Abstract
Objectives
To determine whether specialist nurse intervention improves outcome in patients with chronic heart failure.
Design
Randomised controlled trial.
Setting
Acute medical admissions unit in a teaching hospital.
Participants
165 patients admitted with heart failure due to left ventricular systolic dysfunction. The intervention started before discharge and continued thereafter with home visits for up to 1 year.
Main outcome measures
Time to first event analysis of death from all causes or readmission to hospital with worsening heart failure.
Results
31 patients (37%) in the intervention group died or were readmitted with heart failure compared with 45 (53%) in the usual care group (hazard ratio=0.61, 95% confidence interval 0.33 to 0.96).Compared with usual care, patients in the intervention group had fewer readmissions for any reason (86 v 114, P=0.018), fewer admissions for heart failure (19 v 45, P<0.001) and spent fewer days in hospital for heart failure (mean 3.43 v 7.46 days, P=0.0051).
Conclusions
Specially trained nurses can improve the outcome of patients admitted to hospital with heart failure.
What is already known on this topic
Studies have suggested that nurse intervention may reduce readmission in patients with heart failure
What this study adds
Home based intervention from nurses reduces readmissions for worsening heart failure
Regular contact to review treatment and patient education are likely to contribute to this effect
Introduction
Chronic heart failure is a huge public health problem. Patients have a worse prognosis than those with most cancers and require frequent, prolonged, and costly admissions to hospital.1,2 Readmission rates are also high, and the burden of illness and related expenditure is set to increase considerably in the future.1
Heart failure is not managed optimally.3,4 Most patients are not looked after by specialists and have little knowledge of their condition and its treatment. Effective therapies are underprescribed.3,4 Patients are rarely prescribed exercise or given dietary advice or immunisation against influenza and pneumococcus. Patients often do not adhere to their drugs.3,4 Many hospital admissions may therefore be avoidable.3,4
Specialist nurses may help overcome the deficiencies in care of patients with heart failure.5,6 We describe a randomised controlled trial to determine whether nurse intervention, when used in addition to routine care, can reduce the morbidity and mortality related to chronic heart failure. We randomised patients managed by general physicians and general practitioners, who care for most people with chronic heart failure.
Participants and methods
Participants
Patients who were admitted as an emergency to the acute medical admissions unit at the Western Infirmary, Glasgow, with heart failure due to left ventricular systolic dysfunction were eligible for this study. Patients were recruited between March 1997 and November 1998 and followed up for a mean of 12 months. We excluded patients who were unable or unwilling to give informed consent or to comply with the intervention and those who had an acute myocardial infarction, comorbidity (such as malignancy) likely to lead to death or readmission in the near future, planned discharge to long term residential care, or residence outside the hospital's catchment area. Echocardiographic left ventricular systolic function was graded semiquantitatively (normal or mildly, moderately, or severely reduced) in keeping with the hospital's usual practice.
Randomisation
Eligible patients who gave consent were randomised to usual care or nurse intervention. Study nurses phoned the Robertson Centre for Biostatistics and the patient was allocated to one or other intervention group from a randomisation list. The study was approved by both the local hospital and general practice ethics committees.
Intervention
Patients in the usual care group were managed as usual by the admitting physician and, subsequently, general practitioner. They were not seen by the specialist nurses after hospital discharge.
Details of the nurse intervention are published elsewhere.5,6 Essentially, it consisted of a number of planned home visits of decreasing frequency, supplemented by telephone contact as needed. The aim was to educate the patient about heart failure and its treatment, optimise treatment (drugs, diet, exercise), monitor electrolyte concentrations, teach self monitoring and management (especially the early detection and treatment of decompensation), liaise with other health care and social workers as required, and provide psychological support.
The nurses were given training in these roles before the start of the study. They used written protocols on the use of angiotensin converting enzyme inhibitors, diuretics, and digoxin in chronic heart failure and liaised with members of the department of cardiology as required. Participants were given a pocket sized booklet containing an explanation of heart failure and its treatment; dietary advice; contact details for the heart failure nurses; a list of their drugs, weights, and blood test results; and details of planned visits (dates and times).
End points and statistical analysis
The primary end point of this study was death from all causes or hospital admission for heart failure (emergency or elective). The estimated rate of this end point was 55% at one year in the usual care group. With 82 patients in each treatment group we had an 80% power at a significance of 5% to detect an absolute difference of 23%—that is, a rate in the nurse intervention group of 32%). The reduction in relative risk of 42% was predicted from earlier studies of nurse intervention.7–9
Secondary end points included death or hospital admission for any reason, hospital admission for worsening chronic heart failure, and all cause admission to hospital. We also analysed numbers of patients admitted, number of admissions, and days spent in hospital.
We obtained data on admissions and deaths from the hospital records department, the information and statistics division of the Scottish NHS (hospital admissions) and the Registrar General's Office, Scotland (deaths).2 All hospital admissions were adjudicated blind to treatment allocation.
We compared rates of death, death or readmission, and cause specific readmission between the groups on a time to first event basis using the log rank test. We calculated 95% confidence intervals for hazard ratios from Cox proportional hazard models with treatment as the sole covariate. For the outcome of death before discharge, we compared the results using Fisher's exact test. Rates of readmission were compared by Poisson regression, with adjustment for the length of follow up. We compared the numbers of days spent in hospital using bootstrap two sample t tests. The data were first transformed by taking natural logarithms of the length of stay in days plus one day. Bootstrap 95% confidence intervals were calculated for the differences between the group means of the transformed data. We used the natural exponentials of the estimates and end points of the confidence intervals for presentation purposes, so that they could be interpreted as ratios. We used the Kaplan-Meier method to construct estimated survival curves.
Results
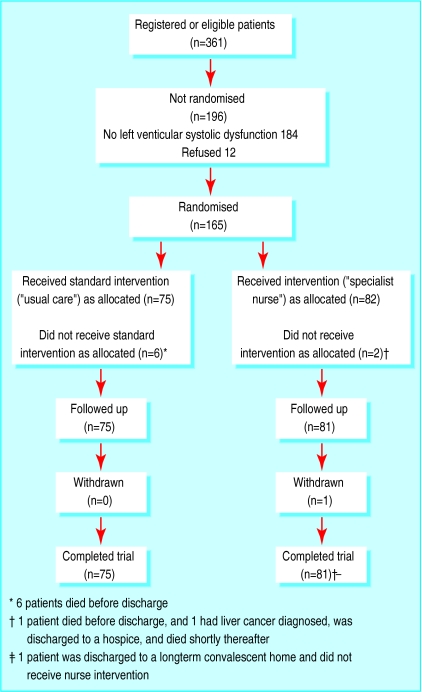
We screened 801 patients thought to have heart failure on admission. Of the 361 who were eligible for the study and survived to have echocardiography, 177 (49%) had left ventricular systolic dysfunction. Of these, 165 gave consent and were randomised, 81 to the usual care group and 84 to the nurse intervention group (fig 1). Table 1 shows their clinical characteristics.
Figure 1.
Patient distribution in trial
Table 1.
Clinical characteristics of patients randomised to usual care or nurse intervention. Values are numbers (percentages) unless stated otherwise
| Usual care (n=81) | Nurse intervention (n=84) | |
|---|---|---|
| Mean (SD) age (years) | 75.6 (7.9) | 74.4 (8.6) |
| Male | 41 (51) | 54 (64) |
| Living alone | 38 (47) | 37 (44) |
| Social services required | 28 (35) | 28 (33) |
| Other medical problems: | ||
| Angina | 40 (49) | 38 (45) |
| Past myocardial infarction | 41 (51) | 46 (55) |
| Diabetes mellitus | 15 (19) | 15 (18) |
| Chronic lung disease | 18 (22) | 23 (27) |
| Hypertension | 42 (52) | 36 (43) |
| Atrial fibrillation* | 24 (30) | 29 (35) |
| Valve disease | 12 (15) | 15 (18) |
| Past admission for chronic heart failure | 36 (44) | 27 (32) |
| New York Heart Association class at admission†: | ||
| II | 16 (20) | 19 (23) |
| III | 33 (42) | 28 (34) |
| IV | 30 (38) | 36 (43) |
| Degree of left ventricular systolic dysfunction‡: | ||
| Mild | 10 (13) | 18 (22) |
| Moderate | 42 (53) | 31 (38) |
| Severe | 28 (35) | 32 (40) |
| Renal function at admission*: | ||
| Median (interquartile range) plasma urea (mmol/l) | 9.7 (6.5-13.9) | 8.1 (6.0-10.3) |
| Median (interquartile range) plasma creatinine (μmol/l) | 116 (90-168) | 108 (84-132) |
| Mean (SD) blood pressure at discharge (mm Hg)§: | ||
| Systolic | 126.1 (21.4) | 116.0 (19.5) |
| Diastolic | 70.1 (12.0) | 68.4 (10.2) |
Information available on 79 of the usual care and 82 of the nurse intervention group.
Information available on 79 of the usual care group.
Information available on 80 of the usual care and 81 of the nurse intervention group.
Information available on 74 of the usual care and 79 of the nurse intervention group.
By discharge, more patients in the intervention group than the usual care group had started an angiotensin converting enzyme inhibitor and stopped a calcium channel blocker (table 2). Length of hospital stay (median, interquartile range) was shorter in the intervention group (median 8.0 (interquartile range 4-10) days v 9.0 (7-12) days in usual care group). The median (interquartile range) time until death or end of study was 365 (277-365) days in the usual care group and 365 (273-365) days in the intervention group.
Table 2.
Drug treatment on admission and at hospital discharge in usual care and nurse intervention groups
| Usual care
|
Nurse intervention
|
||||
|---|---|---|---|---|---|
| Admission (n=81) | Discharge (n=74) | Admission (n=84) | Discharge (n=81) | ||
| No (%) taking drug: | |||||
| Loop diuretic | 55 (69) | 68 (92) | 53 (63) | 76 (94) | |
| Thiazide diuretic | 5 (6) | 4 (5) | 8 (10) | 5 (6) | |
| ACE inhibitor | 41 (51) | 53 (72) | 35 (42) | 65 (80) | |
| Digoxin | 15 (19) | 31 (42) | 16 (19) | 35 (43) | |
| β blocker | 10 (12) | 5 (7) | 11 (13) | 2 (2) | |
| Oral or transdermal nitrate | 22 (28) | 26 (35) | 19 (23) | 21 (26) | |
| Calcium channel blocker | 22 (28) | 17 (23) | 15 (18) | 8 (10) | |
| Median (interquartile range) dose (mg): | |||||
| Furosemide (frusemide) equivalent* | 80 (40-120) | 80 (40-120) | 80 (40-120) | 80 (65-120) | |
| Enalapril equivalent† | 10 (10-20) | 10 (10-20) | 15 (10-20) | 20 (6.3-20) | |
| Digoxin | 0.125 (0.125-0.1875) | 0.125 (0.125-0.1875) | 0.125 (0.125-0.1875) | 0.125 (0.125-0.25) | |
| Median (interquartile range) No of drugs | 5 (3-7) | 6 (4.8-8) | 4 (3-6) | 5 (4-7) | |
ACE=angiotensin converting enzyme.
Based on patients taking loop diuretics.
Based on patients taking angiotensin converting enzyme inhibitor. Data available for 35 of usual care group and 33 of intervention group at admission and for 45 and 60 respectively at discharge.
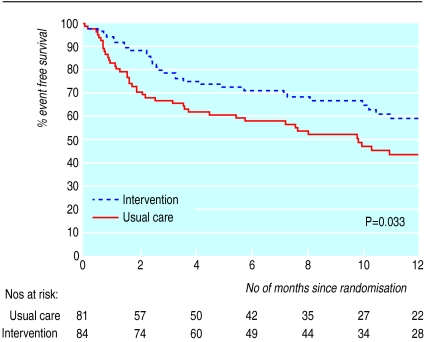
Table 3 summarises the clinical results. Death rates were similar in the two groups, with 31% and 30% dying in the usual care and nurse intervention groups, respectively. For our primary end point (all cause death or admission with chronic heart failure) fewer patients had events in the nurse intervention group than in the usual care group (31 v 43; hazard ratio=0.61, 95% confidence interval 0.38 to 0.96). Figure 2 shows the Kaplan-Meier curve.
Table 3.
Clinical events in usual care and nurse intervention groups
| Usual care (n=81) | Nurse intervention (n=84) | Effect of nurse intervention relative to usual care (95% CI) | P value | |
|---|---|---|---|---|
| No (%) of deaths | ||||
| Before discharge | 6 (7) | 1 (1) | — | 0.061 |
| Total | 25 (31) | 25 (30) | 0.93 (0.54 to 1.63)* | 0.81 |
| No (%) of patients readmitted | ||||
| All causes | 49 (60) | 47 (56) | 0.80 (0.53 to 1.19)* | 0.27 |
| Worsening heart failure | 26 (32) | 12 (14) | 0.38 (0.19 to 0.76)* | 0.0044 |
| No (%) of deaths or readmissions | ||||
| All causes | 61 (75) | 52 (62) | 0.72 (0.49 to 1.04)* | 0.075 |
| Heart failure | 43 (53) | 31 (37) | 0.61 (0.38 to 0.96)* | 0.033 |
| No of readmissions (No/patient/month) | ||||
| All causes | 114 (0.174) | 86 (0.124) | 0.71 (0.54 to 0.94)† | 0.018 |
| Worsening heart failure | 45 (0.069) | 19 (0.027) | 0.40 (0.23 to 0.71)† | 0.0004 |
| Mean (SD) No of days in hospital | ||||
| All causes | 16.7 (24.1) | 10.3 (19.0) | 0.65 (0.40 to 1.06)‡ | 0.081 |
| Worsening heart failure | 7.46 (16.6) | 3.43 (12.2) | 0.60 (0.41 to 0.88)‡ | 0.0051 |
All causes refers to unplanned and planned admissions.
Hazard ratio.
Rate ratio.
Confidence interval for difference in mean loge(duration of hospital stay +1) retransformed to a ratio scale.
Figure 2.
Time to first event (death from any cause or hospital admission for heart failure) in usual care and nurse intervention groups
Death or readmission from all causes was reduced by 28% (0.72, 0.49 to 1.04) in the nurse intervention group compared with usual care (table 3). The risk of admission to hospital for worsening heart failure was reduced by 62% (0.38, 0.19 to 0.76) in the intervention group.
When we took the number of readmissions for each patient into account, the differences between the treatment groups were greater (table 3). The number of admissions/patient/month was 0.174 in the usual care group and 0.124 in the intervention group (rate ratio 0.71, 95% confidence interval 0.54 to 0.94) for all cause admissions; the corresponding rates for admission for heart failure were 0.069 and 0.027 (0.40, 0.23 to 0.71).
Discussion
We found that intervention by a specialist nurse can substantially reduce the risk of readmission to hospital for heart failure. Although 16 fewer primary events occurred per 100 patients treated, the benefit was solely related to hospital admissions and not deaths, as would be expected in a small study with a relatively short follow up. Reduced readmission is, however, a worthwhile aim of treatment. The benefit was seen in older patients, many of whom were women. Both these groups have been under-represented in trials of drugs for heart failure.1
One limitation of our study is that it was conducted before there was good evidence to support the general use of β blockers for heart failure. One objective of nurse intervention, however, is to increase the use of effective treatments, and nurse intervention seems ideally suited to facilitate the slow, cautious, up-titration required with β blockers.
Other studies
Our study differs from three published randomised trials of nurse intervention in heart failure.7–9 Cline et al, in Sweden, used a clinic based nurse intervention.7 They found only a trend to reduced readmissions. In the United States, Rich et al used a multidisciplinary intervention involving a specially trained nurse, dietician, geriatric cardiologist, social services, and home care services.8 The intervention started before discharge and was supplemented after discharge by home visits and telephone contact with members of the study team. The treatment objectives were similar to ours, although it is difficult to tell from the published report whether the level of nurse intervention was as intensive. The benefit of intervention was less clear. Among 282 patients randomised, survival free of readmission at 90 days (the primary end point) was 54% in the control group and 64% in the treatment group (not significant). The risk of readmission was reduced (absolute risk reduction 13%, P=0.03) and the number of admissions for heart failure was halved. Neither of these studies had a follow up of more than six months.
Stewart et al, in Australia, reported a trial in 200 patients using an intervention consisting of only one home visit by a nurse and pharmacist one week after discharge.9 This intervention was similar to that used in our study, although the continuing patient care was devolved to other healthcare workers. More patients in the usual care group than the intervention group had an event within six months (51 v 38, P=0.04), and the intervention reduced the total number of events (129 v 77, P=0.02).
Implications
Collectively, these studies suggest that, in addition to education about heart failure and its treatment, the key components of successful intervention are regular contact with patients to detect clinical deterioration and continued adjustment and optimisation of treatment.5,9 In our study, the dose of angiotensin converting enzyme inhibitor had increased more in the intervention than in the usual care group, even before discharge. This may have contributed to the reduction in hospital admissions.10
Home visiting also seems to be pivotal to reducing admissions, perhaps by ensuring regular and effective patient contact.7,9 Nurses in our study could change drug treatment, within predefined limits, without medical consultation. This may have resulted in problems such as sodium volume overload and deteriorating renal function being corrected more rapidly. Interventions relying on patient initiated telephone communication and visits to hospital clinics may be less effective.
Acknowledgments
We thank Professors Dargie and Reid for their help in the planning and implementation of this study. We also thank the physicians and nurses working in the acute medical admissions unit and local general practitioners for allowing us to study their patients. We thank A Trainer for additional statistical analysis.
Footnotes
Funding: This study was supported by a grant from the Scottish Office, Department of Health.
Competing interests: None declared.
References
- 1.McMurray JJ, Stewart S. Epidemiology, aetiology, and prognosis of heart failure. Heart. 2000;83:596–602. doi: 10.1136/heart.83.5.596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stewart S, MacIntyre K, Hole DJ, Capewell S, McMurray JJ. More ‘malignant’ than cancer? Five-year survival following a first admission for heart failure. Eur J Heart Fail. 2001;3:315–322. doi: 10.1016/s1388-9842(00)00141-0. [DOI] [PubMed] [Google Scholar]
- 3.Ashton CM. Care of patients with failing hearts: evidence for failures in clinical practice and health services research. J Gen Intern Med. 1999;14:138–140. doi: 10.1046/j.1525-1497.1999.00300.x. [DOI] [PubMed] [Google Scholar]
- 4.Chin MH, Goldman L. Factors contributing to the hospitalization of patients with congestive heart failure. Am J Public Health. 1997;87:643–648. doi: 10.2105/ajph.87.4.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McMurray JJ, Stewart S. Nurse led, multidisciplinary intervention in chronic heart failure. Heart. 1998;80:430–431. doi: 10.1136/hrt.80.5.430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stewart S, Blue L, editors. Improving outcomes in chronic heart failure: a practical guide to specialist nurse intervention. London: BMJ; 2001. [Google Scholar]
- 7.Cline CMJ, Israelsson BYA, Willenheimer RB, Broms K, Erhardt LR. Cost effective management programme for heart failure reduces hospitalisation. Heart. 1998;80:442–446. doi: 10.1136/hrt.80.5.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rich MW, Beckham V, Wittenberg C, Leven CL, Freedland KE, Carney RM. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N Engl J Med. 1995;333:1190–1195. doi: 10.1056/NEJM199511023331806. [DOI] [PubMed] [Google Scholar]
- 9.Stewart S, Marley JE, Horowitz JD. Effects of a multidisciplinary, home-based intervention on unplanned readmissions and survival among patients with chronic congestive heart failure: a randomised controlled study. Lancet. 1999;354:1077–1083. doi: 10.1016/s0140-6736(99)03428-5. [DOI] [PubMed] [Google Scholar]
- 10.Packer M, Poole-Wilson PA, Armstrong PW, Cleland JG, Horowitz JD, Massie BM, et al. Circulation. 1999;100:2312–2318. doi: 10.1161/01.cir.100.23.2312. [DOI] [PubMed] [Google Scholar]