Abstract
AIM
To investigate whether DNA vaccine encoding herpes simplex virus 1 (HSV-1) glycoprotein C (gC) and glycoprotein D (gD) will achieve better protective effect against herpes simplex keratitis (HSK) than DNA vaccine encoding gD alone.
METHODS
DNA vaccine expressing gD or gC combined gD (gD.gC) were constructed and carried by chitosan nanoparticle. The expression of fusion protein gD and gC were detected in DNA/nanoparticle transfected 293T cells by Western-blot. For immunization, mice were inoculated with DNA/nanoparticle for 3 times with 2wk interval, and two weeks after the final immunization, the specific immune responses and clinical degrees of primary HSK were evaluated.
RESULTS
Fusion protein gD.gC could be expressed successfully in cultured 293T cells. And, pRSC-gC.gD-IL21 DNA/chitosan nanoparticle could effectively elicit strongest humoral and cellular immune response in primary HSK mice evidenced by higher levels of specific neutralizing antibody and sIgA production, enhanced cytotoxicities of splenocytes and nature killer cells (NK), when compared with those of gD alone or mocked vaccine immunized mice. As a result, gC-based vaccine immunized mice showed least HSK disease.
CONCLUSION
gC-based DNA vaccine could effectively prevent the progress of primary HSK, suggesting that this DNA vaccine could be a promising vaccine for HSK treatment in the future.
Keywords: herpes simplex virus 1, keratitis, gC-based DNA vaccine, nanocarrier, immune response
INTRODUCTION
Herpes simplex keratitis (HSK) is a chief worldwide blind-causing corneal disease that mainly caused by herpes simplex virus type 1 (HSV-1) infection[1]. After infection, HSV-1 virus will exist in host for a lifelong time[2]. Generally, in human there are 3 ongoing phases that finally contribute to the development of HSK, namely primary infection, latent phase and recurrent phase[2].
The antiviral medications, which is the main strategy for HSK management at present, just temporarily control symptoms of HSK, not eradicate the disease or virus[3]. As yet, no methods that can effectively control the spread of virus are available. Due to the ability of causing specific immune response against HSV-1, HSK vaccines are thought to be the most effective approach to deal with HSK[4]–[5]. Among them, DNA vaccine is getting particular attention. After being inoculated, the target genes of DNA vaccine are expressed and presented in host cells and could produce strong and sustained cellular and humoral immune responses[6]–[7]. In some fields such as Venezuelan equine encephalitis, cancer and human immunodeficiency virus infection, DNA vaccine have being designed or tested in clinical trails[8]–[10]. We previously constructed a DNA vaccine encoding glycoprotein D (gD) of HSV-1 and interleukin (IL)-21[11]. There, gD serves as major immunogen and IL-21 is an adjuvant molecular for the purpose of improving the entire immune outcome. After being tested, this DNA vaccine showed protective against primary HSK, but had limited effect when dealing with recurrent HSK. Therefore, more efficient HSV-1 DNA vaccine should be developed.
Different from primary HSK, recurrent HSK occurs in the condition of preexistence of certain HSV-1 neutralizing antibody. One of the most important reasons explaining why neutralizing antibody can't eliminate virus is evolved immune evasion mechanism of HSV-1. A total of 12 glycoproteins were reported on the surface of HSV-1[12]. Among them, gD and glycoprotein B (gB) can elicit strong specific immune response against HSV-1, while glycoprotein C (gC) plays a critical role in mediating immune evasion of HSV-1[13]–[14]. As we all known, complement serving as a major none-specific immune response in body is vital for controlling virus infection[15]. However, gC can disrupt the process of complement activation via binding complement C3b and blocking the C5 and properdin interaction with C3b, thereby benefiting virus infection[16]–[18]. Strategies to prevent gC mediated immune evasion may be required to develop successful HSV vaccines. Chang et al[19] reported that immunization with gC of HSV-1 could totally blocks C3b binding and reduces disease severity. However, gC is not very immunogenic and gC alone can't induce sufficient immune protective effect against HSV-1 disease[20]. Recent studies focus on investigating whether combination gC and gD will have a better therapeutic effect to HSV disease, compared to gC or gD alone. It has been reported that immunizing mice with gD and gC proteins provided better protection than gD alone in preventing HSV-1 or HSV-2 associated infectious diseases[21]–[22]. However, DNA vaccine encoding gC and gD for HSK treatment have not been reported.
In this study, we developed a DNA vaccine construct pRSC-gC.gD-IL21 by fusing gC sequence of HSV-1 with gD and using IL-21 which is well-known adjuvant molecular. Considered the fact that the efficiency of DNA membrane associated transport is extreme low and DNA can be degraded easily without protection, therefore a suitable carrier is needed[23]–[24]. Chitosan, as a natural cationic polysaccharide, can easily combine with the negatively charged plasmid DNA and has the properties of being easily absorbed and biodegraded, allowing gene slow release and long lasting expression, low toxicity and cost, enhancing the immune response, have been widely used as DNA carrier[25]–[26]. Here, we embedded the plasmid DNA into chitosan to form DNA plasmid/chitosan nanoparticle for immunization.
Besides DNA carrier, the inoculation approach also matters. We previously demonstrated that topically administration of nanoparticle-loaded DNA vaccine could induce stronger ocular local immune response of mice than intramuscular inoculation[27]. What's more, it has been noted that nanoparticle could benefit local inoculation by inducing strong local mucosal immunity[28]–[29]. Therefore, we adopted topical immunization in this study. Here, we reported that we successfully constructed gC-based vaccine termed pRSC-gC.gD-IL21 and investigated its effect against primary HSK. This study provided the experimental fundaments for further investigating this vaccine in dealing with recurrent HSK which is the key point for HSK management.
MATERIALS AND METHODS
Mice, Cell Lines and Virus
Balb/c background female mice (4-6wk) were purchased from the Animal Center of Yangzhou University for experimental use. And mice were maintained under pathogen free conditions with a 12h/12h light-dark cycle. Vero cells derived from African green monkey kidney were preserved in our lab. SP2/0 cells derived from Balb/c mice myeloma cells and YAC-1 cells derived from moloney leukemia-induced T cell lymphoma, were acquired from Cellular Institute of China in Shanghai. All the cells were cultured in RPMI1640 containing 10% fetal bovine serum, 100 units/mL penicillin G sodium and 100 g/mL streptomycin sulfate at 37°C in 5% CO2 atmosphere. HSV-1 strain F was obtained from the Institute of Virology in Wuhan, China. All the animal experiments were strictly in accordance with the guidelines of the Animal Research Ethics Board of Southeast University, China.
Plasmids and Primers
Recombined pRSC-gD-IL21 plasmid were constructed and preserved in our lab. The gC gene (whole extracellular sequence from Gly25 to Gly480) was harvested by polymerase chain reaction (PCR) amplifying with a pair of specific primers to the gC gene (forward: 5′-TTTACAAGCTTGGCTCGGAAACTGCCTCCAC-3′, reverse: 5′-ATATGGCTAGCTCATTGCCCCCACCCACTCGATCGCCTCGA-3′) and HSV-1 gene was used as template. The gD (whole extracellular sequence from Met1 to Met340)-linker gene was obtained by double time PCR. Briefly, pRSC-gD-IL21 was set as template for the first round amplifying with a pair of specific primers (forward: 5′-ATATGGGTACCGCCGCCACCATGGGGGGGGCTGCCGCCA-3′, reverse: 5′-CCACCCGAACCTCCACCTTHCCATGTTGTTCGGGGTGGCCGGGGGAT-3′). The product of first round PCR was used as template for the second round PCR and the primers are 5′-ATATGGGTACCGCCGCCACCATGGGGGGGGCTGCCGCCA-3′(forward), and 5′-GCCAAGCTTAGAACCTCCACCTGAACCTCCACCCGAACCTCCACCCATG-3′(reverse).
Construction and Identification of pRSC-gC.gD-IL21 DNA Vaccine
We firstly prepared the plasmid pRSC-gD-Linker-IL21.pRSC-IL21, which was obtained by removing the gD sequence from pRSC-gD-IL21, was connected with gD linker DNA and finally formed pRSC-gD-Linker-IL21. After being digested by HindIII and NheI, gC DNA was connected with pRSC-gD-Linker-IL21 and finally developed the plasmid pRSC-gC.gD-IL21 DNA, which was identified by the analysis of restriction endonuclease digestion, DNA sequence and target protein expression in 293T cells.
Transfection and Western Blot
For transfection, the cultured 293T cells in 6-well plates were transfected with 20 µL mixture of pRSC-gC.gD-IL21 DNA/chitosan or mock plasmid (10 µg plasmid/1×106/cells) by using LipofectAMINETM 2000 reagent (Invitrogen, USA). After incubation for 4h, the transfected cells were washed with RPMI1640 to remove the free nanoparticle mixtures, and the cells were further cultured for 48h. For Western blot, the cell were harvested and homogenized in RIPA buffer containing Tris-HCl (50 mmol/L), NaCl (150 mmol/L), EDTA (1 mmol/L), Triton-X (1%), sodium deoxycholate (0.5%) and SDS (0.1%). Then, the homogenates were centrifuged at 13 000 r/min for 15min at 4°C and the supernatant was acquired as extracted protein. After electrophoresis, proteins were transferred on PVDF membranes. The membranes were soaked in 5% milk/PBST for 2h at room temperature. And then, the membranes were incubated with anti-gD antibody for 1h. The following steps were performed according to the Western-Breeze Kits protocol (Invitrogen, USA).
Preparation and Examination of Chitosan/DNA Nanoparticle
Chitosan was dissolved in NaAc (5 µmol/L, pH5.5) solution at a ratio of 0.02% (w/v). Plasmid DNA (0.8 µg) was diluted in Na2SO4 (5 mmol/L) solution. After bathing in water (55°C) for 10min, chitosan solution and DNA solution were mixed by vortex at equal volume, and the mixture was stored for experimental use. For the purpose of examining the loading efficiency, the naked plasmid DNA, precipitation of chitosan/DNA nanoparticle and supernant of chitosan/DNA nanoparticle were subjected to agarose gel electrophoresis. DNA bands were visualized by EtBr. To determine the protective effect of chitosan on plasmid DNA, the naked plasmid DNA and chitosan/DNA nanoparticle were digested by DnpI and the products were subjected to agarose gel electrophoresis, DNA bands were visualized by EtBr.
Vaccine Immunization and Virus Challenge in Mice
Mice (n=12) were randomly divided into 4 groups: pRSC-gC.gD-IL21/chitosan group; pRSC-gD-IL21/chitosan group; pRSC/chitosan group and chitosan group. The plasmid DNA/chitosan (20 µL containing 100 µg DNA) or chitosan were dropped into conjunctival sacs of each mice. The total immunization was 3 times and with 2wk interval. Two weeks after the last immunization, the mice (n=6) were sacrificed for determining immune efficiency. And, the rest received HSV-1 challenge experiments as previous described. Briefly, after being anesthetized by ketamine (100 mg/kg, i.p.), the corneas of mice were scarified 10 times with a needle and were inoculated with HSV-1 [10 µL of 7.1×106 plaque forming unit (PFU)/mL]. The pathological changes of epithelial or stromal were examined by ophthalmological slit lamp microscope for 15 consecutive days after HSV-1 challenge. Epithelial or stromal lesions were scored as previous described[30].
Measurement of Anti-HSV Neutralizing Antibody in Serum
Two weeks after final immunization, blood were drew from mice by retro-orbital bleeding and centrifuged at 3500 r/min for 15min, then serum were gathered and inactivated in water bath (55°C) for 30min. A two-fold series of dilutions of sera was incubated with an equal volume of the virus (7.1×106 TCID 50/mL). And, the mixture was added in the cultured vero cells for 72h. Cell pathological changes were observed by microscope. The antivirus neutralizing antibody titer was calculated as the reciprocal of the dilution which resulted in 50% reduction in virus titer.
Measurement of sIgA in Mice Tears
For tear collection, a small swab was inserted carefully inside the lower lid of the eyes of an immunized mouse for 5min and this was repeated 5 times at 1h intervals. The swabs were soaked in 0.1 mL phosphate buffer saline (PBS) over night at 4°C. A two-fold dilution of extracted tear was prepared for detecting sIgA by enzyme-linked immunosorbent assay (ELISA). Briefly, tear samples were added in 96-well plates which were coated with anti HSV-1 gD (10 µg/mL) antigen and the plate were kept overnight at 4°C. After being washed in PBS for 3 times, the goat anti mice IgA-HRP antibody were added in the wells for 1h at room temperature. After visualization by DAB, the plates were read at an optical density of 490 nm by using a Fusion or Victor 31420 plate reader (Perkin Elmer, USA).
Measurement of Cellular Immune Responses
Two week after last immunization, the mice were sacrificed and spleen was removed. And then, single cell suspension of spleen at a density of 1×106/mL was prepared as effector cells. The SP2/0 cells which have been transfected with pRSC-gD-IL21/chitosan nanoparticle and YAC-1 cells (not transfected) were set as target cells of splenocytes and nature killer cells (NK) respectively. The target cells were adjusted to a density of 1×104/mL and cultured in RPMI1640 containing 10% fetal bovine serum at 37°C in 5% CO2 atmosphere for 48h. The effector cells were co-cultured with target cells at a ratio of 50:1 and cytotoxicity was detected by LDH release. The detailed procedures of LDH release test were described in manufacturer's instructions (Genmed Scientifics).
Data Analysis
All the values were represented as mean±SD. Unpaired Sudent's t-test was used for comparison between 2 groups, whereas Kruskal-Wallis H test was used for the statistic of clinical data. Data analysis was performed with SPSS9.0.
RESULTS
Identification of Constructed pRSC-gC.gD-IL21 DNA Vaccine
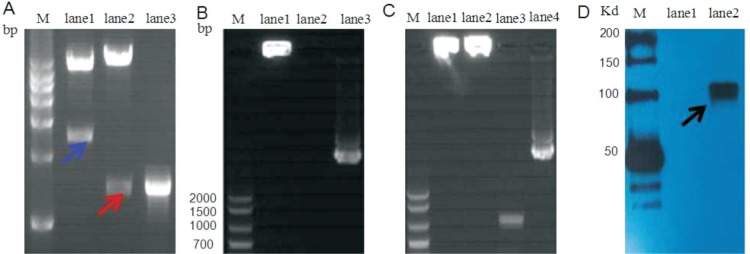
To validate whether the pRSC-gC.gD-IL21 DNA vaccine was constructed successfully, the plasmid were sequenced. The gC sequences we detected are 99.12% consistent with the data existed in the Genebank (only 4 amino acids are different, including P132S, F299L, H306R, I383H), and the gD sequences are 98.22% with only 7 different amino acids, including L50P, Q52R, N71D, T217A, P295Q, V361G, P374R. We consider that these rare mutated sits are due to the different strains of HSV-1 and couldn't affect its function. For further confirmation, the pRSC-gC.gD-IL21 were digested by HindIII/NheI or Hind/NheI and the products were subjected to agarose gel electrophoresis. We observed a 2454 bp DNA band which is equal to the length of gD+gC and a 1393 bp gC DNA band in the gel (Figure 1A).
Figure 1. Identification of constructed pRSC-gC.gD-IL21 DNA vaccine.
A: pRSC-gC.gD-IL21 DNA was validated by endonuclease. pRSC-gC.gD-IL21 DNA was digested by KpnI/NheI (lane1) or Hind/NheI (lane2); Lane3 is gC DNA. Blue arrow indicated the sequence of gD+gC (2454 bp) and red arrow indicated the sequence of gC (1393 bp). B: The precipitation (lane1) or supernant (lane2) of pRSC-gC.gD-IL21 DNA/chitosan and naked pRSC-gC.gD-IL21 DNA (lane3) nanoparticle were subjected to agarose gel electrophoresis. C: Naked pRSC-gC.gD-IL21 DNA or pRSC-gC.gD-IL21 DNA/chitosan nanoparticle were treated with or without DnpI: pRSC-gC.gD-IL21 DNA/chitosan nanoparticle with (lane1) and without DnpI (lane2); Naked pRSC-gC.gD-IL21 DNA with (lane3) or without DnpI (lane4). D: Western blot analysis of gD antibody labeled protein in pRSC-gC.gD-IL21 DNA/chitosan narnoparticle transfected (lane2) or untransfected (lane1) 293T cells. Arrow indicated the target protein (gD+gC). Data are representative of 3 repeated experiments.
To test the packaging efficiency of chitosan to plasmid DNA, the mixture of pRSC-gC.gD-IL21 DNA/nanoparticle was centrifuged and DNA content in the supernant and precipitation were detected by ultraviolet spectrophotometer. The ratio of pRSC-gC.gD-IL21 DNA in chitosan nanoparticle was near 97% and this was further confirmed by agarose gel electrophoresis. Result showed that there was almost no visualized DNA band for supernant (Figure 1B). Furthermore, the electrophoresis analysis revealed that chitosan nanoparticle could efficiently protect the pRSC-gC.gD-IL21 DNA against DnpI (Figure 1C). Western blot analysis revealed that a 117 Kd protein (gD+gC) existed in pRSC-gC.gD-IL21 DNA/chitosan nanoparticle transfected 293T cells (Figure 1D). These results demonstrated that the pRSC-gC.gD-IL21 DNA vaccine was constructed successfully.
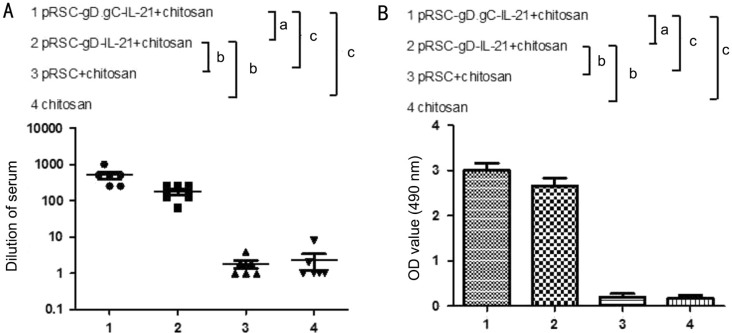
The Levels of HSV-1 Neutralizing Antibody and sIgA in Immunized Mice
To examine the humoral immune responses in immunized mice, we detected the levels of HSV-1 neutralizing antibody and sIgA. Results showed that the levels of HSV-1 neutralizing antibody in pRSC-gC.gD-IL21 DNA/chitosan immunized mice were near ten folds of the mice immunized with pRSC-gD-IL21 DNA/chitosan and the pRSC/chitosan or chitosan immunized mice showed the lowest levels of HSV-1 neutralizing antibody. In addition, the levels of sIgA in tear of pRSC-gC.gD-IL21 DNA/chitosan immunized mice is highest, with intermediate levels of sIgA in tear of pRSC-gD-IL21 DNA/chitosan immunized mice and relatively lower levels in tear of pRSC/chitosan or chitosan immunized mice (Figure 2). These results demonstrated that pRSC-gC.gD-IL21 DNA/chitosan vaccine could effectively induced humoral immune responses in mice.
Figure 2. The level of HSV-1 neutralizing antibody and sIgA in immunized mice.
A: Detection of HSV-1 neutralizing antibody in serum of immunized mice; B: Detection of sIgA in tear of immunized mice. All data were expressed as mean±SD, n=6, aP<0.05; bP<0.01; cP<0.001. Data are representative of 3 repeated experiments.
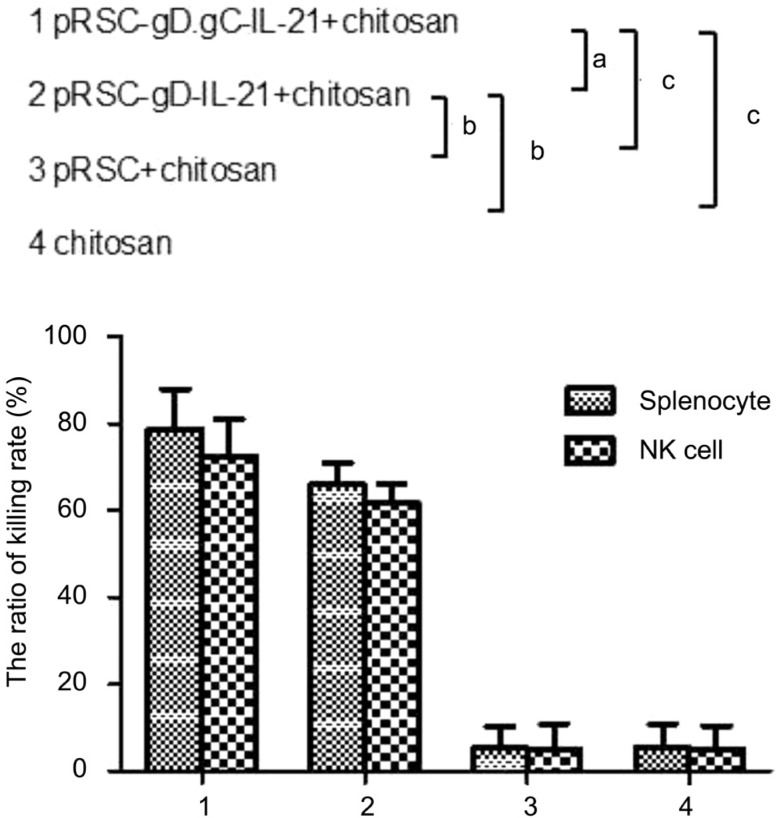
Cellular Immune Response to DNA Vaccine
To determine cellular immune response in immunized mice, we investigated the cytotoxic activities of NK cells or splenocytes. Results showed that pRSC-gC.gD-IL21 DNA/chitosan immunized mice exhibited the highest NK and splenocytes activities, followed by pRSC-gD-IL21 DNA/chitosan immunized mice, and the lowest were pRSC/chitosan and chitosan immunized mice (Figure 3). These results indicated that pRSC-gC.gD-IL21 DNA/chitosan conferred the most robust cellular immune response to gD on mice compared with that of pRSC-gD-IL21 DNA/chitosan or mocked plasmid vaccine.
Figure 3. Cytoxic activities of splenocytes or NK cells in immunized mice.
The splenocytes or NK cells were separated from immunized mice and correspondingly mixed with pRSC-gD-IL21DNA/chitosan nanoparticle transfected SP/2 (target cell of splenocytes) or not transfected YAC-1 cells (target cell of NK cells) at a ratio of 50:1. Cell death were determined by LDH release. All data were expressed as mean±SD, n=6, aP<0.05; bP<0.01; cP<0.001. Data are representative of 3 repeated experiments.
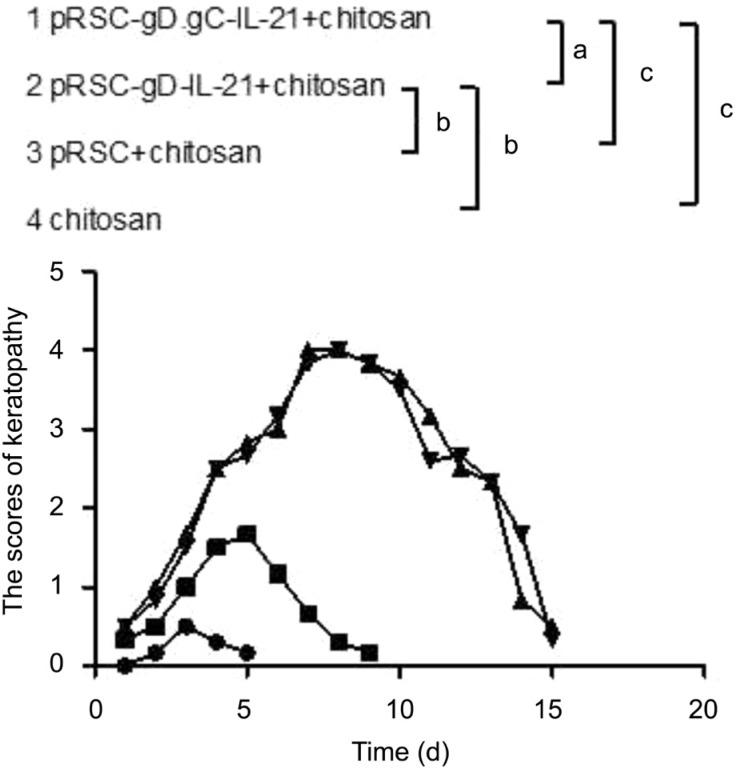
Clinical Keratitis of Vaccine Immunized Mice After Virus Challenge
The vaccine immunized mice were inoculated with HSV-1 virus and the pathological changes of corneas were monitored daily for 15d. After virus challenge, pRSC-gC.gD-IL21 DNA/chitosan immunized mice showed the least severe herpes keratitis and got a total recovery by day 5, while the mocked plasmid/chitosan or chitosan exhibited the most severe herpes keratitis with a recovery in day 15. And the severity of herpes keratitis in pRSC-gD-IL21 DNA/chitosan immunized mice ranked from pRSC-gC.gD-IL21 DNA/chitosan to mocked plasmid/chitosan or chitosan immunized mice (Figure 4). These results demonstrated that pRSC-gC.gD-IL21 DNA/chitosan vaccine could effectively protect mice against herpes keratitis caused by HSV-1 infection when compared with pRSC-gD-IL21 DNA/chitosan vaccine.
Figure 4. Clinical score of herpes keratitis in HSV-1 infected immunized mice.
The plasmid DNA/chitosan nanoparticle vaccine containing pRSC-gC.gD-IL21, pRSC-gD-IL21, pRSC or none plasmid immunized mice received the HSV-1 challenge and the herpes keratitis was scored daily for 15d for each group mice. All data were expressed as mean±SD, n=6, aP<0.05; bP<0.01; cP<0.001. Data are representative of 3 repeated experiments.
DISCUSSION
It has been reported that gC play a critical role in mediating the immune evasion of HSV-1 and the strategy targeting to gC represents a promising approach to control the spread of virus[19],[31]–[32]. Several studies demonstrated that gC could effectively enhance gD induced immune protection against HSV disease[21]–[22]. In present study, we developed a gC based DNA vaccine called pRSC-gC.gD-IL21 DNA vaccine by fusing gD sequence of HSV-1 to gC of HSV-1, and we demonstrated that pRSC-gC.gD-IL21 DNA vaccine could induced strongest humoral and cellular immune response to protect mice against primary HSK, when compared with pRSC-gD-IL21 DNA vaccine.
First of this study, we examined whether our gC based DNA vaccine was developed successfully. Endonuclease digestion experiments revealed that our vaccine constructed successfully. Given low efficiency of cell entry for naked DNA, we loaded DNA vaccine in chitosan to form the DNA/chitosan nanoparticle. After being tested, the chitosan nanoparticle could effectively carry the DNA vaccine, with 97 percent of loading efficiency and protect the DNA vaccine from DnpI. Furthermore pRSC-gC.gD-IL21 DNA/chitosan nanoparticle transfected cells could effectively produced fusion protein gD plus gC. These results demonstrated that gC based DNA vaccine was developed successfully.
It is known that a successful vaccine should be able to induce both high level of humoral and cellular immune response. In this study, we found that chitosan nanoparticle containing pRSC-gC.gD-IL21 DNA immunized mice produced more HSV-1 neutralizing antibody in serum and sIgA in tear when compared with that of pRSC-gD-IL21 DNA vaccine or mock DNA vaccine immunized mice. What's more, cellular immune responses reflected by splenocytes and NK activities in pRSC-gC.gD-IL21 DNA/chitosan immunized mice were the strongest among 4 groups. Above results were consistent with the observations that the corneal pathological grade of pRSC-gC.gD-IL21 DNA/chitosan immunized primary HSK mice was the lowest, and got a total recovery by day 5 while pRSC-gD-IL21 DNA/chitosan immunized primary HSK mice got a total recovery by day 10. These results are similar with the study by Awasthi et al[22] demonstrating that immunization with a vaccine combining herpes simplex virus 2 (HSV-2) gC and gD proteis improved the protection of dorsal root ganglia in mice compared to immunization with gD alone. In their study, they also observed that gD and gC protein combination immunized animals showed a higher level neutralizing antibody, enhanced cellular immune response and less disease. However, it is the first time for our study to report DNA vaccine expressing fusion protein gD and gC for HSK treatment.
In conclusion, this study demonstrated that chitosan nanoparticles loading pRSC-gC.gD-IL21 DNA vaccine could effectively alleviate symptoms of herpes keratitis caused by HSV-1 primary infection in mice via inducing robust humoral and cellular immune response. This study laid the foundation of investigating this DNA vaccine in recurrent HSK treatment.
Acknowledgments
Foundations: Supported by Natural Science Foundation of Jiangsu Province (No.BK20141346); Nanjing Science and Technology Development Plan (No.201402001).
Conflicts of Interest: Dong LL, None; Tang R, None; Zhai YJ, None; Malla T, None; Hu K, None.
REFERENCES
- 1.Farooq AV, Shukla D. Herpes simplex epithelial and stromal keratitis: an epidemiologic update. Surv Ophthalmol. 2012;57(5):448–462. doi: 10.1016/j.survophthal.2012.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rowe AM, St Leger AJ, Jeon S, Dhaliwal DK, Knickelbein JE, Hendricks RL. Herpes keratitis. Prog Retin Eye Res. 2013;32:88–101. doi: 10.1016/j.preteyeres.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arefian E, Bamdad T, Soleimanjahi H, Akhood MR, Parsania M, Ghaemi A. A kinetic study of gamma interferon production in herpes simplex virus-1 DNA prime-protein boost regimen comparing to DNA or subunit vaccination. Mol Biol (Mosk) 2009;43(3):422–428. [PubMed] [Google Scholar]
- 4.Boukhvalova M, McKay J, Mbaye A, Sanford-Crane H, Blanco JC, Huber A, Herold BC. Efficacy of the herpes simplex virus 2 (HSV-2) glycoprotein D/AS04 vaccine against genital HSV-2 and HSV-1 infection and disease in the cotton rat sigmodon hispidus model. J Virol. 2015;89(19):9825–9840. doi: 10.1128/JVI.01387-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Srivastava R, Khan AA, Huang J, Nesburn AB, Wechsler SL, BenMohamed L. A herpes simplex virus type 1 human asymptomatic CD8+ T-cell epitopes-based vaccine protects against ocular herpes in a "Humanized" HLA transgenic rabbit model. Invest Ophthalmol Vis Sci. 2015;56(6):4013–4028. doi: 10.1167/iovs.15-17074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tregoning JS, Kinnear E. Using plasmids as DNA vaccines for infectious diseases. Microbiology Spectrum. 2014;2(6) doi: 10.1128/microbiolspec.PLAS-0028-2014. [DOI] [PubMed] [Google Scholar]
- 7.Arce-Fonseca M, Rios-Castro M, Carrillo-Sanchez Sdel C, Martinez-Cruz M, Rodriguez-Morales O. Prophylactic and therapeutic DNA vaccines against Chagas disease. Parasit Vectors. 2015;8:121. doi: 10.1186/s13071-015-0738-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hannaman D, Dupuy LC, Ellefsen B, Schmaljohn CS. A Phase 1 clinical trial of a DNA vaccine for Venezuelan equine encephalitis delivered by intramuscular or intradermal electroporation. Vaccine. 2016;34(31):3607–3612. doi: 10.1016/j.vaccine.2016.04.077. [DOI] [PubMed] [Google Scholar]
- 9.Kim SW, Goedegebuure P, Gillanders WE. Mammaglobin-A is a target for breast cancer vaccination. Oncoimmunology. 2016;5(2):e1069940. doi: 10.1080/2162402X.2015.1069940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gach JS, Gorlani A, Dotsey EY, Becerra JC, Anderson CT, Berzins B, Felgner PL, Forthal DN, Deeks SG, Wilkin TJ, Casazza JP, Koup RA, Katlama C, Autran B, Murphy RL, Achenbach CJ. HIV-1-specific antibody response and function after DNA prime and recombinant adenovirus 5 boost HIV vaccine in HIV-infected subjects. PLoS One. 2016;11(8):e0160341. doi: 10.1371/journal.pone.0160341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hu K, He X, Yu F, Yuan X, Hu W, Liu C, Zhao F, Dou J. Immunization with DNA vaccine expressing herpes simplex virus type 1 gD and IL-21 protects against mouse herpes keratitis. Immunol Invest. 2011;40(3):265–278. doi: 10.3109/08820139.2010.534219. [DOI] [PubMed] [Google Scholar]
- 12.Rey FA. Molecular gymnastics at the herpesvirus surface. EMBO Rep. 2006;7(10):1000–1005. doi: 10.1038/sj.embor.7400807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ghiasi H, Bahri S, Nesburn AB, Wechsler SL. Protection against herpes simplex virus-induced eye disease after vaccination with seven individually expressed herpes simplex virus 1 glycoproteins. Invest Ophthalmol Vis Sci. 1995;36(7):1352–1360. [PubMed] [Google Scholar]
- 14.Friedman HM. Immune evasion by herpes simplex virus type 1, strategies for virus survival. Trans Am Clin Climatol Assoc. 2003;114:103–112. [PMC free article] [PubMed] [Google Scholar]
- 15.Ghebrehiwet B. The complement system: an evolution in progress. F1000Res. 2016;5:2840. doi: 10.12688/f1000research.10065.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eisenberg RJ, Ponce de Leon M, Friedman HM, Fries LF, Frank MM, Hastings JC, Cohen GH. Complement component C3b binds directly to purified glycoprotein C of herpes simplex virus types 1 and 2. Microb Pathog. 1987;3(6):423–435. doi: 10.1016/0882-4010(87)90012-x. [DOI] [PubMed] [Google Scholar]
- 17.Kostavasili I, Sahu A, Friedman HM, Eisenberg RJ, Cohen GH, Lambris JD. Mechanism of complement inactivation by glycoprotein C of herpes simplex virus. J Immunol. 1997;158(4):1763–1771. [PubMed] [Google Scholar]
- 18.Altgarde N, Eriksson C, Peerboom N, Phan-Xuan T, Moeller S, Schnabelrauch M, Svedhem S, Trybala E, Bergstrom T, Bally M. Mucin-like region of herpes simplex virus type 1 attachment protein glycoprotein C (gC) modulates the virus-glycosaminoglycan interaction. J Biol Chem. 2015;290(35):21473–21485. doi: 10.1074/jbc.M115.637363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chang YJ, Jiang M, Lubinski JM, King RD, Friedman HM. Implications for herpes simplex virus vaccine strategies based on antibodies produced to herpes simplex virus type 1 glycoprotein gC immune evasion domains. Vaccine. 2005;23(38):4658–4665. doi: 10.1016/j.vaccine.2005.04.034. [DOI] [PubMed] [Google Scholar]
- 20.Judson KA, Lubinski JM, Jiang M, Chang Y, Eisenberg RJ, Cohen GH, Friedman HM. Blocking immune evasion as a novel approach for prevention and treatment of herpes simplex virus infection. J Virol. 2003;77(23):12639–12645. doi: 10.1128/JVI.77.23.12639-12645.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Awasthi S, Lubinski JM, Friedman HM. Immunization with HSV-1 glycoprotein C prevents immune evasion from complement and enhances the efficacy of an HSV-1 glycoprotein D subunit vaccine. Vaccine. 2009;27(49):6845–6853. doi: 10.1016/j.vaccine.2009.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Awasthi S, Lubinski JM, Shaw CE, Barrett SM, Cai M, Wang F, Betts M, Kingsley S, Distefano DJ, Balliet JW, Flynn JA, Casimiro DR, Bryan JT, Friedman HM. Immunization with a vaccine combining herpes simplex virus 2 (HSV-2) glycoprotein C (gC) and gD subunits improves the protection of dorsal root ganglia in mice and reduces the frequency of recurrent vaginal shedding of HSV-2 DNA in guinea pigs compared to immunization with gD alone. J Virol. 2011;85(20):10472–10486. doi: 10.1128/JVI.00849-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lawson LB, Freytag LC, Clements JD. Use of nanocarriers for transdermal vaccine delivery. Clin Pharmacol Ther. 2007;82(6):641–643. doi: 10.1038/sj.clpt.6100425. [DOI] [PubMed] [Google Scholar]
- 24.Khatri K, Goyal AK, Vyas SP. Potential of nanocarriers in genetic immunization. Recent Pat Drug Deliv Formul. 2008;2(1):68–82. doi: 10.2174/187221108783331348. [DOI] [PubMed] [Google Scholar]
- 25.Elieh-Ali-Komi D, Hamblin MR. Chitin and chitosan: production and application of versatile biomedical nanomaterials. Int J Adv Res (Indore) 2016;4(3):411–427. [PMC free article] [PubMed] [Google Scholar]
- 26.Poecheim J, Patrulea V, Reichert C, Borchard G. Characterization of pDNA-TMC nanoparticle interaction and stability. Curr Drug Deliv. 2016;13(3):301–308. doi: 10.2174/156720181303160520191305. [DOI] [PubMed] [Google Scholar]
- 27.Hu K, Malla T, Zhai Y, Dong L, Tang R. Topical administration is a promising inoculating route versus intramuscular inoculation for the nanoparticle-carried DNA vaccine to prevent corneal infections. Ophthalmic Res. 2015;55(2):99–110. doi: 10.1159/000441898. [DOI] [PubMed] [Google Scholar]
- 28.Almeida AJ, Alpar HO. Nasal delivery of vaccines. J Drug Target. 1996;3(6):455–467. doi: 10.3109/10611869609015965. [DOI] [PubMed] [Google Scholar]
- 29.Bento D, Staats HF, Goncalves T, Borges O. Development of a novel adjuvanted nasal vaccine: C48/80 associated with chitosan nanoparticles as a path to enhance mucosal immunity. Eur J Pharm Biopharm. 2015;93:149–164. doi: 10.1016/j.ejpb.2015.03.024. [DOI] [PubMed] [Google Scholar]
- 30.Inoue T, Inoue Y, Nakamura T, Yoshida A, Takahashi K, Inoue Y, Shimomura Y, Tano Y, Fujisawa Y, Aono A, Hayashi K. Preventive effect of local plasmid DNA vaccine encoding gD or gD-IL-2 on herpetic keratitis. Invest Ophthalmol Vis Sci. 2000;41(13):4209–4215. [PubMed] [Google Scholar]
- 31.Friedman HM, Wang L, Fishman NO, Lambris JD, Eisenberg RJ, Cohen GH, Lubinski J. Immune evasion properties of herpes simplex virus type 1 glycoprotein gC. J Virol. 1996;70(7):4253–4260. doi: 10.1128/jvi.70.7.4253-4260.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lubinski JM, Wang L, Soulika AM, Burger R, Wetsel RA, Colten H, Cohen GH, Eisenberg RJ, Lambris JD, Friedman HM. Herpes simplex virus type 1 glycoprotein gC mediates immune evasion in vivo. J Virol. 1998;72(10):8257–8263. doi: 10.1128/jvi.72.10.8257-8263.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]