Abstract
Corticosteroid-binding globulin (CBG) is secreted as high-affinity CBG (haCBG), which may be cleaved by tissue proteases to low-affinity CBG (laCBG), releasing free cortisol. Pregnancy and the estrogen-based combined oral contraceptive pill (COCP) increase CBG concentrations twofold to threefold. The relative effects of these two hyperestrogenic states on the CBG affinity forms are unknown. We performed an observational study in 30 pregnant women, 27 COCP takers and 23 controls. We analyzed circulating total CBG, haCBG, laCBG, and free and total cortisol concentrations. In pregnancy, total CBG and haCBG were increased compared to controls (both P < 0.0001); however, laCBG concentrations were similar. In COCP takers, total CBG and haCBG were increased [802 ± 41 vs compared to controls (both P < 0.0001)], but laCBG was also increased (P = 0.03). Pregnancy and use of COCP were associated with a comparable rise in haCBG, but laCBG was lower in pregnancy (P < 0.0001). These results were consistent with an estrogen-mediated increase in CBG synthesis in both hyperestrogenemic states but with reduced CBG cleavage in pregnancy relative to the COCP, perhaps due to pregnancy-induced CBG glycosylation. Speculatively, increased circulating haCBG concentrations in pregnancy may provide an increased reservoir of CBG-bound cortisol to prepare for the risk of puerperal infection or allow for cortisol binding in the face of competition from increased circulating progesterone concentrations.
Keywords: cortisol, high-affinity CBG, low-affinity CBG, pregnancy, oral contraceptive pill, estrogen
Elevated CBG in pregnancy is due to increased haCBG levels. In women who take the COCP, increased CBG is due to haCBG and laCBG. This discrepancy suggests reduced CBG cleavage in pregnancy, perhaps due to glycosylation.
Pregnancy is associated with profound immune and endocrine changes necessary for allograft tolerance and fetal maturation, including activation of the hypothalamic-pituitary-adrenal (HPA) axis, resulting in sustained physiologic hypercortisolism. Total plasma cortisol, either bound to corticosteroid-binding globulin (CBG) or albumin, as well as free-cortisol concentrations are elevated twofold to threefold in pregnancy [1–7]. The mechanisms for this are not fully resolved but include drive from placental corticotropin-releasing hormone under positive feedback from maternal cortisol, hyper-responsiveness of the adrenal cortex to adrenocorticotropic hormone, and increased adrenocorticotropic hormone secretion [8]. Total plasma CBG concentrations in pregnancy are also elevated twofold to threefold [1–5, 7, 9], as they are in women taking combined oral contraceptive pills (COCPs), which result in supraphysiologic estrogen concentrations [3, 4, 10, 11].
CBG binds 80% to 90% of circulating cortisol; a further 10% is bound to albumin and approximately 5% is free. Free-cortisol concentrations increase exponentially when high total cortisol concentrations saturate CBG; low-affinity binding to albumin may then increase. CBG is able to target the delivery of free cortisol to inflamed tissues. This occurs via neutrophil elastase-mediated cleavage of the exposed reactive center loop of high cortisol-binding affinity CBG (haCBG; Ka = 1.4 × 109 M−1), resulting in the formation of 10-fold lower affinity CBG (laCBG; Ka = 1.6 × 108 M−1) and favoring release of free cortisol at inflammatory sites [12]. We have recently shown that the two forms coexist in the circulation [13]. Patients with sepsis have very low haCBG concentrations [14]. This agrees with in vitro data showing that CBG cleavage can be induced by neutrophil elastase [12]. At the tissue level, CBG cleavage increases the interstitial free-cortisol concentration threefold to fourfold, potentially enhancing cortisol’s immunomodulatory effects [15–17].
CBG is heavily glycosylated, with five of six consensus sites typically occupied by biantennary and triantennary N-linked oligosaccharides in a 3:2 molar ratio [18, 19]. Branching increases significantly during pregnancy, producing pregnancy-specific CBG [20–23]. Glycosylation prolongs CBG half-life [24], alters cortisol-binding affinity, increases thermosensitivity [15], and may impair CBG-receptor interactions, particularly with syncytiotrophoblasts [25, 26].
The effect of pregnancy on CBG affinity forms is unknown. We hypothesized that elevated haCBG concentrations may be present in pregnancy. This may serve as a mechanism to prepare for puerperal sepsis, a leading cause of maternal and fetal morbidity and mortality [27], or allow for CBG binding competition from high progesterone concentrations. Hence, we studied CBG affinity-form concentrations in pregnancy, COCP takers, and nonpregnant women (control subjects).
1. Subjects and Methods
A. Study Participants
We performed a prospective observational study in pregnant women, women taking the COCP, and healthy control subjects at two tertiary centers in Adelaide, Australia, between 2013 and 2015. The protocol was approved by the Women's & Children's Health Network and the Royal Adelaide Hospital Human Research Ethics Committees. Pregnant women were recruited from prenatal outpatient clinics or inpatient wards after admission for delivery; women taking the COCP and healthy control subjects were recruited by local advertising. All provided written informed consent. Inclusion criteria were as follows: pregnant women, women taking an estrogen-based oral contraceptive pill for ≥3 months, or healthy control subjects. Exclusion criteria included active labor, concurrent infection or other acute illness, and use of immunosuppressive drugs, including betamethasone to improve fetal lung maturity. A single blood sample was collected at the time of enrolment. Median times (range) for sample collection were as follows: pregnancy, 10:30 am (8:30 to 11:40 am; n = 13); COCP takers, 2:19 pm (8:30 am to 4:45 pm); and control subjects, 10:40 am (8:20 am to 4:15 pm). For women taking the COCP, samples were taken during the active phase of their pill cycle. Medical and demographic data were also recorded.
B. Laboratory Methods
EDTA plasma from pregnant women and serum from COCP takers and control subjects were stored at −70°C until analyzed. Total cortisol level was measured by electrochemiluminescence immunoassay on a Roche e601 analyzer (Roche Diagnostics, Castle Hill, NSW, Australia). Cortisol samples from control subjects and pregnant women were analyzed by the Elecsys Cortisol I assay (Roche Diagnostics). Cortisol samples from women taking the COCP were analyzed after the switch to the second-generation Elecsys Cortisol II assay (Roche Diagnostics). Accordingly, a conversion factor was applied to COCP cortisol samples, using a Passing-Bablock fit equation (i.e., 0.9 + 0.78x). This equation was derived from internal validation analysis of 67 samples (range, 2.7 to 1175 nmol/L) and is similar to published data [28]. The fraction of free cortisol was determined using a temperature-controlled ultrafiltration/ligand-binding method [14] validated against equilibrium dialysis. Free-cortisol level was calculated from total cortisol level and free-cortisol fractions. The purpose of total and free-cortisol measurement was to assess a change in the free fraction in relation to changes in haCBG concentration, not to provide an assessment of cortisolemia.
Measurement of total and haCBG concentrations via two-site noncompetitive direct enzyme-linked immunosorbent assays was performed as previously validated [13, 29]. Briefly, paired microtiter plates were coated with a polyclonal CBG antibody. After addition of a 1:1000 sample in assay buffer or serially diluted recombinant CBG standard (catalog no. 10998-H08H; Sino Biological Inc. Beijing, China), the plates were treated with either the in-house monoclonal antibody RRID:AB_2632404 or RRID:AB_26632405 to measure total CBG and haCBG concentrations, respectively. Commercial peroxidase-conjugated anti-mouse secondary antibodies were then applied to the respective plates before substrate was added. Absorbance was read at 450 nm and concentrations determined by interpolation from standard curves. The level of laCBG was calculated indirectly [30]. Assays were performed in parallel with samples from two control subjects to ensure validity. Intra-assay coefficients of variation were 5.0% and 2.7% for total and haCBG, respectively.
C. Statistical Analyses
Data were analyzed using GraphPad Prism version 6 for Mac OS X (GraphPad Software, San Diego, CA). Results are presented as mean ± standard error of the mean unless otherwise stated. The D’Agostino-Pearson test was applied to confirm the normal distribution of CBG data. Comparison among three or more groups was performed by one-way analysis of variance with post hoc analysis carried out by Tukey multiple-comparison test. Multiplicity-adjusted P values are reported. Correlations between continuous variables were assessed with the Pearson correlation coefficient. P < 0.05 was taken as statistically significant.
2. Results
Thirty pregnant women, 27 COCP takers, and 23 healthy control subjects, were enrolled; their baseline characteristics are detailed in Table 1. Women taking a COCP were younger than women in other groups (P < 0.05). Four pregnant women were in the second trimester, whereas 26 were in the third trimester. Twenty-one women (78%) taking the COCP were receiving 25 to 35 μg of ethinylestradiol per day. Of the remaining six women, four received 20 μg and two received 50 μg of ethinylestradiol per day.
Table 1.
Baseline Characteristics
| Pregnancy (n = 30) | COCP (n = 27) | Healthy Control Subjects (n = 23) | |
|---|---|---|---|
| Age, y | 31.9 (4.9) | 24.0 (6.0)a | 36.0 (8.8) |
| Gravity | 2.4 (1.5) | ||
| Parity | 1.2 (1.2) | ||
| Mode of deliveryb | |||
| NVD | 12 | ||
| LSCS | 9 | ||
| Gestational age at enrolment, wk | 34.2 (4.5) | ||
| Weight at birth, gc | 3329 (488) |
Data given as mean (standard deviation) unless otherwise indicated.
Abbreviations: LSCS, lower segment cesarean section; NVD, normal vaginal delivery.
P < 0.05 when compared with control subjects.
Data missing for nine patients.
Data missing for 11 patients.
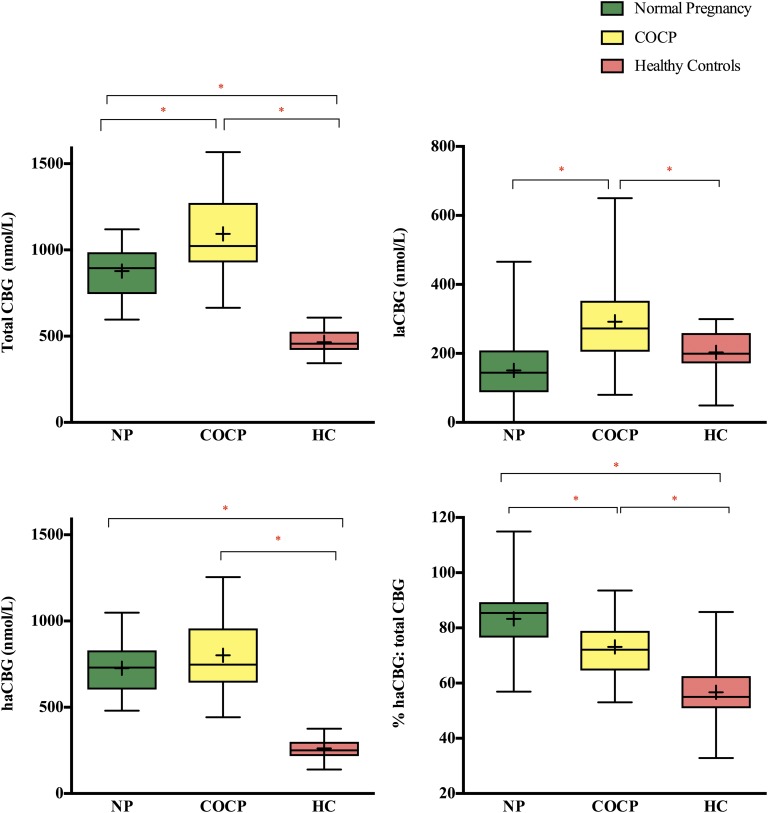
A. CBG in Pregnancy
Total CBG concentrations were greater in pregnant women than control subjects (877 ± 27 vs 466 ± 13 nmol/L; P < 0.0001; Fig. 1). haCBG concentrations were also greater (727 ± 27 vs 262 ± 13 nmol/L; P < 0.0001); however, laCBG concentrations did not differ (151 ± 22 vs 203 ± 14 nmol/L; P = 0.24). The percentage of haCBG to total CBG was significantly higher in pregnant women than in control subjects (83.3% ± 2.3% vs 56.7% ± 2.7%; P < 0.0001).
Figure 1.
Total CBG and haCBG levels and percentage of haCBG to total CBG were higher in pregnant women (n = 30) than in control subjects (n = 23). Women taking the COCP (n = 27) had the highest total CBG, haCBG, and laCBG levels. *P < 0.05 between two groups. The line in each box marks the median; + indicates the mean. Each box extends from the 25th to 75th percentiles; whiskers extend from maximum to minimum. HC, healthy control subjects; NP, normal pregnancy.
B. CBG and the COCP
Women taking the COCP had the highest total CBG concentrations (1093 ± 44 nmol/L; P < 0.0001 vs pregnant and control groups; Fig. 1). haCBG concentrations in women taking the COCP were higher than in control subjects (802 ± 41 nmol/L; P < 0.0001) but similar to that in pregnant women (P = 0.18). The COCP group also had higher concentrations of laCBG than both pregnant women and control subjects (292 ± 27 vs 151 ± 22, P < 0.0001; and 203 ± 14 nmol/L, P = 0.03, respectively). Percentage of haCBG to total CBG was higher in COCP takers compared with that in control subjects (73.1% ± 2.1%; P < 0.0001) but lower compared with pregnant women (P = 0.006).
C. Cortisol in Pregnancy
Total cortisol and free-cortisol concentrations were increased in pregnancy compared with those in control subjects (P < 0.0001 and P = 0.017, respectively; Table 2). The fraction of free cortisol was also increased in pregnant women (P = 0.0003).
Table 2.
Cortisol Levels
| Pregnancy (n = 30) | COCP (n = 27) | Healthy Control Subjects (n = 23) | |
|---|---|---|---|
| Total cortisol, nmol/L | 656 (58)a | 621 (51)a | 319 (34) |
| Free cortisol, nmol/L | 33.8 (3.0)a | 49.7 (4.1)a | 20.0 (2.9) |
| Ratio of free to total cortisol | 5.2 (0.1)a | 8.0 (0.1)a | 6.0 (0.0) |
Data given as mean ± SEM.
P < 0.05 when compared with control subjects.
There was no correlation between CBG affinity-form concentrations and maternal age or gestational age. There was a trend toward higher total cortisol and free-cortisol levels with later gestational age (P = 0.052, r = 0.36; and P = 0.071, r = 0.33, respectively). Total CBG level correlated with total cortisol (P = 0.005; r = 0.5) and free-cortisol levels (P = 0.014; r = 0.440), and with the free-cortisol fraction (P = 0.018; r = −0.43).
D. Cortisol and the COCP
Compared with control subjects, women taking the COCP had higher total cortisol, free cortisol, and fraction of free-cortisol levels (P = 0.0004, P < 0.0001, and P < 0.0001, respectively; Table 2). Total cortisol concentrations were no different compared with those in pregnant women, but free-cortisol level and the fraction of free cortisol were higher in women taking the COCP (P = 0.003 and P < 0.0001, respectively).
Total CBG correlated with total cortisol (P = 0.002; r = 0.58) and free cortisol (P = 0.008; r = 0.5). haCBG correlated with total cortisol (P = 0.021; r = 0.44).
3. Discussion
It is known that total CBG concentrations are elevated in pregnancy [1–5, 7, 9]. We show that this is due to increased uncleaved haCBG. In contrast, COCP use was associated with a comparable rise in haCBG to that during pregnancy; however, cleaved laCBG was also increased. This differential effect on haCBG and laCBG concentrations in pregnancy and the COCP group were consistent with an estrogen-mediated increase in CBG synthesis in both pregnancy and in the COCP group, but with reduced CBG cleavage in pregnancy relative to the COCP group. This may be due to pregnancy-induced CBG glycosylation [20–23].
The threefold elevation in circulating haCBG-cortisol in pregnancy may have a preparatory role to help deal with the risk of puerperal infection. This may be advantageous in reducing sepsis progression, because we have shown that high haCBG concentrations are associated with better prognosis in the cascade of sepsis to septic shock to death in humans [14]. CBG also binds progesterone (Ka = 0.26 × 10−8), which increases 200- to 300-fold during pregnancy and can displace cortisol [2, 6, 31, 32]. Thus, higher levels of haCBG may be necessary to overcome binding competition. The cortisol-progesterone CBG interaction is particularly important at the materno-fetal interface. Here the progesterone-to-cortisol ratio is 75 times higher than in the maternal circulation; thus, intervillous CBG is heavily progesterone laden [33]. Elevated haCBG may also provide a buffer against the increased cortisol concentrations in pregnancy, protecting maternal tissues from excessive free-cortisol exposure.
Estrogen is likely to account for increased total CBG secretion in pregnancy and COCP takers, due to a direct effect on hepatocyte CBG production [34] and perhaps from other sites where CBG gene expression has been determined, including endometrium, ovary, fallopian tube, and placenta [35–38]. Estrogen may also account for sex differences in CBG concentrations: Women have 10% higher total CBG concentrations than men [39–41].
The absence of a corresponding rise in laCBG concentration in pregnancy compared with COCP takers, despite a comparable increase in haCBG concentration, suggests reduced CBG cleavage in pregnancy. This was apparent despite a mild inflammatory state being present in pregnancy [42, 43]. We suggest reduced CBG cleavage in pregnancy may be due to pregnancy-specific glycosylation. The glycosylation site at Asp347 within the reactive center loop cleavage site is normally 80% glycosylated [25]. If specifically hyperglycosylated in pregnancy, it may reduce CBG cleavage.
CBG displays substantial carbohydrate microheterogeneity [34] and, during pregnancy, enhanced oligosaccharide branching is well recognized [20]. The classically described pregnancy-specific variant, containing only triantennary oligosaccharide chains, constitutes 7% to 14% of circulating CBG in pregnancy [44]. Altered CBG glycosylation is thought to affect the interaction of CBG with specific membrane receptors [25, 26, 45]. Specifically, pregnancy-specific variant CBG has a significantly higher binding affinity for syncytiotrophoblast cell membranes than nonpregnant CBG, perhaps facilitating the delivery of maternal cortisol to the fetus or participating in the regulation of placental corticotropin-releasing hormone production [20, 44]. In vitro stimulation of HepG2 cells with estradiol causes an increase in acidic glycoforms of CBG, approximating changes seen in pregnancy [46]. However, reports of in vivo examination of glycoforms present in women exposed to exogenous estrogen, using mass spectrometric techniques [25], are not available.
The maternal HPA axis has an important impact on the fetal HPA axis, with consequent effects in adult life [47, 48]. A CBG mutation, CBG A51V, common in Han Chinese, results in a 30% reduction in circulating total CBG concentrations during pregnancy and is associated with a female-skewed sex ratio in offspring [49]. These observations suggest that CBG elevations in pregnancy are important and, when lacking, may affect fetal survival.
Free cortisol was elevated in both pregnant and COCP groups in this study. However, previous studies using the gold standard of 24-hour urine free-cortisol excretion found no increase in free-cortisol concentrations in women taking the COCP [4]. The single cortisol measurement used here was not intended to provide a measurement of overall cortisolemia in these patients but to determine whether a change in haCBG concentrations related to a change in the free-cortisol fraction, which it did not. We believe the elevated free-cortisol concentrations and free-cortisol fractions seen in young women taking the COCP were an artificial stress effect of venipuncture rather than a reflection of true hypercortisolemia. This effect has been well documented, with up to one-third of patients experiencing a cortisol response to venipuncture [50, 51]. A rest period after intravenous catheter placement may have avoided artifactual hypercortisolemia.
There are data suggesting that CBG can influence the fast actions of cortisol in the brain [52] and CBG has been found in human hypothalamus and cerebrospinal fluid [53, 54]. Hence, CBG may influence feedback in pregnancy; however, to our knowledge, there are no published data on this and further investigation is required.
In conclusion, the rise in total CBG concentrations during pregnancy was due to increased haCBG. The rise in haCBG concentrations in the COCP takers was comparable to that seen in pregnancy; however, laCBG concentration was also increased. These results are consistent with an estrogen-mediated increase in CBG synthesis in both pregnancy and in women taking the COCP, but with reduced CBG cleavage in pregnancy relative to that in women taking the COCP. Increased circulating haCBG concentrations in pregnancy may provide an increased reservoir of CBG-bound cortisol in preparation for the risk of puerperal infection, or they may allow for cortisol binding in the face of competition from high circulating progesterone concentrations.
Acknowledgments
The study was funded by a 2014 Royal Adelaide Hospital/Institute of Medical and Veterinary Science Research Committee Clinical Project Grant and a 2012 Roche/Australian and New Zealand Society of Nephrology Genesis Research Grant. M.A.N. received the Royal Adelaide Hospital/Institute of Medical and Veterinary Science Research Committee 2014 AR Clarkson Fellowship. A.Z. received a Central and Northern Adelaide Renal Transplantation Service Honours Research Scholarship. Funding sources had no role in study design or the collection, analysis, or interpretation of the data.
Disclosure Summary: The authors have nothing to disclose.
Footnotes
- CBG
- corticosteroid-binding globulin
- COCP
- combined oral contraceptive pill
- haCBG
- high-affinity corticosteroid-binding globulin
- HPA
- hypothalamic-pituitary-adrenal
- laCBG
- low-affinity corticosteroid-binding globulin.
References and Notes
- 1.Potter JM, Mueller UW, Hickman PE, Michael CA. Corticosteroid binding globulin in normotensive and hypertensive human pregnancy. Clin Sci (Lond). 1987;72(6):725–735. [DOI] [PubMed] [Google Scholar]
- 2.Rosenthal HE, Slaunwhite WR Jr, Sandberg AA. Transcortin: a corticosteroid-binding protein of plasma. X. Cortisol and progesterone interplay and unbound levels of these steroids in pregnancy. J Clin Endocrinol Metab. 1969;29(3):352–367. [DOI] [PubMed] [Google Scholar]
- 3.Ho JT, Lewis JG, O’Loughlin P, Bagley CJ, Romero R, Dekker GA, Torpy DJ. Reduced maternal corticosteroid-binding globulin and cortisol levels in pre-eclampsia and gamete recipient pregnancies. Clin Endocrinol (Oxf). 2007;66(6):869–877. [DOI] [PubMed] [Google Scholar]
- 4.Jung C, Ho JT, Torpy DJ, Rogers A, Doogue M, Lewis JG, Czajko RJ, Inder WJ. A longitudinal study of plasma and urinary cortisol in pregnancy and postpartum. J Clin Endocrinol Metab. 2011;96(5):1533–1540. [DOI] [PubMed] [Google Scholar]
- 5.Scott EM, McGarrigle HH, Lachelin GC. The increase in plasma and saliva cortisol levels in pregnancy is not due to the increase in corticosteroid-binding globulin levels. J Clin Endocrinol Metab. 1990;71(3):639–644. [DOI] [PubMed] [Google Scholar]
- 6.Dörr HG, Heller A, Versmold HT, Sippell WG, Herrmann M, Bidlingmaier F, Knorr D. Longitudinal study of progestins, mineralocorticoids, and glucocorticoids throughout human pregnancy. J Clin Endocrinol Metab. 1989;68(5):863–868. [DOI] [PubMed] [Google Scholar]
- 7.Demey-Ponsart E, Foidart JM, Sulon J, Sodoyez JC. Serum CBG, free and total cortisol and circadian patterns of adrenal function in normal pregnancy. J Steroid Biochem. 1982;16(2):165–169. [DOI] [PubMed] [Google Scholar]
- 8.Lindsay JR, Nieman LK. The hypothalamic-pituitary-adrenal axis in pregnancy: challenges in disease detection and treatment. Endocr Rev. 2005;26(6):775–799. [DOI] [PubMed] [Google Scholar]
- 9.Moore DE, Kawagoe S, Davajan V, Mishell DR, Nakamura RM. An in vivo system in man for quantitation of estrogenicity. I. Physiologic changes in binding capacity of serum corticosteroid-binding globulin. Am J Obstet Gynecol. 1978;130(4):475–481. [DOI] [PubMed] [Google Scholar]
- 10.Musa BU, Doe RP, Seal US. Serum protein alterations produced in women by synthetic estrogens. J Clin Endocrinol Metab. 1967;27(10):1463–1469. [DOI] [PubMed] [Google Scholar]
- 11.Moore DE, Kawagoe S, Davajan V, Nakamura RM, Mishell DR. An in vivo system in man for quantitation of estrogenicity. II. Pharmacologic changes in binding capacity of serum corticosteroid-binding globulin induced by conjugated estrogens, mestranol, and ethinyl estradiol. Am J Obstet Gynecol. 1978;130(4):482–486. [PubMed] [Google Scholar]
- 12.Pemberton PA, Stein PE, Pepys MB, Potter JM, Carrell RW. Hormone binding globulins undergo serpin conformational change in inflammation. Nature. 1988;336(6196):257–258. [DOI] [PubMed] [Google Scholar]
- 13.Lewis JG, Elder PA. Intact or “active” corticosteroid-binding globulin (CBG) and total CBG in plasma: determination by parallel ELISAs using monoclonal antibodies. Clin Chim Acta. 2013;416:26–30. [DOI] [PubMed] [Google Scholar]
- 14.Nenke MA, Rankin W, Chapman MJ, Stevens NE, Diener KR, Hayball JD, Lewis JG, Torpy DJ. Depletion of high-affinity corticosteroid-binding globulin corresponds to illness severity in sepsis and septic shock; clinical implications. Clin Endocrinol (Oxf). 2015;82(6):801–807. [DOI] [PubMed] [Google Scholar]
- 15.Chan WL, Carrell RW, Zhou A, Read RJ. How changes in affinity of corticosteroid-binding globulin modulate free cortisol concentration. J Clin Endocrinol Metab. 2013;98(8):3315–3322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nguyen PT, Lewis JG, Sneyd J, Lee RS, Torpy DJ, Shorten PR. Development of a formula for estimating plasma free cortisol concentration from a measured total cortisol concentration when elastase-cleaved and intact corticosteroid binding globulin coexist. J Steroid Biochem Mol Biol. 2014;141:16–25. [DOI] [PubMed] [Google Scholar]
- 17.Klieber MA, Underhill C, Hammond GL, Muller YA. Corticosteroid-binding globulin, a structural basis for steroid transport and proteinase-triggered release. J Biol Chem. 2007;282(40):29594–29603. [DOI] [PubMed] [Google Scholar]
- 18.Strel’chyonok OA, Avvakumov GV, Matveentseva IV, Akhrem LV, Akhrem AA. Isolation and characterization of glycopeptides of human transcortin. Biochim Biophys Acta. 1982;705(2):167–173. [DOI] [PubMed] [Google Scholar]
- 19.Akhrem AA, Avvakumov GV, Akhrem LV, Sidorova IV, Strel’chyonok OA. Structural organization of the carbohydrate moiety of human transcortin as determined by methylation analysis of the whole glycoprotein. Biochim Biophys Acta. 1982;714(1):177–180. [DOI] [PubMed] [Google Scholar]
- 20.Mitchell E, Torpy DJ, Bagley CJ. Pregnancy-associated corticosteroid-binding globulin: high resolution separation of glycan isoforms. Horm Metab Res. 2004;36(6):357–359. [DOI] [PubMed] [Google Scholar]
- 21.Strel’chyonok OA, Avvakumov GV, Akhrem AA. Pregnancy-associated molecular variants of human serum transcortin and thyroxine-binding globulin. Carbohydr Res. 1984;134(1):133–140. [DOI] [PubMed] [Google Scholar]
- 22.Avvakumov GV, Hammond GL. Glycosylation of human corticosteroid-binding globulin. Differential processing and significance of carbohydrate chains at individual sites. Biochemistry. 1994;33(19):5759–5765. [DOI] [PubMed] [Google Scholar]
- 23.Avvakumov GV, Strel’chyonok OA. Properties and serum levels of pregnancy-associated variant of human transcortin. Biochim Biophys Acta. 1987;925(1):11–16. [DOI] [PubMed] [Google Scholar]
- 24.Hossner KL, Billiar RB. Plasma clearance and organ distribution of native and desialylated rat and human transcortin: species specificity. Endocrinology. 1981;108(5):1780–1786. [DOI] [PubMed] [Google Scholar]
- 25.Sumer-Bayraktar Z, Kolarich D, Campbell MP, Ali S, Packer NH, Thaysen-Andersen M. N-glycans modulate the function of human corticosteroid-binding globulin. Mol Cell Proteomics 2011;10(8):M111.009100. [DOI] [PMC free article] [PubMed]
- 26.Avvakumov GV, Strel’chyonok OA. Evidence for the involvement of the transcortin carbohydrate moiety in the glycoprotein interaction with the plasma membrane of human placental syncytiotrophoblast. Biochim Biophys Acta. 1988;938(1):1–6. [DOI] [PubMed] [Google Scholar]
- 27.Chebbo A, Tan S, Kassis C, Tamura L, Carlson RW. Maternal sepsis and septic shock. Crit Care Clin. 2016;32(1):119–135. [DOI] [PubMed] [Google Scholar]
- 28.Vogeser M, Kratzsch J, Ju Bae Y, Bruegel M, Ceglarek U, Fiers T, Gaudl A, Kurka H, Milczynski C, Prat Knoll C, Suhr AC, Teupser D, Zahn I, Ostlund RE. Multicenter performance evaluation of a second generation cortisol assay [published online ahead of print November 29, 2016]. Clin Chem Lab Med. [DOI] [PubMed] [Google Scholar]
- 29.Nenke MA, Holmes M, Rankin W, Lewis JG, Torpy DJ. Corticosteroid-binding globulin cleavage is paradoxically reduced in alpha-1 antitrypsin deficiency: implications for cortisol homeostasis. Clin Chim Acta. 2016;452:27–31. [DOI] [PubMed] [Google Scholar]
- 30.Lewis JG, Elder PA. Corticosteroid-binding globulin reactive centre loop antibodies recognise only the intact natured protein: elastase cleaved and uncleaved CBG may coexist in circulation. J Steroid Biochem Mol Biol. 2011;127(3-5):289–294. [DOI] [PubMed] [Google Scholar]
- 31.Abou-Samra AB, Pugeat M, Dechaud H, Nachury L, Bouchareb B, Fevre-Montange M, Tourniaire J. Increased plasma concentration of N-terminal beta-lipotrophin and unbound cortisol during pregnancy. Clin Endocrinol (Oxf). 1984;20(2):221–228. [DOI] [PubMed] [Google Scholar]
- 32.Doe RP, Dickinson P, Zinneman HH, Seal US. Elevated nonprotein-bound cortisol (NPC) in pregnancy, during estrogen administration and in carcinoma of the prostate. J Clin Endocrinol Metab. 1969;29(6):757–766. [DOI] [PubMed] [Google Scholar]
- 33.Benassayag C, Souski I, Mignot TM, Robert B, Hassid J, Duc-Goiran P, Mondon F, Rebourcet R, Dehennin L, Nunez EA, Ferré F. Corticosteroid-binding globulin status at the fetomaternal interface during human term pregnancy. Biol Reprod. 2001;64(3):812–821. [DOI] [PubMed] [Google Scholar]
- 34.Hammond GL, Smith CL, Goping IS, Underhill DA, Harley MJ, Reventos J, Musto NA, Gunsalus GL, Bardin CW. Primary structure of human corticosteroid binding globulin, deduced from hepatic and pulmonary cDNAs, exhibits homology with serine protease inhibitors. Proc Natl Acad Sci USA. 1987;84(15):5153–5157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Misao R, Hori M, Ichigo S, Fujimoto J, Tamaya T. Corticosteroid-binding globulin mRNA levels in human uterine endometrium. Steroids. 1994;59(10):603–607. [DOI] [PubMed] [Google Scholar]
- 36.Misao R, Nakanishi Y, Fujimoto J, Iwagaki S, Tamaya T. Levels of sex hormone-binding globulin and corticosteroid-binding globulin mRNAs in corpus luteum of human subjects: correlation with serum steroid hormone levels. Gynecol Endocrinol. 1999;13(2):82–88. [DOI] [PubMed] [Google Scholar]
- 37.Miska W, Peña P, Villegas J, Sánchez R. Detection of a CBG-like protein in human Fallopian tube tissue. Andrologia. 2004;36(1):41–46. [DOI] [PubMed] [Google Scholar]
- 38.Misao R, Iwagaki S, Sun WS, Fujimoto J, Saio M, Takami T, Tamaya T. Evidence for the synthesis of corticosteroid-binding globulin in human placenta. Horm Res. 1999;51(4):162–167. [DOI] [PubMed] [Google Scholar]
- 39.Fernandez-Real JM, Pugeat M, Grasa M, Broch M, Vendrell J, Brun J, Ricart W. Serum corticosteroid-binding globulin concentration and insulin resistance syndrome: a population study. J Clin Endocrinol Metab. 2002;87(10):4686–4690. [DOI] [PubMed] [Google Scholar]
- 40.Lewis JG, Shand BI, Elder PA, Scott RS. Plasma sex hormone-binding globulin rather than corticosteroid-binding globulin is a marker of insulin resistance in obese adult males. Diabetes Obes Metab. 2004;6(4):259–263. [DOI] [PubMed] [Google Scholar]
- 41.Lewis JG, Borowski KK, Shand BI, George PM, Scott RS. Plasma sex hormone-binding globulin, corticosteroid-binding globulin, cortisol, and free cortisol levels in outpatients attending a lipid disorders clinic: a cross-sectional study of 1137 subjects. Horm Metab Res. 2010;42(4):274–279. [DOI] [PubMed] [Google Scholar]
- 42.Belo L, Santos-Silva A, Rocha S, Caslake M, Cooney J, Pereira-Leite L, Quintanilha A, Rebelo I. Fluctuations in C-reactive protein concentration and neutrophil activation during normal human pregnancy. Eur J Obstet Gynecol Reprod Biol. 2005;123(1):46–51. [DOI] [PubMed] [Google Scholar]
- 43.Larsson A, Palm M, Hansson LO, Basu S, Axelsson O. Reference values for alpha1-acid glycoprotein, alpha1-antitrypsin, albumin, haptoglobin, C-reactive protein, IgA, IgG and IgM during pregnancy. Acta Obstet Gynecol Scand. 2008;87(10):1084–1088. [DOI] [PubMed] [Google Scholar]
- 44.Strel’chyonok OA, Avvakumov GV. Specific steroid-binding glycoproteins of human blood plasma: novel data on their structure and function. J Steroid Biochem. 1990;35(5):519–534. [DOI] [PubMed] [Google Scholar]
- 45.Strel’chyonok OA, Avvakumov GV. Interaction of human CBG with cell membranes. J Steroid Biochem Mol Biol. 1991;40(4-6):795–803. [DOI] [PubMed] [Google Scholar]
- 46.Mihrshahi R, Lewis JG, Ali SO. Hormonal effects on the secretion and glycoform profile of corticosteroid-binding globulin. J Steroid Biochem Mol Biol. 2006;101(4-5):275–285. [DOI] [PubMed] [Google Scholar]
- 47.Henley D, Brown S, Pennell C, Lye S, Torpy DJ. Evidence for central hypercortisolism and elevated blood pressure in adolescent offspring of mothers with pre-eclampsia. Clin Endocrinol (Oxf). 2016;85(4):583–589. [DOI] [PubMed] [Google Scholar]
- 48.Sandman CA, Davis EP, Buss C, Glynn LM. Prenatal programming of human neurological function. Int J Pept 2011;2011:837596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lei JH, Yang X, Peng S, Li Y, Underhill C, Zhu C, Lin HY, Wang H, Hammond GL. Impact of corticosteroid-binding globulin deficiency on pregnancy and neonatal sex. J Clin Endocrinol Metab. 2015;100(5):1819–1827. [DOI] [PubMed] [Google Scholar]
- 50.Weckesser LJ, Plessow F, Pilhatsch M, Muehlhan M, Kirschbaum C, Miller R. Do venepuncture procedures induce cortisol responses? A review, study, and synthesis for stress research. Psychoneuroendocrinology. 2014;46:88–99. [DOI] [PubMed] [Google Scholar]
- 51.Briet C, Saraval M, Loric S, Topolinski-Duyme H, Fendri S, Desailloud R. The use of intravenous catheterisation with a rest period is useful for determination of plasma cortisol levels but not plasma prolactin levels. Ann Endocrinol (Paris). 2007;68(1):34–38. [DOI] [PubMed] [Google Scholar]
- 52.Moisan MP, Minni AM, Dominguez G, Helbling JC, Foury A, Henkous N, Dorey R, Béracochéa D. Role of corticosteroid binding globulin in the fast actions of glucocorticoids on the brain. Steroids. 2014;81:109–115. [DOI] [PubMed] [Google Scholar]
- 53.Predine J, Brailly S, Delaporte P, Milgrom E. Protein binding of cortisol in human cerebrospinal fluid. J Clin Endocrinol Metab. 1984;58(1):6–11. [DOI] [PubMed] [Google Scholar]
- 54.Sivukhina EV, Jirikowski GF, Bernstein HG, Lewis JG, Herbert Z. Expression of corticosteroid-binding protein in the human hypothalamus, co-localization with oxytocin and vasopressin. Horm Metab Res. 2006;38(4):253–259. [DOI] [PubMed] [Google Scholar]