Highlights
-
•
A rare case of metachronous mediastinal lymph node metastasis from colon cancer.
-
•
Resection of mediastinal lymph node metastasis may lead to an improved prognosis.
-
•
We summarize our case and 6 cases previously reported in the English literature.
Keywords: Colorectal cancer, Mediastinal lymph node metastasis, Surgery
Abstract
Introduction
Metachronous mediastinal lymph node metastasis without pulmonary metastasis is extremely rare in colorectal cancer, which makes the clinical diagnosis difficult and treatment strategy unclear.
Prsentation of case
A case was a 59-year-old man, who had undergone right hemicolectomy for ascending colon cancer 2 years and 8 months previously, presented with enlarged mediastinal lymph nodes. 18F-fluorodeoxyglucose (FDG) positron emission tomography revealed FDG was accumulated only into the mediastinal lymph nodes. Serum carcinoembryonic antigen (CEA) level was within the normal range. Six months later, the size and FDG uptake of the mediastinal lymph nodes had increased. We assumed a possibility that the mediastinal lymph nodes were metastasized from ascending colon cancer and so performed thoracoscopic-assisted resection of the mediastinal lymph nodes. Histopathological analysis revealed the resected lymph nodes were filled with moderately differentiated adenocarcinoma and a diagnosis of mediastinal lymph nodes metastasis from previously-resected ascending colon cancer was made. The patient was postoperatively followed for more than 1 year and 8 months without any sign of recurrence.
Discussion
Only 7 cases of metachronous mediastinal lymph node metastasis from colorectal cancer, including our case, have been reported in the English literature. It is difficult to clinically diagnose mediastinal lymph node metastasis.
Conclusion
We report a rare case of metachronous mediastinal lymph node metastasis from ascending colon cancer with literature review. If the mediastinal lymph nodes are enlarged after colorectal cancer resection, we need to make a treatment strategy as well as a diagnostic approach considering the possibility of mediastinal lymph node metastasis.
1. Introduction
The primary sites of metastasis from colorectal cancer are the liver, lung, bone, and brain [1]. Mediastinal lymph node metastasis from colorectal cancer is extremely rare, which makes the clinical diagnosis difficult and treatment strategy unclear. We report a rare case of metachronous mediastinal lymph node metastasis from ascending colon cancer. We also summarize our case and 6 cases previously reported in the English literature. This work has been reported in line with the SCARE criteria [2].
2. Presentation of case
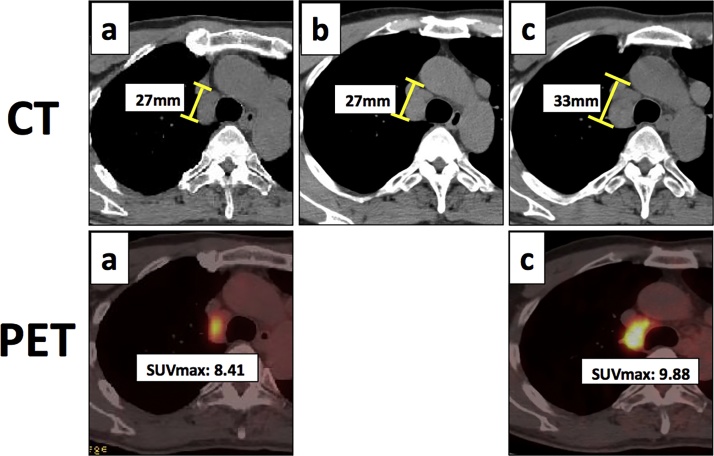
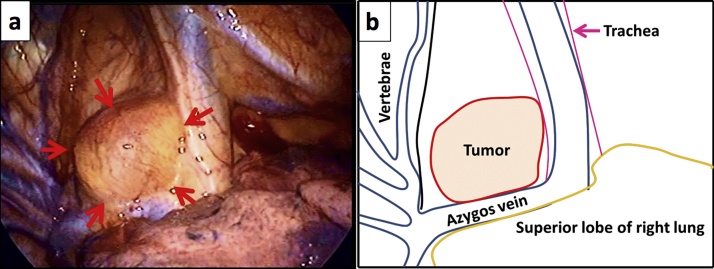
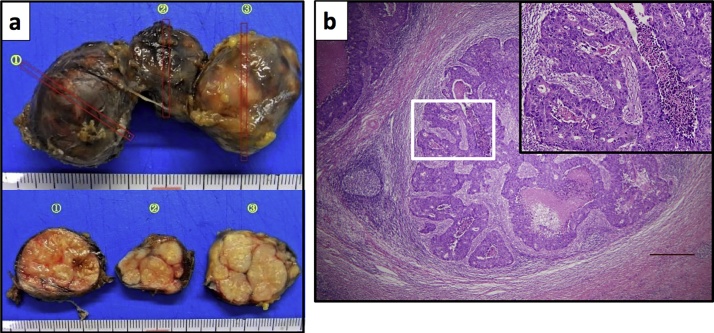
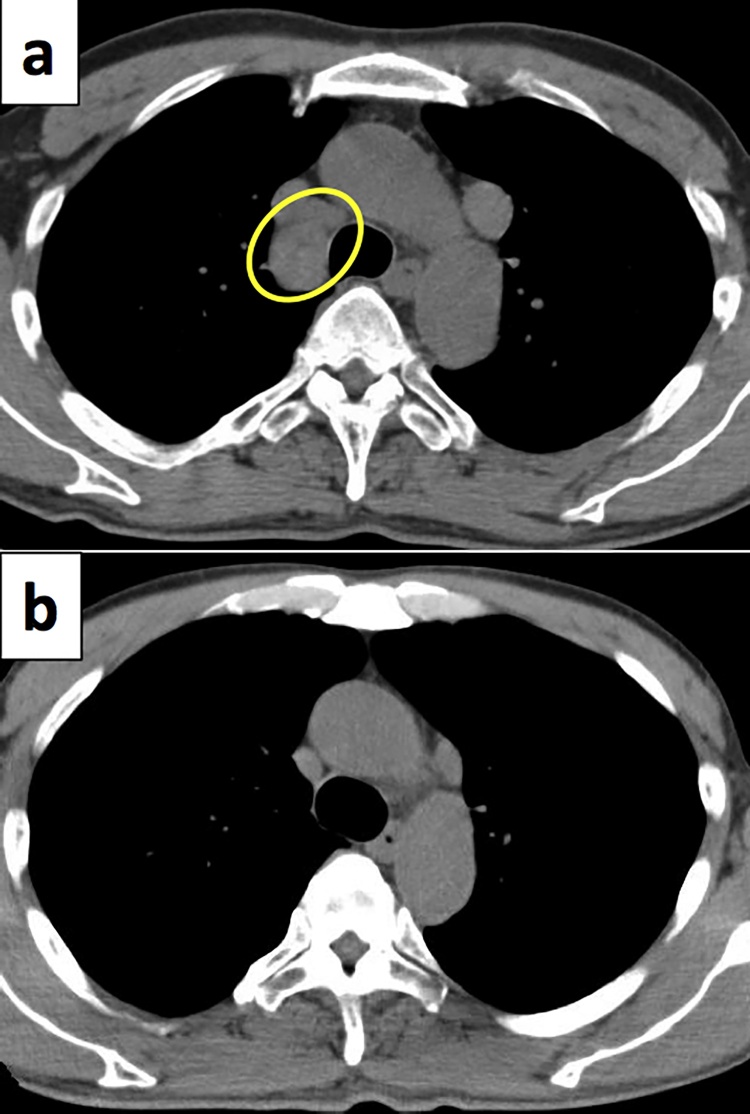
A 56-year-old man underwent right hemicolectomy for ascending colon cancer. Histopathological analysis revealed that the primary colon cancer was a moderately differentiated adenocarcinoma with lymphovascular invasion: pT3, pN1, pM0, ly1, v1, and pStage IIIB. The patient was followed without adjuvant chemotherapy. Two years and 8 months later, a follow-up computed tomography (CT) scan showed bulky, swollen mediastinal lymph nodes with no evidence of a pulmonary mass. The serum carcinoembryonic antigen (CEA) level (1.1 ng/ml) was within the normal range. 18F-fluorodeoxyglucose (FDG) positron emission tomography showed that FDG was accumulated only into the mediastinal lymph nodes. (Fig. 1a). The size and maximum standardized uptake value (SUVmax) of the mediastinal lymph nodes were 27 mm and 8.41, respectively. At this stage, we could not determine whether the mediastinal lymph nodes were malignant or not. Therefore, we decided to continue the follow-up every 3 months. Three months later, CT scan showed the size of the mediastinal lymph nodes was almost unchanged (Fig. 1b). Therefore, we suspected the swollen mediastinal lymph nodes were not malignant but non-specific. However, six months later, FDG-PET/CT scan showed the size and SUVmax of the mediastinal lymph nodes had increased to 33 mm and 9.88, respectively (Fig. 1c). There was no other abnormal FDG uptake in the rest of the body (data not shown). The serum CEA level (1.89 ng/ml) remained within the normal range. Due to the time-course change over the previous 6 months, we suspected that the mediastinal lymph nodes were metastasized from the ascending colon cancer and so performed thoracoscopic-assisted resection of the mediastinal lymph nodes (Fig. 2a and b). Macroscopic findings of the resected specimen showed a cluster of three solid masses, measuring 85 × 35 × 30 mm in size (Fig. 3a). Histopathological analysis revealed that the lymph nodes were filled with moderately differentiated adenocarcinoma in a cribriform pattern (Fig. 3b), which was completely consistent with the histopathological features of the primary colon cancer. Taken together, we diagnosed that the patient presented the metachronous mediastinal lymph node metastasis from colon cancer. The patient has been followed for more than 1 years and 8 months without any signs of recurrence (Fig. 4a and b).
Fig. 1.
18F-fluorodeoxyglucose positron emission tomography (FDG-PET) and computed tomography (CT).
(a) First detected mediastinal lymph nodes. (b) 3 months later, CT scan showed that the size of mediastinal lymph nodes was almost unchanged. (c) 6 months later, the size and the maximum standardized uptake value (SUVmax) of mediastinal lymph nodes had increased.
Fig. 2.
Intraoperative finding.
(a) Thoracoscopic image in the left lateral decubitus position. Tumor(arrows).
(b) Schema of (a).
Fig. 3.
Histopathological findings of resected specimen.
(a) Resected specimen. (b) Lymph nodes were filled with moderately differentiated adenocarcinoma in cribriform pattern. H&E, x40, scale bar: 500 μm. An insert shows a higher magnification of the boxed area.
Fig. 4.
Computed tomography at both preoperation and 1 year and 4 months after operation.
(a) Mediastinal lymph nodes at preoperation(yellow circle). (b) 1 year and 4 months later, there was no evidence of recurrence.
3. Discussion
Colorectal cancer is one of the most common causes of cancer-related death. Tumor recurrence is often observed in distant organs, but curative surgical resection may be a treatment option for selected patients [3]. Mediastinal lymph node metastasis is quite rare in colorectal cancer without lung metastasis. In fact, including the current case, only 7 cases of metachronous mediastinal lymph node metastasis from colorectal cancer have been reported in the English literature (Table 1) [4], [5], [6], [7], [8]. The location of primary colorectal cancer was consisted of ascending colon (n = 2), sigmoid colon (n = 2), and rectum (n = 3). In all cases, the mediastinal lymph node metastasis occurred more than 2 years after resection of the primary cancer.
Table 1.
Description of metachronous mediastinal lymph node metastasis cases from colorectal cancer.
| Case No. | Reference | Age | Sex | Primary location | Primary stage | CEA | FDG-PET | Time after primary resection (months) | Treatment | Follow-up period (months) | Recurrence |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Kuba et al. [4] | 60 | F | sigmoid | IIIB | elevated | NL | 33 | resection | NL | NL |
| 2 | Iwata et al. [5] | 75 | M | ascending | IIIA | elevated | uptake | 42 | resection | 13 | none |
| 3 | Musallam et al. [6] | 67 | M | rectum | IIIB | normal | uptake | 26 | NL | NL | NL |
| 4 | Matsuda et al. [7] | 65 | M | sigmoid | IIIB | normal | uptake | 101 | resection | 72 | none |
| 5 | Matsuda et al. [7] | 50 | M | rectum | IIIB | elevated | uptake | 96 | resection | 4 | none |
| 6 | Shirakawa et al. [8] | 65 | M | rectum | IIIA | elevated | uptake | 55 | resection | NL | NL |
| 7 | Our case, 2016 | 59 | M | ascending | IIIB | normal | uptake | 32 | resection | 20 | none |
CEA: carcinoembryonic antigen.
FDG-PET: 18F-fluorodeoxyglucose positron emission tomography.
NL: not listed.
The pathway by which cancer cells metastasized from ascending colon to mediastinal lymph nodes is unclear. The lymphatics of colon flows into the thoracic duct, but there is no direct communication between the thoracic duct and bronchomediastinal trunk [9]. MacLoud et al. reported that the reflux of tumor emboli from the thoracic duct into the bronchomediastinal trunk might occur by incompetent valves of lymphatics [10].
It is difficult to clinically diagnose mediastinal lymph node metastasis. All of the previously reported cases were asymptomatic and the serum CEA levels were not necessarily elevated (Table 1). FDG uptake was observed in 6 of 7 cases to date (85.7%). However, it was reported that false-positive FDG uptake in the mediastinal lymph nodes was found on FDG-PET [11]. The sensitivity of FDG-PET in the detection of mediastinal lymph node metastasis in pulmonary metastasis of colorectal cancer is only 35% [12]. FDG-PET is useful to clarify the localization and extent of metastasis, although it cannot distinguish between metastasis and other diseases. We continued follow-up for a further 6 months in order to determine if the lymph node swelling was due to malignancy. Six months later, the size and FDG uptake of the mediastinal lymph nodes had increased; therefore, we performed mediastinal lymph node resection. Enlarged mediastinal lymph nodes may indicate malignant disease.
In the previous reports, there were no recurrence after mediastinal lymph node resection despite small number of cases (Table 1). A systematic review reported that the median overall survival and median disease-free survival in patients who underwent curative surgical resection for retroperitoneal nodal recurrence were 34–44 months and 17–21 months, respectively [13]. The mediastinal lymph nodes are distant organs in primary colorectal cancer, but resectable mediastinal lymph node metastasis can also be associated with a better prognosis. In our case, postoperative adjuvant chemotherapy was administered at the patient’s request, although there is still no standard treatment and the efficacy of the postoperative adjuvant chemotherapy after metastasectomy of colorectal cancer remains controversial [14].
4. Conclusion
We report a case of mediastinal lymph metastasis with a review of the literature. Mediastinal lymph node metastasis of colorectal cancer is extremely rare. If enlarged mediastinal lymph nodes are detected after colorectal cancer resection, we need to make a treatment strategy as well as a diagnostic approach considering the possibility of mediastinal lymph node metastasis. Surgical resection of mediastinal lymph node metastasis may lead to an improved prognosis.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Funding
None.
Ethics approval and consent to participate
Not applicable.
Consent
Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of the journal.
Authors’ contributions
KT and HI participated in the surgery. KT analyzed and interpreted the patient data. KT and KK were major contributors in writing the manuscript. YS gave the useful comment of this manuscript. All authors read and approved the final manuscript.
Guarantor
Kosuke Toda and Kenji Kawada are the guarantor.
Contributor Information
Kosuke Toda, Email: kotoda@kuhp.kyoto-u.ac.jp.
Kenji Kawada, Email: kkawada@kuhp.kyoto-u.ac.jp.
Yoshiharu Sakai, Email: ysakai@kuhp.kyoto-u.ac.jp.
Hiroshi Izumi, Email: cbi77140@pop02.odn.ne.jp.
References
- 1.Eisenberg B., Decosse J.J., Harford F., Michalek J. Carcinoma of the colon and rectum: the natural history reviewed in 1704 patients. Cancer. 1982;49:1131–1134. doi: 10.1002/1097-0142(19820315)49:6<1131::aid-cncr2820490611>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 2.Agha R.A., Fowler A.J., Saeta A., Barai I., Rajmohan S., Orgill D.P. The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 3.Ribeiro Gomes J., Belotto M., D'Alpino Peixoto R. The role of surgery for unusual sites of metastases from colorectal cancer: a review of the literature. Eur. J. Surg. Oncol. 2017;43:15–19. doi: 10.1016/j.ejso.2016.05.019. [DOI] [PubMed] [Google Scholar]
- 4.Kuba H., Sato N., Uchiyama A., Nakafusa Y., Mibu R., Yoshida K., Kuroiwa K. Mediastinal lymph node metastasis of colon cancer: report of a case. Surg. Today. 1999;29:375–377. doi: 10.1007/BF02483068. [DOI] [PubMed] [Google Scholar]
- 5.Iwata T., Chung K., Hanada S., Toda M., Nakata K., Kato T., Miura T. Solitary bulky mediastinal lymph node metastasis from colon cancer. Ann. Thorac. Cardiovasc. Surg. 2013;19:313–315. doi: 10.5761/atcs.cr.12.01998. [DOI] [PubMed] [Google Scholar]
- 6.Musallam K.M., Taher A.T., Tawil A.N., Chakhachiro Z.I., Habbal M.Z., Shamseddine A.I. Solitary mediastinal lymph node metastasis in rectosigmoid carcinoma: a case report. Cases J. 2008;1:69. doi: 10.1186/1757-1626-1-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Matsuda Y., Yano M., Miyoshi N., Noura S., Ohue M., Sugimura K., Motoori M. Solitary mediastinal lymph node recurrence after curative resection of colon cancer. World J. Gastrointest. Surg. 2014;6:164–168. doi: 10.4240/wjgs.v6.i8.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shirakawa Y., Noma K., Koujima T., Maeda N., Tanabe S., Ohara T., Fujiwara T. Prone-position thoracoscopic resection of posterior mediastinal lymph node metastasis from rectal cancer. World J. Surg. Oncol. 2015;13:45. doi: 10.1186/s12957-015-0466-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grant T., Levin B. Lymphangiographic visualization of pleural and pulmonary lymphatic in a patient without chylothorax. Radiology. 1974;113:49–50. doi: 10.1148/113.1.49. [DOI] [PubMed] [Google Scholar]
- 10.McLoud T.C., Kalisher L., Stark P., Greene R. Intrathoracic lymph node metastases from extrathoracic neoplasms. AJR Am. J. Roentgenol. 1978;131:403–407. doi: 10.2214/ajr.131.3.403. [DOI] [PubMed] [Google Scholar]
- 11.Tsukada T., Nakano T., Matoba M., Sasaki S., Higashi K. False-Positive mediastinal lymphadenopathy on 18F-fluorodeoxyglucose positron emission tomography and computed tomography after rectal cancer resection: a case report of thoracoscopic surgery in the prone position. Case Rep. Oncol. 2011;4:569–575. doi: 10.1159/000335017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hamaji M., Cassivi S.D., Shen K.R., Allen M.S., Nichols F.C., Deschamps C., Wigle D.A. Is lymph node dissection required in pulmonary metastasectomy for colorectal adenocarcinoma? Ann. Thorac. Surg. 2012;6:1796–1800. doi: 10.1016/j.athoracsur.2012.04.049. [DOI] [PubMed] [Google Scholar]
- 13.Ho T.W., Mack L.A., Temple W.J. Operative salvage for retroperitoneal nodal recurrence in colorectal cancer: a systematic review. Ann. Surg. Oncol. 2011;18:697–703. doi: 10.1245/s10434-010-1322-7. [DOI] [PubMed] [Google Scholar]
- 14.Brandi G., De Lorenzo S., Nannini M., Curti S., Ottone M., Dall'Olio F.G., Barbera M.A. Adjuvant chemotherapy for resected colorectal cancer metastases: literature review and meta-analysis. World J. Gastroenterol. 2016;22:519–533. doi: 10.3748/wjg.v22.i2.519. [DOI] [PMC free article] [PubMed] [Google Scholar]