Abstract
Nonalcoholic fatty liver disease (NAFLD) affects 25–30% of the general population worldwide and this high prevalence is linked with lifestyle and dietetic changes, not only in Western countries, but also in the urban areas of developing countries. Several pharmacological approaches were proposed in the treatment of NAFLD, but the reported results are inconclusive. International guidelines recommended the reduction of dietary fat and fructose, in association with some physical activity. In this context, it was reported that the protective effects of traditional Mediterranean diet, related to the high concentration of antioxidant compounds, particularly of polyphenols. Polyphenols are a heterogeneous class of plant derived compounds, with some proven hepatoprotective effects. Our opinion is that the adherence to traditional Mediterranean diet characterized by the consumption of antioxidant-rich foods in general and of polyphenols in particular, can be considered as a potential new approach in the treatment of NAFLD.
Key words: nonalcoholic fatty liver disease, steatosis, polyphenols, Mediterranean diet, antioxidant
Introduction
In the last few decades, the term nonalcoholic fatty liver disease (NAFLD) has been evoked increasingly in research frameworks and in clinical practice. It defines the presence of significant fat accumulation in the liver (> 5% of hepatocytes), in the absence of alcohol abuse and any other cause of liver diseases.[1] The term NAFLD includes different clinical entities, and in particular, the fat accumulation in liver, also known as simple fatty liver and nonalcoholic steatohepatitis (NASH); it is characterized by steatosis along with necroinflammation, fibrosis and finally cirrhosis with its complications. NAFLD is a pathological entity histologically characterized by the presence certain symptoms in the liver, such as cellular ballooning, lobular inflammation, perisinusoidal and perivenular fibrosis, features hardly distinguishable from the ones detected in cases with alcoholic liver disease.[2] Insulin resistance, visceral fat mass, obesity, dyslipidemia, diabetes, and metabolic syndrome are well known risk factors largely associated to NAFLD.[3] Studies on genetic and molecular mechanisms predisposed to NAFLD highlight the role of variants enhancing oxidative stress, pro-inflammatory profile of circulating cytokines, and abnormalities in the metabolism of glucose and fatty acids.[4, 5] NAFLD affects 25–30% of the general population; however, prevalence change in function of gender, age, ethnicity and metabolic features.[6]. The worldwide spread of NAFLD diagnosis is clearly linked with changes in dietary profiles and increased sedentary lifestyle, not only in Western countries but also in urban area of developing countries.[6]
Several pharmacological treatments have been proposed for the treatment of NAFLD, but the reported results are inconclusive.[7] International recommendations indicate that the first therapeutic step for the treatment of NAFLD is to reduce the intake of total fat, saturated fatty acids, trans fatty acids and fructose, along with undergoing physical activity[8]
Mediterranean Diet
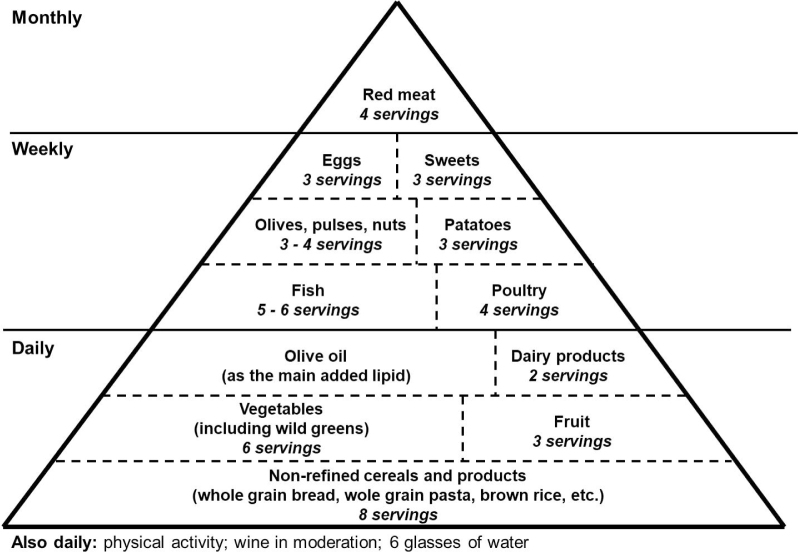
The profile of NAFLD patients is characterized by higher dietary energy and higher simple carbohydrate intake, as compared with the healthy controls[3,9] The standard care to treat NAFLD patients is focused on lifestyle interventions, and in particular, healthy diet and physical exercise. In this way, literature has reported the benefits of Mediterranean diet. In November 2010, UNESCO officially recognized the Mediterranean diet as an Intangible Cultural Heritage of Humanity and defines it as a “set of traditional practices, knowledge and skills passed on from generation to generation, providing a sense of belonging and continuity to the concerned communities”.[10] Mediterranean diet is a way of eating, rather than a formal diet plan. The exact Mediterranean diet is difficult to define precisely, if considered that Mediterranean region is a virtual geographic area that represents many cultures and lifestyles. There are major differences in the dietetic profile between different countries and between some regions within a country, for example, as found in Italy. However, the traditional Mediterranean diet can be represented by a pyramid characterized by high consumption of cereals and vegetables, such as salads, pulses/legumes, bread, pasta, fruits and nuts, and lower intakes of eggs and sweets[11,12] (Figure 1). Extra-virgin olive oil is the main source of fat with a moderate intake of fish, poultry, eggs and dairy products. In addition, moderate amounts of red wine are usually consumed with meals in the European region of the Mediterranean area.[13]
Figure 1.
the traditional Mediterranean diet pyramid.
Adherence to the traditional Mediterranean diet is associated with low mortality risk and reduced incidence of chronic diseases, and in particular, cardiovascular and metabolic disorders, neurodegenerative diseases, depression and several types of cancer.[14,15] These protective effects are related to the high concentration of antioxidants in compounds of this diet. Since the 1950s, Ancel Keys and his co-workers have been studying the Mediterranean diet effects on health, and they found that Greek people, especially belonging to the island of Crete, had the longest life expectancy in the world until the 1960s, followed by the people of Southern Italy, Spain and France.[16] These data were confirmed by subsequent studies on the elderly population in Greece and other European Countries, and showed that the Mediterranean dietary pattern in toto influenced the longevity rather than a single nutrient in the diet, with a significant reduction in the overall mortality.[17] This assumption is a cornerstone for public health, and in particular, in the context of prevention policy based on the Mediterranean style in the primary prevention of major chronic diseases not only in Western Countries, but also in all urban area worldwide.[18]
Polyphenols And Nafld
Polyphenols are a heterogeneous class of plant derived compounds, that include several hydro soluble antioxidants reported as health promoting agents and proposed in the treatment of different metabolic disorders[19,20] Fruits, vegetables, beverages including coffee, tea, red wine, and dark chocolate are the important sources of these bioactive compounds. On the basis of their chemical structure, two categories of polyphenols are described: the flavonoids containing a common diphenylpropane skeleton (e.g., flavonoids, flavones, flavanols, flavonols, isoflavones, proanthocyanidins and anthocyanins); the non-flavonoids, mainly comprising mono-phenols alcohols (e.g., hydroxytyrosol) or stilbene phenolic acids (e.g., resveratrol).[20] In the short-term, polyphenols are not essential for life such as vitamins, however, nowadays they are considered responsible for the beneficial effects of fruits and vegetables. Their potential role in the prevention and treatment of oxidative stress and inflammation has been investigated recently.[21] In particular, polyphenols may present hepatoprotective effects by increasing the fatty acid oxidation and modulation of insulin resistance, oxidative stress and inflammation, which are the main pathogenetic factors linked to the progression from simple fat accumulation to NASH.[20] Several evidences in vitro, pre-clinical and emerging clinical trials reported beneficial effects on liver steatosis and its pathogenic and clinical setting.[20-23]
Few clinical studies were focused on the polyphenols use in NAFLD patients. Three were undertaken with 500 mg and 600 mg resveratrol daily for 12 weeks, or 3000 mg daily for 8 weeks respectively.[24-26] Other two studies were carried out using 150 mg polyphenols (1.43% of flavonoids, 2.5% anthocyanins and 1.7% phenolic acid) extract of Hibiscus sabdariffa L. or 1350 mg of bayberry juice, daily for 12 weeks and 4 weeks in overweight and in young adults with NAFLD, respectively.[27,28] Finally, one study utilized 250 mL of pomegranate juice or orange juice per day associated with hypocaloric diet over a period of 12 weeks.[29] Some studies reported a significant impact of polyphenols’ importance on NAFLD. Chang et al. and Ekhlasi et al. showed a significant improvement of anthropometric parameters after treatment with polyphenols.[27,29] Faghihzadeh et al. observed a reduction in weight, body mass index, waist circumference, liver enzymes, and steatosis degree, while resveratrol was associated with lifestyle changes and particularly with physical activity.[24] The reduction of serum transaminase levels was also noted by Chen et al. in association with a significant improvement of insulin resistance assessed by homeostasis model assessment insulin resistance index.[25] The polyphenols used by humans through consumption of the bayberry juice and resveratrol showed anti-inflammatory effects, with a reduction in serum cytokines and in particular of TNF-α, interelukin-6 and -8, and increased serum levels of adiponectin.[24,25,28] In addition, Faghihzadeh et al. described a reduction in NF-ϰB activity in the peripheral blood mononuclear cells.[24] Finally, Ekhlasi et al. reported the reduction of high liver enzymes and improvement of total antioxidant capacity in the NAFLD patients treated with pomegranate juice.[29] Nowadays, data on the effects of polyphenols in the histology of NAFLD, assessed by liver biopsy, are absent. However, the information obtained by non-invasive tools like the liver ultrasound reported a significant improvement of liver damage and liver steatosis degree when polyphenol supplementation is associated with lifestyle changes.[24,25,28]
Conclusion
NAFLD is the liver board of over nutrition and an upcoming challenge for hepatologists and health systems worldwide. Patients with liver steatosis have an increased prevalence of chronic diseases. Therefore, the treatment of NAFLD patients should be focused on reducing predisposing factors, such as insulin resistance, oxidative stress, and dyslipidemia. In this way, nutraceuticals may have an important role in the treatment of NAFLD. Supported by literature data, it can be concluded that adherence to the traditional Mediterranean diet characterized by the consumption of antioxidant-rich foods in general and of polyphenols in particular, can be considered as a potential new approach in the treatment of NAFLD, and even a valuable instrument of prevention of this disorder. Further studies are needed to define the achievable doses of individual polyphenols or select their combination.
Footnotes
Conflict of Interest: Authors declare no conflict of interest related to this publication.
References
- 1.Nascimbeni F, Pais R, Bellentani S, Day CP, Ratziu V, Loria P. et al. From NAFLD in clinical practice to answers from guidelines. J Hepatol. 2013;59:859–71. doi: 10.1016/j.jhep.2013.05.044. [DOI] [PubMed] [Google Scholar]
- 2.Kobyliak N, Abenavoli L.. The role of liver biopsy to assess non-alcoholic fatty liver disease. Rev Recent Clin Trials. 2014;9:159–69. doi: 10.2174/1574887109666141216102231. [DOI] [PubMed] [Google Scholar]
- 3.Abenavoli L, Milic N, Di Renzo L, Preveden T, Medić-Stojanoska M, De Lorenzo A.. Metabolic aspects of adult patients with nonalcoholic fatty liver disease. World J Gastroenterol. 2016;22:7006–16. doi: 10.3748/wjg.v22.i31.7006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anstee QM. DayCP The genetics of NAFLD. Nat Rev Gastroenterol Hepatol. 2013;10:645–55. doi: 10.1038/nrgastro.2013.182. [DOI] [PubMed] [Google Scholar]
- 5.Severson TJ, Besur S, Bonkovsky HL.. Genetic factors that affect non-alcoholic fatty liver disease: A systematic clinical review. World J Gastroenterol. 2016;22:6742–56. doi: 10.3748/wjg.v22.i29.6742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Masarone M, Federico A, Abenavoli L, Loguercio C, Persico M.. Non alcoholic fatty liver: epidemiology and natural history. Rev Recent Clin Trials. 2014;9:126–33. doi: 10.2174/1574887109666141216111143. [DOI] [PubMed] [Google Scholar]
- 7.Italian Association for the Study of the Liver (AISF). AISF position paper on nonalcoholic fatty liver disease (NAFLD): Updates and future directions. Dig Liver Dis. 2017;49:471–83. doi: 10.1016/j.dld.2017.01.147. [DOI] [PubMed] [Google Scholar]
- 8.European Association for the Study of the Liver (EASL); European Association for the Study of Diabetes (EASD); European Association for the Study of Obesity (EASO). EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64:1388–402. doi: 10.1016/j.jhep.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 9.Katsagoni CN, Papatheodoridis GV, Papageorgiou MV, Ioannidou P, Deutsch M, Alexopoulou A. et al. A “healthy diet-optimal sleep” lifestyle pattern is inversely associated with liver stiffness and insulin resistance in patients with nonalcoholic fatty liver disease. Appl Physiol Nutr Metab. 2017;42(3):250–256. doi: 10.1139/apnm-2016-0492. PMID:28133993. [DOI] [PubMed] [Google Scholar]
- 10. http://www.unesco.org/culture/ich/RL/00884 Available from. [Google Scholar]
- 11.Abenavoli L, Milic N, Peta V, Alfieri F, De Lorenzo A, Bellentani S.. Alimentary regimen in non-alcoholic fatty liver disease: Mediterranean diet. World J Gastroenterol. 2014;20:16831–40. doi: 10.3748/wjg.v20.i45.16831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gelli C, Tarocchi M, Abenavoli L, Di Renzo L, Galli A, De Lorenzo A.. Effect of a counseling-supported treatment with the Mediterranean diet and physical activity on the severity of the non-alcoholic fatty liver disease. World J Gastroenterol. 2017;23:3150–62. doi: 10.3748/wjg.v23.i17.3150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Di Renzo L, Carraro A, Valente R, Iacopino L, Colica C, De Lorenzo A.. Intake of red wine in different meals modulates oxidized LDL level, oxidative and inflammatory gene expression in healthy people: a randomized crossover trial. Oxid Med Cell Longev. 2014;2014:6813–18. doi: 10.1155/2014/681318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Lorenzo A, Noce A, Bigioni M, Calabrese V, Della Rocca DG, Di Daniele N. et al. The effects of Italian Mediterranean organic diet (IMOD) on health status. Curr Pharm Des. 2010;16:814–24. doi: 10.2174/138161210790883561. [DOI] [PubMed] [Google Scholar]
- 15.Sofi F, Abbate R, Gensini GF, Casini A.. Accruing evidence on benefits of adherence to the Mediterranean diet on health: an updated systematic review and meta-analysis. AmJ ClinNutr. 2010;92:1189–96. doi: 10.3945/ajcn.2010.29673. [DOI] [PubMed] [Google Scholar]
- 16.Keys A, Menotti A, Aravanis C, Blackburn H, Djordevic BS, Buzina R. et al. The seven countries study: 2,289 deaths in 15 years. Prev Med. 1984;13:141–54. doi: 10.1016/0091-7435(84)90047-1. [DOI] [PubMed] [Google Scholar]
- 17.Di Daniele N, Noce A, Vidiri MF, Moriconi E, Marrone G, Annicchiarico-Petruzzelli M. et al. Impact of Mediterranean diet on metabolic syndrome, cancer and longevity. Oncotarget. 2017;8:8947–79. doi: 10.18632/oncotarget.13553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schwingshackl L, Hoffmann G.. Mediterranean dietary pattern, inflammation and endothelial function: a systematic review and meta-analysis of intervention trials. Nutr Metab Cardiovasc Dis. 2014;24:929–39. doi: 10.1016/j.numecd.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 19.Del Ben M, Polimeni L, Baratta F, Pastori D, Angelico F.. The role of nutraceuticals for the treatment of non-alcoholic fatty liver disease. Br J Clin Pharmacol. 2017;83:88–95. doi: 10.1111/bcp.12899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rodriguez-Ramiro I, Vauzour D, Minihane AM.. Polyphenols and non-alcoholic fatty liver disease: impact and mechanisms. Proc Nutr Soc. 2016;75:47–60. doi: 10.1017/S0029665115004218. [DOI] [PubMed] [Google Scholar]
- 21.Zhang PY.. Polyphenols in Health and Disease. Cell BiochemBiophys. 2015;73:649–64. doi: 10.1007/s12013-015-0558-z. [DOI] [PubMed] [Google Scholar]
- 22.Salomone F, Godos J, Zelber-Sagi S.. Natural antioxidants for non-alcoholic fatty liver disease: molecular targets and clinical perspectives. Liver Int. 2016;36:5–20. doi: 10.1111/liv.12975. [DOI] [PubMed] [Google Scholar]
- 23.Van De Wier B, Koek GH, Bast A, Haenen GR.. The potential of flavonoids in the treatment of non-alcoholic fatty liver disease. Crit Rev Food SciNutr. 2017;57:834–55. doi: 10.1080/10408398.2014.952399. [DOI] [PubMed] [Google Scholar]
- 24.Faghihzadeh F, Adibi P, Rafiei R, Hekmatdoost A.. Resveratrol supplementation improves inflammatory biomarkers in patients with nonalcoholic fatty liver disease. Nutr Res. 2014;34:837–43. doi: 10.1016/j.nutres.2014.09.005. [DOI] [PubMed] [Google Scholar]
- 25.Chen S, Zhao X, Ran L, Wan J, Wang X, Qin Y. et al. Resveratrol improves insulin resistance, glucose and lipid metabolism in patients with non-alcoholic fatty liver disease: a randomized controlled trial. Dig Liver Dis. 2015;47:226–32. doi: 10.1016/j.dld.2014.11.015. [DOI] [PubMed] [Google Scholar]
- 26.Chachay VS, Macdonald GA, Martin JH, Whitehead JP, O’Moore-Sullivan TM, Lee P. et al. Resveratrol does not benefit patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2014;12:2092–103e1-6. doi: 10.1016/j.cgh.2014.02.024. [DOI] [PubMed] [Google Scholar]
- 27.Chang HC, Peng CH, Yeh DM, Kao ES, Wang CJ.. Hibiscus sabdariffa extract inhibits obesity and fat accumulation, and improves liver steatosis in humans. Food Funct. 2014;5:734–9. doi: 10.1039/c3fo60495k. [DOI] [PubMed] [Google Scholar]
- 28.Guo H, Zhong R, Liu Y, Jiang X, Tang X, Li Z. et al. Effects of bayberry juice on inflammatory and apoptotic markers in young adults with features of nonalcoholic fatty liver disease. Nutrition. 2014;30:198–203. doi: 10.1016/j.nut.2013.07.023. [DOI] [PubMed] [Google Scholar]
- 29.Ekhlasi G, Shidfar F, Agah S, Merat S, Hosseini AF.. Effects of Pomegranate and Orange Juice on Antioxidant Status in Non-Alcoholic Fatty Liver Disease Patients: A Randomized Clinical Trial. Int J Vitam Nutr Res. 2016;14:1–7. doi: 10.1024/0300-9831/a000292. [DOI] [PubMed] [Google Scholar]