Abstract
Bronchopulmonary dysplasia (BPD) is the most common chronic respiratory complication of preterm birth. Preterm infants are at risk for acute lung injury immediately after birth, which predisposes to BPD. In this article, we review the current evidence for interventions applied during neonatal transition (delivery room and first postnatal hours of life) to prevent BPD in extremely preterm infants: continuous positive airway pressure (CPAP), sustained lung inflation, supplemental oxygen use during neonatal resuscitation, and surfactant therapy including less-invasive surfactant administration (LISA)
Preterm infants should be stabilized with CPAP in the delivery room, reserving invasive mechanical ventilation for infants who fail non-invasive respiratory support. For infants who require endotracheal intubation and mechanical ventilation soon after birth, surfactant should be given early (<2 hours of life). We recommend prudent titration of supplemental oxygen in the delivery room to achieve targeted oxygen saturations. Promising interventions that may further reduce BPD, such as sustained inflation and non-invasive surfactant administration, are currently under investigation.
Keywords: bronchopulmonary dysplasia, preterm, infant, resuscitation, surfactant, continuous positive airway pressure, sustained inflation, oxygen
Background
Extremely preterm infants are at high risk for acute lung injury and subsequent chronic lung disease, or bronchopulmonary dysplasia (BPD). BPD affects approximately 25%–40% of surviving very low birth weight (VLBW) infants, (1,2) with the highest incidence among those born at the lowest gestational ages. (3,4) BPD is associated with impaired lung function that persists into adolescence and adulthood. (5–8) In addition, BPD is an important risk factor for adverse non-respiratory outcomes including growth failure, (9,10) neurodevelopment impairment, (11,12) and poor school-age performance. (13)
Considerable data suggest that early lung and systemic inflammation contribute to the pathogenesis of BPD. (14–17) These discoveries led to significant research into early postnatal interventions to prevent or ameliorat early lung inflammation and injury in extremely preterm infants. Immediately after birth, the newborn infant must open and aerate the lung to initiate the transition from a fetal to a post-natal circulation and physiology. However, most extremely preterm infants struggle to independently aerate the lung, owing to a compliant chest wall, (18,19) weak respiratory muscles, altered epithelial sodium channels, (20) and immature surfactant. (21) Consequently, most extremely preterm infants require positive pressure ventilation and/or supplemental oxygen after birth. Although these therapies are often necessary to ensure adequate gas exchange, they may induce acute lung injury from baro- and volutrauma and oxygen free radical formation. Therefore, ideal strategies for BPD prevention should start immediately after preterm birth to limit lung injury and oxidative stress.
About This Article
The focus of this narrative review is an analysis of the current literature describing interventions applied during neonatal transition to prevent BPD in extremely preterm infants. We present the current evidence for therapies used in the delivery room or initial hours of life: continuous positive airway pressure (CPAP), sustained lung inflation, supplemental oxygen use during resuscitation, surfactant therapy (via endotracheal tube), and less-invasive surfactant administration (LISA). Subsequent therapies to prevent BPD have been reviewed elsewhere and are not the focus of this article. (22–24)
We included high-quality randomized controlled trials (RCTs), meta-analyses, and key observational studies. Further, we conducted a meta-analysis of published RCTs comparing LISA versus control therapies in infants born ≤32 weeks gestational age (GA) with a reported outcome of BPD or the composite of BPD or death as an outcome. This analysis was performed with Review Manager (RevMan) Version 5.3 (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014).
1. CPAP
Use of non-invasive continuous positive airway pressure (CPAP) immediately after birth facilitates lung recruitment and formation of a functional residual capacity (FRC). Non-invasive CPAP mitigates lung injury by avoiding baro-volu-trauma from mechanical ventilation or atelecto-trauma that can result from repeated collapse and expansion of the alveoli during room air breathing. Early observational data from 1987 suggested that aggressive early use of CPAP reduced BPD. (25) Protocols describing the successful use of CPAP for delivery room resuscitation of extremely low birth weight (ELBW) infants with selective intubation and surfactant administration reserved for infants who failed CPAP followed soon after. (26)
Some 10–15 years after these initial descriptions, several large multicenter randomized trials of respiratory management after birth compared an initial strategy of early CPAP with immediate intubation and surfactant administration. The largest of these were COIN, (27) SUPPORT, (28) and the Vermont Oxford Network delivery room management trial. (29)
In the COIN trial, Morley et al. randomized 610 infants from 25 to 28 6/7 weeks gestation to initial respiratory management of either initial CPAP therapy or mechanical ventilation. (27) The SUPPORT trial enrolled 1316 infants between 24–27 6/7 weeks gestation who were randomized before birth to initial CPAP therapy with subsequent selective surfactant administration and a limited ventilation strategy versus mechanical ventilation and prophylactic surfactant therapy. (28) Last, in the Vermont Oxford Network trial, Dunn et al. randomized 648 infants between 26–29 6/7 weeks gestation to the following modes of respiratory support: prophylactic surfactant followed by mechanical ventilation, prophylactic surfactant followed by extubation to CPAP, or initial CPAP therapy with selective surfactant treatment. (29)
Many study design elements varied between these trials, including enrollment size, the gestational ages of enrolled infants, antenatal versus postnatal randomization, timing of respiratory interventions, and initial CPAP settings (ranging from 5cm H2O to 8cm H2O). Despite these differences, all three trial results were consistent for the outcome of BPD. Each trial demonstrated a non-significant reduction in the rate of death or BPD at 36 weeks PMA among infants treated with CPAP, compared to empiric intubation and mechanical ventilation. In pooled analyses of these RCTs, there was a small, but statistically significant reduction in the risk for death or BPD in the CPAP treated infants. The NNT reported by these meta-analyses (some of which included smaller RCTs) ranged from 20–35. (30–32)
While the rate of pneumothorax was higher in CPAP-treated infants in the COIN trial, (27) neither of the other trials reported increased risk for air leaks among infants treated with initial CPAP. In meta-analysis, initial CPAP with selective surfactant was not associated with increased risk for pneumothorax or other adverse events. (31,32)
Based on these findings, the American Academy of Pediatrics Committee on Fetus and Newborn subsequently published a policy statement concluding that, “the early use of CPAP with subsequent selective surfactant administration in extremely preterm infants results in lower rates of BPD/death when compared with treatment with prophylactic or early surfactant therapy.” (33)
2. Sustained Inflation
Sustained inflation (SI) is a lung recruitment strategy used immediately after birth. SI holds an inflating pressure for a prolonged duration to achieve lung fluid clearance and to establish the FRC. In 1981, Vyas et al. described a 5-second SI to asphyxiated term newborns after birth. (34) Subsequent observational studies demonstrated the feasibility and safety of performing SI in preterm infants during neonatal transition.
Five randomized trials of SI in extremely preterm infants have been published to date (Table 1). (35–39) Harling et al. randomized 52 infants <31 weeks gestation to receive either a 5-second SI or a 2-second “conventional” lung inflation as the initial positive pressure inflation delivered after birth. (35) There were no significant differences between groups for the primary outcome, bronchoalveolar lavage cytokine levels, or secondary outcomes of death, BPD, or major neonatal morbidities. (35) Since there was only a 3-second difference in duration of the initial lung inflation, the SI maneuver in this trial may not have been long enough to demonstrate significant differences between groups.
Table 1.
Published randomized trials comparing SI with IPPV in extremely preterm infants
| Study | Population | Comparison | Primary outcome | Comments |
|---|---|---|---|---|
| Lindner 2005 (36) | 61 infants 25–28 6/7 weeks GA | Up to three SI (20–30 cm H2O X15 seconds) vs. IPPV Both via NP tube |
Intubation at 48 HOL: SI (61%) vs. IPPV (70%), OR 0.68 (95 % CI 0.23–1.97) | Closed early for slow recruitment; under powered to detect a significant difference in primary outcome rates |
| Harling 2005 (35) | 52 infants <31 weeks GA | One SI (25–30 cm H2O X5 seconds) vs. IPPV (2 second inflation), via facemask or ETT | Cytokine concentrations from BAL at 12 hours of life: no significant differences between groups | Minimal treatment difference between groups Non-clinical primary outcome |
| te Pas 2007 (37) | 207 infants 25–326/7 weeks GA | Up to two SI (20–25cm H2O X10 seconds) with PEEP via NP tube vs. IPPV without PEEP via facemask | Intubation within 72 HOL: SI (37%) vs. IPPV (51%), OR 0.57 (95% CI 0.32–0.98) | No PEEP during IPPV for the control group, Different devices and interfaces used between groups |
| Lista 2015 (38) | 291 infants 25–286/7 weeks GA | Up to two prophylactic SI (25 cm H2O X15 seconds) via facemask vs. nasal CPAP with subsequent resuscitation per NRP guidelines | Intubation within 72 HOL: SI (53%) vs. CPAP (65%), OR 0.62 (95% CI 0.38–0.99) | Infants received prophylactic SI, regardless of respiratory status after birth |
| Jiravisitkul 2017 (39) | 81 infants 25–32 weeks GA | Up to two SI (25 cm H2O X15 seconds) via facemask vs. IPPV with PEEP via facemask | Mean FiO2 at 10 minutes after birth: SI (0.28, 95% CI: 0.26–39) vs. control (0.47, 95% CI: 0.43–0.52), p<0.001 | Proximal primary outcomes. Heart rate and pulse oximetry in first 10 minutes and delivery room intubation: no significant differences between groups |
Abbreviations: BAL: bronchoalveolar lavage, BPD: bronchopulmonary dysplasia, CI: confidence interval, CPAP: continuous positive airway pressure, GA: gestational age, HOL: hours of life, IPPV: intermittent positive pressure ventilation, NRP: neonatal resuscitation program, OR: odds ratio, PEEP: positive end expiratory pressure, SI: sustained inflation
In a RCT stopped early for slow recruitment, Lindner et al. randomized 61 preterm infants to treatment with up to three 15-second SIs vs. intermittent positive pressure ventilation (IPPV) with positive end expiratory pressure (PEEP). (36) There was no significant difference between treatment groups in the primary outcome, intubation in the first 48 hours of life, or secondary outcomes of death or chronic lung disease. (36)
te Pas et al. enrolled 207 infants <33 weeks gestation who required positive pressure ventilation after birth in a single-site RCT comparing one to two SIs (10 seconds each) with IPPV. (37) Infants treated with SI experienced a reduced rate of the primary outcome, intubation in the first 72 hours of life, and the secondary outcome of moderate/severe BPD (9% vs. 19%, OR 0.41, 95% CI 0.18–0.96). Unfortunately, different interfaces and respiratory devices were used between treatment groups, making it difficult to isolate SI as the single cause of improved outcomes. (37)
The multisite SLI (Sustained Lung Inflation) trial randomized infants between 25–286/7 weeks gestation to receive up to two 15-second SIs or nasal CPAP, with subsequent resuscitation according to Neonatal Resuscitation Program guidelines. (38) The primary outcome of this trial, mechanical ventilation within the first 72 hours after birth, was significantly lower in infants treated with SI. This trial was not powered for the outcome of BPD, and BPD rates did not significantly differ between groups. (38)
Jiravisitkul et al. performed a single-site RCT of 81 infants between 25–32 weeks gestation who were randomized to receive up to two 15-second SIs or IPPV with subsequent resuscitation per NRP guidelines. (39) The mean fraction of inspired oxygen 10 minutes after birth- a primary outcome- was lower in the SI group compared with infants in the IPPV group. There were no significant differences in the other primary outcomes (heart rate and SpO2 in the first 10 minutes of life, or rates of delivery room intubation) between groups. There was no significant difference between treatment groups in the secondary outcome of BPD. (39)
A meta-analysis, comprising 611 preterm infants from four of these trials, found no significant differences in the rates of BPD, death, or the composite outcome of BPD or death among those treated with SI compared to the control therapy. (40) However, these results should be interpreted cautiously, as the individual trials varied considerably with regards to the duration and peak pressures of the SI, the administered control therapies, resuscitation devices, and demographic characteristics of the enrolled infants (Table 1). Two ongoing trials of SI with the primary outcome of BPD or death will provide important information on the safety and efficacy of SI for the prevention of BPD in extremely preterm infants. (41,42)
3. Supplemental Oxygen during Resuscitation
The transition from the relatively hypoxemic fetal state to a normal post-natal oxygen saturation (SpO2) is a gradual process after birth. To adequately support gas exchange while avoiding hyperoxia-related toxicity to developing organs, such as the lungs and retina, clinicians try to judiciously regulate supplemental oxygen use in preterm infants. This effort is hampered by the lack of robust data on the normal SpO2 transition in extremely preterm infants, which in turn complicates efforts to determine the optimal approach to FiO2 titration after birth.
Dawson et al. published nomograms of SpO2 after birth, which were generated from 468 infants who did not require respiratory support after birth. (43) However, only 39 (8%) of the infants included in the Dawson curves cohort were born preterm (<32 weeks GA). To address this gap, Vento et al. recorded serial SpO2 measurements in 102 preterm infants (median GA 29 weeks) who were stabilized using CPAP without supplemental O2 after birth. Infants in that study achieved reference values of SpO2 faster than the preterm infants in Dawson’s study (who received no respiratory support). (44) In contrast, Mian et al. found that rise in SpO2 lagged behind both the Dawson and Vento nomograms, in their cohort of 55 preterm infants (mean GA 31 weeks) supported on CPAP, despite provision of supplemental oxygen to many of these infants. (45) Importantly, the normative ranges for SpO2 rise described in all these studies were derived mostly in moderately preterm infants. They therefore may not be generalizable to the most extremely preterm infants, who are at highest risk for both impaired gas exchange due to immature lungs as well as injury from oxygen toxicity.
Several RCTs have compared an initial approach of low versus high oxygen administration during delivery room resuscitation of preterm infants. (46–54) These trials varied considerably in study design and many of are limited by small sample sizes and use of only very proximal outcomes (Table 2). Two of these RCTs reported a significant reduction in BPD among infants in whom resuscitation was initiated with lower FiO2. (49,52) However, a meta-analysis comprising RCTs conducted in preterm infants (≤32 weeks GA) demonstrated no significant difference in the risks for BPD (RR 1.11, 95% CI 0.73–1.68) or mortality (RR 0.62, 95% CI 0.37–1.04) between infants treated with low versus high initial concentrations of supplemental oxygen. (55) More recently, Oei et al. performed a meta-analysis restricted to RCTs comparing low (≤ 0.3) vs. high (≥0.6) FiO2 for resuscitation in infants born ≤28 weeks GA. (56) There was no significant difference between groups for the outcomes of BPD among survivors (37% low oxygen vs. 41% high oxygen, RR 0.88, 95% CI 0.68–1.14) or mortality (14% low oxygen vs. 12% high oxygen, RR 0.99, 95% CI 0.52–1.91). (56)
Table 2.
Published randomized trials comparing low versus high FiO2 during delivery room stabilization
| Author | Population | Comparison | Primary outcome | Comments |
|---|---|---|---|---|
| Lundstrøm, 1995 (46) | 70 infants <33 weeks GA | Initial FiO2 21% vs. 80%, titrated clinically by response in HR. | Cerebral blood flow (measured by xenon clearance) at 2 HOL higher in low oxygen group (median 15.9 vs. 12.3 ml/100g/min), p<0.0001 | FiO2 titrated based on HR, not SpO2. Secondary outcome: No significant difference in supplemental O2 at 28 days |
| Harling, 2005 (47) | 52 infants <31 weeks GA | FiO2 50% vs. 100% | Cytokine concentrations in BAL collected at 12 HOL: no significant differences | Secondary outcome: No significant difference in survival without BPD |
| Wang, 2008 (48) | 41 infants 23–316/7 weeks GA | Initial FiO2 21% vs. 100%, titrated per protocol | SpO2 values during stabilization. SpO2 significantly lower in 21% FiO2 group from 2–10 MOL. | Secondary outcome: No significant difference in supplemental O2 at 36 weeks PMA |
| Vento, 2009 (49) | 78 infants 24–28 weeks GA | Initial FiO2 30% vs. 90%, titrated per protocol | Neonatal death (<28 days) and BPD at 36 weeks PMA. No difference in neonatal death. Less BPD among survivors in low FiO2 group (15% vs. 32%, p<0.05). | Secondary outcomes: Low FiO2 group had significantly fewer days of supplemental O2 and mechanical ventilation and lower markers of oxidative stress and inflammation |
| Rabi, 2011 (50) | 106 infants ≤32 weeks GA | FiO2: high (100% static), moderate (initial 100%, titrated), or low (initial 21%, titrated) | Time within target SpO2 85–92% No differences in time to reach target SpO2. Moderate group with greater proportion of time spent in target SpO2 range than high group. | Secondary outcomes: no significant difference in BPD, death, or duration of mechanical ventilation |
| Armanian, 2012 (51) | 32 infants 29–34 weeks GA | Initial FiO2 30% vs. 100%, titrated per protocol | Outcomes reported: SpO2 and HR per minute of life. More infants In 100% FiO2 with HR>100 bpm at 2 MOL (94% vs. 50%, p=0.008) | Unclear primary outcome. All proximal outcomes (within first 5 MOL). Clinically relevant in-hospital outcomes not reported |
| Kapadia, 2013 (52) | 88 infants 24–346/7 weeks GA | Initial FiO2 21% versus 100%, titrated per protocol | Improved oxidative balance ratio (serum [BAP/TH]) at 1 HOL in 21% FiO2 group (median 13 vs. 8, p<0.01) | Secondary outcome: 21% FiO2 with less BPD (7% vs. 25%, p<0.05) |
| Rook, 2014 (53) | 193 infants <32 weeks GA | Initial FiO2 30% vs. 65%, titrated per protocol | BPD at 36 weeks PMA: no significant difference between groups, 24% (low FiO2) vs. 17% (high FiO2), p=0.15 | Secondary outcomes: no differences in duration of mechanical ventilation or markers of oxidative stress |
| Oei (2017) (54) | 287 infants <32 weeks GA | Initial FiO2 21% versus 100%, titrated per protocol | Primary outcome (death or major disability at 2 years) not yet reported. | No significant difference in BPD between groups. Ancillary analysis of 119 enrolled infants revealed higher oxidative stress markers in the 100% FiO2 group (91) |
Abbreviations BAL: bronchoalveolar lavage, BAP: biological antioxidant potential, BPD: bronchopulmonary dysplasia, BPM: beats per minute, FiO2: fraction of inspired oxygen, GA: gestational age, HOL: hour(s) of life, HR: heart rate, MOL: minute(s) of life, PMA: post-menstrual age, SpO2 oxygen saturation (pulse oximetry), TH: total hydroperoxide
The Oei meta-analysis included results from the TO2RPIDO trial, which randomized infants <32 weeks gestation to delivery room resuscitation started with 21% vs. 100% oxygen. (54)This was an early-stopped trial, which ceased recruitment after just 292 of the targeted 1986 subjects were recruited (of which 287 were included in the analysis). An un-prespecified subgroup analysis of infants <28 weeks gestation in this trial demonstrated higher mortality in the 21% FiO2 group (22% vs. 6%, p =0.01). (54) In an observational study, Rabi et al. studied 2,326 infants ≤ 27 weeks GA born in Canada before and after local practice changed from initiating resuscitation with 100% FiO2 to lower oxygen concentrations (typically 21–40%) with subsequent titration. (57) Rates of BPD were similar between the two epochs. However, the composite outcome of death or severe neurologic injury was significantly more frequent among infants resuscitated with an initially lower FiO2 (adjusted OR 1.36, 95% CI 1.11–1.66). (57)Results from both of these studies should be interpreted cautiously, due to limitations from stopping early (58) (the TO2RPIDO trial) (54) and the before/after study design relying on an exposure of reported policy changes (Rabi et al.). (57)
While the pooled available data do not suggest that initial FiO2 during resuscitation influences the outcome of BPD, the optimal initial concentration of supplemental oxygen used during neonatal resuscitation and time to reach “normal” SpO2 in extremely preterm infants remains an important evidence gap. The 2015 International Liaison Committee on Resuscitation recommended starting resuscitation for preterm infants with a low FiO2 concentration (21–30%), but acknowledged the need for more evidence.(59) The ongoing PreSOX trial (60) may provide more information about the optimal use of oxygen during resuscitation to minimize mortality and morbidity in preterm infants.
4. Surfactant Administration after Standard Endotracheal Intubation
Beginning in the 1980s, several high-quality RCTs assessed the safety and timing of surfactant administration in preterm infants. (61–63) Early RCTs demonstrated that administration of surfactant to preterms with established RDS reduced pulmonary air leak and lowered the risk of death or supplemental oxygen use at 28 days of age (the standard definition of BPD at that time). (61–63) Subsequent studies found that prophylactic administration of surfactant soon after birth also reduced pulmonary morbidity and improved BPD-free survival. (61,62) However, most of these RCTs were conducted prior to the routine use of antenatal corticosteroids and aggressive use of non-invasive CPAP. As discussed above in the section on CPAP, prophylactic intubation and surfactant administration, compared with early non-invasive CPAP therapy, does not reduce BPD risk in preterm infants.(30–32)
Unfortunately, stabilization with non-invasive respiratory support is not possible in all preterm infants. Up to 65% of spontaneously breathing extremely preterm babies require intubation and mechanical ventilation despite early CPAP therapy.(31) In these instances, early rescue surfactant therapy is appropriate. Providing early rescue surfactant (within the first 2 hours of life) to mechanically ventilated preterm infants, as compared to delayed surfactant administration (after second hour of life), reduces the risk of BPD (RR 0.69, 95% CI 0.55–0.86) and the composite of death or BPD (RR 0.83, 95% CI 0.75–0.91). (64)
When surfactant is indicated, there are several animal-derived (modified or purified from bovine or porcine lungs) and synthetic formulations available for use. Animal-derived surfactants compared to first-generation protein free surfactants are associated with a marginal reduction in mortality (RR 0.89, 95% CI 0.79 to 0.99) and death or BPD (RR 0.95, 95% CI 0.91 to 1.00). (65)Meta-analysis of trials comparing modified bovine mined lung surfactant to porcine minced lung surfactant raised concern that bovine surfactant may increase risk for mortality, BPD, and other adverse outcomes. (66) However, in a subgroup analysis, the improvement in morbidity and mortality risk was limited to the trials using a higher initial dose of porcine minced lung surfactant (> 100mg/kg). (66) It is uncertain whether the differences in outcome risks are from differences in the surfactant dose or extraction source. A second-generation synthetic surfactant (lucinactant) containing a peptide analog of surfactant protein-B is also now available and has similar efficacy as animal-derived products. (67,68)
To maximize the potential benefits of early surfactant administration without undergoing prolonged mechanical ventilation, Victorin et al. introduced the technique of INtubation, SURfactant administration during brief mechanical ventilation, followed by Extubation (INSURE approach). (69) Initial RCTs found that the INSURE approach compared to selective administration of surfactant to infants with established RDS reduced the need for mechanical ventilation and use of supplemental oxygen at 28 days of life. (70) However, when compared to early stabilization with CPAP alone, INSURE does not reduce BPD. In a meta-analysis of 9 RCTs that included a total of 1551 preterm infants, Isayama et al. reported that INSURE compared to CPAP did not significantly affect the risk for death or BPD (RR 0.88, 95% CI 0.76–1.02). (71)
5. Less Invasive Surfactant Administration
In an effort to avoid standard endotracheal intubation, several less invasive techniques of surfactant administration have been developed. These include intratracheal instillation of surfactant with a thin catheter (e.g. nasogastric tube), aerosolized administration, intrapartum pharyngeal instillation, and delivery via a laryngeal mask airway (LMA). (72)Of these strategies, surfactant instillation via thin catheter, often referred to as less invasive surfactant administration (LISA) or minimally invasive surfactant therapy (MIST), is the most studied. Verder et al. first published their experience with LISA in the early 1990s. (73) In a large, multi-center observational study (n=2,206) of preterm infants treated with LISA versus matched controls, LISA was associated with lower rates of mechanical ventilation (41% vs. 62%, p<0.001) and death or BPD (14% vs. 21%, p < 0.001). (74)
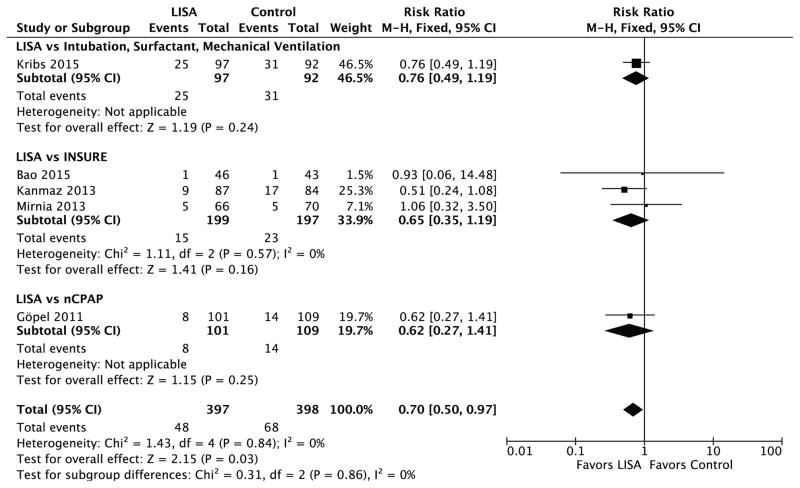
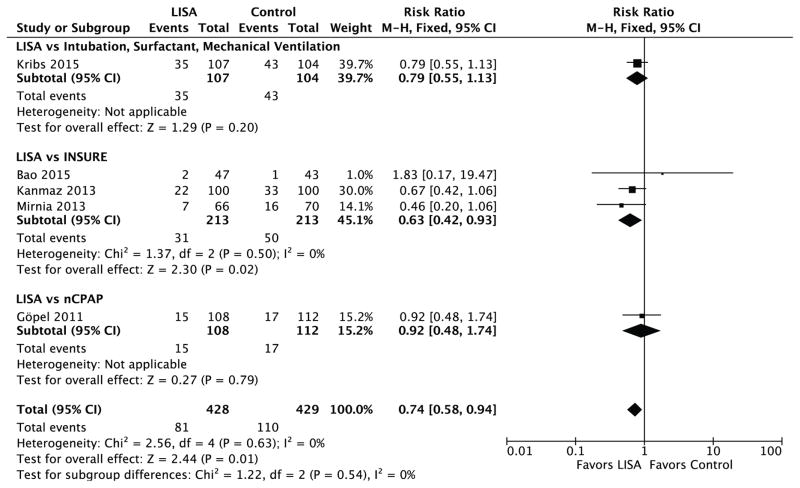
Four RCTs conducted in extremely preterm infants compared LISA to surfactant administration via endotracheal tube (3 versus INSURE, 1 versus continued mechanical ventilation after surfactant therapy), (75–78) and one compared LISA to ongoing nasal CPAP therapy. (79) Here, we report a meta-analysis of data combined from these five RCTs (total n=857). Using data combined from all 5 trials, LISA versus control therapy reduced the risk for BPD among survivors to at least 36 weeks PMA (RR 0.70, 95% CI 0.50 to 0.97; typical risk difference −0.05, 95% CI −0.10 to −0.01; number needed to treat [NNT] 19; 95% CI 10 to 189) (Figure 1) and the composite of death or BPD (RR 0.74, 95% CI 0.58 to 0.94; typical risk difference −0.07; 95% CI −0.12 to −0.01; NNT 15; 95% CI 8 to 70) (Figure 2). When compared to INSURE therapy alone (3 trials, n=426), LISA also reduced the risk for death or BPD (RR 0.63, 95% CI 0.42 to 0.93; typical risk difference −0.09, 95% CI −0.16 to −0.015; NNT 12, 95% CI 6 to 66) but not BPD among survivors (RR 0.65, 95% CI 0.35 to 1.19, typical risk difference −0.04; 95% CI −0.10 to 0.02). Of note, one published RCT comparing LISA to INSURE (n=38) was excluded from this analysis owing to enrollment of moderate and extremely preterm infants (GA < 35 weeks). (80)Two meta-analyses inclusive of this RCT were recently reported. (81,82)
Figure 1.
Forrest plot for the outcome of BPD among survivors, comparing less invasive surfactant administration (LISA) versus control therapy in extremely preterm infants.
Figure 2.
Forrest plot for the outcome of death or BPD, comparing less invasive surfactant administration (LISA) versus control therapy in extremely preterm infants.
Isayama et al. recently reported a Bayesian random-effects network meta-analysis evaluating the efficacy of 6 early ventilation strategies (mechanical ventilation, nasal CPAP, non-invasive positive pressure ventilation, INSURE, LISA, and nebulized surfactant administered via LMA) for prevention of BPD in infants born less than 33 weeks gestation. (83) This approach allowed for simultaneous estimation of the relative effects of multiple interventions regardless of whether they were directly compared in individual trials. The study results indicated that LISA was associated with the largest reduction in the risk for death or BPD (OR 0.49; 95% Credible Interval 0.30–0.79) of any of the evaluated interventions. (83) However, the authors noted the findings were limited by the overall low quality of the available evidence. An ongoing trial (anticipated n=606 for a primary composite outcome of death or physiological BPD) comparing LISA to sham treatment in extremely preterm infants without a history of prior intubation will provide additional important data on this topic. (84)
6. Other strategies
Intratracheal budesonide
Yeh et al. recently randomized 265 VLBW infants with RDS who were mechanically ventilated in the first four hours of life to treatment with intratracheal surfactant versus intratracheal budesonide and surfactant. (85) Infants treated with budesonide and surfactant experienced a significant reduction in the outcome of death or BPD (any supplemental O2 requirement) at 36 weeks (42% vs. 66%, p<0.001). (85) Further, interleukin concentrations in tracheal aspirates were transiently lower among infants in the intervention arm, suggesting intratracheal budesonide may diminish BPD risk through local anti-inflammatory effects. (85)Notably, the effect size of this trial is rather large (number needed to treat, 4.1; 95% CI 2.8–7.8). (85) Thus, while these study results are promising, further large RCTs of intratracheal budesonide plus surfactant are needed before this therapy should be introduced into clinical practice.
Caffeine
In the Caffeine for Apnea of Prematurity (CAP) trial, over 2000 infants with birth weight 500 to 1250 grams were randomized to receive to caffeine or placebo within the first 10 days of life. (86) Infants randomized to caffeine experienced significantly less BPD than placebo infants, which was largely attributed to the fact that caffeine-treated infants received an average of 1 less week of positive pressure ventilation.
Caffeine is now a standard of care therapy in the respiratory management for preterm infants. Early initiation of caffeine is especially critical in the CPAP era, as more preterm infants are managed via non-invasive support immediately after birth and require a sustained respiratory drive to avoid intubation and mechanical ventilation. (87) A meta-analysis comprising both cohort studies and RCT demonstrated that early caffeine administration is association with a reduction in BPD, when compared with later administration. The timing of “early” caffeine administration varied from the first 2 hours after birth to the first three days after birth. (88)
Two small RCTs demonstrated that caffeine administration within the first minutes (89) to first 2 hours of life (90) is feasible and may improve short-term physiologic outcomes. (89,90) Neither trial was designed or powered to detect differences in BPD. While caffeine therapy should be administered early in the NICU to prevent BPD in preterm infants, there are insufficient RCT data to recommend immediate caffeine administration in the delivery room to prevent BPD.
Conclusions
Acute lung injury sustained in the immediate perinatal period directly contributes to the development of BPD in premature infants. Strategies to decrease lung injury and inflammation should begin prior to and continue following preterm delivery (Box). Initial stabilization of all infants at risk for RDS should begin with CPAP, reserving endotracheal intubation and surfactant administration for infants who fail non-invasive support. Prudent titration of supplemental oxygen in the delivery room is also recommended. Promising interventions that may further reduce BPD risk are currently under investigation and include sustained inflation and non-invasive surfactant administration.
Box. Summary of Evidence for Perinatal Interventions to Prevent BPD.
Continuous Positive Airway Pressure (CPAP) vs. Mechanical Ventilation
Evidence: Cochrane meta-analysis of 3 large RCTs (n=2,358) reporting outcome of BPD or death at 36 weeks PMA (32)
Results: Primary CPAP therapy compared with mechanical ventilation reduced the risk of BPD/death.
Treatment Effect: Relative Risk 0.89 (95% CI: 0.81–0.97)
Number Needed to Treat: 20 (95% CI: 11–100)
Sustained Inflation vs. Intermittent Positive Pressure Ventilation or CPAP
Evidence: Meta-analysis of 4 RCTs (n= 611 infants) comparing SI with IPPV or CPAP reporting the outcome of BPD or death at 36 weeks PMA (40)
Results: Neither SI or IPPV was superior to reduce the risk of BPD/death.
Treatment Effect: Relative Risk 0.92 (95% CI: 0.66–1.29)
Supplemental Oxygen during Delivery Room Resuscitation
Evidence: Meta-analysis of 10 RCTs (n=677 infants ≤32 weeks gestation) comparing low (≤30%) with high (≥60%) initial FiO2 for delivery room resuscitation reporting outcome of BPD (55)
Results: Neither approach to supplemental FiO2 was superior to reduce the risk of BPD
Treatment Effect: Relative Risk 1.11 (95% CI: 0.73–1.68)
Surfactant
INSURE vs. nasal CPAP
Evidence: Meta-analysis of 6 RCTs (n=1,250) reporting the outcome of BPD or death at 36 weeks PMA (71)
Results: Neither INSURE or nasal CPAP was superior to reduce the risk of BPD/death.
Treatment Effect: Relative Risk 0.88 (95% CI: 0.76–1.02)
Early (< 2hr of life) vs. Late (≥ 2hr of life) administration among infants receiving invasive mechanical ventilation
Evidence: Cochrane meta-analysis of 3 RCTs (n=3,050) reporting the outcome of BPD or death at 36 weeks PMA (64)
Results: Early compared with late surfactant reduced the risk of BPD/death.
Treatment Effect: Relative Risk 0.83 (95% CI: 0.75–0.91)
Number Needed to Treat: 16 (95% CI: 11–34)
Less Invasive Surfactant Administration (LISA) vs. all control therapies
Evidence: Meta-analysis of 5 RCTs (n=857) reporting the outcome of BPD or death at 36 weeks PMA (Figure 2)
Results: LISA compared with control therapy reduced the risk of BPD/death.
Treatment Effect: Relative Risk 0.74 (95% CI 0.58–0.94).
Number Needed to Treat: 15 (95% CI 8–70)
Less Invasive Surfactant Administration (LISA) vs. INSURE
Evidence: Meta-analysis of 3 RCTs (n=426) reporting the outcome of BPD or death at 36 weeks PMA (Figure 2)
Results: LISA compared with INSURE reduced the risk of BPD/death.
Treatment Effect: Relative Risk 0.63 (95% CI 0.42–0.93)
Number Needed to Treat: 12 (95% CI 6–66)
Acknowledgments
Funding: Dr. Foglia is supported by a Career Development Award, NICHD K23HD084727. No other funding sources supported this manuscript.
Abbreviations
- ACS
Antenatal corticosteroids
- BPD
bronchopulmonary dysplasia
- CI
confidence interval
- CPAP
continuous positive airway pressure
- ELBW
extremely low birth weight
- FRC
functional residual capacity
- GA
gestational age
- INSURE
intubation, surfactant administration, extubation
- IPPV
intermittent positive pressure ventilation
- LISA
less invasive surfactant administration
- NNT
number needed to treat
- PEEP
positive end expiratory pressure
- PMA
post-menstrual age
- OR
odds ratio
- RCT
randomized controlled trial
- RR
relative risk
- SI
sustained inflation
- VLBW
very low birth weight
Footnotes
Conflicts of Interest: Drs. Foglia and Kirpalani are investigators on the ongoing Sustained Aeration of Infant Lungs (SAIL) trial (clinicaltrials.gov Identifier NCT NCT02139800), which is referenced in this article. The authors have no other conflicts of interest to disclose
References
- 1.Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993–2012. JAMA. 2015;314:1039–51. doi: 10.1001/jama.2015.10244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Horbar JD, Carpenter JH, Badger GJ, Kenny MJ, Soll RF, Morrow KA, et al. Mortality and neonatal morbidity among infants 501 to 1500 grams from 2000 to 2009. Pediatrics. 2012;129:1019–26. doi: 10.1542/peds.2011-3028. [DOI] [PubMed] [Google Scholar]
- 3.Laughon MM, Langer JC, Bose CL, Smith PB, Ambalavanan N, Kennedy KA, et al. Prediction of bronchopulmonary dysplasia by postnatal age in extremely premature infants. Am J Respir Crit Care Med. 2011;183:1715–22. doi: 10.1164/rccm.201101-0055OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Klinger G, Sokolover N, Boyko V, Sirota L, Lerner-Geva L, Reichman B, et al. Perinatal risk factors for bronchopulmonary dysplasia in a national cohort of very-low-birthweight infants. Am J Obstet Gynecol. 2013;208:115, e1–9. doi: 10.1016/j.ajog.2012.11.026. [DOI] [PubMed] [Google Scholar]
- 5.Doyle LW, Faber B, Callanan C, Freezer N, Ford GW, Davis NM. Bronchopulmonary dysplasia in very low birth weight subjects and lung function in late adolescence. Pediatrics. 2006;118:108–13. doi: 10.1542/peds.2005-2522. [DOI] [PubMed] [Google Scholar]
- 6.Fawke J, Lum S, Kirkby J, Hennessy E, Marlow N, Rowell V, et al. Lung function and respiratory symptoms at 11 years in children born extremely preterm: The epicure study. Am J Respir Crit Care Med. 2010;182:237–45. doi: 10.1164/rccm.200912-1806OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sanchez-Solis M, Garcia-Marcos L, Bosch-Gimenez V, Pérez-Fernandez V, Pastor-Vivero MD, Mondéjar-Lopez P. Lung function among infants born preterm, with or without bronchopulmonary dysplasia. Pediatr Pulmonol. 2012;47:674–81. doi: 10.1002/ppul.21609. [DOI] [PubMed] [Google Scholar]
- 8.Vollsæter M, Røksund OD, Eide GE, Markestad T, Halvorsen T. Lung function after preterm birth: Development from mid-childhood to adulthood. Thorax. 2013;68:767–76. doi: 10.1136/thoraxjnl-2012-202980. [DOI] [PubMed] [Google Scholar]
- 9.Natarajan G, Pappas A, Shankaran S, Kendrick DE, Das A, Higgins RD, et al. Outcomes of extremely low birth weight infants with bronchopulmonary dysplasia: Impact of the physiologic definition. Early Hum Dev. 2012;88:509–15. doi: 10.1016/j.earlhumdev.2011.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang L-Y, Luo H-J, Hsieh W-S, Hsu C-H, Hsu H-C, Chen P-S, et al. Severity of bronchopulmonary dysplasia and increased risk of feeding desaturation and growth delay in very low birth weight preterm infants. Pediatr Pulmonol. 2010;45:165–73. doi: 10.1002/ppul.21171. [DOI] [PubMed] [Google Scholar]
- 11.Schmidt B, Asztalos EV, Roberts RS, Robertson CMT, Sauve RS, Whitfield MF, et al. Impact of bronchopulmonary dysplasia, brain injury, and severe retinopathy on the outcome of extremely low-birth-weight infants at 18 months: Results from the trial of indomethacin prophylaxis in preterms. JAMA. 2003;289:1124–9. doi: 10.1001/jama.289.9.1124. [DOI] [PubMed] [Google Scholar]
- 12.Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA, et al. Validation of the national institutes of health consensus definition of bronchopulmonary dysplasia. Pediatrics. 2005;116:1353–60. doi: 10.1542/peds.2005-0249. [DOI] [PubMed] [Google Scholar]
- 13.Short EJ, Klein NK, Lewis BA, Fulton S, Eisengart S, Kercsmar C, et al. Cognitive and academic consequences of bronchopulmonary dysplasia and very low birth weight: 8-Year-Old outcomes. Pediatrics. 2003;112:e359. doi: 10.1542/peds.112.5.e359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Björklund LJ, Ingimarsson J, Curstedt T, John J, Robertson B, Werner O, Vilstrup CT. Manual ventilation with a few large breaths at birth compromises the therapeutic effect of subsequent surfactant replacement in immature lambs. Pediatr Res. 1997;42:348–55. doi: 10.1203/00006450-199709000-00016. [DOI] [PubMed] [Google Scholar]
- 15.Hillman NH, Moss TJM, Kallapur SG, Bachurski C, Pillow JJ, Polglase GR, et al. Brief, large tidal volume ventilation initiates lung injury and a systemic response in fetal sheep. Am J Respir Crit Care Med. 2007;176:575–81. doi: 10.1164/rccm.200701-051OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Albertine KH, Jones GP, Starcher BC, Bohnsack JF, Davis PL, Cho SC, et al. Chronic lung injury in preterm lambs. Disordered respiratory tract development. Am J Respir Crit Care Med. 1999;159:945–58. doi: 10.1164/ajrccm.159.3.9804027. [DOI] [PubMed] [Google Scholar]
- 17.Wallace MJ, Probyn ME, Zahra VA, Crossley K, Cole TJ, Davis PG, et al. Early biomarkers and potential mediators of ventilation-induced lung injury in very preterm lambs. Respir Res. 2009;10:19. doi: 10.1186/1465-9921-10-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heldt GP, McIlroy MB. Distortion of chest wall and work of diaphragm in preterm infants. J Appl Physiol (1985) 1987;62:164–9. doi: 10.1152/jappl.1987.62.1.164. [DOI] [PubMed] [Google Scholar]
- 19.Heldt GP, McIlroy MB. Dynamics of chest wall in preterm infants. J Appl Physiol (1985) 1987;62:170–4. doi: 10.1152/jappl.1987.62.1.170. [DOI] [PubMed] [Google Scholar]
- 20.Barker PM, Gowen CW, Lawson EE, Knowles MR. Decreased sodium ion absorption across nasal epithelium of very premature infants with respiratory distress syndrome. J Pediatr. 1997;130:373–7. doi: 10.1016/s0022-3476(97)70198-7. [DOI] [PubMed] [Google Scholar]
- 21.Obladen M. Factors influencing surfactant composition in the newborn infant. Eur J Pediatr. 1978;128:129–43. doi: 10.1007/BF00444298. [DOI] [PubMed] [Google Scholar]
- 22.Jensen EA, Foglia EE, Schmidt B. Evidence-Based pharmacologic therapies for prevention of bronchopulmonary dysplasia: Application of the grading of recommendations assessment, development, and evaluation methodology. Clin Perinatol. 2015;42:755–79. doi: 10.1016/j.clp.2015.08.005. [DOI] [PubMed] [Google Scholar]
- 23.Shinwell ES, Portnov I, Meerpohl JJ, Karen T, Bassler D. Inhaled corticosteroids for bronchopulmonary dysplasia: A meta-analysis. Pediatrics. 2016;138:e20162511. doi: 10.1542/peds.2016-2511. [DOI] [PubMed] [Google Scholar]
- 24.Lemyre B, Laughon M, Bose C, Davis PG. Early nasal intermittent positive pressure ventilation (NIPPV) versus early nasal continuous positive airway pressure (NCPAP) for preterm infants. Cochrane Database Syst Rev. 2016;12:CD005384. doi: 10.1002/14651858.CD005384.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Avery ME, Tooley WH, Keller JB, Hurd SS, Bryan MH, Cotton RB, et al. Is chronic lung disease in low birth weight infants preventable? A survey of eight centers. Pediatrics. 1987;79:26–30. [PubMed] [Google Scholar]
- 26.Lindner W, Vossbeck S, Hummler H, Pohlandt F. Delivery room management of extremely low birth weight infants: Spontaneous breathing or intubation? Pediatrics. 1999;103:961–7. doi: 10.1542/peds.103.5.961. [DOI] [PubMed] [Google Scholar]
- 27.Morley CJ, Davis PG, Doyle LW, Brion LP, Hascoet JM, Carlin JB, et al. Nasal CPAP or intubation at birth for very preterm infants. N Engl J Med. 2008;358:700–8. doi: 10.1056/NEJMoa072788. [DOI] [PubMed] [Google Scholar]
- 28.Finer NN, Carlo WA, Walsh MC, Rich W, Gantz MG, Laptook AR, et al. Early CPAP versus surfactant in extremely preterm infants. N Engl J Med. 2010;362:1970–9. doi: 10.1056/NEJMoa0911783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dunn MS, Kaempf J, de Klerk A, de Klerk R, Reilly M, Howard D, et al. Randomized trial comparing 3 approaches to the initial respiratory management of preterm neonates. Pediatrics. 2011;128:e1069–76. doi: 10.1542/peds.2010-3848. [DOI] [PubMed] [Google Scholar]
- 30.Fischer HS, Bührer C. Avoiding endotracheal ventilation to prevent bronchopulmonary dysplasia: A meta-analysis. Pediatrics. 2013;132:e1351–60. doi: 10.1542/peds.2013-1880. [DOI] [PubMed] [Google Scholar]
- 31.Schmolzer M, Kumar M, Pichler G, Aziz K, O’Reilly M, Cheung Y. Non-invasive versus invasive respiratory support in preterm infants at birth: Systematic review and meta-analysis. BMJ. 2013;347:f5980. doi: 10.1136/bmj.f5980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Subramaniam P, Ho JJ, Davis PG. Prophylactic nasal continuous positive airway pressure for preventing morbidity and mortality in very preterm infants. Cochrane Database Syst Rev. 2016;6:CD001243. doi: 10.1002/14651858.CD001243.pub3. [DOI] [PubMed] [Google Scholar]
- 33.COMMITTEE ON FETUS AND NEWBORN. Respiratory support in preterm infants at birth. Pediatrics. 2014;133:171–4. doi: 10.1542/peds.2013-3442. [DOI] [PubMed] [Google Scholar]
- 34.Vyas H, Milner AD, Hopkin IE, Boon AW. Physiologic responses to prolonged and slow-rise inflation in the resuscitation of the asphyxiated newborn infant. J Pediatr. 1981;99:635–9. doi: 10.1016/s0022-3476(81)80279-x. [DOI] [PubMed] [Google Scholar]
- 35.Harling AE, Beresford MW, Vince GS, Bates M, Yoxall CW. Does sustained lung inflation at resuscitation reduce lung injury in the preterm infant? Arch Dis Child Fetal Neonatal Ed. 2005;90:F406–10. doi: 10.1136/adc.2004.059303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lindner W, Högel J, Pohlandt F. Sustained pressure—controlled inflation or intermittent mandatory ventilation in preterm infants in the delivery room? A randomized, controlled trial on initial respiratory support via nasopharyngeal tube. Acta Paediatr. 2005;94:303–9. doi: 10.1111/j.1651-2227.2005.tb18431.x. [DOI] [PubMed] [Google Scholar]
- 37.te Pas AB, Walther FJ. A randomized, controlled trial of delivery-room respiratory management in very preterm infants. Pediatrics. 2007;120:322–9. doi: 10.1542/peds.2007-0114. [DOI] [PubMed] [Google Scholar]
- 38.Lista G, Boni L, Scopesi F, Mosca F, Trevisanuto D, Messner H, et al. Sustained lung inflation at birth for preterm infants: A randomized clinical trial. Pediatrics. 2015;135:e457–64. doi: 10.1542/peds.2014-1692. [DOI] [PubMed] [Google Scholar]
- 39.Jiravisitkul P, Rattanasiri S, Nuntnarumit P. Randomised controlled trial of sustained lung inflation for resuscitation of preterm infants in the delivery room. Resuscitation. 2017;111:68–73. doi: 10.1016/j.resuscitation.2016.12.003. [DOI] [PubMed] [Google Scholar]
- 40.Schmölzer GM, Kumar M, Aziz K, Pichler G, O’Reilly M, Lista G, Cheung P. Sustained inflation versus positive pressure ventilation at birth: A systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2014;100:F361–8. doi: 10.1136/archdischild-2014-306836. [DOI] [PubMed] [Google Scholar]
- 41.Foglia EE, Owen LS, Thio M, Ratcliffe SJ, Lista G, Te Pas A, et al. Sustained aeration of infant lungs (SAIL) trial: Study protocol for a randomized controlled trial. Trials. 2015;16:95. doi: 10.1186/s13063-015-0601-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Assessment of Lung Aeration at Birth. [Accessed March 31, 2017];Clinicaltrials.Gov Identifier NCT01739114. at: https://clinicaltrials.gov/ct2/show/NCT01739114?term=assessment+lung+aeration&rank=3.
- 43.Dawson JA, Kamlin CO, Vento M, Wong C, Cole TJ, Donath SM, et al. Defining the reference range for oxygen saturation for infants after birth. Pediatrics. 2010;125:e1340–7. doi: 10.1542/peds.2009-1510. [DOI] [PubMed] [Google Scholar]
- 44.Vento M, Cubells E, Escobar JJ, Escrig R, Aguar M, Brugada M, et al. Oxygen saturation after birth in preterm infants treated with continuous positive airway pressure and air: Assessment of gender differences and comparison with a published nomogram. Arch Dis Child Fetal Neonatal Ed. 2013;98:F228–32. doi: 10.1136/archdischild-2012-302369. [DOI] [PubMed] [Google Scholar]
- 45.Mian QN, Pichler G, Binder C, O’Reilly M, Aziz K, Urlesberger B, et al. Tidal volumes in spontaneously breathing preterm infants supported with continuous positive airway pressure. J Pediatr. 2014;165:702–706. doi: 10.1016/j.jpeds.2014.06.047. [DOI] [PubMed] [Google Scholar]
- 46.Lundstrom E, Pryds O, Greisen G. Oxygen at birth and prolonged cerebral vasoconstriction in preterm infants. Arch Dis Child Fetal Neonatal Ed. 1995;73:F81–6. doi: 10.1136/fn.73.2.f81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Harling AE, Beresford MW, Vince GS, Bates M, Yoxall CW. Does the use of 50% oxygen at birth in preterm infants reduce lung injury? Arch Dis Child Fetal Neonatal Ed. 2005;90:F401–5. doi: 10.1136/adc.2004.059287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang CL, Anderson C, Leone TA, Rich W, Govindaswami B, Finer NN. Resuscitation of preterm neonates by using room air or 100% oxygen. Pediatrics. 2008;121:1083–9. doi: 10.1542/peds.2007-1460. [DOI] [PubMed] [Google Scholar]
- 49.Vento M, Moro M, Escrig R, Arruza L, Villar G, Izquierdo I, et al. Preterm resuscitation with low oxygen causes less oxidative stress, inflammation, and chronic lung disease. Pediatrics. 2009;124:e439–49. doi: 10.1542/peds.2009-0434. [DOI] [PubMed] [Google Scholar]
- 50.Rabi Y, Singhal N, Nettel-Aguirre A. Room-air versus oxygen administration for resuscitation of preterm infants: The ROAR study. Pediatrics. 2011;128:e374–81. doi: 10.1542/peds.2010-3130. [DOI] [PubMed] [Google Scholar]
- 51.Armanian AM, Badiee Z. Resuscitation of preterm newborns with low concentration oxygen versus high concentration oxygen. J Res Pharm Pract. 2012;1:25–9. doi: 10.4103/2279-042X.99674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kapadia VS, Chalak LF, Sparks JE, Allen JR, Savani RC, Wyckoff MH. Resuscitation of preterm neonates with limited versus high oxygen strategy. Pediatrics. 2013;132:e1488–96. doi: 10.1542/peds.2013-0978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rook D, Schierbeek H, Vento M, Vlaardingerbroek H, van der Eijk AC, Longini M, et al. Resuscitation of preterm infants with different inspired oxygen fractions. J Pediatr. 2014;164:1322–6. doi: 10.1016/j.jpeds.2014.02.019. [DOI] [PubMed] [Google Scholar]
- 54.Oei JL, Saugstad OD, Lui K, Wright IM, Smyth JP, Craven P, et al. Targeted oxygen in the resuscitation of preterm infants, a randomized clinical trial. Pediatrics. 2017;139:e20161452. doi: 10.1542/peds.2016-1452. [DOI] [PubMed] [Google Scholar]
- 55.Saugstad OD, Aune D, Aguar M, Kapadia V, Finer N, Vento M. Systematic review and meta-analysis of optimal initial fraction of oxygen levels in the delivery room at ≤32 weeks. Acta Paediatr. 2014;103:744–51. doi: 10.1111/apa.12656. [DOI] [PubMed] [Google Scholar]
- 56.Oei JL, Vento M, Rabi Y, Wright I, Finer N, Rich W, et al. Higher or lower oxygen for delivery room resuscitation of preterm infants below 28 completed weeks gestation: A meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2017;102:F24–30. doi: 10.1136/archdischild-2016-310435. [DOI] [PubMed] [Google Scholar]
- 57.Rabi Y, Lodha A, Soraisham A, Singhal N, Barrington K, Shah PS. Outcomes of preterm infants following the introduction of room air resuscitation. Resuscitation. 2015;96:252–9. doi: 10.1016/j.resuscitation.2015.08.012. [DOI] [PubMed] [Google Scholar]
- 58.Guyatt GH, Briel M, Glasziou P, Bassler D, Montori VM. Problems of stopping trials early. BMJ. 2012;344:e3863. doi: 10.1136/bmj.e3863. [DOI] [PubMed] [Google Scholar]
- 59.Perlman JM, Wyllie J, Kattwinkel J, Wyckoff MH, Aziz K, Guinsburg R, et al. Part 7: Neonatal resuscitation: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2015;132:S204–41. doi: 10.1161/CIR.0000000000000276. [DOI] [PubMed] [Google Scholar]
- 60.Study of room air versus 60% oxygen for resuscitation of premature infants (PRESOX) [Accessed March 31, 2017];Clinicaltrials.gov Identifier NCT01773746. at: https://clinicaltrials.gov/ct2/show/NCT01773746?term=presox&rank=1.
- 61.Soll RF. Prophylactic natural surfactant extract for preventing morbidity and mortality in preterm infants. Cochrane Database Syst Rev. 2000;2:CD000511. doi: 10.1002/14651858.CD000511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Soll RF. Prophylactic synthetic surfactant for preventing morbidity and mortality in preterm infants. Cochrane Database Syst Rev. 2000;2:CD001079. doi: 10.1002/14651858.CD001079. [DOI] [PubMed] [Google Scholar]
- 63.Soll RF. Synthetic surfactant for respiratory distress syndrome in preterm infants. Cochrane Database Syst Rev. 2000;2:CD001149. doi: 10.1002/14651858.CD001149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bahadue FL, Soll R. Early versus delayed selective surfactant treatment for neonatal respiratory distress syndrome. Cochrane Database Syst Rev. 2012;11:CD001456. doi: 10.1002/14651858.CD001456.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ardell S, Pfister RH, Soll R. Animal derived surfactant extract versus protein free synthetic surfactant for the prevention and treatment of respiratory distress syndrome. Cochrane Database Syst Rev. 2015;5:CD000144. doi: 10.1002/14651858.CD000144.pub2. [DOI] [PubMed] [Google Scholar]
- 66.Singh N, Halliday HL, Stevens TP, Suresh G, Soll R, Rojas-Reyes MX. Comparison of animal-derived surfactants for the prevention and treatment of respiratory distress syndrome in preterm infants. Cochrane Database Syst Rev. 2015;12:CD010249. doi: 10.1002/14651858.CD010249.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Moya F, Sinha S, Gadzinowski J, D’Agostino R, Segal R, Guardia C, et al. One-year follow-up of very preterm infants who received lucinactant for prevention of respiratory distress syndrome: Results from 2 multicenter randomized, controlled trials. Pediatrics. 2007;119:e1361–70. doi: 10.1542/peds.2006-0149. [DOI] [PubMed] [Google Scholar]
- 68.Sinha SK, Lacaze-Masmonteil T, Valls i Soler A, Wiswell TE, Gadzinowski J, Hajdu J, et al. A multicenter, randomized, controlled trial of lucinactant versus poractant alfa among very premature infants at high risk for respiratory distress syndrome. Pediatrics. 2005;115:1030–8. doi: 10.1542/peds.2004-2231. [DOI] [PubMed] [Google Scholar]
- 69.Victorin LH, Deverajan LV, Curstedt T, Robertson B. Surfactant replacement in spontaneously breathing babies with hyaline membrane disease - a pilot study. Biol Neonate. 1990;58:121–6. doi: 10.1159/000243250. [DOI] [PubMed] [Google Scholar]
- 70.Stevens TP, Harrington EW, Blennow M, Soll RF. Early surfactant administration with brief ventilation vs. Selective surfactant and continued mechanical ventilation for preterm infants with or at risk for respiratory distress syndrome. Cochrane Database Syst Rev. 2007;4:CD003063. doi: 10.1002/14651858.CD003063.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Isayama T, Chai-Adisaksopha C, McDonald SD. Noninvasive ventilation with vs without early surfactant to prevent chronic lung disease in preterm infants: A systematic review and meta-analysis. JAMA Pediatr. 2015;169:731–9. doi: 10.1001/jamapediatrics.2015.0510. [DOI] [PubMed] [Google Scholar]
- 72.More K, Sakhuja P, Shah PS. Minimally invasive surfactant administration in preterm infants: A meta-narrative review. JAMA Pediatr. 2014;168:901–8. doi: 10.1001/jamapediatrics.2014.1148. [DOI] [PubMed] [Google Scholar]
- 73.Verder H, Robertson B, Greisen G, Ebbesen F, Albertsen P, Lundstrøm K, et al. Surfactant therapy and nasal continuous positive airway pressure for newborns with respiratory distress syndrome. Danish-Swedish multicenter study group. N Engl J Med. 1994;331:1051–5. doi: 10.1056/NEJM199410203311603. [DOI] [PubMed] [Google Scholar]
- 74.Göpel W, Kribs A, Härtel C, Avenarius S, Teig N, Groneck P, et al. Less invasive surfactant administration is associated with improved pulmonary outcomes in spontaneously breathing preterm infants. Acta Paediatr. 2015;104:241–6. doi: 10.1111/apa.12883. [DOI] [PubMed] [Google Scholar]
- 75.Mirnia K, Heidarzadeh M, Hosseini MB, Sadeghnia A, Balila M, Ghojazadeh M. Comparison outcome of surfactant administration via tracheal catheterization during spontaneous breathing with insure. Medical Journal of Islamic World Academy of Sciences. 2013;21:143–8. [Google Scholar]
- 76.Kanmaz HG, Erdeve O, Canpolat FE, Mutlu B, Dilmen U. Surfactant administration via thin catheter during spontaneous breathing: Randomized controlled trial. Pediatrics. 2013;131:e502–9. doi: 10.1542/peds.2012-0603. [DOI] [PubMed] [Google Scholar]
- 77.Kribs A, Roll C, Göpel W, Wieg C, Groneck P, Laux R, et al. Nonintubated surfactant application vs conventional therapy in extremely preterm infants: A randomized clinical trial. JAMA Pediatr. 2015;169:723–30. doi: 10.1001/jamapediatrics.2015.0504. [DOI] [PubMed] [Google Scholar]
- 78.Bao Y, Zhang G, Wu M, Ma L, Zhu J. A pilot study of less invasive surfactant administration in very preterm infants in a chinese tertiary center. BMC Pediatr. 2015;15:342. doi: 10.1186/s12887-015-0342-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Göpel W, Kribs A, Ziegler A, Laux R, Hoehn T, Wieg C, et al. Avoidance of mechanical ventilation by surfactant treatment of spontaneously breathing preterm infants (AMV): An open-label, randomised, controlled trial. Lancet. 2011;378:1627–34. doi: 10.1016/S0140-6736(11)60986-0. [DOI] [PubMed] [Google Scholar]
- 80.Mohammadizadeh M, Ardestani AG, Sadeghnia AR. Early administration of surfactant via a thin intratracheal catheter in preterm infants with respiratory distress syndrome: Feasibility and outcome. J Res Pharm Pract. 2015;4:31–6. doi: 10.4103/2279-042X.150053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rigo V, Lefebvre C, Broux I. Surfactant instillation in spontaneously breathing preterm infants: A systematic review and meta-analysis. Eur J Pediatr. 2016;175:1933–42. doi: 10.1007/s00431-016-2789-4. [DOI] [PubMed] [Google Scholar]
- 82.Aldana-Aguirre JC, Pinto M, Featherstone RM, Kumar M. Less invasive surfactant administration versus intubation for surfactant delivery in preterm infants with respiratory distress syndrome: A systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2017;102:F17–23. doi: 10.1136/archdischild-2015-310299. [DOI] [PubMed] [Google Scholar]
- 83.Isayama T, Iwami H, McDonald S, Beyene J. Association of noninvasive ventilation strategies with mortality and bronchopulmonary dysplasia among preterm infants: A systematic review and meta-analysis. JAMA. 2016;316:611–24. doi: 10.1001/jama.2016.10708. [DOI] [PubMed] [Google Scholar]
- 84.Dargaville PA, Kamlin CO, De Paoli AG, Carlin JB, Orsini F, Soll RF, et al. The OPTIMIST-A trial: Evaluation of minimally-invasive surfactant therapy in preterm infants 25–28 weeks gestation. BMC Pediatr. 2014;14:213. doi: 10.1186/1471-2431-14-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Yeh TF, Chen CM, Wu SY, Husan Z, Li TC, Hsieh WS, et al. Intratracheal administration of budesonide/surfactant to prevent bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2016;193:86–95. doi: 10.1164/rccm.201505-0861OC. [DOI] [PubMed] [Google Scholar]
- 86.Schmidt B, Roberts RS, Davis P, Doyle LW, Barrington KJ, Ohlsson A, et al. Caffeine therapy for apnea of prematurity. N Engl J Med. 2006;354:2112–21. doi: 10.1056/NEJMoa054065. [DOI] [PubMed] [Google Scholar]
- 87.Kribs A, Hummler H. Ancillary therapies to enhance success of non-invasive modes of respiratory support - approaches to delivery room use of surfactant and caffeine? Semin Fetal Neonatal Med. 2016;21:212–8. doi: 10.1016/j.siny.2016.02.011. [DOI] [PubMed] [Google Scholar]
- 88.Kua KP, Lee SW. Systematic review and meta-analysis of clinical outcomes of early caffeine therapy in preterm neonates. Br J Clin Pharmacol. 2017;83:180–91. doi: 10.1111/bcp.13089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Dekker J, Hooper SB, van Vonderen JJ, Witlox R, Lopriore E, te Pas AB. Caffeine to improve breathing effort of preterm infants at birth; a randomized controlled trial. Pediatr Res. doi: 10.1038/pr.2017.45. e-pub ahead of print 13 March 2017. [DOI] [PubMed] [Google Scholar]
- 90.Sauberan J, Akotia D, Rich W, Durham J, Finer N, Katheria A. A pilot randomized controlled trial of early versus routine caffeine in extremely premature infants. Am J Perinatol. 2015;32:879–86. doi: 10.1055/s-0034-1543981. [DOI] [PubMed] [Google Scholar]
- 91.Tataranno ML, Oei JL, Perrone S, Wright IM, Smyth JP, Lui K, et al. Resuscitating preterm infants with 100% oxygen is associated with higher oxidative stress than room air. Acta Paediatr. 2015;104:759–65. doi: 10.1111/apa.13039. [DOI] [PubMed] [Google Scholar]