Abstract
Organophosphorus (OP) pesticide poisoning is a major clinical and public health problem in a developing country like India. Cardiac injury is a strong predictor of death in these patients. Cardiac complications usually described include cardiac arrest, pulmonary edema, and arrhythmia. Rarely, myocardial infarction has also been reported. The possible mechanisms for myocardial injury include sympathetic/parasympathetic overactivity, hypoxemia, acidosis, dyselectrolytemia, and direct cardiotoxicity. We describe herein one case of OP poisoning, recently admitted in our emergency department and which was complicated by acute onset atrial fibrillation which reverted to sinus rhythm following detoxification of OP compound.
Keywords: Atrial fibrillation, cardiac toxicity, organophosphorus pesticides
INTRODUCTION
Organophosphorus (OP) pesticide poisoning accounts for as much as 80% of pesticide-related hospital admissions.[1] The mortality rate is between 2% and 30% despite appropriate treatment; cardiac complications of acute OP poisoning are fatal but often overlooked; therefore, earliest prediction of profile of cardiac toxicity of OP poisoning is important to allow proper resource allocation and therapeutic aggressiveness so as to reduce mortality.[2] We describe herein one case of OP poisoning, complicated by acute onset atrial fibrillation.
CASE PRESENTATION
A 40-year-old man was referred in emergency department following OP compound ingestion accidentally. On examination, his pulse rate was 70/min irregular and a blood pressure of 110/80 mmHg; the sensorium altered by bilateral pinpoint pupils.
Auscultation revealed bilateral chest crepitations with no other adventitious heart sounds or murmur. Chest skiagram showed normal sized cardiac shadow with mild pulmonary congestion. Exteremitist Fasciculations noted in calf muscles.
There was no significant past history of chronic alcoholism, hypertension, ischemic, or any valvular heart disease.
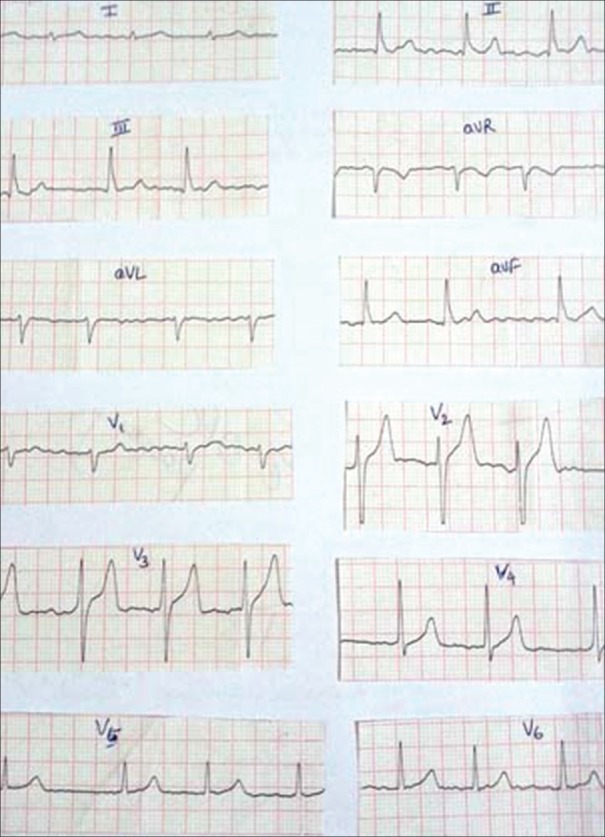
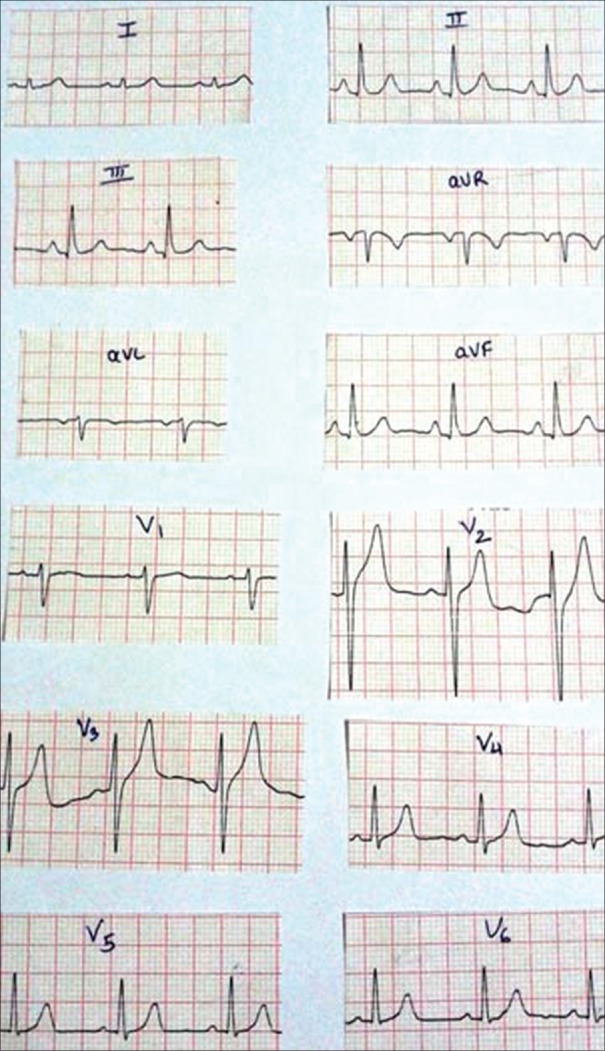
Electrocardiographic (ECG) revealed atrial fibrillation [Figure 1]. A two-dimensional echocardiogram was then done, which showed normal study with respect to valvular morphology and ventricular functions. Routine laboratory findings demonstrated adequate hemoglobin, normoglycemia with normal serum electrolytes, and total leukocytic count. Renal, liver, and thyroid function tests were within normal limit. Following gastric lavage, patient was started intravenous atropine, pralidoxime, and magnesium sulfate infusion, to which he responded and started improving clinically. Subsequent ECG done showed reversion to normal sinus rhythm [Figure 2].
Figure 1.
Electrocardiogram showing atrial fibrillation
Figure 2.
Subsequent electrocardiographic showing reversion to sinus rhythm
DISCUSSION
OP compounds act as irreversible cholinesterase inhibitors. Toxicity of these compounds leads to cholinergic excess symptoms through the muscarinic, nicotinic, and central nervous system receptors.
Cardiac complications may vary from asymptomatic ECG abnormalities such as sinus tachycardia, sinus bradycardia, atrioventricular block, prolonged Q-Tc interval, and ST-T changes to life-threatening complications such as cardiac arrhythmias, hypertension, hypotension, myocardial ischemia, and noncardiogenic pulmonary edema.[3,4] Paul and Bhattacharyya[5] found prolonged Q-Tc interval was the most common ECG abnormality in OP poisoning patients, found in 67 patients (62.6%), followed by sinus tachycardia in 36 patients (33.6%) and sinus bradycardia in 33 patients (30.8%). Elevation of ST segment was seen in 27 patients (25.2%) with T-wave inversion in 21 patients (19.6%). First-degree heart block (P-R interval >0.20 s) occurred in 9 cases (8.4%). Atrial fibrillation was seen in 5 patients (4.6%). Ventricular tachycardia occurred in 6 cases (5.6%) and ventricular premature complexes were noted in 3 patients (2.8%).
The mechanism of the cardiotoxic effect of OP compounds is complex.
Ludomirsky et al.[6] described the mechanism in three phases. First phase is a brief period of sympathetic overactivity which causes tachycardia and hypertension. These are considered nicotinic effects and may be due to excessive release of catecholamines. In practice, tachycardia is usually observed as a result of fear and anxiety. In the second phase, parasympathetic overactivity predominates for a more prolong period which is characterized by cholinergic excess and causes bradycardia, hypotension along with ST-T changes, and life-threatening arrhythmias. The last and third phase is longer, usually associated with a prolonged QT interval and polymorphic ventricular tachycardia (torsades de pointes) that can result in sudden death. Hence, daily ECG recording should be warranted in every patient of OP poisoning so as to reduce cardiac mortality.
CONCLUSION
Organophosphorus poisoning can be complicated by atrial fibrillation. So, daily electrocardiographic monitoring is warranted by the treating physician in such patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.International Programme on Chemical Safety, World Health Organization (WHO). Epidemiology of pesticide poisoning: Harmonized collection of data on human pesticide exposure in selected countries. Geneva, Switzerland: WHO Press; 2004. [Google Scholar]
- 2.Yamashita M, Yamashita M, Tanaka J, Ando Y. Human mortality in organophosphate poisonings. Vet Hum Toxicol. 1997;39:84–5. [PubMed] [Google Scholar]
- 3.Karki P, Ansari JA, Bhandary S, Koirala S. Cardiac and electrocardiographical manifestations of acute organophosphate poisoning. Singapore Med J. 2004;45:385–9. [PubMed] [Google Scholar]
- 4.Yurumez Y, Yavuz Y, Saglam H, Durukan P, Ozkan S, Akdur O, et al. Electrocardiographic findings of acute organophosphate poisoning. J Emerg Med. 2009;36:39–42. doi: 10.1016/j.jemermed.2007.08.063. [DOI] [PubMed] [Google Scholar]
- 5.Paul UK, Bhattacharyya AK. ECG manifestations in acute organophosphorus poisoning. J Indian Med Assoc. 2012;110:98, 107–8. [PubMed] [Google Scholar]
- 6.Ludomirsky A, Klein HO, Sarelli P, Becker B, Hoffman S, Taitelman U, et al. Q-T prolongation and polymorphous (torsade de pointes) ventricular arrhythmias associated with organophosphorus insecticide poisoning. Am J Cardiol. 1982;49:1654–8. doi: 10.1016/0002-9149(82)90242-9. [DOI] [PubMed] [Google Scholar]