Abstract
Heavy drinking by college students is exceedingly harmful to the individuals and to the overall college environment. Current interventions to reduce drinking and negative consequences are infrequently utilized. This randomized clinical trial examined an alternative approach that sought to increase exercise behavior, a substance free activity, in sedentary heavy drinking college students. Participants (N = 70) were randomized to an 8-week exercise intervention: (1) motivational interviewing plus weekly exercise contracting (MI+EC) or (2) motivational interviewing and weekly contingency management for exercise (MI+CM). Follow-up evaluations occurred at post-treatment (2 months) and 6 months post baseline. Participants in both interventions significantly increased exercise frequency initially, and the MI+CM participants exercised significantly more than the MI+EC intervention participants during the intervention period (d = 1.70). Exercise behavior decreased during the follow-up period in both groups. Significant reductions in drinking behaviors and consequences were noted over time, but were not related to changes in exercise or the interventions (ds ≤ 0.01). This study underscores the complex nature of promoting one specific health behavior change with the goal of changing another.
Keywords: motivational interviewing, contingency management, alcohol, physical activity
Approximately 45% of college students engage in heavy drinking in the past month, defined as drinking five or more drinks for men and four or more drinks for women (5/4 criterion; Hingson, 2010). Heavy drinking in college students is strongly associated with negative consequences, such as injuries, blackouts, and interpersonal problems. In addition, heavy drinking college students engage in other risky behaviors such as unprotected sex and driving while intoxicated (White & Hingson, 2013). Although brief interventions, such as those based upon motivational interviewing (MI), have been shown to significantly reduce heavy drinking in college students (Carey, Scott-Sheldon, Carey, & DeMartini, 2007), few college students recognize it as a problem and infrequently voluntarily seek help (~2%; Wu, Pilowsky, Schlenger, & Hasin, 2007). Stigma, combined with a desire to handle a problem on one’s own, is a primary reason why college students do not seek mental health services (Jennings et al., 2015). Alternative non-stigmatizing interventions are therefore needed to increase the number of individuals who access treatment. This study examined exercise as a potentially non-stigmatizing intervention for heavy drinking college students who also met criteria for hazardous drinking.
Substance use, including drinking, can be conceptualized as a goal-directed behavior that is governed by the principles of reinforcement. Both animal and human studies repeatedly demonstrate that rates of alcohol and drug self-administration vary inversely with the availability of and participation in substance-free reinforcers (Ahmed, 2005; Van Etten, Higgins, Budney, & Badger, 1998). Within heavy drinking college students, Correia and colleagues (2003) found lower frequency and enjoyment in certain substance-free activities (e.g., hiking, art projects, pleasure reading) in comparison to non-heavy drinkers, suggesting increases in these activities as a potential intervention target.
Exercise, a substance free activity, has been proposed as having both potential preventive and treatment effects for alcohol use disorders (Linke & Ussher, 2015) in part because exercise has been shown to decrease urges to drink alcohol (Ussher, Sampuran, Doshi, West, & Drummond, 2004) and has substantial mental and physical health benefits, including reducing symptoms of depression and anxiety (Penedo & Dahn, 2005). Benefits of exercise can occur acutely (e.g., positive mood induction; Killingsworth & Gilbert, 2010) while others require weeks of consistent exercise before emerging (e.g., cardiovascular benefits; Wilson, Ellison, & Cable, 2015). Another mechanism by which exercise may alter drinking is through self-regulation. Oaten and Cheng (2006) found a two-month exercise intervention in college students generated significant improvements in self-regulation, which had broad impacts upon a variety of self-regulatory behaviors including alcohol consumption. Alcohol consumption decreased by about 5 drinks per week during the intervention - without directly targeting of the behavior. Conversely, being sedentary and engaging in heavy drinking frequently co-occur in college students (Luo, Agley, Hendryx, Gassman, & Lohrmann, 2015; Quintiliani, Allen, Marino, Kelly-Weeder, & Li, 2010).
Interventions aimed at increasing engagement in substance-free activities, such as exercise, in heavy drinking college students have an inverse relationship to problematic substance use in some studies (Correia, Benson, & Carey, 2005; Murphy et al., 2012; Murphy, Pagano, & Marlatt, 1986), albeit some data are mixed (Weinstock, Capizzi, Weber, Pescatello, & Petry, 2014). For example, Murphy and colleagues (1986) in randomized clinical trial of 60 heavy drinking college students found that a supervised exercise intervention in comparison to a no-treatment and meditation conditions not only showed an increase in physical fitness but also had the greatest reductions in alcohol consumption during the 8-week intervention and 6-week follow-up. Reductions were significantly greater than the assessment-only control group (ds = 0.97 to 1.19) and moderate in size in comparison to the meditation group (ds = 0.56 to 0.71); however, individuals who dropped out of the study were not included in the analyses (n = 29). Correia and colleagues (2005) used brief advice to increase exercise behavior in college students and found significant reductions in drinking over a one month intervention period; however, the study included a brief advice to reduce drinking condition which had greater reductions in drinking. Finally, a control condition showed no changes in drinking over time. The study did not include any long-term follow-up. Meanwhile, Weinstock and colleagues (2014) in an 8-week pilot study (n = 31) with no follow-up found two different MI exercise interventions did not result in any significant reductions in drinking behavior in heavy drinking college students. Type II error is likely in that study as it was underpowered, and effect size estimates found small to medium effect sizes for drinking outcomes (ds = 0.15–0.48). Unfortunately, these studies did not examine directly whether changes in drinking were attributable to changes in exercise. Therefore, while these types of interventions have shown promise, more work is needed to fully examine the efficacy of exercise as an intervention for heavy drinking. Incorporating long-term follow-up assessments that yield information about adherence to exercise and stability of changes in drinking behaviors are needed.
Research on interventions for engaging in exercise highlight the difficulty of initiating and maintaining this behavior (O'Brien et al., 2015). Within college students, a majority are sedentary (Dinger, Brittain, & Hutchinson, 2014) and those who start an exercise program exercise sporadically or completely stop exercising prior to realizing its many potential benefits (~ 30%; e.g., Dishman, Jackson, & Bray, 2014; Mailey et al., 2010; Martens, Buscemi, Smith, & Murphy, 2012). Several factors have been identified that are associated with successful initiation and maintenance of an exercise program. These factors include social support, self-efficacy, motivation, having physical activity choices, goal setting and behavioral contracts, positive reinforcement, intervention duration, and feedback (Plotnikoff et al., 2015). More broadly, studies have found that while extrinsic motivation may be important for initiating exercise, intrinsic motivation is an important component for sustaining it (Buckworth, Lee, Regan, Schneider, & DiClemente, 2007), and interventions that are designed to enhance intrinsic and/or extrinsic motivation to start and maintain an exercise program demonstrate a range of positive effect sizes (Martins & McNeil, 2009; O’Halloran et al., 2014; Webb & Sheeran, 2006). With these factors in mind, a combination of MI and prize-based contingency management (CM) to increase exercise in sedentary heavy drinking college students was created for this study.
The combined intervention sought to address difficulties associated with initiating and sustaining an exercise program. MI is defined as a client-centered, directive method for enhancing intrinsic motivation to change by exploring and resolving ambivalence (Miller & Rollnick, 2013). MI is efficacious as a stand-alone intervention or as a module of a larger intervention for exercise across a variety of populations, including healthy adults, with small to moderate effect sizes in comparison to no-treatment or placebo control groups (Lundahl et al., 2013; O’Halloran et al., 2014). Therefore, MI appears to be an appropriate and efficacious intervention for exercise and was used as the control condition and platform therapy for CM.
Prize-based CM is a behavioral treatment in which tangible reinforcement (e.g., retail goods and services) is provided to individuals when target behaviors are completed and objectively verified (e.g., drug abstinence verified via urine samples). The use of CM to reinforce drug abstinence in substance use disorders treatment is empirically supported (Benishek et al., 2014; Prendergast, Podus, Finney, Greenwell, & Roll, 2006). Successful CM interventions are designed around three central tenets: (1) the environment is arranged such that target behaviors are frequently and easily monitored, (2) tangible reinforcers are provided whenever the target behavior is demonstrated, and (3) when the target behavior does not occur, rewards are systematically withheld (and sometimes a slight punisher may also be delivered). Immediacy and magnitude of rewards are significant moderators of CM interventions’ effect sizes with more immediate access to large reinforcement increasing the effect size (Lussier, Heil, Mongeon, Badger, & Higgins, 2006).
Although CM can alter a variety of behaviors (e.g., drug abstinence, medication adherence, group therapy attendance; Benishek et al., 2014; Mbuagbaw et al., 2015; Petry, Weinstock, & Alessi, 2011), few studies have utilized CM procedures for exercise. Several exercise interventions utilizing contingent incentives have shown effects, while others have been ineffective. These differences in outcome appear to be related to the implementation of the interventions and adherence to CM principles. Small magnitude and delayed provision of reinforcement (e.g., ≥ monthly basis) appears to limit the efficacy of CM exercise interventions (e.g., DeVahl, King, & Williamson, 2005; Jeffery, Wing, Thorson, & Burton, 1998). Conversely, studies showing more pronounced effects for incentives on exercise are those that adhere to the central tenets of CM (e.g., Irons, Pope, Pierce, Van Patten, & Jarvis, 2013; Patel et al., 2016; Petry, Andrade, Barry, & Byrne, 2013). Thus, exercise behavior changes in response to CM interventions when it is monitored frequently, immediate and desirable rewards are offered, and reinforcement is withheld for non-adherence.
In this study, we evaluated a combined MI+CM intervention for exercise in comparison to MI plus weekly exercise activity contracting (MI+EC) in sedentary heavy drinking college students who were not seeking treatment for alcohol-related problems. The comparison condition (MI+EC) was constructed to control for attention and self-monitoring of exercise behavior without providing reinforcement for exercise. Prior work suggested a MI for exercise only condition would potentially suffer from poor exercise adherence (Weinstock et al., 2014). First, we examined exercise outcomes, with the hypothesis that the combined MI+CM intervention would lead to greater exercise engagement during the 8 week intervention and 4 month follow-up period. Second, we hypothesized that engagement in exercise would predict reductions in alcohol consumption and alcohol-related negative consequences.
Methods
Participants
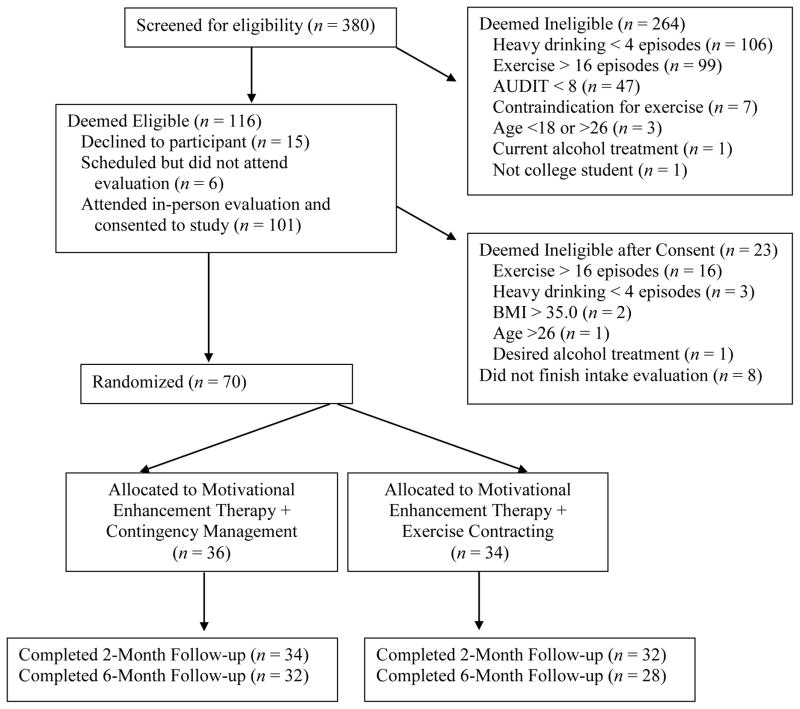
Participants (N = 70) in this study were enrolled in a randomized clinical trial (Clinical Trials Identifier: NCT01057979). Data were collected from January 2010 to September 2011. Individuals were included in the study if they were between the ages of 18–25 years, sedentary as indicated by exercising less than 2 days per week within the last 2 months, enrolled in more than 6 credit hours in the current semester, reported ≥ 4 heavy drinking episodes (4/5 standard drink criterion) in the past 2 months, and met criteria related to hazardous drinking (Alcohol Use Disorders Identification Test scores ≥ 8; Saunders, Aasland, Babor, de la Fuente, & Grant, 1993). The definition for sedentary has been used previously in exercise clinical trials (e.g., Brown et al., 2010) and is of an intensity that is unlikely to yield lasting benefits (American College of Sports Medicine [ACSM], 2013). Individuals were excluded if they indicated they were currently receiving or expressed a desire to receive treatment for alcohol-related problems, disclosed acute psychiatric problems requiring immediate treatment, had medical contra-indications for exercise as assessed by the Physical Activity Readiness Questionnaire (Shepard, Thomas, & Weller, 1991), or a Body Mass Index (BMI) ≥ 35.0 kg/m2. Participants were recruited via flyers posted on campus, email announcements, and direct screening of the student body. All participants provided written informed consent, and the study was approved by the university’s Institutional Review Board. As shown in Figure 1, 70 individuals were randomized to an exercise intervention condition for 8 weeks. Two participants were withdrawn from the study after randomization due to medical problems that arose.
Figure 1.
Flowchart of participants through the study
We conducted a power analysis for a latent growth curve model (see Data Analysis below) simulated in Mplus (Version 7.1; Muthén & Muthén, 2002). Previous studies of prize-based CM have found large effect sizes for substance use outcomes (Benishek et al., 2014), and a pilot study testing the combination of MI+CM implemented in the current study resulted in a large effect size for exercise outcomes and a moderate effect size for alcohol use (Weinstock et al., 2014). We conducted power simulations using parameter estimates from Weinstock et al. (2014) and a moderate effect size (d = .50). Assuming a Type I error rate of α = .05, optimal power of .80 (Type II error rate of β = .20), and a sample size of 70 resulted in power of .83, indicating the sample size was sufficient to detect medium effect sizes.
Randomized participants had a mean age of 20.0 years (SD = 1.47; age range 18–25). The sample was comprised of 31 men and 39 women (55.7% female). With regard to race/ethnicity, 86.8% of individuals identified themselves as Caucasian/White, 5.9% as Hispanic, 2.9% as Asian, 2.9% as Other, and 1.5% as African American, which is reflective of the larger student body at the university. Participants ranged from freshmen to fifth-year seniors with 34.7% reporting to be in their first year of college, 20.6% in their second year, 14.7% in their third year, 25.0% were in their fourth year of college, and 4.4% reporting five years or more of college education. Participants’ BMI ranged from 17.5 to 34.2 with a mean BMI of 24.7 (SD = 3.3).
Measures
Demographic Questionnaire
It assessed age, gender, ethnicity, and year in school.
BMI
BMI was assessed from height (assessed in stocking feet and measured to the nearest 0.10cm) and weight (with excessive clothing and materials such as keys and wallet removed and measured to the nearest 0.10 kg) with a Health-o-meter® Professional scale 597 KL with height rod (Pelstar, Bridgeville, IL). BMI is weight in kg/height in m2.
YMCA Submaximal Bicycle Ergometer Test (YSET)
The YSET is a standardized submaximal assessment of predicted VO2 maximum, a criterion of cardiorespiratory fitness (Poldermans et al., 1993; ACSM, 2013) A regression plot of heart rate versus work load estimates VO2 maximum.
Timeline Followback (TLFB)
The TLFB is the gold standard for self-reported retrospective assessment of drug and alcohol use (Donovan et al., 2012). It demonstrates good psychometric properties for assessing exercise as well (Panza, Weinstock, Ash, & Pescatello, 2012). Two separate TLFBs assessed: (1) frequency, duration, and intensity of exercise and (2) alcohol, marijuana and other drug use in the 60-days prior to baseline and throughout the follow-up. Using the Compendium of Physical Activities (Ainsworth et al., 2011), exercise behavior on the TLFB was then coded into metabolic equivalents (METs) hours per week, a measure of overall exercise volume that reflects the frequency, intensity, and time of exercise.
Brief Young Adult Alcohol Consequences Questionnaire (BYAACQ)
The BYAACQ is a 24-item comprehensive self-report measure of negative consequences due to drinking alcohol with good reliability and validity while being sensitive to changes in drinking over time (Kahler, Hustad, Barnett, Strong, & Borsari, 2008; Kahler, Strong, & Read, 2005). It assesses a range of consequences with minimal gender bias. Cronbach’s alpha internal consistency in this sample ranged from 0.81 to 0.90.
Treatment Services Review (TSR)
The TSR assessed receipt of medical and mental health services (McLellan et al., 1992), including alcohol treatment, in the 2-months prior to intake and throughout the study. It assessed exclusion criteria and monitored serious adverse events.
Client Satisfaction Questionnaire
An investigator derived questionnaire administered at the post-treatment evaluation only and assessed participants’ satisfaction with the intervention they received. Using a 5-point Likert-scale questions asked about overall intervention satisfaction (1 = very satisfied; 5 = very dissatisfied), how participants’ condition changed since the start of the intervention (1 = I’m much better; 5 = I’m much worse), and whether the changes were related to the intervention (1 = definitely related; 5 = definitely not related).
Procedures
In a private research office, trained research assistants obtained written informed consent and completed the baseline evaluation with participants, which included the questionnaires and the submaximal cardiorespiratory assessment. At subsequent evaluations, post-treatment (2-months post-baseline) and follow-up (6-months after baseline), the same assessment was completed by participants. Participants were compensated $65 for the baseline and post-treatment evaluations and $45 for the 6-month follow-up. Follow-up rates exceeded 85% at each post-baseline evaluation (see Figure 1).
Upon completion of the baseline assessment, participants were randomized to one of two study intervention conditions using a computerized urn-randomization procedure (Stout, Wirtz, Carbonari, & Del Boca, 1994) balancing groups on baseline heavy drinking episodes (≤ 5 episodes versus > 5 episodes per month) and BMI (≤ 30.0 versus >30.0). Six different therapists (1 clinical psychologist, 5 ACSM certified exercise specialists who trained and supervised by the first and third author) delivered the interventions. All therapists underwent an initial two-day workshop on motivational interviewing lead by an outside expert and a one-day workshop on contingency management followed by annual one-day refresher trainings. Ongoing supervision consisted of regular review of intervention binders, audiotapes, and case discussion.
Interventions
The study had two intervention conditions: (1) motivational interviewing plus exercise contracting (MI+EC) and (2) motivational interviewing plus contingency management (MI+CM). The interventions were alike in that participants received two 50-minute MI sessions, plus 8 weekly individually-delivered exercise contracting sessions. The difference between the conditions was that the MI+EC intervention reinforced participants for attending the exercise contracting sessions (regardless of exercise activity completion) while the MI+CM intervention reinforced participants only for completion of verified exercise activities. Specific components of the interventions are described below.
MI Sessions
The first MI session was provided immediately after completion of the baseline assessment to ensure delivery of at least part of the intervention. The second MI session was scheduled 4 weeks later. The MI sessions were framed as a “wellness intervention” for increasing exercise and adhered to the principles of MI (Miller & Rollnick, 2013). As the focus of the intervention was to promote exercise, motivation to reduce heavy drinking was not discussed unless first raised by participants within the context of starting and maintaining an exercise routine. The second MI session occurred 4 weeks later and served as a booster session.
EC Sessions
The exercise contracting sessions were held over 8 consecutive weeks, with the first exercise contract completed at the end of the first MI session. These sessions were approximately 10–15 minutes in length. Collaboratively, the therapist and participant completed an exercise contract. The contract contained at least three specific exercise activities to be completed within the upcoming week. Exercise activities were selected by the participants to ensure the activities were of interest. Activities ranged widely and included jogging on a treadmill, attending an exercise class, and swimming. Each activity was explicitly defined in terms of intensity and duration (minutes), as well as objective verification needed for proving completion. Objective verification included pedometers, cellphone videos of instructors verifying attendance at an exercise class, and digital pictures for team sports participation.
In the subsequent weeks, the therapist met briefly with participants to review the prior week’s exercise contract and verification, problem-solve any issues with exercising, and create a new exercise contract for the upcoming week. As participants were sedentary at the baseline evaluation, the goal of the intervention via the exercise contracting was to increase over time and maintain a level of moderate to vigorous intensity exercise consistent with public health guidelines of at least 150 minutes per week of moderate intensity or at least 75 minutes per week of vigorous intensity exercise (ACSM, 2013). Participants assigned to the MI+EC intervention received $5 in gift certificates for attending the EC sessions for a possible total of $40.
CM
Participants in the MI+CM were reinforced for completion and verification of exercise activities specified on the weekly exercise contract. Participants earned one draw from a prize bowl for each exercise activity completed. For each week in which at least three activities were completed, participants received bonus draws, and bonus draws started at 3 and escalated over time by 1 draw per week to a maximum of 10 bonus draws per week. In total, participants could earn up to 79 draws from the prize bowl if they completed the 24 exercise activities. If participants did not complete three exercise activities in a week, they earned a draw for each activity completed (if any) but forfeited the bonus draws. In addition, the bonus draws were reset back to 3 on the next week’s contract.
The prize bowl for drawings contained 80 slips of paper. Half (40) of them stated “Good job!” and were not associated with a prize. The other half were winning slips: 34 state “small prize”, 5 state “large prize”, and 1 states “jumbo prize”. Small prizes were worth $1, large prizes were worth $20, and the jumbo was worth $100. When participants drew a winning slip, they chose amongst the available gift certificates in that category: small, large, and jumbo. A large selection of gift certificates consistent with a healthy lifestyle was available, and participants were solicited for suggestions of types of gift certificates they wanted at each CM session. Average maximal reinforcement of CM was estimated at $230 per participant.
Treatment Fidelity
Using a modification of the Yale Adherence and Competence Scale (Carroll et al., 2000) and the Contingency Management Competency Scale (Petry, Alessi, Ledgerwood, & Sierra, 2010) six independent raters assessed 127 randomly selected audiotapes (about 20% of all sessions). MI, EC, and CM items were rated on a seven point Likert scale (1 = none/poor, 3 = some/adequate, 7 = extensive/excellent). One of the MI items was: “To what extent were the therapist’s questions open-ended and reflective?” One of the exercise contracting items was: “To what extent did the therapist develop a new exercise contract for the upcoming week with specific exercise activities outlining duration and intensity, potential barriers, means of verification?” One of the CM items was: “To what extent did the therapist state how many draws would be earned at the next session if the client were to complete all three exercise activities?” Inter-rater reliability ranged from 0.90 to .99 across the items rated.
For the MI sessions, mean and standard deviation of the MI items was 4.67 (1.31) (reflecting average rankings of ‘good/quite a bit’) with no significant difference in the ratings of the MI sessions between the MI+EC and the MI+CM conditions, p = .75. Meanwhile, in the EC sessions the rating of the MI items was 1.02 (0.10), which was significantly different from the MI sessions, p < .001. For the EC sessions, which was an aspect of every session rated, mean and standard deviation of the EC items was 5.02 (1.03) with no significant differences between the two intervention conditions, p = .51. Lastly, for the CM sessions, mean and standard deviation of the CM items was 5.21 (1.30), which was significantly different from the MI+EC sessions’ means and standard deviations: 1.46 (0.64), p <.001. Thus, the interventions were distinguishable and rated as having ‘good’ therapist adherence and competence.
Data Analysis
Analysis of variance and chi-square tests examined group differences at baseline. Because distributions of the METs expended with exercise and standard drinks per week substantially deviated from normality, we applied log transformations, which were successful in bringing skewness within acceptable levels (<± 2; Gravetter & Wallnau, 2014). Whereas skewness values ranged between 1.34 and 3.44 for untransformed drinks per week values, log transformed values ranged between −0.34 and 0.78. Likewise, untransformed values for METs ranged from 1.24 to 2.94 and transformed values ranged from −0.32 and −0.03.
Using intent-to-treat analyses, which includes all randomized participants regardless of their participation, the primary analytical strategy was latent growth curve (LGC; Curran & Hussong, 2003) to analyze individual client change in exercise behavior. The primary outcomes were selected a priori and included: weekly exercise frequency, METs hours per week, and estimated cardiorespitatory fitness. Secondary outcomes consisted of alcohol use outcomes, specifically binge drinking episodes, frequency of alcohol use (measured in standard drinks per week), and consequences associated with alcohol use. Missing data were handled with full information maximum likelihood (FIML) estimation, under the assumption that the data were missing at random (MAR; Little & Rubin, 1989). LGC modeling was conducted using Mplus (Version 7; Muthén & Muthén, 1998–2014) and proceeded in two stages. First, we tested a series of growth curve models representing possible forms of growth (e.g., no change, linear change, discontinuous change) to determine the overall shape of the individual change trajectories. Because several of the outcomes we examined yielded count data, we also compared the fit of negative-binomial models to conventional models assuming continuous data using Bayesian Information Criterion (BIC) statistics. With the exception of one outcome, exercise frequency, the conventional models indicated better fit. Second, we added intervention condition and gender as covariates to the models to test the impact of intervention type and gender on initial status and change over time (i.e., intercept, slope growth parameters). Gender was included as covariate due to potential differences by gender in terms of drinking behaviors and alcohol-related consequences (e.g., Cranford, Eisenberg, & Serras, 2009). Intervention effects were demonstrated by a statistically significant slope parameter, as tested by the pseudo-z test associated with treatment condition. In addition to the transformations mentioned above, the robust maximum likelihood estimator was used to minimize the impact of non-normality on the results. Both effect sizes (Cohen’s d), calculated using Feingold’s (2009) method for growth curve modeling, and significance tests associated with intervention effects are reported.
As part of the interventions, all participants completed weekly exercise contracts, which required verification of exercise and serves as an objective and reliable source of information regarding exercise behavior during the intervention period. TLFB data were used rather than data from the exercise contracts in the analyses because the TLFB data allow for examining adherence/change over time (i.e., 2 months prior to study enrollment through the 6 month follow-up). The prospective contracts were only available for the 8 week intervention period. Pearson r correlations between the TLFB and exercise contracts for the intervention time period demonstrated excellent convergence (r’s = .55 – .80).
Results
Baseline Indices
Baseline data appear in Tables 1 and 2. In the two months prior to enrolling in the study, MI+EC participants reported exercising significantly more frequently than the MI+CM participants, F(1,69) = 4.33, p < .05. Therefore, we adjusted for baseline exercise frequency in LGC models examining treatment differences in outcomes. In models examining change in outcomes other than exercise frequency, this was accomplished by including baseline frequency as a covariate. However, this produced a convergence problem in the model for exercise frequency; therefore, the adjustment was accomplished by regressing slope parameters on the intercept (which estimates baseline functioning). No other baseline or demographic variables differed significantly between the groups, ps >.05.
Table 1.
Demographics and baseline characteristics.
| MI+EC | MI+CM | Statistic (df) | p-value | |
|---|---|---|---|---|
| (n =34) | (n =36) | |||
| Age | 19.9 (1.3) | 20.1 (1.6) | F(1,69) = 0.44 | .512 |
| Male, no. (%) | 13 (37.1) | 18 (51.4) | χ2(1) = 1.45 | .229 |
| Ethnicity, no. (%) | χ2(2) = 1.67 | .439 | ||
| African American | 1 (2.9) | 0 (0.0) | ||
| Caucasian | 29 (82.9) | 32. (91.4) | ||
| Other | 5 (14.3) | 3 (8.6) | ||
| Years of Education | 14.2 (1.5) | 14.3 (1.7) | F(1,69) = 0.02 | .880 |
| Cumulative Grade Point Average | 3.2 (0.5) | 3.3 (0.5) | F(1,69) = 0.64 | .428 |
| AUDIT Score, past year | 13.9 (5.9) | 13.7 (4.9) | F(1,69) = 0.03 | .859 |
| Body Mass Index (kg2/m) | 24.1 (3.2) | 25.1 (3.3) | F(1,69) = 1.60 | .210 |
Note. AUDIT = Alcohol Use Disorders Identification Test; MI+EC = motivational interviewing plus exercise contracting; MI+CM = motivational interviewing plus contingency management.
Table 2.
Mean and standard deviation of exercise and drinking behavior and consequences at baseline, post-treatment, and follow-up
| Baseline | Post-Treatment | Follow-up | ||||
|---|---|---|---|---|---|---|
| MI+EC | MI+CM | MI+EC | MI+CM | MI+EC | MI+CM | |
| Cardiorespiratory Fitness | 35.9 (6.1)a | 37.8 (6.8)a | 38.3 (7.7)a | 37.5 (5.9)a | 37.6 (9.5)a | 38.1 (7.2)a |
| Weekly Exercise Frequency | 1.2 (0.5)a | 0.9 (0.5)b | 2.7 (1.0)c | 3.1 (0.9)d | 1.7 (1.4)e | 1.7 (1.2)e |
| Weekly Exercise MET Hours | 7.1 (5.6)a | 5.6 (5.8)a | 17.7 (12.3)b | 17.8 (9.6)b | 7.9 (9.2)c | 6.7 (6.2)c |
| Weekly Total Standard Drinks | 15.7 (12.9)a | 14.0 (12.8)a | 14.2 (10.8)b | 14.2 (9.3)b | 11.2 (8.2)b | 12.8 (15.5)b |
| Weekly Binge Drinking Episodes | 1.8 (1.1)a | 1.5 (0.7)a | 1.6 (1.0)b | 1.6 (0.9)b | 1.2 (0.9)c | 1.3 (1.0)c |
| BYAACQ Score | 10.6 (4.4)a | 9.9 (4.6)a | 9.0 (5.2)b | 9.5 (5.1)b | 9.2 (5.7)c | 8.0 (5.5)c |
Note. BYAACQ = Brief Young Adult Alcohol Consequences Questionnaire; MI+EC = motivational interviewing plus exercise contracting; MI+CM = motivational interviewing plus contingency management; MET = Metabolic Equivalent. Like letter superscripts within a row denote no significant differences. Unlike superscripts within a row denote significant differences.
Treatment Participation and Satisfaction
As shown in Table 3, attendance at the MI and exercise contracting sessions did not differ between the intervention groups, ps > .05, with all participants completing at least one MI session and 91.4% of participants completing both MI sessions. Approximately 89% of participants in both intervention groups attended all 8 exercise contracting sessions. In terms of number of exercise activities selected and completed with verification, again there were no significant differences between the intervention groups, with an overall average of 30.4 activities selected (out of a total possible 32; SD = 4.9) and 17.9 activities completed with verification (SD = 7.0), ps > .05. Costs of reinforcement for the interventions totaled an average of $37.1 (SD = 9.1) for the MI+EC and $166.5 (SD = 118.4) for the MI+CM. As also shown in Table 3, no differences were noted between groups on treatment satisfaction, p > .05, with both groups rating their satisfaction in the moderately to very satisfied range. Lastly, all participants endorsed improvement and attributed it to the intervention they received with no differences in ratings between the intervention groups, ps > .05.
Table 3.
Treatment participation and satisfaction by intervention group.
| MI+EC | MI+CM | Statistic (df) | p-value | |
|---|---|---|---|---|
| (n =34) | (n =36) | |||
| MI Sessions Attended | 1.91 (0.3) | 1.91 (0.3) | F(1,69) = 0.00 | 1.00 |
| EC Sessions Attended | 7.46 (1.6) | 7.71 (0.7) | F(1,69) = 1.16 | .387 |
| Exercise Activities Selected | 29.74 (6.3) | 31.00 (2.8) | F(1,69) = 1.24 | .293 |
| Exercise Activities Completed | 16.43 (6.7) | 19.37 (7.1) | F(1,69) = 3.18 | .079 |
| CSQ Overall Satisfaction | 1.64 (0.8) | 1.30 (0.5) | F(1,64) = 3.83 | .055 |
| CSQ Change During Intervention | 1.67 (0.5) | 1.72 (0.6) | F(1,64) = 0.20 | .660 |
| CSQ Changes Attributed to Intervention | 1.39 (0.7) | 1.45 (0.7) | F(1,64) = 1.32 | .254 |
Note. MI+EC = motivational interviewing plus exercise contracting; MI+CM = motivational interviewing plus contingency management; CSQ = Client Satisfaction Questionnaire.
Effects on Exercise
See Table 2 for means and standard deviations for each outcome measure at each assessment point. Table 4 displays model fit indices for the best-fitting models for each outcome. Best-fitting LGC models for exercise volume and standard drinks per week showed unacceptable fit to the data and therefore will not be considered further. A comparison of likelihood ratio difference tests revealed that growth in exercise frequency was best depicted by piecewise models (Crawford, Pentz, Chou, Li, & Dwyer, 2003) with two distinct phases of growth representing change during the intervention period (between baseline and 2-month follow-up) and the post-intervention period (between 2- and 6-month follow-up). Coefficients for the assessment points were coded as 0, 1, 1, 1 for the first piece and 0, 0, 1, 2 for the second, and the variance of the first piece was fixed to 0 to permit model identification. As hypothesized, college students in both treatments significantly increased their exercise frequency during the intervention period (Mean Slope = 1.04, standard error [SE] = 0.71, pseudo-z = 14.63, p < .001) followed by a significant decrease over the following 4 months (Mean Slope = −0.49, SE = 0.11, pseudo-z = −4.29, p < .001). Although participants as a whole showed a decrease in exercise frequency between 2- and 6-month follow-up, they were still exercising at greater frequency than baseline. Although exercise frequency increased, participants showed no change in cardiorespiratory fitness, as the linear slope model showed no improvement in fit over an intercept-only (i.e., no change) model.
Table 4.
Chi-square, CFI, and RMSEA Model Fit Indices for Best-Fitting Models for Exercise and Drinking Outcomes
| Variable | χ2(df) | CFIa | RMSEAb | TLIa | SRMRb |
|---|---|---|---|---|---|
| Exercise Volume | 33.88 (7)* | 0.54 | .236 | −.17 | .102 |
| Binge Drinking Episodes | 14.68 (11) | 0.97 | .069 | .95 | .042 |
| Drinks per Week | 12.80 (7) | 0.91 | .109 | .77 | .104 |
| Drinking Consequences | 2.21 (4) | >0.99 | <.001 | 1.08 | .025 |
Note. CFI = Comparative Fit Index. RMSEA = Root Mean Square Error of Approximation. SRMR = Standardized Root Mean Square Residual. TLI = Tucker-Lewis Index.
Cardiorespiratory fitness model fit indices are not depicted because this variable showed no change over time. Exercise frequency model fit indices are not depicted because negative binomial models produced in Mplus do not yield fit indices. Variations in degrees of freedom between models are due to differences in model specification (i.e., linear vs. piecewise) and number of assessment points.
CFI and TLI values of .95 and larger indicate good model fit and values of .90 and larger indicate adequate fit.
RMSEA and SRMR values of .05 and lower indicate good model fit and values of .08 and lower indicate adequate fit.
p < .05
Comparing the intervention conditions, participants who received the MI+CM condition increased their exercise frequency during the intervention period to a greater extent than those who received MI+EC (treatment slope = 0.23, SE = 0.09, pseudo-z = 2.51, p = .012, d = 1.70). There was also a marginal effect favoring the MI+CM condition for changes in exercise frequency between 2- and 6-month follow-ups (treatment slope = 0.15, SE = 0.09, pseudo-z = 1.73, p = .083, d = 0.58). There were no gender differences, ps > .05. During the last two weeks of the intervention, 60.0% of the sample was exercising according to ACSM guidelines, with no differences between the groups, χ2(1) = 2.14, p = .143.
Effects on Drinking
First, examining change over time, participants significantly decreased the number of binge episodes (Mean Slope = −0.07, SE = 0.02, pseudo z = −2.72, p = .007) and consequences associated with alcohol use (Mean Slope = −0.29, SE = 0.09, pseudo z = −3.29, p = .001). Yet, there were no differences in change when the treatment conditions were compared (Binge Episodes: treatment slope = −0.01, SE = 0.03, pseudo z = −0.34, ns, d = 0.01; Consequences: treatment slope = 0.01, SE = 0.18, pseudo z = 0.06, ns, d = 0.00). There were also no gender differences in treatment outcomes, ps > .05.
Finally, we examined parallel process LGC models examining associations between change in exercise and change in alcohol use. In general, these models did not provide adequate fit to the data, and in no case did change in exercise predict change in alcohol use.
Serious Adverse Events
One participant broke her hand while exercising as part of this study. No other study related adverse events were noted, and no participant reported receiving any alcohol-related treatment throughout the 6 month study and follow-up period.
Discussion
This study found that sedentary heavy drinking college students not only actively engaged in an 8 week motivational intervention to help start and maintain a regular exercise routine, but that they significantly increased their exercise behavior in comparison to baseline (when they were exercising approximately once per week). Differences were noted between the intervention conditions in that individuals in the MI+CM condition exercised significantly more often than the individuals randomized to MI+EC condition, with 3.1 episodes per week versus 2.7 episodes per week, respectively, during the 8 week intervention. In comparison to prior studies with sedentary heavy drinkers, our results are similar to the MI+CM condition in Weinstock et al. (2014) in which individuals exercised 2.5 times per week. Results are also similar to Murphy et al.’s (1986) supervised exercise intervention in which individuals exercised 3.4 times per week; however, this is likely an overestimate as they did not account for attrition, in which over a third of the sample randomized to the exercise condition dropped out.
It is not surprising that the interventions increased engagement in exercise, as a meta-analyses find MI yields small to moderate effect sizes in facilitating behavior change (Huh et al., 2015; O’Halloran et al., 2014). Both exercise interventions incorporated other effective components that likely impacted adherence to exercise such as weekly contracting. However, we expected and found that the combination of MI+CM enhanced outcomes over MI+EC. This expectation is rooted in prior research that found a large effect size of prize-based CM interventions (Benishek et al., 2014) and the success of CM in increasing exercise behavior in previous research (e.g., Petry et al., 2013; Weinstock et al., 2014). Thus, despite a strong comparison condition, reinforcing the identified behavior target (i.e., exercise) yielded a moderate to large effect size for exercise outcomes during the intervention period in comparison to reinforcing attendance to the exercise contracting sessions.
In addition to positive changes in exercise behavior, significant reductions in drinking behavior and drinking consequences during the intervention and follow-up periods occurred, with no differences noted between the intervention conditions. Although statistically significant, the differences do not appear to be clinically significant with reductions of less than one binge episode per week and endorsement of one to two fewer consequences over time. These reductions in drinking were consistent with prior studies (Correia et al., 2005; Murphy et al., 1986). However, contrary to our hypothesis, changes in exercise were not predictive of changes in drinking. More research is needed to substantiate these findings.
There are several possible explanations for the failure to find any correspondence between the two behaviors. First, change in drinking outcomes could be a reactivity effect from general study assessments, such that change in drinking is associated with the study procedures. Prior research has shown that completion of an assessment regarding drinking and its negative consequences leads to reductions in college students’ drinking behavior (Walters, Vader, Harris, & Jouriles, 2009). Second, the benefits of exercise can vary across individuals such that these benefits may have differential impact upon drinking; therefore, muddling the relationship between exercise and drinking. For example, in some women exercise may be a compensatory strategy for calories consumed while drinking (e.g., “I can drink tonight since I burned 350 calories running this morning”). In fact, Buchholz and Crowther (2014) found that women who exercised as a compensatory strategy drank at a greater intensity than their peers who were not using exercise as a compensatory strategy. On the other hand, exercise may lead to reductions in drinking via improvements in self-regulation or reductions in impulsivity. Impulsivity is associated with heavy drinking (Coskunpinar, Dir, & Cyders, 2013), and exercise has been shown to reduce impulsivity (Cerrillo-Urbina et al., 2015). To compound matters, drinking consequences can also influence future drinking behavior, such that it can lead to reductions in drinking (Read, Wardell, & Bachrach, 2013). It is possible that our exercise intervention highlighted specific negative consequences that spurred changes in drinking. These examples highlight the many possible divergent effects of exercise upon drinking within college students.
Another reason why exercise may not have been related to drinking outcomes is that the interventions did not directly link the two behaviors with each other. Prior work suggested targeting exercise without addressing drinking would be successful (e.g., Correia et al., 2005; Murphy et al., 1986). However, results from a recent health behavior change meta-analysis find interventions that directly target and link two health behaviors have greater effects than interventions that target only one health behavior with the goal of changing an additional health behavior (Wilson et al., 2015). Going forward, reframing and linking exercise with reductions in heavy drinking under the guise of a health and wellness intervention may be an appropriate means to link and address both behaviors simultaneously, as approximately 33% of college students are sedentary and drink heavily (Luo et al., 2015; Quintiliani et al., 2010).
Long-term exercise outcomes of the study were less robust. Over a four month post-treatment follow-up period engagement in exercise decreased significantly over time with participants averaging slightly less than two episodes per week, which is below current exercise guidelines. Unfortunately, the falloff in exercise behavior over time is common (e.g., Dishman et al., 2014; Murphy et al., 1986; Patel et al., 2016). As there were no differences on outcomes between intervention conditions during the follow-up period, reductions in exercise behavior are not likely due to the removal of incentives specifically for exercise. More likely, other factors contributed to this decline, such as discontinuation of weekly meetings and exercise contracts (i.e., attention, accountability), changes in the environment requiring new behavioral patterns (i.e., going home for breaks), or a failure to develop sufficient intrinsic motivation to sustain exercise over time. Adding a third motivational interview at the completion of the 8-week intervention may enhance intrinsic motivation to sustain the behavioral changes over time.
Limitations of this study inform future research in this area. While objective verification of exercise was required for the weekly exercise contracts, the study did not have an objective measure of physical activity (e.g., accelerometers) and relied on participant self-report. The self-reporting of exercise allowed for assessment over longer periods of time (i.e., months) than would be feasible for objective monitoring, and self-reports converged with the weekly prospective exercise contracts completed during the intervention. Related, changes in exercise behavior did not translate into significant changes in objective markers of cardiorespiratory fitness. The exercise intervention in this study only prescribed and monitored exercise behavior for 8 weeks. A longer, more intensive, supervised exercise program with specific heart rate reserve targets would likely improve cardiorespiratory fitness. Another limitation is that the study was conducted at one university and drinking and other health behaviors differ by college campus (Seo & Li, 2009). Specific attributes of the campus may enhance or diminish engagement in these behaviors (e.g., spring festival weekend, snowy winter climate). Another limitation is that MI intervention did not explicitly address heavy drinking. A few students discussed the relationship between exercise and heavy drinking in their MI sessions; sadly, this information was not systematically tracked which prevents us for examining its impact. Finally, model fit statistics suggested that the models for the exercise volume measure (METs per week) and drinks per week fit the data poorly, although model comparisons suggested the piecewise model provided the best fit of the models we examined. Strengths of the study include the long-term follow-up and the fidelity with which the interventions were delivered.
Overall, exercise interventions devised for this study engaged sedentary heavy drinking college students and facilitated adoption of a consistent exercise routine during the 8-week intervention. Once the intervention was completed exercise behavior diminished over time. Significant reductions in drinking and drinking consequences were found over time, but were not associated with engagement in exercise. This study contributes to a line of literature examining exercise as an intervention for addictive behaviors, and highlights the many complexities in promoting one specific health behavior change with the goal of changing another.
Supplementary Material
Acknowledgments
This research was supported in part by National Institutes of Health grant R21-AA-0177171 and R01-DA-033411-01A1.
Footnotes
Results from this study were previously disseminated at the 45th annual convention of the Association for Cognitive and Behavioral Therapies.
References
- Ahmed SH. Imbalance between drug and non-drug reward availability: A major risk factor for addiction. European Journal of Pharmacology. 2005;526:9–20. doi: 10.1016/j.ejphar.2005.09.036. [DOI] [PubMed] [Google Scholar]
- Ainsworth BE, Haskwell WL, Herrmann SD, Meckes N, Bassett DR, Tudor-Locke C, … Leon AS. 2011 Compendium of Physical Activities: A second update of codes and MET values. Medicine and Science in Sports and Exercise. 2011;43(8):1575–1581. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- American College of Sports Medicine. ACSM's guidelines for exercise testing and prescription. Lippincott Williams & Wilkins; 2013. [DOI] [PubMed] [Google Scholar]
- Benishek LA, Dugosh KL, Kirby KC, Matejkowski J, Clements NT, Seymour BL, Festinger DS. Prize-based contingency management for the treatment of substance abusers: A meta-analysis. Addiction. 2014;109(9):1426–1436. doi: 10.1111/add.12589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Abrantes AM, Read JP, Marcus BH, Jakicic J, Strong DR, … Gordan AA. A pilot study of aerobic exercise as an adjunctive treatment for drug dependence. Mental Health and Physical Health. 2010;3:27–34. doi: 10.1016/j.mhpa.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchholz LJ, Crowther JH. Women who use exercise as a compensatory behavior: How do they differ from those who do not? Psychology of Sport and Exercise. 2014;15(6):668–674. doi: 10.1016/j.psychsport.2014.06.010. [DOI] [Google Scholar]
- Buckworth J, Lee RE, Regan G, Schneider LK, DiClemente LC. Decomposing intrinsic and extrinsic motivation for exercise: Application to stages of motivational readiness. Psychology of Sport and Exercise. 2007;8:399–410. [Google Scholar]
- Carey KB, Scott-Sheldon LAJ, Carey MP, DeMartini KS. Individual-level interventions to reduce college student drinking: A meta-analytic review. Addictive Behaviors. 2007;32(11):2469–2494. doi: 10.1016/j.addbeh.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Nich C, Sifry RL, Nuro KF, Frankforter TL, Ball SA, … Rounsaville BJ. A general system for evaluating therapist adherence and competence in psychotherapy research in the addictions. Drug and Alcohol Dependence. 2000;57:225–238. doi: 10.1016/s0376-8716(99)00049-6. [DOI] [PubMed] [Google Scholar]
- Cerrillo-Urbina AJ, García-Hermoso A, Sánchez-López M, Pardo-Guijarro MJ, Santos Gómez JL, Martínez-Vizcaíno V. The effects of physical exercise in children with attention deficit hyperactivity disorder: A systematic review and meta-analysis of randomized control trials. Child: Care, Health and Development. 2015 doi: 10.1111/cch.12255. [DOI] [PubMed] [Google Scholar]
- Correia CJ, Benson TA, Carey KB. Decreased substance use following increases in alternative behaviors: A preliminary investigation. Addictive Behaviors. 2005;30:19–27. doi: 10.1016/j.addbeh.2004.04.006. [DOI] [PubMed] [Google Scholar]
- Correia CJ, Carey KB, Simons J, Borsari BE. Relationship between binge drinking and substance-free reinforcement in a sample of college students: A preliminary investigation. Addictive Behaviors. 2003;28:361–368. doi: 10.1016/s0306-4603(01)00229-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coskunpinar A, Dir AL, Cyders MA. Multidimensionality in impulsivity and alcohol use: A meta-analysis using the UPPS model of impulsivity. Alcoholism: Clinical and Experimental Research. 2013;37(9):1441–1450. doi: 10.1111/acer.12131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cranford JA, Eisenberg D, Serras AM. Substance use behaviors, mental health problems, and use of mental health services in a probability sample of college students. Addictive Behaviors. 2009;34(2):134–145. doi: 10.1016/j.addbeh.2008.09.004. [DOI] [PubMed] [Google Scholar]
- Curran PJ, Hussong AM. The use of latent trajectory models in psychopathology research. Journal of Abnormal Psychology. 2003;112(4):526–544. doi: 10.1037/0021-843X.112.4.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeVahl J, King R, Williamson JW. Academic incentives for students can increase participating in and effectiveness of a physical activity program. Journal of American College Health. 2005;53:295–298. doi: 10.3200/JACH.53.6.295-298. [DOI] [PubMed] [Google Scholar]
- Dinger MK, Brittain DR, Hutchinson SR. Associations between physical activity and health-related factors in a national sample of college students. Journal of American College Health. 2014;62(1):67–74. doi: 10.1080/07448481.2013.849710. [DOI] [PubMed] [Google Scholar]
- Dishman RK, Jackson AS, Bray MS. Self-regulation of exercise behavior in the TIGER study. Annals of Behavioral Medicine. 2014;48(1):80–91. doi: 10.1007/s12160-013-9573-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan DM, Bigelow GE, Brigham GS, Carroll KM, Cohen AJ, Gardin JG, … Wells EA. Primary outcome indices in illicit drug dependence treatment research: Systematic approach to selection and measurement of drug use endpoints in clinical trials. Addiction. 2012;107(4):694–708. doi: 10.1111/j.1360-0443.2011.03473.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feingold A. Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychological Methods. 2009;14(1):43–53. doi: 10.1037/a0014699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gravetter FJ, Wallnau LB. Statistics for the behavioral sciences. 8. Belmont, CA, US: Thomson Wadsworth; 2014. [Google Scholar]
- Hingson RW. Magnitude and prevention of college drinking and related problems. Alcohol Research & Health. 2010;33(1–2):45–54. [PMC free article] [PubMed] [Google Scholar]
- Huh D, Mun EY, Larimer ME, White HR, Ray AE, Rhew IC, … Atkins DC. Brief motivational interventions for college student drinking may not be as powerful as we think: An individual participant-level data meta-analysis. Alcoholism: Clinical and Experimental Research. 2015;39(5):919–931. doi: 10.1111/acer.12714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irons JG, Pope DA, Pierce AE, Van Patten RA, Jarvis BP. Contingency management to induce exercise among college students. Behaviour Change. 2013;30(2):84–95. [Google Scholar]
- Jeffery RW, Wing RR, Thorson C, Burton LR. Use of personal trainers and financial incentives to increase exercise in a behavioral weight-loss program. Journal of Consulting and Clinical Psychology. 1998;66(5):777–783. doi: 10.1037//0022-006x.66.5.777. [DOI] [PubMed] [Google Scholar]
- Jennings KS, Cheung JH, Britt TW, Goguen KN, Jeffirs SM, Peasley AL, Lee AC. How are perceived stigma, self-stigma, and self-reliance related to treatment-seeking? A three-path model. Psychiatric Rehabilitation Journal. 2015;38(2):109–116. doi: 10.1037/prj0000138. [DOI] [PubMed] [Google Scholar]
- Kahler CW, Hustad J, Barnett NP, Strong DR, Borsari B. Validation of the 30-day version of the Brief Young Adult Alcohol Consequences Questionnaire for use in longitudinal studies. Journal of Studies on Alcohol and Drugs. 2008;69(4):611–615. doi: 10.15288/jsad.2008.69.611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler CW, Strong DR, Read JP. Toward efficient and comprehensive measurement of the alcohol problems continuum in college students: The Brief Young Adult Alcohol Consequences Questionnaire. Alcoholism: Clinical and Experimental Research. 2005;29(7):1180–1189. doi: 10.1097/01.alc.0000171940.95813.a5. [DOI] [PubMed] [Google Scholar]
- Killingsworth MA, Gilbert DT. A wandering mind is an unhappy mind. Science. 2010;330(6006):932–932. doi: 10.1126/science.1192439. [DOI] [PubMed] [Google Scholar]
- Linke SE, Ussher M. Exercise-based treatments for substance use disorders: Evidence, theory, and practicality. The American Journal of Drug and Alcohol Abuse. 2015;41(1):7–15. doi: 10.3109/00952990.2014.976708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. The analysis of social science data with missing values. Sociological Methods & Research. 1989;18(2–3):292–326. doi: 10.1177/0049124189018002004. [DOI] [Google Scholar]
- Lundahl B, Moleni T, Burke BL, Butters R, Tollefson D, Butler C, Rollnick S. Motivational interviewing in medical care settings: A systematic review and meta-analysis of randomized controlled trials. Patient Education and Counseling. 2013;93(2):157–168. doi: 10.1016/j.pec.2013.07.012. [DOI] [PubMed] [Google Scholar]
- Luo J, Agley J, Hendryx M, Gassman R, Lohrmann D. Risk patterns among college youth: Identification and implications for prevention and treatment. Health Promotion Practice. 2015;16(1):132–141. doi: 10.1177/1524839914520702. [DOI] [PubMed] [Google Scholar]
- Lussier JP, Heil SH, Mongeon JA, Badger GJ, Higgins ST. A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction. 2006;101:192–203. doi: 10.1111/j.1360-0443.2006.01311.x. [DOI] [PubMed] [Google Scholar]
- Mailey EL, Wójcicki TR, Motl RW, Hu L, Strauser DR, Collins KD, McAuley E. Internet-delivered physical activity intervention for college students with mental health disorders: A randomized pilot trial. Psychology, Health & Medicine. 2010;15(6):646–659. doi: 10.1080/13548506.2010.498894. [DOI] [PubMed] [Google Scholar]
- Martens MP, Buscemi J, Smith AE, Murphy JG. The short-term efficacy of a brief motivational intervention designed to increase physical activity among college students. Journal of Physical Activity & Health. 2012;9(4):525–532. doi: 10.1123/jpah.9.4.525. [DOI] [PubMed] [Google Scholar]
- Martins RK, McNeil DW. Review of motivational interviewing in promoting health behaviors. Clinical Psychology Review. 2009;29(4):283–293. doi: 10.1016/j.cpr.2009.02.001. [DOI] [PubMed] [Google Scholar]
- Mbuagbaw L, Sivaramalingam B, Navarro T, Hobson N, Keepanasseril A, Wilczynski NJ, Haynes RB. Interventions for enhancing adherence to antiretroviral therapy (ART): A systematic review of high quality studies. AIDS Patient Care STDS. 2015;29(5):248–266. doi: 10.1089/apc.2014.0308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Helping people change. 3. New York, NY, US: Guilford Press; 2013. [Google Scholar]
- Murphy JG, Dennhardt AA, Skidmore JR, Borsari B, Barnett NP, Colby SM, Martens MP. A randomized controlled trial of a behavioral economic supplement to brief motivational interventions for college drinking. Journal of Consulting and Clinical Psychology. 2012;80(5):876–886. doi: 10.1037/a0028763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy TJ, Pagano RR, Marlatt GA. Lifestyle modification with heavy alcohol drinkers: Effects of aerobic exercise and meditation. Addictive Behaviors. 1986;11:175–186. doi: 10.1016/0306-4603(86)90043-2. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. How to use a Monte Carlo study to decide on sample size and determine power. Structural Equation Modeling. 2002;9(4):599–620. doi: 10.1207/S15328007SEM0904_8. [DOI] [Google Scholar]
- O’Brien N, McDonald S, Araujo-Soares V, Lara J, Errington L, Godfrey A, … Sniehotta FF. The features of interventions associated with long-term effectiveness of physical activity interventions in adults aged 55 to 70 years: a systematic review and meta-analysis. Health Psychology Review. 2015:1–29. doi: 10.1080/17437199.2015.1012177. [DOI] [PubMed] [Google Scholar]
- O’Halloran PD, Blackstock F, Shields N, Holland A, Iles R, Kingsley M, … Taylor NF. Motivational interviewing to increase physical activity in people with chronic health conditions: A systematic review and meta-analysis. Clinical Rehabilitation. 2014;28(12):1159–1171. doi: 10.1177/0269215514536210. [DOI] [PubMed] [Google Scholar]
- Oaten M, Cheng K. Longitudinal gains in self-regulation from regular physical exercise. British Journal of Health Psychology. 2006;11(4):717–733. doi: 10.1348/135910706X96481. [DOI] [PubMed] [Google Scholar]
- Panza GA, Weinstock J, Ash GI, Pescatello LS. Psychometric evaluation of the Timeline Followback for Exercise among college students. Psychology of Sport and Exercise. 2012;13(6):779–788. doi: 10.1016/j.psychsport.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel MS, Asch DA, Rosin R, Small DS, Bellamy SL, Heuer J, … Volpp KG. Framing financial incentives to increase physical activity among overweight and obese adults: A randomized, controlled trial. Annals of Internal Medicine. 2016 doi: 10.7326/m15-1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penedo FJ, Dahn JR. Exercise and well-being: A review of mental and physical health benefits associated with physical activity. Current Opinion in Psychiatry. 2005;18:189–193. doi: 10.1097/00001504-200503000-00013. [DOI] [PubMed] [Google Scholar]
- Petry NM, Alessi SM, Ledgerwood DM, Sierra S. Psychometric properties of the Contingency Management Competence Scale. Drug and Alcohol Dependence. 2010;109:167–174. doi: 10.1016/j.drugalcdep.2009.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Andrade LF, Barry D, Byrne S. A randomized study of reinforcing ambulatory exercise in older adults. Psychology and Aging. 2013;28(4):1164–1173. doi: 10.1037/a0032563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Weinstock J, Alessi SM. A randomized trial of contingency management delivered in the context of group counseling. Journal of Consulting and Clinical Psychology. 2011;79(5):686–696. doi: 10.1037/a0024813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plotnikoff RC, Costigan SA, Williams RL, Hutchesson MJ, Kennedy SG, Robards SL, … Germov J. Effectiveness of interventions targeting physical activity, nutrition and healthy weight for university and college students: A systematic review and meta-analysis. International Journal of Behavioral Nutrition and Physical Activity. 2015;12(1):45. doi: 10.1186/s12966-015-0203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poldermans D, Fioretti PM, Forster T, Thompson IR, Boersma E, el-Said EM, … HvU Dobutamine stress echocardiography for assessment of perioperative cardiac risk in patients undergoing major vascular surgery. Circulation. 1993;87:1506–1512. doi: 10.1161/01.cir.87.5.1506. [DOI] [PubMed] [Google Scholar]
- Prendergast M, Podus D, Finney J, Greenwell L, Roll J. Contingency management for substance use disorders: A meta-analysis. Addiction. 2006;101:1546–1560. doi: 10.1111/j.1360-0443.2006.01581.x. [DOI] [PubMed] [Google Scholar]
- Quintiliani L, Allen J, Marino M, Kelly-Weeder S, Li Y. Multiple health behavior clusters among female college students. Patient Education and Counseling. 2010;79(1):134–137. doi: 10.1016/j.pec.2009.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Wardell JD, Bachrach RL. Drinking consequence types in the first college semester differentially predict drinking the following year. Addictive Behaviors. 2013;38(1):1464–1471. doi: 10.1016/j.addbeh.2012.07.005. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption: II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Seo DC, Li K. Effects of college climate on students’ binge drinking: Hierarchical generalized linear model. Annals of Behavioral Medicine. 2009;38(3):262–268. doi: 10.1007/s12160-009-9150-3. [DOI] [PubMed] [Google Scholar]
- Shepard RJ, Thomas S, Weller I. The Canadian home fitness test: 1991 update. Sports Medicine. 1991;11 doi: 10.2165/00007256-199111060-00002. [DOI] [PubMed] [Google Scholar]
- Stout RL, Wirtz PW, Carbonari JP, Del Boca FK. Ensuring balance distributions of prognostic factors in treatment outcome research. Journal of Studies on Alcohol. 1994;12:70–75. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- Ussher M, Sampuran AK, Doshi R, West R, Drummond DC. Acute effect of a brief bout of exercise on alcohol urges. Addiction. 2004;99:1542–1547. doi: 10.1111/j.1360-0443.2004.00919.x. [DOI] [PubMed] [Google Scholar]
- Van Etten ML, Higgins ST, Budney AJ, Badger GJ. Comparison of the frequency and enjoyability of pleasant events in cocaine abusers vs. non-abusers using a standardized behavioral inventory. Addiction. 1998;93:1669–1680. doi: 10.1046/j.1360-0443.1998.931116695.x. [DOI] [PubMed] [Google Scholar]
- Walters ST, Vader AM, Harris TR, Jouriles EN. Reactivity to alcohol assessment measures: An experimental test. Addiction. 2009;104(8):1305–1310. doi: 10.1111/j.1360-0443.2009.02632.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb TL, Sheeran P. Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychological Bulletin. 2006;132:249–268. doi: 10.1037/0033-2909.132.2.249. [DOI] [PubMed] [Google Scholar]
- Weinstock J, Capizzi J, Weber SM, Pescatello LS, Petry NM. Exercise as an intervention for sedentary hazardous drinking college students: A pilot study. Mental Health and Physical Activity. 2014;7(1):55–62. doi: 10.1016/j.mhpa.2014.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White A, Hingson R. The burden of alcohol use: Excessive alcohol consumption and related consequences among college students. Alcohol Research: Current Reviews. 2013;35(2):201–218. [PMC free article] [PubMed] [Google Scholar]
- Wilson K, Senay I, Durantini M, Sánchez F, Hennessy M, Spring B, Albarracín D. When it comes to lifestyle recommendations, more is sometimes less: A meta-analysis of theoretical assumptions underlying the effectiveness of interventions promoting multiple behavior domain change. Psychological Bulletin. 2015;141(2):474–509. doi: 10.1037/a0038295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson MG, Ellison GM, Cable NT. Basic science behind the cardiovascular benefits of exercise. Heart. 2015;101(10):758–765. doi: 10.1136/heartjnl-2014-306596. [DOI] [PubMed] [Google Scholar]
- Wu LT, Pilowsky DJ, Schlenger WE, Hasin D. Alcohol use disorders and the use of treatment services among college-age young adults. Psychiatric Services. 2007;58(2):192–200. doi: 10.1176/appi.ps.58.2.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.