Abstract
Objectives
Researchers documenting persistent racial/ethnic and socioeconomic status disparities in chances of cesarean delivery have speculated that women’s birth attitudes and preferences may partially explain these differences, but no studies have directly tested this hypothesis. We examined whether women’s prenatal attitudes toward vaginal delivery differed by race/ethnicity or socioeconomic status, and whether attitudes were differently related to delivery mode depending on race/ethnicity or socioeconomic status.
Methods
Data were from the First Baby Study, a cohort of 3,006 women who gave birth to a first baby in Pennsylvania between 2009 and 2011. We used regression models to examine 1) predictors of prenatal attitudes toward vaginal delivery, and 2) the association between prenatal attitudes and actual delivery mode. To assess moderation, we estimated models adding interaction terms.
Results
Prenatal attitudes toward vaginal delivery were not associated with race/ethnicity or socioeconomic status. Positive attitudes toward vaginal delivery were associated with lower odds of cesarean delivery (AOR=0.60, p<0.001). However, vaginal delivery attitudes were only related to delivery mode among women who were white, highly educated, and privately insured.
Conclusions
There are racial/ethnic differences in chances of cesarean delivery, and these differences are not explained by birth attitudes. Furthermore, our findings suggest that white and high- socioeconomic status women may be more able to realize their preferences in childbirth.
Keywords: cesarean delivery, birth attitudes, maternity care, health disparities, race
Introduction
Thirty-two percent of the nearly 4 million U.S. women that give birth each year deliver by cesarean,1 and chances of delivering by cesarean vary by race/ethnicity and socioeconomic status. Even after accounting for a variety of risk factors (e.g. age and medical conditions), black women, and in some studies Latina women, have a higher risk of delivering by cesarean compared to white women.2–5 Lower-socioeconomic status women may also be at higher risk of cesarean delivery compared to their higher-socioeconomic status counterparts,6 although this has been less frequently explored in the U.S. Despite the well-documented nature of racial/ethnic disparities in cesarean delivery, the mechanisms driving them remain poorly understood. Some researchers have suggested that women’s birth attitudes and preferences may vary by race/ethnicity and socioeconomic status, and that this may be one reason for disparities in cesarean delivery.4,5,7,8 However, this possibility has not been directly examined.
As the cesarean rate rose to nearly one-third of births in the 2000s, researchers and physicians hypothesized that this was because women increasingly preferred to give birth by cesarean.9 Subsequent studies examining the idea of “maternal request” cesarean have shown that, while a small minority of U.S. women (2.5% or less) do prefer to give birth by cesarean, these numbers are small and do not explain the rise in the cesarean rate.10 Maternal request cesarean can be conceptualized as one end of a spectrum of attitudes toward birth mode.11 Most women report that they would prefer to deliver vaginally, but one U.S. study has shown that strength of preference for vaginal delivery predicts actual birth mode.12 This adds to the evidence that cesarean deliveries do not occur due to medical risk alone; there is wide variation across hospitals in cesarean delivery rates that is not explained by medical conditions.13
Rather, patterns of cesarean delivery are driven by a complex interplay of factors including hospital environment and culture, clinician practice patterns, patient-clinician communication, and women’s preferences and attitudes. These non-medical factors may be particularly relevant for cesarean indications that have lower diagnostic accuracy and may be more subject to the interpretation of the clinician.10,14 Indeed, these indications, which include nonreassuring fetal heart tracing and labor arrest, comprise a large proportion of primary cesarean deliveries.15
Even if women’s preferences and attitudes related to childbirth and delivery mode are shaped by race and socioeconomic status, people in less privileged social positions may be less able to enact their preferences, including in childbirth.6 Power dynamics within the clinician-patient relationship and patient-clinician communication may play an important role. Power—the ‘ability to do or act’, is an inescapable aspect of all social relationships and an important consideration in the clinician-patient relationship.16 Shared decision making and enhanced autonomy models of care encourage patients and clinicians to actively share power. While shared power has become the norm in many clinical practices, the unequal power dynamic between a clinician and a patient persists in some cases.17 Unbalanced power dynamics may be even more salient for women from marginalized social positions who may have less agency and be more heavily impacted by structural and interpersonal racism when accessing the health care system. Other work suggests that vestiges of a health care system built on creating a power dynamic that allowed for inequitable treatment by race is still a part of the underlying and unconscious values and norms of health care delivery systems and can strongly influence a patient’s ability to feel empowered.18
In healthcare settings, race/ethnicity and socioeconomic status can impact the quality of patient-clinician interaction.19 Racial/ethnic minority patients and low-socioeconomic status patients are less likely to experience patient-centered communication and shared decision-making in clinical encounters, and more likely to perceive that they are being discriminated against.20–22 Clinician bias, or the implicit attitudes of clinicians toward different sociodemographic groups, can affect patient-clinician interactions, including both interpersonal behavior and diagnostic and treatment decisions.23 To our knowledge, implicit bias among maternity care providers has not been specifically examined; however, there is a body of literature that demonstrates its relevance in other areas of health care delivery. For example, previous work has found that physicians have an implicit preference for white Americans and implicit beliefs that blacks are less cooperative with medical procedures.24 If this phenomenon were to carry over to maternity care, it is possible that women of color with specific attitudes around cesarean delivery may be viewed as less cooperative by their clinician.
In this study, we examined whether women’s prenatal attitudes toward delivery mode varied by social position (race/ethnicity and socioeconomic status), using data from a cohort of 3,000 first time mothers. We also investigated whether women’s prenatal attitudes toward delivery mode explained race/ethnicity and socioeconomic status differences in chances of cesarean delivery (mediation), or whether attitudes were differently related to cesarean delivery depending on race/ethnicity or socioeconomic status (moderation).
Methods
Data
Data are from the First Baby Study, a cohort of 3,006 women who gave birth to their first baby in a Pennsylvania hospital in 2009–2011. Women were recruited into the study through a variety of methods. Participants completed a baseline interview during the third trimester of pregnancy and a second interview about 1 month after the birth, and were followed for 36 months after the birth. Interview responses were linked to birth certificate and hospital discharge data. Study participants gave birth across 76 different Pennsylvania hospitals, although most gave birth at one of seven hospitals in Central and Western Pennsylvania. The primary purpose of the First Baby Study was to assess the relationship between cesarean delivery and subsequent childbearing; details of the study population have been previously described.25 Measures for the present study are drawn from the baseline and 1-month interviews, as well as linked birth certificate and hospital discharge data.
Measures
The measure of women’s prenatal attitudes toward vaginal delivery consisted of 10 items in the baseline interview assessing attitudes toward vaginal and cesarean delivery. Women could agree or disagree with each statement on a 5-point Likert scale. Items included statements such as, “I would be very happy if I could have my baby vaginally,” and, “I would prefer to have my baby by cesarean section so that I do not have to go through labor.” Scores for the items were added together, divided by the number of items, and some items reversed, so that the resulting scale also had a theoretical range of 1–5, with higher scores representing a more positive attitude toward vaginal delivery. Scale scores ranged from 1.4 to 5, and Cronbach’s alpha was 0.85, indicating good internal validity.
Women reported whether they delivered vaginally or by cesarean. Women who delivered by cesarean were asked, “Did you have a planned cesarean section that was scheduled to occur before you went into labor, that is before regular contractions began, or did you have an unplanned cesarean section delivery?” We used these responses to categorize cesarean deliveries as planned or unplanned.
Other key variables were race/ethnicity, and two measures of socioeconomic status: education level and insurance type (private or Medicaid), since eligibility for Medicaid is based on income level. Race/ethnicity was categorized as white (reference), black, Latina, or other. Education was categorized as high school degree or less (reference), some college, and Bachelor’s degree or higher. About three-quarters of women in the cohort had private insurance and few were uninsured, so insurance was a dichotomous measure of whether the woman had private insurance (reference) or not.
In addition to race/ethnicity and socioeconomic status, we examined the following variables as potential predictors of delivery mode preference: age (18–24, 25–30, 31–35), rurality (rural zip code of residence or not), partnership status (married and living together, not married but living with partner, or other), nativity (foreign- or U.S.-born), chronic or pregnancy-induced hypertension, pre-existing or gestational diabetes, pre-pregnancy obesity, and fear of childbirth. Fear of childbirth was an ordinal variable based on responses to a question on the baseline interview, “to what extent do you feel fearful about your upcoming delivery?” Response choices were: extremely (5), quite a bit (4), moderately (3), a little bit (2), or not at all (1). Cesarean models also included the baby’s gestational age at birth (less than 37 weeks, 37–38 weeks, 39–40 weeks, 41+ weeks).
Analysis
We first examined whether women’s attitudes toward cesarean varied by race/ethnicity and socioeconomic status. We then used multivariate linear regression to investigate the independent association of race/ethnicity and socioeconomic status with women’s attitudes toward vaginal delivery, controlling for covariates.
Next, we used multivariate logistic regression models to examine the association between women’s prenatal attitudes toward vaginal delivery and actual delivery mode (vaginal or cesarean). We also estimated a multinomial logit model to examine the association between prenatal attitudes toward vaginal delivery and planned or unplanned cesarean delivery, compared to vaginal delivery.
To test whether attitudes toward vaginal delivery mediated, or explained, racial/ethnic and socioeconomic status differences in delivery mode, we used Karlson-Holm-Breen models to formally test whether coefficients were different in models including or excluding vaginal delivery attitudes.26 Finally, to assess whether the relationship between vaginal delivery attitudes and delivery mode varied by race/ethnicity or socioeconomic status (i.e. moderation), we estimated models including interactions between race/ethnicity, education, insurance type, and vaginal delivery attitudes. For each interaction, we computed average marginal effects and predicted probabilities. The vast majority of cesarean deliveries among women in the cohort were unplanned, and we therefore did not have the sample size to examine planned cesarean in the interaction analyses.
In models with cesarean delivery outcomes, we used clustered standard errors to account for correlation among women giving birth at the same hospital. All analyses were conducted in Stata 14.
The First Baby Study was approved by the Penn State College of Medicine Institutional Review Board (IRB) and by the IRBs of participating hospitals. The present study used de-identified existing records, and was determined to be exempt by the University of Minnesota IRB.
Results
Characteristics of the First Baby Study cohort are presented in Table 1. About 84% of women in the sample were white, while 7% were black and 5% were Latina. Nearly 23% had some graduate education, and three-quarters were privately insured. The mean score on the attitude toward vaginal birth scale was 4.3, indicating favorable attitudes toward vaginal birth, given that the maximum scale score was 5. Attitudes toward vaginal birth were not associated with race/ethnicity or insurance type in bivariate or multivariate models (Table 2). In bivariate analyses, women with some college had more favorable attitudes toward vaginal birth compared to women in both the lowest and highest education categories. After controlling for other characteristics, the relationship between education and attitudes toward delivery mode was no longer statistically significant.
Table 1.
Characteristics of First Baby Study respondents, Pennsylvania, 2009–2011.
| Characteristic | Respondents (N=2,939) n (%) |
|---|---|
| Race/ethnicity | |
| White | 2462 (83.8) |
| Black | 208 (7.1) |
| Latina | 156 (5.3) |
| Other | 113 (3.84) |
| Education | |
| High school or less | 477 (16.2) |
| Some college | 780 (26.5) |
| Bachelor’s degree or higher | 1682 (57.2) |
| Insurance type | |
| Private | 2244 (76.4) |
| No private coverage | 695 (23.6) |
| Age category | |
| 18–24 | 777 (26.4) |
| 25–30 | 1442 (29.1) |
| 31+ | 720 (24.5) |
| Rurality | |
| Not rural | 2693 (91.6) |
| Lives in rural zip code | 246 (8.4) |
| Partnership status | |
| Married and living together | 2092 (71.2) |
| Not married but living with partner | 510 (17.3) |
| Other | 337 (11.5) |
| Diabetes (pre-pregnancy or gestational) | 195 (6.6) |
| Hypertension (pre-pregnancy or gestational) | 209 (7.1) |
| Pre-pregnancy obesity | 601 (20.5) |
| Foreign born | 174 (5.9) |
| Fearful of childbirth | |
| Not at all | 403 (13.7) |
| A little bit | 1055 (35.9) |
| Moderately | 875 (29.8) |
| Quite a bit | 358 (12.2) |
| Extremely | 248 (8.4) |
| Prenatal attitude toward vaginal delivery (mean [SD])a | 4.3 [0.47] |
| Delivery mode | |
| Vaginal | 2099 (71.4) |
| Planned cesarean | 152 (5.2) |
| Unplanned cesarean | 688 (23.4) |
Range 1–5, with higher scores indicating more positive attitude toward vaginal birth.
Table 2.
Women’s attitudes toward vaginal delivery by race ethnicity and socioeconomic status, First Baby Study, Pennsylvania, 2009–2011.
| Mean vaginal delivery attitude scale score (range 1–5) |
p-valuea | Coeff.b | p-value | |
|---|---|---|---|---|
| Race/ethnicity | 0.55 | |||
| White | 4.29 | Reference | ||
| Black | 4.32 | 0.06 | 0.096 | |
| Latina | 4.32 | 0.03 | 0.417 | |
| Other | 4.24 | −0.06 | 0.270 | |
| Education | 0.03 | |||
| High school or less | 4.26 | Reference | ||
| Some college | 4.32 | 0.05 | 0.087 | |
| Bachelor’s degree or higher | 4.29 | 0.01 | 0.728 | |
| Insurance type | 0.58 | |||
| Private | 4.30 | Reference | – | |
| No private coverage | 4.28 | 0.03 | 0.260 |
Bivariate p-values are from Kruskall-Wallis tests.
Coefficients are from a multivariate linear regression model controlling for the variables listed as well as age, rurality, partnership status, diabetes, hypertension, obesity, nativity, and prenatal fear of birth.
p<0.05;
p<0.01;
p<0.001
As reported in Table 3, women’s prenatal attitudes toward delivery mode were strongly related to odds of delivering by cesarean. A one-point increase in the vaginal delivery attitude scale was associated with 40% lower odds of delivering by cesarean (p<0.001). Positive attitude toward vaginal birth was related to lower odds of both planned and unplanned cesarean, although the magnitude of the association was larger for planned cesarean delivery. A one-point increase in the vaginal delivery attitudes scale was associated with 75% lower relative risk of planned cesarean, and 21% lower odds of unplanned cesarean delivery, compared to vaginal birth. In these adjusted models, black and Latina women had higher odds of delivering by cesarean overall compared to white women, and higher odds of delivering by unplanned cesarean compared to white women. Education and insurance type were not significantly associated with delivery mode.
Table 3.
Adjusted odds or relative risk of cesarean delivery by attitude toward vaginal delivery in the third trimester of pregnancy, First Baby Study, Pennsylvania, 2009–2011.
| Model 1a | Model 2b | ||
|---|---|---|---|
|
|
|||
| Any cesarean | Planned cesarean | Unplanned cesarean | |
|
|
|||
| OR (95% CI) | RRR (95% CI) | RRR (95% CI) | |
| Vaginal delivery attitude scale | 0.60 (0.51, 0.72)*** | 0.25 (0.20, 0.32)*** | 0.79 (0.66, 0.93)** |
| Race/ethnicity | |||
| White | Reference | Reference | Reference |
| Black | 1.69 (1.29, 2.23)*** | 1.73 (0.75, 3.99) | 1.69 (1.29, 2.22)*** |
| Latina | 1.53 (1.11, 2.10)** | 1.46 (0.37, 5.84) | 1.53 (1.21, 1.93)*** |
| Other | 1.44 (0.87, 2.37) | 0.29 (0.03, 2.71) | 1.67 (0.99, 2.82) |
| Education | |||
| High school or less | Reference | Reference | Reference |
| Some college | 0.89 (0.75, 1.04) | 0.78 (0.50, 1.22) | 0.893 (0.75, 1.06) |
| Bachelor’s degree or higher | 0.89 (0.68, 1.15) | 0.78 (0.50, 1.23) | 0.90 (0.68, 1.19) |
| Insurance type | |||
| Private | Reference | Reference | Reference |
| No private coverage | 0.85 (0.67, 1.10) | 0.94 (0.54, 1.63) | 0.83 (0.62, 1.13) |
Logistic regression model.
Multinomial logit model. OR – odds ratio. RRR – relative risk ratio. Models adjust for race, education, insurance type, age, partnership status, nativity, rurality, diabetes, hypertension, obesity, gestational age at birth, and prenatal fear of delivery. Models use clustered standard errors to account for correlation between women giving birth at the same hospital.
p<0.05;
p<0.01;
p<0.001
Although the lack of variation in delivery mode attitudes by race/ethnicity makes this an unlikely mediator, we estimated Karlson-Holm-Breen models as a formal test. There was no difference in the magnitude of the association between race/ethnicity and cesarean delivery depending on inclusion of vaginal delivery attitudes in the model, indicating that attitudes do not mediate the relationship between race/ethnicity and cesarean delivery (results not shown).
Finally, we estimated multivariate models including interaction terms to examine whether women’s prenatal attitudes toward vaginal delivery were differentially related to actual delivery mode depending on race/ethnicity and socioeconomic status (moderation). These models revealed a consistent pattern whereby prenatal attitudes toward delivery mode were related to actual delivery mode only among more socially privileged women, or more strongly among more socially privileged women (Table 4). The average marginal effect of the vaginal delivery attitudes scale among white women was −0.11; that is, among white women, a one-unit increase in the vaginal delivery attitudes scale (indicating a more favorable view of vaginal delivery) was associated with a 0.11 decrease on average in the predicted probability of delivering by cesarean. In contrast, the average marginal effect of vaginal delivery attitudes on cesarean delivery was non-significant among women in other racial/ethnic groups, indicating that for racial/ethnic minority women, there was no change in the predicted probability of delivering by cesarean based on attitudes toward vaginal delivery. As shown in Figure 1, a white woman with a score of 4 on the vaginal delivery attitudes scale had a predicted probability of cesarean delivery of 0.30, while for a white woman with a score of 5 (most favorable to vaginal delivery), the predicted probability of cesarean delivery dropped to 0.19. For women of other racial/ethnic groups, there was no statistically significant difference in the predicted probability of cesarean based on the vaginal delivery attitudes scale. Similarly, the average marginal effect of the vaginal delivery attitudes scale was statistically significant and negative among women with a Bachelor’s degree or higher (−0.13), but non-significant among women with less education (Table 4). The vaginal delivery attitudes scale had a negative average marginal effect on delivering by cesarean among women regardless of insurance coverage type, but the average marginal effect was about twice as large in magnitude among women with private insurance compared to those without private insurance (−0.12 vs. −0.05). Figures 1 and 2 display predicted probabilities by education, insurance type and vaginal delivery attitudes scale scores. Results were similar for unplanned cesarean delivery (Table 4).
Table 4.
Average marginal effect (AME) of vaginal delivery attitudes scale by race/ethnicity, education and insurance type, First Baby Study, Pennsylvania, 2009–2011.
| Any cesarean | Unplanned cesarean | |||
|---|---|---|---|---|
|
|
||||
| AME | p | AME | ||
| Race/ethnicitya | ||||
| White | −0.11 | <0.01 | −0.06 | <0.01 |
| Black | 0.03 | 0.61 | 0.07 | 0.29 |
| Latina | 0.07 | 0.51 | 0.15 | 0.10 |
| Other | −0.05 | 0.70 | −0.01 | 0.93 |
| Educationb | ||||
| High school or less | −0.04 | 0.13 | −0.02 | 0.54 |
| Some college | −0.06 | 0.10 | 0.01 | 0.77 |
| Bachelor’s degree or higher | −0.13 | <0.01 | −0.07 | <0.01 |
| Insurance typec | ||||
| Private coverage | −0.12 | <0.01 | −0.05 | <0.01 |
| No private coverage | −0.05 | 0.03 | −0.01 | 0.60 |
From models including interaction between cesarean attitudes and race/ethnicity.
From models including interaction between cesarean attitudes and education.
From models including interaction between cesarean attitudes and insurance type. AME – average marginal effect. The average marginal effect indicates the average change in the predicted probability of the outcome associated with a one-unit increase in the vaginal delivery attitudes scale.
Figure 1.
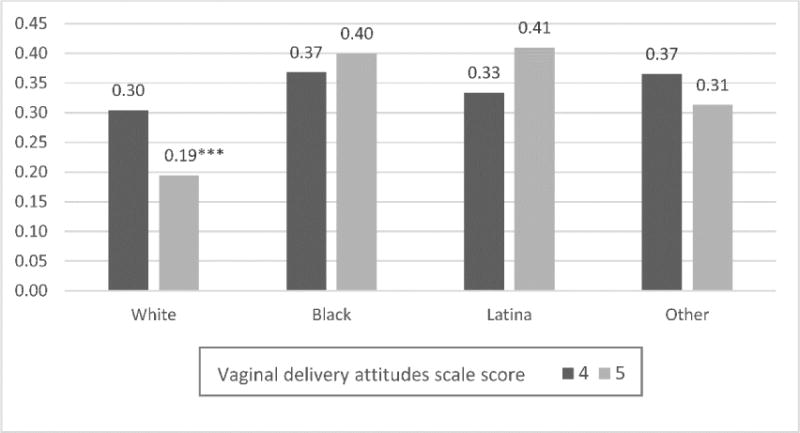
Predicted probability of cesarean delivery by race/ethnicity and vaginal delivery attitudes scale score. Model adjusted for covariates listed in Table 3 and included an interaction term between race/ethnicity and vaginal delivery attitudes scale score. *p<0.05; **p<0.01; ***p<0.001
Figure 2.
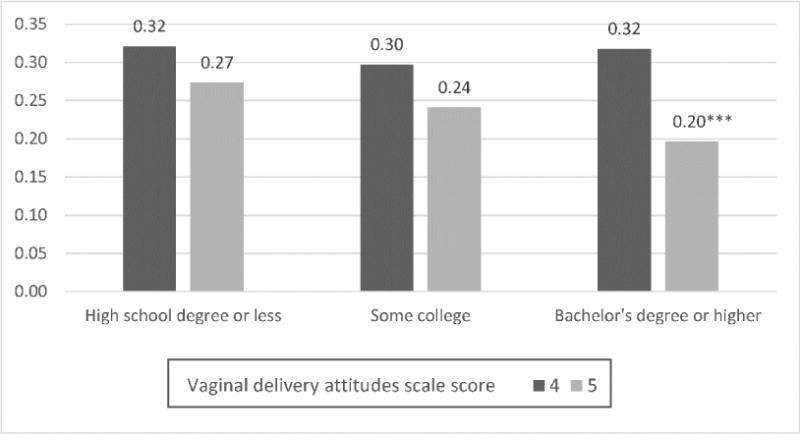
Predicted probability of cesarean delivery by education level and vaginal delivery attitudes scale score. Model adjusted for covariates listed in Table 3 and included an interaction term between education level and vaginal delivery attitudes scale score. *p<0.05; **p<0.01; ***p<0.001
Discussion
Consistent with previous studies, we found that women who had a more positive attitude toward vaginal birth were more likely to deliver vaginally. Our exploration of birth attitudes by race/ethnicity and socioeconomic status provides important new information. First, prenatal attitudes toward vaginal delivery did not vary by race/ethnicity or socioeconomic status, indicating that attitudes toward delivery mode cannot be the mechanism behind differential odds of cesarean delivery in this cohort. There were marginally significant differences in attitudes toward vaginal birth between black and white women, but the direction of this trend was the opposite of what would be expected if birth attitudes were a mechanism behind cesarean delivery disparities: black women reported more positive attitudes vaginal birth than did white women. Moreover, we found that the relationship between delivery mode preference and actual delivery mode was only present among white women, more highly educated women, and women with private insurance.
These findings suggest that women occupying positions of social privilege may be more able to realize their preferences in the context of childbirth. There are a wide range of resources associated with race/ethnicity and socioeconomic status that could impact birth experiences. Women with more material resources may have a greater capacity to seek out a care provider whose practice style matches their preferences. They may have more generous health insurance and access to a wider range of clinicians. They also may be more able to find a clinician and hospital that are compatible with their wishes for birth, due to greater job flexibility or fewer transportation challenges (e.g. can take time off for appointments to meet different providers, or travel farther distances to the provider’s practice).27
Women who are white, more highly educated, and privately insured may also have greater access to resources like doula services that may enhance their chances of receiving care that is consistent with their preferences. Women with doula support are less likely to deliver by cesarean and report greater satisfaction with their birth experiences.28 However, doula services are costly and usually not covered by health insurance, limiting access.29 Additionally, doulas tend to be upper-middle-class and white, so racial/ethnic minority women may have difficulty finding a doula that shares their language or cultural background, even if cost is not a barrier.30 In addition to providing physical and emotional support, doula support may improve patient-clinician communication for some low income women and women of color.31
Patient-clinician interaction can be structured by social factors, including the patient’s race/ethnicity and socioeconomic status.19 Attributes such as health literacy and knowledge of medical terminology are unequally distributed across racial/ethnic and socioeconomic status groups.19 Prior studies have documented higher-quality patient-clinician communication and more patient involvement in decision making among white and higher socioeconomic status patients compared to patients who are from racial/ethnic minority groups and lower socioeconomic status.20,21,32 These aspects of the patient-clinician relationship may be linked to women’s ability and empowerment to have the type of birth they desire. That is, patient-clinician communication and patient involvement in decision-making may be important mechanisms for having a birth consistent with one’s preferences, but the quality of the patient-clinician relationship may be lower for low-socioeconomic status women and women of color.19,33
Furthermore, literature on clinician bias demonstrates that clinicians’ perceptions and beliefs about the race and socioeconomic status of the patient influence the care that they deliver, resulting in disparities in patient outcomes.23 This may be particularly salient in labor management decisions, which are subject to the interpretation of individual clinicians.5 If clinicians believe, for example, that black women are more likely to end up delivering by cesarean, they may be quicker to recommend cesarean delivery, setting aside other labor management options or the woman’s goals for her birth experience. Understanding the clinician-patient relationship and clinical decision-making style of clinicians (e.g. shared decision-making) may augment our understanding of how birth preferences are enacted.
Structural racism, which describes a confluence of institutions, culture, history, ideology, and codified practices that generate and perpetuate inequity based on race, has a profound influence on health care generally, and women’s reproductive health care specifically.34,35 Structural racism, which is distinct from interpersonal racism, may play a role in generating the findings reported here, due to the experiences pregnant women of different races have in institutional settings, like hospitals, and with power and privilege both inside and outside the health care system. Indeed, a recent study in New York City found that differences between hospitals where black and white women gave birth contributed to the racial disparities in maternal morbidity.36 Beyond institutional factors, structural racism may shape expectations and decisions made by clinicians, and by women and families.
Little is currently understood about how birth preferences form in the United States. Developing greater understanding of the development of preferences may reveal how these are shaped by interactions with clinicians, prior birth experiences, the advice of friends and family, and traditional or social media. Future work should examine factors related to structural racism as well as the formation of birth preferences to inform efforts to improve equity in maternity care.
Strengths and Limitations
Our results must be considered alongside some limitations. First, women in this study were not representative of all women giving birth in Pennsylvania. Study participants were disproportionately white, highly educated, and privately insured,25 meaning that the sample included fewer women of color and lower-socioeconomic status women. However, this cohort was much larger than previous studies of women’s birth preferences in the U.S.,12 and we were able to detect differences based on race/ethnicity and socioeconomic status despite sample size limitations. Second, regarding the planned cesarean findings, women who delivered by planned cesarean may already have known this at the baseline interview, or at least believed that they were more likely to give birth by cesarean; these women may have adjusted their expectations and expressed more positive feelings toward cesarean delivery. Third, women’s reported positive attitudes toward vaginal delivery may be partially due to social desirability bias. Finally, it is possible that lower-socioeconomic status women and/or women of color had more health problems before or during pregnancy, resulting in a higher likelihood of medically necessary cesarean regardless of preferences or attitudes toward delivery mode. As a sensitivity analysis, we excluded women from the sample who had obesity, diabetes or hypertension, and results were unchanged.
Strengths of this study include the assessment of vaginal birth attitudes prenatally, and the fact that all women in the sample were giving birth for the first time. This reduces the potential for women’s attitudes toward vaginal birth to have been influenced by previous birth experiences.
Conclusions
This analysis found that attitudes toward vaginal delivery did not vary by race/ethnicity or socioeconomic status. Women’s attitudes toward vaginal delivery in pregnancy were strongly related to odds of delivering by cesarean, but this relationship differed by race/ethnicity and socioeconomic status, suggesting that women occupying positions of social privilege are more able to realize their preferences in the context of childbirth. Efforts to foster equity in maternity care should focus on ensuring access to high-quality, patient-centered care consistent with women’s preferences.
Figure 3.
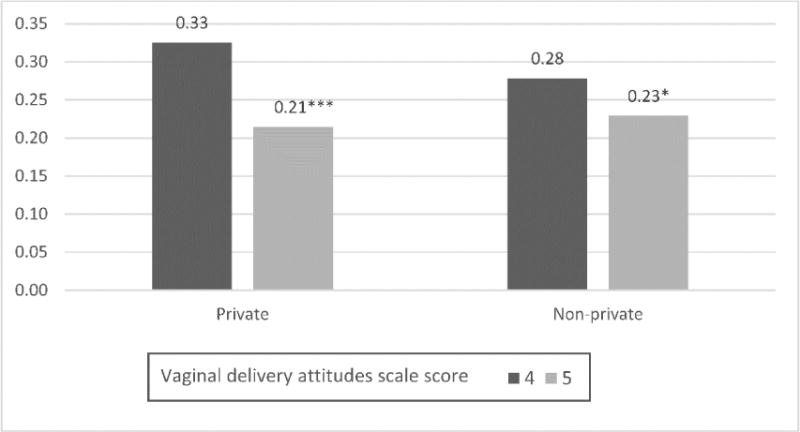
Predicted probability of cesarean delivery by insurance type and vaginal delivery attitudes scale score. Model adjusted for covariates listed in Table 3 and included an interaction term between insurance type and vaginal delivery attitudes scale score. *p<0.05; **p<0.01; ***p<0.001
Acknowledgments
Funding
The First Baby Study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH (R01 HD052990). Dr. Attanasio’s effort on this study was supported by a dissertation grant from the Agency for Healthcare Research and Quality (R36HS024215-01).
Footnotes
DR. LAURA BOWMAN ATTANASIO (Orcid ID : 0000-0001-9294-0718)
DR. KRISTEN KJERULFF (Orcid ID : 0000-0002-5376-2581)
Contributor Information
Laura B. Attanasio, Mellon Postdoctoral Fellow at Sewanee: The University of the South
Rachel R. Hardeman, Assistant Professor in the Division of Health Policy and Management, University of Minnesota School of Public Health, Minneapolis, MN
Katy B. Kozhimannil, Associate Professor in the Division of Health Policy and Management, University of Minnesota School of Public Health, Minneapolis, MN
Kristen H. Kjerulff, Professor in the Department of Public Health Sciences and Department of Obstetrics and Gynecology, College of Medicine, Penn State University, Hershey, PA
References
- 1.Hamilton BE, Martin JA, Osterman J, et al. Births: Final Data for 2014. Natl Vital Stat Reports. 2015;64(12):1–104. [PubMed] [Google Scholar]
- 2.Edmonds JK, Yehezkel R, Liao X, Moore Simas Ta. Racial and ethnic differences in primary, unscheduled cesarean deliveries among low-risk primiparous women at an academic medical center: a retrospective cohort study. BMC Pregnancy Childbirth. 2013;13(1):168. doi: 10.1186/1471-2393-13-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Washington S, Caughey AB, Cheng YW, Bryant AS. Racial and Ethnic Differences in Indication for Primary Cesarean Delivery at Term: Experience at One US Institution. Birth. 2012;39(2):128–134. doi: 10.1111/j.1523-536X.2012.00530.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huesch M, Doctor JN. Factors Associated With Increased Cesarean Risk Among African American Women: Evidence From California, 2010. Am J Public Health. 2015;105(5):956–962. doi: 10.2105/AJPH.2014.302381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Janevic T, Loftfield E, Savitz Da, Bradley E, Illuzzi J, Lipkind H. Disparities in cesarean delivery by ethnicity and nativity in new york city. Matern Child Health J. 2014;18(1):250–257. doi: 10.1007/s10995-013-1261-6. [DOI] [PubMed] [Google Scholar]
- 6.Roth LM, Henley MM. Unequal Motherhood : Racial-Ethnic and Socioeconomic Disparities in Cesarean Sections in the United States. Soc Probl. 2012;59(2):207–227. doi: 10.1525/sp.2012.59.2.207. [DOI] [Google Scholar]
- 7.Chung JH, Garite TJ, Kirk AM, Hollard AL, Wing Da, Lagrew DC. Intrinsic racial differences in the risk of cesarean delivery are not explained by differences in caregivers or hospital site of delivery. Am J Obstet Gynecol. 2006;194(5):1323–1328. doi: 10.1016/j.ajog.2005.11.043. [DOI] [PubMed] [Google Scholar]
- 8.Edmonds JK, Hawkins SS, Cohen BB. The Influence of Detailed Maternal Ethnicity on Cesarean Delivery: Findings from the U.S. Birth Certificate in the State of Massachusetts. Birth. 2014;41(3):290–298. doi: 10.1111/birt.12108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Young D. Cesarean delivery on maternal request”: Was the NIH conference based on a faulty premise? Birth. 2006;33(3):171–174. doi: 10.1111/j.1523-536X.2006.00101.x. [DOI] [PubMed] [Google Scholar]
- 10.American College of Obstetricians and Gynecologists. Safe prevention of the primary cesarean delivery. Obstetric Care Consensus No. 1. Obstet Gynecol. 2014;123:693–711. doi: 10.1097/01.AOG.0000444441.04111.1d. [DOI] [PubMed] [Google Scholar]
- 11.Green J, Baston H. Have women become more willing to accept obstetric interventions and does this relate to mode of birth? Data from a prospective study. Birth. 2007;34(1):6–13. doi: 10.1111/j.1523-536X.2006.00140.x. [DOI] [PubMed] [Google Scholar]
- 12.Wu E, Kaimal AJ, Houston K, Yee LM, Nakagawa S, Kuppermann M. Strength of preference for vaginal birth as a predictor of delivery mode among women who attempt a vaginal delivery. Am J Obstet Gynecol. 2013;210(5):1–6. doi: 10.1016/j.ajog.2013.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kozhimannil KB, Law MR, Virnig BA. Cesarean delivery rates vary tenfold among US hospitals; reducing variation may address quality and cost issues. Health Aff (Millwood) 2013;32(3):527–535. doi: 10.1377/hlthaff.2012.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaimal AJ, Kuppermann M. Decision making for primary cesarean delivery: the role of patient and provider preferences. Semin Perinatol. 2012;36(5):384–389. doi: 10.1053/j.semperi.2012.04.024. [DOI] [PubMed] [Google Scholar]
- 15.Barber EL, Lundsberg LS, Belanger K, Pettker CM, Funai EF, Illuzzi JL. Indications contributing to the increasing cesarean delivery rate. Obstet Gynecol. 2011;118(1):29–38. doi: 10.1097/AOG.0b013e31821e5f65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Quill TE, Brody H. Physician recommendations and patient autonomy: Finding a balance between physician power and patient choice. Ann Intern Med. 1996;125(9):763–769. doi: 10.1059/0003-4819-125-9-199611010-00010. [DOI] [PubMed] [Google Scholar]
- 17.Cooper LA, Beach MC, Johnson RL, Inui TS. Delving below the surface: Understanding how race and ethnicity influence relationships in health care. J Gen Intern Med. 2006;21(SUPPL. 1):21–27. doi: 10.1111/j.1525-1497.2006.00305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Feagin J, Bennefield Z. Systemic racism and U.S. health care. Soc Sci Med. 2014;103:7–14. doi: 10.1016/j.socscimed.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 19.Shim JK. Cultural Health Capital: A Theoretical Approach to Understanding Health Care Interactions and the Dynamics of Unequal Treatment. J Health Soc Behav. 2010;51(1):1–15. doi: 10.1177/0022146509361185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cooper LA, Roter DL, Carson KA, et al. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health. 2012;102(5):979–987. doi: 10.2105/AJPH.2011.300558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ratanawongsa N, Zikmund-Fisher BJ, Couper MP, Van Hoewyk J, Powe NR. Race, ethnicity, and shared decision making for hyperlipidemia and hypertension treatment: the DECISIONS survey. Med Decis Making. 2010;30(5 Suppl):65S–76S. doi: 10.1177/0272989X10378699. [DOI] [PubMed] [Google Scholar]
- 22.Lin MY, Kressin NR. Race/ethnicity and Americans’ experiences with treatment decision making. Patient Educ Couns. 2015;98(12):1636–1642. doi: 10.1016/j.pec.2015.07.017. [DOI] [PubMed] [Google Scholar]
- 23.van Ryn M, Burgess DJ, Dovidio JF, et al. The Impact of Racism on Clinician Cognition, Behavior, and Clinical Decision Making. Du Bois Rev Soc Sci Res Race. 2011;8(1):199–218. doi: 10.1017/S1742058X11000191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Green AR, Carney DR, Pallin DJ, et al. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. J Gen Intern Med. 2007;22(9):1231–1238. doi: 10.1007/s11606-007-0258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kjerulff KH, Velott DL, Zhu J, et al. Mode of first delivery and women’s intentions for subsequent childbearing: findings from the First Baby Study. Paediatr Perinat Epidemiol. 2013;27(1):62–71. doi: 10.1111/ppe.12014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kohler U, Karlson KB, Holm A. Comparing coefficients of nested nonlinear probability models. Stata J. 2011;11(3):420–438. [Google Scholar]
- 27.Kullgren JT, Mclaughlin CG, Mitra N, Armstrong K. Nonfinancial Barriers and Access to Care for U.S. Adults. Health Serv Res. 2012;47(1):462–485. doi: 10.1111/j.1475-6773.2011.01308.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hodnett ED, Gates S, Hofmeyr GJ, Sakala C, Weston J. Continuous Support for Women During Childbirth (Review) Cochrane Database Syst Rev. 2013;3(10) [Google Scholar]
- 29.Strauss N, Giessler K, McAllister E. How Doula Care Can Advance the Goals of the Affordable Care Act: A Snapshot From New York City. J Perinat Educ. 2015;24(1):8–158. doi: 10.1891/1058-1243.24.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lantz PM, Low LK, Varkey S, Watson RL. Doulas as childbirth paraprofessionals: results from a national survey. Women’s Heal Issues. 2005;15(3):109–116. doi: 10.1016/j.whi.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 31.Kozhimannil KB, Vogelsang CA, Hardeman RR, Prasad S. Disrupting the Pathways of Social Determinants of Health: Doula Support during Pregnancy and Childbirth. J Am Board Fam Med. 2016;29(3):308–317. doi: 10.3122/jabfm.2016.03.150300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Willems S, De Maesschalck S, Deveugele M, Derese a, De Maeseneer J. Socio-economic status of the patient and doctor-patient communication: does it make a difference? Patient Educ Couns. 2005;56(2):139–146. doi: 10.1016/j.pec.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 33.Attanasio L, Kozhimannil KB. Patient-reported Communication Quality and Perceived Discrimination in Maternity Care. Med Care. 2015;53(10):863–871. doi: 10.1097/MLR.0000000000000411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roberts D. Killing the Black Body: Race, Reproduction, and the Meaning of Liberty. New York: Vintage; 1997. [Google Scholar]
- 35.Hardeman RR, Medina EM, Kozhimannil KB. Structural Racism and Supporting Black Lives – The Role of Health Professionals. N Engl J Med. 2016 doi: 10.1056/NEJMp1002530. Epub ahead. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Howell EA, Egorova NN, Balbierz A, Zeitlin J, Hebert PL. Site of delivery contribution to black-white severe maternal morbidity disparity. Am J Obstet Gynecol. 2016;215(2):143–152. doi: 10.1016/j.ajog.2016.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]


