Highlights
-
•
Vaginal cuff dehiscence (VCD) and evisceration (VCDE) is a rare but rather serious complication of any type of hysterectomy.
-
•
The overall incidence was ranged betwenn 0% and 7,5%.
-
•
Historically, laparotomy was recommended for VCD repair.
-
•
In our case we choosed to add a Polyglactine mesh and in the limit of our review it’s the only case reported.
Keywords: Vaginal dehiscence, Evisceration, Hysterectomy, Surgery
Abstract
Introduction
Vaginal cuff dehiscence (VCD) and evisceration (VCDE) are rare but rather serious complications of hysterectomy procedures.
We aimed to report a case of VCDE happening eleven years after the initial surgery and review a treatment protocol of this rare complication.
Case
A 68 years old Tunisian female patient
In 2004, the patient underwent concomitant chemoradiation followed by total abdominal radical hysterectomy for a squamous cell carcinoma of the cervix.
Eleven years later, after an abdominal thrust due to a strong cough the patient had a protrusion of the two small bowels.
Patient was surgically treated following a combined approach.
The follow-up did not show any sign of relapse.
Conclusion
VCDE is a rare complication of hysterectomy that carries a lot of mobimortality if not treated on time.
Surgery without delay is usually a guarantee for a god outcome.
1. Introduction
Vaginal cuff dehiscence (VCD) and evisceration (VCDE) are rare but rather serious complication of any type of hysterectomy.
It’s defined by partial or total separation of the vaginal cuff with the protrusion of intraabdominal content usually the small bowel [1].
Prolapse of the omentum, appendix and fallopian tubes have also been reported [2].
When it occurs, prompt surgical and medical intervention is required to ensure optimal care due to their high morbidity [3], [4].
Throughout this study, we are reporting a case of VCDE which happened eleven years after the initial surgery. We are also reviewing the steps followed to manage this rare complication.
This work have been reported in line with the SCARE criteria [5].
2. Case presentation
A 68 years old Tunisian female patient treated for high blood pressure.
In 2004, the patient underwent concomitant chemoradiation followed by total abdominal radical hysterectomy for a squamous cell carcinoma of the cervix.
After four years,the patient underwent midline scar eventration repair using a polypropylene mesh.
No recurrence was observed during the follow-up.
Eleven years post-surgery,the patient was interned in our department for an abdominal thrust due to a strong cough the patient had a protrusion of two the small bowel.
During the physical examination, two protruding ileal segments with good vitality were found (Picture 1).
Picture 1.
Vaginal evisceration of ileum segment.
The manual reduction was not attempted since the full examination of the protruding ileum was not possible and because of the absence of bowel movements.
An abdominal X ray was made and showed several centrally located dilated gas loops filled bowel (Picture 2).
Picture 2.
Abdominal X ray showing dilated Gas filled bowel.
and the patient was made nil per os and immediately taken to the operating room with the bowel wrapped in a moist towel.
First we started with a midline incision, after the adhesiolysis no sign of recurrence were found. We found a 3 cm dehiscence of the vaginal cuff with the protrusion of two ileal segments.
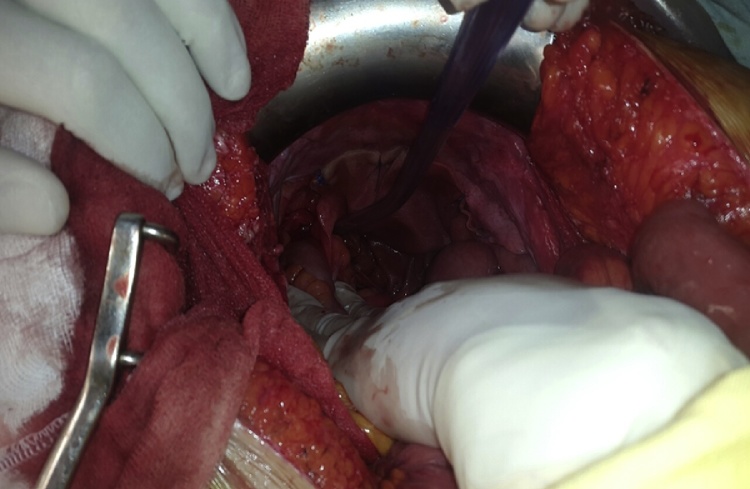
We cautiously reduced the protrusing ileum reduced using a combined vaginal and abdominal approach. (Picture 3, Picture 4)
Picture 3.
Cautious reduction of the ileum with an atraumatic forceps.
Picture 4.
Perineal view after Reduction.
During the examination, we found a healthy ileum with no need for small bowel resection.
We closed the vagina with resorbable polyglactine 910 stitures. A polyglactine mesh was fixed above the vaginal cuff. (Picture 4, Picture 5)
Picture 5.
Polyglactine mesh fixation over the vaginal cuff.
the patient was normal during the post-surgery follow up.
She recovered her bowel motility after 24 h, and she was discharged after 5 days with no need to major analgesic during her stay.
She was last seen three years post- surgery with no sign of recurrence.
3. Discussion
VCDE post hysterectomy is a rare but severe complication that can, if not rapidly treated, lead to significant morbi-mortality [4].
In Hur et al. [3], 2016 review of the literature, the overall incidence was ranged betwenn 0% and 7,5% the same numbers were also found in 2008 by Denardis et al. [6].
Hur et al. [3] also looked for the incidence of dehiscence by mode of hysterectomy showing that robotic hysterectomy was carrying the greatest incidence with 2,33% compared to total laparoscopic hysterectomy (0,87%), abdominal hysterectomy (0,28%) and vaginal hysterectomy (0,15%).
In De Iaco et al. [7] review of 3593 hysterectomies, the incidence of VCDE was of 0,28% and no statistical differences between the different mode of hysterectomies were observed.
The majority of VCDE patients present symptoms of pain (58–100%), bleeding (23.5–90%), and/or vaginal discharge (55.6%) [8]. Patients may also present signs of peritonitis [3].
In some rare cases, patients were asymptomatic [3], [8].
The initial management should be prompt. A radiologic examination by a abdominopelvic computed tomography should be done if intraperitoneal process is suspected [1] but should not delay surgery [3]. When associated to evisceration, a surgical care is mandatory in order to save the protruded bowel.
Historically, laparotomy was recommended for VCD management [3].
In the last ten years, however, the trends have changed towards less invasive methods and the majority of the reported cases in the literature have been treated without laparotomies [1], [9], [10].
Hur et al. [3] stated that in the absence of consensus around the optimal way of repair, both patient’s health and the surgeons’ skills should be assessed to determine the best treatment strategy.
The way to reclose the vagina varies between authors, some uses vaginal repair, others prefers an abdominal approach [3].
There are different ways to close the vagina where some surgeons prefer to use continuous suture and others separated ones.
Narducci et al. [11], proposed to reinforce the vaginal cuff using a peritoneal graft.
Based on this idea of reinforcing the vaginal cuff we decided to use a polyglactin mesh.
This technique have been reported in two other case reports for women with relapsing VCDE showing good result [12], [13].
Jurus et al. concluded his work stating that The use of synthetic mesh to reinforce the vaginal apex along with an abdominal sacrocolpopexy may eliminate the chance of recurrent bowel evisceration in select cases [13].
Preventive measures were described in the literature in order to avoid VCD.
Soper et al. [12], found that treating of bacterial vaginosis and trichomonas vaginitis associated with antibiotic prophylaxis was associated with less VCD due to the reduction of vaginal cuff cellulites.
According to Hur et al. [3], doses should be increased for over weighted patients and in cases of blood loss.
Factors that should be assessed preoperatively in order to avoid VCDE are smoking cessation, anemia, diabetes and poor nutritional status [3].
Some authors found that the use of local estrogen in postmenopausal women can increase vaginal thickness [13].
Intraoperatively, some authors advised the use of cold energy rather than electrosurgery while doing the colpectomy to minimize tissue necrosis [12].
In the postoperative setting, Hur et al. [3], recommend pelvic rest for a six to eight weeks and that sexual intercourse should be resumed after the assessment of cuff integrity.
They also recommend to avoid situations that induce intraabdominal pressure.
4. Conclusion
Despite being rare, VCDE can carry a lot of morbimortality if not treated on time.
In the presence of evisceration, surgery should not be delayed to avoid harming the bowel and further morbidity.
The abdominal route is historically the preferred way although it could be managed by a vaginal approach. The route to treat the VCDE should be decided depending on patient health status and surgeon skills.
Some preventing measure can be taken but none of them have shown to be 100% efficient.
Conflicts of interest
NO financial and personal relationships with other people or organisations that could inappropriately influence (bias) their work.
Funding
No source of funding.
Ethical approval
Charles nicolle hospital ethic comitee.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Authors’ contribution
Bensafta y; concept or design, data collection, data analysis or interpretation, writing the pape.
Ghalleb M; concept or design, data collection, data analysis or interpretation, writing the paper.
Baccari Aymen; data collection, data analysis or interpretation.
Hamdi el kebir G; data collection.
Daldoul S; data collection, data analysis or interpretation, writing the paper.
SAyari S; writing the paper.
BEN Moussa M writing the paper.
Guarantor
Yacine Ben Safta.
Acknowledgement
We want to acknowledge the archive department of Charles Nicolle hospital for their help.
Contributor Information
Yacine Ben Safta, Email: bsyacine@gmail.com.
Montassar Ghalleb, Email: montaghalleb@gmail.com.
Aymen Baccari, Email: Baccariaymen85@gmail.com.
Ghassen Hamdi El kebir, Email: hamdikbir@gmail.com.
Sami Daldoul, Email: samidaldoul@yahoo.fr.
Sofiene Sayari, Email: sayari_sofiene@yahoo.fr.
Mounir Ben Moussa, Email: mounirbm1966@gmail.com.
References
- 1.Matthews C.A., Kenton K. Treatment of vaginal cuff evisceration. Obstet. Gynecol. 2014;124(October (4)):705–708. doi: 10.1097/AOG.0000000000000463. [DOI] [PubMed] [Google Scholar]
- 2.Ceccaroni M., Berretta R., Malzoni M., Scioscia M., Roviglione G., Spagnolo E. Vaginal cuff dehiscence after hysterectomy: a multicenter retrospective study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2011;158(October (2)):308–313. doi: 10.1016/j.ejogrb.2011.05.013. [DOI] [PubMed] [Google Scholar]
- 3.Hur H.-C., Lightfoot M., McMillin M.G., Kho K.A. Vaginal cuff dehiscence and evisceration: a review of the literature. Curr. Opin. Obstet. Gynecol. 2016;28(August (4)):297–303. doi: 10.1097/GCO.0000000000000294. [DOI] [PubMed] [Google Scholar]
- 4.Kim M.J., Kim S., Bae H.S., Lee J.K., Lee N.W., Song J.Y. Evaluation of risk factors of vaginal cuff dehiscence after hysterectomy. Obstet. Gynecol. Sci. 2014;57(2):136. doi: 10.5468/ogs.2014.57.2.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., the SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 6.DeNardis S.A., Holloway R.W., Bigsby G.E., Pikaart D.P., Ahmad S., Finkler N.J. Robotically assisted laparoscopic hysterectomy versus total abdominal hysterectomy and lymphadenectomy for endometrial cancer. Gynecol. Oncol. 2008;111(December (3)):412–417. doi: 10.1016/j.ygyno.2008.08.025. [DOI] [PubMed] [Google Scholar]
- 7.Iaco P.D., Ceccaroni M., Alboni C., Roset B., Sansovini M., D’Alessandro L. Transvaginal evisceration after hysterectomy: is vaginal cuff closure associated with a reduced risk? Eur. J. Obstet. Gynecol. Reprod. Biol. 2006;125(March (1)):134–138. doi: 10.1016/j.ejogrb.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 8.Cronin B., Sung V.W., Matteson K.A. Vaginal cuff dehiscence: risk factors and management. Am. J. Obstet. Gynecol. 2012;206:284–288. doi: 10.1016/j.ajog.2011.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Uccella S., Ghezzi F., Mariani A., Cromi A., Bogani G., Serati M. Vaginal cuff closure after minimally invasive hysterectomy: our experience and systematic review of the literature. Am. J. Obstet. Gynecol. 2011;205(August (2)) doi: 10.1016/j.ajog.2011.03.024. 119. e1-119. e12. [DOI] [PubMed] [Google Scholar]
- 10.Uccella S., Ceccaroni M., Cromi A., Malzoni M., Berretta R., De Iaco P. Vaginal cuff dehiscence in a series of 12,398 hysterectomies: effect of different types of colpotomy and vaginal closure. Obstet. Gynecol. 2012;120(September (3)):516–523. doi: 10.1097/AOG.0b013e318264f848. [DOI] [PubMed] [Google Scholar]
- 11.Narducci F., Sonoda Y., Lambaudie E., Leblanc E., Querleu D. Vaginal evisceration after hysterectomy: the repair by a laparoscopic and vaginal approach with a omental flap. Gynecol. Oncol. 2003;89(June (3)):549–551. doi: 10.1016/s0090-8258(03)00153-7. [DOI] [PubMed] [Google Scholar]
- 12.Soper D.E., Bump R.C., Glenn Hurt W.G. Bacterial vaginosis and trichomoniasis vaginitis are risk factors for cuff cellulitis after abdominal hysterectomy. Am. J. Obstet. Gynecol. 1990;163:1016–1021. doi: 10.1016/0002-9378(90)91115-s. [DOI] [PubMed] [Google Scholar]
- 13.Rahn D.D., Good M.M., Roshanravan S.M. Effects of preoperative local estrogen in postmenopausal women with prolapse: a randomized trial. J. Clin. Endocrinol. Metab. 2014;99:3728–3736. doi: 10.1210/jc.2014-1216. [DOI] [PMC free article] [PubMed] [Google Scholar]