Abstract
Mode of delivery (vaginal or cesarean section) is thought to affect gut microbiota, which in turn may affect psychological well-being. As such, mode of delivery is potentially a modifiable factor for psychological well-being. Here we examined the association of mode of delivery with child and adolescent psychological well-being. We used multivariable linear regression in a population-representative Hong Kong Chinese birth cohort, “Children of 1997,” to examine the adjusted associations of mode of delivery with behavioral problems assessed from parent-reported Rutter score at ~7 (n = 6294) and ~11 years (n = 5598), self-esteem assessed from self-reported Culture-Free Self-Esteem Inventory score at ~11 years (n = 6937) and depressive symptoms assessed from self-reported Patient Health Questionnaire-9 score at ~13 years (n = 5797). Cesarean Section (CS) was associated with children born in private hospitals, boys, and firstborns, higher maternal body mass index, higher maternal age, preeclampsia, higher socioeconomic position (SEP) and maternal birth in Hong Kong. CS was unrelated to behavior, self-esteem and depressive symptoms adjusted for infant characteristics (sex, gestational age, birthweight, parity and breast feeding), maternal characteristics (mother’s age and place of birth) and SEP. In a developed non-Western setting, mode of delivery was not clearly associated with childhood or early adolescent psychological well-being.
Introduction
Childhood psychological well-being is a growing concern in public health as mental health issues often emerge in adolescence and extend throughout adulthood with many other related adverse effects affecting health and social functioning. Cesarean section (CS) is a potentially modifiable factor that may be associated with the child’s psychological well-being. A growing body of evidence suggests that mode of delivery affects the infant’s gut microbiota. Infants born vaginally acquire gut microbiota from the maternal vaginal and fecal microbiota while infants born by CS acquire their gut microbiota from the environment1. Infants born vaginally initially have more microbes from the Firmicutes family and fewer from the Bacteroidetes family2–4. Although gut microbiota eventually normalize5, early life is a sensitive period when exposures may have lifelong consequences. Children born via CS have a higher risk of allergies6, asthma7 and diabetes8 later in life, with differences in gut microbiota during early life as a possible explanation. Gut microbiota are also associated with psychological well-being, through neural, endocrine and immune pathways, i.e., the gut-brain axis, which may affect brain function and behavior9. The idea that the gut could affect psychological well-being has been recognized since the middle of the nineteenth century and is generally accepted in the biological sciences10, and has been shown in several animal studies11–13.
The association of mode of delivery with cognitive development has previously been examined, with no association found for intelligence14,15 or cognitive delay15, and inconsistent associations for behavioral disorders16–20 and autistic spectrum disorder (ASD)21,22. Two recent Swedish cohort studies reported associations of CS with higher risk of ASD and psychosis, but the lack of associations in the sibling-matched analyses indicated that the observations were likely due to unmeasured genetic and environmental (i.e., differences in gut microbiota at birth) factors21,23. Another Swedish sibling-matched study found that birth by CS was associated with higher risk of attention-deficit/hyperactivity disorder (ADHD), but only elective CS had positive sibling associations, thus also implying that findings were confounded18. Curran et al. (2015) reported null associations of mode of delivery with ADHD and ASD in the Millennium Cohort in the United Kingdom19. However, the association of mode of delivery with other indicators of psychological well-being, as self-esteem during childhood and adolescent depressive symptoms during early adolescence has not, to our knowledge, previously been examined. CS rates tend to be higher than recommended by the World Health Organization (WHO) and thus represent a modifiable intervention target. To clarify the role of mode of delivery in psychological well-being, we examined prospectively in a large population-representative birth cohort, Hong Kong’s “Children of 1997,” the association of mode of delivery with child and adolescent psychological well-being, including measures of behavior, self-esteem, and depressive symptoms.
Results
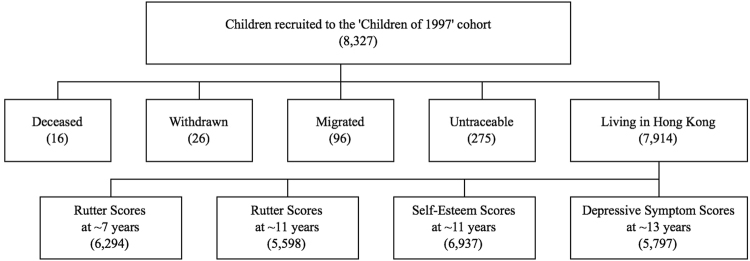
As shown in Fig. 1, of the original 8,327 cohort participants, as of December 2013, 16 (0.2%) were known to have died, 26 (0.3%) had permanently withdrawn, 96 (1.2%) were known to have migrated and 275 (3.3%) were untraceable, probably migrated, whereas 7,914 (95%) remained living in Hong Kong. Of these, 6,294 (80% follow-up) had parent-reported Rutter scores at ~7 years and 5,598 (71% follow-up) at ~11 years, 6,937 (88% follow-up) had self-reported self-esteem scores at ~11 years and 5,797 (73%) had depressive symptom scores at ~13 years.
Figure 1.
Hong Kong’s ‘Children of 1997’ birth cohort recruitment and follow-up (numbers) as of December 2013.
About a quarter of the births were CSs (26.8%), 56.6% were unassisted vaginal birth and 16.6% assisted vaginal birth (Table 1). Private hospitals had higher rates of CS (48%) than public hospitals (18%). CS was positively associated with male sex, being firstborn, no breastfeeding, higher maternal BMI, higher maternal age, preeclampsia, higher SEP (parental education, occupation and household income at birth) and a Hong Kong-born mother.
Table 1.
Baseline Characteristics by Mode of Delivery in Hong Kong’s “Children of 1997” Birth Cohort.
| Characteristics | N | Model of Delivery | |
|---|---|---|---|
| Vaginal % (n = 5,815) | Cesarean % (n = 2,143) | ||
| Birth hospital | |||
| Public | 5,430 | 79.6 | 48.4 |
| Private | 2,190 | 20.4 | 51.6 |
| Infant characteristics | |||
| Sex | |||
| Girl | 3,769 | 48.3 | 44.9 |
| Boy | 4,189 | 51.8 | 55.1 |
| Birthweight (in grams) | |||
| Mean (SD) | — | 3,200 (400) | 3,200 (500) |
| Gestational age (in weeks) | |||
| Mean (SD) | — | 39.1 (1.5) | 38.9 (1.8) |
| Parity | |||
| 1 | 3,778 | 44.8 | 55.0 |
| 2 | 3,287 | 43.1 | 36.8 |
| 3 or above | 878 | 12.1 | 8.3 |
| Breastfeeding | |||
| Never breastfed | 4,518 | 54.4 | 63.3 |
| Partially breastfed | 2,954 | 38.6 | 33.3 |
| Exclusively breastfed for ≥3 months | 483 | 7.0 | 3.5 |
| Maternal characteristics | |||
| Mother’s birthplace | |||
| Hong Kong | 4,708 | 58.0 | 72.8 |
| Non-Hong Kong | 2,879 | 42.0 | 27.2 |
| Maternal age at birth (in years) | |||
| ≤24 | 990 | 14.7 | 6.5 |
| 25–29 | 2,470 | 34.0 | 23.7 |
| 30–34 | 3,023 | 36.1 | 43.6 |
| ≥35 | 1,441 | 15.2 | 26.3 |
| Maternal BMI | |||
| Mean (SD) | — | 22.4 (3.2) | 23.1 (3.4) |
| Gestational diabetes | |||
| Yes | 382 | 6.5 | 7.1 |
| No | 5353 | 93.5 | 92.9 |
| Preeclampsia | |||
| Yes | 279 | 4.4 | 6.2 |
| No | 5457 | 95.6 | 93.8 |
| Family SEP at birth | |||
| Highest parental education | |||
| Grade 9 or below | 2,392 | 32.7 | 23.2 |
| Grade 10–11 | 3,388 | 42.7 | 42.5 |
| Grade 12 or above | 2,161 | 24.6 | 34.4 |
| Highest parental occupationa | |||
| I (professional) | 1,684 | 22.8 | 29.4 |
| II (managerial) | 1,094 | 14.5 | 20.0 |
| IIINM (non-manual skilled) | 1,990 | 29.3 | 28.5 |
| IIIM (manual skilled) | 1,145 | 18.8 | 11.3 |
| IV (semi-skilled) | 696 | 11.2 | 7.6 |
| V (unskilled) | 226 | 3.4 | 3.2 |
| Household income, dollarsb [mean (SD)]a | |||
| 1st quintile [1,791 (432)] | 1,358 | 21.9 | 12.9 |
| 2nd quintile [2,913 (331)] | 1,403 | 22.0 | 15.2 |
| 3rd quintile [4,434 (538)] | 1,397 | 20.0 | 20.2 |
| 4th quintile 6,906 (887)] | 1,394 | 18.4 | 24.4 |
| 5th quintile [15,057 (15,852)] | 1,418 | 17.8 | 27.3 |
Abbreviation: HK, Hong Kong; n, number; SD, standard deviation; SEP, socioeconomic position.
aAt recruitment.
bIn Hong Kong dollars (HK $7.80 = US $1.
Table 2 shows that mode of delivery was not associated with Rutter score or its subscores in any model. Mode of delivery was not associated with overall self-esteem, or most of its subscores, but was associated with lower social self-esteem. Mode of delivery was not associated with depressive symptoms in any model.
Table 2.
Adjusteda Associations of Mode of Delivery with Psychological Well-Being in Hong Kong’s “Children of 1997” Birth Cohort (Multiple Imputation).
| Psychological Well-Being | Model 1a | Model 2b | Model 3c | ||||
|---|---|---|---|---|---|---|---|
| Vaginal Delivery | Cesarean | Vaginal Delivery | Cesarean | Vaginal Delivery | Cesarean | ||
| β | β (95% CI) | β | β (95% CI) | β | β (95% CI) | ||
| Rutter scores at ~7 years | (n = 6,294) | ||||||
| Total | Ref | −0.30 (−0.63, 0.03) | Ref | −0.29 (−0.64, 0.05) | Ref | −0.27 (−0.63, 0.08) | |
| Conduct | Ref | −0.03 (−0.10, 0.04) | Ref | −0.02 (−0.10, 0.05) | Ref | −0.02 (−0.10, 0.06) | |
| Emotional | Ref | 0.02 (−0.05, 0.08) | Ref | −0.04 (−0.11, 0.03) | Ref | −0.04 (−0.12, 0.03) | |
| Hyperactivity | Ref | −0.11 (−0.20, −0.03) | Ref | −0.08 (−0.17, 0.01) | Ref | −0.08 (−0.17, 0.02) | |
| Rutter scores at ~11 years | (n = 5,598) | ||||||
| Total | Ref | −0.13 (−0.48, 0.22) | Ref | −0.03 (−0.40, 0.34) | Ref | −0.01 (−0.39, 0.38) | |
| Conduct | Ref | −0.01 (−0.09, 0.07) | Ref | 0.01 (−0.07, 0.09) | Ref | 0.02 (−0.07, 0.10) | |
| Emotional | Ref | 0.05 (−0.03, 0.12) | Ref | 0.0002 (−0.08, 0.08) | Ref | −0.01 (−0.09, 0.08) | |
| Hyperactivity | Ref | −0.09 (−0.18, 0.001) | Ref | −0.02 (−0.11, 0.07) | Ref | −0.02 (−0.12, 0.08) | |
| Self-esteem scores | (n = 6,937) | ||||||
| Overall | Ref | 0.54 (0.14, 0.95) | Ref | −0.24 (−0.65, 0.18) | Ref | −0.36 (−0.78, 0.07) | |
| General | Ref | 0.19 (0.003, 0.37) | Ref | −0.11 (−0.30, 0.09) | Ref | −0.15 (−0.35, 0.05) | |
| Social | Ref | −0.22 (−0.30, −0.13) | Ref | −0.13 (−0.24, −0.02) | Ref | −0.12 (−0.23, −0.01) | |
| Academic | Ref | 0.20 (0.10, 0.31) | Ref | 0.03 (−0.08, 0.14) | Ref | −0.02 (−0.13, 0.09) | |
| Parent-related | Ref | 0.14 (0.03, 0.25) | Ref | −0.03 (−0.14, 0.08) | Ref | −0.06 (−0.18, 0.05) | |
| Depressive symptoms | (n = 5,797) | ||||||
| PHQ-9 scores | Ref | −0.05 (−0.25, 0.14) | Ref | 0.08 (−0.13, 0.29) | Ref | 0.15 (−0.06, 0.37) | |
Abbreviation: HK, Hong Kong; CI, confidence interval; Ref, reference.
aAdjusted for sex, age at assessment and survey mode (PHQ-9 scores).
bAdditionally adjusted for highest parental education, parental occupation, household income per head, mother’s birthplace and birth hospital.
cAdditionally adjusted for birthweight, gestational age, parity, maternal age, maternal BMI, gestational diabetes and preeclampsia.
Table 3 shows that results were generally similar considering vaginal birth as unassisted and assisted. In a fully adjusted model (Model 3), CS compared to unassisted or assisted vaginal delivery was associated with lower social self-esteem. Results from a complete case analysis were similar (see Supplementary Tables S1 and S2).
Table 3.
Adjusteda Association of Mode of Delivery Separated by Unassisted and Assisted Vaginal Delivery with Psychological Well-Being in Hong Kong’s “Children of 1997” Birth Cohort (Multiple Imputation)
| Psychological Well-Being | Model 1a, b | Model 2a, c | Model 3a. d | |||
|---|---|---|---|---|---|---|
| Assisted Vaginal Delivery | Cesarean | Assisted Vaginal Delivery | Cesarean | Assisted Vaginal Delivery | Cesarean | |
| β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) | |
| Rutter scores at ~7 years (n = 6,294) | ||||||
| Total | 0.03 (−0.38, 0.43) | −0.29 (−0.63, 0.05) | 0.08 (−0.34, 0.50) | −0.27 (−0.63, 0.10) | −0.12 (−0.55, 0.31) | −0.31 (−0.68, 0.07) |
| Conduct | −0.07 (−0.16, 0.02) | −0.04 (−0.12, 0.03) | −0.05 (−0.14, 0.04) | −0.04 (−0.12, 0.04) | −0.10 (−0.19, −0.003) | −0.05 (−0.13, 0.03) |
| Emotional | 0.09 (0.01, 0.18) | 0.04 (−0.03, 0.11) | 0.05 (−0.04, 0.13) | −0.02 (−0.10, 0.05) | 0.003 (−0.09, 0.09) | −0.04 (−0.12, 0.04) |
| Hyperactivity | −0.05 (−0.16, 0.05) | −0.13 (−0.22, −0.04) | 0.001 (−0.11, 0.11) | −0.08 (−0.18, 0.01) | −0.03 (−0.14, 0.08) | −0.09 (−0.19, 0.01) |
| Rutter scores at ~11 years (n = 5,598) | ||||||
| Total | −0.26 (−0.69, 0.17) | −0.20 (−0.57, 0.16) | −0.13 (−0.56, 0.31) | −0.07 (−0.47, 0.32) | −0.28 (−0.73, 0.17) | −0.11 (−0.52, 0.30) |
| Conduct | −0.03 (−0.12, 0.06) | −0.02 (−0.10, 0.06) | −0.002 (−0.10, 0.09) | 0.004 (−0.08, 0.09) | −0.04 (−0.14, 0.06) | 0.001 (−0.09, 0.09) |
| Emotional | 0.03 (−0.06, 0.12) | 0.06 (−0.02, 0.14) | −0.01 (−0.10, 0.09) | −0.002 (−0.09, 0.08) | −0.03 (−0.13, 0.07) | −0.01 (−0.10, 0.08) |
| Hyperactivity | −0.14 (−0.24, −0.03) | −0.12 (−0.22, −0.03) | −0.06 (−0.17, 0.05) | −0.04 (−0.14, 0.06) | −0.08 (−0.19, 0.04) | −0.05 (−0.15, 0.05) |
| Self-esteem scores (n = 6,937) | ||||||
| Overall | 1.42 (0.93, 1.90) | 0.87 (0.45, 1.28) | 0.51 (0.02, 1.00) | −0.10 (−0.53, 0.34) | 0.29 (−0.21, 0.80) | −0.27 (−0.73, 0.18) |
| General | 0.57 (0.35, 0.80) | 0.32 (0.13, 0.51) | 0.24 (0.01, 0.47) | −0.04 (−0.24, 0.16) | 0.15 (−0.09, 0.38) | −0.11 (−0.32, 0.11) |
| Social | 0.17 (0.05, 0.29) | 0.05 (−0.05, 0.16) | −0.002 (−0.13, 0.12) | −0.13 (−0.24, −0.02) | −0.002 (−0.13, 0.13) | −0.12 (−0.24, −0.004) |
| Academic | 0.39 (0.26, 0.52) | 0.29 (0.18, 0.40) | 0.19 (0.06, 0.32) | 0.08 (−0.03, 0.20) | 0.11 (−0.02, 0.25) | 0.01 (−0.11, 0.13) |
| Parent-related | 0.28 (0.15, 0.41) | 0.20 (0.09, 0.31) | 0.08 (−0.05, 0.21) | −0.01 (−0.13, 0.10) | 0.04 (−0.10, 0.18) | −0.06 (−0.18, 0.06) |
| Depressive symptoms (n = 5,797) | ||||||
| PHQ-9 scores | −0.26 (−0.50, −0.02) | −0.11 (−0.31, 0.09) | −0.15 (−0.40, 0.09) | 0.04 (−0.17, 0.26) | −0.09 (−0.34, 0.16) | 0.13 (−0.10, 0.35) |
Abbreviation: HK, Hong Kong; CI, confidence interval
aReference group: Unassisted vaginal delivery.
bAdjusted for sex, age at assessment and survey mode (PHQ-9 scores).
cAdditionally adjusted for highest parental education, parental occupation, household income per head, mother’s birthplace and birth hospital.
dAdditionally adjusted for birthweight, gestational age, parity, maternal age, maternal BMI, gestational diabetes and preeclampsia.
Discussion
In this large, population-representative birth cohort from the developed non-Western setting of Hong Kong, consistent with one of two previous studies16, mode of delivery was not associated with child or adolescent behavior. Our study adds by showing CS was also not associated with depressive symptoms or overall self-esteem in adolescence, although CS was perhaps associated with lower social self-esteem.
“Children of 1997” is a large, population-representative birth cohort from a unique setting; nevertheless, our study has limitations. First, type of delivery was obtained by parent-report (mostly mothers), as opposed to clinical records, which could introduce measurement error. However, type of delivery was obtained shortly after delivery and is quite memorable. Second, screening tools were used to assess behavioral problems, self-esteem, and depressive symptoms as opposed to clinical diagnosis. However, these questionnaires have been validated in Chinese populations24–26, and our large sample size compensates for any lack of precision. Third, difficult and stressful births can lead to hypoxia and asphyxia resulting in neonatal encephalopathy and long-term neurodevelopmental impairments27. We do not know whether this occurred for any specific type of delivery. Fourth, we have no information regarding analgesic use during the prenatal and perinatal periods. Analgesic exposure during the fetal or neonatal period has been found to be associated with changes to the brain in animal studies28,29. However, no association has been found between obstetric anesthetic techniques and behavior or long-term neurodevelopmental outcomes in humans30. Fifth, we did not have data differentiating whether CS was elective or emergency. Infants born via emergency CS are typically exposed to the mother’s vaginal flora, as compared to elective CS, where infants are not20. A recent study reported that emergency CS, compared to spontaneous vaginal delivery, was associated with delayed gross motor function at 9 months and null associations across various modes of delivery with cognitive and motor development at 3 years20. However, there are no studies examining the longer term effects of emergency CS with psychological well-being. Finally, given the large number of associations examined, any positive associations might be false positives due to multiple comparisons and need to be confirmed in future studies.
Our study is not consistent with a link between gut microbiota, established early in life, and psychological well-being. In adults, probiotics, of the Lactobacillus or Bifidobacterium genera31–33, may have a role in the treatment of depression, as seen in some preliminary randomized controlled trials31,32. Differences may have occurred for a number of reasons. Mode of delivery may affect proportions of bacteria from the Firmicutes and Bacteroidetes families, but may only be associated with short-term differences in gut microbiota, rather than representing differences that continue into adolescence, although early life is a key phase for neurological development. Alternatively, any effects of events at birth may operate via different mechanisms, such as cortisol from a stress response34–36 leading to child behavioral problems. For example, Li et al. (2011) found elective cesarean delivery associated with fewer behavioral and emotional problems compared to unassisted vaginal delivery while assisted vaginal delivery was associated with more problems17. However, we found no associations of assisted vaginal delivery with behavioral problems. Furthermore, Li et al. (2011) did not examine the differences between the implications for CS, thereby not allowing further examination of how cortisol may mediate the pathway between mode of delivery and psychological well-being.
Mode of delivery does not appear to be associated with the psychological well-being of children and adolescents. However, a clearer understanding of the long-term effects of mode of delivery on gut microbiota will help elucidate the impact of CS on health, delineate any possible pathways involving the gut-brain-axis and identify where modification of gut microbiota in infants could potentially be beneficial.
Methods
Ethics Statement
Since our participants are children, informed consent was obtained from the parents, next of kin, caretakers or guardians (informants) on behalf of the participants by completing the questionnaire at enrollment as approved by The University of Hong Kong Medical Faculty Ethics Committee. Ethical approval for further studies was obtained from the University of Hong Kong-Hospital Authority Hong Kong West Cluster, Joint Institutional Review Board and/or the Ethics Committee of the Department of Health, Government of the Hong Kong SAR as appropriate. All methods were performed in accordance with the relevant guidelines and regulations.
Participants
The Hong Kong “Children of 1997” birth cohort is a population representative Chinese birth cohort (n = 8,327) that covered 88.0% of all births in Hong Kong from April 1, 1997 to May 31, 1997, and has been described in detail elsewhere37. The study was initially established to investigate the effects of secondhand smoke exposure on infant health. Families were recruited at the first postnatal visit to one of the 49 Maternal and Child Health Centers (MCHCs) in Hong Kong, which parents of all newborns were encouraged to attend. Characteristics obtained using a self-administered questionnaire in Chinese at recruitment and subsequent routine visits included maternal characteristics (mother’s birthplace and age at birth), infant characteristics (type of delivery, type of birth hospital, sex, gestational age, birth weight, parity and breastfeeding) and socioeconomic position (SEP).
Passive follow-up via record linkage was instituted in 2005 to obtain routinely collected information including bi-annual assessments of emotional and behavioral problems using the Revised Parent’s Rutter Scales in Chinese (grade 2, 4 and 6 (i.e., ages 7-8, 9-10 and 11-12 years)) and self-esteem using Form A of the Culture-Free Self-Esteem Inventories for Children by Battle in Chinese (grade 4 (age 9-10 years) onwards) from the Student Health Service, Department of Health, which provides free annual check-ups for all school students. Active follow-up via direct contact was instituted in 2007, including postal surveys. Maternal height and weight, gestational diabetes and preeclampsia were obtained from surveys I (conducted in 2008 and 2009) and III (conducted in 2011 and 2012). Survey II, including the Patient Health Questionnaire-9 (PHQ-9), was first sent in February 2010 then re-sent a second and third time as necessary over the following 5 months. Non-responses were followed-up via two-waves of telephone interviews from November 2010 to April 2011 and from July 2011 to June 2012 and during pilot studies for in-person follow-up (June to August 2011 and June to August 2012). The study obtained ethical approval from the University of Hong Kong-Hospital Authority Hong Kong West Cluster Joint Institutional Review Board.
Exposures
Mode of delivery was categorized as vaginal delivery or CS. Mode of delivery was obtained from the baseline survey completed by the primary caregiver (typically the mother). Mode of delivery was recorded as normal vaginal birth without instrumentation, vaginal birth with suction or forceps or CS. We considered vaginal births together (including unassisted and assisted vaginal delivery). Given that unassisted and assisted vaginal deliveries would be expected to have the same effect on gut microbiota, we also classified mode of delivery as unassisted vaginal delivery, assisted vaginal delivery or CS to check whether any associations were specific to CS. We did not collect information on the possible indications for CS or whether the CS was primary versus repeat.
Outcomes
Emotional and behavioral problems
Emotional and behavioral problems at ~7 years (6- <9 years) and ~11 years (9- <13 years) were assessed from the Revised Parent’s Rutter Scales in Chinese for parents25,38. The scales consist of a set of 31 items describing emotional and behavioral difficulties, with each item scored 0 for does not apply, 1 for applies somewhat or 2 for certainly applies. A total score (range 0–62) and subscores for conduct problems (5 items, range 0–10), emotional problems (5 items, range 0–10) and inattention/hyperactivity (3 items, range 0–6) were calculated, where a higher score indicated more emotional and behavioral problems. When considering the presence of emotional and behavioral problems, a total score of 13 or more was considered as overall emotional and behavioral problems39. Presence of conduct problems, emotional problems or hyperactivity was defined as having the corresponding subscore above the sex-specific 97th percentile (≥5 for boys and ≥4 for girls for conduct, ≥4 for boys and ≥4 for girls for emotion, 6 for boys and ≥5 for girls for hyperactivity) for this population.
Self-esteem
Self-esteem at ~11 years (9- <13 years) was assessed from the Form A of the Culture-Free Self Esteem Inventories (SEI) in Chinese for children40. Assessment inventories developed in Western countries may be less valid in non-Western settings. However, the items of the SEI were chosen with concern for content that is least sensitive to change across cultures41. The SEI has good validation in assessing self-esteem in adolescents and has been used in Hong Kong Chinese42. Responses are of the forced-choice variety that the respondent checks either “yes” or “no” for each item. A total score (range 0–50) and subscores for general self-esteem (perception of self-worth in general) (20 item, range 0–20), social self-esteem (perception of quality of relationships with peer) (10 items, range 0–10), academic self-esteem (perception of ability to academic success) (10 items, range 0–10), and parent-related self-esteem (perception of status at home) (10 items, range 0–10) were calculated, where a lower score indicated lower self-esteem. Based on the findings from the same study, we excluded unreliable scores with a lie scale of 2 or less (n = 158), although a lie scale of 5 or more had been used to indicate a lack of defensiveness and a reliable self-esteem inventories40. Presence of low self-esteem was defined as having a total score of 19 or less40. Each subscale score can be classified into one of five categories (‘very low,’ ‘low,’ ‘intermediate,’ ‘high’ or ‘very high’). A ‘very low’ subscale score indicated low self-esteem in the respective subscale category (≤7 for general self-esteem and ≤2 for social, academic and parent-related self-esteem)40.
Depressive symptoms
Depressive symptoms at ~13 years (12- ≤15 years) were assessed from the PHQ-943 in Chinese. The PHQ-9 scale has good sensitivity and specificity in detecting depression in youth44, is an effective screening tool for the risk of depression among adolescents45 and has been validated in Chinese adolescents46. The scales consist of a set of 9 items describing symptoms and functional impairment, with each item scored 0 for not at all, 1 for several days, 2 for more than half the days or 3 for nearly everyday. A total PHQ-9 score (range 0–27) was calculated, where a higher score indicated more depressive symptoms. Presence of PHQ-9 Major Depressive Disorder was defined as having a total score of 11 or more mapping on the DSM-IV-TR44.
Statistical analysis
We used multivariable linear regression to estimate the adjusted associations of mode of delivery with Rutter, SEI and depressive symptom scores from which estimated beta-coefficients with 95% confidence intervals (CIs) are presented. We adjusted for potential confounders, which are presented in three models. Model 1 adjusted for sex, age at assessment and survey mode for depressive symptoms since for PHQ-9 was obtained by postal questionnaire, telephone interview and in-person interview. Model 2 additionally adjusted for SEP (highest parental education at birth, highest parental occupation at birth and monthly household income per head at birth), mother’s birthplace and birth hospital. Model 3 additionally adjusted for birth weight, gestational age, parity, maternal age, maternal body mass index (BMI), gestational diabetes and preeclampsia.
Among the 7,681 birth cohort members included, 3.6% were missing mode of delivery. Overall, 13.2% of data points were missing, mainly maternal BMI (58.8% missing) and gestational diabetes (23.6%) because these were obtained from Survey I or Survey III. We used multiple imputation to predict missing values of exposures and confounders incorporating data on the primary outcomes (Rutter, SEI and PHQ-9 scores), exposures (mode of delivery), confounders and other factors potentially associated with mode of delivery based on a flexible additive regression model with predictive mean matching47 as multiple imputation is the gold standard in this situation48. We used the ‘Hmisc’ package in R 3.0.1 (R Development Care Team, Vienna, Austria) for the multiple imputation. We summarized the results from 20 imputed datasets into single estimated beta-coefficients with CIs adjusted for missing data uncertainty. The results were based off 20 imputations due to fraction of missing information (γ) and the preventable power falloff of less than 1%. We also performed a complete case analysis for comparison using Stata version 10 (Stata Corp, College station, Texas).
Data Availability
Data are available upon request from the “Children of 1997” data access committee: aprmay97@hku.hk.
Electronic supplementary material
Acknowledgements
The authors thank colleagues at the Student Health Service and Family Health Service of the Department of Health for their assistance and collaboration. They also thank the late Dr. Connie O for coordinating the project and all the fieldwork for the initial study in 1997–8. This work is a sub-study of the “Children of 1997” birth cohort which was initially supported by the Health Care and Promotion Fund, Health and Welfare Bureau, Government of the Hong Kong SAR [HCPF Grant #216106]. Since 2005, the “Children of 1997” birth cohort has been funded by the Health and Health Services Research Fund [HHSRF Grant #03040771], Government of the Hong Kong SAR, the Research Fund for the Control of Infectious Diseases [RFCID Grant #04050172], Government of the Hong Kong SAR and the University Research Committee Strategic Research Theme (SRT) of Public Health, The University of Hong Kong. This sub-study was funded by the Health and Health Services Research Fund [HHSRF Grant #07080751], Government of the Hong Kong SAR.
Author Contributions
C.Y.L. performed the literature review, conducted data analysis, interpreted findings and drafted the manuscript. C.M.S. conceptualized ideas, designed and directed analytic strategy, interpreted findings, revised drafts of the manuscript and supervised the study from conception to completion. G.M.L. and C.M.S. resurrected the birth cohort. All authors have read and approved the submission of the manuscript; the manuscript has not been published and is not being considered for publication elsewhere, in whole or in part, in any language, except as an abstract. C.Y.L. also thanks the University Grants Committee for funding her research through the Hong Kong PhD Fellowship Scheme.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-017-15810-x.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gronlund MM, Lehtonen OP, Eerola E, Kero P. Fecal microflora in healthy infants born by different methods of delivery: permanent changes in intestinal flora after cesarean delivery. J. Pediatr. Gastroenterol. Nutr. 1999;28:19–25. doi: 10.1097/00005176-199901000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Lin SL, Leung GM, Schooling CM. Mode of delivery and adiposity: Hong Kong’s “Children of 1997” birth cohort. Ann. Epidemiol. 2013;23:693–699. doi: 10.1016/j.annepidem.2013.06.090. [DOI] [PubMed] [Google Scholar]
- 3.Biasucci G, et al. Mode of delivery affects the bacterial community in the newborn gut. Early Hum. Dev. 2010;86:S13–S15. doi: 10.1016/j.earlhumdev.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 4.Salminen S, Gibson GR, McCartney AL, Isolauri E. Influence of mode of delivery on gut microbiota composition in seven year old children. Gut. 2004;53:1388–1389. doi: 10.1136/gut.2004.041640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moloney RD, Desbonnet L, Clarke G, Dinan TG, Cryan JF. The microbiome: stress, health and disease. Mamm. Genome. 2014;25:49–74. doi: 10.1007/s00335-013-9488-5. [DOI] [PubMed] [Google Scholar]
- 6.Cho CE, Norman M. Cesarean section and development of the immune system in the offspring. Am. J. Obstet. Gynecol. 2013;208:249–254. doi: 10.1016/j.ajog.2012.08.009. [DOI] [PubMed] [Google Scholar]
- 7.Relman DA. The human microbiome: ecosystem resilience and health. Nutr. Rev. 2012;70(Suppl 1):S2–9. doi: 10.1111/j.1753-4887.2012.00489.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Romero R, Korzeniewski SJ. Are infants born by elective cesarean delivery without labor at risk for developing immune disorders later in life? Am. J. Obstet. Gynecol. 2013;208:243–246. doi: 10.1016/j.ajog.2012.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cryan JF, Dinan TG. Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour. Nat. Rev. Neurosci. 2012;13:701–712. doi: 10.1038/nrn3346. [DOI] [PubMed] [Google Scholar]
- 10.Rhee SH, Pothoulakis C, Mayer EA. Principles and clinical implications of the brain-gut-enteric microbiota axis. Nat. Rev. Gastroenterol. Hepatol. 2009;6:306–314. doi: 10.1038/nrgastro.2009.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Diaz Heijtz R, et al. Normal gut microbiota modulates brain development and behavior. Proc. Natl. Acad. Sci. USA. 2011;108:3047–3052. doi: 10.1073/pnas.1010529108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Forsythe P, Kunze WA, Bienenstock J. On communication between gut microbes and the brain. Curr Opin Gastroen. 2012;28:557–562. doi: 10.1097/MOG.0b013e3283572ffa. [DOI] [PubMed] [Google Scholar]
- 13.Lyte M, Varcoe JJ, Bailey MT. Anxiogenic effect of subclinical bacterial infection in mice in the absence of overt immune activation. Physiol. Behav. 1998;65:63–68. doi: 10.1016/S0031-9384(98)00145-0. [DOI] [PubMed] [Google Scholar]
- 14.Broman, S. H., Nichols, P. L. & Kennedy, W. A. Preschool IQ: Prenatal and early developmental correlates. (Lawrence Erlbaum Associates, Inc., John Wiley & Sons (1975).
- 15.McGee R, Silva PA, Williams S. Perinatal, neurological, environmental and developmental characteristics of seven-year-old children with stable behaviour problems. J. Child Psychol. Psychiatry. 1984;25:573–586. doi: 10.1111/j.1469-7610.1984.tb00173.x. [DOI] [PubMed] [Google Scholar]
- 16.Pasamanick B, Rogers ME, Lilienfeld AM. Pregnancy experience and the development of behavior disorders in children. Am J Psychiatry. 1956;112:613–618. doi: 10.1176/ajp.112.8.613. [DOI] [PubMed] [Google Scholar]
- 17.Li HT, et al. Caesarean delivery on maternal request and childhood psychopathology: a retrospective cohort study in China. BJOG. 2011;118:42–48. doi: 10.1111/j.1471-0528.2010.02762.x. [DOI] [PubMed] [Google Scholar]
- 18.Curran EA, et al. Obstetric mode of delivery and attention-deficit/hyperactivity disorder: a sibling-matched study. Int. J. Epidemiol. 2016;45:532–542. doi: 10.1093/ije/dyw001. [DOI] [PubMed] [Google Scholar]
- 19.Curran EA, et al. Obstetrical Mode of Delivery and Childhood Behavior and Psychological Development in a British Cohort. J. Autism Dev. Disord. 2016;46:603–614. doi: 10.1007/s10803-015-2616-1. [DOI] [PubMed] [Google Scholar]
- 20.Al Khalaf SY, et al. The impact of obstetric mode of delivery on childhood behavior. Soc. Psychiatry Psychiatr. Epidemiol. 2015;50:1557–1567. doi: 10.1007/s00127-015-1055-9. [DOI] [PubMed] [Google Scholar]
- 21.Curran EA, et al. Association between obstetric mode of delivery and autism spectrum disorder: A population-based sibling design study. JAMA Psychiatry. 2015;72:8. doi: 10.1001/jamapsychiatry.2015.0846. [DOI] [PubMed] [Google Scholar]
- 22.Weisman O, et al. Oxytocin-augmented labor and risk for autism in males. Behav. Brain Res. 2015;284:207–212. doi: 10.1016/j.bbr.2015.02.028. [DOI] [PubMed] [Google Scholar]
- 23.O’Neill SM, et al. Birth by Caesarean Section and the Risk of Adult Psychosis: A Population-Based Cohort Study. Schizophr. Bull. 2016;42:633–64. doi: 10.1093/schbul/sbv152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yu X, Tam WW, Wong PT, Lam TH, Stewart SM. The Patient Health Questionnaire-9 for measuring depressive symptoms among the general population in Hong Kong. Comprehensive Psychiatry. 2012;53:95–102. doi: 10.1016/j.comppsych.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 25.Wong CK. The Rutter Parent Scale A2 and Teacher Scale B2 in Chinese. II. Clinical validity among Chinese children. Acta Psychiatr. Scand. 1988;78:11–17. doi: 10.1111/j.1600-0447.1988.tb06295.x. [DOI] [PubMed] [Google Scholar]
- 26.Leung PW, et al. Prevalence of DSM-IV disorders in Chinese adolescents and the effects of an impairment criterion: a pilot community study in Hong Kong. Eur. Child. Adolesc. Psychiatry. 2008;17:452–461. doi: 10.1007/s00787-008-0687-7. [DOI] [PubMed] [Google Scholar]
- 27.van Handel M, Swaab H, de Vries LS, Jongmans MJ. Long-term cognitive and behavioral consequences of neonatal encephalopathy following perinatal asphyxia: a review. Eur. J. Pediatr. 2007;166:645–654. doi: 10.1007/s00431-007-0437-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mellon RD, Simone AF, Rappaport BA. Use of anesthetic agents in neonates and young children. Anesth. Analg. 2007;104:509–520. doi: 10.1213/01.ane.0000255729.96438.b0. [DOI] [PubMed] [Google Scholar]
- 29.Rizzi S, Carter LB, Ori C, Jevtovic-Todorovic V. Clinical anesthesia causes permanent damage to the fetal guinea pig brain. Brain Pathol. 2008;18:198–210. doi: 10.1111/j.1750-3639.2007.00116.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sprung J, et al. Anesthesia for Cesarean Delivery and Learning Disabilities in a Population-based Birth Cohort. Anesthesiology. 2009;111:302–310. doi: 10.1097/ALN.0b013e3181adf481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Messaoudi M, et al. Assessment of psychotropic-like properties of a probiotic formulation (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in rats and human subjects. Br. J. Nutr. 2011;105:755–764. doi: 10.1017/S0007114510004319. [DOI] [PubMed] [Google Scholar]
- 32.Benton D, Williams C, Brown A. Impact of consuming a milk drink containing a probiotic on mood and cognition. Eur. J. Cli.n Nutr. 2007;61:355–361. doi: 10.1038/sj.ejcn.1602546. [DOI] [PubMed] [Google Scholar]
- 33.Rao AV, et al. A randomized, double-blind, placebo-controlled pilot study of a probiotic in emotional symptoms of chronic fatigue syndrome. Gut Pathog. 2009;1:6. doi: 10.1186/1757-4749-1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gitau R, et al. Umbilical cortisol levels as an indicator of the fetal stress response to assisted vaginal delivery. Eur. J. Obstet. Gyn. 2001;98:14–17. doi: 10.1016/S0301-2115(01)00298-6. [DOI] [PubMed] [Google Scholar]
- 35.Mears K, McAuliffe F, Grimes H, Morrison JJ. Fetal cortisol in relation to labour, intrapartum events and mode of delivery. J. Obstet. Gynaecol. 2004;24:129–132. doi: 10.1080/01443610410001645389. [DOI] [PubMed] [Google Scholar]
- 36.Miller NM, Fisk NM, Modi N, Glover V. Stress responses at birth: determinants of cord arterial cortisol and links with cortisol response in infancy. BJOG. 2005;112:921–926. doi: 10.1111/j.1471-0528.2005.00620.x. [DOI] [PubMed] [Google Scholar]
- 37.Schooling CM, Hui LL, Ho LM, Lam TH, Leung GM. Cohort profile: ‘children of 1997’: a Hong Kong Chinese birth cohort. Int. J. Epidemiol. 2012;41:611–620. doi: 10.1093/ije/dyq243. [DOI] [PubMed] [Google Scholar]
- 38.Wong CK. The Rutter Parent Scale A2 and Teacher Scale B2 in Chinese. I. Translation study. Acta Psychiatr. Scand. 1988;77:724–728. doi: 10.1111/j.1600-0447.1988.tb05194.x. [DOI] [PubMed] [Google Scholar]
- 39.Elander J, Rutter M. Use and development of the Rutter parents’ and teachers’ scales. Int. J. Method. Psych. 1996;6:16. doi: 10.1002/(SICI)1234-988X(199607)6:2<63::AID-MPR151>3.3.CO;2-M. [DOI] [Google Scholar]
- 40.Battle, J. Culture-free self-esteem inventories (2nd Edition) (Pro-Ed, 1992).
- 41.Battle, J. Culture-free self-esteem inventories: Examiner’s manual (2002).
- 42.Tin SPP, Ho DSY, Mak KH, Wan KL, Lam TH. Association Between Television Viewing and Self-Esteem in Children. J. Dev. Behav. Pediatr. 2012;33:479–485. doi: 10.1097/DBP.0b013e31825ab67d. [DOI] [PubMed] [Google Scholar]
- 43.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 44.Richardson LP, et al. Evaluation of the Patient Health Questionnaire-9 Item for detecting major depression among adolescents. Pediatrics. 2010;126:1117–1123. doi: 10.1542/peds.2010-0852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Allgaier A-K, Pietsch K, Frühe B, Sigl-Glöckner J, Schulte-Körne G. Screening for depression in adolescents: validity of the Patient Health Questionnaire in pediatric care. Depression and Anxiety. 2012;29:906–913. doi: 10.1002/da.21971. [DOI] [PubMed] [Google Scholar]
- 46.Lee, W. Body dissatisfaction, depressive symptoms, and pubertal timing in Hong Kong Chinese Doctor of Philosophy thesis (The University of Hong Kong, 2008).
- 47.Harrell, F. E. Regression modeling strategies: With applications to linear models, logistic regression, and survival analysis (Springer, 2001).
- 48.Schafer JL. Multiple imputation: a primer. Stat. Methods Med. Res. 1999;8:3–15. doi: 10.1177/096228029900800102. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon request from the “Children of 1997” data access committee: aprmay97@hku.hk.