Abstract
Background
Prior studies have reported that community health centers perform as well as other sites of care, despite serving more vulnerable patient populations. However, there is little prior study of geographic variation in quality outcomes and disparities in outcomes in this setting. Quantifying geographic variation is important so as to target quality improvement efforts and funding and to learn from states where total quality is highest and racial/ethnic disparities are lowest.
Objectives
To estimate between-state variation in hypertension, diabetes, and pregnancy outcomes and racial/ethnic disparities in these outcomes for health center patients.
Methods
Using data on all US health centers from 2010–2014 (N=1047 health centers/year, or 21.2 million patients in 2014), we used linear regression models to estimate adjusted quality outcomes and racial/ethnic disparities in quality outcomes by state for hypertension control, diabetes control, and normal birthweight.
Results
We found wide variation in both outcomes and racial/ethnic disparities in outcomes between states for patients seen at health centers. For instance, between states, the mean proportion of patients with hypertension control ranged from 58% to 70% for white patients, from 49% to 64% for black patients, and from 53% to 74% for Hispanic patients (p<0.001). Racial/ethnic disparities in outcomes ranged from negative or non-significant in some states to positive in others.
Conclusions
Wide variation in health center patient outcomes and disparities in outcomes is observed between states. This variation suggests that policymakers should target funding and interventions to underperforming states, and identify determinants of high quality in higher performing states.
Keywords: community health centers, quality of care, health disparities, geographic variation
Introduction
Federally-funded community health centers play a critical role in the US health care system. They provide access to “high quality, culturally competent, comprehensive primary care” for low-income patients in medically underserved communities.1 As of 2014, 62% of health center patients were from racial/ethnic minority groups, 23% had limited English proficiency, 92% had income <200% of the federal poverty level (FPL), and 28% were uninsured.2 Despite serving sociodemographically vulnerable populations, the quality of care provided at health centers is similar to care provided in other settings, on average.3 Racial/ethnic disparities are generally narrower among health center patients compared to patients seen in other care settings, though they are still present.4,5,6,7
While there is some evidence on nationwide quality of and disparities in care for health center patients, no known peer-reviewed research examines how quality outcomes and disparities in outcomes vary between states. However, in other populations, research suggests that there is wide between-state variation in quality of care. For example, among adult diabetic patients in 2012, annual foot exam rates ranged from 57% in Nevada to 82% in New Hampshire, dilated eye exam rates ranged from 53% in Utah to 78% in Delaware, and rates of A1c levels being checked at least twice per year ranged from to 57% in Idaho to 81% in Hawaii.8 Rates of low birthweight also vary widely by state, from an average rate of 6% in Alaska to 11% in Mississippi in 2014.9
Not only does research suggest wide variation in quality between states, but wide variation in racial/ethnic disparities in quality is also evident. For instance, in 2014, absolute differences in the rates of low birthweight for white versus black patients ranged from 2.8 percentage points in Minnesota and West Virginia to 8.4 percentage points in New Mexico.9 White/black disparities in the percent of adults reporting fair or poor health status ranged from 1.3 percentage points in Kentucky to 15.6 percentage points in the District of Columbia (DC).10 A study by Kang-Kim et al. using Behavioral Risk Factor Surveillance System data suggested that white/Hispanic disparities in rates of preventative service utilization vary widely between states as well.11
While state variation is evident in the general population, variation in outcomes for health center patients is not documented in the literature. However, quantifying health center variation at the state-level is important for two main reasons. First, many of the interventions and policies that could affect quality of care occur at the state-level; this includes Medicaid eligibility levels, state funding for health centers, investment in public health and social services, and payment and delivery reform efforts. We can also learn from states where quality is highest and disparities are lowest so as to maximize outcomes for all health center patients. Second, when looking within Census regions, we find considerable heterogeneity between states within regions. This limits our ability to make generalizations at the regional level. Thus, our objective was to estimate between-state variation in quality outcomes and disparities in quality outcomes for health center patients.
Methods
Data Source and Study Population
We acquired the 2010–2014 Uniform Data System (UDS) data, which are collected annually by the Health Resources & Services Administration (HRSA) Bureau of Primary Health Care from all US health centers. The UDS includes health center-level information on all Section 330 health center grantees (N=1278); thus, these were reported as facility-level rather than patient-level data. Each center reported data on quality measures, service utilization, organizational features, and patient characteristics. We excluded health centers located in US territories (N=29); those where all sites were school-based, mobile, or seasonal (N=2); and those that were newly established or lost their health center status during the 2009–2014 period (N=200). Our final sample size was 1047 health centers per year, which served 18.6 million patients in 2010 and 21.2 million patients in 2014. Final sample sizes varied by measure, racial/ethnic group, and state, as shown in the Supplemental Digital Content (eTables 3–11).
Study Variables
Three intermediate quality outcomes were examined separately for each racial/ethnic group: (1) glycosylated hemoglobin (HbA1c) <=9% among patients with diabetes, (2) blood pressure <140/90mmHg among patients with hypertension, and (3) normal birthweight (>=2500 grams) among patients giving birth. This represents all available outcome measures in the UDS. Measure definitions are shown in the Supplemental Digital Content (eTable 1). These outcomes were reported annually by each center for non-Hispanic white, non-Hispanic black, and Hispanic patients. For each health center, we also calculated absolute disparities between non-Hispanic whites and each racial/ethnic group for each measure in each year. We refer to all differences as disparities, in accordance with the Centers for Disease Control and Prevention’s (CDC) definition of health disparities,30 because clinical targets are set such that they should be achievable by all. We used non-Hispanic whites as the reference population per suggested guidelines that disparities are measured from the most favorable group rate.31
Covariates, all assessed at the facility-level, were the following patient characteristics: percent male, percent age 65 or older, percent uninsured, percent with income below FPL, percent homeless, and percent whose primary language was not English. We also included number of patients served and urban versus rural location.
Statistical Analyses
The unit of analysis was the health center. For each state and measure, we examined unadjusted mean quality by race/ethnicity and mean racial/ethnic disparity in quality. For each measure, we then estimated performance rates that adjusted for the health center characteristics noted above, as these characteristics are known to be associated with quality and vary by state. We first fit linear regression models with standard errors clustered at facility-level, which generated “predicted” rates based on the included covariates. Next, the adjusted rates were calculated as the ratio of the “observed,” or actual, performance rate to the “predicted” performance rate, multiplied by the overall mean unadjusted rate in the health center population.13,14 The unadjusted analyses are largely consistent with the results of the adjusted models and are therefore presented in the Supplemental Digital Content only (eTable 3, eTable 5, eTable 7).
To assess between-state variation in quality outcomes, we used linear regression models to test whether adjusted performance rates (main dependent variable) varied by state (main independent variable) for each racial/ethnic group. From the regression model, we estimated the pooled 2010–2014 mean adjusted performance rates for each state and descriptively compared the range of estimates across states, including the median, interquartile range (IQR), the minimum, and the maximum. In all analyses, we weighted each observation by the center’s population size and used robust standard errors. We clustered observations at the health center level to account for repeated measures. Rates are pooled across years as to maximize sample size within a state. Where fewer than 100 patients were reported in a state across the five years, that state was excluded from our reported results.
To estimate between-state variation in disparities in outcomes, for each quality measure, we used linear regression models to estimate mean marginal rates of within-center disparities by state in 2010–2014. These within-center analyses were limited to health centers with at least 20 eligible white and 20 eligible minority patients in the measure denominator in a given year.15 All observations were clustered at the health center level to account for repeated measures. We estimated disparities between non-Hispanic white and non-Hispanic black patients and non-Hispanic white and Hispanic patients. As above, we descriptively compared the range of estimates across states for each disparity measure.
In additional sensitivity analyses, we repeated all quality analyses for each racial/ethnic group using generalized linear models with a binomial distribution and logit link. The results were robust to model specification.
All statistical analyses were performed using Stata v.14. Two-sided statistical tests with p-values <=0.05 were considered statistically significant. Brown University’s IRB approved the study.
Results
Characteristics of the 2010–2014 health center population are shown in Table 1. On average, the majority (64%) of patients were age 18–64, over half were non-white, 35% had Medicaid coverage, 37% were uninsured, and nearly all (92%) had incomes below 200% FPL. These health center patient characteristics varied between states. Mean health center characteristics for each state are shown in the Supplemental Digital Content (eTable 2).
Table 1.
State Variation in Characteristics of the Health Center Population, 2010–2014
| US Mean | SE | State Min | State Max | |
|---|---|---|---|---|
| Patients, no. per center | 19,005 | 287 | 3,610 (WY) | 33,547 (DC) |
| Age, % | ||||
| 0–17 | 27.5 | 16.6 | 13.7 (WY) | 39.1 (NV) |
| 18–64 | 64.4 | 16.3 | 54.2 (NV) | 81.6 (WY) |
| 65+ | 8.1 | 7.7 | 3.7 (IN) | 17.8 (ME) |
| Male, % | 42.6 | 9.5 | 36.9 (DE) | 51.6 (WY) |
| Race/ethnicity, % | ||||
| White | 44.1 | 42.3 | 3.8 (DC) | 92.7 (WV) |
| Black | 19.5 | 33.8 | 0.6 (MT) | 61.1 (MS) |
| Hispanic | 25.4 | 37.7 | 0.9 (WV) | 63.6 (NM) |
| Asian | 2.5 | 11.5 | 0.2 (WV) | 19.1 (HI) |
| AIAN | 2.4 | 14.5 | <0.1 (WV) | 40.3 (AK) |
| Insurance coverage, % | ||||
| Medicaid | 35.1 | 22.9 | 9.8 (WY) | 57.0 (CT) |
| Medicare | 9.1 | 8.7 | 3.7 (DC) | 19.7 (ME) |
| Other Public | 1.7 | 05.2 | <0.1 (AZ) | 17.5 (DC) |
| Private | 16.9 | 18.2 | 6.5 (DC) | 37.0 (ND) |
| Uninsured | 37.2 | 26.9 | 10.5 (VT) | 71.9 (WY) |
| Income level, % | ||||
| Under 100% FPL | 68.5 | 24.7 | 34.2 (VT) | 77.2 (IL) |
| Under 200% FPL | 91.8 | 14.6 | 71.4 (VT) | 97.6 (NV) |
| Primary language other than English, % | 16.4 | 28.8 | 0.4 (WV) | 50.4 (DC) |
| Homeless, % | 8.2 | 30.2 | 0.9 (WV) | 41.2 (WY) |
| Urban, % | 51.0 | 69.1 | 0.0 (ME) | 95.6 (NJ) |
| EHR use, %a | 65.7 | 65.6 | 57.0 (CA) | 80.0 (AR, DE, NV) |
All estimates represent pooled 2010–2014 rates. The number of health centers and number of patients varies by state. State-specific estimates represent the mean rate in the state. See Supplemental Digital Content for all state estimates (eTable 2). AIAN indicates American Indian/Alaskan Native; FPL, federal poverty level; EHR, electronic health record; SE, standard error.
represents 2011–2014 average, measure not available in 2010.
State variation in quality by race/ethnicity
As shown in Table 2, between all states, there was wide variation in adjusted quality outcomes for each racial/ethnic group. When comparing aggregate, state-level rates of diabetes control by race/ethnicity, the median state rate was highest amongst white (71%) patients and lowest amongst black (66%) and Hispanic (66%) patients. State-level rates of diabetes control for white patients varied (IQR 68–73%), from a low of 50% to a high of 79%. Thus, the average white diabetic patient in the lowest state was less likely to have controlled diabetes as compared to the average black or Hispanic diabetic patient nationwide. Between-state variation in diabetes control was also evident for black patients (IQR 63–69%), from a low of 44% to a high of 80%, and for Hispanic patients (IQR 64–69%), from a low of 54% to a high of 81% (p<0.001, respectively).
Table 2.
State Variation in Adjusted Quality Outcomes by Race/Ethnicity, 2010–2014
| US Mean | State Performance Rates | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Mean | SE | State Mediana | State IQR | Lowest State | 95% CI | Highest State | 95% CI | |||
| Diabetes Control, % | ||||||||||
|
| ||||||||||
| White | 69.4 | 22.3 | 71.2 | 67.8 – 73.1 | 50.2 | 44.5 | 55.9 | 78.6 | 77.2 | 80.0 |
| Black | 65.1 | 32.6 | 66.1 | 62.7 – 69.0 | 43.8 | 26.5 | 61.1 | 79.6 | 75.0 | 84.3 |
| Hispanic | 65.4 | 30.2 | 66.0 | 63.7 – 68.8 | 54.0 | 43.2 | 64.9 | 80.7 | 78.6 | 82.7 |
|
| ||||||||||
| Hypertension Control, % | ||||||||||
|
| ||||||||||
| White | 64.0 | 20.1 | 64.2 | 62.5 – 65.2 | 58.1 | 55.3 | 61.0 | 69.9 | 67.2 | 72.7 |
| Black | 56.9 | 30.0 | 56.8 | 54.4 – 58.8 | 48.6 | 45.7 | 51.5 | 64.3 | 56.6 | 72.0 |
| Hispanic | 63.5 | 29.4 | 63.0 | 61.7 – 66.0 | 52.5 | 47.6 | 57.3 | 74.3 | 66.6 | 82.0 |
|
| ||||||||||
| Normal Birthweight, % | ||||||||||
|
| ||||||||||
| White | 86.9 | 30.0 | 89.1 | 88.0 –90.3 | 82.5 | 69.8 | 95.2 | 92.2 | 88.7 | 95.7 |
| Black | 86.2 | 32.1 | 88.1 | 85.5 – 89.4 | 78.8 | 65.3 | 92.2 | 98.1 | 97.0 | 99.2 |
| Hispanic | 88.9 | 27.6 | 91.3 | 89.0 – 92.3 | 79.6 | 71.1 | 88.1 | 93.9 | 92.8 | 95.0 |
All estimates represent pooled 2010–2014 rates. The number of health centers and number of patients varies by measure, race/ethnicity, and state. See Supplemental Digital Content (eTable 4, eTable 6, eTable 8) for all sample sizes and for all state estimates. If a state with fewer than 100 patients in the denominator or with a statistically insignificant (p>0.05) point estimate exhibited the highest or lowest quality rate, it was excluded. SE indicates standard error; IQR, interquartile range; CI, confidence interval. Estimates are adjusted for factors that may confound quality: % male, % age65+, % uninsured, % <100% FPL, % homeless, % primary language other than English, number of patients at health center, and urban v rural indicator.
State median represents the median of within-state means
When comparing aggregate, state-level rates of hypertension control by race/ethnicity, the median state rate was highest amongst white (64%) and Hispanic (63%) patients and lowest amongst black (57%) patients. Hypertension control rates ranged from 58% to 70% for white patients (IQR 63–65%), from 49% to 64% for black patients (IQR 54–59%), and from 53%to 74% for Hispanic patients (IQR 62–66%) (p<0.001, respectively).
When comparing aggregate, state-level rates of normal birthweight between racial/ethnic groups, less variation was observed as compared to the other outcomes, though black patients on average had slightly lower rates of normal birthweight as compared to other racial/ethnic groups (state median: 88%).Hispanic patients had the highest rates of normal birthweight (state median: 91%), while the state median for white patients was 89%. Between-state variation was evident. For example, rates of normal birthweight ranged from 83% to 92% for white patients (IQR 88–90%), from 79% to 98% for black patients (IQR 86–89%), and from 80% to 94% for Hispanic patients (IQR 89–92%) (p<0.001, respectively).
State variation in racial/ethnic disparities
As shown in Table 3, we observed between-state variation in the magnitude of racial/ethnic disparities in outcomes within health centers. The mean difference in diabetes control rates between white and black patients was 2.5 percentage points (IQR 1.4–4.6 percentage points). While one state exhibited a white/black disparity of 21.0 percentage points (p<0.001), 33 of the 51 states and districts showed no statistical disparity (p>=0.05). A statistically significant white/black disparity was detected in 18 states, and in each of those states, white patients had higher rates of diabetes control than black patients within the same health centers, on average. Furthermore, across all states the mean difference in rates of diabetes control for white versus Hispanic patients was 3.3 percentage points. However, 26 of the 51 states had no statistically significant white/Hispanic disparity.
Table 3.
State Variation in Within-Center Racial/Ethnic Disparities in Quality Outcomes, 2010–2014
| US Mean (SE) | State Performance
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| State Median | State IQR | Largest Disparity | 95% CI | Smallest Disparity | 95% CI | |||||
| Diabetes Control | ||||||||||
|
| ||||||||||
| white/black | 2.5 | 0.2 | 2.5 | 1.4–4.6 | 21.0 | 18.1 | 23.8 | −2.8a | −8.1 | 2.5 |
| white/Hispanic | 3.1 | 0.2 | 3.3 | 2.5–6.9 | 12.6 | 2.1 | 23.1 | −2.4b | −6.1 | 1.3 |
|
| ||||||||||
| Hypertension Control | ||||||||||
|
| ||||||||||
| white/black | 7.4 | 0.2 | 7.6 | 6.1–9.7 | 13.8 | 5.4 | 22.2 | 1.9c | −2.6 | 6.5 |
| white/Hispanic | 0.1 | 0.2 | 0.0 | −1.0–2.8 | 13.0 | 4.0 | 22.0 | −4.8 | −9.6 | −0.1 |
|
| ||||||||||
| Normal Birthweight | ||||||||||
|
| ||||||||||
| white/black | 2.3 | 0.3 | 2.5 | 0.1–3.8 | 9.1 | 1.6 | 16.5 | −6.9 | −12.9 | −1.0 |
| white/Hispanic | −1.8 | 0.3 | −2.0 | −2.7–0.0 | 8.1 | 0.7 | 15.5 | −9.4 | −9.4 | −9.4 |
All estimates represent pooled 2010–2014 rates. All disparities represent the absolute percentage point difference between non-Hispanic white and black patients or non-Hispanic white and Hispanic patients. IQR indicates interquartile range; CI, confidence interval; SE, standard error. A positive estimate indicates higher performance for white patients. A negative estimate indicates higher performance for black or Hispanic patients. Largest Disparity indicates the state with the largest absolute difference between white and black or Hispanic patients, while Smallest Disparity indicates the state with the smallest difference, which is often negative. The number of health centers and number of patients varies by measure, race/ethnicity, and state. See Supplemental Digital Content (eTables 9–11) for all sample sizes and for all state estimates. If a state had fewer than 100 patients in the denominator, it was excluded.
33 of 51 states had no statistical disparity, on average (p>=0.05)
26 of 51 states had no statistical disparity, on average (p>=0.05)
6 of 51 states had no statistical disparity, on average (p>=0.05)
We observed the largest within-center disparities for rates of hypertension control in white versus black patients, with a state median disparity of 7.6 percentage points (IQR 6.1–9.7 percentage points). This variation is further depicted in Figure 1, where states located near or below the 45-degree angle line exhibit no disparity, on average, and states above the line have exhibit disparities in favor of white patients, on average. Six of the 51 states had no white/black statistical disparity on average, with just two states falling below the 45-degree line. On average, there was no white/Hispanic disparity in hypertension control, with a median state disparity of 0.0 percentage points (IQR −1.0–2.8 percentage points). This is shown in Figure 2, where forty states exhibited no statistical white/Hispanic disparity in hypertension control, with 26 states falling below the 45-degree line. Five states exhibited statistically higher rates control for Hispanic patients as compared to white patients (p>0.05).
Figure 1. State Variation in Hypertension Control for White versus Black Patients, 2010–2014.
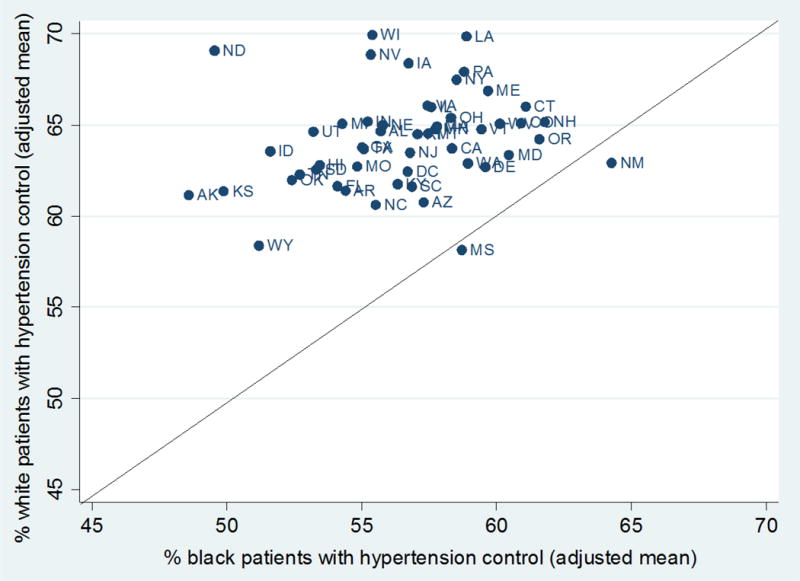
As you move further up the y-axis, average hypertension control rates increase for white patients and as you move further down the x-axis, average hypertension control rates increase for black patients. A 45-agree angle line dissects the graph, where states close to or on the line exhibit no aggregate disparity between the two racial/ethnic groups; the further above the line a state appears, the larger the disparity in that state. Each state estimate represents the adjusted, population-weighted mean rate from 2010–2014 across all health centers in the state. All state estimates have p<0.001. All state estimates, including 95% confidence intervals, in addition to analogous figures for diabetes control and normal birthweight, are included in the Supplemental Digital Content (eTable 4, eTable 6, eTable 8).
Figure 2. State Variation in Hypertension Control for White versus Hispanic Patients, 2010–2014.
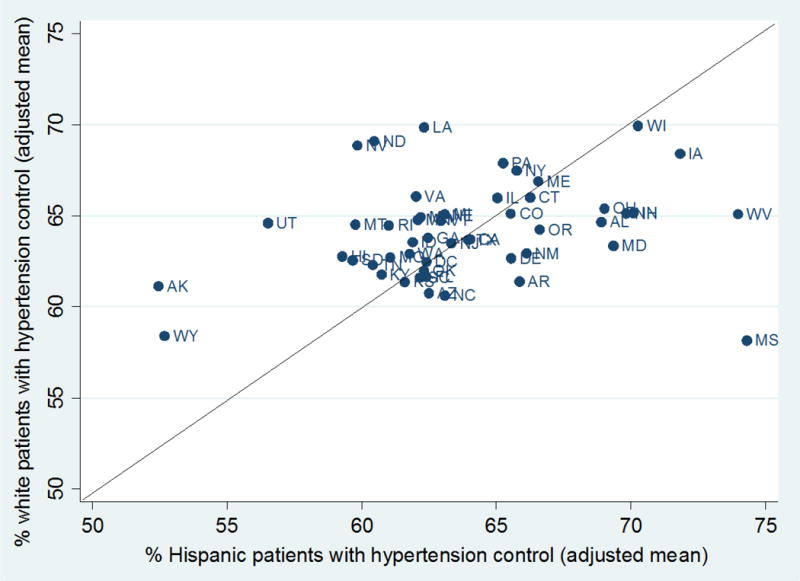
As you move further up the y-axis, average hypertension control rates increase for white patients and as you move further down the x-axis, average hypertension control rates increase for Hispanic patients. A 45-agree angle line dissects the graph, where states close to or on the line exhibit no aggregate disparity between the two racial/ethnic groups; the further above the line a state appears, the larger the disparity in that state. Each state estimate represents the adjusted, population-weighted mean rate from 2010–2014 across all health centers in the state. All state estimates have p<0.001. All state estimates, including 95% confidence intervals, in addition to analogous figures for diabetes control and normal birthweight, are included in the Supplemental Digital Content (eTable 4, eTable 6, eTable 8).
We again found that within-center disparities for normal birthweight varied notably by state. Both white/black disparities (state median: 2.5 percentage points, IQR: 0.1–3.8) and white/Hispanic disparities (state median: −2.0, IQR: −2.7–0.0) ranged from negative in some states to positive in others.
Across all measures and racial/ethnic groups, states ranking in the top quartile for more than half of all measures included Connecticut, Maine, Minnesota, North Dakota, Nebraska, New Hampshire, New York, and Oregon. States most often ranking in the bottom quartile for quality outcomes included Alaska, Hawaii, Idaho, Kansas, Louisiana, Mississippi, and Wyoming. The state most consistently exhibiting the lowest levels of racial/ethnic disparities was New Hampshire, whereas states most consistently exhibiting the largest levels of disparities included Montana, North Dakota, Nevada, South Dakota, and Vermont.
Finally, though we report adjusted estimates for each measure and each state, we found similar results in unadjusted analyses, as the covariates explained less than 10 percent of the variation in outcomes (see Supplemental Digital Content, eTable 3, eTable 5, eTable 7).
Discussion
Prior studies have reported that community health centers perform as well as other sites of care, on average, despite serving a more vulnerable patient population. However, such averages often mask important underlying variation. In this study, we find wide variation in outcomes and racial/ethnic disparities in outcomes between states for patients seen at community health centers, which persisted after adjusting for observable patient characteristics at the health center level. Some centers and states far exceed national averages for key outcome measures, while others fall short. Racial/ethnic disparities in outcomes range from negative or non-significant in some states to positive in others. We further find that when comparing state averages, compared to white patients, there are widespread disparities for some measures (e.g. hypertension control among black patients, diabetes control among black and Hispanic patients) but minimal disparities for other measures (e.g. low birthweight for all racial/ethnic groups and hypertension control among Hispanic patients).
Existing literature on other patient populations also suggests wide state-level variation in diabetes, hypertension, and birthweight outcomes. For example, in 2008, Ezzati et al. documented between-state variation in uncontrolled hypertension using nationally representative survey data and found the highest rates of uncontrolled hypertension in areas such as DC, Mississippi, and Alabama, and the lowest rates in areas such as Vermont, Minnesota, and New Hampshire.32 Data from the CDC illustrate across-state variation in rates of low birthweight,8 while both CDC data and a study using Medicare claims have documented across-state variation in diabetes care.8,12 While state-level variation in outcomes has been documented in non-health center populations, we extend our findings to the health center population while also examining racial/ethnic disparities in outcomes.
Many factors may explain the observed variation in outcomes and disparities in outcomes between states. First, this may be a result of unmeasured patient complexity, such as differences in prevalence of comorbid conditions or social and behavioral risk factors. Variation may also be explained, in part, by differences in capacity and staffing in health centers, where health centers in some states may be better resourced to employ more clinicians, case managers, quality improvement specialists, and/or enabling service staff. Such staff can follow up with patients about their care regimens or better connect them to necessary social programs. Previous research suggests that there is wide variation in staffing, which may affect a centers’ ability to maximize quality and outcomes for all patients.16,17 Access to care outside of the health center, particularly to specialists, may also vary. Such variations may reflect underlying geographic variations in primary care physicians or specialists per capita18, Medicaid provider networks or network standards19, the extent of collaboration between health centers and local safety net or social service providers20, or the number and proximity of referral hospitals21. Though we adjust for distribution of uninsured patients in a health center, insurance status is also a strong determinant of access to services outside of health centers22, which may be especially important to diabetic and hypertensive patients. Whether or not a patient has insurance coverage is likely associated with Medicaid eligibility levels in a state, which vary widely. State spending on public health and social services also vary widely by state and may explain variations in outcomes.28,29 Finally, variations may be due to differences in patient trust or lack of adequate culturally competent services in some settings. This may apply particularly to populations that make up a small minority of patients, such as black patients in Maine or Hispanic patients in North Dakota. Better data and more research are needed to understand each of these hypothesized determinants.
Regardless of the underlying mechanism, our results have a number of important policy implications. First, though health centers on average have patient outcomes and disparities that are similar to or better than national averages, understanding the underlying variation is critical to maximizing outcomes for all health center patients. We may look to states where quality is high and/or disparities are low to better understand determinants of high quality. For example, New Hampshire exhibits amongst the highest rates of quality outcomes and lowest rates of racial/ethnic disparities in outcomes for health center patients. Better understanding how social policies, structural factors, and/or care delivery in this state positively affect quality may benefit lower-performing states.
HRSA may also wish to target funding and interventions to areas where quality is low and/or disparities are high. Currently, most HRSA quality awards are given to high performers, which may exacerbate geographic variations. Furthermore, HRSA may want to consider placing greater emphasis on rewarding health equity or reductions in health disparities. As of August 2016, only one of eight quality awards directly addressed disparities, known as Health Equity Advancers awards. These awards were given to health centers that “met or exceeded Healthy People 2020 goals by each race/ethnic group, or made marked advances in moving each race/ethnic group towards the Healthy People 2020 goals.”23 While this is important, such funding should be sustained and enhanced in future years given the persistent disparities observed. Furthermore, in alignment with HRSA’s goal of improving health equity24, HRSA may wish to target technical assistance and conduct targeted outreach to states and/or health centers where overall quality is low or disparities are high.
Our results may also motivate lower performing states to invest more in health center grant funding or better target the specific disease conditions in which they underperform. The percent of health center revenue that comes from state or local grant funds varies widely, from 1% in North Dakota to 23% in New Jersey in 2013.25 Given that direct state funding for health centers has experienced a decline since peaking in 2008—from $626 million in 2008 to $335 million in 201626—reinvesting these state funds, especially in lower performing states, could help maximize outcomes. As discussed by the National Association of Community Health Centers, the two most common uses of state health center funds include funding for (1) uncompensated care and (2) expanded access for underserved communities, including “longer clinic hours, a broader array of enabling services, [and] telemedicine.”26 Each of these uses may help improve outcomes in the state.
Ultimately, more research is needed to better understand determinants of quality and disparities within quality across states. Now that 92% of health centers use EHRs at all sites as of 201527, it may become easier for health centers to report more data by race/ethnicity, including patient characteristics and clinical measures, or to further stratify racial/ethnic outcomes by characteristics such as insurance status. This would better allow researchers and policymakers to assess adjusted differences in quality by race/ethnicity and to better understand determinants of outcomes.
Our study has several limitations. First, our findings are descriptive in nature and should be interpreted as such. Second, we were limited by our inability to adjust outcome measures by patient-level characteristics, given that individual-level data are unavailable. However, these measures are not adjusted in the reporting done by HRSA, nor by other entities such as the National Committee for Quality Assurance that collect analogous measures, and we improve these estimates by adjusting for facility-level patient characteristics. Third, because we examined state-level estimates, confidence intervals are wide for many states, though nearly all point estimates are statistically significant at a 95% confidence level due to the pooling of data across years. Fourth, for our unweighted disparities measures, by limiting analyses to centers reporting at least 20 patients in a denominator, we lose many health centers, yet still capture 70–97% of the patient population, depending on the measure. Fifth, while HRSA provides detailed guidance to health centers on measure reporting, measurement error certainly exists, though we have no reason to believe that the direction of error is consistent within a state. Additional limitations include small denominator sizes within some states, particularly for birthweight, and lack of other available quality measures by race/ethnicity that are related to the study outcomes.
Conclusions
We observed wide variation in health center patient outcomes and disparities in outcomes between states, for all races/ethnicities. Though health centers perform as well as other sites of care, on average, understanding the underlying variation is critical for targeting funding and interventions. Doing so will serve to maximize quality and equity for all health center patients. Further research will be important in better understanding state and facility-level factors associated with high levels of quality and low levels of disparities.
Supplementary Material
Supplemental Digital Content 1. Supplemental Appendix containing eTable 1 – eTable 11 and eFigure 1 – eFigure 4.
Acknowledgments
Disclosure of funding received for this work from any of the following organizations: National Institutes of Health (NIH); Wellcome Trust; Howard Hughes Medical Institute (HHMI); and any other(s): Funding for this work was provided by the Agency for Healthcare Research and Quality (Grant No. 1R36HS024652-01) and the Nora Kahn Prior Award.
Footnotes
Disclosure of potential conflicts of interest for all authors for the past three years, including an explicit statement that no potential conflicts exist when that is the case: Dr. Wilson discloses a small consulting relationship with Pfzier, for whom he organized a December 2016 meeting. Cole discloses past part-time employment with The Lewin Group (July 2013-June 2017). No other known conflicts exist.
Contributor Information
Megan B. Cole, Dept. of Health Law, Policy, & Management, Boston University School of Public Health, 715 Albany Street, Talbot 240W, Boston, MA 02118; Brown University School of Public Health, Dept. of Health Services, Policy, and Practice, 121 South Main Street, 7th Floor, Providence, RI 02912, Phone: 617-414-1306, Fax: 401-863-3489.
Ira B. Wilson, Brown University School of Public Health, Dept. of Health Services, Policy, and Practice, 121 South Main Street, 7th Floor, Providence, RI 02912, Phone: 401-863-9736, Fax: 401-863-3489.
Amal N. Trivedi, Brown University School of Public Health, Dept. of Health Services, Policy, and Practice, 121 South Main Street, 7th Floor, Providence, RI 02912, Phone: 401-863-9941, Fax: 401-863-3489.
References
- 1.Health Resources and Services Administration(HRSA) What is a health center? 2016 Available at: http://bphc.hrsa.gov/about/index.html. Accessed October 1, 2016.
- 2.HRSA. 2014 Health Center Data. 2016 Available at: http://bphc.hrsa.gov/uds/datacenter.aspx. Accessed March 2, 2016.
- 3.Shi L, Lebrun LA, Zhu J, et al. Clinical quality performance in U.S. health centers. Health Serv Res. 2012;47(6):2225–2249. doi: 10.1111/j.1475-6773.2012.01418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Politzer R, Yoon J, Shi L, et al. Inequality in America: the contribution of health centers in reducing and eliminating disparities in access to care. Med Care Res Rev. 2001;58(2):234–248. doi: 10.1177/107755870105800205. [DOI] [PubMed] [Google Scholar]
- 5.Shi L, Tsai J, Higgins PC, et al. Racial/ethnic and socioeconomic disparities in access to care and quality of care for US health center patients compared with non-health center patients. J Ambul Care Manage. 2009;32(4):342–250. doi: 10.1097/JAC.0b013e3181ba6fd8. [DOI] [PubMed] [Google Scholar]
- 6.Wright B, Potter A, Trivedi A. Federally Qualified Health Center use among dual eligibles: rates of hospitalizations and emergency department visits. Health Aff (Millwood) 2015;34(7):1147–1155. doi: 10.1377/hlthaff.2014.0823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lebrun LA, Shi L, Zhu J, et al. Racial/ethnic differences in clinical quality performance among health centers. J Ambul Care Manage. 2013;36(1):24–34. doi: 10.1097/JAC.0b013e3182473523. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention (CDC) Diabetes Report Card. Atlanta, GA: CDC; 2015. Available at: https://www.cdc.gov/diabetes/pdfs/library/diabetesreportcard2014.pdf. Accessed December 2, 2016. [Google Scholar]
- 9.Kaiser Family Foundation (KFF) Births of Low Birthweight as a Percent of All Births by Race/Ethnicity. Menlo Park, CA: KFF; 2014. Available at: http://kff.org/other/state-indicator/low-birthweight-by-raceethnicity/?currentTimeframe=0. Accessed December 2, 2016. [Google Scholar]
- 10.Kaiser Family Foundation. Percent of Adults Reporting Fair or Poor Health Status, by Race/Ethnicity. Menlo Park, CA: KFF; 2015. Available at: http://kff.org/other/state-indicator/percent-of-adults-reporting-fair-or-poor-health-status-by-raceethnicity/?currentTimeframe=0. Accessed December 2, 2016. [Google Scholar]
- 11.Kang-Kim M, Betancourt JR, Ayanian JZ, et al. Access to care and use of preventative services by Hispanics: state-based variations from 1991 to 2004. Medical Care. 2008;46(5):507–515. doi: 10.1097/MLR.0b013e31816dd966. [DOI] [PubMed] [Google Scholar]
- 12.Arday DR, Fleming BB, Keller DK, et al. Variation in diabetes care among states. Diabetes Care. 2002;25(12):2230–2237. doi: 10.2337/diacare.25.12.2230. [DOI] [PubMed] [Google Scholar]
- 13.Drye E, Normand ST, Wang Y, et al. Comparison of hospital risk-standardized mortality rates using in-hospital and 30-day models: implications for hospital profiling. Ann Intern Med. 2012;156(1 Pt 1):19–26. doi: 10.1059/0003-4819-156-1-201201030-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agency for Healthcare Research and Quality. How CMS measures the “30-day all cause rehospitalization rate” on the hospital compare web site. Rockville, MD: AHRQ; 2013. Mar, Available from: http://www.ahrq.gov/professionals/systems/hospital/red/toolkit/redtool-30day.html. Accessed September 2, 2016. [Google Scholar]
- 15.Trivedi AN, Zaslavsky AM, Schneider EC, et al. Relationship between quality of care and racial disparities in Medicare health plans. JAMA. 2006;296(16):1998–2004. doi: 10.1001/jama.296.16.1998. [DOI] [PubMed] [Google Scholar]
- 16.Wells R, Punekar RS, Vasey J. Why do some health centers provide more enabling services than others? J Health Care Poor Underserved. 2009;20(2):507–523. doi: 10.1353/hpu.0.0151. [DOI] [PubMed] [Google Scholar]
- 17.National Association of Community Health Centers. Highlighting the role of enabling services at community health centers. 2010 Available from: http://nachc.org/wp-content/uploads/2015/06/EnablingServicesReport.pdf. Accessed September 24, 2016.
- 18.Goodman DC, Brownlee S, Chang C, et al. Regional and Racial Variation in Primary Care and the Quality of Care among Medicare Beneficiaries. The Dartmouth Atlas. 2010 Sep; Available from: http://www.dartmouthatlas.org/downloads/reports/Primary_care_report_090910.pdf. Accessed December 12, 2016. [PubMed]
- 19.Office of Inspector General, Dept. of Health and Human Services. State standards for access to care in Medicaid managed care. 2014 Available at: https://oig.hhs.gov/oei/reports/oei-02-11-00320.pdf. Accessed December 12, 2016.
- 20.HRSA. Program Assistance Letter. 2010 Nov; Available from: https://bphc.hrsa.gov/programrequirements/pdf/pal201102.pdf. Accessed December 12, 2016.
- 21.HRSA. Health Center Program Compliance Manual, Chapter 8. 2016 Available from: https://bphc.hrsa.gov/programrequirements/pdf/healthcentercompliancemanual.pdf. Accessed December 12, 2016.
- 22.Cook NL, Hicks LS, O’Malley AJ, et al. Access to specialty care and medical services in community health centers. Health Aff (Millwood) 2007;26(5):1459–1468. doi: 10.1377/hlthaff.26.5.1459. [DOI] [PubMed] [Google Scholar]
- 23.HRSA. Quality Improvement Awards – Frequently Asked Questions. 2016 Available from: https://bphc.hrsa.gov/programopportunities/fundingopportunities/quality/qia_faqs_for_website_final.pdf.
- 24.HRSA. Strategic Plan, Goal 4: Improve Health Equity. 2016 Mar; Available from: https://www.hrsa.gov/about/strategicplan/goal4.html. Accessed December 12, 2016.
- 25.Kaiser Family Foundation (KFF) Distribution of Revenue by Source for Federally-Funded Federally Qualified Health Centers. 2013 Available from: http://kff.org/other/state-indicator/fqhc-revenue-by-source/?currentTimeframe=0. Accessed December 12, 2016.
- 26.National Association of Community Health Centers. State Funding for Community Health Centers (Fiscal Year 2016) 2016 Mar; Available from: http://nachc.org/wp-content/uploads/2015/10/funding-brief-3-21-16.pdf. Accessed December 12, 2016.
- 27.HRSA. 2015 Health Center Data – Health Center Program Grantee Data. 2016 Available from: https://bphc.hrsa.gov/uds/datacenter.aspx. Accessed December 12, 2016.
- 28.Trust for America’s Health and the Robert Wood Johnson Foundation. Investing in America’s Health: A State-by-State Look At Public Health Funding And Key Health Facts. 2014 Available from: http://healthyamericans.org/assets/files/TFAH2014-InvestInAmericaRpt08.pdf. Accessed May 2, 2017.
- 29.Bradley EH, Canavan M, Rogan E, et al. Variation in health outcomes: the role of spending on social services, public health, and health care, 2000–09. Health Aff (Millwood) 2016;35(5):760–768. doi: 10.1377/hlthaff.2015.0814. [DOI] [PubMed] [Google Scholar]
- 30.CDC. Health Disparities. 2015 Available from: https://www.cdc.gov/healthyyouth/disparities/. Accessed May 2, 2017.
- 31.Keppel K, Pamuk E, Lynch J, et al. Methodological issues in measuring health disparities. Vital Health Stat 2. 2005;(141):1–16. [PMC free article] [PubMed] [Google Scholar]
- 32.Ezzati M, Oza S, Danaei G, Murray CJL. Trends and cardiovascular mortality effects of state-level blood pressure and uncontrolled hypertension in the United States. Circulation. 2008;117(7):905–914. doi: 10.1161/CIRCULATIONAHA.107.732131. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content 1. Supplemental Appendix containing eTable 1 – eTable 11 and eFigure 1 – eFigure 4.


