Abstract
Neurofibromatosis 1 (NF1) patients are generally at higher risk of developing common malignant tumors such as brain and soft tissue tumors. These patients are 5-fold increased the risk of developing breast cancer by the age of 50 years after that the risk remains the same. The most common reported cancer is infiltrating duct carcinoma. We report a case of 61-year-old female with NF1 presented with pain and breast lump for the past 2 months. On mammography, a retroareolar solid cystic lesion measuring 32 mm × 30 mm × 30 mm was noted which was definitive for malignancy. Right-modified radical mastectomy with axillary lymph node dissection was done which revealed a neoplasm composed of glandular and squamous components. Immunohistochemically, these cells were triple negative for estrogen receptor, progesterone receptor, and human epidermal growth factor receptor 2-neu and expressed markers of basal cell differentiation. The final pathological staging was T2N0M0. This is the fourth case report in the English literature with such association. In this case report, we discussed the importance of breast cancer screening in such patients along with a review of the literature.
Keywords: Breast screening, metaplastic, neurofibromatosis
Introduction
Neurofibromatosis 1 (NF1) is an autoimmune dominant disorder characterized by development of multiple peripheral nerve sheath tumors, café au lait spots, skeletal dysplasia, and learning disabilities with an estimated incidence of 1 in 2500 and prevalence of 1 in 4000 individuals.[1] The gene which is cloned is neurofibromin, a tumor suppressor gene that aids in the hydrolysis of RAS GTP (guanosine triphosphate), to RAS GDP (guanosine diphosphate). Due to its absence, RAS will be inactive form thereby stimulating cell proliferation. These patients are more prone to the development of brain tumors, malignant peripheral nerve sheath tumors, and soft tissue tumors, but they are also susceptible to develop cancers that occur in the general population.
Women with NF1 are at 5-fold risk of developing breast cancers with the most common subtype being duct carcinoma.[2] Metaplastic cancer is a rare variant of duct carcinoma and accounts for <5% of breast cancers.[3] It can occur in patients with NF1. Only three cases are reported in the English literature.[4,5,6] Herein, we discussed a case of metaplastic carcinoma in an elderly female and stressed on the importance of diagnosing such cancers in NF1 patients.
Case Report
A 61-year-old female patient presented with complaints of pain in the right breast for 2 months associated with swelling for 1½ months. She was a known case of neurofibromatosis diagnosed at the age of 17. She gave a history of hormone injection for the breast development, after which she developed cutaneous nodules. On examination, multiple cutaneous nodules and an ill-defined hard mass in the central quadrant of the right breast were noted. Her left breast and bilateral axilla were normal. A retroareolar solid cystic lesion measuring 32 mm × 30 mm × 30 mm was noted in mammogram which was reported as BIRADS 5. Her other routine investigations were within the normal limits. The clinical staging was cT2N0M0. Fine-needle aspiration cytology yielded a cellular discohesive cluster of neoplastic cells exhibiting vesicular nuclei, prominent nucleoli, and moderate amount of cytoplasm-favoring ductal carcinoma. The patient underwent right-modified radical mastectomy with axillary lymph node dissection.
On gross examination, a grayish-white hard lesion was noted in the central quadrant measuring 3.5 cm × 3 cm × 3 cm with focal areas of cystic degeneration. The overlying skin showed multiple cutaneous nodules ranging in size from 0.3 to 1 cm. On histopathology, an infiltrating neoplasm composed of markedly pleomorphic cells arranged in sheets, nests, and cords with areas of squamous differentiation. Lymphovascular and perineural invasion were absent. Sections from the cutaneous nodules revealed a neoplasm composed of wavy spindle-shaped cells. There was no evidence of metastasis in the harvested eight axillary lymph nodes. On immunohistochemistry, the cells were negative for estrogen receptor, progesterone receptor, and human epidermal growth factor receptor 2-neu and positive for luminal markers such as CK5/6, P63, SMA, and S-100. The cutaneous nodules showed interspersed S-100-positive cells which were consistent with neurofibromas [Figure 1]. A final diagnosis of grade III metaplastic carcinoma with the pathological staging of pT2N0M0 was made. After surgery, the patient was advised chemotherapy, but she lost to follow up.
Figure 1.
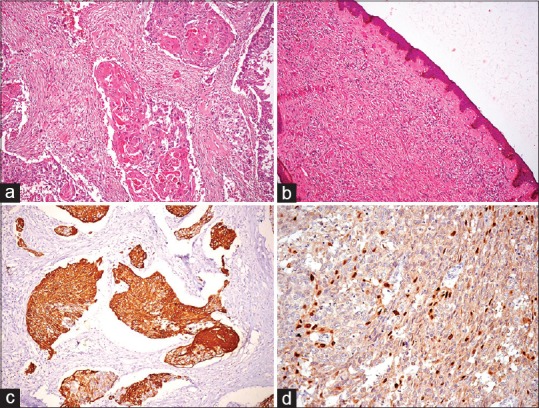
(a) Infiltrating neoplasm composed of sheets and nests of atypical cells exhibiting squamous differentiation (H and E, ×200). (b) Section from nipple showing wavy spindle-shaped cells admixed with fibroblasts (H and E, ×200). (c) Immunohistochemistry for CK5/6 showing diffuse cytoplasmic positivity (×200). (d) Immunohistochemistry for P63 showing nuclear positivity (×200)
Discussion
NF1 patients are at increased risk of developing common malignancies particularly before the age of 50 with an estimated cumulative risk of 20%.[7] Sharif et al. had first reported that women with NF1 were 4.9-fold risk of developing breast cancer by the age of 50 as compared to the general population.[2] In a study conducted in the United States by Madanikia et al., the standardized incidence ratio was 4.41 for women <50 years versus 0.94 for women aged more than or equal to 50 years.[8] Hence, women with NF1 are fivefold at increased risk of developing breast cancer. The most commonly reported subtype is duct carcinoma. The relationship of NF1 with breast cancer is still unclear. Loss of heterozygosity in the NF1 gene supported its role in tumor progression.[9]
Metaplastic carcinomas are a heterogeneous group of breast cancers accounting for <5% of overall breast cancers. It is defined as in which adenocarcinoma component is found to coexist with squamous, spindle cell, chondroid, or bone-forming neoplastic cells. The nonglandular component can be found in varying proportions. The association of metaplastic cancer with NF1 is very rare. There are only three such cases which are reported in the English literature,[4,5,6] of which two are more than 50 years of age as similar to this case. NF1 patients generally are at increased risk of breast cancer before the age of 50. Metaplastic carcinomas occur generally in older patients hence is not surprise to found large majority of these cancers in patients aged more than 50 years. The diagnosis is usually delayed in the reported cases due to the misinterpretation of breast mass as neurofibromas. In this case, in spite of pain for 2 months, the patient took medical advice at a later date due to the thought that the pain may be due to neurofibromas. Of three reported cases, two had histology of carcinoma sarcoma and one had histology of squamous cell carcinoma. Our case had both glandular and squamous component-favoring adenosquamous carcinomas. Metaplastic carcinoma generally present at a later stage (stage II or III) with a tumor size >3 cm as similar to this case. The incidence of axillary lymph node metastasis is generally low ranging from 13% to 54%.[10] The reason is hematogenous spread is more common in this subtype than lymphatic spread. In this case, the harvested eight axillary lymph nodes showed no evidence of metastasis. These neoplasms are generally triple negative. The prognosis is generally considered poor[11] due to the presentation at a higher grade, larger tumor size, and lack of benefit from hormonal therapy.
Conclusion
Patients with NF1 generally seek medical attention at a later date for breast lumps hence should undergo routine breast screening not only till the age of 50 years but also throughout their life due to the development of these rare high-grade cancers at a later date with poor prognosis. The association of this subtype with NF1 needs to evaluate on larger studies.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Evans DG, Howard E, Giblin C, Clancy T, Spencer H, Huson SM, et al. Birth incidence and prevalence of tumor-prone syndromes: Estimates from a UK family genetic register service. Am J Med Genet A. 2010;152A:327–32. doi: 10.1002/ajmg.a.33139. [DOI] [PubMed] [Google Scholar]
- 2.Sharif S, Moran A, Huson SM, Iddenden R, Shenton A, Howard E, et al. Women with neurofibromatosis 1 are at a moderately increased risk of developing breast cancer and should be considered for early screening. J Med Genet. 2007;44:481–4. doi: 10.1136/jmg.2007.049346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosen PP. Rosen's Breast Pathology. 3rd ed. Philadelphia, PA, USA: Wolters Kluwer; 2009. [Google Scholar]
- 4.Natsiopoulos I, Chatzichristou A, Stratis I, Skordalaki A, Makrantonakis N. Metaplastic breast carcinoma in a patient with Von Recklinghausen's disease. Clin Breast Cancer. 2007;7:573–5. doi: 10.3816/CBC.2007.n.015. [DOI] [PubMed] [Google Scholar]
- 5.Vivas AP, Bomfin LE, Pinto CA, Nicolau UR, Alves FA. Oral metastasis of metaplastic breast carcinoma in a patient with neurofibromatosis 1. Case Rep Oncol Med 2014. 2014:719061. doi: 10.1155/2014/719061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chaudhry US, Yang L, Askeland RW, Fajardo LL. Metaplastic breast cancer in a patient with neurofibromatosis. J Clin Imaging Sci. 2015;5:17. doi: 10.4103/2156-7514.154102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Walker L, Thompson D, Easton D, Ponder B, Ponder M, Frayling I, et al. A prospective study of neurofibromatosis type 1 cancer incidence in the UK. Br J Cancer. 2006;95:233–8. doi: 10.1038/sj.bjc.6603227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Madanikia SA, Bergner A, Ye X, Blakeley JO. Increased risk of breast cancer in women with NF1. Am J Med Genet A. 2012;158A:3056–60. doi: 10.1002/ajmg.a.35550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Güran S, Safali M. A case of neurofibromatosis and breast cancer: Loss of heterozygosity of NF1 in breast cancer. Cancer Genet Cytogenet. 2005;156:86–8. doi: 10.1016/j.cancergencyto.2004.04.019. [DOI] [PubMed] [Google Scholar]
- 10.Choi BB, Shu KS. Metaplastic carcinoma of the breast: Multimodality imaging and histopathologic assessment. Acta Radiol. 2012;53:5–11. doi: 10.1258/ar.2011.110341. [DOI] [PubMed] [Google Scholar]
- 11.Hu Q, Chen WX, Zhong SL, Li J, Luo Z, Tang JH, et al. Current progress in the treatment of metaplastic breast carcinoma. Asian Pac J Cancer Prev. 2013;14:6221–5. doi: 10.7314/apjcp.2013.14.11.6221. [DOI] [PubMed] [Google Scholar]


