Abstract
IN BRIEF Bariatric surgery is the most efficacious treatment for obesity, type 2 diabetes, and other obesity-related comorbidities. In this article, the authors review the current indications for bariatric surgery and discuss the most commonly performed procedures. They analyze medical outcomes of bariatric procedures by reviewing key prospective trials and discuss changes in physiology after these procedures. They conclude by discussing long-term management of bariatric patients by reviewing current guidelines for nutritional support and listing common complications related to these procedures.
Obesity is a global pandemic affecting nearly 2.1 billion adults worldwide (1). In the United States, more than one-third of adults are obese (2). The accumulation of adiposity is linked to hyperlipidemia, impaired insulin sensitivity, susceptibility to thrombosis, inflammation, and endothelial dysfunction, resulting in increased risk for cardiovascular disease, nonalcoholic fatty liver disease (NAFLD), and type 2 diabetes (3–5). Even modest weight loss among people with obesity has been shown to improve overall morbidity (6). Unfortunately, weight recidivism and relapse is common among patients undergoing medical management of weight loss (7).
Bariatric surgery is currently the most efficacious long-term treatment for weight loss and improvement in obesity-related diseases (8–10). Although bariatric surgery has become increasingly safe with advancements in laparoscopic and endoscopic technologies, it remains an invasive and life-altering procedure with many possible short- and long-term complications (9). Several mechanisms for the efficacy of bariatric surgery have been postulated, and these may provide useful pharmacological targets to narrow the gap between medical and surgical management of obesity in the future.
To assist primary care providers (PCPs) in managing patients with bariatric surgery and properly referring patients who may benefit from bariatric surgery, we provide a review of the current indications for bariatric surgery, the most common procedures, common short- and long-term complications, and current proposed mechanisms contributing to the efficacy of surgery.
Indications for Bariatric Surgery
Current indications for surgery are shown in Table 1. Initially developed by the National Institutes of Health in 1991 as a consensus guideline statement, the accepted indications have not changed noticeably since then. However, periodic reviews by associated societies have been performed and published (11,12).
TABLE 1.
Indications for Bariatric Surgery
| • BMI ≥40 kg/m2 without comorbidities or |
| • BMI 35.0–39.9 kg/m2 with at least one serious comorbidity, including but not limited to: |
| ❍ Type 2 diabetes |
| ❍ Obstructive sleep apnea |
| ❍ Hypertension |
| ❍ Hyperlipidemia |
| ❍ NASH/NAFLD |
| ❍ Obesity-hypoventilation syndrome |
Patients should be considered for referral to a bariatric surgery center if they have a current BMI ≥40 kg/m2 or a BMI of 35.0–39.9 kg/m2 with at least one comorbidity, including type 2 diabetes, obstructive sleep apnea, hypertension, NAFLD, and others (13). There is evidence from Asian trials supporting the expansion of the criteria for bariatric surgery to include patients with uncontrollable type 2 diabetes or metabolic syndrome and a BMI of 30.0–34.9 kg/m2 (14). However, the long-term effects of surgery in this population are unknown.
Importantly, there are several contraindications to bariatric surgery that must be addressed before undertaking operative intervention. Medical conditions, including severe coagulopathy and cardiac/pulmonary diseases, may preclude the surgical and anesthetic risks associated with a procedure. Another important consideration is a patient’s mental fitness to undergo this life-altering intervention. A thorough psychiatric evaluation is necessary to screen out undiagnosed or untreated mental illness, drug or alcohol abuse, an insufficient social support system, and inability to observe lifelong nutritional requirements. Inadequate psychological assessment can lead to diminished metabolic efficacy and significant long-term morbidity (15).
As part of the preoperative assessment of patients being considered for metabolic surgery, some bariatric centers suggest or require a prespecified weight loss, and most use a prescribed meal-replacement plan with protein shakes or a similar regimen during the 2 weeks before surgery. The rationale behind presurgical weight loss includes a possible mitigation of operative complications with modest weight loss, reduction of liver size before surgery, and a period of demonstration of ability to adhere to strict nutritional requirements postoperatively (16). Some insurance plans require patients to achieve some weight loss before bariatric surgery. At our center, we require weight loss of at least 10 lb (4.5 kg) after a patient’s initial dietitian consultation before we finalize plans for bariatric surgery.
Operative Procedures
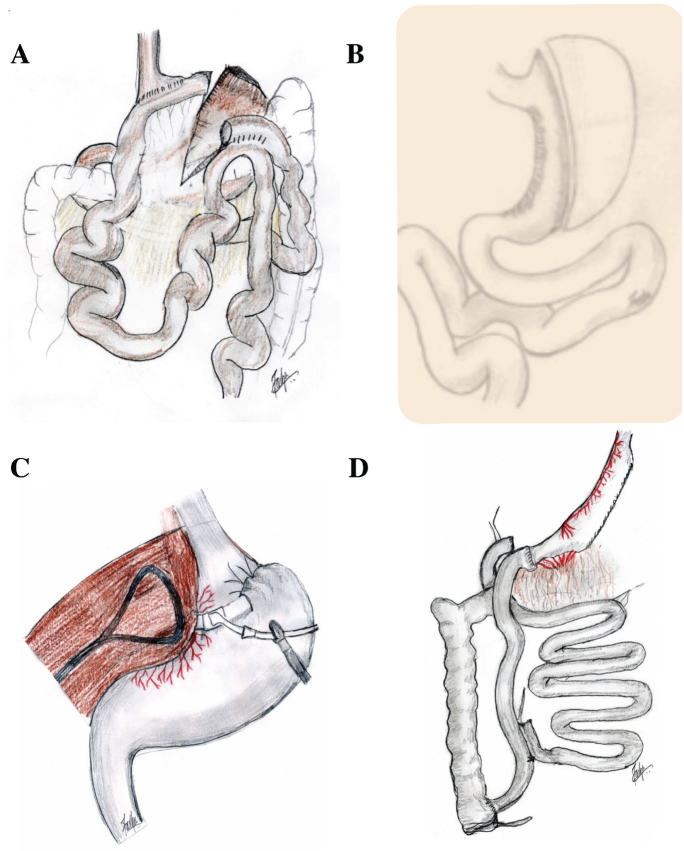
To manage patients appropriately, it is important for PCPs to understand the anatomical changes underlying bariatric procedures. The most commonly performed procedures today include the vertical sleeve gastrectomy (VSG) and the Roux-en-Y gastric bypass (RYGB). Laparoscopic adjustable gastric banding (LAGB) and biliopancreatic diversion with duodenal switch (DS) are performed less commonly now but were routinely performed in the past. Patients who have undergone these procedures may still present to PCPs in clinic, and thus it is important to understand their anatomy as well. Currently, most bariatric procedures are routinely performed laparoscopically, which reduces the incidence of surgical site infection, abdominal wall hernia, and postsurgical stress (17). The resultant surgical anatomies of the three most common procedures are shown in Figure 1.
FIGURE 1.
Modern bariatric surgical procedures: A) Roux-en-Y gastric bypass, B) vertical sleeve gastrectomy, C) adjustable gastric banding, and D) duodenal switch.
Although RYGB is diminishing in popularity, it remains the gold standard of efficacy for metabolic procedures. This procedure is performed by creating a small proximal gastric pouch and separating this pouch from the distal stomach. The small intestine is then divided 30–100 cm distal to the ligament of Treitz, thus creating the biliopancreatic limb. A gastrojejunostomy is formed between the distal end of the separated limb of small bowel and the gastric pouch. This portion of intestine is the alimentary limb, called the Roux limb after a 19th century Swiss surgeon. The biliopancreatic conduit is then connected to the Roux limb 75–150 cm from the gastrojejunostomy. An increase in the length of the Roux limb increases the malabsorption seen after the procedure, although it has not always been clear how much of this is calorie malabsorption versus micronutrient malabsorption. Roux-en-Y anatomy is thus created with the alimentary Roux limb, the biliopancreatic limb diverting digestive enzymes, and the common channel distally, where most nutrient absorption occurs.
The VSG was initially developed as the initial portion of a two-stage approach to weight loss (18). The procedure entails mobilization of the greater curvature of the stomach from the fat and vessels of the omentum. The anesthesia team passes a bougie (typically 32–40 French in size) into the stomach, and the stomach is divided using laparoscopic stapling devices starting several centimeters from the pylorus and continuing toward the angle of His close to the gastroesophageal junction. In this manner, the greater curvature of the stomach is removed as a partial gastrectomy specimen, and, as a result, the operation cannot be reversed.
The LAGB is a purely restrictive procedure that was commonly performed years ago, but is now only rarely performed except in Australia (19). It involves encircling the upper stomach with a soft silicone balloon below the gastroesophageal junction. The silicone ring is connected to an infusion port that is placed subcutaneously. This allows adjustment of the degree of restriction by infusion or removal of saline from the subcutaneous port.
The DS is typically performed at fewer centers because of its complexity and challenges with postoperative care (19). In this procedure, the proximal duodenum is divided, and a sleeve gastrectomy is performed. Subsequently, the distal ileum is divided, with the distal portion of the ileum connected to the stomach and the proximal portion anastamosed to the terminal ileum 50–100 cm from the ileocecal valve. DS was originally and is now sometimes performed in two steps: the first creating the sleeve gastrectomy and the second performing the intestinal rearrangement. The DS offers the greatest weight loss (20) but carries a significant morbidity profile given the induced malabsorption.
There are also a number of U.S. Food and Drug Administration (FDA)-approved medical devices available for weight loss other than the adjustable gastric banding devices, although these are typically classified as investigational by insurance companies, and treatment availability for patients is limited because of lack of insurance coverage. These include intragastric balloon, vagal blockade, and aspiration therapy (21–23). The vagal blockade device and two intragastric balloon devices are now FDA-approved and have demonstrated modest weight loss in randomized, controlled trials (21,22). Otherwise, these procedures are primarily investigative and are beyond the scope of this review, although they are described elsewhere in this issue (p. 258).
Medical Outcomes After Bariatric Surgery
Bariatric surgery has been analyzed with numerous randomized trials and retrospective reviews. Overall, results suggest that RYGB and VSG have similar weight loss profiles. Patients normally lose weight rapidly during the first few months, followed by continued but slower weight loss for 1–2 years until weight loss plateaus (24). The Swiss Multicenter Bypass or Sleeve Study demonstrated similar weight loss between VSG and RYGB at 1 year (72.3 vs. 76.6% loss of excess BMI [BMI ≥25 kg/m2] for VSG and RYGB, respectively) (25). The latest results demonstrate that there is no difference in weight loss outcomes at 3 years (70.9 vs. 73.8% excess BMI loss for VSG and RYGB, respectively) (10). Long-term randomized trials are lacking, but retrospective reviews show that weight loss after RYGB peaks at 74% reduction in excess BMI at 2 years, and 52% at 10 years (24). Given the relatively new rise in popularity of the VSG, long-term data are sparse. Weight loss is slower after LAGB than after RYGB or VSG and also usually stabilizes after 2 years (26).
Bariatric surgery is also effective for the treatment of type 2 diabetes. A number of randomized trials have confirmed the benefits of bariatric surgery over medical management alone for type 2 diabetes. Interestingly, there appears to be improvement in metabolism acutely after RYGB, suggesting weight loss–independent mechanisms in the improvement in glycemic control (27).
The randomized trials exploring the effects of bariatric surgery on type 2 diabetes are summarized in Table 2. Schauer et al. (28,29) randomized patients with an A1C of >7.0% and a BMI of 27–43 kg/m2 to RYGB, VSG, or medical management alone. At 1 year, 42% of RYGB, 37% of VSG, and 12% of medically managed patients reached the endpoint of an A1C <6.0%. Recently, the 5-year results of this trial were published, demonstrating that 29% of RYGB and 23% of VSG patients had fulfilled the primary outcome, whereas 5% of medically managed patients had achieved this endpoint (30).
TABLE 2.
Randomized Trials Evaluating the Effects of Bariatric Surgery on Type 2 Diabetes
| Surgical Procedure(s) | Inclusion Criteria | Primary Endpoint | Percentages of Patients Reaching Primary Endpoint | |
|---|---|---|---|---|
| Schauer et al. (28–30) | RYGB (n = 50), VSG (n = 50), and LS/MM (n = 50) | BMI 27.0–43.0 kg/m2 and A1C >7.0% | A1C <6.0%, with or without medications | • 1 year: RYGB 42%, VSG 37%, LS/MM 12% |
| • 3 years: RYGB 38%, VSG 24%, LS/MM 5% | ||||
| • 5 years: RYGB 29%, VSG 23%, LS/MM 5% | ||||
| Mingrone et al. (20) | RYGB (n = 20), DS (n = 20), and LS/MM (n = 20) | BMI ≥35 kg/m2, A1C ≥7.0%, and >5-year history of type 2 diabetes | Fasting glucose <101 mg/dL, A1C ≤6.5%, and off diabetes medication for 1 year | • 2 years: RYGB 75%, DS 95%, LS/MM 0% |
| • 5 years: RYGB 37%, DS 63%, LS/MM 0% | ||||
| Ikramuddin et al. (8,31) | RYGB (n = 60) and LS/MM (n = 60) | BMI 30.0–39.9 kg/m2, A1C ≥8.0%, C-peptide >1.0 ng/mL, and >6-month history of type 2 diabetes | A1C <7.0%, LDL cholesterol <100 mg/dL, and systolic blood pressure <130 mmHg | • 1 year: RYGB 49%, LS/MM 11% |
| • 2 years: RYGB 43%, LS/MM 14% | ||||
| • 3 years: RYGB 28%, LS/MM 9% | ||||
| Courcoulas et al. (26) | RYGB (n = 20), LAGB (n = 21), and LS/MM (n = 20) | BMI 30.0–40.0 kg/m2, fasting glucose >125 mg/dL, and treatment with antidiabetic medications | Absence of diabetes medications, A1C <6.5%, and fasting glucose <125 mg/dL | • 1 year: RYGB 67%, LAGB 50%, LS/MM 0% |
| • 3 years: RYGB 40%, LAGB 29%, LS/MM 0% |
LS/MM, lifestyle modification and medical management.
The Diabetes Surgery Study (8,31) was another multicenter randomized trial evaluated the role of RYGB in patients with type 2 diabetes (A1C >8%) and a BMI of 30–39.9 kg/m2. Intensive medical management with RYGB improved achievement of the primary endpoint (A1C <7%, LDL cholesterol <100 mg/dL, and systolic blood pressure <130 mmHg) when compared to intensive medical management alone (49 vs. 19% for RYGB and medical management, respectively).
An Italian randomized trial by Mingrone et al. (20) found that, compared to medical management, RYGB and DS were more successful than medical management at achieving remission of diabetes (defined as fasting glucose <100 mg/dL, A1C <6.5%, and the absence of pharmacological therapy) (75, 95, and 0% for RYGB, DS, and medical management cohorts, respectively). At 5 years, 37% of the RYGB and 63% of the DS patients had maintained remission of type 2 diabetes, whereas none in the medically managed group achieved remission.
Courcoulas et al. (26) completed a single-center trial comparing bariatric surgery (RYGB and LAGB) and intensive medical management. This study found that bariatric surgery resulted in partial remission of type 2 diabetes (defined as the absence of medications for type 2 diabetes with an A1C <6.5% and fasting glucose ≤125 mg/dL) or complete remission of type 2 diabetes (defined as the absence of medications for type 2 diabetes with an A1C <5.7% and fasting glucose ≤100 mg/dL) in 60% of patients undergoing RYGB, 29% of those having LAGB, and 0% of those receiving intensive medical management 1 year after initiation of the intervention. At 3 years, there was a decline in any remission for the RYGB cohort to 40%, whereas the remission rate in the LAGB group remained stable at 29% (26).
Other obesity-related comorbidities, including hypertension, hyperlipidemia, and obstructive sleep apnea, are significantly improved after bariatric surgery (9,32,33). Most of these benefits are also observed after lifestyle modifications inducing weight loss; however, some of these modifications may not be feasible for all obese patients.
Resolution of gastroesophageal reflux disease (GERD) after bariatric surgery is inconclusive. RYGB may improve GERD symptoms, use of anti-reflux medications, and esophagitis (34). LAGB may also improve reflux postoperatively (35). Overall, it appears that the VSG may actually exacerbate GERD symptoms, although studies are mixed (36).
The resolution of nonalcoholic steatohepatitis (NASH) and NAFLD is also unclear. Some studies have shown histological improvements after bariatric surgery, but others have found no improvement and even worsening of fibrosis after RYGB (37). More study is necessary to evaluate the effect of bariatric surgery on these comorbidities.
In a burgeoning area of research, oncological outcomes may be affected by bariatric surgery. There has been an association between obesity and certain cancers; however, the impact of bariatric surgery on oncological outcomes is difficult to assess given the need for long-term intervals to evaluate for risk reductions. In studies evaluating an effect on long-term survival, all-cause mortality appeared to be reduced after bariatric surgery compared to an obese control group (38,39). Not surprisingly, bariatric surgery demonstrated a 56% reduction in cardiovascular death (40). However, cancer risk was also found to be reduced in bariatric surgery patients compared to obese control subjects. In the Swedish Obesity Database, bariatric surgery was found to lower the risk of cancer mortality with a more pronounced benefit seen in women (38). A review of the Utah Cancer Registry found that bariatric surgery decreased the incidence of cancer and cancer-related mortality (39).
Important to PCPs is the effect of bariatric surgery on pregnancy. Based on retrospective reviews and meta-analyses, it appears that bariatric surgery may improve obstetrical outcomes, including preeclampsia, gestational diabetes, and macrosomia (likely as a function of maternal reductions in BMI, insulin resistance, and hypertension) (41–44). For the infants of mothers who have previously undergone bariatric surgery, the effect of changes in metabolism and deficiencies in nutrition may increase the rate of prematurity, low APGAR scores, and small-for-gestational-age births. This is especially true in the first 2 years after bariatric surgery (42). This has lead the American College of Obstetricians and Gynecologists to recommend avoiding pregnancy during this period (43). Neonatal outcomes appear to improve 2–3 years after bariatric surgery (42). Research on this effect has focused on RYGB and has not been confirmed for VSG.
Changes in Physiology Associated With RYGB and VSG
Altered foregut anatomy is accompanied by a host of changes in enterohepatic physiology that are linked to whole-body energy metabolism. In particular, attention has been focused on changes in endocrine physiology in gastrointestinal (GI) tract, as well as from adipose tissue, changes in bile acid concentrations and signaling, and, more recently, shifts in the composition of the intestinal microbiota. This section will briefly discuss the basic physiology of each of these aspects, and changes that occur after bariatric surgery. These changes are summarized in Table 3.
TABLE 3.
Physiological Changes Associated With Bariatric Surgery
| Target | Function | Effect of RYGB | Effect of VSG |
|---|---|---|---|
| GLP-1 | Increases insulin production, reduces glucagon production, and reduces food intake | Increased | Increased |
| Peptide YY | Reduces food intake | Increased | Increased |
| Ghrelin | Increases food intake | Decreased | Decreased |
| Leptin | Increases with fat mass and regulates energy balance by reducing food intake | Decreased | Decreased |
| Adiponectin | Increases insulin sensitivity | Increased | Increased |
| Gut microbiome diversity | Thought to influence energy metabolism and inflammation | Increased | Increased |
| Bile acids | Thought to regulate lipid and glucose metabolism | Increased | Increased |
Endocrine Response
The GI tract is responsible for the secretion of myriad hormones that may affect dietary intake. Chief among these are the anorexigenic hormones glucagon-like peptide 1 (GLP-1) and peptide YY and the orexigenic hormone ghrelin (45,46). GLP-1, an incretin produced by the ileum, increases insulin and reduces glucagon production and has been a primary target of antidiabetic therapies (47). Strong evidence suggests that bariatric surgery induces an exaggerated incretin response, possibly accounting for one of its mechanisms of action beyond simple caloric restriction (48,49). Although both VSG and RYGB affect the incretin response, RYGB does so to a greater extent (50). This effect is not observed with LAGB, hypocaloric restriction, or intensive medical management (46,48,49). Furthermore, the degree of postprandial GLP-1 response after surgery has been proposed as an important determinant of weight loss and diabetes remission (51).
Peptide YY, also released from the distal GI tract, induces satiety and reduces food intake and has been observed to increase after bariatric surgery (45,50–53). In contrast, a reduction in peptide YY is observed after weight loss resulting from caloric restriction (54).
Circulating ghrelin concentrations, which are reduced with obesity, increase in the fasted state and in diet-induced weight loss (55–57). There appear to be distinct responses after VSG and RYGB. Whereas ghrelin appears to decrease after VSG, the impact of RYGB on ghrelin is controversial and unclear, with various studies indicating reductions, no change, or even increases (45,50,58).
In addition to enteric-derived hormones, adipose tissue has gained recognition as a complex endocrine organ intimately involved in energy metabolism and the development of metabolic syndrome (59,60). In the obese state, as adipocytes undergo hypertrophy, a spillover effect is observed at which point organs are exposed to the deleterious effects of unoxidized free fatty acids. Macrophage tissue infiltration and cytokine release ensues in adipose tissue (60,61).
Two important adipokines are leptin and adiponectin. Serum leptin concentrations increase in proportion to body fat stores and act on the central nervous system to regulate energy balance directly by reducing food intake (62–65). Thus, it is not surprising that a reduction in leptin is common after bariatric surgeries, including gastric banding, as well as medical weight loss (54,66–68). Adiponectin, a hormone with anti-atherogenic and insulin-sensitizing properties, has been observed to inversely correlate with serum tumor necrosis factor-α (69,70). Adiponectin markedly increases after weight loss from either caloric restriction or bariatric surgery (46,71,72).
Shifts in the Intestinal Microbiota
The gut microbiome has emerged as a new and exciting research frontier, particularly in the past decade. Although this field holds therapeutic potential, much remains unknown regarding underlying mechanistic relationships with the host. Evidence continues to emerge linking alterations in the composition of the intestinal microbiota with obesity, insulin resistance, and type 2 diabetes.
Nearly a decade ago, Turnbaugh et al. (73) identified compositional shifts in the intestinal microbiota favoring an increased capacity to harvest energy from the diet, thus linking the microbiome to obesity. Obesity is associated with reduced microbial diversity and richness and an altered composition (5). After bariatric surgery, the gut microbiome changes significantly and may contribute to weight loss. It is unclear whether these changes are the result of changes in diet or weight loss or are purely surgically driven.
At a functional level, it is predicted that shifts favor an increased potential for microbial utilization of macro- and micronutrients (74). Despite similar shifts at the phyla level, diversity appears to increase with RYGB, but not necessarily with VSG (74–77). Several specific changes appear to correlate with metabolic improvements, and the microbial composition among patients who achieve diabetes remission differed from that of patients who do not achieve remission by 1 year after RYGB or VSG.
Studies in mice have corroborated findings in humans. The transference of gut microbiota from mice having undergone RYGB to germ-free mice resulted in weight loss and decreased fat mass relative to recipients of microbiota from mice after sham surgery (78). Tremaroli et al. (79) built on these observations and found that transference of microbiota from humans post-bariatric surgery into germ-free mice led to reduced adiposity relative to mice humanized from obese controls.
It is important to note that, despite a large body of research in basic science, at present, clinical evidence of the effect of the microbiome on obesity and metabolic disease remains scarce. Overall, more evaluation is needed in this realm to confirm the importance of gut microbiota in obesity and characterize the effect of bariatric surgery on the microbiome.
Roles of Bile Acids
Bile acids (BAs) are synthesized from cholesterol by the liver and modified by intestinal microbiota (80). BAs and their relative composition are closely linked to the composition of intestinal microbiota (81,82). BAs function as signaling molecules, playing significant roles in metabolic pathways involved in lipid and glucose metabolism via the nuclear receptor farnesoid X receptor (FXR) and G protein–coupled receptor TGR5 (83,84). When activated, FXR induces the production of fibroblast growth factor-19 (FGF19). FGF19 enters the portal circulation and inhibits hepatic BA synthesis via CYP7A1, responsible for producing the primary BAs cholic acid and chenodeoxycholic acids. In the gut, the microbiome converts primary BAs into secondary BAs by dehydroxylation, creating deoxycholic and lithocholic acids. More than 95% of BAs are reabsorbed by the gut and transported back to the liver (85–87).
Strong evidence implicates FXR and TGR5 as crucial to the efficacy of VSG (88,89). In conjunction with studies in mice, humans studies have identified increased serum concentrations of BAs after bariatric surgery (90–94).
Interestingly, changes in BAs appear to accompany RYGB and VSG, but not necessarily medically managed weight loss. For example, in a cohort of patients calorically matched to our surgical cohorts, BAs actually decreased (90). Studies involving long-term weight loss programs of 6 months have observed reductions in serum BAs and GLP-1 despite significant weight loss (95). In patients included in the Diabetes Surgery Study (94), medically managed patients had no changes in BAs despite significant weight loss and metabolic improvement 1 year after treatment. Thus, an increase in serum BAs might be an important physiological change promoting metabolic improvement after RYGB and VSG.
Nutritional Management of Post-Bariatric Patients
Specific diets early after surgery are surgeon- and institution-dependent, but in all cases, patients should be instructed with the guidance of a bariatric registered dietitian (RD). Maintaining hydration is the most important factor in the early postoperative state. It is customary after bariatric surgery to introduce different textures and volumes in stages. Initially, patients are maintained on a clear-liquid diet for several days, followed by institution of a full-liquid diet as a source of protein. Eventually, patients are introduced to soft solid foods in several small, controlled meals (13).
In the long term, patients are normally followed through annual visits with a bariatric RD. It is important for PCPs to understand the key elements of post–bariatric surgery nutrition to provide excellent care to these patients. Micronutrient supplementation is essential for the long-term care of bariatric surgery patients (96).
The American Association of Clinical Endocrinologists, The Obesity Society, and the American Society for Metabolic & Bariatric Surgery released guidelines on the metabolic support of bariatric surgery patients (13). Although lacking a malabsorptive component, the VSG and LAGB are treated similarly to the RYGB. The guidelines recommend routine nutritional supplementation, including a standard multivitamin (containing the daily recommended intake of vitamin B12, thiamine, folic acid, vitamin K, biotin, zinc, iron, and copper), calcium, vitamin D, and elemental iron. Per these guidelines, patients should undergo routine laboratory monitoring every 3–6 months in the first year after surgery and annually thereafter. Laboratory testing should include complete blood count, electrolyte panel, iron studies, liver function tests, lipid panels and measurement of glucose, vitamin B12, and vitamin D.
It is also important to understand the complexities of micro- and macronutrient deficiencies associated with the DS procedure. Given the profound malabsorption in post-DS patients, this procedure carries a high risk for protein malnutrition, hypoalbuminemia, and micronutrient deficiency. Overall, patients who have undergone DS should be managed at specialized bariatric centers with expertise in this procedure.
Complications After Bariatric Surgery
Despite the success of bariatric surgery in treating obesity and metabolic disease, there are important complications to consider when managing post-bariatric patients. Each procedure has its own set of late complications. Understanding these complications allows PCPs a differential diagnosis when evaluating these patients after surgery.
The RYGB was previously the most commonly performed bariatric procedure in the United States. Despite its excellent medical outcomes, there are a number of complications resulting from its relatively complex alteration of GI anatomy.
Small-bowel obstruction is one relatively common complication after RYGB. The estimated lifetime incidence is 3–5% (97). Small-bowel obstruction presents with decreased bowel function, abdominal pain, nausea/vomiting, and bloating. Small-bowel obstruction after RYGB can be the result of surgical adhesions but is more commonly caused by internal hernias through the newly formed mesenteric defects. They can also be caused by intussusception or stenosis at the created anastomoses. Internal hernias can occur in up to 5% of patients after RYGB, despite current recommendations to close all mesenteric defects (17,98). Defects are normally found between the transverse mesocolon and Roux-limb mesentery or the mesenteries of the jejunojejunostomy. Internal hernias are diagnosed on CT scan with a characteristic “mesenteric swirl” sign and routinely require surgical decompression with closure of the defect (99). If a patient develops signs and symptoms of peritonitis and surgical treatment is delayed, that patient is at a high risk for bowel strangulation and ischemia.
Another potentially lethal long-term complication of RYGB is gastric remnant distension. Gastric remnant distension presents similarly to small-bowel obstruction and may occur in the same setting. Because the gastric remnant is not in continuity with the esophagus, patients with this condition may not develop vomiting. Although rare, gastric remnant distension can also occur in the setting of a paralytic ileus of the biliopancreatic limb. The gastric remnant represents a blind pouch and is at a higher risk of perforation if distended (100). The relatively large inoculum of bile and stomach acid creates a significant septic response should perforation occur; thus, this condition is a surgical emergency if diagnosed. Treatment requires immediate decompression either via surgical decompression or percutaneous gastrostomy tube placement.
Because two anastomoses are created during RYGB, this procedure is especially prone to stomal complications (101). Leaks, stenosis, and marginal ulcerations are all possible after RYGB.
Leaks occurs in up to 1% of RYGB (102). Leaks normally occur soon after surgery but can occur years later. These normally present with abdominal pain, which can radiate to the shoulders if there is diaphragmatic irritation; sepsis; and peritonitis. A number of possible treatment modalities exist that are beyond the scope of this review.
Stomal stenosis is a common complication after RYGB, occurring in 5–20% of patients (103). Several factors contribute to stenosis, including tissue ischemia or ulcer formation. Patients typically present with nausea, vomiting, and dysphagia. Soon after surgery, stenosis of the gastrojejunostomy may be caused by postoperative edema and should be treated conservatively until the edema resolves. After the perioperative period, stenosis is treated endoscopically with serial dilations (104). If endoscopic management fails, surgical revision of the gastrojejunostomy may be required.
Marginal ulcer is another common complication after RYGB, occurring in up to 15% of patients (105). Ulcers commonly form at the gastrojejunostomy site because of the acidic load on the nearby jejunum, but they can also form at other sites. Marginal ulcers present as either acute or chronic pain that worsens after eating. Similar to peptic ulcer disease, marginal ulcers are also caused by nonsteroidal anti-inflammatory use, smoking, and Helicobacter pylori infection (106). Removal of the inciting agent and proton pump inhibitors are the mainstays of treatment. Medical management is successful in the majority of patients, but surgical therapy may be required should the ulcer perforate or the patient remain symptomatic.
The rapidity of weight loss and altered BA profile after RYGB predisposes patients to cholelithiasis. About 40% of people who undergo RYGB develop gallstones postoperatively, and 40% of these people develop symptoms (107). There is evidence that ursodeoxycholic acid may decrease the frequency of stone formation (108). Some surgeons advocate for cholecystectomy to be performed at the time of RYGB, but this has not been shown to be efficacious (109). The development of choledocholithiasis is also a challenge after RYGB because the altered surgical anatomy makes endoscopically accessing the common bile duct challenging. Depending on the bariatric center’s level of endoscopic comfort, choledocholithiasis can be managed through combined surgical/endoscopic techniques or with surgical common bile duct exploration alone. Symptoms of cholelithiasis and its associated manifestations are similar to those of patients who have not undergone bariatric surgery.
Dumping syndrome is also a common complication after RYGB. Up to 10% of patients have moderate to severe symptoms of dumping syndrome after ingestion of high levels of carbohydrates (110). Early dumping refers to a rapid onset of symptoms, including abdominal pain, diarrhea, and tachycardia, after carbohydrate bolus. Early dumping syndrome occurs because of a rapid fluid shift and an alteration in sympathetic tone resulting from the hyperosmolar load in the bowel (111). This can usually be treated by lifestyle intervention to limit the amount of simple carbohydrates ingested at one time. Late dumping syndrome is a rare complication that occurs several hours after ingestion of carbohydrates (111). Although not thoroughly understood, symptoms are usually the result of hypoglycemia caused by a series of changes in neurohormonal pathways. Again, most patients can be treated with dietary modifications.
VSG has a lower complication rate than RYGB (112). Nevertheless, VSG still causes significant morbidity (113). The most common complications after VSG include gastric staple line leaks and stricture or narrowing of the sleeve.
Leaks are the most worrisome complication after VSG and can occur in 2–5% of patients (114). They are normally caused by ischemic factors at the relatively long staple line required to form the gastrectomy. Leaks present with abdominal pain sometimes radiating to the left shoulder, nausea, vomiting, peritonitis, and signs of sepsis. Treatment of leaks ranges from reoperation with primary repair to more conservative endoscopic/radiological management. Most bariatric surgeons prefer conservative management of leaks.
Sleeve stricture can cause cyclic vomiting syndrome and dehydration, along with dysphagia (115). This condition may be caused by technical factors at the time of surgery or by exuberant healing afterward. Treatment includes endoscopic dilation. However, if refractory, conversion to RYGB may be necessary.
Complications of LAGB include band erosion and slippage. Restriction of the band system may be reversed by removal of saline or by removal of the band, port, and tubing. Surgical removal has been necessitated by longer-term complications such as gastric prolapse, dysphagia associated with esophageal dysmotilty or dilatation, or chronic regurgitation syndromes.
Conclusion
Bariatric surgery is a life-altering intervention proven to induce weight loss and improve type 2 diabetes and other obesity-related comorbidities. Although efficacious, the currently performed bariatric procedures require lifelong adherence to nutritional supplementation and observation for potential complications.
Acknowledgments
The authors thank all of the members of University of Minnesota Department of Bariatric Surgery for their assistance and discussion in preparing this article. The authors also thank Megan Hadely for her assistance in preparing the manuscript.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
Footnotes
Co-primary authors
References
- 1.World Health Organization Obesity and overweight fact sheet [Internet]. Available from http://www.who.int/mediacentre/factsheets/fs311/en. Accessed 15 June 2017
- 2.Ogden CL, Carroll MD, Lawman HG, et al. . Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA 2016;315:2292–2299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Farb MG, Gokce N. Visceral adiposopathy: a vascular perspective. Horm Mol Biol Clin Investig 2015;21:125–136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tewari N, Awad S, Macdonald IA, Lobo DN. Obesity-related insulin resistance: implications for the surgical patient. Int J Obes (Lond) 2015;39:1575–1588 [DOI] [PubMed] [Google Scholar]
- 5.Fuster JJ, Ouchi N, Gokce N, Walsh K. Obesity-induced changes in adipose tissue microenvironment and their impact on cardiovascular disease. Circ Res 2016;118:1786–1807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Look AHEAD Research Group; Gregg EW, Jakicic JM, Blackburn G, et al. . Association of the magnitude of weight loss and changes in physical fitness with long-term cardiovascular disease outcomes in overweight or obese people with type 2 diabetes: a post-hoc analysis of the Look AHEAD randomised clinical trial. Lancet Diabetes Endocrinol 2016;4:913–921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Diabetes Prevention Program Research Group Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ikramuddin S, Korner J, Lee W-J, et al. . Roux-en-Y gastric bypass vs intensive medical management for the control of type 2 diabetes, hypertension, and hyperlipidemia: the Diabetes Surgery Study randomized clinical trial. JAMA 2013;309:2240–2249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hutter MM, Schirmer BD, Jones DB, et al. . First report from the American College of Surgeons Bariatric Surgery Center Network: laparoscopic sleeve gastrectomy has morbidity and effectiveness positioned between the band and the bypass. Ann Surg 2011;254:410–420; discussion 420–422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peterli R, Wölnerhanssen BK, Vetter D, et al. . Laparoscopic sleeve gastrectomy versus Roux-Y-gastric bypass for morbid obesity: 3-year outcomes of the prospective randomized Swiss Multicenter Bypass Or Sleeve Study (SM-BOSS). Ann Surg 2017;265:466–473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Institutes of Health Consensus Development Conference Panel Gastrointestinal surgery for severe obesity. Ann Intern Med 1991;115:956–961 [PubMed] [Google Scholar]
- 12.Burguera B, Agusti A, Arner P, et al. . Critical assessment of the current guidelines for the management and treatment of morbidly obese patients. J Endocrinol Invest 2007;30:844–852 [DOI] [PubMed] [Google Scholar]
- 13.Mechanick JI, Youdim A, Jones DB, et al. . Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient: 2013 update: cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Obesity (Silver Spring) 2013;21(Suppl. 1):S1–S27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hsu WC, Araneta MRG, Kanaya AM, Chiang JL, Fujimoto W. BMI cut points to identify at-risk Asian Americans for type 2 diabetes screening. Diabetes Care 2015;38:150–158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sogg S, Lauretti J, West-Smith L. Recommendations for the presurgical psychosocial evaluation of bariatric surgery patients. Surg Obes Relat Dis 2016;12:731–749 [DOI] [PubMed] [Google Scholar]
- 16.Glenn NM, Raine KD, Spence JC. Mandatory weight loss during the wait for bariatric surgery. Qual Health Res 2014;25:51–61 [DOI] [PubMed] [Google Scholar]
- 17.Nguyen NT, Goldman C, Rosenquist CJ, et al. . Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and costs. Ann Surg 2001;234:279–291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Almogy G, Crookes PF, Anthone GJ. Longitudinal gastrectomy as a treatment for the high-risk super-obese patient. Obes Surg 2004;14:492–497 [DOI] [PubMed] [Google Scholar]
- 19.Abraham A, Ikramuddin S, Jahansouz C, Arafat F, Hevelone N, Leslie D. Trends in bariatric surgery: procedure selection, revisional surgeries, and readmissions. Obes Surg 2016;26:1371–1377 [DOI] [PubMed] [Google Scholar]
- 20.Mingrone G, Panunzi S, De Gaetano A, et al. . Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet 2015;386:964–973 [DOI] [PubMed] [Google Scholar]
- 21.Ponce J, Woodman G, Swain J, et al. . The REDUCE pivotal trial: a prospective, randomized controlled pivotal trial of a dual intragastric balloon for the treatment of obesity. Surg Obes Relat Dis 2015;11:874–881 [DOI] [PubMed] [Google Scholar]
- 22.Ikramuddin S, Blackstone RP, Brancatisano A, et al. . Effect of reversible intermittent intra-abdominal vagal nerve blockade on morbid obesity: the ReCharge randomized clinical trial. JAMA 2014;312:915–922 [DOI] [PubMed] [Google Scholar]
- 23.Sullivan S, Stein R, Jonnalagadda S, Mullady D, Edmundowicz S. Aspiration therapy leads to weight loss in obese subjects: a pilot study. Gastroenterology 2013;145:1245–1252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mehaffey JH, LaPar DJ, Clement KC, et al. . 10-year outcomes after Roux-en-Y gastric bypass. Ann Surg 2016;264:121–126 [DOI] [PubMed] [Google Scholar]
- 25.Peterli R, Borbély Y, Kern B, et al. . Early results of the Swiss Multicentre Bypass or Sleeve Study (SM-BOSS): a prospective randomized trial comparing laparoscopic sleeve gastrectomy and Roux-en-Y gastric bypass. Ann Surg 2013;258:690–695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Courcoulas AP, Christian NJ, Belle SH, et al. . Weight change and health outcomes at three years after bariatric surgery among patients with severe obesity. JAMA 2013;310:2416–2425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Camastra S, Gastaldelli A, Mari A, Bonuccelli S. Early and longer term effects of gastric bypass surgery on tissue-specific insulin sensitivity and beta cell function in morbidly obese patients with and without type 2 diabetes. Diabetologia 2011;54:2093–2102 [DOI] [PubMed] [Google Scholar]
- 28.Schauer PR, Bhatt DL, Kirwan JP, et al. . Bariatric surgery versus intensive medical therapy for diabetes: 3-year outcomes. N Engl J Med 2014;370:2002–2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schauer PR, Kashyap SR, Wolski K, et al. . Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med 2012;366:1567–1576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schauer PR, Bhatt DL, Kirwan JP, et al. . Bariatric surgery versus intensive medical therapy for diabetes: 5-year outcomes. N Engl J Med 2017;376:641–651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ikramuddin S, Korner J, Lee W-J, et al. . Durability of addition of Roux-en-Y gastric bypass to lifestyle intervention and medical management in achieving primary treatment goals for uncontrolled type 2 diabetes in mild to moderate obesity: a randomized control trial. Diabetes Care 2016;39:1510–1518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nguyen NT, Varela E, Sabio A, Tran C-L, Stamos M, Wilson SE. Resolution of hyperlipidemia after laparoscopic Roux-en-Y gastric bypass. J Am Coll Surg 2006;203:24–29 [DOI] [PubMed] [Google Scholar]
- 33.Sarkhosh K, Switzer NJ, El-Hadi M, Birch DW, Shi X, Karmali S. The impact of bariatric surgery on obstructive sleep apnea: a systematic review. Obes Surg 2013;23:414–423 [DOI] [PubMed] [Google Scholar]
- 34.Madalosso CAS, Gurski RR, Callegari-Jacques SM, Navarini D, Thiesen V, Fornari F. The impact of gastric bypass on bastroesophageal reflux disease in patients with morbid obesity: a prospective study based on the Montreal consensus. Ann Surg 2010;251:244–248 [DOI] [PubMed] [Google Scholar]
- 35.De Jong JR, Besselink MGH, Van Ramshorst B, Gooszen HG, Smout AJPM. Effects of adjustable gastric banding on gastroesophageal reflux and esophageal motility: a systematic review. Obes Rev 2010;11:297–305 [DOI] [PubMed] [Google Scholar]
- 36.Oor JE, Roks DJ, Ünlü Ç, Hazebroek EJ. Laparoscopic sleeve gastrectomy and gastroesophageal reflux disease: a systematic review and meta-analysis. Am J Surg 2016;211:250–267 [DOI] [PubMed] [Google Scholar]
- 37.Chavez-Tapia NC, Tellez-Avila FI, Barrientos-Gutierrez T, Mendez-Sanchez N, Lizardi-Cervera J, Uribe M. Bariatric surgery for non-alcoholic steatohepatitis in obese patients. Cochrane Database Syst Rev 2010;CD007340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sjöström L, Gummesson A, Sjöström CD, et al. . Effects of bariatric surgery on cancer incidence in obese patients in Sweden (Swedish Obese Subjects Study): a prospective, controlled intervention trial. Lancet Oncol 2009;10:653–662 [DOI] [PubMed] [Google Scholar]
- 39.Adams TD, Stroup AM, Gress RE, et al. . Cancer incidence and mortality after gastric bypass surgery. Obesity (Silver Spring) 2009;17:796–802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Adams TD, Gress RE, Smith SC, et al. . Long-term mortality after gastric bypass surgery. N Engl J Med 2007;357:753–761 [DOI] [PubMed] [Google Scholar]
- 41.Santulli P, Mandelbrot L, Facchiano E, et al. . Obstetrical and neonatal outcomes of pregnancies following gastric bypass surgery: a retrospective cohort study in a French referral centre. Obes Surg 2010;20:1501–1508 [DOI] [PubMed] [Google Scholar]
- 42.Parent B, Martopullo I, Weiss NS, Khandelwal S, Fay EE, Rowhani-Rahbar A. Bariatric surgery in women of childbearing age, timing between an operation and birth, and associated perinatal complications. JAMA Surg 2017;152:128–135 [DOI] [PubMed] [Google Scholar]
- 43.American College of Obsteticians and Gynecologists ACOG practice bulletin no. 105: bariatric surgery and pregnancy. Obstet Gynecol 2009;113:1405–1413 [DOI] [PubMed] [Google Scholar]
- 44.Roos N, Neovius M, Cnattingius S, et al. . Perinatal outcomes after bariatric surgery: nationwide population based matched cohort study. BMJ 2013;347:f6460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Karamanakos SN, Vagenas K, Kalfarentzos F, Alexandrides TK. Weight loss, appetite suppression, and changes in fasting and postprandial ghrelin and peptide YY levels after Roux-en-Y gastric bypass and sleeve gastrectomy. Ann Surg 2008;247:401–407 [DOI] [PubMed] [Google Scholar]
- 46.Nguyen KT, Billington CJ, Vella A, et al. . Preserved insulin secretory capacity and weight loss are the predominant predictors of glycemic control in patients with type 2 diabetes randomized to Roux-en-Y gastric bypass. Diabetes 2015;64:3104–3110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Holst JJ. The physiology of glucagon-like peptide 1. Physiol Rev 2007;87:1409–1439 [DOI] [PubMed] [Google Scholar]
- 48.Korner J, Bessler M, Inabnet W, Taveras C, Holst JJ. Exaggerated glucagon-like peptide-1 and blunted glucose-dependent insulinotropic peptide secretion are associated with Roux-en-Y gastric bypass but not adjustable gastric banding. Surg Obes Relat Dis 2007;3:597–601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Laferrère B, Reilly D, Arias S, et al. . Differential metabolic impact of gastric bypass surgery versus dietary intervention in obese diabetic subjects despite identical weight loss. Sci Transl Med 2011;3:80re2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Alamuddin N, Vetter ML, Ahima RS, et al. . Changes in fasting and prandial gut and adiposity hormones following vertical sleeve gastrectomy or Roux-en-Y gastric bypass: an 18-month prospective study. Obes Surg 2017;27:1563–1572 [DOI] [PubMed] [Google Scholar]
- 51.Nannipieri M, Baldi S, Mari A, et al. . Roux-en-Y gastric bypass and sleeve gastrectomy: mechanisms of diabetes remission and role of gut hormones. J Clin Endocrinol Metab 2013;98:4391–4399 [DOI] [PubMed] [Google Scholar]
- 52.Batterham RL, Cowley MA, Small CJ, et al. . Gut hormone PYY(3-36) physiologically inhibits food intake. Nature 2002;418:650–654 [DOI] [PubMed] [Google Scholar]
- 53.le Roux CW, Aylwin SJB, Batterham RL, et al. . Gut hormone profiles following bariatric surgery favor an anorectic state, facilitate weight loss, and improve metabolic parameters. Ann Surg 2006;243:108–114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sumithran P, Prendergast LA, Delbridge E, et al. . Long-term persistence of hormonal adaptations to weight loss. N Engl J Med 2011;365:1597–1604 [DOI] [PubMed] [Google Scholar]
- 55.Cummings DE, Weigle DS, Frayo RS, et al. . Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N Engl J Med 2002;346:1623–1630 [DOI] [PubMed] [Google Scholar]
- 56.Tschöp M, Weyer C, Tataranni PA, Devanarayan V, Ravussin E, Heiman ML. Circulating ghrelin levels are decreased in human obesity. Diabetes 2001;50:707–709 [DOI] [PubMed] [Google Scholar]
- 57.Müller TD, Nogueiras R, Andermann ML, et al. . Ghrelin. Mol Metab 2015;4:437–460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tymitz K, Engel A, McDonough S, Hendy MP, Kerlakian G. Changes in ghrelin levels following bariatric surgery: review of the literature. Obes Surg 2011;21:125–130 [DOI] [PubMed] [Google Scholar]
- 59.Schipper HS, Prakken B, Kalkhoven E, Boes M. Adipose tissue-resident immune cells: key players in immunometabolism. Trends Endocrinol Metab 2012;23:407–415 [DOI] [PubMed] [Google Scholar]
- 60.Olefsky JM, Glass CK. Macrophages, inflammation, and insulin resistance. Ann Rev Physiol 2010;72:219–246 [DOI] [PubMed] [Google Scholar]
- 61.Cinti S, Mitchell G, Barbatelli G, et al. . Adipocyte death defines macrophage localization and function in adipose tissue of obese mice and humans. J Lipid Res 2005;46:2347–2355 [DOI] [PubMed] [Google Scholar]
- 62.Considine RV, Sinha MK, Heiman ML, et al. . Serum immunoreactive-leptin concentrations in normal-weight and obese humans. N Engl J Med 1996;334:292–295 [DOI] [PubMed] [Google Scholar]
- 63.Baskin DG, Breininger JF, Schwartz MW. Leptin receptor mRNA identifies a subpopulation of neuropeptide Y neurons activated by fasting in rat hypothalamus. Diabetes 1999;48:828–833 [DOI] [PubMed] [Google Scholar]
- 64.Halaas JL, Boozer C, Blair-West J, Fidahusein N, Denton DA, Friedman JM. Physiological response to long-term peripheral and central leptin infusion in lean and obese mice. Proc Natl Acad Sci U S A 1997;94:8878–8883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rosenbaum M, Leibel RL. Role of leptin in energy homeostasis in humans. J Endocrinol 2014;223:T83–T96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Infanger D, Baldinger R, Branson R, Barbier T, Steffen R, Horber FF. Effect of significant intermediate-term weight loss on serum leptin levels and body composition in severely obese subjects. Obes Surg 2003;13:879–888 [DOI] [PubMed] [Google Scholar]
- 67.Sweeney TE, Morton JM. Metabolic surgery: action via hormonal milieu changes, changes in bile acids or gut microbiota? A summary of the literature. Best Pract Res Clin Gastroenterol 2014;28:727–740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yousseif A, Emmanuel J, Karra E, et al. . Differential effects of laparoscopic sleeve gastrectomy and laparoscopic gastric bypass on appetite, circulating acyl-ghrelin, peptide YY3-36 and active GLP-1 levels in non-diabetic humans. Obes Surg 2014;24:241–252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Maeda N, Shimomura I, Kishida K, et al. . Diet-induced insulin resistance in mice lacking adiponectin/ACRP30. Nat Med 2002;8:731–737 [DOI] [PubMed] [Google Scholar]
- 70.Weiss EP, Racette SB, Villareal DT, et al. . Improvements in glucose tolerance and insulin action induced by increasing energy expenditure or decreasing energy intake: a randomized controlled trial. Am J Clin Nutr 2006;84:1033–1042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Salas-Salvadó J, Bulló M, García-Lorda P, et al. . Subcutaneous adipose tissue cytokine production is not responsible for the restoration of systemic inflammation markers during weight loss. Int J Obes (Lond) 2006;30:1714–1720 [DOI] [PubMed] [Google Scholar]
- 72.Woelnerhanssen B, Peterli R, Steinert RE, Peters T, Borbély Y, Beglinger C. Effects of postbariatric surgery weight loss on adipokines and metabolic parameters: comparison of laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomya prospective randomized trial. Surg Obes Relat Dis 2011;7:561–568 [DOI] [PubMed] [Google Scholar]
- 73.Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature 2006;444:1027–1031 [DOI] [PubMed] [Google Scholar]
- 74.Palleja A, Kashani A, Allin KH, et al. . Roux-en-Y gastric bypass surgery of morbidly obese patients induces swift and persistent changes of the individual gut microbiota. Genome Med 2016;8:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Damms-Machado A, Mitra S, Schollenberger AE, et al. . Effects of surgical and dietary weight loss therapy for obesity on gut microbiota composition and nutrient absorption. Biomed Res Int 2015;2015:806248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Murphy R, Tsai P, Jüllig M, Liu A, Plank L, Booth M. Differential changes in gut microbiota after gastric bypass and sleeve gastrectomy bariatric surgery vary according to diabetes remission. Obes Surg 2017;27:917–925 [DOI] [PubMed] [Google Scholar]
- 77.Kong L, Aron-Wisnewsky J, Pelloux V, et al. . Gut microbiota after gastric bypass in human obesity: increased richness and associations of bacterial genera with adipose tissue genes. Am Soc Nutr 2013;98:16–24 [DOI] [PubMed] [Google Scholar]
- 78.Liou AP, Paziuk M, Luevano J-M, Machineni S, Turnbaugh PJ, Kaplan LM. Conserved shifts in the gut microbiota due to gastric bypass reduce host weight and adiposity. Sci Transl Med 2013;5:178ra41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Tremaroli V, Karlsson F, Werling M, Roux CW, Kovatcheva-Datchary P. Roux-en-Y gastric bypass and vertical banded gastroplasty induce long-term changes on the human gut microbiome contributing to fat mass regulation. Cell Metab 2015;22:228–238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.De Aguiar Vallim TQ, Tarling EJ, Edwards PA. Pleiotropic roles of bile acids in metabolism. Cell Metab 2013;17:657–669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sayin SI, Wahlström A, Felin J, et al. . Gut microbiota regulates bile acid metabolism by reducing the levels of tauro-beta-muricholic acid, a naturally occurring FXR antagonist. Cell Metab 2013;17:225–235 [DOI] [PubMed] [Google Scholar]
- 82.Wahlström A, Sayin SI, Marschall H-U, Bäckhed F. Intestinal crosstalk between bile acids and microbiota and its impact on host metabolism. Cell Metab 2016;24:41–50 [DOI] [PubMed] [Google Scholar]
- 83.Thomas C, Gioiello A, Noriega L, et al. . TGR5-mediated bile acid sensing controls glucose homeostasis. Cell Metab 2009;10:167–177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Parséus A, Sommer N, Sommer F, et al. . Microbiota-induced obesity requires farnesoid X receptor. 2017;66:429–437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Glicksman C, Pournaras DJ, Wright M, et al. . Postprandial plasma bile acid responses in normal weight and obese subjects. Ann Clin Biochem 2010;47:482–484 [DOI] [PubMed] [Google Scholar]
- 86.Angelin B, Bjorkhem I, Einarsson K, Ewerth S. Hepatic uptake of bile acids in man: fasting and postprandial concentrations of individual bile acids in portal venous and systemic blood serum. J Clin Invest 1982;70:724–731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Song K-H, Li T, Owsley E, Strom S, Chiang JYL. Bile acids activate fibroblast growth factor 19 signaling in human hepatocytes to inhibit cholesterol 7alpha-hydroxylase gene expression. Hepatology 2009;49:297–305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ryan KK, Tremaroli V, Clemmensen C, et al. . FXR is a molecular target for the effects of vertical sleeve gastrectomy. Nature 2014;509:183–188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mcgavigan AK, Garibay D, Henseler ZM, et al. . TGR5 contributes to glucoregulatory improvements after vertical sleeve gastrectomy in mice. Gut 2015;66:226–234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Jahansouz C, Xu H, Hertzel A, et al. . Bile acids increase independently from hypocaloric restriction after bariatric surgery. Ann Surg 2016;264:1022–1028 [DOI] [PubMed] [Google Scholar]
- 91.Cole AJ, Teigen LM, Jahansouz C, Earthman CP, Sibley SD. The influence of bariatric surgery on serum bile acids in humans and potential metabolic and hormonal implications: a systematic review. Curr Obes Rep 2015;4:41–450 [DOI] [PubMed] [Google Scholar]
- 92.Kohli R, Bradley D, Setchell KD, Eagon JC, Abumrad N, Klein S. Weight loss induced by Roux-en-Y gastric bypass but not laparoscopic adjustable gastric banding increases circulating bile acids. J Clin Endocrinol Metab 2013;98:E708–E712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Albaugh VL, Flynn CR, Cai S, Xiao Y, Tamboli RA, Abumrad NN. Early increases in bile acids post Roux-en-Y gastric bypass are driven by insulin-sensitizing, secondary bile acids. J Clin Endocrinol Metab 2015;100:E1225–E1233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sachdev S, Wang Q, Billington C, et al. . FGF 19 and bile acids increase following Roux-en-Y gastric bypass but not after medical management in patients with type 2 diabetes. Obes Surg 2016;26:957–965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Biemann R, Penner M, Borucki K, et al. . Serum bile acids and GLP-1 decrease following telemetric induced weight loss: results of a randomized controlled trial. Sci Rep 2016;6:30173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Colossi FG, Casagrande DS, Chatkin R, et al. . Need for multivitamin use in the postoperative period of gastric bypass. Obes Surg 2008;18:187–191 [DOI] [PubMed] [Google Scholar]
- 97.Al Harakeh AB, Kallies KJ, Borgert AJ, Kothari SN. Bowel obstruction rates in antecolic/antegastric versus retrocolic/retrogastric Roux limb gastric bypass: a meta-analysis. Surg Obes Relat Dis 2016;12:194–198 [DOI] [PubMed] [Google Scholar]
- 98.Ghiassi S, Nguyen SQ, Divino CM. Internal hernias: clinical findings, management, and outcomes in 49 nonbariatric cases. J Gastrointest Surg 2007;11:291–295 [DOI] [PubMed] [Google Scholar]
- 99.Iannuccilli JD, Grand D, Murphy BL, Evangelista P, Roye GD, Mayo-Smith W. Sensitivity and specificity of eight CT signs in the preoperative diagnosis of internal mesenteric hernia following Roux-en-Y gastric bypass surgery. Clin Radiol 2009;64:373–380 [DOI] [PubMed] [Google Scholar]
- 100.Papasavas PK, Yeaney WW, Caushaj PF, Keenan RJ, Landreneau RJ, Gagné DJ. Perforation in the bypassed stomach following laparoscopic Roux-en-Y Gastric Bypass. Obes Surg 2003;13:797–799 [DOI] [PubMed] [Google Scholar]
- 101.Lee S, Carmody B, Wolfe L, et al. . Effect of location and speed of diagnosis on anastomotic leak outcomes in 3828 gastric bypass cases. J Gastrointest Surg 2007;11:708–713 [DOI] [PubMed] [Google Scholar]
- 102.Edwards MA, Jones DB, Ellsmere J, Grinbaum R, Schneider BE. Anastomotic leak following antecolic versus retrocolic laparoscopic Roux-en-Y gastric bypass for morbid obesity. Obes Surg 2007;17:292–297 [DOI] [PubMed] [Google Scholar]
- 103.Podnos YD, Jimenez JC, Wilson SE, Stevens CM, Nguyen NT. Complications after laparoscopic gastric bypass. Arch Surg 2003;138:957–961 [DOI] [PubMed] [Google Scholar]
- 104.Barba CA, Butensky MS, Lorenzo M, Newman R. Endoscopic dilation of gastroesophageal anastomosis stricture after gastric bypass. Surg Endosc 2003;17:416–420 [DOI] [PubMed] [Google Scholar]
- 105.Ribeiro-Parenti L, Arapis K, Chosidow D, Marmuse J-P. Comparison of marginal ulcer rates between antecolic and retrocolic laparoscopic Roux-en-Y gastric bypass. Obes Surg 2015;25:215–221 [DOI] [PubMed] [Google Scholar]
- 106.Dallal RM, Bailey LA. Ulcer disease after gastric bypass surgery. Surg Obes Relat Dis 2006;2:455–459 [DOI] [PubMed] [Google Scholar]
- 107.Shiffman ML, Sugerman HJ, Kellum JM, Brewer WH, Moore EW. Gallstone formation after rapid weight loss: a prospective study in patients undergoing gastric bypass surgery for treatment of morbid obesity. Am J Gastroenterol 1991;86:1000–1005 [PubMed] [Google Scholar]
- 108.Sugerman HJ, Brewer WH, Shiffman ML, et al. . A multicenter, placebo-controlled, randomized, double-blind, prospective trial of prophylactic ursodiol for the prevention of gallstone formation following gastric-bypass-induced rapid weight loss. Am J Surg 1995;169:91–96 [DOI] [PubMed] [Google Scholar]
- 109.Villegas L, Schneider B, Provost D, et al. . Is routine cholecystectomy required during laparoscopic gastric bypass? Obes Surg 2004;14:206–211 [DOI] [PubMed] [Google Scholar]
- 110.Ukleja A. Dumping syndrome: pathophysiology and treatment. Nutr Clin Pract 2005;20:517–525 [DOI] [PubMed] [Google Scholar]
- 111.Berg P, McCallum R. Dumping syndrome: a review of the current concepts of pathophysiology, diagnosis, and treatment. Dig Dis Sci 2016;61:11–18 [DOI] [PubMed] [Google Scholar]
- 112.Osland E, Yunus RM, Khan S, Alodat T, Memon B, Memon MA. Postoperative early major and minor complications in laparoscopic vertical sleeve gastrectomy (LVSG) versus laparoscopic Roux-en-Y gastric bypass (LRYGB) procedures: a meta-analysis and systematic review. Obes Surg 2016;26:2273–2284 [DOI] [PubMed] [Google Scholar]
- 113.Armstrong J, O’Malley SP. Outcomes of sleeve gastrectomy for morbid obesity: a safe and effective procedure? Int J Surg 2010;8:69–71 [DOI] [PubMed] [Google Scholar]
- 114.Felberbauer FX, Langer F, Shakeri-Manesch S, et al. . Laparoscopic sleeve gastrectomy as an isolated bariatric procedure: intermediate-term results from a large series in three Austrian centers. Obes Surg 2008;18:814–818 [DOI] [PubMed] [Google Scholar]
- 115.Dapri G, Vaz C, Cadière GB, Himpens J. A prospective randomized study comparing two different techniques for laparoscopic sleeve gastrectomy. Obes Surg 2007;17:1435–1441 [DOI] [PubMed] [Google Scholar]