Abstract
Metabolic syndrome is one of today’s most important health problems. Due to increased prevalence of metabolic syndrome in society, studies done on this topic have increased in number. Although metabolic syndrome was previously considered to be important only for cardiovascular health, it has been learned that with new data, human health is compromised more thoroughly by metabolic syndrome and is also a danger to malignancy. As a result, a new definition in the form of metabesity has been introduced. In this review, available information on metabesity and urological cancers is presented.
Keywords: Metabolic syndrome, metabesity, prostate cancer, renal cancer
Because of becoming widespread of sedentary life style and changes in dietary habits, the incidence of obesity and weight gain has increased.[1,2] Metabolic syndrome which occurs to be connected to/with weight gain and obesity has become one of the most important health problems. In the Western World the incidence of metabolic syndrome in adult population was detected as 35–41%.[3,4]
Nowadays, a standard definition of metabolic syndrome has not been made yet. Various societies have suggested different definitions. The first institutionalized definition was made by the World Health Organization (WHO) in the year 1998. Subsequently European Group for the Study of Insulin Resistance (EGIR) (1999), National Cholesterol Education Program-Adult Treatment Panel-III (NCEP-ATP-3) (2001), International Diabetes Foundation (IDF) (2005), American Heart Association /National Heart, Lung, and Blood Institute (AHA/NHLBI) (2005) defined metabolic syndrome. Lastly, joint interim definition made by IDF and AHA/NHLBI was published in 2009.[5] The most current diagnostic criteria of metabolic syndrome are shown in Table 1.[6] Basic criteria used in these definitions include waist circumference, diabetes mellitus, dyslipidemia (decreased HDL, and increased TG), and hypertension. In addition to metabolic syndrome, the concept of diabesity has come to an end. Diabesity is a combination of diabetes and obesity. Dyslipidemia and hypertension may or may not be included in this entity.[7] Recently, Dr. Alexander Fleming who is an endocrinologist and strategist added a different dimension to the definition of metabolic syndrome in a panel speech in the year 2013 and introduced the concept of metabesity (Figure 1). According to Dr. Fleming, metabesity describes all relevant conditions (diabetes mellitus, obesity, metabolic syndrome, cardiovascular disease, dyslipidemia, cancer promoting factors and accelerated aging) which impose a serious burden on healthcare, and economic state.[8] The difference between concepts of metabesity and diabesity is that metabesity describes conditions within a larger spectrum which deteriorate human health.
Table 1.
Diagnostic criteria of metabolic syndrome[6]
| Body weight | Waist circumference specific to the ethnicity and population in question |
|
| |
| Lipid panel | |
| Triglyceride level | ≤150 mg/dL |
| HDL level | Male, <40 mg/dL; women, <50 mg/dL or use of HDL-lowering drug |
|
| |
| Hypertension | ≤135/85 mmHg or receiving antihypertensive medical treatment |
|
| |
| Glycemia | ≤100 mg/dL |
Figure 1.
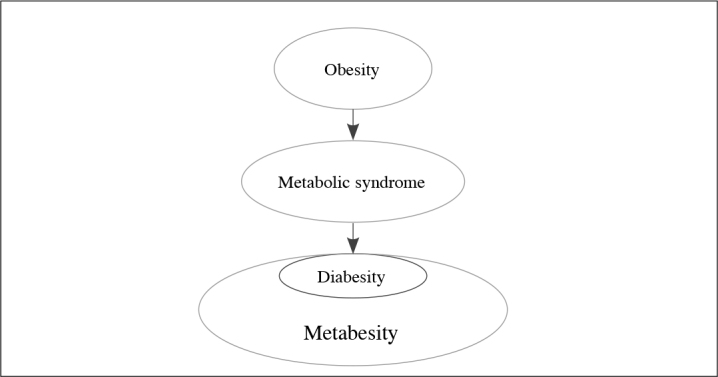
Relationship between obesity and metabesity
Although metabolic syndrome is generally perceived as an important health problem regarding cardiovascular health, with the concept of metabesity more comprehensive definition has been targeted. Regardless of the name, the most common urological problem associated with this clinical picture was erectile dysfunction. However, various studies performed have detected an association between metabolic syndrome and infertility, stone disease, overactive bladder, female urinary incontinence, benign prostatic hyperplasia, prostate cancer and renal cancer.[9–11] In the light of the data obtained, the association between metabolic syndrome, and development of malignity has attracted attention of many researchers. In a recent review article this issue has been analyzed in detail.[12] In the presence of metabolic syndrome, though very precise data concerning the mechanisms which lead to development of cancer have not been available[13,14] some information about the role of obesity on the cancerogenesis have been obtained (Figure 2).[15] In this review, the relationship between metabesity, and urologic malignancies will be presented in the light of international literature.
Figure 2.
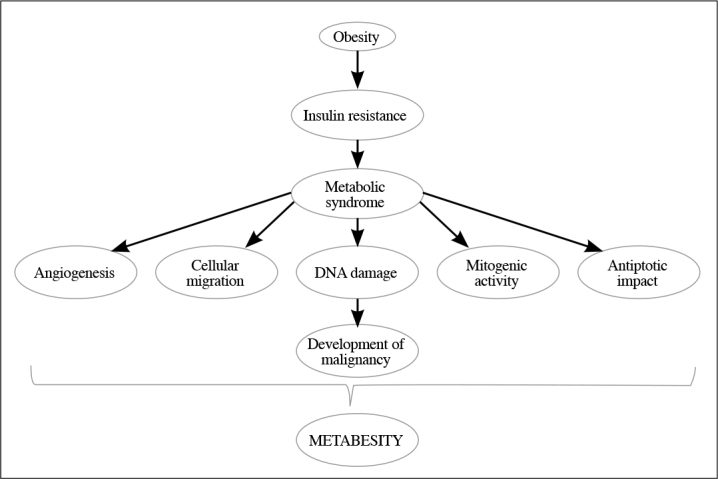
Association between obesity, and malignancy[15]
1. Renal cancer
Clear-cut data are not available about which metabolic syndrome component(s) is/are effective on the development of renal cancer associated with metabesity. In various studies the impact of obesity has been indicated.[15–22] Some authors also reported effectiveness of diabetes mellitus and hypertension in their studies.[17,22–25] Development of renal cancer due to these conditions has been associated with inflammation, insulin, and insulin-like growth factor-1, renal hypoxia, hyperfiltration, and lipid peroxidation.[11,26]
However in a study performed by Haggstrom et al.[27] all components of metabolic syndrome have been correlation with the development of renal cancer. Increased body mass index, hypertension, hyperglycemia and hypertriglyceridemia especially in men and increased body mass index especially in women have been found to be important adverse factors.
2. Prostate cancer
Diverse results have been cited in the international literature about the development of prostate cancer in the presence of metabolic syndrome. Some authors reported that metabolic syndrome did not promote the development of prostate cancer.[28,29] In an Australian study, it was found that increases in waist circumference, and triglyceride levels decreased the risk of development of prostate cancer.[13] In a more recent study, decrease in the development of prostate cancer in the presence of overweightness or obesity and diabetes mellitus has been indicated.[30]
Although general opinion asserts that metabolic syndrome has an impact on the development of prostate cancer, any consensus does not exits concerning which component(s) of metabolic syndrome play(s) a role in the development of prostate cancer. Some authors have reported that none of the components of metabolic syndrome are directly associated with the development of prostate cancer. However, they have also indicated that with an increase in the number of metabolic syndrome components, risk of development of prostate cancer and its aggressiveness also increase.[31]
Also in a most current meta-analysis, it has been detected that metabolic syndrome is a probable risk factor for the development of prostate cancer, besides it is an important factor predicting worse prognosis. In this group of patients, metabolic syndrome is associated with worse pathologic outcomes after radical prostatectomy as Gleason score ≥8, extracapsular invasion, seminal vesicle involvement, positive surgical margin, and biochemical.[32] In this study, it is determined that only one component of metabolic syndrome, namely hypertension, plays a role in the development of prostate cancer.[32] In another study, evidence suggesting the role of higher TG levels (another metabolic syndrome component) in the development of prostate cancer was obtained.[33] Besides, some studies have demonstrated the association between overweightness/ obesity and prostate cancer.[34,35]
The factors which are thought to be effective between components of metabolic syndrome and biology of prostate cancer include sex hormones, endocrine disruptors, inflammation, lipids and proteins modified by prooxidative microenvironment. Insulin and insulin-like hormones as growth factors play important roles.[36,37] Increases in the levels of estradiol, and sex hormone-binding globulin and sex hormone-binding globulin, and decreased free testosterone levels have been indicated to be effective on this process.[38,39] Endocrine disruptors are substances which disrupts synthesis, secretions, effects, elimination of naturally existing hormones in human beings, and their binding to receptors including drugs, pesticides, plastic additives, organic contaminants. Most of them are xenoestrogens or antiandrogens.[40] Changes in cytokines and leptin levels due to increased inflammation in metabolic syndrome have been shown to play a role in prostate cancer development.[41]
In conclusion, metabesity which is introduced as a novel concept into our use will occupy an important place in our clinical practice. Therefore components of metabolic syndrome should be considered in the practice of urological oncology.
Footnotes
Peer-review: This manuscript was prepared by the invitation of the Editorial Board and its scientific evaluation was carried out by the Editorial Board.
Conflict of Interest: No conflict of interest was declared by the author.
Financial Disclosure: The author declared that this study has received no financial support.
References
- 1.Ford ES, Li C. Physical activity or fitness and the metabolic syndrome. Expert Rev Cardiovasc Ther. 2006;4:897–915. doi: 10.1586/14779072.4.6.897. https://doi.org/10.1586/14779072.4.6.897. [DOI] [PubMed] [Google Scholar]
- 2.Koszowska AU, Nowak J, Dittefeld A, Bronczyk-Puzon A, Kulpok A, Zubelewicz-Szkodzinska B. Obesity, adipose tissue function and the role of vitamin D. Centr Eur J Immunol. 2014;39:260–4. doi: 10.5114/ceji.2014.43732. https://doi.org/10.5114/ceji.2014.43732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Golden SH, Robinson KA, Saldanha I, Anton B, Ladenson PW. Clinical review: prevalence and incidence of endocrine and metabolic disorders in the United States: a comprehensive review. J Clin Endocrinol Metab. 2009;94:1853–78. doi: 10.1210/jc.2008-2291. https://doi.org/10.1210/jc.2008-2291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rutter MK, Sullivan LM, Fox CS, Wilson PW, Nathan DM, Vasan RS, et al. Baseline levels, and changes over time in body mass index and fasting insulin, and their relationship to change in metabolic trait clustering. Metab Syndr Relat Disord. 2014;12:372–80. doi: 10.1089/met.2013.0148. https://doi.org/10.1089/met.2013.0148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fleshnern NE, Bhindi B. Metabolic syndrome and diabetes for the urologist. Can Urol Assoc J. 2014;8:159–61. doi: 10.5489/cuaj.2314. https://doi.org/10.5489/cuaj.2314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–5. doi: 10.1161/CIRCULATIONAHA.109.192644. https://doi.org/10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 7.Kalra S. Diabesity. J Pak Med Assoc. 2013;63:532–4. [PubMed] [Google Scholar]
- 8.Available from: www.prweb.com/releases/2013/1/prweb10339273.htm
- 9.Hammarsten J, Peeker R. Urological aspects of the metabolic syndrome. Nat Rev Urol. 2011;8:483–94. doi: 10.1038/nrurol.2011.112. https://doi.org/10.1038/nrurol.2011.112. [DOI] [PubMed] [Google Scholar]
- 10.Gorbachinsky I, Akpinar H, Assimos DG. Metabolic syndrome and urologic diseases. Rev Urol. 2010;12:157–80. [PMC free article] [PubMed] [Google Scholar]
- 11.Chu KF, Rotker K, Ellsworth P. The Impact of obesity on benign and malignant urologic conditions. Postgrad Med. 2013;125:53–69. doi: 10.3810/pgm.2013.07.2679. https://doi.org/10.3810/pgm.2013.07.2679. [DOI] [PubMed] [Google Scholar]
- 12.Uzunlulu M, Caklili OT, Oguz A. Association between Metabolic Syndrome and Cancer. Ann Nutr Metab. 2016;68:173–9. doi: 10.1159/000443743. https://doi.org/10.1159/000443743. [DOI] [PubMed] [Google Scholar]
- 13.Harding J, Sooriyakumaran M, Anstey KJ, Adams R, Balkau B, Briffa T, et al. The metabolic syndrome and cancer: Is the metabolic syndrome useful for predicting cancer risk above and beyond its individual components? Diabetes Metab. 2015;41:463–9. doi: 10.1016/j.diabet.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 14.Mendonça FM, de Sousa FR, Barbosa AL, Martins SC, Araújo RL, Soares R, et al. Metabolic syndrome and risk of cancer: Which link? Metabolism. 2015;64:182–9. doi: 10.1016/j.metabol.2014.10.008. [DOI] [PubMed] [Google Scholar]
- 15.Cowey S, Hardy RW. The metabolic syndrome: a high-risk state for cancer? Am J Pathol. 2006;169:1505–22. doi: 10.2353/ajpath.2006.051090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Choi Y, Park B, Jeong BC, Seo SI, Jeon SS, Choi HY, et al. Body mass index and survival in patients with renal cell carcinoma: A clinical-based cohort and meta-analysis. Int J Cancer. 2013;132:625–34. doi: 10.1002/ijc.27639. https://doi.org/10.1002/ijc.27639. [DOI] [PubMed] [Google Scholar]
- 17.Lipworth L, Tarone RE, Lund L, McLaughlin JK. Epidemiologic characteristics and risk factors for renal cell cancer. Clin Epidemiol. 2009;1:33–43. doi: 10.2147/clep.s4759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Samanic C, Chow WH, Gridley G, Jarvohm B, Fraumeni JF., Jr Relation of body mass index to cancer risk in 362,552 Swedish men. Cancer Causes Control. 2006;17:901–9. doi: 10.1007/s10552-006-0023-9. https://doi.org/10.1007/s10552-006-0023-9. [DOI] [PubMed] [Google Scholar]
- 19.Eskelinen TJ, Kotsar A, Tammela TLJ, Murtola TJ. Components of metabolic syndrome and prognosis of renal cell cancer. Scand J Urol. 2017:1–7. doi: 10.1080/21681805.2017.1352616. [DOI] [PubMed] [Google Scholar]
- 20.Brock K, Gridley G, Lynch C, Ershow A, Cantor K. Obesity and hypertension interact to increase risk of renal cell carcinoma in Iowa, USA. Obes Res Clin Pract. 2007;1:1–2. doi: 10.1016/j.orcp.2007.02.004. https://doi.org/10.1016/j.orcp.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 21.Stewart SB, Freedland SJ. Influence of obesity on the incidence and treatment of GU malignancies. Urol Oncol. 2011;29:476–86. doi: 10.1016/j.urolonc.2009.12.011. https://doi.org/10.1016/j.urolonc.2009.12.011. [DOI] [PubMed] [Google Scholar]
- 22.Navai N, Wood CG. Environmental and modifiable risk factors in renal cell carcinoma. Urol Oncol. 2012;30:220–4. doi: 10.1016/j.urolonc.2011.10.001. https://doi.org/10.1016/j.urolonc.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 23.Larsson SC, Wolk A. Diabetes mellitus and incidence of kidney cancer: a meta-analysis of cohort studies. Diabetologia. 2011;54:1013–8. doi: 10.1007/s00125-011-2051-6. https://doi.org/10.1007/s00125-011-2051-6. [DOI] [PubMed] [Google Scholar]
- 24.Grossman E, Messerli FH, Boyko V, Goldbourt U. Is there an association between hypertension and cancer mortality? Am J Med. 2002;112:479–86. doi: 10.1016/s0002-9343(02)01049-5. [DOI] [PubMed] [Google Scholar]
- 25.Weikert S, Boeing H, Pischon T, Weikert C, Olsen A, Tjonneland A, et al. Blood pressure and risk of renal cell carcinoma in the European prospective investigation into cancer and nutrition. Am J Epidemiol. 2008;167:438–46. doi: 10.1093/aje/kwm321. https://doi.org/10.1093/aje/kwm321. [DOI] [PubMed] [Google Scholar]
- 26.Gago-Dominguez M, Castelao JE, Yuan JM, Ross RK, Yu MC. Lipid peroxidation: A novel and unifying concept of the etiology of renal cell carcinoma (United States) Cancer Control. 2002;13:287–93. doi: 10.1023/a:1015044518505. https://doi.org/10.1023/A:1015044518505. [DOI] [PubMed] [Google Scholar]
- 27.Haggstrom C, Rapp K, Stocks T, Manjer J, Bjørge T, Ulmer H, et al. Metabolic factors associated with risk of renal cell carcinoma. PLoS One. 2013;8:e57475. doi: 10.1371/journal.pone.0057475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Esposito K, Chiodini P, Colao A, Lenzi A, Giugliano D. Metabolic Syndrome and Risk of Cancer: A systematic review and meta-analysis. Diabetes Care. 2012;35:2402–11. doi: 10.2337/dc12-0336. https://doi.org/10.2337/dc12-0336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xiang YZ, Xiong H, Cui ZL, Jiang SB, Xia QH, Zhao Y, et al. The association between metabolic syndrome and the risk of prostate cancer, high-grade prostate cancer, advanced prostate cancer, prostate cancer-specific mortality and biochemical recurrence. J Exp Clin Cancer Res. 2013;32:9. doi: 10.1186/1756-9966-32-9. https://doi.org/10.1186/1756-9966-32-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Perez-Cornago A, Key TJ, Allen NE, Fensom GK, Bradbury KE, Martin RM, et al. Prospective investigation of risk factors for prostate cancer in the UK Biobank cohort study. Br J Cancer. 2017 doi: 10.1038/bjc.2017.312. https://doi.org/10.1038/bjc.2017.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bhindi B, Locke J, Alibhai SMH, Kulkarni GS, Margel DS, Hamilton RJ, et al. Dissecting the Association Between Metabolic Syndrome and Prostate Cancer Risk: Analysis of a Large Clinical Cohort. Eur Urol. 2015;67:64–70. doi: 10.1016/j.eururo.2014.01.040. https://doi.org/10.1016/j.eururo.2014.01.040. [DOI] [PubMed] [Google Scholar]
- 32.Gacci M, Russo GI, De Nunzio C, Sebastianelli A, Salvi M, Vignozz L, et al. Meta-analysis of metabolic syndrome and prostate cancer. Prostate Cancer Prostatic Dis. 2017;20:146–55. doi: 10.1038/pcan.2017.1. https://doi.org/10.1038/pcan.2017.1. [DOI] [PubMed] [Google Scholar]
- 33.Wuermli L, Joerger M, Henz S, Schmid HP, Riesen WF, Thomas G, et al. Hypertriglyceridemia as a possible risk factor for prostate cancer. Prostate Cancer Prostatic Dis. 2005;8:316–20. doi: 10.1038/sj.pcan.4500834. https://doi.org/10.1038/sj.pcan.4500834. [DOI] [PubMed] [Google Scholar]
- 34.Moyad MA. Is obesity a risk factor for prostate cancer, and does it even matter? A hypothesis and different perspective. Urology. 2002;59(Suppl 4A):41–50. doi: 10.1016/s0090-4295(01)01175-x. [DOI] [PubMed] [Google Scholar]
- 35.Muppala S, Konduru SKP, Merchant N, Ramsoondar J, Rampersad CK, Rajitha B, et al. Adiponectin: Its role in obesity-associated colon and prostate cancers. Crit Rev Oncol Hematol. 2017;116:125–33. doi: 10.1016/j.critrevonc.2017.06.003. https://doi.org/10.1016/j.critrevonc.2017.06.003. [DOI] [PubMed] [Google Scholar]
- 36.Carroll KK. Obesity as a risk factor for certain types of cancer. Lipids. 1988;33:1055–9. doi: 10.1007/s11745-998-0305-8. https://doi.org/10.1007/s11745-998-0305-8. [DOI] [PubMed] [Google Scholar]
- 37.Barnard RJ, Aronson WJ, Tymchuk CN, Ngo TH. Prostate cancer: another aspect of the insulin-resistance syndrome? Obes Rev. 2002;3:303–8. doi: 10.1046/j.1467-789x.2002.00081.x. [DOI] [PubMed] [Google Scholar]
- 38.Han JH, Choi NY, Bang SH, Kwon OJ, Jin YW, Myung SC, et al. Relationship between serum prostate-specific antigen levels and components of metabolic syndrome in healthy men. Urology. 2008;72:749–54. doi: 10.1016/j.urology.2008.01.084. https://doi.org/10.1016/j.urology.2008.01.084. [DOI] [PubMed] [Google Scholar]
- 39.Zhang PL, Rosen S, Veeramachaneni R, Kao J, DeWolf WC, Bubley G. Association between prostate cancer and serum testosterone levels. Prostate. 2002;53:179–82. doi: 10.1002/pros.10140. https://doi.org/10.1002/pros.10140. [DOI] [PubMed] [Google Scholar]
- 40.Quagliariello V, Rossetti S, Cavaliere C, Di Palo R, Lamantia E, Castaldo L, et al. Metabolic syndrome, endocrine disruptors and prostate cancer associations: biochemical and pathophysiological evidences. Oncotarget. 2017;8:30606–16. doi: 10.18632/oncotarget.16725. https://doi.org/10.18632/oncotarget.20631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.De Nunzio C, Aronson W, Freedland SJ, Giovannucci E, Parsons JK. The correlation between metabolic syndrome and prostatic diseases. Eur Urol. 2012;61:560–70. doi: 10.1016/j.eururo.2011.11.013. https://doi.org/10.1016/j.eururo.2011.11.013. [DOI] [PubMed] [Google Scholar]


