 8 mm of clavicle and securing it to the glenoid with suture anchors or a 3.75-mm cannulated screw [61•]. The graft provides an articular surface that is congruent with the glenoid, and it has a large surface area for fixation and bony union [61•]. In a biomechanical study evaluating glenohumeral contact area and pressures, an articular-sided distal clavicle bone graft and a coracoid bone graft were comparable when used for restoration of an anterior glenoid bone defect [62•]. Tokish et al. reported positive early outcomes for a small sample of patients in their initial pilot study, but clinical studies are needed to evaluate the effectiveness and safety of this new technique for the management of recurrent shoulder instability due to glenoid bone loss [61•].
Future Directions
Determining the optimal treatment for so-called “subcritical” bone loss (13.5% or more) remains an unanswered question as balancing recurrent instability risk with graft osteolysis is important. Additional research to identify the optimal technique for graft fixation is necessary as multiple screw types and materials exist. It is unknown if osteolyisis is related to graft fixation strength.
Growing interest and research in the management of glenoid bone loss has led to the development of new surgical techniques and graft options. The arthroscopic Latarjet procedure was first reported in the literature 10 years ago [63]. Athwal et al. found a 24% adverse event rate in their recently published study on short-term complications of the arthroscopic Latarjet procedure [64•], which is similar to the short-term adverse event rate found by Shah et al. in their series of open Latarjet procedures [65]. Nourissat et al. performed a recently published prospective study comparing open Latarjet procedures to arthroscopic Latarjet procedures and found a reduction in immediate postoperative pain scores in the arthroscopic group, but no difference in pain or function at 1 year [66•]. There is a lack of prospective studies or long-term follow-up in the current literature to adequately assess the efficacy of arthroscopic Latarjet procedures compared to the traditional open techniques.
Conclusions
Glenoid bone loss is well established in the literature as an important cause of recurrent anterior shoulder instability. Advanced imaging technology has led to improved methods for diagnosing and accurately quantifying glenoid bone loss for surgical planning. Surgical management has evolved from the historical Latarjet procedure to new techniques and graft options that may better anatomically match the native glenoid and reduce the risk of recurrent instability and early glenohumeral arthritis. While the Latarjet procedure remains the gold standard, a growing body of literature provides good evidence for the use of new techniques. In the subset of patients with failed Latarjet or large amount of bone loss, either the classic iliac crest bone grafting or distal tibia allograft can be used as reconstruction options. Despite the significant graft resorption rates seen with the Latarjet procedure and bone grafting, functional outcome and recurrence rate is good to excellent in majority of patients after glenoid bone grafting. Continued research is required to identify a universally accepted method for quantifying glenoid bone loss, and to identify surgical techniques and grafts that best reconstruct the glenoid rim.
Compliance with Ethical Standards
Conflict of Interest
All authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Management of Anterior Shoulder Instability
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Lynch JR, Clinton JM, Dewing CB, Warme WJ, Matsen FA., 3rd Treatment of osseous defects associated with anterior shoulder instability. J Shoulder Elbow Surg. 2009;18(2):317–328. doi: 10.1016/j.jse.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 2.Provencher MT, Bhatia S, Ghodadra NS, Grumet RC, Bach BR, Jr, Dewing CB, et al. Recurrent shoulder instability: current concepts for evaluation and management of glenoid bone loss. J Bone Joint Surg Am. 2010;92(Suppl 2):133–151. doi: 10.2106/JBJS.J.00906. [DOI] [PubMed] [Google Scholar]
- 3.Edwards TB, Boulahia A, Walch G. Radiographic analysis of bone defects in chronic anterior shoulder instability. Arthroscopy. 2003;19(7):732–739. doi: 10.1016/S0749-8063(03)00684-4. [DOI] [PubMed] [Google Scholar]
- 4.Taylor DC, Arciero RA. Pathologic changes associated with shoulder dislocations: arthroscopic and physical examination findings in first-time, traumatic anterior dislocations. Am J Sports Med. 1997;25(3):306–311. doi: 10.1177/036354659702500306. [DOI] [PubMed] [Google Scholar]
- 5.Piasecki DP, Verma NN, Romeo AA, Levine WN, Bach BR, Jr, Provencher MT. Glenoid bone deficiency in recurrent anterior shoulder instability: diagnosis and management. J Am Acad Orthop Surg. 2009;17(8):482–493. doi: 10.5435/00124635-200908000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Bigliani LU, Newton PM, Steinmann SP, Connor PM, McLlveen SJ. Glenoid rim lesions associated with recurrent anterior dislocation of the shoulder. Am J Sports Med. 1998;26(1):41–45. doi: 10.1177/03635465980260012301. [DOI] [PubMed] [Google Scholar]
- 7.Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16(7):677–694. doi: 10.1053/jars.2000.17715. [DOI] [PubMed] [Google Scholar]
- 8.Mologne TS, Provencher MT, Menzel KA, Vachon TA, Dewing CB. Arthroscopic stabilization in patients with an inverted pear glenoid: results in patients with bone loss of the anterior glenoid. Am J Sports Med. 2007;35(8):1276–1283. doi: 10.1177/0363546507300262. [DOI] [PubMed] [Google Scholar]
- 9.Sugaya H, Moriishi J, Dohi M, Kon Y, Tsuchiya A. Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Joint Surg Am. 2003;85-A(5):878–884. doi: 10.2106/00004623-200305000-00016. [DOI] [PubMed] [Google Scholar]
- 10.Visser CP, Coene LN, Brand R, Tavy DL. The incidence of nerve injury in anterior dislocation of the shoulder and its influence on functional recovery. A prospective clinical and EMG study. J Bone Joint Surg Br Vol. 1999;81(4):679–685. doi: 10.1302/0301-620X.81B4.9005. [DOI] [PubMed] [Google Scholar]
- 11.de Laat EA, Visser CP, Coene LN, Pahlplatz PV, Tavy DL. Nerve lesions in primary shoulder dislocations and humeral neck fractures. A prospective clinical and EMG study. J Bone Joint Surg British Vol. 1994;76(3):381–383. [PubMed] [Google Scholar]
- 12.Robinson CM, Shur N, Sharpe T, Ray A, Murray IR. Injuries associated with traumatic anterior glenohumeral dislocations. J Bone Joint Surg Am. 2012;94(1):18–26. doi: 10.2106/JBJS.J.01795. [DOI] [PubMed] [Google Scholar]
- 13.Galvin JW, Eichinger JK. Outcomes following closed axillary nerve injury: a case report and review of the literature. Mil Med. 2016;181(3):e291–e297. doi: 10.7205/MILMED-D-15-00205. [DOI] [PubMed] [Google Scholar]
- 14.Lazarus MD, Sidles JA, Harryman DT, 2nd, Matsen FA., 3rd Effect of a chondral-labral defect on glenoid concavity and glenohumeral stability. A cadaveric model. J Bone Joint Surg Am. 1996;78(1):94–102. doi: 10.2106/00004623-199601000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Howell SM, Galinat BJ. The glenoid-labral socket. A constrained articular surface. Clin Orthop Relat Res. 1989;243:122–125. [PubMed] [Google Scholar]
- 16.Balg F, Boileau P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br Vol. 2007;89(11):1470–1477. doi: 10.1302/0301-620X.89B11.18962. [DOI] [PubMed] [Google Scholar]
- 17.Garth WP, Jr, Slappey CE, Ochs CW. Roentgenographic demonstration of instability of the shoulder: the apical oblique projection. A technical note. J Bone Joint Surg Am. 1984;66(9):1450–1453. doi: 10.2106/00004623-198466090-00020. [DOI] [PubMed] [Google Scholar]
- 18.Pansard E, Klouche S, Billot N, Rousselin B, Kraus TM, Bauer T, et al. Reliability and validity assessment of a glenoid bone loss measurement using the Bernageau profile view in chronic anterior shoulder instability. J Shoulder Elb Surg. 2013;22(9):1193–1198. doi: 10.1016/j.jse.2012.12.032. [DOI] [PubMed] [Google Scholar]
- 19.Pavlov H, Warren RF, Weiss CB, Jr, Dines DM. The roentgenographic evaluation of anterior shoulder instability. Clin Orthop Relat Res. 1985;194:153–158. [PubMed] [Google Scholar]
- 20.Rokous JR, Feagin JA, Abbott HG. Modified axillary roentgenogram. A useful adjunct in the diagnosis of recurrent instability of the shoulder. Clin Orthop Relat Res. 1972;82:84–86. doi: 10.1097/00003086-197201000-00012. [DOI] [PubMed] [Google Scholar]
- 21.Saliken DJ, Bornes TD, Bouliane MJ, Sheps DM, Beaupre LA. Imaging methods for quantifying glenoid and Hill-Sachs bone loss in traumatic instability of the shoulder: a scoping review. BMC Musculoskelet Disord. 2015;16:164. doi: 10.1186/s12891-015-0607-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gross DJ, Golijanin P, Dumont GD, Parada SA, Vopat BG, Reinert SE, et al. The effect of sagittal rotation of the glenoid on axial glenoid width and glenoid version in computed tomography scan imaging. J Shoulder Elb Surg. 2016;25(1):61–68. doi: 10.1016/j.jse.2015.06.017. [DOI] [PubMed] [Google Scholar]
- 23.Kwon YW, Powell Ka Fau-Yum JK, Yum Jk Fau-Brems JJ, Brems Jj Fau-Iannotti JP, Iannotti JP. Use of three-dimensional computed tomography for the analysis of the glenoid anatomy. J Shoulder Elb Surg. 2005;14(1):85–90. doi: 10.1016/j.jse.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 24.Bishop JY, Jones Gl Fau-Rerko MA, Rerko Ma Fau-Donaldson C, Donaldson C. 3-D CT is the most reliable imaging modality when quantifying glenoid bone loss. Clin Orthop Relat Res. 2013;471(4):1251–1256. doi: 10.1007/s11999-012-2607-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rerko MA, Pan X, Fau-Donaldson C, Fau-Jones GL, Bishop JY. Comparison of various imaging techniques to quantify glenoid bone loss in shoulder instability. J Shoulder Elb Surg. 2013;22(4):528–534. doi: 10.1016/j.jse.2012.05.034. [DOI] [PubMed] [Google Scholar]
- 26.Cho SH, Cho NS, Rhee YG. Preoperative analysis of the Hill-Sachs lesion in anterior shoulder instability: how to predict engagement of the lesion. Am J Sports Med. 2011;39(11):2389–2395. doi: 10.1177/0363546511398644. [DOI] [PubMed] [Google Scholar]
- 27.Murachovsky J, Bueno RS, Nascimento LG, Almeida LH, Strose E, Castiglia MT, et al. Calculating anterior glenoid bone loss using the Bernageau profile view. Skelet Radiol. 2012;41(10):1231–1237. doi: 10.1007/s00256-012-1439-9. [DOI] [PubMed] [Google Scholar]
- 28.Gyftopoulos S, Yemin A, Mulholland T, Bloom M, Storey P, Geppert C, et al. 3DMR osseous reconstructions of the shoulder using a gradient-echo based two-point Dixon reconstruction: a feasibility study. Skelet Radiol. 2013;42(3):347–352. doi: 10.1007/s00256-012-1489-z. [DOI] [PubMed] [Google Scholar]
- 29.Gyftopoulos S, Beltran LS, Yemin A, Strauss E, Meislin R, Jazrawi L, et al. Use of 3D MR reconstructions in the evaluation of glenoid bone loss: a clinical study. Skelet Radiol. 2014;43(2):213–218. doi: 10.1007/s00256-013-1774-5. [DOI] [PubMed] [Google Scholar]
- 30.Stillwater L, Koenig J, Maycher B, Davidson M. 3D-MR vs. 3D-CT of the shoulder in patients with glenohumeral instability. Skelet Radiol. 2017;46(3):325–331. doi: 10.1007/s00256-016-2559-4. [DOI] [PubMed] [Google Scholar]
- 31.Bois AJ, Fening SD, Polster J, Jones MH, Miniaci A. Quantifying glenoid bone loss in anterior shoulder instability: reliability and accuracy of 2-dimensional and 3-dimensional computed tomography measurement techniques. Am J Sports Med. 2012;40(11):2569–2577. doi: 10.1177/0363546512458247. [DOI] [PubMed] [Google Scholar]
- 32.Baudi P, Campochiaro G, Rebuzzi M, Matino G, Catani F. Assessment of bone defects in anterior shoulder instability. Joints. 2013;1(1):40–48. [PMC free article] [PubMed] [Google Scholar]
- 33.Chuang TY, Adams CR, Burkhart SS. Use of preoperative three-dimensional computed tomography to quantify glenoid bone loss in shoulder instability. Arthroscopy. 2008;24(4):376–382. doi: 10.1016/j.arthro.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 34.Gerber C, Nyffeler RW. Classification of glenohumeral joint instability. Clin Orthop Relat Res. 2002;400:65–76. doi: 10.1097/00003086-200207000-00009. [DOI] [PubMed] [Google Scholar]
- 35.• JW MN, Beaulieu-Jones BR, Bernhardson AS, LE LC, Dewing CB, Lynch JR, et al. Classification and analysis of attritional glenoid bone loss in recurrent anterior shoulder instability. Am J Sports Med. 2016; 10.1177/0363546516677736. This retrospective review included 265 patients and measured glenoid bone loss using 3D CT reconstructions of the shoulder. In addition, they measured attritional bone loss of the displaced bone fragment. Total time of instability prior to the CT scan was significantly associated with the degree of attritional bone loss of the displaced fragment. Therefore, in patient with a long history of instability the remaining bone fragment may not be able to fully reconstruct the glenoid.
- 36.Yamamoto N, Itoi E, Abe H, Minagawa H, Seki N, Shimada Y, et al. Contact between the glenoid and the humeral head in abduction, external rotation, and horizontal extension: a new concept of glenoid track. J Shoulder Elb Surg. 2007;16(5):649–656. doi: 10.1016/j.jse.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 37.Di Giacomo G, Itoi E, Burkhart SS. Evolving concept of bipolar bone loss and the Hill-Sachs lesion: from “engaging/non-engaging” lesion to “on-track/off-track” lesion. Arthroscopy. 2014;30(1):90–98. doi: 10.1016/j.arthro.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 38.Shaha JS, Cook JB, Rowles DJ, Bottoni CR, Shaha SH, Tokish JM. Clinical validation of the glenoid track concept in anterior glenohumeral instability. J Bone Joint Surg Am. 2016;98(22):1918–1923. doi: 10.2106/JBJS.15.01099. [DOI] [PubMed] [Google Scholar]
- 39.Noonan B, Hollister SJ, Sekiya JK, Bedi A. Comparison of reconstructive procedures for glenoid bone loss associated with recurrent anterior shoulder instability. J Shoulder Elb Surg. 2014;23(8):1113–1119. doi: 10.1016/j.jse.2013.11.011. [DOI] [PubMed] [Google Scholar]
- 40.• Provencher MT, Frank RM, Golijanin P, Gross D, Cole BJ, Verma NN, et al. Distal tibia allograft glenoid reconstruction in recurrent anterior shoulder instability: clinical and radiographic outcomes. Arthroscopy. 2016; 10.1016/j.arthro.2016.09.029. This is a retrospective review that evaluated post-operative clinical and radiographic outcomes at a minimum of two years in 27 patients who were treated with a fresh distal tibia allograft (DTA). Inclusion criteria included recurrent anterior shoulder instability and a minimum of 15% glenoid bone loss. There were significant improvements in post-operative clinical outcome measures, no episodes of recurrent instability, and an allograft healing rate of 89% with average lysis of 3%.
- 41.Warner JJ, Gill TJ, O'Hollerhan JD, Pathare N, Millett PJ. Anatomical glenoid reconstruction for recurrent anterior glenohumeral instability with glenoid deficiency using an autogenous tricortical iliac crest bone graft. Am J Sports Med. 2006;34(2):205–212. doi: 10.1177/0363546505281798. [DOI] [PubMed] [Google Scholar]
- 42.Itoi E, Lee SB, Berglund LJ, Berge LL, An KN. The effect of a glenoid defect on anteroinferior stability of the shoulder after bankart repair: a cadaveric study. J Bone Joint Surg Am. 2000;82:35–46. doi: 10.2106/00004623-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 43.Shaha JS, Cook JB, Song DJ, Rowles DJ, Bottoni CR, Shaha SH, et al. Redefining “critical” bone loss in shoulder instability: functional outcomes worsen with “subcritical” bone loss. Am J Sports Med. 2015;43(7):1719–1725. doi: 10.1177/0363546515578250. [DOI] [PubMed] [Google Scholar]
- 44.Shin SJ, Kim RG, Jeon YS, Kwon TH. Critical value of anterior glenoid bone loss that leads to recurrent glenohumeral instability after arthroscopic bankart repair. Am J Sports Med. 2017;45(9):1975–1981. doi: 10.1177/0363546517697963. [DOI] [PubMed] [Google Scholar]
- 45.Blonna D, Bellato E, Caranzano F, Assom M, Rossi R, Castoldi F. Arthroscopic Bankart repair versus open Bristow-Latarjet for shoulder instability. Am J Sports Med. 2016;44(12):3198–3205. doi: 10.1177/0363546516658037. [DOI] [PubMed] [Google Scholar]
- 46.Zimmermann SM, Scheyerer MJ, Farshad M, Catanzaro S, Rahm S, Gerber C. Long-term restoration of anterior shoulder stability: a retrospective analysis of arthroscopic Bankart repair versus open latarjet procedure. JBJS. 2016;98(23):1954–1961. doi: 10.2106/JBJS.15.01398. [DOI] [PubMed] [Google Scholar]
- 47.Di Giacomo G, de Gasperis N, Costantini A, De Vita A, Beccaglia MA, Pouliart N. Does the presence of glenoid bone loss influence coracoid bone graft osteolysis after the Latarjet procedure? A computed tomography scan study in 2 groups of patients with and without glenoid bone loss. J Shoulder Elb Surg. 2014;23(4):514–518. doi: 10.1016/j.jse.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 48.Di Giacomo G, Costantini A, de Gasperis N, De Vita A, Lin BK, Francone M, et al. Coracoid graft osteolysis after the Latarjet procedure for anteroinferior shoulder instability: a computed tomography scan study of twenty-six patients. J Shoulder Elb Surg. 2011;20(6):989–995. doi: 10.1016/j.jse.2010.11.016. [DOI] [PubMed] [Google Scholar]
- 49.Latarjet M. Treatment of recurrent dislocation of the shoulder. Lyon Chir. 1954;49(8):994–997. [PubMed] [Google Scholar]
- 50.Helfet AJ. Coracoid transplantation for recurring dislocation of the shoulder. J Bone Joint Surg Br Vol. 1958;40-B(2):198–202. doi: 10.1302/0301-620X.40B2.198. [DOI] [PubMed] [Google Scholar]
- 51.Montgomery SR, Katthagen JC, Mikula JD, Marchetti DC, Tahal DS, Dornan GJ, et al. Anatomic and biomechanical comparison of the classic and congruent-arc techniques of the Latarjet procedure. Am J Sports Med. 2017;45(6):1252–1260. doi: 10.1177/0363546516685318. [DOI] [PubMed] [Google Scholar]
- 52.de Beer JF, Roberts C. Glenoid bone defects--open latarjet with congruent arc modification. Orthop Clin N Am. 2010;41(3):407–415. doi: 10.1016/j.ocl.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 53.Giles JW, Puskas G, Welsh M, Johnson JA, Athwal GS. Do the traditional and modified Latarjet techniques produce equivalent reconstruction stability and strength? Am J Sports Med. 2012;40(12):2801–2807. doi: 10.1177/0363546512460835. [DOI] [PubMed] [Google Scholar]
- 54.Burkhart SS, De Beer JF, Barth JR, Cresswell T, Roberts C, Richards DP. Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy. 2007;23(10):1033–1041. doi: 10.1016/j.arthro.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 55.Hovelius L, Sandstrom B, Sundgren K, Saebo M. One hundred eighteen Bristow-Latarjet repairs for recurrent anterior dislocation of the shoulder prospectively followed for fifteen years: study I—clinical results. J Shoulder Elb Surg. 2004;13(5):509–516. doi: 10.1016/j.jse.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 56.Matton D, Van Looy F, Geens S. Recurrent anterior dislocations of the shoulder joint treated by the Bristow-Latarjet procedure. Historical review, operative technique and results. Acta Orthop Belg. 1992;58(1):16–22. [PubMed] [Google Scholar]
- 57.Mook WR, Petri M, Greenspoon JA, Horan MP, Dornan GJ, Millett PJ. Clinical and anatomic predictors of outcomes after the latarjet procedure for the treatment of anterior glenohumeral instability with combined glenoid and humeral bone defects. Am J Sports Med. 2016;44(6):1407–1416. doi: 10.1177/0363546516634089. [DOI] [PubMed] [Google Scholar]
- 58.Cowling PD, Akhtar MA, Liow RY. What is a Bristow-Latarjet procedure? A review of the described operative techniques and outcomes. Bone Joint J. 2016;98-B(9):1208–1214. doi: 10.1302/0301-620X.98B9.37948. [DOI] [PubMed] [Google Scholar]
- 59.Auffarth A, Schauer J, Matis N, Kofler B, Hitzl W, Resch H. The J-bone graft for anatomical glenoid reconstruction in recurrent posttraumatic anterior shoulder dislocation. Am J Sports Med. 2008;36(4):638–647. doi: 10.1177/0363546507309672. [DOI] [PubMed] [Google Scholar]
- 60.Provencher MT, Ghodadra N, LeClere L, Solomon DJ, Romeo AA. Anatomic osteochondral glenoid reconstruction for recurrent glenohumeral instability with glenoid deficiency using a distal tibia allograft. Arthroscopy. 2009;25(4):446–452. doi: 10.1016/j.arthro.2008.10.017. [DOI] [PubMed] [Google Scholar]
- 61.Tokish JM, Fitzpatrick K, Cook JB, Mallon WJ. Arthroscopic distal clavicular autograft for treating shoulder instability with glenoid bone loss. Arthrosc Tech. 2014;3(4):e475–e481. doi: 10.1016/j.eats.2014.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Petersen SA, Bernard JA, Langdale ER, Belkoff SM. Autologous distal clavicle versus autologous coracoid bone grafts for restoration of anterior-inferior glenoid bone loss: a biomechanical comparison. J Shoulder Elb Surg. 2016;25(6):960–966. doi: 10.1016/j.jse.2015.10.023. [DOI] [PubMed] [Google Scholar]
- 63.Lafosse L, Lejeune E, Bouchard A, Kakuda C, Gobezie R, Kochhar T. The arthroscopic Latarjet procedure for the treatment of anterior shoulder instability. Arthroscopy. 2007;23(11):1242 e1–1242 e5. doi: 10.1016/j.arthro.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 64.Athwal GS, Meislin R, Getz C, Weinstein D, Favorito P. Short-term complications of the arthroscopic Latarjet procedure: a North American experience. Arthroscopy. 2016;32(10):1965–1970. doi: 10.1016/j.arthro.2016.02.022. [DOI] [PubMed] [Google Scholar]
- 65.Shah AA, Butler RB, Romanowski J, Goel D, Karadagli D, Warner JJ. Short-term complications of the Latarjet procedure. J Bone Joint Surg Am. 2012;94(6):495–501. doi: 10.2106/JBJS.J.01830. [DOI] [PubMed] [Google Scholar]
- 66.Nourissat G, Neyton L, Metais P, Clavert P, Villain B, Haeni D, et al. Functional outcomes after open versus arthroscopic Latarjet procedure: a prospective comparative study. Orthop Traumatol Surg Res. 2016;102(8S):S277–S2S9. doi: 10.1016/j.otsr.2016.08.004. [DOI] [PubMed] [Google Scholar]


