Highlights
-
•
The longus colli muscle is situated on the anterior surface of C1-C2 disk space.
-
•
Calcific tendinitis of the longus colli muscle is a reactive self-limiting inflammatory response to the subacute deposition of calcium hydroxyapatite crystals on the tendon of the muscle.
-
•
The clinical presentation is usually mistaken with other serious conditions, such as a retropharyngeal abscess, disk herniation, neck tumor or trauma.
-
•
The importance of recognizing this pathology lies in preventing its misdiagnosis and mismanagement.
-
•
This condition is usually managed conservatively with nonsteroidal anti-inflammatory drugs (NSAIDs).
Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging; NSAID, non-steroidal anti-inflammatory drug
Keywords: Neck pain, Odynophagia, Acute longus colli calcific tendinitis, Acute calcific prevertebral tendinitis, Retropharyngeal tendinitis
Abstract
Introduction
Acute calcific longus colli tendinitis, also known as retropharyngeal or acute calcific prevertebral tendinitis, is a reactive self-limiting inflammatory response to acute or subacute deposition of amorphous calcium hydroxyapatite crystals in the tendons of the longus colli muscle, anterior to the C1–C2 disk space.
Case presentation
A 53-year-old man presented with a complaint of neck pain and odynophagia over a few days. Blood test findings showed mild leukocytosis and elevated C-reactive protein level. Computed tomography findings showed mild edematous prevertebral thickening involving the retropharyngeal space, predominantly on the left side, with no appreciable surrounding peripheral enhancement. A small amount of linear calcification/ossification involving the superior fibers of the left longus colli muscle, anterior to the C1 arch were also noted.
Discussion
The patient’s presentation could be easily misdiagnosed as a retropharyngeal abscess. However, the presence of subtle findings on CT would lead to the correct diagnosis. The management of this condition is mainly with nonsteroidal anti-inflammatory drugs.
Conclusion
This study presents the characteristic radiological features of retropharyngeal calcific tendinitis. These features are subtle and could be missed. Once an accurate diagnosis is made, treatment with nonsteroidal anti-inflammatory drugs is indicated. The purpose of this case report is to highlight this rare condition’s diagnosis and management.
1. Introduction
Acute longus colli calcific tendinitis, also known as retropharyngeal tendinitis, is a self-limiting condition resulting from deposition of amorphous calcium hydroxyapatite crystals in the tendons of the longus colli muscle. Although the deposition typically occurs anterior to the C1–C2 disk space, it can also be seen at other vertebral levels (C4–C5 or C5–C6) [1]. The clinical presentation of this condition is usually mistaken with that of other serious conditions such as retropharyngeal abscess, disk herniation, neck tumor, and trauma. Symptoms include neck stiffness, odynophagia, limited cervical rotational range of motion, mild fever, trismus, and/or neck pain/swelling. Retropharyngeal tendinitis is presumed to originate from a noninfectious inflammatory response in the superior oblique tendons of the longus colli muscle secondary to calcium hydroxyapatite crystal deposition. The arrangement of these muscle tendons—which extend from the upper mediastinum at the level of T2 to the anterior tubercle of the atlas—places them in the vicinity of the prevertebral cervical space [2], [3], [4].
The importance of recognizing this pathology lies in preventing misdiagnosis of retropharyngeal abscess, which could result in unnecessary surgical intervention instead of conservative measures. Here, we present a case of acute calcific longus colli tendinitis in a 53-year-old patient, with the aim of describing the characteristic radiological features of this condition. This case report has been prepared in compliance with the SCARE criteria [1].
2. Case presentation
A 53-year-old man who was otherwise healthy and had no drug allergies presented at the emergency room with sudden onset of progressively worsening left-sided neck pain and odynophagia, which did not initially improve despite treatment with flexeril (cyclobenzaprine 10 mg three times a day), percocet, and cefixime (400 mg two times a day) over a week. The patient revisited the emergency department 2 days later with the same complaints and was, therefore, subjected to enhanced computed tomographic (CT) evaluation.
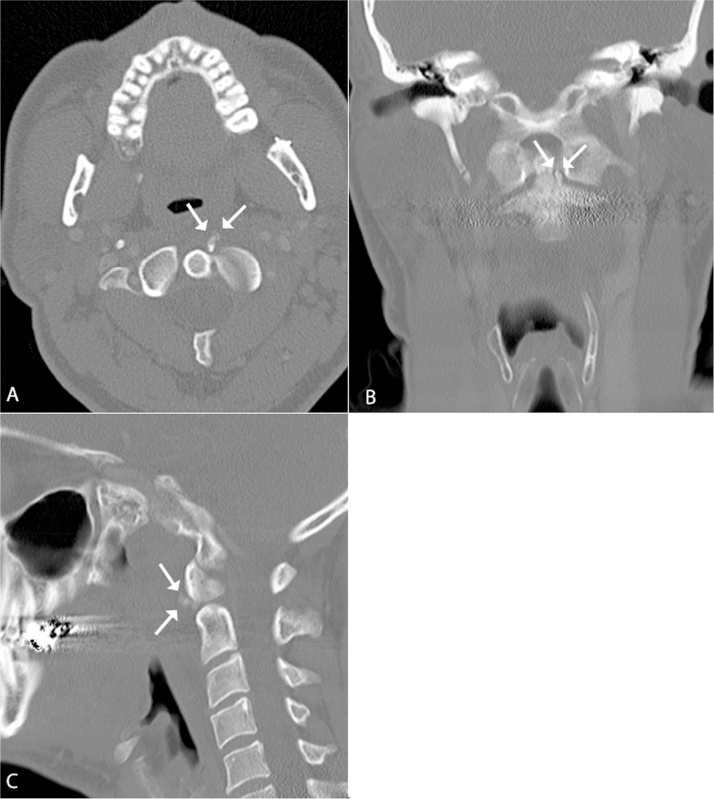
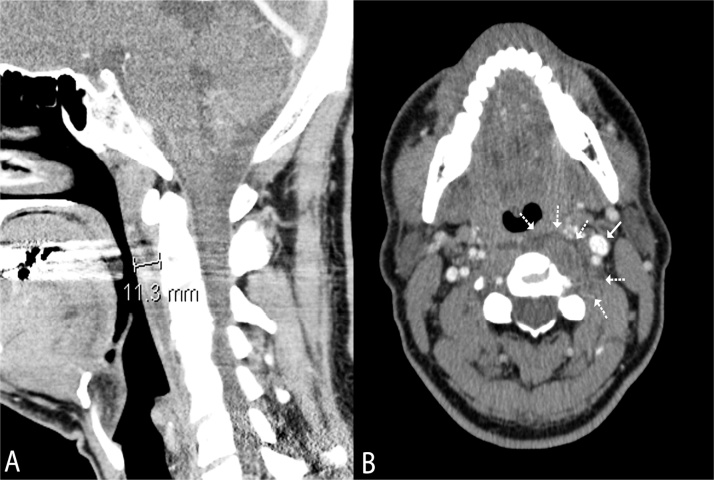
The CT findings demonstrated small amounts of linear calcification/ossification involving the left longus colli muscle, adjacent to the C1 arch as well as the base of the odontoid process of C2 (arrows in Fig. 1A–C). There was no evidence of adjacent intervertebral disc-space narrowing or bony destruction to suggest underlying diskitis. Slightly inferior to this position and predominantly on the left side, there was mild prevertebral thickening and edema involving the retropharyngeal space (Fig. 2A), which tapered inferiorly at the C3–C4 level. There was evidence of obliteration of the left parapharyngeal space, with mild adjacent mass effect on the nasopharynx anteriorly and on the ipsilateral carotid sheath vessels laterally. There was no evidence of venous thrombosis within the bilateral internal jugular veins. The edematous changes described above extended to the right retropharyngeal space as well, with no central gas locules or surrounding peripheral enhancement suggestive of underlying phlegmon or abscess formation (arrows in Fig. 2B).
Fig. 1.
Axial (A), coronal (B), and sagittal (C) enhanced computed tomography images of the neck at the bone window (left to right) demonstrating linear calcifications (white arrows) adjacent to the C1 arch and the odontoid process of C2. Note that there is no evidence of destruction of adjacent vertebral-body bony tissue or narrowing of intervertebral disc space suggestive of underlying diskitis.
Fig. 2.
Sagittal (A) and axial (B) enhanced computed tomography images of the neck at the soft-tissue window (left to right) demonstrating mild prevertebral thickening with edema (dotted white arrows), of up to 1.1-cm thickness. There is mild obliteration of the left parapharyngeal space with mild adjacent mass effect on the nasopharynx and on the left carotid sheath vessels laterally (smooth white arrow). There is no evidence of peripheral enhancement or venous thrombosis suggestive of underlying infection.
At this point, the patient was prescribed a non-steroidal anti-inflammatory drug (NSAID; naproxen). A consult to the otolaryngology service was made to rule out and manage any acute surgical conditions. The main complaint when we examined the patient was limitation of left-sided rotational neck movement. The odynophagia had improved with the pain-control regimen, and the patient had not developed any airway or constitutional symptoms. Physical examination revealed limited cervical rotational range of motion but no neck mass/swelling or pain upon flexion or extension. Oral cavity and oropharyngeal examination findings were normal. The findings of flexible pharyngolaryngoscopy revealed no pharyngeal wall bulging or pus; the uvula was U-shaped, but with no signs of inflammation. The supraglottic structures and vocal folds were normal. Blood analysis findings revealed mildly elevated white blood cell count (13.74 × 109/L) and C-reactive protein level (8.22 mg/L); however, the blood culture results were negative, and there were no other laboratory abnormalities. On the basis of CT findings, the patient was diagnosed with acute longus colli calcific tendinitis and treated conservatively with ibuprofen as needed for 10–14 days. Two weeks later, the family physician of the patient reported complete resolution of neck pain but residual left shoulder pain, for which he scheduled the patient for ultrasonographic evaluation.
3. Discussion
Acute longus colli calcific tendinitis is a reactive self-limiting inflammatory response to acute or subacute deposition of amorphous calcium hydroxyapatite crystals in the tendons of the longus colli muscle at the anterior C1–C2 or other (C4–C6) disk spaces [2], [3], [4]. In 1994, Ring et al. described five cases of calcific retropharyngeal tendinitis and reported that biopsy findings of these lesions revealed an inflammatory response to hydroxyapatite crystal deposition [5].
This pathology has no ethnic overexpression and usually affects young adults between 30 and 60 years of age, with the range of age distribution reported to be between 21 and 80 years [6]. The specific etiology of the condition is not known, but some of the postulated mechanisms involve excessive mechanical trauma in conjunction with existing degenerative cervical spinal diseases, collagen vascular disorders, renal failure, or osteoarthritis, which can result in deposition of calcium crystals in muscle tendons [7], [8].
In a literature review, Park et al. reported that the most common symptoms of acute longus colli calcific tendinitis were neck pain in 94%, limited range of neck motion and odynophagia in 45%, neck stiffness in 42%, dysphagia in 27%, sore throat in 17%, and neck spasm in 11% of cases. Laboratory findings include slightly elevated white blood cell count, erythrocyte sedimentation rate, and C-reactive protein levels [7], [9], [10].
Computed tomography is the gold standard for diagnosis of retropharyngeal tendinitis, since it can detect both prevertebral edema and calcium hydroxyapatite crystal deposition in longus colli tendons; in contrast, magnetic resonance imaging (MRI) can detect prevertebral edema and fluid effusion but not calcium deposits. Thus, CT is more sensitive than MRI for diagnosis of prevertebral calcification. In addition, CT is the most sensitive radiological method for distinguishing retropharyngeal abscess from retropharyngeal tendinitis [5], [9], [11], [12]. The latter condition presents typical radiological findings such as calcific deposits anterior to C1–C2 and prevertebral soft-tissue swelling. Although diffuse prevertebral soft-tissue thickening typically extends from C1 to C4, it can extend as far below as C6 [13].
Calcific retropharyngeal tendonitis is a self-limiting, benign disease that rarely requires hospitalization. Successful treatment can be achieved by medication with NSAIDs and supportive care. Although patients will usually notice instant improvement with the NSAIDs in 48–72 h, recovery could sometimes take up to 2 weeks, and calcium deposits normally resolve in a couple of weeks. If symptoms are severe, a course of corticosteroid treatment can be implemented [14], [15].
4. Conclusion
In conclusion, calcific retropharyngeal tendonitis is thought to be a self-limiting condition that resolves spontaneously after 1–2 weeks of treatment with anti-inflammatory medications, analgesics, and rest. To this end, accurate diagnosis should be made—while avoiding invasive examinations and surgical intervention—in order to rule out life-threatening conditions, especially retropharyngeal abscess.
Competing interests
None.
Funding source
None.
Ethical approval
Not applicable.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Uthman Alamoudi Ahmed Alsayed and Yasser Alsallumi: collected data, wrote article and perform literature review; Mathew Rigby, Robert Hart, S. Mark Taylor and Jonathan Trites: designed study, revised article.
Guarantor
Uthman Alamoudi.
References
- 1.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., the SCARE group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 2.Boikov A.S., Griffith B., Stemer M., Jain R. Acute calcific longus colli tendinitis: an unusual location and presentation. Arch. Otolaryngol.–Head Neck Surg. 2012;138(July (7)):676–679. doi: 10.1001/archoto.2012.910. [DOI] [PubMed] [Google Scholar]
- 3.Hartley J. Acute cervical pain associated with retropharyngeal calcium deposit. A case report. J. Bone Joint Surg. Am. 1964;46:1753–1754. [PubMed] [Google Scholar]
- 4.Silva C.F., Soffia P.S., Pruzzo E. Acute prevertebral calcific tendinitis: a source of non-surgical acute cervical pain. Acta Radiol. 2014;55:91–94. doi: 10.1177/0284185113492151. [DOI] [PubMed] [Google Scholar]
- 5.Zibis A.H., Giannis D., Malizos K.N., Kitsioulis P., Arvanitis D.L. Acute calcific tendinitis of the longus colli muscle: case report and review of the literature. Eur. Spine J. 2013;22(Suppl. 3):S434–8. doi: 10.1007/s00586-012-2584-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ring D., Vaccaro A.R., Scuderi G., Pathria M.N., Garfin S.R. Acute calcific retropharyngeal tendinitis. J. Bone Joint Surg. 1994;76:1636–1642. doi: 10.2106/00004623-199411000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Kaplan M.J., Eavey R.D. Calcific tendinitis of the longus colli muscle. Ann. Otol. Rhinol. Laryngol. 1984;93:215–219. doi: 10.1177/000348948409300305. [DOI] [PubMed] [Google Scholar]
- 8.Gabra N., Belair M., Ayad T. Retropharyngeal calcific tendinitis mimicking a retropharyngeal phlegmon. Case Rep. Otolaryngol. 2013;2013:912628. doi: 10.1155/2013/912628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oliva F., Via A., Maffulli N. Physiopathology of intratendinous calcific deposition. BMC Med. 2012;10:95. doi: 10.1186/1741-7015-10-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Park R., Halpert D.E., Baer A., Kunar D., Holt P.A. Retropharyngeal calcific tendinitis: case report and review of the literature. Semin. Arthritis Rheum. 2010;39:504–509. doi: 10.1016/j.semarthrit.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 11.Mihmanli I., Karaarslan E., Kanberoglu K. Inflammation of vertebral bone associated with acute calcific tendonitis of the longus colli muscle. Neuroradiology. 2001;43:1098–1101. doi: 10.1007/s002340100644. [DOI] [PubMed] [Google Scholar]
- 12.Razon R.V., Nasir A., Wu G.S., Soliman M., Trilling J. Retropharyngeal calcific tendonitis: report of two cases. J. Am. Board Fam. Med. 2009;22:84–88. doi: 10.3122/jabfm.2009.01.080034. [DOI] [PubMed] [Google Scholar]
- 13.Omezzine S.J., Hafsa C., Lahmar I., Driss N., Hamza H. Calcific tendinitis of the longus colli: diagnosis by CT. Joint Bone Spine. 2008;75:90–91. doi: 10.1016/j.jbspin.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 14.Fahlgren H. Retropharyngeal tendinitis. Cephalalgia. 1986;6:169–174. doi: 10.1046/j.1468-2982.1986.0603169.x. [DOI] [PubMed] [Google Scholar]
- 15.Tezuka F., Sakai T., Miyagi R., Takata Y., Higashino K., Katoh S. Complete resolution of a case of calcific tendinitis of the longus colli with conservative treatment. Asian Spine J. 2014;8:675–679. doi: 10.4184/asj.2014.8.5.675. [DOI] [PMC free article] [PubMed] [Google Scholar]