Abstract
Background:
Atypical femur fractures (AFFs) are associated with long-term bisphosphonate (BP) therapy. Early identification of AFF prior to their completion provides an opportunity to intervene, potentially reducing morbidity associated with these fractures. Single-energy X-ray absorptiometry (SE) is an imaging method recently shown to detect incomplete AFF (iAFF) prior to fracture completion.
Methods:
Between May 2013 and September 2014, we assessed 173 patients who had been prescribed BP therapy for >5 years for iAFF using SE at their presentation for routine bone mineral density testing. We compared these findings with those of our previously published prospective study (n = 257) in which the femur was imaged for iAFF using dual-energy X-ray absorptiometry. In addition, we estimated the yearly prevalence of complete AFF among patients with subtrochanteric fracture at our institution from 2006 to 2014, and we evaluated prescribing trends for BP in Ireland from 2009 to 2014.
Results:
No patients had iAFF using SE femur compared with a prevalence of 2.7% in the earlier study. Between 2006 and 2014, we observed a rise and decline in AFFs at our hospital and a similar national trend in BP prescribing.
Conclusions:
AFFs appear to be decreasing. New customized scan modes of dual-energy X-ray absorptiometry systems, which visualize the entire femur at high image quality and take measurements, have the potential to identify iAFF prior to fracture completion and to ascertain those at highest risk of AFF.
Keywords: atypical femur fracture, bisphosphonate therapy, DXA
Atypical femur fractures (AFFs) are rare events that are associated with long-term bisphosphonate therapy. Using high-definition imaging with dual-energy X-ray absorptiometry machines, AFFs may be identified in the incomplete form.
A crisis in the treatment of osteoporosis is attributed, in part, to patient fear of harms from bisphosphonate (BP) therapy that includes atypical femur fracture (AFF) [1]. The criteria for defining AFF were established by an American Society of Bone and Mineral Research (ASBMR) task force in 2010 and further refined in 2014 [2, 3]. AFFs are associated strongly with long-term BP therapy [3, 4]. They share many features with other types of stress fractures [5, 6] but being located on the outer convex surface of the femur, they are more apt to convert from incomplete to complete fracture, and patients may report prodromal pain at the fracture site for weeks and sometimes months prior to fracture completion [7]. Because completed AFFs have been associated with delayed healing and poorer surgical outcomes [8], recognizing the prodromal pain of an incomplete AFF (iAFF) may spare the patient these morbidities. Another opportunity for early detection of iAFF is to assess the lateral femur cortex using an extended femur scan field modification of dual-energy X-ray absorptiometry (DXA) imaging at the time of scheduled bone mineral density (BMD) testing [5]. We previously reported results of a study in which patients on long-term BP therapy were evaluated for iAFFs using this extended femur field strategy [9]. In a consecutive sample of 257 patients from October 2011 to January 2013 who were on BP therapy for more than 5 years, we diagnosed iAFFs in 2.7% of patients [10]. At the time of that publication, a similar high prevalence was reported by two other investigators using different imaging modalities [11, 12].
Given the substantive morbidity gap for the patient and the technical gap for the surgeon between fixing an iAFF compared with fixing a complete AFF, an improvement in DXA systems for early detection of iAFF could close the gap. The single-energy X-ray absorptiometry (SE) mode, used by Hologic (Waltham, MA) DXA systems for lateral spine imaging, can be adapted for femur imaging. SE femur imaging has a number of advantages over DXA femur imaging: the image resolution is nearer to X-ray quality, the entire length of the femur can be visualized, and image acquisition is fivefold faster (Fig. 1) [10]. We now report the results of a second prospective study of patients on long-term BP therapy using SE femur imaging to detect iAFF as point of service at the time of routine BMD measurement. In addition, we assessed the prevalence of completed AFF in our hospital by evaluating all radiographs of patients with subtrochanteric femur fractures from 2006 to 2014, and we evaluated the prescribing trends for osteoporosis in Ireland from 2009 to 2014.
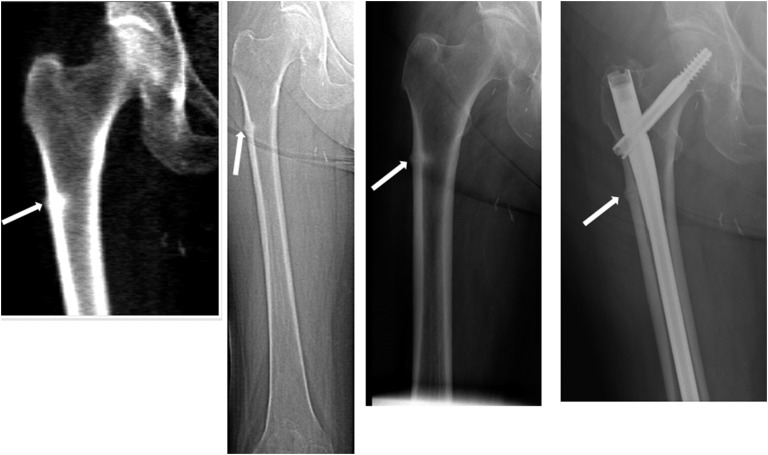
Figure 1.
An 82-year-old woman, who had been treated with ibandronate 150 mg monthly for 9 years, presented with a 6-month history of left thigh pain. Images show iAFF in the right femur using extended femur field imaging with DXA (left panel), SE femur imaging (center left panel), and plain radiograph (center right panel). An intramedullary nail was inserted electively (right panel).
1. Methods
A. SE Femur Imaging Study
This SE femur imaging study was approved by the St. Vincent’s Ethics Committee, and informed consent was obtained. Consecutive patients referred for routine DXA from all sources in our catchment area were selected for study if they had been treated with BP therapy for more than 5 years, as identified by questionnaire or on the referral request. The study was conducted between May 2013 and September 2014. Patient selection was identical to that for our first study, which was conducted between October 2011 and January 2013. Based on the prevalence of iAFF in our first study of 2.7% (95% confidence interval, 1.7% to 3.7%), using an identical study design, the number needed to monitor to detect one iAFF should range from 27 to 59.
BMD was measured at the lumbar spine and bilateral hips using a Hologic Discovery Model A. According to the Official Positions of the International Society of Clinical Densitometry, we calculated the least significant change as 0.027 g/cm2 at the spine and 0.020 g/cm2 at the hip [13]. Reference range was based on the National Health and Nutrition Examination Survey III population-based database for the total femur site and on the manufacturer’s range for lumbar 1 to 4 [14]. Results are presented as standard deviation units (T scores) based on comparison with young adult reference BMD.
An SE femur image from the proximal tip of the femur to the distal end of the femur shaft was acquired from both sides immediately after conducting a DXA examination of the femur with the leg internally rotated. The SE femur images were printed and viewed independently by two International Society of Clinical Densitometry–certified densitometrists who were experienced in iAFF evaluation (M.J.M., S.K.). If any localized abnormality was seen on the lateral cortex that was suspicious for thickening (namely, “flaring” or “beaking”), which would indicate an iAFF [3], then the patient was referred for a plain radiograph. Radiographs were interpreted by a musculoskeletal radiologist experienced in iAFF evaluation (E.H.).
B. Radiographic Survey
The prevalence of complete AFF in our institution from 2006 to 2014 was determined by viewing all images from patients with subtrochanteric fractures. Information about these femur fractures was obtained from the Hospital Inpatient Inquiry, which is a computer-based discharge abstracting system designed to collect demographic, clinical, and administrative data on discharges and in-hospital deaths from acute general hospitals in Ireland nationally. The coding of the diagnoses and procedures performed used the International Classification of Diseases, Tenth Revision, Clinical Modification from 2005 to 2014. Using these codes, the following specific hip fracture types were identified—namely, fractures of the neck of femur (S720), pertrochanteric fractures (S721), subtrochanteric fractures (S722), and fractures of the shaft of femur (S723). One of the authors (E.H.), who was blinded to the date of the radiographs, examined all images that were coded as S722 and adjudicated on those with complete AFF according to the ASBMR criteria [3].
C. Trends in the Prescribing of Antiosteoporosis Medications in Ireland, 2009 to 2014
Analysis of national prescribing trends from 2009 to 2014 was conducted using data from the Irish Health Service Executive–Primary Care Reimbursement Services national primary care prescribing database [15]. The scheme covers all patients older than 70 years and approximately 35% of the total population but accounts for approximately 70% of all prescribing in Ireland [16]. Full details on medications dispensed are recorded in the database using the World Health Organization Anatomical Therapeutic Chemical (ATC) classification system. All prescription data on the main types of antiosteoporosis treatments in all persons aged ≥50 years by sex and in 5-year age bands from 2009 to 2014 were included in the analyses: 1) bisphosphonates ATC code M05BA and bisphosphonates plus calcium ATC code M05BB; 2) calcium products alone ATC code A12AX or in combination with bisphosphonates ATC code M05BB, 3) strontium ranelate ATC code M05BX03, 4) denosumab ATC code M05BX04, and 5) raloxifene ATC code G03XC01.
D. Statistical Analysis
Results are presented as frequency and percent or as mean and standard deviation. Difference between means was determined by an independent t test following Levene’s test for equality of variances; difference between frequencies of categorical variables was tested by the χ2 test. Linear regression analysis was used to calculate the yearly percent change in the absolute number of prescriptions in the national survey. Significance at P < 0.05 is assumed. Statistical analysis was performed using IBM SPSS for Windows version 22.0 (Armonk, NY).
2. Results
A. SE Femur Imaging Study
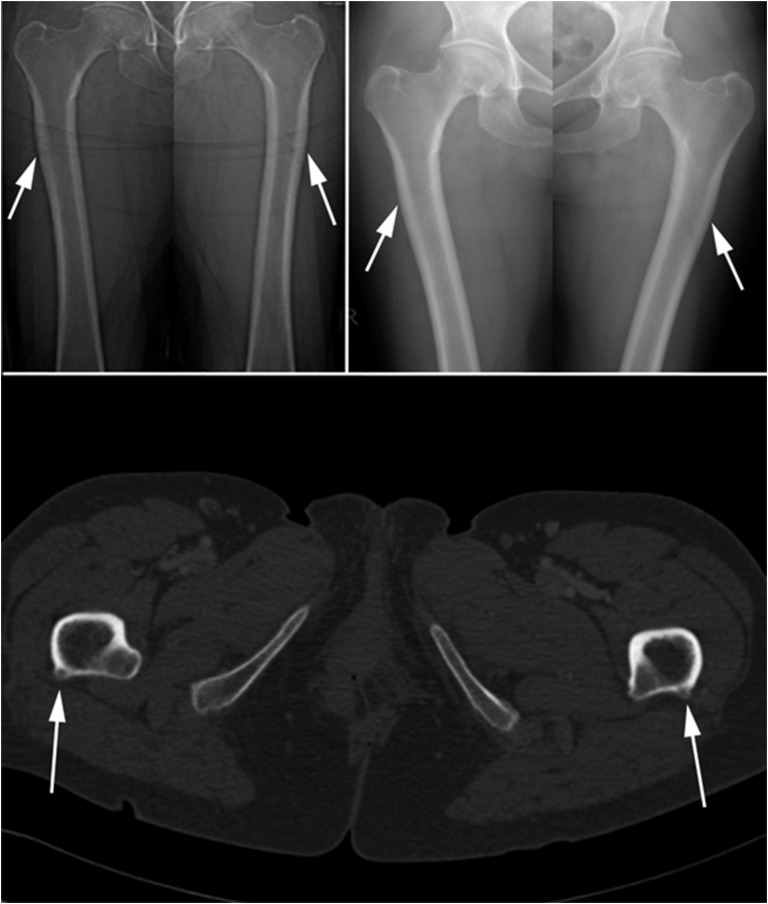
SE femur examination was performed in 173 consecutive qualifying patients from May 2013 to September 2014; no eligible patients declined entry into the study. Compared with our previous study performed between October 2011 and January 2013, the current population showed a shorter duration of BP treatment (P = 0.004), higher femur neck T score (P = 0.031), and higher total hip T score (P = 0.019) but no difference in lumbar spine T score (P = 0.207) (Table 1). Abnormalities suspicious for iAFF were observed in 12 patients, although none had evidence of iAFF on radiographic imaging. Radiographic abnormalities mimicking iAFF were identified in six patients, four of whom had prominence of the gluteus maximus insertion confirmed by computerized tomography in one patient (Fig. 2).
Table 1.
Descriptive Statistics
| Variable | First Study: DXA Imaging (n = 257) | Second Study: SE Imaging (n = 173) |
|---|---|---|
| Sex, female/male, no. (%) | 238/19 (93/7) | 166/7 (96/4) |
| Age, y, mean (SD) | 72.2 (8.8) | 69.1 (10.1) |
| Lumbar 1 to 4, T score, mean (SD) | −2.08 (1.11) | −1.93 (1.20) |
| Femur neck, T score, mean (SD) | −2.02 (0.78) | −1.84 (0.89)a |
| Hip, T score, mean (SD) | −1.56 (0.89) | −1.35 (0.95)a |
| Treatment, y, mean (SD) | 7.6 (2.7) | 6.8 (2.5)a |
| Bisphosphonates, no. (%) | ||
| Alendronate | 170 (66.3) | 111 (64.2) |
| Risedronate | 59 (23.0) | 29 (16.8) |
| Ibandronate | 24 (9.3) | 33 (19.1) |
| Zoledronate | 3 (1.2) | 0 (0) |
| Etidronate | 1 (0.4) | 0 (0) |
| DXA-suspected AFF, no. (%) | 19 (7.4) | 12 (6.9) |
| X-ray findings, no. (%) | ||
| Normal | 7 (2.7) | 6 (3.5) |
| Abnormal: non-AFF | 5 (2.0) | 6 (3.5) |
| Abnormal: AFF | 7 (2.7) | 0 (0) |
Abbreviation: SD, standard deviation.
Significant difference (P < 0.05) between groups as per independent t test.
Figure 2.
Bilateral symmetric foci of cortical thickening on the lateral aspects of both femora are marked by arrows on both SE images (top left image) and on plain radiographs (top right image). Computed tomography imaging identifies a posterolateral rather than a lateral location and shows that they represent insertion of the gluteus maximus tendon onto the femur at the proximal end of the linea aspera. The internal rotation of the femur at the time of DXA imaging accounts for the lateral location of the linea aspera.
B. Radiographic Survey
On the radiographic review of patients admitted with femur fracture, the prevalence of subtrochanteric fractures among the total number of femur fractures from 2006 to 2014 was 4.9% (n = 157/3211). The corresponding prevalence nationally of subtrochanteric fractures as a percentage of all femur fractures for the same time period was 4% (n = 1573/37,649) [17]. The overall prevalence of AFF was 0.65% (n = 21/3211); no AFFs were noted in 2006 or in 2014 (Table 2).
Table 2.
Frequency of AFF Among Hospital Admissions With Subtrochanteric Femur Fracture
| Year | No. of Subtrochanteric Fractures | Yearly No. of AFFs | Yearly Frequency of AFF, % |
|---|---|---|---|
| 2006 | 15 | 0 | 0 |
| 2007 | 14 | 5 | 35 |
| 2008 | 17 | 1 | 6 |
| 2009 | 15 | 2 | 13 |
| 2010 | 28 | 3 | 11 |
| 2011 | 24 | 4 | 17 |
| 2012 | 19 | 2 | 11 |
| 2013 | 18 | 4 | 22 |
| 2014 | 7 | 0 | 0 |
C. Trends in the Prescribing of Antiosteoporosis Medications in Ireland, 2009 to 2014
The number of prescription items dispensed for BP-containing compounds increased between 2009 and 2011, after which there was a total decrease of 25% from 699,778 in 2011 to 547,394 in 2014 and a year-on-year percent decrease of 5% (P = 0.05) (Table 3). There was no statistically significant difference in the decrease in the prescribing of BP-containing products across the individual age bands. In contrast, the number of prescription items for all calcium-containing compounds increased from 838,258 items in 2009 to 1,055,123 items in 2014, giving an overall increase of 26% with a significant year-on-year increase of 4% (P = 0.013). The greatest increase was identified in men (60%). The most significant increase in prescriptions was in the 75+-year age group, in which there was a 20% increase (P ≤ 0.05). Prescriptions for denosumab rose to 25,369 in 2014, having been launched in Ireland in 2010. The total number of prescriptions for strontium ranelate has fallen since mid-2013, with a year-on-year decrease of 16% and an overall reduction of 66% from 64,283 prescriptions in 2012 to 15,817 in 2014. Similarly, prescriptions for raloxifene have fallen by 58% from 26,312 in 2009 to 13,631 in 2014, corresponding to an 11% year-on-year decrease.
Table 3.
Prescribing Trends for BPs and Calcium in Ireland Between 2009 and 2014
| Year | BPs |
Calcium |
||
|---|---|---|---|---|
| No. | Year-on-Year Change, % | No. | Year-on-Year Change, % | |
| 2009 | 637,233 | 838,258 | ||
| 2010 | 683,031 | 7 | 924,970 | 10 |
| 2011 | 699,778 | 2 | 1,004,193 | 9 |
| 2012 | 687,167 | −2 | 1,098,721 | 9 |
| 2013 | 624,554 | −9 | 1,098,623 | 0 |
| 2014 | 547,394 | −12 | 1,055,123 | −4 |
| Change 2009 to 2014, % | −14 | 26 | ||
| Year-on-year change, % | −5 | 4 | ||
| P value | 0.05 | 0.013 | ||
3. Discussion
Using SE femur imaging in a prospective study of 173 patients who were taking BP therapy for greater than 5 years, we did not identify any new case of iAFF between May 2013 and September 2014. The study group was similar with respect to recruitment to an earlier group of patients who were studied using extended femur DXA imaging in whom we noted iAFF in 2.7%, but the earlier group had a longer duration of treatment and lower BMD at both femur neck and total hip. Because the differences between the two study groups were small, we speculate that the greater awareness of AFF and the subsequent change in prescribing practice of BP has led to a decline in AFF. In our hospital survey, we noted a low prevalence of complete AFF over a 9-year period from 2006 to 2014, but our survey suggests that frequency of AFF increased and then declined.
Every test is subject to diagnostic uncertainty. Given the design of our study, we were not in a position to estimate sensitivity and specificity but were able to identify false-positive cases. In our first study using the poorer imaging modality, we had an assorted number of explanations for false positives, with the most unusual being an enchondroma [10]. In the second study, with higher quality imaging, we identified a number of the false-positive cases as being due to prominence of the insertion point of the gluteus maximus along the linea aspera. Although the linea aspera has a posterolateral position, the hip is internally rotated as part of the correct positioning for DXA imaging that brings the linea aspera into relief along the lateral femur cortex (Fig. 2).
Because codes from the International Classification of Diseases, Tenth Revision, Clinical Modification for AFF, both complete and incomplete, were only published in 2016, it was not possible to evaluate epidemiologic trends in AFF in Ireland over the time period of this study. As regards trends in femur fracture rates in Ireland, we previously reported a downward trend in age-standardized femur rate from 2000 to 2009 (including neck of femur, pertrochanteric and subtrochanteric) but an increase in the absolute numbers of hospitalizations [18]. Regarding national prescribing trends for osteoporosis medications in Ireland between 2009 and 2014, we noted discordance between calcium prescribing and BP prescribing, with the former increasing and the latter decreasing. In a population-based study of trends in femur fracture rates and BP prescribing rates in the United States, Jha et al. [19] showed a steady and significant increase in subtrochanteric and diaphyseal fracture incidence between 2002 and 2011, followed by a subsequent decline [19]. This decline was preceded by a steady fall in oral BP prescriptions beginning in 2006 and coinciding with consecutive high-profile media reports of concerns about adversities of long-term BP use [19]. The trends in prescribing identified in our study may represent a response in prescribing practices in primary care to statements published by the US Food and Drug Administration in 2010 and by European Medicines Agency in 2011 [20, 21]. These statements highlighted the association between BPs and AFF and the need to evaluate continuation of BP treatment periodically on an individual basis, particularly after 5 years of treatment [21].
The association between long-term BP therapy and AFF prompted so much debate about the harms and benefits of both continuing and discontinuing BP that the ASBMR charged a task force to provide guidance on the duration of BP therapy with respect to both safety and efficacy [22]. The principal sources of evidence were gathered from two extension trials: the Fracture Intervention Trial Long-term Extension study with alendronate and the Health Outcomes and Reduced Incidence with Zoledronic Acid Once Yearly extension study with zoledronic acid. Benefit with respect to ongoing fracture prevention seemed to be confined to vertebral fracture both in Health Outcomes and Reduced Incidence with Zoledronic Acid Once Yearly (for those who had incident fracture during the study, without prevalent vertebral fracture at entry, and with a persistent T score ≤−2.5 at hip or femoral neck) and in Fracture Intervention Trial Long-term Extension (for those who had a femoral neck T score above −2.5 but ≤−2.0) [22]. The task force concluded that those at low fracture risk should discontinue at 5 years with reassessment at 2 to 3 years. They recommended that for those deemed to be at high risk of fracture, clinicians should discuss with patients the option of continuing oral BP for 10 years and intravenous zoledronic acid for 6 years. In the absence of very long-duration registration trials of BPs, there was no guidance for their use beyond 10 years.
That the proportion of AFF with respect to hip fracture is very low and that the strong association between iAFF and long-term BP therapy is robust means that the risk of AFF will persist and likely increase with long-term BP therapy even if at a low rate [23]. The ASBMR task force on long-term BP therapy did not give any guidance about screening for iAFF for those deemed to need long-term BP therapy. SE femur imaging is a simple, fast, effective, convenient, and safe way to identify iAFF at point of service. Should a clinician opt for BP therapy beyond 5 years in line with the ASBMR task force report, then vigilance and a strategy for early detection of AFF should be optimized. In addition, we suggest that any patients who complain of pain in the outer aspect of the femur at the time that they attend for routine DXA, regardless of the duration of BP therapy, should have SE femur imaging for iAFF; if this feature is not available, then they should be referred for more definitive imaging. Should femur imaging be performed, then bilateral imaging is warranted given the likelihood of bilaterality [7, 24, 25]. Finally, the presence of localized thickening on the lateral cortex warrants further imaging to determine if a fracture line is extant because early insertion of an intramedullary nail may be warranted, as exemplified by the vignette in Fig. 1 [3].
The early studies on the role of DXA systems in the identification of iAFF were conducted by DXA operators in the field who adapted their DXA systems by using extended femur field length at the time of DXA imaging or by using the scan mode for SE imaging of the spine to image the femur as in this study. Even routine DXA imaging using the standard femur field length has been shown, retrospectively, to identify iAFF prior to fracture completion [10, 26]. In response to these observations and innovations, DXA manufacturers have customized their DXA systems with new scan modes to facilitate imaging of the full extent of the femur as a Food and Drug Administration–approved feature, and they have added extra options. Hologic (Waltham, MA) added a scan mode to its latest model, the Horizon DXA system, called the “SE femur” that uses SE imaging. This scan mode is conducted while the patient is still positioned on the table after the femur DXA examination, the entire femur is visualized rapidly, the image can be annotated, and measurement of cortical thickness or distance from a landmark can be made [27]. GE Healthcare (Chicago, IL) devised a software upgrade called “Atypical Femur Fracture,” which can be installed on current Prodigy and Lunar iDXA models. It is a form of DXA imaging starting at the patella with a distal and a proximal component; cortical width, both medial and lateral, is measured; the widths are profiled, permitting detection of focal thickening; and serial trends can be analyzed [28]. Not only can DXA systems aid in the early detection of iAFF, but the additional features may assist in identifying those at highest risk of AFF.
In conclusion, the incidence of AFF in Ireland seems to be waning, coincident with declining BP prescribing practice at the primary care level. Deploying DXA systems for early detection of AFF may assist in allaying patient concern about a rare but serious harm of BP therapy. New customized scan modes of DXA systems, which visualize the entire femur at high image quality and take measurements, have the potential both to identify iAFF early and to ascertain those at highest risk of AFF. If point-of-service femur imaging identifies an iAFF, then there is an opportunity to prevent fracture completion, averting morbidity associated with a complete AFF.
Acknowledgments
Disclosure Summary: The authors have nothing to disclose.
Footnotes
- AFF
- atypical femur fracture
- ASBMR
- American Society of Bone and Mineral Research
- ATC
- Anatomical Therapeutic Chemical
- BMD
- bone mineral density
- BP
- bisphosphonate
- DXA
- dual-energy X-ray absorptiometry
- iAFF
- incomplete atypical femur fracture
- SE
- single-energy X-ray absorptiometry
References and Notes
- 1.Khosla S, Shane E. A crisis in the treatment of osteoporosis. J Bone Miner Res. 2016;31(8):1485–1487. [DOI] [PubMed] [Google Scholar]
- 2.Shane E, Burr D, Ebeling PR, Abrahamsen B, Adler RA, Brown TD, Cheung AM, Cosman F, Curtis JR, Dell R, Dempster D, Einhorn TA, Genant HK, Geusens P, Klaushofer K, Koval K, Lane JM, McKiernan F, McKinney R, Ng A, Nieves J, O’Keefe R, Papapoulos S, Sen HT, van der Meulen MC, Weinstein RS, Whyte M; American Society for Bone and Mineral Research . Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2010;25(11):2267–2294. [DOI] [PubMed] [Google Scholar]
- 3.Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, Cheung AM, Cosman F, Curtis JR, Dell R, Dempster DW, Ebeling PR, Einhorn TA, Genant HK, Geusens P, Klaushofer K, Lane JM, McKiernan F, McKinney R, Ng A, Nieves J, O’Keefe R, Papapoulos S, Howe TS, van der Meulen MC, Weinstein RS, Whyte MP. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2013;29(1):1–23. [DOI] [PubMed] [Google Scholar]
- 4.Schilcher J, Michaëlsson K, Aspenberg P. Bisphosphonate use and atypical fractures of the femoral shaft. N Engl J Med. 2011;364(18):1728–1737. [DOI] [PubMed] [Google Scholar]
- 5.McKenna MJ, Kleerekoper M, Ellis BI, Rao DS, Parfitt AM, Frame B. Atypical insufficiency fractures confused with Looser zones of osteomalacia. Bone. 1987;8(2):71–78. [DOI] [PubMed] [Google Scholar]
- 6.McKenna MJ, Heffernan E, Hurson C, McKiernan FE. Clinician approach to diagnosis of stress fractures including bisphosphonate-associated fractures. QJM. 2013;107(2):99–105. [DOI] [PubMed] [Google Scholar]
- 7.Schneider JP, Hinshaw WB, Su C, Solow P. Atypical femur fractures: 81 individual personal histories. J Clin Endocrinol Metab. 2012;97(12):4324–4328. [DOI] [PubMed] [Google Scholar]
- 8.Bogdan Y, Tornetta P III, Einhorn TA, Guy P, Leveille L, Robinson J, Bosse MJ, Haines N, Horwitz D, Jones C, Schemitsch E, Sagi C, Thomas B, Stahl D, Ricci W, Brady M, Sanders D, Kain M, Higgins TF, Collinge C, Kottmeier S, Friess D. Healing time and complications in operatively treated atypical femur fractures associated with bisphosphonate use: a multicenter retrospective cohort. J Orthop Trauma. 2016;30(4):177–181. [DOI] [PubMed] [Google Scholar]
- 9.McKiernan FE. Atypical femoral diaphyseal fractures documented by serial DXA. J Clin Densitom. 2010;13(1):102–103. [DOI] [PubMed] [Google Scholar]
- 10.McKenna MJ, van der Kamp S, Heffernan E, Hurson C. Incomplete atypical femoral fractures: assessing the diagnostic utility of DXA by extending femur length. J Clin Densitom. 2013;16(4):579–583. [DOI] [PubMed] [Google Scholar]
- 11.La Rocca Vieira R, Rosenberg ZS, Allison MB, Im SA, Babb J, Peck V. Frequency of incomplete atypical femoral fractures in asymptomatic patients on long-term bisphosphonate therapy. AJR Am J Roentgenol. 2012;198(5):1144–1151. [DOI] [PubMed] [Google Scholar]
- 12.Allison MB, Markman L, Rosenberg Z, Vieira RL, Babb J, Tejwani N, Peck V. Atypical incomplete femoral fractures in asymptomatic patients on long term bisphosphonate therapy. Bone. 2013;55(1):113–118. [DOI] [PubMed] [Google Scholar]
- 13.McKenna MJ, van der Kamp S, Au-Yeong M, FitzGerald O. Improving standards of DXA. Ir Med J. 2008;101(4):101–102. [PubMed] [Google Scholar]
- 14.Kanis JA, Adachi JD, Cooper C, Clark P, Cummings SR, Diaz-Curiel M, Harvey N, Hiligsmann M, Papaioannou A, Pierroz DD, Silverman SL, Szulc P; Epidemiology and Quality of Life Working Group of IOF . Standardising the descriptive epidemiology of osteoporosis: recommendations from the Epidemiology and Quality of Life Working Group of IOF. Osteoporos Int. 2013;24(11):2763–2764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Health Service Executive. Primary care reimbursement service. 2015. http://www.hse.ie/eng/staff/PCRS/PCRS_Publications. Accessed December 7, 2015.
- 16.Hiligsmann M, McGowan B, Bennett K, Barry M, Reginster JY. The clinical and economic burden of poor adherence and persistence with osteoporosis medications in Ireland. Value Health. 2012;15(5):604–612. [DOI] [PubMed] [Google Scholar]
- 17.Health Service Executive Health Atlas Ireland. 2015.. https://www.healthatlasireland.ie/. Accessed December 16, 2015.
- 18.McGowan B, Casey MC, Silke C, Whelan B, Bennett K. Hospitalisations for fracture and associated costs between 2000 and 2009 in Ireland: a trend analysis. Osteoporos Int. 2012;24(3):849–857. [DOI] [PubMed] [Google Scholar]
- 19.Jha S, Wang Z, Laucis N, Bhattacharyya T. Trends in media reports, oral bisphosphonate prescriptions, and hip fractures 1996-2012: an ecological analysis. J Bone Miner Res. 2015;30(12):2179–2187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Food and Drug Administration. Bisphosphonates (osteoporosis drugs): label change—atypical fractures update. 2010. http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm229244.htm. Accessed May 9, 2012.
- 21.European Medicines Agency Assessment report for bisphosphonates containing medicinal products. 2011. www.ema.europa.eu. Accessed October 7, 2013.
- 22.Adler RA, El-Hajj Fuleihan G, Bauer DC, Camacho PM, Clarke BL, Clines GA, Compston JE, Drake MT, Edwards BJ, Favus MJ, Greenspan SL, McKinney R Jr, Pignolo RJ, Sellmeyer DE. Managing osteoporosis in patients on long-term bisphosphonate treatment: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2016;31(1):16–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Black DM, Rosen CJ. Clinical practice: postmenopausal osteoporosis. N Engl J Med. 2016;374(3):254–262. [DOI] [PubMed] [Google Scholar]
- 24.Probyn L, Cheung AM, Lang C, Lenchik L, Adachi JD, Khan A, Josse RG, Tomlinson G, Bleakney R. Bilateral atypical femoral fractures: how much symmetry is there on imaging? Skeletal Radiol. 2015;44(11):1579–1584. [DOI] [PubMed] [Google Scholar]
- 25.Harborne K, Hazlehurst JM, Shanmugaratnam H, Pearson S, Doyle A, Gittoes NJ, Choudhary S, Crowley RK. Compliance with established guidelines for the radiological reporting of atypical femoral fractures. Br J Radiol. 2016;89(1057):20150443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim S, Yang KH, Lim H, Lee Y-K, Yoon HK, Oh C-W, Park KK, Min B-W, Ryu JA, Kwack K-S, Lee YH. Detection of prefracture hip lesions in atypical subtrochanteric fracture with dual-energy X-ray absorptiometry images. Radiology. 2014;270(2):487–495. [DOI] [PubMed] [Google Scholar]
- 27.Hologic. Horizon DXA system. 2017. http://www.hologic.com/products/imaging/skeletal-health/horizon-dxa-system. Accessed January 22, 2017.
- 28.GE Healthcare. Quatify incipient atypical femur fractures with our new enCore 17 software. 2017. http://landing1.gehealthcare.com/AD-16-12-DGS-BMD-enCORE-17-Trial_enCORE-17.html. Accessed January 22, 2017.