Highlights
-
•
Extramedullary hematopoiesis may occur as mimicking intrathoracic mediastinal tumor.
-
•
Surgical diagnostic confirmation should be considered in conjunction with radiology and clinical judgment.
-
•
EMH mimicking mediastinal tumor mass is required to obtain exact histological diagnosis and secure resection.
-
•
Video-assisted thoracoscopic surgery (VATS) is amendable and less invasive alternative for the definite diagnosis as well as surgical removal.
Keywords: Hematopoiesis, extramedullay; Mediastinal mass or neoplasm; Hereditary spherocytosis; Video assisted thoracoscopic surgery (VATS); A case report
Abstract
Introduction
Extramedullary hematopoiesis (EMH) is a rare disorder, defined as the appearance of hematopoietic elements outside the bone marrow or peripheral blood. The exact mechanism of this development is still unknown. We herein report a case of intrathoracic EMH, manifesting as a posterior mediastinal tumor in a patient with hereditary spherocytosis.
Presentation of case
A 45-year-old man who presented with anemia, jaundice and abdominal pain was diagnosed with hereditary spherocytosis. A 2.6 cm homogeneous right paravertebral (at the level of T8) round mass of soft tissue density was discovered incidentally on computed tomography. We performed a complete excision of mass lesion by video-assisted thoracoscopic surgery (VATS) to confirm the diagnosis. It appeared to be well encapsulated and contained bloody, fragile material. A pathological result disclosed a normal diffuse hematopoiesis consisting of megakaryocytes, immature granulocytic and myeloid precursor cells, and finally confirmed a diagnosis of EMH. Furthermore, laparoscopic splenectomy and cholecystectomy surgery was accomplished uneventfully as well.
Discussion
It was very significant to differentiate posterior mediastinal neurogenic tumor from EMH, as it can be clinically confused with other tumors of the mediastinum. Radiological examination has limitations, so definite diagnostic confirmation by surgical approach should be considered.
Conclusion
We successfully performed a complete removal of intrathoracic mediastinal mass and confirmed a diagnosis of extramedullary hematopoiesis (EMH) which is mimicking mediastinal neoplasm.
1. Introduction
Extramedullary hematopoiesis (EMH) is a compensatory response in which normal precursors of blood cells are produced outside of the bone marrow. It is usually associated with myeloproliferative disorders or hematologic disorders such as hemolytic anemia [1]. However, the exact mechanism of this development is still unknown. The most common sites of EMH are liver and spleen, but it has been documented in other organs such as the mediastinum, lymph nodes, breast, and central nervous system [1]. Among them, intrathoracic EMH is commonly encountered as a mass in the posteroinferior mediastinum, though there have been a few reports of the anterior mediastinum or pleura [2]. In patients with a medical history of neoplastic or hematologic disorders presenting with intrathoracic mass, a diagnosis of EMH should be considered in the differential diagnosis. Definite diagnosis of tissues can be easily established by VATS excisional biopsy. As for this report, intrathoracic EMH especially associated with hereditary spherocytosis (HS) is a rare phenomenon, which only a few cases have been reported. This work has been reported in line with the Surgical Case Report (SCARE) criteria [3].
2. Presentation of case
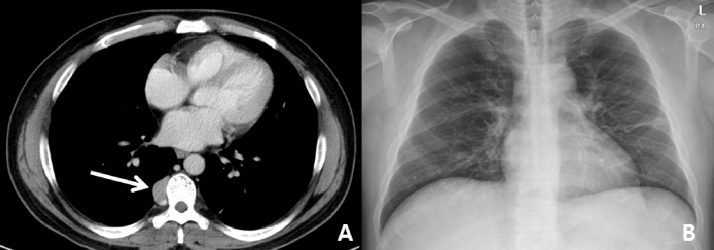
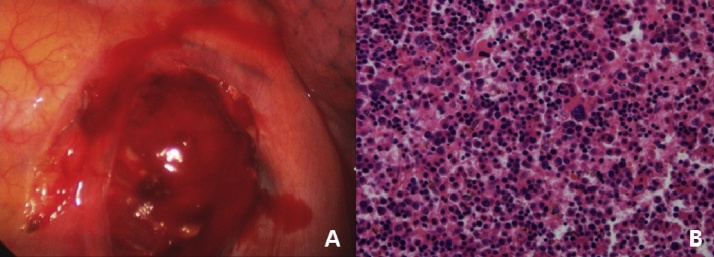
A 45-year-old man visited our hospital with a complaint of anemia, severe jaundice, and abdominal pain. There were no specific past medical history. On his physical examination, there could be examined hepatosplenomegaly on palpation, but no other specific abnormalities were identified except for a pale conjunctiva and icteric sclera. The initial whole blood counts were as follows: white blood cells 8.21 × 103/μL, hemoglobin 11.7 g/dl, hematocrit 34.0%, platelets 162,000/μL, and reticulocytes 318 × 103/μL. Chemistry analysis findings revealed total bilirubin 14.5 mg/dl, direct bilirubin 12.6 mg/dl, alanine aminotransferase (ALT) 59 IU/L, alkaline phosphatase (ALP) 167 IU/L, and haptoglobin <10 mg/dl. A peripheral blood smear showed marked spherocytes with anisocytosis, and prominent polychromatic erythrocytes. The osmotic fragility test was increased as well. As mentioned above, the results of the laboratory investigations somewhat substantiate the diagnosis of hereditary spherocytosis (HS). Then, computed tomography (CT) scan was performed, which disclosed chronic calculous cholecystitis and marked splenomegaly measuring almost 20 cm at maximum diameter. It also incidentally identified a 2.6 cm homogenous right paravertebral (at the level of T8) mediastinal mass of soft tissue density, which did not erode the adjacent bony structure (Fig. 1A). Meanwhile, chest radiography displayed no remarkable abnormal findings except fibrotic scar on left lower lobe field (Fig. 1B). At this point, the radiologist suggested an impression of neurogenic tumor such as ganglioneuroma or neurilemmoma. Accordingly, a splenectomy surgery was planned under the diagnosis of HS, and video-assisted thoracoscopic surgery (VATS) was concurrently performed to confirm the pathologic diagnosis to differentiate some kinds of neoplastic mediastinal tumors. After mobilizing the right lower lung, a 2.6 × 2 x 2 cm sized, ovoid shape soft friable mass was encountered in the right paravertebral (at the level of T8) area. It was located at the upper margin of posterior arc of 8th rib (Fig. 2A). It was well encapsulated and contained bloody, fragile material. Complicated small connected vessels and stalks were ligated with Endo-Clips. Invasion into the intervertebral foramen was not observed, and the mass was totally removed without difficulty. A permanent histopathological examination demonstrated a normal diffuse hematopoiesis consisting of megakaryocytes, immature granulocytic and myeloid precursor cells (Fig. 2B), and confirmed a diagnosis of EMH. The patient recovered uneventfully and was discharged on the 7th postoperative day. No postoperative complication or adverse events were found six months after surgery.
Fig. 1.
(A) Computed tomographic scan of chest showing a 2.6 cm homogenous right paravertebral mediastinal mass (B) Posteroanterior chest radiography.
Fig. 2.
(A) Thoracoscopic findings of extramedullary hematopoiesis at the upper margin of posterior arc of 8th rib (B) The microscopic findings of the specimen (H&E, x400). Note diffuse hematopoiesis consisting of megakaryocytes, immature granulocytic and myeloid precursor cells.
3. Discussion
EMH is considered as a physiologic compensatory process which occurs when the bone marrow is not able to sustain its function of proper red cell production, but it has been found occasionally without obvious reason [4]. Intrathoracic EMH is a rare condition which was first described by Guizetti during an autopsy in 1912. The following reports are also based on autopsy findings until 1945, when Ask-Upmark made a diagnosis in a living person by percutaneous needle biopsy [5]. In most cases, it is situated in the posteroinferior mediastinum, and usually accompanied by chronic hemolytic anemia presenting in a male adult predominantly. These intrathoracic neoplasms could be solitary or multiple masses, even unilaterally or bilaterally [6].
In general, the patients with hereditary spherocytosis (HS) are almost asymptomatic. Symptoms may originated from hemolytic anemia such as jaundice and splenomegaly. Hereditary spherocytosis (HS), an autosomal dominant genetic disorder of cell membrane abnormality can lead to the destruction of normal cellular structure, which may cause development of spherical morphological change in red blood cells and subsequent cell lysis [7]. This can explain the reason why the patients with HS present with symptoms of jaundice, anemia and hepatosplenomegaly, and it can be also associated with EMH as a compensatory reaction [8]. Various diagnositc studies including computed tomography (CT) scan, scintigram and MRI can assist to diagnose the disease entity. CT finding is chracterized by the presence of homogenous round or lobulated soft tissure density masses usually in the posterior mediastinum, below the level of T6. They mosly do not have calcification content, and are not associated with adjacent bony destruction [9]. EMH may also be identified by radionuclide imaging with 111In chloride or 99Tcm sulfur colloid [10]. Even though diverse radiological examination is utilized to detect the disease, histological confirmation is indispensable.
However, there are actually potential hazard in case of invasive diagnostic procedures such as needle aspiration biosy or thoracotomy, because it is well known these masses contain highly vascular nature and significant bleeding risks during the procedure of biopsy [11]. In principle, asymptomatic patients with intrathoracic EMH require no treatment. If there are associated pain or relevant symptoms, eradication may be indicated. Surgical resection is recommend in patients whom a sort of malignancy is suspected or in the presence of a symptomatic mass with space occupying effects or spontaneous bleeding [12]. Meanwhile, in some cases, relatively small dose of radiation may be applied for the adjuvant thrapy in association with complications such as hemothorax, pleural effusion,and spinal cord compression [13].
4. Conclusion
In conclusion, EMH is a rare cause of an intrathoracic mass in a patient with hemolytic disorder. It may be easily confused with other mediastinal tumors in clinical diagnosis. Intrathoracic EMH mimicking mediastinal tumor mass is required to obtain exact histological diagnosis and secure resection. In this respect, video-assisted thoracoscopic surgery (VATS) is amendable and less invasive alternative for the definite diagnosis of tissues as well as surgical removal. VATS allows direct visualization and is more efficient way of controlling unexpected bleeding and hemorrhage in comparison with percutaneous needle approach. We hereby report a surgical experience of EMH that presented as a paravertebral mediastinal mass, which was treated by complete resection through VATS in a patient of hereditary spherocytosis. Concurrently, laparoscopic splenectomy and cholecystectomy surgery was accomplished uneventfully as well.
Conflicts of interest
All authors have no potential conflicts of interests to disclose.
Funding
All authors have no sources of funding to declare for this case report.
Ethical approval
This is not considered a research study. This is a descriptive case report.
Consent
Written informed consent was obtained from the patient's and his first degree relatives for publication of this case and involving images.
Author contribution
Jae Bum, Park: examination of the patient prior to surgery, operating assistant, writing the paper, data collection and interpretation.
Song Am, Lee and Yo Han, Kim: follow up, contribution to the writing process, proof-reading.
Woo Surng, Lee: proof-reading, comments
Jae Joon, Hwang: operator, study concept, follow-up, proof-reading, comments.
Guarantor
All authors accept full responsibility for the work in this case report and control the decision to publish.
References
- 1.Koch C.A., Li C.Y., Mesa R.A., Tefferi A. Nonhepatosplenic extramedullary hematopoiesis: associated diseases, pathology, clinical course, and treatment. Mayo Clin. Proc. 2003;78:1223–1233. doi: 10.4065/78.10.1223. [DOI] [PubMed] [Google Scholar]
- 2.Kupferschmid J.P., Shahian D.M., Villanueva A.G. Massive hemothorax associated with intrathoracic extramedullary hematopoiesis involving the pleura. Chest. 1993;103:974–975. doi: 10.1378/chest.103.3.974. [DOI] [PubMed] [Google Scholar]
- 3.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S. Orgill DP and the SCARE Group: The SCARE statement: Consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 4.Petit J., Estany C. Mediastinal extramedullary erythropoiesis in hereditary spherocytosis. Clin. Lab. Haematol. 1987;327:9. doi: 10.1111/j.1365-2257.1987.tb00098.x. [DOI] [PubMed] [Google Scholar]
- 5.Ash-Upmark E. Tumor-stimulating intra-thoracic heterotopia of bone marrow. Acta Radiol. 1945;425:26. [Google Scholar]
- 6.Ng C.S., Wan S., Lee T.W., Sihoe A.D., Wan I.Y., Arifi A.A., Yim A.P. Video assisted thoracic surgery for mediastinal extramedullary hematopoiesis. Ann. R. Coll. Surg. Engl. 2002;84:161–163. [PMC free article] [PubMed] [Google Scholar]
- 7.Hassoun H., Palek J. Hereditary spherocytosis: a review of the clinical and molecular aspect of the disease. Blood Rev. 1996;10:129–147. doi: 10.1016/s0268-960x(96)90021-1. [DOI] [PubMed] [Google Scholar]
- 8.Smith J., Rahilly M., Davidson K. Extramedullary hematopoiesis secondary to hereditary spherocytosis. Br. J. Haematol. 2011;154:153. doi: 10.1111/j.1365-2141.2011.08692.x. [DOI] [PubMed] [Google Scholar]
- 9.Alam R., Padmanabhan K., Rao H. Paravertebral mass in a patient with thalassemia. Chest. 1997;112:265–267. doi: 10.1378/chest.112.1.265. [DOI] [PubMed] [Google Scholar]
- 10.Jackson A., Burton I.E. Retroperitoneal mass and spinal cord compression due to extramedually hematopoiesis in polycythaemia rubra vera. J. Radiol. 1989;62:944–947. doi: 10.1259/0007-1285-62-742-944. [DOI] [PubMed] [Google Scholar]
- 11.Smith P.R., Manjoney D.L., Teicher J.B., Choi K.N., Braverman A.S. Massive hemothorax due to intrathoracic extramedually hematopoiesis in a patient with thalassemia intermedia. Chest. 1988;94:658–660. doi: 10.1378/chest.94.3.658. [DOI] [PubMed] [Google Scholar]
- 12.Xiros N., Economopoulos T., Papageorgiou E., Mantzios G., Raptis S. Massive hemothorax due to intrathoracic extramedually hematopoiesis in a patient with hereditary spherocytosis. Ann. Haematol. 2001;80:38–40. doi: 10.1007/s002770000222. [DOI] [PubMed] [Google Scholar]
- 13.Dore F., Pardini S., Gaviano E., Longinotti M., Bonfigli S., Rovasio S. Recurrence of spinal cord compression from extramedullary hematopoiesis in thalassemia intermedia treated with low doses of radiotherapy. Am. J. Hematol. 1993;44:148. doi: 10.1002/ajh.2830440216. [DOI] [PubMed] [Google Scholar]