Abstract
Introduction:
Primary open angle glaucoma is an insidious and chronic vision-threatening eye ailment due to neuro-retino-optic nerve degeneration, which may be due to the raised intraocular pressure (IOP) or due to independent factors. Management of glaucoma is mainly concentrated on lowering IOP that requires lifetime topical medication, different ocular medicaments for lowering of IOP, and surgical interventions, but it has its own limitations to control the progression of glaucomatous optic neuropathy (GON), and this is the reason behind the use of alternative neuroprotective adjuvants.
Aim:
To evaluate the neuroprotective effect of Ayurvedic line of management of progressive GON.
Materials and Methods:
Ingredients of trial drug Vara Fort powder (Chakshushya Rasayana) were procured from the Institute Pharmacy, except Swarnamakshika Bhasma, which was purchased from Dhootapapeshwar Pharmaceuticals. The patients fulfilling inclusion criteria, attending outpatient and inpatient departments, irrespective of their sex, race, religion, occupation, etc., were selected and divided into two groups with open-labeled randomization. In Group A, in addition to betaxolol (0.1%) or timolol (0.5%) (non-iobrim), Chakshushya Rasayana 6 g/day orally with Triphala Ghrita and honey along with Koshtha-Shuddhi (body-microchannel clearing treatment) protocol was tried. Nasya (oleation through nasal route) with Jeevantyadi Taila and Tarpana (eye satiation) with Go-Ghrita were also performed. In Group B (control), brimonidine (iobrim) 0.2% eye drop was used for 3 months.
Results:
Significant improvement was observed in subjective parameters in Group A such as blurred vision, frequent change of presbyopic glasses, and delayed dark adaptation.
Conclusion:
Chakshushya Rasayana, if administered in a systematic approach along with a modern topical betaxolol or timolol eye drops, has a definite role in improving the lost retinal sensitivity as much as up to 12 dB in 3 months duration.
Keywords: Chakshushya Rasayana, glaucoma, glaucomatous optic neuropathy, Jeevantyadi Taila, Triphala Ghrita, Ayurveda
Introduction
Primary open angle glaucoma (POAG) is a neurodegenerative condition, wherein search for an effective therapeutic modality to address the neuroretinal damage is going on throughout the world so as to treat and prevent this condition from causing irreversible blindness. POAG considered as a chronic, progressive, anterior optic neuropathy that is accompanied by the characteristic cupping and atrophy of the optic disc (OD), visual field loss, open angles, with no obvious causative ocular or systemic conditions, leading to death of retinal ganglion cells (RGCs) which contribute to optic neuropathy.[1]
Glaucoma is the second leading cause of irreversible blindness worldwide and the third leading cause of it in India.[2,3] Globally, POAG affects more than angle closure glaucoma (ACG) with ratio of 3:1. In India, 4.7% of people having country’s total blindness are affected with glaucoma.[4] Population-based studies reported a prevalence rate between 2% and 13%. Glaucoma can affect any age group, including newborn, infants, children, and elderly.[5] Early detection is the key to preserve vision-related quality of life. The current strategy of modern management of glaucoma is mainly concentrated on lowering intraocular pressure (IOP) that requires life time topical medication to be instilled. Some patients do not respond to mono therapy, demanding for multiple drug therapy. Sometimes, surgical intervention is required, which includes filtration and nonfiltrating surgeries that have their own advantages and disadvantages. Meticulous efforts in treating the other important pathological events such as hypo-perfusion to optic nerve head (ONH) and management of glaucomatous optic neuropathy (GON) are non-yielding. It is established in management of glaucoma that along with control of IOP, perfusion of ONH, nerve regeneration and adaptability should also be addressed.[6] Therefore, search for few alternative therapeutic approaches independent of IOP reduction is highly demanded.
Critical analysis of pathophysiology of OAG in Ayurvedic perspective has four important events; first of all, Margavarana leading to Sroto-Avarodha (increased resistance to aqueous humor outflow secondary to the degeneration/sclerosis of filtering apparatus which results in increased IOP) followed by Sokshma-Sroto Sanga/Rasayani Avarodha (ischemia/hypoperfusion to ONH/nutrient channels obstruction) which may or may not be due to IOP. Third, Dhatu Rupi Ojo Hrasa/Vyadhi Kshamatva Hani (failure of local immunity) and finally Dhatu Kshaya (remodeling/changes of ONH) secondary to the above three factors occurs.
Considering the limitations of the contemporary system in managing the condition and after analyzing the Samprapti (pathophysiology) of the OAG in Ayurveda; it was planned to complement Ayurveda management with few modifications in addition to modern topical anti-glaucomatous drugs. This method was followed in one group, while the patients of control group were kept only on modern topical anti-glaucomatous drugs in another group.
Aims and objectives
To evaluate the neuroprotective effect of Ayurvedic line of management of progressive GON.
Materials and Methods
Drugs
Ingredients of trial drug Varafort powder (VFP) were procured from the Institute Pharmacy, except Swarnamakshika Bhasma (which was purchased from Dhootapapeshwar Pharmaceuticals, Mumbai, with Quality Analysis Certificate). The rest was prepared in Institute Pharmacy, packed in 1 kg per packets, and stored in a cool and dry atmosphere.[7]
Ingredients of Jeevantyadi Taila (JT) were procured from local market. JT was prepared in the Department of Rasashastra and Bhaishajya Kalpana, packed in 10 ml dropper bottles, and stored in cool dry dark place.[8] Authentication of each drug of the formulation before pharmaceutical process was done in the Pharmacognosy Laboratory.
The study is open-labeled, randomized, controlled study, started after obtaining Ethical Clearance from Institutional Ethics Committee (PGT/7-A/Ethics 2011-2012/2796 dated 09/12/2011). The study was registered at CTRI prospectively (CTRI/2013/06/003725).
The patients fulfilling inclusion criteria attending outpatient department (OPD) and inpatient department (IPD), irrespective of their chronicity of POAG, sex, race, religion, and occupation, were selected. All the patients were subjected to a thorough ophthalmic examination including automated static perimetry and optical coherence tomography.
Sampling method
A total of 91 patients (174 eyes) of POAG were included in the study. The type of study was randomized controlled clinical study with black box design. The patients were randomly divided between the two groups. The number of patients in Group A was 45 (86 eyes) and in Group B was 46 (88 eyes). Group A (trial group): The patients who were on topical antiglaucoma treatment (betaxolol [0.1%] or timolol [0.5%]) (non-iobrim) were subjected for Ayurvedic treatment protocol. The herbomineral compound VFP (Chakshushya Rasayana) orally was given with Triphala Ghrita and Madhu as vehicle along with JT Nasya (oleation through nasal route) and Tarpana (ocular therapeutic procedure eye satiation) with Go-Ghrita. Group B (control group): The patients of this group were put on for brimonidine (iobrim) 0.2% eye drops, 1 drop once daily or twice daily depending on the condition.
Inclusion criteria
Patients aged between 40 and 70 years
Patients of POAG having IOP <21 mmHg with GON, normotensive glaucoma, and IOP >21 mmHg with GON
GON of early to severe stage
Patients with IOP >26, having parapapillary changes, having elaborate retinal nerve fiber layer (RNFL) defects, and having a vertical elaborate CDR 0.4 or more who are glaucoma suspects (ocular hypertension with high risk of POAG).
Exclusion criteria
All types of ACG
End-stage GON having only central vision (tunnel vision)
Ocular hypertension having very low/moderate risk of POAG
Secondary and developmental glaucoma including exfoliative glaucoma, pigmentary glaucoma, trauma induced and inflammatory glaucoma
POAG with advanced stage of optic atrophy with blindness
POAG associated with any other chorioretinal lesions such as severe myopic degeneration, atypical RP (BRVO elaborate) and chorio retinitis
OAG associated with OD lesions such as drusen, coloboma, papillitis, papilledema and any compressive optic nerve lesions
Patients of POAG who have media opacities due to well-developed cataract or any other causes which is sufficient to interfere with detailed ONH evaluation.
Investigations
Hemoglobin %, random blood sugar and lipid profile were carried out before treatment (if history of anemia, diabetes, and obese patient).
Grouping and posology
Group A
Forty-five patients completed the study in this group. The patients were subjected for preparatory phase as follows:
Deepana-Pachana (drugs which improve digestion and metabolism) – given for the duration of 2–3 days using Amapachana Vati/Chitrakadi Vati in the dose as per the requirement of the patient[9]
Sadhyo Virechana (purgation) with Dashamoola Kwatha - 50 ml, Dugdha (milk) - 100 ml, Eranda Taila (castor oil) - 20 ml at bed time for 1 to 2 days after step 1 as per the requirement.
After preparatory phase, the following main line of management was adopted in addition to betaxolol (0.1%) or timolol (0.5%) topical antiglaucoma (IOP lowering) treatment.
Nasya Karma (oleation through nasal route) - 8 drops/nostril of JT transnasally for seven days/month for 3 sittings in 3 months was given
Akshi Tarpana (eye satiation) - Akshi Tarpana was performed with plain Go-Ghrita for 7 days/month, average quantity 40 ml/sitting for 15 min/day for 3 sittings in 3 months.
Nasya and Tarpana procedures were carried out simultaneously on the same day. Second and third month sitting of Nasya Karma and Tarpana preceded by 7 days gap.
Schedule of Nasya and Tarpana: First month: From 1st to 7th day of the month, Nasya Karma and Akshi Tarpana were performed
Second and third month: From 1st to 7th day of the month, Nasya Karma was performed, followed by Akshi Tarpana from day 15th to 21th of the month.
Oral medicine – VFP 6 g/day for 3 months added with Triphla Ghrita and honey at night followed by 100 ml milk (3 h after dinner) once a day.
Group B (control group)
Forty-six patients completed this study in this group. The patients of this group were put on for brimonidine (iobrim) 0.2% eye drops, 1 drop once daily or twice daily depending on the condition.
Total duration of treatment was 3 months.
Follow-up
Follow-up was done for 60 days after treatment. During this period, the patients were asked to visit once in a month for assessment.
Enrolled patients in both the groups were advised to continue modern antiglaucoma treatment and stay away from the identified and known etiological factors. They were also advised to have a control over DM and HTN illnesses if any.
Assessment
Effect of treatment was assessed on the basis of subjective and objective parameters. The parameters included are as follows:
-
Subjective parameters
- Blurred vision (BV)
- Frequent changes of presbyopic glasses (FCPG)
- Delayed dark adaptation (DDA)
- Visual field defects (VFDs)
-
Objective parameters
- Best-corrected visual acuity (BCVA)
- Goldmann applanation tonometry (GAT)
-
ONH changes examined by direct/indirect ophthalmoscopy (DO/IDO) examination and slit lamp examination (SLE) with 90 D lens[10]
- Vertical cup-disc ratio
- Polar notching
- Diffuse thinning
- Disc hemorrhages (splinter hemorrhage)
- Retinal nerve fiber layer defect
- Peripapillary atrophy
- Nasalization of blood vessels
- Bayonetting of blood vessels
- Baring of blood vessels
- Over passing/bridging of blood vessels
- Disc damage likelihood scale
-
Automated static perimetry (Opto/Medmont) with central 22°/glaucoma screening/glaucoma threshold patterns
- Mean deviation (MD)
- Number of points (NOP) depressed at P < 0.5% level
- NOP depressed at P < 0.1% level
- NOP present in central 5° at <15 dB
- NOP present in central 5° at <0 dB
- Hemifield pairs in central 5° with <15 dB
-
Optical coherence tomography (OCT) by Zeiss Stratus OCT to assess[11]
- Average RNFL thickness
- Superior average RNFL thickness
- Inferior average RNFL thickness
- Hodapp glaucoma staging.[12]
All the investigations were carried out in the Institute Hospital, except the OCT that was performed in the eye care hospital at Jamnagar.
Analysis of the data and presentation of the results
The data obtained were assessed using paired and unpaired t-test.
Observations
Total patients enrolled in this study were 102 (52 in Group A, 50 in Group B), of which 91 have completed the study (45 in Group A, 46 in Group B). Six patients could not visit the OPD at regular intervals because of their busy working schedules. Two patients shifted from the study center to other places, while three did not turn up after baseline examination due to unknown causes.
Positive family history of glaucoma was observed in 5.88% patients, 80.39% patients were under medical management, and 59.80% were taking allopathic treatment for GON. Highest number of patients (39.21%) had a chronicity of 1–3 years. Diabetes mellitus was associated with POAG, i.e., 15.55% in Group A and 12.75% in Group B.
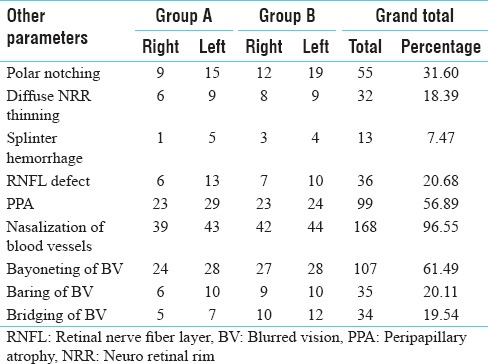
Table 1 shows the incidence of ONH signs observed on DO/IDO/90 D SLE.
Table 1.
Incidence of optic nerve head signs observed on DO/IDO/90 D slit lamp examination
Results
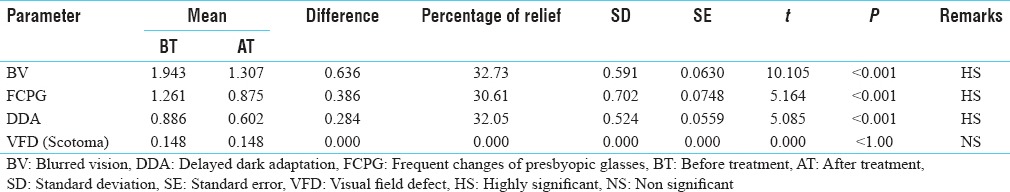
Statistically highly significant (P < 0.001) improvement was observed in BV, FCPG, and DDA as depicted in Table 2 in Group A; analysis of the VFD shows that the result was statistically significant (P < 0.1). Statistically highly significant (P < 0.001) improvement was observed in BV, FCPG, and DDA in Group B [Table 3]; analysis of the VFD shows that the result was statistically insignificant (P < 1.0).
Table 2.
Effect of therapy on subjective parameters in Group A (n=86)
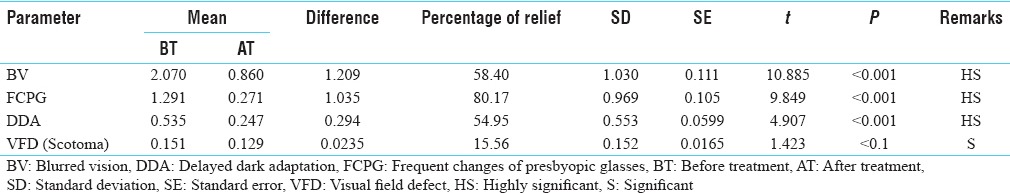
Table 3.
Effect of therapy on subjective parameters in Group B (n=88)
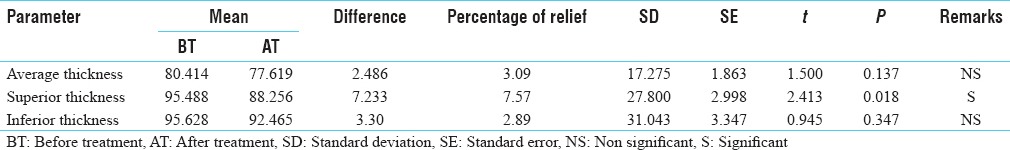
Statistically highly significant (P < 0.001) improvement was observed in BCVA and GAT in Group A [Table 4]; analysis of the GON staging showed that the result was statistically insignificant (P < 0.5). Statistically highly significant (P < 0.001) improvement was observed in NOP depressed at P < 5% and NOP depressed at P < 1% level. Analysis of the MD showed that the result was statistically significant (P < 0.02) and analysis of the NOP depressed < 15 dB level in central 5°, NOP depressed < 0 dB level in central 5°, and hemifield pairs in central 5° <15 dB showed that the result was statistically insignificant (P < 0.5) in Group A [Table 5]. Statistically highly significant (P < 0.001) improvement was observed in RNFL superior thickness; analysis of the total average thickness and inferior average thickness showed that the result was statistically in significant (P < 0.5) in Group A [Table 6].
Table 4.
Effect of therapy on objective parameters (best-corrected visual acuity/Goldmann applanation tonometry/glaucomatous optic neuropathy) in Group A (n=86)
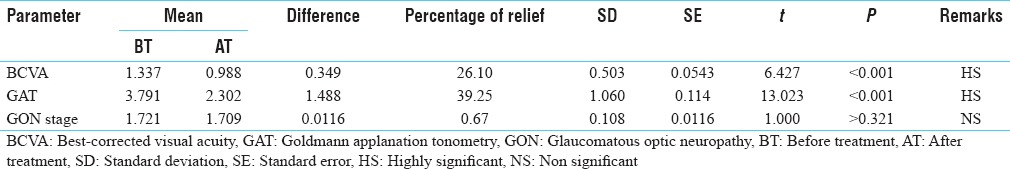
Table 5.
Effect of therapy on perimetry examination findings in Group A (n=86)
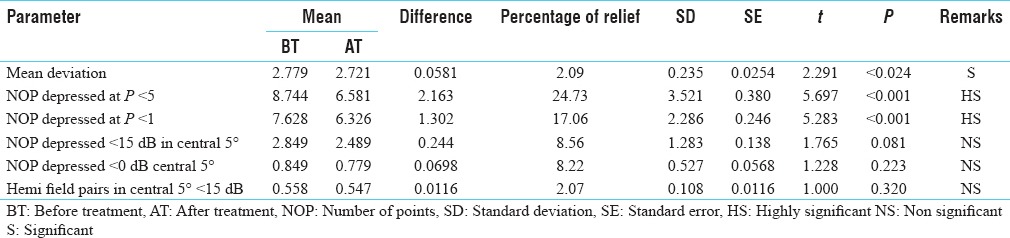
Table 6.
Effect of therapy on retinal nerve fiber thickness in Group A (n=86)
Statistically highly significant (P < 0.001) improvement was observed in BCVA and GAT and analysis of the GON staging showed that the result was statistically insignificant (P < 1.0) in Group B [Table 7]. Analysis of the NOP depressed at P < 5% probability showed that the result was statistically significant (P < 0.1) and other perimetry findings such as MD, NOP depressed at P < 1% level, NOP depressed <15 dB level in central 5°, NOP depressed < 0 dB level central 5°, and hemifield pairs in central 5° <15 dB, all were found to be statistically insignificant in Group B [Table 8]. Statistically significant (P < 0.1) improvement was observed in RNFL superior thickness and analysis of total average thickness and inferior average thickness showed that the result was statistically insignificant (P > 0.5) in Group B [Table 9].
Table 7.
Effect of therapy on objective parameters (best-corrected visual acuity/Goldmann applanation tonometry/glaucomatous optic neuropathy) in Group B (n=88)
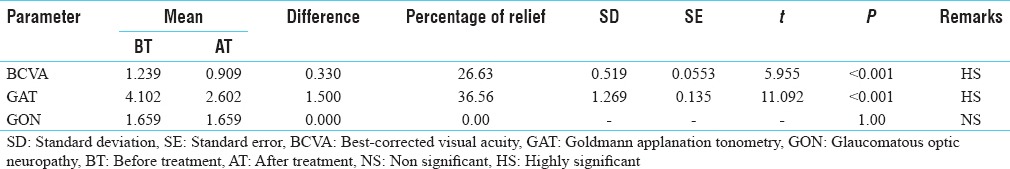
Table 8.
Effect of therapy on perimetry examination findings in Group B (n=88)
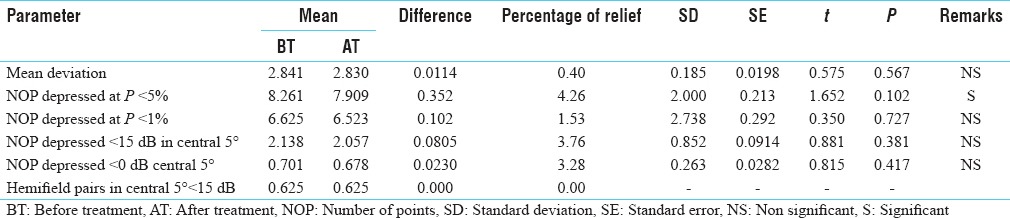
Table 9.
Effect of therapy on retinal nerve fiber thickness in Group B (n=88)
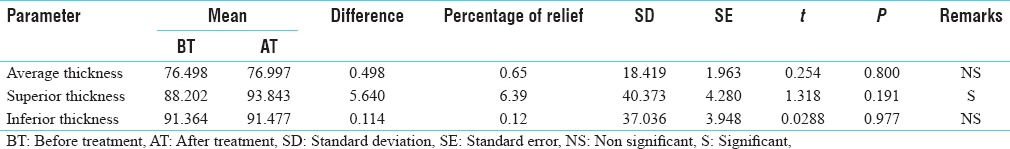
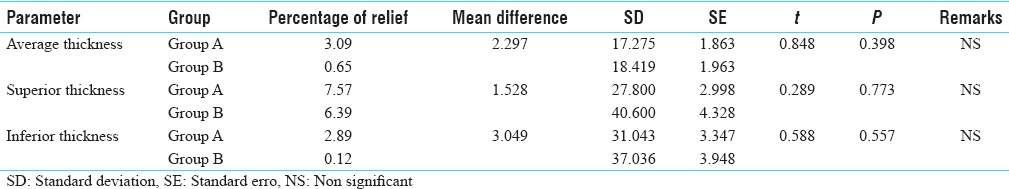
Comparative effect of treatment [Table 10] between the groups showed difference in BV and FCPG which was statistically highly significant. Group A treatment showed better percentage of improvement than Group B. The difference between the two methods of treatment, in DDA and VFD, was statistically significant. Group A clinically (subjectively) provided better percentage of improvement than Group B. However the difference between the two methods of treatment in BCVA, GAT and GON staging was statistically insignificant.
Table 10.
Combined effect of therapy on subjective parameters in both Group A and Group B (n=174)
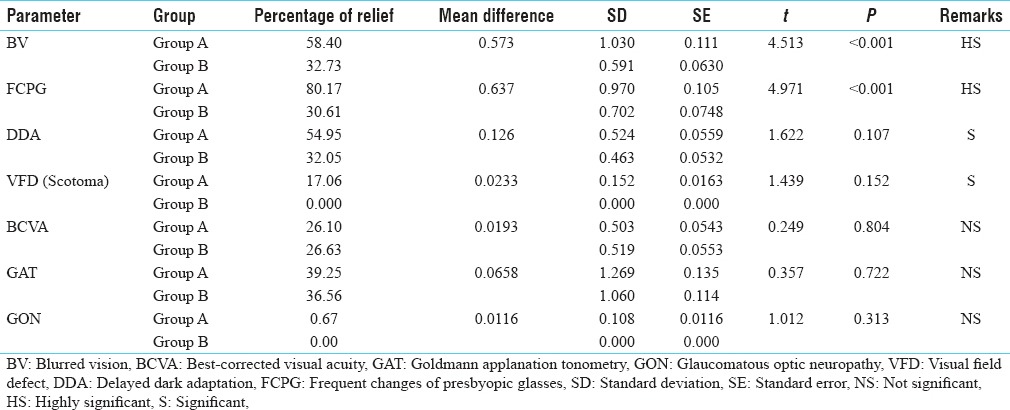
Analysis of the comparative effect of treatment on perimetry findings between the Group A and B showed that the difference between the two methods of treatment in NOP depressed at P < 5% and NOP depressed at P < 1% level was statistically highly significant. Group A treatment plan showed better percentage of improvement than Group B. The difference between two groups in treating MD was statistically significant (P < 0.1). However, the difference between the two methods of treatment in NOP depressed <15 dB level in central 5°, NOP depressed <0 dB level in central 5°, and hemifield pairs in central 5° <15 dB is statistically insignificant. Group A clinically provided better percentage of improvement than Group B [Table 11].
Table 11.
Combined effect of therapy on perimetry findings in both Group A and Group B (n=174)
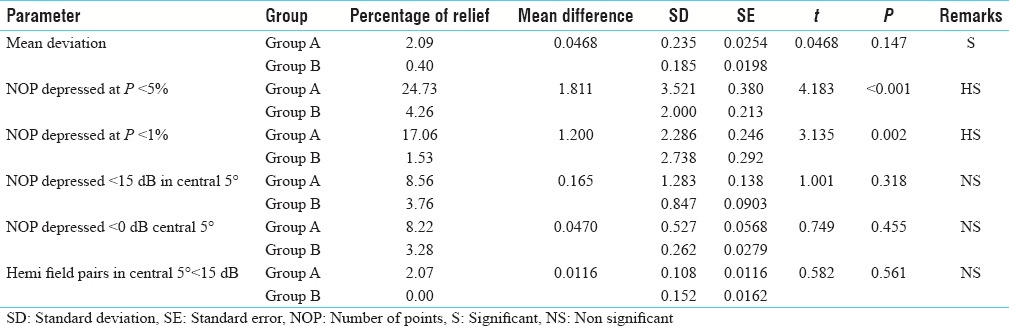
A careful analysis of the comparative effect of treatment between the Groups A and B on RNFL thickness showed that the difference between the two methods of treatment was statistically insignificant (P < 0.5). However, Group A strategy provided better percentage of relief than Group B clinically [Table 12].
Table 12.
Combined effect of therapy on retinal nerve fiber layer thickness in both Group A and Group B (n=174)
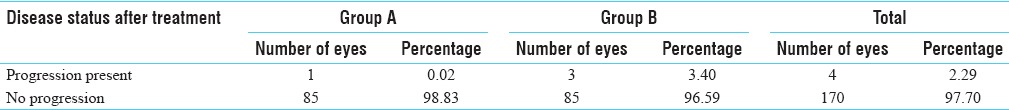
The overall assessment of the treatment showed that in Group A, progression was observed, and in 98.83% of the eyes, there was no progression, whereas in Group B, 3.40% of the eyes showed signs of progression and the rest 96.59% of the eyes showed no progression in the disease [Table 13].
Table 13.
Progression of glaucoma after treatment
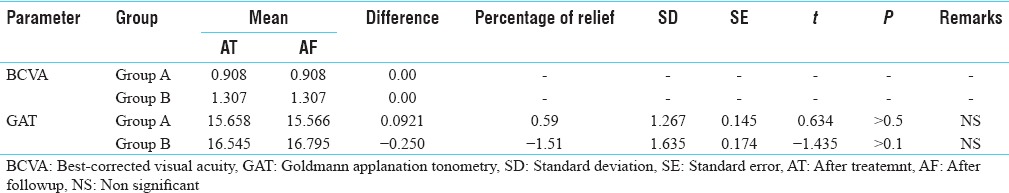
After a follow-up of 3 months analysis of recurrence BCVA rate showed that there was no change in the condition during the follow-up period in both the groups. Analysis of GAT rate of recurrence showed that even in the follow-up period, GAT value was well maintained in Group A than in Group B [Table 14].
Table 14.
Rate of recurrence in best-corrected visual acuity and Goldmann applanation tonometry after follow-up period in Group A and Group B (N=86 and 88)
Discussion
Rasayana refers to the nutrition and its transportation in the body. Rasayana is actually that which increases the essence of each Dhatu, starting from Rasa. Such a state of improved nutrition is claimed to lead to a series of secondary attributes such as longevity, immunity against diseases, enhancing the function of sense organs, increasing the mental competence and delaying of aging. Immunomodulators are considered now as one of the most potent tools in the preservation of health and management of disease by modern medicine. VFP is a unique rejuvenating poly-herbomineral compound used in the treatment of Vataja Timira. The drug taken in a powder form offers some unique advantages such as it can be administered easily with Anupana to all people who are averse to swallow tablets/capsules and powders will have a rapid onset of action since disintegration is not required; hence, the drug was selected in powder form.
Chakshushya Rasayana group of drugs are defined as the one which apart from having Rasayana property possess the special affinity to visual apparatus resulting in vision promotion, helps in bringing homeostasis in the eye, rejuvenates the eye structurally and functionally and thus protecting the eye from easily getting afflicted by any disease. The drugs and treatment protocol selected are having antioxidants, neuroprotective, healing, adaptability, and immunity enhancing properties. The previously diagnosed patients who were on timolol/betaxolol eye drops were asked to continue their antiglaucoma topical medicines and taken under Group A. Newly diagnosed patients were advised with brimonidine eye drops after consultation with modern ophthalmologist (Group B). Brimonidine has got some neuroprotective effect with its IOP lowering effect that is why to avoid summative effect of neuroprotection of brimonidine, Group A was designed with beta-blocker eye drops.[13] This was also helpful to compare the neuroprotective effect of Chakshushya Rasayana and brimonidine. With this background in mind, the present clinical study was planned.
Of 102 registered patients of glaucoma, maximum patients had Swapna Viparyaya (im proper sleep pattern) and in this, about 40% patients had Alpa Nidra (insomnia) due to various causes. In the Aharaja Nidana (dietetic factor), maximum numbers of patients were having regular habit of taking Masha-Kulatha-Amla-Suktha Aharas. In the Viharaja Nidana (daily activities) a maximum number of patients had Atapa-Anala Sevana of about 23.52 % was repoted. Swapna Viparyaya leads to Agni Mandya and Vata Prakopa. Vidahi-Katu-Amla Rasa leads to Pitta-Vata Prakopa and Sama Rasa-Rakta Dhatu. The researches have shown excessive exposure to intense light (including UV radiation) may damage or cause the death of RGCs leading to formation of glaucoma. Excessive near-work requires excessive convergence, i.e., strain in the eyes which may bring the degenerative changes in the eye including trabecular meshwork resulting in glaucoma. This also causes Vata Prakopa in the Netra which brings loss of equilibrium of other two Doshas resulting in Netra Roga.
Effects of therapies were assessed in a total of 91 patients of Group A and Group B. Both the groups showed statistically highly significant results in many of the subjective as well as objective parameters. According to the percentage relief-wise observation in clinical features, few parameters showed some variations in the efficacy between the groups. On analysis of the effect of therapy, it was observed that BV, FCPG, and DDA were statistically highly significant (P < 0.001) improved in both Groups A and B. However, the percentage of improvement in Group A was greater than Group B. The literature also says that the cause for these symptoms is raised IOP. The Chakshushya drugs such as Jeevanti, Shatavari, Triphala, Rasayana Choorna, and Swarna Makshika Bhasma by virtue of their Guru-Snigdha Guna, Madhura-Kashaya-Tikta Rasa, Sheeta Veerya, Madhura Vipaka, and Jivaniya/Brimhaniya (anabolic) property might have shown this improvement. On analysis of the effect of therapy, it was observed that there was no change in the morphologic changes seen in ONH, before and after treatment in both the groups. This indicates that the visible structural damages once occurred are variable. A long period treatment protocol is required for its treatment.
The effect of therapy on BCVA in both the groups was statistically highly significant (P < 0.001) with equal percentage of relief (26%). BCVA is not directly related with the severity of glaucoma unless the refractive media including cornea, quality of aqueous humor and macular regions are not involved. The incidence of higher visual disturbance was greater in Group A than Group B. This may be the cause for not getting higher percentage of relief in Group A. In Group A, better control of IOP with Chakshushya Rasayana therapy and its neuroenhancer effect might have brought this much of improvement in BCVA in spite of having higher visual disturbance in the patients compared to Group B which may have accidentally occurred on its own without any bias. The effect of therapy on GAT in both the groups was statistically highly significant (P < 0.001). The literature says that raised IOP is one of the major risk factors for glaucoma progression and optic nerve damage. The Guru-Snigdha Guna, Madhura-Tikta-Kashaya Rasa and Sheeta Veerya checks the degeneration and enhance repairing of the tissue, there by re-establishing channels. By this way, the IOP might have better controlled in trial group than the control group where IOP was reduced by inhibiting the production of aqueous. Hence, the combined approach of modern antiglaucoma treatment along with the Chakshushya Rasayana regimen will definitely better manage the condition. Analysis showed that the effect of therapy in perimetry on NOP depressed at P < 5% probability, P < 1% probability was statistically highly significant (P < 0.001) in trial group, whereas in control group for NOP depressed at <5%, probability was significant, and <1%, probability was insignificant (P > 0.5). This implies that the loss of retinal sensitivity within <12 dB (3–6 dB at 5% probability and 6–12 dB at 1% probability) was improved after treatment in Group A.
The RGCs which are the cause for the retinal sensitivity may be improving their functional level which was severely damaged earlier. This might have been occurred in many ways by the drug therapy interrupting the pathogenesis at many levels. The drugs with their Sukshma Srotogami and Marga Vishodhana property cleared the channels (removing Sanga/Margavarodha). The drugs by their Guru-Snigdha Guna, Madhura Rasa, Sheeta Veerya, and Vata Shamana properties cause Vatanulomana and Dhatu Poshana (anabolic function). The Kashaya-Tikta-Madhura Rasa might have helped in healing the degenerated Dhatu. The drugs by of their Balya-Jeevaniya (anabolic function) action strengthen the microvessels, and thus, the overall effect was improved by nourishment, healing, and regeneration of the lost tissue. This overall drug effect at multilevel improved the RGC functions, thereby improving the retinal sensitivity. This proves that the Ayurvedic Chakshushya Rasayana therapy has a significant level of effect in bringing back the lost RGCs function, especially when administered as adjuvant along with the modern antiglaucoma therapy.
Analysis of the effect of therapy on RNFL thickness showed that the superior thickness of RNFL improved statistically which was highly significan in Group A, when compared to statistically significant improvement in Group B. This is one of the important indicators to assess the structural damage for GON. RNFL thickness which was decreased before the treatment was improved after treatment significantly. This indicates improved retinal sensitivity after the treatment which also justifies the improvement of retinal sensitivity seen in the perimetry findings at P < 5% and P < 1% probability. The mechanism of function may be similar to that as explained to effect of therapy in perimetry findings. Overall assessment of the treatment showed that in Group A, showed 1 (1.3%) eyes progression was observed, and in 85 (98.83%) eyes, there was no progression, whereas in Group B, 3 (3.40%) eyes had shown signs of progression and the rest 85 (96.59%) eyes had no progression in the disease. This proves that better prevention of rate of progression in Group A as compared to Group B, may be due to the effect of overall Chakshushya Rasayana therapy. Better maintenance of IOP during follow-up period in group A compared to Group B patients can be attributed to the effect of overall Chakshushya Rasayana therapy, effect of which was still persisting during the follow-up period of 2 months.
Conclusion
Deepana/Pachana and Koshtha-Shuddhi (digestion and metabolism) protocol as the preparatory phase was adopted in this clinical trial for relieving the Srotorodha (microchannel obstruction) thus preparing the body for Rasayana therapy.Nasya Karma (Trans nasal medication) as the main treatment protocol further helped in the microchannel clearance and revitalization of the supraclavicular structures.[14] Chakshushya Rasayana the rejuvenating/revitalizing drugs with special affinity to visual apparatus structurally and physiologically enhanced adaptability and immunity of eye thus helped in maintaining the homeostasis. Significant improvement was observed in subjective parameter in Group A such as BV, FCPG and DDA. Improvement in the MD i.e., the average retinal sensitivity in Group A (trial group) showed just significant effect on statistical analysis, whereas in Group B (control group), the response was statistically insignificant. The inference is that RGCs normal physiology may have started to reverse with Chakshushya Rasayana treatment protocol within 3 months of duration. The antioxidants, neuroprotection, healing, immunomodulatory action of flavonoids, alkaloids, glycosides, carbohydrates, and tannins on phytochemical analysis of compound formulation seems to be responsible for altering the status of GON.[15]
Thus, it can be concluded that Chakshushya Rasayana protocol if administered in a systematic approach along with a modern topical antiglaucoma drops has a definite role in improving the lost retinal sensitivity as much as up to 12 dB in 3 months duration. Early intervention with this treatment protocol is expected to fourfold the outcome.
Financial support and sponsorship
IPGT and RA, GAU.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Shields MB. Shields Textbook of Glaucoma. 6th ed. Baltimore, Maryland: Lippincott Williams and Wilkins Publishers; 2005. p. 129. 176. [Google Scholar]
- 2.Sihota R, Tandon R. Parsons Diseases of the Eye. 22nd ed. Gurgaon: Elsevier Publication; 2015. p. 563. [Google Scholar]
- 3.Sihota R, Tandon R. Parsons Diseases of the Eye. 22nd ed. Gurgaon: Elsevier Publication; 2015. p. 296. [Google Scholar]
- 4.National Survey on Blindness. Report. 2001-2002. Govt. of India, NBCP-India newsletter, Jan.-March. 2013:4. [Google Scholar]
- 5.Khurana AK. Comprehensive Ophthalmology. 6th ed. New Delhi: Jaypee The Health Science Publisher; 2015. p. 478. [Google Scholar]
- 6.Khurana AK. Comprehensive Ophthalmology. 6th ed. New Delhi: Jaypee The Health Science Publisher; 2015. p. 224. [Google Scholar]
- 7.Arundutta H, editor. Ashtanga Hridayam of Vagbhatta, Uttaratantra. 9th ed. Ch. 13. Ver. 16. Varanasi: Chaukhamba Orientalia; 2005. p. 949. [Google Scholar]
- 8.Arundutta H, editor. Ashtanga Hridayam of Vagbhatta, Uttaratantra. 9th ed. Ch. 13, Ver. 51. Varanasi: Chaukhamba Orientalia; 2005. p. 956. [Google Scholar]
- 9.Acharya YT, editor. Charaka Samhita of Agnivesha, Chikitsa Sthana. 2nd ed. Ch. 15. Ver. 97. Varanasi: Chaukhamba Sanskrit Sansthan; 1990. p. 567. [Google Scholar]
- 10.Weinreb RN, Krieglstein K. Glaucoma in the 21st Century. 1st ed. California: Harcourt Health Communications; 2000. p. 9. [Google Scholar]
- 11.Weinreb RN, Krieglstein K. Glaucoma in the 21st Century. 1st ed. California: Harcourt Health Communications; 2000. p. 15. [Google Scholar]
- 12.Hodappe E, Parish RK, Anderson DR. Clinical Decision in Glaucoma. St. Louis, Missouri: C.V. Mosby Co; 1993. pp. 52–61. [Google Scholar]
- 13.Galanopoulos A, Goldberg I. Clinical efficacy and neuroprotective effects of brimonidine in the management of glaucoma and ocular hypertension. Clin Ophthalmol. 2009;3:117–22. [PMC free article] [PubMed] [Google Scholar]
- 14.Shastri AD, editor. Sushruta Samhita of Sushruta, Chikisa Sthana. Reprint ed. Ch. 40. Ver. 23. Varanasi: Chaukhamba Sanskrit Sansthan; 2012. p. 225. [Google Scholar]
- 15.Adoor V, Dhiman KS. Pharmacognostical & physico-chemical evaluation of vara fort powder – A poly herbo-mineral compound in the management of GON. Int J Recent Adv Pharm Res. 2013;3:38–46. [Google Scholar]


