Abstract
Rhabdomyosarcoma (RMS) is a rare soft tissue sarcoma. The already documented data regarding RMS state that it is more prevalent in males than females and also that its occurrence is more in Caucasians than Asians. The current incidence of RMS is 4.5 cases/million, and thus, it is a very rare cancer. The undifferentiated type is the most aggressive one with a rare presentation in the retroperitoneum. Overall, this case emphasizes that consideration should be given to wide range of diagnosis and that frozen section is the gold standard for a confirmatory diagnosis, as the first biopsy showed benign cells within the tumor. The emphasis on the interventions related to imaging to prevent the chance of aggravated presentation in the terminal stage of somatic comorbidities like loss of power. Radical excision of the mass along with normal iliopsoas tendon was done and referred to a cancer specialty center for further chemotherapy. To the best of my knowledge, this is the only case of RMS of the iliopsoas.
Keywords: Iliopsoas, pleomorphic, retroperitoneal, rhabdomyosarcoma
Introduction
Rhabdomyosarcoma (RMS) is a soft tissue sarcoma most commonly found in children and adults below the age of 18 years. It is considered to be a disease of the childhood and less common in old age.[1] Overall, a RMS is already very aggressive and rare in its nature. The incidence of RMS is 4.5 cases/million children/adolescents/year and in more than 50% of cases, RMS occurs during the first decade of life.[2,3] The common primary sites for RMS are head and neck region (25%), genitourinary tract (22%), and extremities (18%).[4,5] Less common primary sites include the trunk, perineal region, and abdomen, including the retroperitoneum.[5] Thus, the presence of RMS on the iliopsoas muscle in a 65-year-old female patient makes it an infrequent case. On biopsy, the histology report confirmed an undifferentiated sarcoma, which has a higher incidence (19%) than children do (<2%).[6]
Case Report
A 65-year-old female patient presented with the chief complaints of pain in the left iliac fossa (LIF) radiating to the left thigh for the past 2 months. Initially, she could carry out her routine work with a performance status (Eastern Cooperative Oncology Group) of 1 which worsened to a status of 2 as the pain intensified to be spasmodic. There was no history of bleeding per rectum, constipation. On clinical examination, a mass-like sensation which was felt after deep palpation in the LIF. Due to the adhesive mass, there was a flexion deformity with inhibition of hip extension. The flexion deformity gradually increased over 2 months with complete loss of extension [Figure 1]. A provisional diagnosis of an abdominal lump in the LIF was made. On palpation, there was tenderness, mass felt smooth, firm, and afebrile. Application of Thomas test helped me define the exact flexion deformity, which was around 40°–45°. She was evaluated with computed tomography (CT) scan of the abdomen and the pelvis which showed a large well defined soft tissue density mildly enhancing lesion in LIF involving the psoas and iliac muscles and extending to the inguinal region of the size: 11.3 cm × 7.4 cm × 5.8 cm [Figure 2]. There were calcific foci within the mass. A confirmatory histopathological examination represented a mass showing diffuse undifferentiated sarcoma cells. Thus, the diagnosis of the tumor was pleomorphic RMS with a pathological staging of pT2 N0 M0. Complete surgical resection of the main tumor, along with some surrounding normal tissue of the iliopsoas was achieved [Figure 3].
Figure 1.
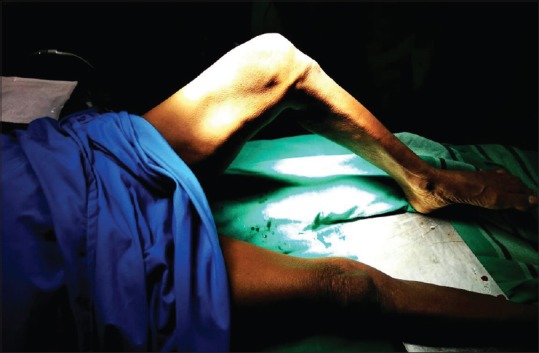
Involuntary flexion of the hip depicting flexion deformity due to the retroperitoneal mass over iliopsoas muscle
Figure 2.

There is a mass present retroperitoneally on the left side in the area of iliacus and psoas muscle (T12–L1)
Figure 3.

Complete surgical excision of the sarcoma with surrounding tissue around it
Discussion
We present a case of RMS with a rare presentation at the iliopsoas in an elderly female which was diagnosed on CT scan and core biopsy. RMS is mainly considered to be a children's disease with the predilection of alveolar and embryonal type.[3] Less commonly in adult males.[7] The histopathology shows that males have a higher incidence of pleomorphic histology (19%) than do children (<2%). However over here, the patient is a female in her sixties. The statistics are predominantly applicable for adolescents, but in elderly, a higher incidence of tumors are seen in unfavorable sites.[6] A CT guided management of this patient was a simple resection of the tumor along with some normal iliopsoas inserting at the lesser trochanter of the femur, which led to the loss of power [Figure 4]. Usually, the prognosis is good for the patients below <15 years of age, but poor for adults associated with a high mortality.[6,8] The 5-year survival rate for tumours in the retroperitoneum showed just 67% as stated by Crist et al.[4] Due to unavailable immunohistochemistry, the tumour did not undergo differential diagnosis. Due to the insidious signs, symptoms, negative investigations, and delayed imaging lead to a postsurgical loss of power, leaving the patient crippled; which could have been avoided. By examining the muscles in both the legs. The tone was normal in both the limbs along with nutrition. The power of the left limb decreased to a grade of 3.
Figure 4.
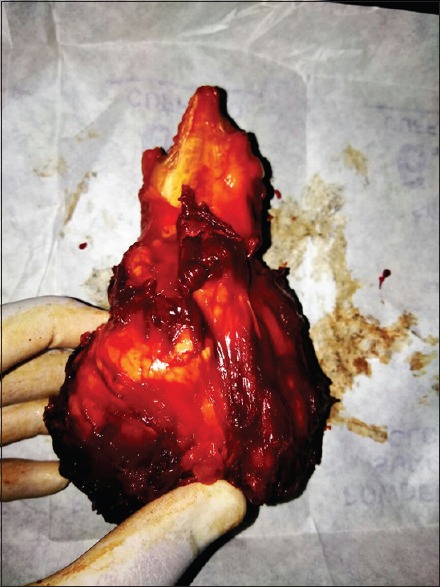
Totally resected mass along with the iliopsoas tendon in its upper pole defining loss of the corresponding muscle action (hip flexion)
Implication
RMS should not be diagnosed with a scan and biopsy. An excisional biopsy is a way to go and confirmed by frozen section during the surgery. Furthermore, delayed investigations and imaging can lead to added burden postoperatively. To the best of our knowledge, this is the only reported case of RMS involving the iliopsoas.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to acknowledge Mr Ramprasad Bhosale (JRF) for collection of patient's details
References
- 1.Perez EA, Kassira N, Cheung MC, Koniaris LG, Neville HL, Sola JE, et al. Rhabdomyosarcoma in children: A SEER population based study. J Surg Res. 2011;170:e243–51. doi: 10.1016/j.jss.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 2.Ries LG, Smith MA, Gurney JG, Linet M, Tamra T, Young JL, et al. Cancer Incidence and Survival among Children and Adolescents: United States SEER Program 1975-1995. National Cancer Institute (NCI), Bethesda, USA. 1999 [Google Scholar]
- 3.Ognjanovic S, Linabery AM, Charbonneau B, Ross JA. Trends in childhood rhabdomyosarcoma incidence and survival in the United States, 1975-2005. Cancer. 2009;115:4218–26. doi: 10.1002/cncr.24465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crist W, Gehan EA, Ragab AH, Dickman PS, Donaldson SS, Fryer C, et al. The third intergroup rhabdomyosarcoma study. J Clin Oncol. 1995;13:610–30. doi: 10.1200/JCO.1995.13.3.610. [DOI] [PubMed] [Google Scholar]
- 5.Maurer HM, Gehan EA, Beltangady M, Crist W, Dickman PS, Donaldson SS, et al. The intergroup rhabdomyosarcoma study-II. Cancer. 1993;71:1904–22. doi: 10.1002/1097-0142(19930301)71:5<1904::aid-cncr2820710530>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 6.Sultan I, Qaddoumi I, Yaser S, Rodriguez-Galindo C, Ferrari A. Comparing adult and pediatric rhabdomyosarcoma in the surveillance, epidemiology and end results program, 1973 to 2005: An analysis of 2,600 patients. J Clin Oncol. 2009;27:3391–7. doi: 10.1200/JCO.2008.19.7483. [DOI] [PubMed] [Google Scholar]
- 7.Lim SM, Yoo CJ, Han JW, Cho YJ, Kim SH, Ahn JB, et al. Incidence and survival of pediatric soft tissue sarcomas: Comparison between adults and children. Cancer Res Treat. 2015;47:9–17. doi: 10.4143/crt.2013.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salunke AA, Shah J, Gupta N, Pandit J. Adult rhabdomyosarcoma: Multimodality management and results. J Cancer Res Ther. 2017;13:384. doi: 10.4103/0973-1482.180606. [DOI] [PubMed] [Google Scholar]


