Abstract
A wide range of diabetes-directed interventions – including novel medications, devices and comprehensive education programmes – have been shown to be effective in clinical trials. But in the real world of diabetes care their efficacy is often dependent upon on how well a clinician is able to support personal engagement and motivation of the person with diabetes to use these new tools and knowledge consistently, and as directed. Although many person-centred motivational and behavioural strategies have been developed, for example, action planning, motivational interviewing and empowerment-based communication, the sheer number and apparent lack of clear differences among them have led to considerable confusion. The primary goal of this review, therefore, is to provide a practical framework that organizes and structures these programmes to enhance their more systematic use in clinical care. Its purpose is to enhance clinician efforts to respectfully encourage and support engagement and motivation for behaviour change in people with diabetes. The three-step framework for organizing and describing the specific clinical processes involved is based on self-determination theory and includes: clinician preparation for a different type of clinical encounter, clinician/person with diabetes relationship building, and clinician utilization of specific behavioural tools. We conclude with practical considerations for application of this framework to the real world of clinical care.
Introduction
Despite the plethora of new diabetes-related medications, devices and education programmes developed over the last 10–15 years, many people with diabetes continue to experience significant problems maintaining adequate glycaemic control and altering their lifestyle behaviours to reduce risk and improve health [1]. Although many interventions have been shown to be highly effective in clinical trials, their efficacy in the real world of diabetes care is primarily dependent on the engagement of the person with diabetes, and their motivation and knowledge to adopt and use these interventions as directed over time.
New care delivery programmes that make use of the Chronic Care Model [2] and Patient Centered Medical Home [3] illustrate how health systems are trying to reconfigure themselves to support self-management and motivation through person-centred strategies for those with diabetes [4]. The goal of these programmes is to assure that treatment regimens are sensitive to personal preferences and that people with diabetes have the motivational support and resources to be actively informed and influential in their care [5].
To achieve these ends, many person-centred motivational strategies have been introduced over the years, all designed to provide clinicians with tools to support and encourage improvements in disease management among people with diabetes. Unfortunately, the sheer number and lack of apparent differences among these strategies have led to considerable confusion that has hampered their appropriate selection and systematic application [6]. For example, it is unclear what the critical differences are among commonly advocated clinical approaches, such as empowerment-based communication, engagement, cognitive–behavioural action planning, goal setting, patient activation, informed decision-making, autonomy support, partnership building, tailoring, agenda setting, motivational interviewing or mindfulness, and when during the course of behaviour change each should be employed.
Although the growing literature suggests that many of these strategies are effective [7–9], it remains unclear how these commonly used patient-centred strategies and programmes can be organized in ways that will make it easier for clinicians to use them thoughtfully and systematically in the real word of clinical care. The primary goal of this review, therefore, is to provide a practical framework that organizes and structures these programmes to enhance their more systematic use. Such a framework can then enhance clinician efforts to respectfully encourage and support engagement and motivation for behaviour change in people with diabetes.
We begin by providing a brief historical background of these programmes to provide context and to highlight the differences between traditional and patient-centred approaches to behaviour change in diabetes. We then present a three-step framework for understanding the specific interactional processes involved and conclude with practical considerations for application to clinical care.
Brief contextual overview
The current emphasis on engagement and motivation for behaviour change in diabetes and other chronic diseases has evolved through two overlapping developments. First is the shift in health care from episodic acute care for urgent medical needs to one that provides continuity of care for chronic medical needs [10], a shift that began in the 1930s but expanded dramatically after World War II. In the acute care approach, clinicians gathered and dispensed information about an acute medical condition and then focused heavily on diagnosis and specific treatment. People were expected to follow treatment recommendations until the acute condition resolved. The clinician–person relationship was hierarchical, with the clinician collecting information and dispensing treatment, and the person following through passively with little responsibility for ongoing disease management. In this sense, clinicians treated conditions, not people.
Two linked developments turned this traditional approach on its head: the ageing population and the dramatic rise of chronic conditions, like diabetes. Funnel and Anderson [11] suggest that chronic care differs from acute care insofar as in chronic care the choices that individuals make each day in the management of their disease have a greater impact on their health than the decisions made by clinicians; people are more in control of these choices than clinicians; and because the consequences of personal decisions regarding their disease management affect people directly, they have a major responsibility to manage their disease in ways that best fit their personal preferences and needs.
Furthermore, the shift to a chronic care model pointed to the need for a comprehensive reconfiguration of the clinician/person with diabetes relationship from a hierarchical to a more egalitarian structure. This shift was necessary because, compared with acute care, in chronic care increased personal control and responsibility necessitated a more collaborative approach that takes personal preference into account. It became clear that people with diabetes, not clinicians, make the key daily self-management decisions; without personal engagement and motivation, nothing ordered or recommended by a clinician will make a bit of difference. Therefore, although clinicians can retain their role as experts, they also must become partners with make the key daily self-management decisions, acting as guides and interactive facilitators to help people assume responsibility, make informed decisions and find practical ways to implement mutually agreed upon treatment plans. In this new world, clinicians must treat people and not just conditions.
The second development was the emergence in the 1950s of an approach that views disease within the broad context of an individual's personal, social and cultural worlds, and not just through the lens of physiology [12]. For example, Balint's emphasis on treating the entire person, including their feelings, social setting and response to disease [13]; Carl Rogers' client-centred therapy with an emphasis on unconditional positive regard [14], George Engel's biopsychosocial model [15], Arthur Kleinman's emphasis on the personal and cultural understanding of disease [16], the emergence of family medicine as a primary care specialty [17], and Mulhauser and Berger's patient-centred approaches to diabetes education [18] all contributed to an orientation to care that included viewing the disease within the context of the entire person, understanding the disease from the individual's perspective, and collaboratively developing a treatment plan in ways that fit the personal, social and cultural preferences and goals of individuals.
These two developments led to a dramatic and underappreciated change in the very the role of the clinician and the structure of the traditional clinician/person with diabetes relationship, with several scholars considering this to be a true ‘paradigm shift’ [19,20]. The shift in power and control suggested that clinicians needed to carefully re-examine their skills and strategies for supporting and encouraging autonomy, self-reflection, personal responsibility, and problem-solving in people with diabetes; skills that were rarely necessary in acute care, but are crucial if the person with diabetes is to truly succeed with disease self-management in the real world [21]. This restructuring led to several studies that tried to identify which aspects of clinician activity within this newly restructured relationship affected directly the engagement, motivation and enactment of people with diabetes [22,23]. If people were no longer to be viewed as passive recipients of clinician information and direction, then what would clinicians need to do in their interactions to help people engage actively and responsibly in their own care?
The past 20 years has witnessed the introduction of a host of different approaches to what is now generally called person-centred care. These range from training programmes that guide clinicians to develop more collaborative interactions with people with diabetes to specific tools that structure behaviour change, planning and follow-up. What is needed now is a framework for integrating these approaches into a structure that enables them to be more easily, effectively and systematically applied in clinical care.
A framework for supporting engagement and motivation in people with diabetes
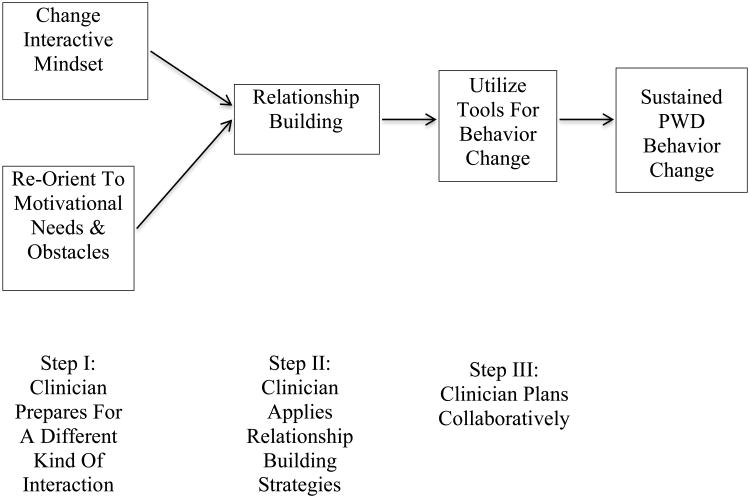
We present a graphical framework in Fig. 1 to organize the processes involved and to describe the landscape of current strategies to enhance person-centred care. Although it may be argued that person-centred strategies should underlie all clinical encounters, they require special expertise and attention when the clinical conversation centres around the motivation for behaviour change in chronic disease [19]. The framework is represented by an ordered, three-step process, with the sequence of clinician activities flowing from left to right.
Figure 1.
A framework to promote motivation for behaviour change in diabetes. PWD, person with diabetes.
At Step I, clinicians undertake two tasks. First, they must shift their mindset from a traditional hierarchical mode of interaction with people to a more empathic, shared, collaborative interactional style. Second, clinicians must re-orient themselves from an information delivery focus to listening for and addressing the nuances of personal engagement and motivation, since both drive behaviour change. This re-orientation is difficult – it takes active clinician effort. It is accomplished by directing clinician attention away from gathering and dispensing information to addressing the motivational needs and conflicts of the person with diabetes. Satisfaction of these needs is crucial if the person with diabetes is to make informed decisions about what they want to do and how they want do it over time.
Step II focuses on applying this re-orientation through the powerful medium of the interaction between clinician and the person with diabetes. We call this process ‘relationship building’, utilizing a different kind of interactional style that employs the principles of motivational change outlined below. Once engagement and motivation have been addressed through the interaction, and only then, Step III comes into play: employing specific behavioural and educational tools and resources to guide and support positive behaviour change, e.g. action plans and structured follow-up visits.
In total, this process focuses on changing clinician behaviour; it encourages clinicians to shift to a different interactional mindset and to focus attention on the motivational needs of the person with diabetes (Step I); apply both through the medium of the clinician/person with diabetes interaction by relationship building (Step II); and then, once engagement and motivation are addressed by this process, and only then, use specific behavioural tools to facilitate behaviour change (Step III). Enactment of all three steps, especially Steps I and II, which often are given short shrift in clinical care, are crucial for maximizing outcomes. We review each below in more detail with illustrations from the literature provided in Table 1.
Table 1. Illustrative applications at each of the three steps of the framework.
| Step | Programme name | Description | Unique characteristics |
|---|---|---|---|
| I – Preparation | Self-determination theory [27,37] | Clinicians change mindset to address three fundamental patient motivational needs: competence, autonomy and relatedness. Clinicians prepare to shift from a hierarchical to an egalitarian, collaborative interaction. Prepare to structure interactions in ways that optimize satisfaction of person's motivational needs. | A focus on personal autonomy and self-direction to satisfy needs and enhance effective behavioural change. Emphasizes that the individual, not the clinician, is the autonomous agent of change. |
| II – Relationship building | Empowerment-based communication [10,11,19] | Focus on person's values to explore areas for self-identified change. Examine their thoughts, meanings and feelings, leading to a five-step behavioural change protocol: explore the problem, clarify feelings and meanings, develop a plan, commit to action and evaluate results. | Strategies to help a person self-identify areas for change through clarifying values and exploring feelings and motivations. |
| Motivational interviewing (MI) [34,38] | A clinician-directed approach to drive a person's ambivalence toward the direction of change by exploring and resolving ambivalence for and against taking action. A seven-step system of questioning called DARN-CAT can be used (desire to change, ability to change, reasons to change, need to change, commitment to change, activation to change, steps toward change). | Clinicians drive change by fostering ambivalence: identify factors that foster change vs. factors that foster maintaining the status quo. Roll with resistance and initiate ‘change talk’ to tilt the ambivalence toward change. | |
| AASAP [39] | Collaborate with the person to label and normalize underlying affect, and show how their feelings drive their actions. | Clinicians identify and label affect to help people understand how their feelings and emotions drive their management behaviour. | |
| Common-sense self-regulatory model [40] | Clinicians help individuals examine their personal beliefs and subsequent emotional responses to illness, especially those beliefs related to disease control, the identity of the condition itself, the anticipated consequences, and the cause of the disease. | A focus on basic beliefs and cognitive perceptions about disease and its management. How people think about disease impacts how they manage it. | |
| III-Behavior change tools | Cognitive-behavioral tools [41, 42] | A broad range of tools based on cognitive-behavioral theory, including highly structured action plans, goal setting, shared decision-making, education, obstacle identification, and a variety of decision aids. Little if any emphasis on motivation, or support for autonomy. | Emphasis on actions regarding specific types of defined behaviour change using highly structured cognitive/behavioural methods. |
| Mindfulness [43,44] | Training to enhance the acceptance and non-judgemental awareness of experience in the present moment to identify internal stressors and states of being that block behaviour change, increase rumination and stimulate over-reactions to disease events. | Training to be aware and accepting of internal emotional states to facilitate decisions around action. | |
| Diabetes Education (DAFNE, DESMOND) [45,46] | Delivering information about diabetes and its management, most often delivered in a group setting. | Providing information delivery. | |
| Web-based, wearable, and other electronic information storage and delivery systems [47,48] | Personalized web-based or worn devices that generally are used to prompt or monitor disease management behaviours over time, e.g. exercise, diet, medication taking. Easily accessed and portable, sometimes linked to clinician support and contact. | Electronic prompting, monitoring and data storage of specific behaviors. |
Step I: Clinician preparation for a different kind of clinical encounter
Having a productive conversation with the person with diabetes about behaviour change in diabetes is quite different from traditional clinician–person with diabetes interactions. Hence the need for a brief period of transition to help clinicians achieve a shift in mindset. The shift is necessary to help clinicians slow the pace of the encounter and prepare to do more listening and reflecting, and possibly to rearrange the examination room chairs and turn off the computer screen to support equality and respect for the person with diabetes. Most clinicians require a moment to separate themselves from the fast pace of regular clinical care to the slower, more reflective pace required by this different kind of clinical conversation [24]. This pace does not necessarily mean that the upcoming visit will require more time; it only means that the clinician will be behaving differently.
This moment of transition also enables clinicians to refocus on the major task of their interaction with the person with diabetes: supporting and encouraging the person's motivation for behaviour change. Self-determination theory [20,25–27] is a straightforward and useful framework that clinicians can use to structure and direct this task. It is a well-documented theory of human motivation frequently applied to the healthcare setting. Developed by Ryan and Deci [28] and applied to the diabetes context primarily by Williams et al. [29], self-determination theory suggests that all human beings have three primary needs that form the basis for self-motivation: needs for competence (feeling personally active, capable and confident), relatedness (feeling connected, understood and supported by important others – like clinicians) and autonomy (needing to act in self-initiated ways with personal control, acting on one's own). ‘Autonomous motivation’, motivation that is intrinsic to the individual and personally driven, emerges when all three of these needs are addressed and supported by clinicians. Autonomous motivation leads to high confidence in the self-determination theory, a positive quality of life, and sustained behavioural change [29]. By contrast, ‘controlled or extrinsic motivation’ occurs when motivation for action is directed by others, for example, by clinicians or family members. Studies show that controlled motivation leads to internal conflict and that the initial behaviour change prompted by this kind of motivation is rarely sustained [29].
Social environments and relationships, especially those between clinicians and people with diabetes, can thwart or enhance the development of autonomous motivation as they play out in the clinician/person with diabetes interaction (Table 2). For example, it has been shown that clinician offers of tangible external rewards (you'll feel better when you …), threats (complications will occur sooner unless you …), deadlines (you'll have to start insulin now unless you …), directives (you must test your blood sugar every morning) and imposed goals (a 5% weight loss is your target) all lead people with diabetes to experience a loss of internal control (autonomy); whereas clinician support for self-direction, personal decision-making, and a secure and trusting relationship enhance autonomous motivation [30]. In general, studies show that clinicians can be trained to increase their support for autonomous motivation; furthermore, those clinicians with high ratings on autonomy support have patients who display better self-regulation, competence, diabetes management and quality of life [27,29,31]. Thus, self-determination theory is clinician-focused; it helps clinicians organize and direct their interactions with people with diabetes in ways that enhance autonomy, competence and relatedness. It is from this conceptual platform that many strategies that support behaviour change, like empowerment-based communication and motivational interviewing, have evolved [20,32].
Table 2. An overview of clinician actions that detract from and enhance relationship building.
| Detract | Enhance |
|---|---|
|
|
The adoption of this more holistic and empathic mindset can generate a deeper understanding of the needs and concerns of people with diabetes, and can dramatically change the interaction clinicians have with them. With this new mindset, clinicians cannot conclude that a person with diabetes is ‘in denial’, is ‘blind’ to how their current disease management practices may be self-destructive, or is simply a ‘bad’ person with diabetes. These perceptions reflect an outdated and less fruitful model of care in which clinicians assume that people with diabetes should follow clinical directives to the letter, and that there is something ‘wrong’ with them if they fail do so. In truth, no person with diabetes wants complications, diabetic ketoacidosis or severe hypoglycaemic episodes. All would prefer to live long and healthy lives. Thus, the changed mindset reminds clinicians that people with diabetes often have their own very good reasons for why they manage their disease as they do, even if their behaviour may be contrary to clinician recommendations. When successful and applied with expertise, this different approach creates a mutually safe, trusting and encouraging environment for a kind of clinician–person with diabetes dialogue that can inform both of underlying their beliefs, expectations, worries and concerns, which can then set the stage for a more effective therapeutic relationship. In this way, clinicians and people with diabetes can work together to develop a more timely, realistic and personally meaningful plan of action, one that people with diabetes are more likely to follow. In sum, Step I helps clinicians prepare for a clinical encounter defined by empathetic active listening and reflection in ways that enable a fuller understanding of the engagement and motivation of people with diabetes.
Step II: Relationship Building
Relationship building occurs through the medium of face-to-face clinical encounters; it is where the clinician's new mindset that was established in Step I is now directly implemented. Relationship building also plays out longitudinally through extensions of the face-to-face encounter, e.g. e-mail interactions, contact with other staff, follow-up phone calls. Thus, relationship building is a process that develops over time; it is typically not an event that occurs at a single encounter.
Numerous studies have tried to identify the specific types of clinician skills and behaviours that enhance relationship building. For example, Gruman et al. [33] listed 48 potential components, Funnell et al. [10] listed 9, Lipkin and Putnam [24] identified 11, and we summarize 23, somewhat overlapping, skills extracted from the literature (Table 2). All are directed at building a collaborative relationship in which people receive support for making their own primary decisions about their diabetes and how to implement them. Clinicians maintain control by expertly guiding the conversation through open-ended questioning, making reflective statements and exploring motivations about change.
Although each of these techniques has a place in a clinician's skill set, truly effective relationship building requires something more: the adoption of a different, overarching clinical style and orientation to the interaction. For example, Funnell and Anderson [11] emphasize that empowerment-based communication is not simply a technique or protocol; rather, it is a vision or orientation that guides each encounter. Likewise, Miller and Rollnick [34] describe motivational interviewing as a conversational style, such that to be successful clinicians need to adopt the ‘motivational interviewing spirit’ through engaging, affirming, reflecting and advising. Hence, a shared component of commonly used programmes involves a form of relationship building that requires that specific interactional techniques become embedded within a broader ‘vision’ or ‘conversational style’ that is deeply sincere, collaborative and affirming. Clinicians may enact many of the techniques listed in Table 2 with no real change in outcome; structured protocols alone do not necessarily lead to trusting, affirming environments for meaningful clinical conversation.
This broader vision includes recognition that regardless of what clinicians think, people with diabetes make most of the decisions about their own disease management and that, ultimately, clinicians cannot ‘get’ people to do much of anything – people with diabetes shape, accept or reject recommendations, and carry them out as they wish independently. An acceptance of this perspective requires a fundamental change in the power hierarchy, with clinicians eschewing the putative role of ‘commander’, ‘doer’, ‘decider’ and ‘treater’ in favour of the role of facilitator, ‘summarizer’, advisor, ‘reflecter’ and ‘guider’. With this perspective, clinicians retain control through their knowledge, expertise and guidance, but they shape the interaction by utilizing a fuller understanding of the values, needs and perspectives of the person with diabetes. Thus, in Step II clinicians are no longer responsible for people with diabetes but are responsible to people with diabetes; they are no longer problem-focused but are people-focused [11].
Interestingly, all of the illustrative programmes listed in Table 1 advocate for a clinician interactional style that is collaborative, empathetic and respectful in ways that conform with self-determination theory; however, they do so with uniquely different emphases. For example, through ‘change talk’, motivational interviewing focuses on the clinician identifying and driving the overt recognition of conflicting motivations; AASAP focuses on identifying, labelling and normalizing the feelings and expectations that drive behavioural change; and the common sense regulatory model emphasizes the need to address underlying beliefs and cognitions associated with the disease held by the person with diabetes.
Step III: Utilize tools for behaviour change
There are many tools and decision aids that can facilitate behaviour change once the engagement and decision-making of the person with diabetes have been addressed successfully in Steps I and II (see Table 1). Some comprehensive programmes that focus initially on the first two steps also include Step III components so that there is a relatively seamless flow from one step to the next. For example, empowerment-based communication focuses on three Step II components (‘active listening’ through open-ended questioning; making reflective, summarizing statements; and ‘building motivation’ by clarifying values and identifying and addressing emotions) and five Step III components, all centred on goal setting. In this manner, comprehensive relationship-building strategies are utilized as a medium of interaction as goal setting and action planning proceed.
By contrast, there are several Step III programmes in Table 1 that do not have explicit built-in Step I or II components. These include most programmes of mindfulness-based stress reduction, web-based or electronic monitoring or behaviour-prompting programmes, and decision aids. Although most diabetes education programmes include patient-centred approaches to information delivery, goal setting, behavioural decision-making, and other self-management support activities, by and large they rarely include the types of specific relationship-building processes described here.
Practical considerations to aid in implementation
Several issues may be helpful when applying this framework in both primary and secondary care settings. First, we suggest that the successful implementation of the framework to support behaviour change in diabetes management requires that all three steps in the framework be fully addressed for each person with diabetes. A very common and critical clinical error occurs when there is a rush to utilize Step III behaviour change tools, such as action plans, without fully developing Steps I and II. Clinicians have a tendency to encourage immediate action without recognizing that careful and timely preparation is required to help people with diabetes achieve sufficient autonomous motivation for a successful outcome. Unless all three steps are thoroughly addressed, behaviour change will not occur, or if it does occur, it will rarely be sustained and, sadly, people with diabetes will experience another management failure.
Collaboratively addressing the needs and perspectives of the person with diabetes also suggests that clinicians and people with diabetes may need to establish more modest initial treatment goals than clinicians might wish. Likewise, the pace of change leading, for example, to improved glycaemic control, might be slower than desired. Thus, clinician needs for immediate, speedy success have to be tempered by what the person with diabetes wants and is able to achieve.
Second, people with diabetes present with varying degrees of motivation for change. The amount of time and clinical energy that is needed for relationship building, therefore, can vary among people with diabetes, and within the same person over time as motivation ebbs and flows based on a host of disease- and non-disease-related factors. Likewise, an individual person with diabetes can present with different levels of motivation for change based on the type of change being considered. For example, a person with diabetes may be more willing to consider a new medication than to begin a structured physical activity or smoking cessation programme. Consequently, because motivation for behaviour change is not consistent both across and within people with diabetes, and across areas of diabetes management within the same person, it is critically important that clinicians address motivation carefully, at each encounter and for each area of change considered. Again, a major caution – the rush to behaviour change without building a solid motivational foundation reduces the probability of sustained positive outcomes.
Third, ideally all members of the diabetes care team should be sensitive to these issues and adopt relationship-building strategies as an overall strategy of good care. It may not be necessary, however, for all team members to be equally skilled and experienced in this regard, as long as all are overtly supportive. Given the variety of practice preferences, personal clinical styles and staffing configurations across clinical settings, it is important to ensure that at least one team member has the requisite skills and abilities to fulfil this function. Programmes that train physicians, specialty nurses, medical assistants, diabetes educators and peer health coaches have shown that almost any active member of the clinical team can fulfil this function given the requisite interest, stylistic proclivity, training and support.
Fourth, developing the requisite relationship-building skills can be difficult and cannot be achieved simply by attending a lecture or a brief workshop [35]. Short-term staff training programmes are rarely effective because relationship building cannot easily be ‘protocolized’. Furthermore, clinicians require time for these skills to develop, and they require ongoing clinical consultation to assure effective application [36]. Although several reports document that training can be highly effective [9], the requirements of successful implementation need to be recognized at the outset; otherwise time and financial resources will be lost.
Fifth, the shift toward collaborative clinician–person with diabetes relationships provides a remarkable counterpoint to current trends in health care, with their emphasis on big data, algorithms for decision-making, and quality assessment based on levels of glycaemic control and other ‘objective’ markers. Conflicting pressures urge clinicians to be time and resource efficient while at the same time addressing the unique, personal needs and preferences of individual people with diabetes. Consequently, to be effective, the adoption of these kinds of relationship-building programmes requires the overt support of clinic managers and practice champions. Otherwise, the well-documented potential of these strategies for improved clinical outcomes will not be achieved.
Conclusions
The explosion of diabetes around the world has evolved into a healthcare crisis, with large numbers of patients not achieving satisfactory metabolic control. Clinician-directed treatment and education alone have in many ways not fully recognized that people with diabetes make far more health management decisions than clinicians. Ultimately, the preferences and needs of the person with diabetes must be respected and addressed in the clinical setting, and must form the basis of treatment. Yet our traditional hierarchical models of care and current ‘data-driven’ health systems often ignore or undermine the very the motivations and preferences of people with diabetes that need to be harnessed so that they can make informed decisions about the management of their disease. Using self-determination theory as a template for addressing motivational needs, we suggest a conceptual rationale and a three-step framework for an alternative approach, one that fully recognizes personal needs for autonomy, competence and relatedness, and that channels these needs into the clinical encounter through the effective use of specific clinician relationship-building skills and behavioural tools.
Acknowledgments
Funding sources: Funded through grants RO1DK094863, R18DK108039 National Institutes of Health, USA.
Footnotes
Competing interests: None declared.
References
- 1.DiMatteo MR. Variations in patients' adherence to medical recommendations: a qualitative review of 50 years of research. Med Care. 2004;42:200–209. doi: 10.1097/01.mlr.0000114908.90348.f9. [DOI] [PubMed] [Google Scholar]
- 2.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Millbank Q. 1996;74:511–544. [PubMed] [Google Scholar]
- 3.Berenson RA, Hammons T, Gans DN. A house is not a home: keeping patients at the center of practice redesign. Health Affairs. 2008;27:1219–1230. doi: 10.1377/hlthaff.27.5.1219. [DOI] [PubMed] [Google Scholar]
- 4.Coulter A. Engaging Patients in Healthcare. New York: McGraw Hill; 2011. [Google Scholar]
- 5.Carman KL, Dardess P, Maurer M, Sofaer S, Adams K, Bechtel C, et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Affairs. 2014;32:223–231. doi: 10.1377/hlthaff.2012.1133. [DOI] [PubMed] [Google Scholar]
- 6.Mead N, Bower P. Patient-centeredness: a conceptual framework and review of the empirical literature. Soc Sci Med. 2000;5:1087–1100. doi: 10.1016/s0277-9536(00)00098-8. [DOI] [PubMed] [Google Scholar]
- 7.Anderson RM, Funnell MM, Butler PM, Arnold MS, Fitzgerald JT, Feste CC. Patient empowerment: results of a randomized controlled trial. Diabetes Care. 1995;18:943–949. doi: 10.2337/diacare.18.7.943. [DOI] [PubMed] [Google Scholar]
- 8.Keeley RD, Brody DS, Engel M, Burke BL, Nordstrom K, Moralez E, et al. Motivational interviewing improves depression outcome in primary care: a cluster randomized trial. J Consult Clin Psychol. 2016;84:993–1007. doi: 10.1037/ccp0000124. [DOI] [PubMed] [Google Scholar]
- 9.Williams GC, McGregor HA, Sharp D, Levesque C, Kouides RW, Ryan RM, et al. Promoting glycemic control through diabetes self-management: evaluating a patient activation intervention. Patient Educ Counsel. 2005;56:58–66. doi: 10.1016/j.pec.2003.11.008. [DOI] [PubMed] [Google Scholar]
- 10.Funnell MM, Tang TS, Anderson RM. From DSME to DSMS: developing empowerment-based diabetes self-mangagement support. Diabetes Spectrum. 2007;20:221–226. [Google Scholar]
- 11.Funnell MM, Anderson RM. Empowerment and self-management of diabetes. Clin Diabetes. 2004;22:123–127. [Google Scholar]
- 12.Robinson JH, Callister LC, Berry JA, Dearing KA. Patient-centered care and adherence: definitions and applications to improve outcomes. J Am Acad Nurse Pract. 2008;20:600–607. doi: 10.1111/j.1745-7599.2008.00360.x. [DOI] [PubMed] [Google Scholar]
- 13.Balint M. The Doctor, his Patient and the Illness. Madison, CT: International Universities Press; 1957. [Google Scholar]
- 14.Rogers C. Client-Centered Therapy: Its Current Practice, Implications and Theory. Cambridge, MT: Riverside Press; 1951. [Google Scholar]
- 15.Engel GL. The clinical applicaiton of the biopsychosocial model. Am J Psychiat. 1980;137:535–537. doi: 10.1176/ajp.137.5.535. [DOI] [PubMed] [Google Scholar]
- 16.Kleinman A. Patients and Healers in the Context of Culture. Berkeley: University of California Press; 1980. [Google Scholar]
- 17.Ransom DC. The rise of family medicine: new roles for behavioral science. Marriage Fam Rev. 1981;4:31–72. [Google Scholar]
- 18.Muhlhauser I, Berger M. Diabetes education and insulin therapy: when will they ever learn? J Intern Med. 1993;233:321–326. doi: 10.1111/j.1365-2796.1993.tb00679.x. [DOI] [PubMed] [Google Scholar]
- 19.Anderson RM, Funnell MM. Patient empowerment: reflections on the challenge of fostering the adoption of a new paradigm. Patient Educ Counsel. 2005;57:153–157. doi: 10.1016/j.pec.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 20.Zoffmann V, Hornsten A, Storbaekken S, Graue M. Translating person-centered care into practice: a comparative analysis of motivational interviewing, illness integration support and guided self-determination. Patient Educ Counsel. 2016;99:400–407. doi: 10.1016/j.pec.2015.10.015. [DOI] [PubMed] [Google Scholar]
- 21.Anderson RM, Funnell MM. Patient empowerment: myths and misconceptions. Patient Educ Counsel. 2010;79:277–282. doi: 10.1016/j.pec.2009.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kaplan SH, Greenfield S, Ware JF. Assessing the effects of physician–patient interaction on outcomes of chronic disease. Med Care. 1989;27:S110–S127. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- 23.Roter D, Stewart M, Putnam S, Lipkin M, Soles W, Inui TS. Communication patterns of primary care physicians. JAMA. 1997;227:350–356. [PubMed] [Google Scholar]
- 24.Lipkin M, Putnam S. The Medical Interview. New York: Springer; 1995. [Google Scholar]
- 25.Friederichs SA, Oenema A, Bolamn C, Lechner L. Motivational interviewing and self-determination theory in a web-based computer tailored physical activity intervention: a randomized controlled trial. Psychol Health. 2016;31:907–930. doi: 10.1080/08870446.2016.1151018. [DOI] [PubMed] [Google Scholar]
- 26.Vansteenkiste M, Williams GC, Resnicow K. Toward systematic integration between self-determnation theory and motivational interviewing as examples of top-down and bottom-up intervention development: autonomy or volition as a fundamental theoretical principle. Int J Behav Nutr Phys Act. 2012;9:23–34. doi: 10.1186/1479-5868-9-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ng YY, Ntoumanis N, Thogersen-Ntoumani C, Deci EL, Ryan RM, Duda JL, et al. Self-determination theory applied to health contexts: a meta-analysis. Psychol Sci. 2012;7:325–340. doi: 10.1177/1745691612447309. [DOI] [PubMed] [Google Scholar]
- 28.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development and well-being. Am Psychol. 2000;55:68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- 29.Williams GC, Patrick H, Niemiec CP, Williams LK, Divine G, Lafata JE, et al. Reducing the health risks of diabetes: how self-determination theory may help improve medication adherence and quality of life. Diabetes Educ. 2009;35:484–492. doi: 10.1177/0145721709333856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Williams GC, Freedman ZR, Deci EL. Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care. 1998;21:1644–1651. doi: 10.2337/diacare.21.10.1644. [DOI] [PubMed] [Google Scholar]
- 31.Williams GC, McGregor HA, Zeldman A, Freedman ZR, Deci EL. Testing a self-determnation theory process model for promoting glycemic control through diabetes self-management. Health Psychol. 2004;23:58–66. doi: 10.1037/0278-6133.23.1.58. [DOI] [PubMed] [Google Scholar]
- 32.Anderson RM, Funnell MM. Ten things patient empowerment is not. Diabetes. 2010;59:185–192. [Google Scholar]
- 33.Gruman J, Rovner M, French ME, Jeffress D, Sofaer S, Shaller D, et al. From patient education to patient engagement: implications for the field of patient educaiton. Patient Educ Counsel. 2010;78:350–356. doi: 10.1016/j.pec.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 34.Miller WR, Rollnick S. Motivational Interviewing Helping People Change. New York: Guilford Press; 2013. [Google Scholar]
- 35.Schwalbe CS, Oh HY, Zweben A. Sustaining motivational interviewing: a meta-analysis of training studies. Addiction. 2014;109:1287–1294. doi: 10.1111/add.12558. [DOI] [PubMed] [Google Scholar]
- 36.Brown JB, Boles M, Mullooly JP, Levinson W. Effect of clinician communication skills training on patient satisfaction A randomized, controlled trial. Ann Int Med. 1999;131:822–829. doi: 10.7326/0003-4819-131-11-199912070-00004. [DOI] [PubMed] [Google Scholar]
- 37.Ryan RM, Patrick H, Deci EL, Williams GC. Facilitating health behavior change and its maintenance: interventions based on self-determination theory. Eur Health Psychol. 2008;10:2–5. [Google Scholar]
- 38.Copeland L, McNamara R, Kelson M, Simpson S. Mechanisms of change within motivational interviewing in relation to health behaviors outcomes: a systematic review. Patient Educ Counsel. 2015;98:401–411. doi: 10.1016/j.pec.2014.11.022. [DOI] [PubMed] [Google Scholar]
- 39.Fisher L, Hessler DH, Naranjo D, Polonsky WH. AASAP: a program to increase recruitment and retention in clinical trials. Patient Educ Counsel. 2011;86:372–377. doi: 10.1016/j.pec.2011.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jones CJ, Smith HE, Llewellyn C. A systematic review of the effectiveness of interventions using the common-sense self-regulatory model to improve adherence behaviors. J Health Psychol. 2016;21:2709–2724. doi: 10.1177/1359105315583372. [DOI] [PubMed] [Google Scholar]
- 41.Norris SL, Engelgau MM, Narayan KM. Effectiveness of self-management training in type 2 diabetes. Diabetes Care. 2001;24:561–587. doi: 10.2337/diacare.24.3.561. [DOI] [PubMed] [Google Scholar]
- 42.Handley M, MacGregor K, Schillinger D, Sharifi D, Wong S, Bodenheimer T. Using action plans to help primary care patients adopt healthy behaviors: a descriptive study. J Am Board Fam Med. 2006;19:224–231. doi: 10.3122/jabfm.19.3.224. [DOI] [PubMed] [Google Scholar]
- 43.Demarzo MM, Montero-Marin J, Zabeleta-del-Olmo E, Mabtani KR, Vellinga A, Vicens C, et al. The efficacy of mindfulness-based interventions in primary care: a meta-analytic review. Ann Fam Med. 2015;13:573–582. doi: 10.1370/afm.1863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gu J, Strauss C, Bond R, Cavanagh K. How do mindfulness-based cogntive therapy and mindfullness-based stress reduction improve mental health and well-being? A systematic reivew of mediation studies. Clin Psychol Rev. 2015;37:1–12. doi: 10.1016/j.cpr.2015.01.006. [DOI] [PubMed] [Google Scholar]
- 45.DAFNE. Trining in flexible, intensive insulin management to enable dietary freedom in people with type 1 diabetes: dose adjustment for normal eating (DAFNE) rnadomized controlled trial. BMJ. 2002;325–331:746. doi: 10.1136/bmj.325.7367.746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Davies MJ, Heller S, Skinner TC, Campbell MJ, Carey ME, Cradock S, et al. Effectiveness of the diabates education and self-management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: cluster randomized controlled trial. BMJ. 2008;336:491–495. doi: 10.1136/bmj.39474.922025.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Glasgow RE. Interactive media for diabetes self-management: issues in maximizing public health impact. Med Decis Making. 2010;30:745–758. doi: 10.1177/0272989X10385845. [DOI] [PubMed] [Google Scholar]
- 48.Glasgow RE, Kurz D, King DK, Dickman JM, Faber AJ, Halterman E, et al. Twelve-month outcomes of an Internet-based diabetes self-management support program. Patient Educ Counsel. 2012;87:81–92. doi: 10.1016/j.pec.2011.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]