Highlights
-
•
An isolated fracture through the radial bicipital tuberosity is rare.
-
•
The posterior approach has lower complication and is suitable for this fracture.
-
•
IM nailing is not recommended in fractures through the radial bicipital tuberosity.
Abbreviations: PIN, posterior interosseous nerve; IM, intramedullary
Keywords: Radial bicipital tuberosity, Posterior approach, Posterior interosseous nerve, Shaft fracture
Abstract
Introduction
Generally, anatomical reduction of shaft fractures through operative treatment is necessary to restore the anatomical relationship of the forearm bones. However, a number of nerves and vessels are located in the proximal radius, which complicates surgery. In this study, we aimed to reduce postoperative complications by using a posterior approach.
Presentation of case
We describe an isolated fracture through the radial bicipital tuberosity in a 69-year-old man caused by direct blunt force and our management of the fracture. The patient underwent an operation for the fracture under brachial plexus block. The injury was explored using the posterior approach, and plate fixation was performed after confirming the absence of obstacles to rotation on pronation and supination. One year later, the patient did not have any difficulties in activities of daily living.
Discussion
Since an isolated fracture through the radial bicipital tuberosity is more distal than the radial head and neck and more proximal than a common radius diaphysis fracture, we had to consider a different operative approach. The nerve and blood vessels of the forearm, such as the radial nerve and artery, run in a complicated fashion around the proximal radius; thus, we chose the posterior approach because of its simpler surgical technique and lower complication risk, compared with the anterior approach.
Conclusion
Surgeons can obtain a favorable treatment result using the posterior approach to the fracture and reduce complications by ensuring with rigid fixation using a locking plate.
1. Introduction
Forearm shaft fractures in adults occur in 1.35 per 10,000 people per year, and 80% of the forearm shaft fractures in male patients occur between the ages of 15 and 39 years [1]. The forearm plays an important role in rotation owing to the anatomical relationships between the radius and the ulna. A forearm fracture can disrupt this anatomical relationship, and if the treatment is ineffective, the patient might have a significant functional disorder of the forearm. Generally, anatomical reduction through operative treatment of shaft fractures is necessary to restore the anatomical relationship of the forearm bones [2].
There are many reports on forearm shaft fractures, but to the best of our knowledge, there is no report on isolated fractures through the radial bicipital tuberosity in the English literature. We report a case of an isolated fracture through the radial bicipital tuberosity.
The work has been reported in line with the SCARE criteria [3].
2. Presentation of case
A 69-year-old man was struck on the right side of the body by a tree branch (∼50 cm in diameter) after it was cut by a co-worker. He was transferred to our hospital from a secondary emergency hospital. The patient was on anti-hypertension medication (calcium antagonist) in the past. Informed consent was obtained from the patient, and this case report was approved by our institutional review board.
On physical examination, he was in a good state of consciousness, but he complained of right elbow pain, headache, and chest pain. His right temporal region, right chest, and right elbow had bruising, swelling, and tenderness. There was no wound or deformation. Because of the pain, he could not move his right elbow, and it was impossible to measure the range of motion of the joint. The sensory and motor functions of his right fingers and wrist were intact, and he did not have evidence of neural damage. Radiographs revealed an isolated fracture through the radial bicipital tuberosity as well as osteoarthritis of the distal radioulnar joint (Fig. 1, Fig. 2). The patient also sustained skull fracture and multiple right rib fractures, and right hemothorax was noted using computed tomography. He was hospitalized after the insertion of a thoracic catheter and was evaluated by neurosurgeons and thoracic surgeons on the day of admission.
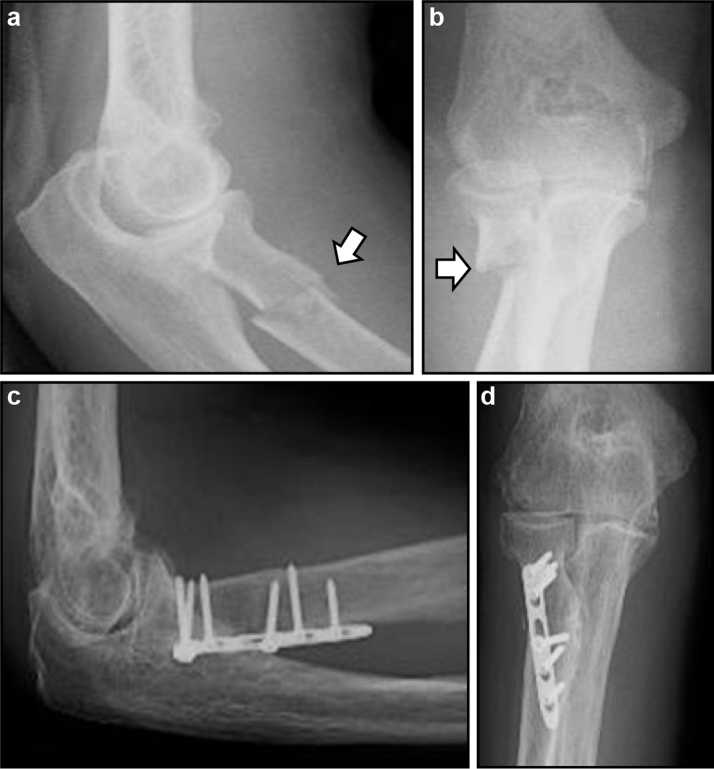
Fig. 1.
(a,b) In the initial X-ray scan, the white arrow indicates the shaft fracture of the radial bicipital tuberosity; (c,d) at 1 year after surgery, the fracture of the radial bicipital tuberosity demonstrates bony union.
Fig. 2.
Radiographs of the shaft fracture: (a) anteroposterior and (b) lateral views. The distal radioulnar joint had osteoarthritis.
Two weeks after he recovered from his multiple injuries, he underwent an operation for the fracture under brachial plexus block (0.25% bupivacaine 37.5 mg and 1% mepivacaine 150 mg) in supine position. A hand surgical specialist with more than 15 years of experience administered the anesthesia and performed the surgery.
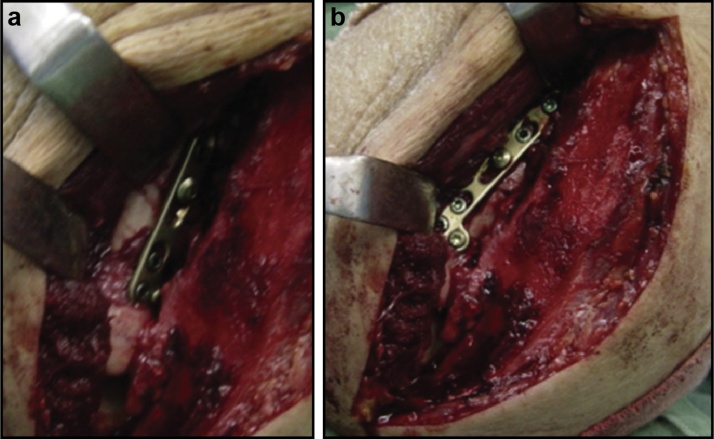
The injury was explored using Boyd’s approach (posterior). The forearm was pronated in order to move the posterior interosseous nerve (PIN) away from the operative field. The PIN was protected by subperiosteally reflecting the supinator that arises from the ulna. No dissection of the PIN was performed. The annular ligament was detached from the ulna. Reduction was performed. Then, the placement of the plate was determined after confirming that there was no obstacle to rotation on pronation and supination (Fig. 3), and it was placed opposite to the attachment point of the biceps tendon. This was followed with fixation with six screws using the LCP distal radius system 2.4 dorsal plate (Synthes Holding AG, Solothurn, Switzerland). The annular ligament was then repaired by suturing it to the periosteum and surrounding soft tissues.
Fig. 3.
(a) On supination, the plate does not impinge upon the proximal radioulnar joint; (b) on pronation, the posterior interosseous nerve was retracted away from the fracture while the plate was applied.
His right upper extremity was placed in a long arm splint immediately after operation, and he began rehabilitation on the fifth day. There was no evidence of PIN paralysis. Follow-ups on the condition of the bone and the implant, using X-ray to check for loosening of the screw and presence of callus formation, were done once a week. The splint was removed 6 weeks after surgery. He underwent rehabilitation 2 times a week for 5 months. One year later, the patient did not have any difficulties in activities of daily living, but the range of motion of his elbow joint was limited to −10° extension, 110° flexion, 10° supination, and 45° pronation (Fig. 1); his Disabilities of the Arm, Shoulder and Hand score was 19.4, and he was satisfied by the treatment.
3. Discussion
Avulsion fracture of the radial tuberosity has only been reported once in the literature [4], and to the best of our knowledge, isolated fracture through the radial bicipital tuberosity has not been reported in the English literature. Radial shaft fractures often occur with indirect force and are generally more distal to the radial bicipital tuberosity, but in our case, it resulted from a direct force. Our patient had range of motion restriction between the radius and ulna due to osteoarthritis of the distal and proximal radioulnar joints, which may have predisposed to this unusual fracture.
Since an isolated fracture through the radial bicipital tuberosity is more distal than the radial head and neck and more proximal than a common radius diaphysis fracture, we had to consider a different operative approach. The nerve and blood vessels of the forearm, such as the radial nerve and artery, run in a complicated fashion around the proximal radius, and Bartoníček et al. [5] reported using an anterior approach, but they noted that it should be performed carefully to avoid neurovascular damage during surgery. The anterior approach requires isolation and protection of the neurovascular structures and detachment of the bicep insertion for plate placement. A lateral approach, as described by Kocher and Kaplan, is generally used for radial head and neck fractures, but Kim et al. [6] reported that plate fixation of radial shaft fractures near the radial bicipital tuberosity is difficult. Robinson et al. [7] reported that the posterior approach (Boyd’s method) is useful for the treatment of radial head and neck fractures and it reduces the risk of PIN paralysis. Nasab et al. [8] found that the results and short-term complications of the anterior and posterior approaches used in the operative treatment of proximal radius fractures were similar.
We chose the posterior approach because of its simpler surgical technique and lower complication risk, compared with the anterior approach. We reduced the risk of PIN paralysis by allowing the patient’s forearm to pronate as much as possible and then separating the nerve from the surgical site [9]. We achieved a clear field of vision during the operation, which enabled us to perform plate fixation while protecting the proximal radioulnar joint.
To reduce the risk of PIN injury, intramedullary (IM) nailing may be used. A study recently reported that IM nailing achieves a good result for radial shaft fractures distal to the radial bicipital tuberosity while reducing soft tissue damage [5]. Because the distance from the radial bicipital tuberosity to the radial head is too short to provide adequate fixation if the surgeon cannot insert a sufficient length of the nail, the nail may not provide enough fixation for the radial bicipital tuberosity bone fracture. Therefore, we do not suggest the use of IM nailing for proximal radius fractures involving the radial bicipital tuberosity.
We consider surgery to be necessary in the anatomical reduction of radius shaft fracture. If the fracture site is not proximal, the anterior approach can be used, but in the case of proximal sites, the posterior approach should be used to reduce the risk of complications during surgery. Since anatomical reduction and fixation that can withstand rehabilitation on the early stage are necessary, we selected a locking plate for fixation. If firm fixation is possible, rehabilitation can be started during the early stage. When planning treatment, the approach should be considered in order to reduce the risk of complications as well as the fixation method needed to achieve functional recovery. The limitation of this study is that the number of cases is small, making it impossible to conduct sufficient verification. The weak point is that with a good surgeon, the risk of complications is low, even in the anterior approach. However, the posterior approach is considered the most promising in reducing intraoperative complications irrespective of years of experience.
4. Conclusion
We described a very rare case of an isolated fracture through the radial bicipital tuberosity. We achieved a favorable treatment result using the posterior approach to the fracture and reduced complications through rigid fixation using a locking plate.
Conflicts of interest
None.
Sources of funding
We have no sources of funding for our research.
Ethical approval
The patient provided informed consent, and the study design was approved by Niigata Prefectural Shibata Hospital’s ethics review board, with approval number 156.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Author contribution
All the authors have been actively involved in the planning and performance of the study and have also assisted with the preparation of the submitted article.
Guarantor
Kanta Imao.
References
- 1.Streubel P.N., Pesantez R. Rockwood and Green’s Fractures in Adults. Wolters Kluwer Health; Philadelphia: 2015. Diaphyseal fractures of the radius and ulna; pp. 1121–1177. [Google Scholar]
- 2.Dumont C.E., Thalmann R., Macy J.C. The effect of rotational malunion of the radius and the ulna on supination and pronation. J. Bone Joint Surg. Br. 2002;84:1070–1074. doi: 10.1302/0301-620x.84b7.12593. [DOI] [PubMed] [Google Scholar]
- 3.Agha R.A., Fowler A.J., Saeta A., Barai I., Rajmohan S., Orgill D.P., for the SCARE Group The SCARE guidelines: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 4.Strouse P.J., Ellis B.I., Kolowich P.A. Case report 811: avulsion injury of radial tuberosity (avulsion of the distal attachment of the biceps brachii) Skelet. Radiol. 1993;22:547–548. doi: 10.1007/BF00209108. [DOI] [PubMed] [Google Scholar]
- 5.Bartoníček J., Naňka O., Tuček M. Approaches to radial shaft. Rozhl. Chir. 2015;94:415–424. [PubMed] [Google Scholar]
- 6.Kim S.B., Heo Y.M., Yi J.W., Lee J.B., Lim B.G. Shaft fractures of both forearm bones: the outcomes of surgical treatment with plating only and combined plating and intramedullary nailing. Clin. Orthop. Surg. 2015;7:282–290. doi: 10.4055/cios.2015.7.3.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Robinson P.M., Li M.K., Dattani R., Van Rensburg L. The Boyd interval: a modification for use in the management of elbow trauma. Tech. Hand Upper Extremity Surg. 2016;20:37–41. doi: 10.1097/BTH.0000000000000112. [DOI] [PubMed] [Google Scholar]
- 8.Nasab S.A.M., Sarrafan N., Fakoor M., Mohammadzadeh M. Comparison of volar and dorsal approaches for surgical treatment in fracture of proximal half of the radius. Pak. J. Med. Sci. 2013;29:532–535. doi: 10.12669/pjms.292.3226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Calfee R.P., Wilson J.M., Wong A.H.W. Variations in the anatomic relations of the posterior interosseous nerve associated with proximal forearm trauma. J. Bone Joint Surg. Am. 2011;93:81–90. doi: 10.2106/JBJS.I.01242. [DOI] [PMC free article] [PubMed] [Google Scholar]