Abstract
Sub-axial cervical spine injuries are commonly seen in patients with blunt trauma. They may be associated with spinal cord injury resulting in tetraplegia and severe permanent disability. Immobilization of the neck, maintenance of blood pressure and oxygenation, rapid clinical and radiological assessment of all injuries, and realignment of the spinal column are the key steps in the emergency management of these injuries. The role of intravenous methylprednisolone administration in acute spinal cord injuries remains controversial. The definitive management of these injuries is based upon recognition of the fracture pattern, assessment of the degree of instability, the presence or absence of neurologic deficit, and other patient related factors that may influence the outcome. Nonoperative treatment comprises of some form of external immobilization for 8 to 12 weeks, followed by imaging to assess fracture healing, and to rule out instability. The goals of surgery are realignment of the vertebral column, decompression of the neural elements and instrumented stabilization.
Keywords: Subaxial cervical spine injury, emergency management, decision making, surgical management
MeSH terms: Spinal cord injuries, cervical vertebrae, neurological aspects, emergency treatment
Introduction
A cervical spine injury occurs in 2%–3% of all blunt trauma victims.1 Injuries may range from minor ligament strains to complete fracture-dislocations resulting in severe spinal cord injury (SCI). Approximately two-third of all fractures, and three-fourth of all dislocations involve the subaxial cervical spine.2 The sixth and seventh cervical vertebra together account for 39% of all cervical spine fractures. The most common causes of cervical spine injury are motor vehicular accidents (41%), falls (27%), violence (15%), sports-related injuries (8%), and fall of a heavy object on the head.3,4
A SCI is seen in 1.3% of all blunt trauma victims.5,6 Eighty percent of patients with associated SCI are males, and 40% are between 18 and 44 years of age.7 The C5–C7 region contributes to 60% of all SCI in patients with cervical spine trauma. Incomplete quadriplegia is found in 40% of patients with spinal cord involvement, complete paraplegia in 22%, incomplete paraplegia in 22%, and complete quadriplegia in 16%.6 The overall mortality rate from cervical spine injuries is approximately 6%.8
The management of patients with cervical spine injuries involves three phases – pre-hospital care, emergency in-hospital care, and definitive treatment. In countries such as the USA, improvements in patient retrieval methods, the use of effective restraints including airbags and enforcement of drunk driving laws has resulted in a lower incidence of SCI, and a higher proportion of incomplete rather than complete SCI.5 Improvement in prehospital and emergency in-hospital care has also resulted in an improved prognosis for survival and possibly even recovery from incomplete neurologic injury.6
This study discusses current concepts in the in-hospital care of the patient including the clinical assessment, the radiological assessment, the neuroprotective strategy, closed reduction, as well as the indications for surgery and the surgical approach based on the pattern of injury.
Emergency In-hospital Care
The early in-hospital management includes hemodynamic stabilization which proceeds concurrently with a clinical and radiological assessment of the patient. During this period, immobilization of the cervical spine is a priority. It is estimated that 3%–25% of SCI are incurred after the initial impact.9 Immobilization of the cervical spine is done in the “neutral position,” defined as the normal anatomic position of the head and torso that one assumes while standing and looking ahead. This is usually achieved by providing 1.5–5 cm of padding below the occiput when on the spine board.10 A rigid cervical collar should be used along with tapes to secure the patient at the forehead, thorax, and extremities.
The goals of emergency management are to:
Stabilize vital parameters
Look for head/chest/long bone injuries
Identify a cervical spine injury
Look for other spinal injuries
Assess the neurological status
Administration of steroids
Perform appropriate imaging
Reduction of fractures/dislocations.
Stabilize vital parameters
All patients with a suspected cervical spine injury must undergo a primary survey as per the Advanced Trauma Life Support protocols.11 This includes clearance of airway, support of breathing, maintenance of circulation, assessment of disability (neurological status), and exposure. A severe cervical SCI may present with neurogenic shock (hypotension), bradycardia, and hypothermia. This should be differentiated from hypotensive shock where hypotension is accompanied by tachycardia. Hypoventilation occurs due to paralysis of respiratory musculature. Management includes giving a Trendelenburg position, intravenous (IV) fluids and if necessary, administration of inotropic agents such as dopamine or dobutamine (2.5–20 μg/kg/min). Bradycardia may need to be treated with IV atropine. Maintenance of blood pressure and oxygenation is vital to prevent secondary SCI. Neurogenic shock may take from 1 to 3 weeks to recover.
As hemodynamic stability is achieved, the patient goes through a secondary survey, which includes a detailed history and examination to ascertain the mechanism of injury and ascertain any underlying conditions such as ankylosing spondylitis, and medical comorbidities.
Look for head/chest/long bone injuries
Approximately 47% of spinal trauma victims have associated injuries.12 Hyperflexion and axial compression of the cervical spine associated with vehicular accidents or falls may result in concomitant head injuries in 35% of patients.13 Chest injuries are seen in 24% of patients, and extra-spinal fractures to ribs, sternum, clavicle, scapula, mandible, etc., occur in 28% of patients.14
Vertebral artery injuries (VAIs) occur in 17%–46% of non-penetrating cervical spine trauma.15,16,17 Injury to the cervical spine at multiple levels (73%) is more likely to cause VAI than single level injury (27%). Flexion-distraction and flexion-compression injuries are a frequent cause (19.7%) of VAI.18 Unilateral VAI is more common than bilateral involvement. Stretching or compression of the vertebral artery, are the mechanisms by which this injury can occur. Many of these injuries are asymptomatic and hence missed. Symptoms such as dysarthria, dizziness, diplopia, dysphagia, blurred vision, and tinnitus may appear immediately or even up to 3 months following the injury. Magnetic resonance (MR) angiogram is used to diagnose this injury in a symptomatic patient.19 In asymptomatic patients, no formal treatment is recommended. In symptomatic patients, the treatment options range from fibrinolysis with streptokinase to anticoagulation with heparin and warfarin to surgical treatment.20 When surgery is required for a dissecting vertebral artery, ligation of the injured artery proximal and distal to the site of lesion is recommended provided there is adequate collateral blood flow.21
Identify a cervical spine injury
The presence of point tenderness, bruising or hematoma, a palpable step, and restricted/painful neck movements help to diagnose a cervical spine injury. A laceration of the forehead may indicate an extension injury, and one on the occiput suggests a flexion injury. However, Duane et al.22 have reported limited sensitivity (77%) of clinical examination in diagnosing cervical spine fractures in patients with blunt trauma so that as many as 30% of cervical spine injuries are initially missed23 and up to 29% can develop secondary neurological deterioration.24
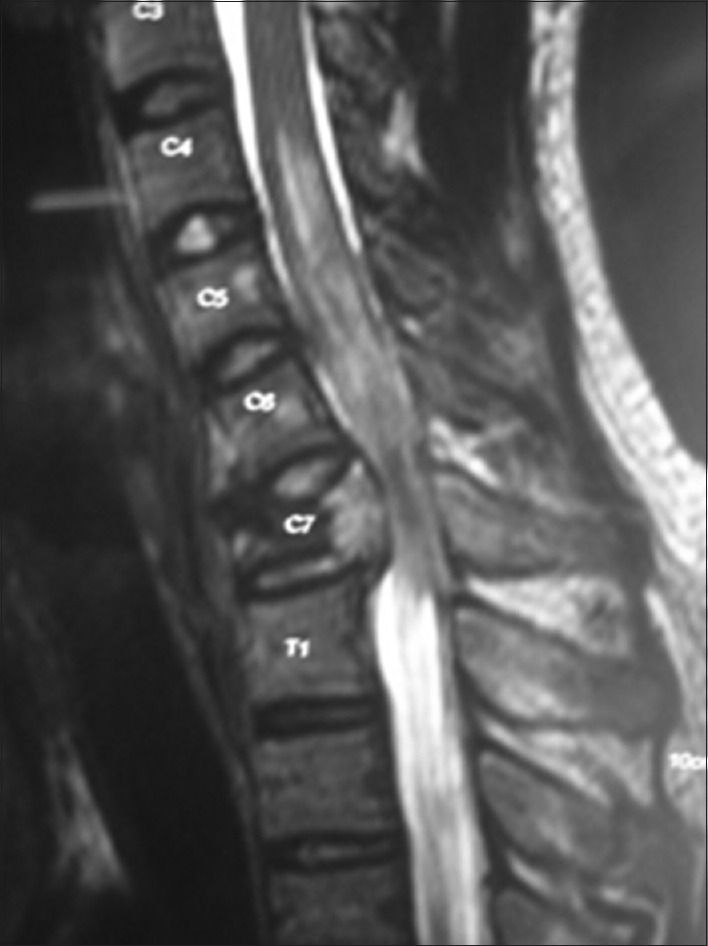
To easily identify patients with significant cervical spine injuries who may benefit from radiographic assessment, the NEXUS study [Table 1]25 suggests that in an awake, alert and asymptomatic patient, who is not intoxicated and does not suffer from any major distracting injuries or a focal neurological deficit, the absence of posterior midline tenderness is a sensitive (99.6%) predictor of the absence of a significant cervical spine injury. All symptomatic patients must undergo imaging.
Table 1.
Criteria established by NEXUS group to screen for patients with cervical spine injuries
Look for other spinal injuries
The incidence of a second noncontiguous cervical injury or an injury elsewhere in the spine is 15%–20%.26,27 Hence, the entire spine must be palpated and imaged to rule out a second spinal injury, especially in patients with neurological deficits who may not complain of pain below the level of the lesion.
Assess the neurological status
A thorough, accurate and well-documented neurological examination is absolutely vital. Periodic re-assessment should be done and compared to the baseline neurology to identify improvement or deterioration.
Patients with SCI often present with spinal shock. This results in loss of reflexes and sensorimotor function below the level of a SCI, and manifests as flaccid paralysis, including loss of bladder and bowel reflexes and anal tone. Spinal shock generally lasts for 24–72 h. Recovery from spinal shock is heralded by the reappearance of the bulbocavernosus reflex and the anal wink. Once the patient recovers from the spinal shock, a detailed neurological examination must be done and recorded.
The absence of voluntary motor function and sensations below the level of SCI, including the absence of sacral sparing, indicates a complete lesion. The sacral fibers at the periphery of the spinal cord are extremely resistant to injury, and hence may be spared from trauma. The presence of voluntary rectal tone, perianal sensations, and great toe flexion are indicators of sacral sparing. A complete lesion after the termination of spinal shock is unlikely to show significant neurological recovery. An incomplete lesion has a relatively better prognosis in terms of neurological recovery.
Role of steroids
In recent years, a number of neuroprotective agents have been extensively studied with the goal of limiting the secondary SCI. Most of these agents have failed to provide substantial benefit and are not recommended for routine use. However, glucocorticoids such as methylprednisolone have been widely used over the past few decades although their role in preventing secondary SCI is still controversial. They may help by minimizing local edema and improving spinal cord blood flow. High dose methylprednisolone (30 mg/kg bolus followed by a 5.4 mg/kg/h infusion) has been recommended for patients with SCI based on recommendations from the NASCIS II and III trials.28,29 If the patient presents within 3 h of injury, steroids are administered for 24 h. For patients presenting between 3 and 8 h after injury, steroids are recommended for 48 h, and for those presenting after 8 h, steroids are contraindicated. In patients with isolated nerve root injury, penetrating injuries or gunshot wounds, steroids are not benseficial.
The methodology used and the interpretation of data from the two NASCIS trials have come under intense criticism in recent years.30 In both the studies, methylprednisolone did not show a significant benefit over placebo, and only post-study stratification into arbitrary groups showed an improvement in neurological outcome in patients treated within 8 h of injury. Hence, a number of centers have now discontinued the use of steroids in the management of SCI. The Spine Focus Panel31 however, continues to recommend the use of steroids based on its modest neuroprotective effect, its favorable risk-benefit ratio and the lack of alternative therapies.
Imaging
The relative role of plain radiographs, dynamic X-rays, computed tomography (CT) scan, and magnetic resonance imaging (MRI) scan in the evaluation of a blunt cervical trauma is still evolving. Hence, the development of a standard protocol for their use is as yet controversial.
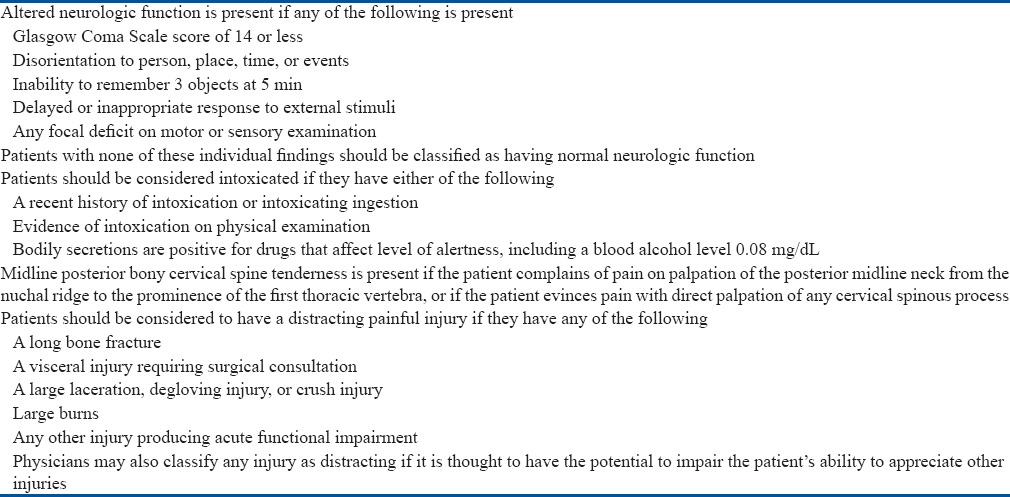
The standard imaging protocol has been a 3-view plain film series including lateral, anteroposterior (AP) and open mouth views. In addition, swimmers’ view may be necessary to visualize the C7-T1 region which accounts for 17% of subaxial injuries2. Increase in width of the prevertebral soft tissue shadow [Figure 1a], loss of alignment on any of the three contour lines [Figure 1b - anterior, posterior, spinolaminar], increase in the interspinous interval, reduction in disc space or vertebral body height, segmental kyphosis/translation and loss of alignment of the spinous processes on the AP view are indicators of a significant cervical spine injury. Inadequate plain radiographs and improper interpretation of images are the most common cause of missed spinal injuries.22
Figure 1.
Lateral cervical spine x-ray showing (a) normal prevertebral soft tissue shadow (b) the three contour lines
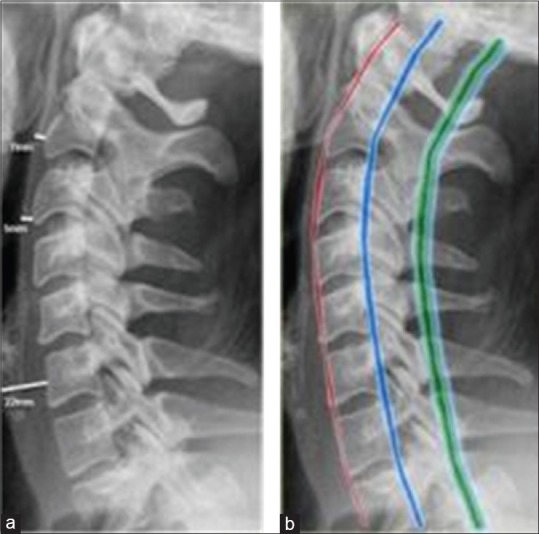
Dynamic views such as flexion extension films help to identify ligament damage by demonstrating abnormal translation/angulation. They are recommended in awake and alert patients with neck pain where plain films are normal. However, pain and spasm may prevent meaningful interpretation of the results, and there is also a danger of worsening the neurological injury.32,33 CT scans help to define the osseous anatomy better. They are especially useful in identifying fractures of the posterior elements [Figure 2] and injuries at the occipitocervical and cervicothoracic junction. Spiral CT has been found to have a sensitivity of 99% and specificity of 100%, with the risk of missed spine injury being 0.04%;34 whereas plain film radiography has a sensitivity of 70%.35 Besides CT scans can be done even on intubated patients. Hence, a number of institutions now routinely use CT scans over plain X-rays in trauma victims who may be at a risk for significant cervical spine injury.36
Figure 2.
Axial computed tomography showing laminar fractures at C7 that were missed on plain X-rays
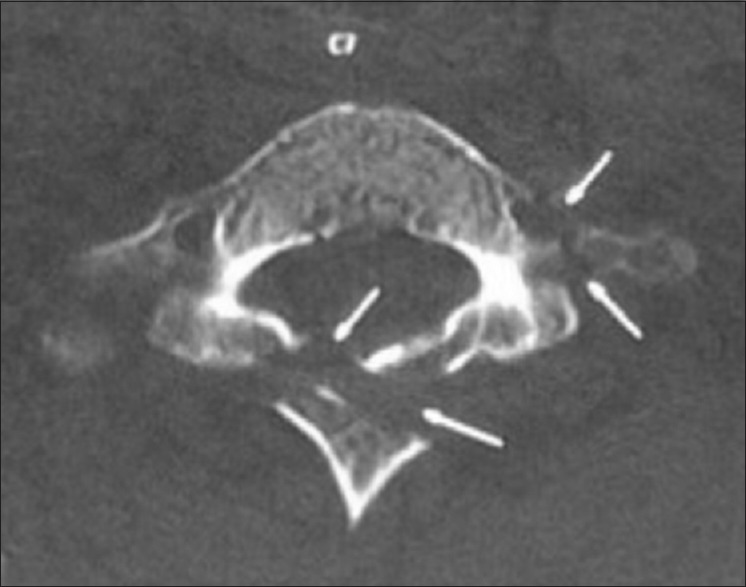
MRI scans are extremely sensitive in identifying injuries to the spinal cord, the intervertebral disc and the posterior ligament complex (PLC)37 [Figure 3]. Besides, they also show the severity of SCI and the direction of compression. However, they do not reveal osseous anatomy adequately. MRI scan is usually advised in any patient with the neurological deficit, or to identify the status of the ligaments, especially in unconscious/intoxicated victims of severe trauma. MR angiography and CT angiography are useful to identify VAI that may occur in up to 11% of cervical spine trauma.38,39
Figure 3.
Sagittal T2W MRI of cervical spine showing severe spinal cord contusion secondary to a C7 fracture with retropulsion
Reduction of fractures/dislocation
Reduction of dislocations and realignment of the spine is probably the single most important intervention in the emergency management that may alter long term neurological outcome by decompressing the neural elements. Hence, it is important to achieve a reduction as early as possible. Restoration of normal alignment also reduces the abnormal stretch of the ligaments and muscles, thereby reducing the pain. Gardner-wells skull tongs are preferred for reduction when the planned definitive treatment after reduction is operative. If nonoperative treatment is planned, then a halo is preferred which can be extended into a halo-vest for definitive nonoperative treatment. The halo has the advantage of multiple point fixation and hence can be used when larger weights are required for reduction or when a manipulative reduction is planned.
A rapid reduction is performed in an awake, alert patient in the Intensive Care Unit. For patients with a unifacet or bifacet dislocation,40 axial traction is applied through the skull tongs with the neck in 20°–30° flexion. A weight of 5 kg is initially applied to the skull tongs. Weights are then progressively added (2 kg every 10 min) until either the facet joints get unlocked or signs of over distraction are seen on X-ray. If there is any worsening of neurological symptoms/signs, then the procedure is abandoned. Once the facet joints are unlocked on the lateral cervical X-ray, then the neck is extended while maintaining the traction force. If the lateral X-ray confirms the reduction of the facet joint, then the traction force can be reduced. Usually, it takes between 12 and 30 kg and from 10 min to 3 h to achieve a reduction.41,42 Rapid reduction is successful in up to 98% of patients with dislocation and has been reported to promote neurological recovery in patients in whom the reduction is achieved within 8 h of injury.43 The success rate is higher in pure dislocations than in facet fracture-dislocations and in bifacet dislocations as compared to unifacet dislocations.
Grant et al.,42 Star et al.43 and Vaccaro et al.44 have not observed neurological worsening when attempting closed reduction in awake, alert patients who can provide feedback regarding neurological status. Hence, they recommend immediate closed reduction based on the plain films rather than wasting critical time obtaining a MRI scan.
However, pre-reduction MRI scans reveal a 50%–80% incidence of disc disruption/herniation in patients with facet dislocations.42,45 Eismont et al. have reported two cases of neurological worsening due to the posterior migration of pre-existing or fresh disc fragments with closed reduction under general anesthesia, and hence recommend a prior MRI.46 The middle path is that in awake, alert patients with severe neurological deficits, closed reduction should be performed immediately. In patients without neurological deficits, unconscious/intoxicated patient and in those presenting after 8 h from injury, MRI may be performed before performing a reduction.47 No clear consensus exists regarding performing closed reduction without prior MRI in awake, alert patients with incomplete deficits.
In an attempt to hasten the reduction process and reduce locked facets, manipulative reduction may be attempted using conscious sedation in the operation theater.48,49 This is reported to be successful in about 90% of patients, but there is a small risk of worsening the neurological deficit.50
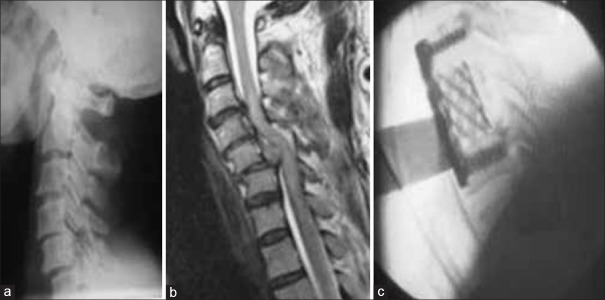
In patients where closed reduction has been unsuccessful, emergency open reduction is recommended to realign the spine and decompress the neural elements. Some surgeons recommend an anterior open reduction be performed immediately in all patients with jumped facets based on plain films, even without an MRI.51 They argue that open reduction is the quickest method of realigning the spine and that an anterior approach ensures that any herniated disc fragments can be dealt with simultaneously so that MRI scans are unnecessary [Figure 4].
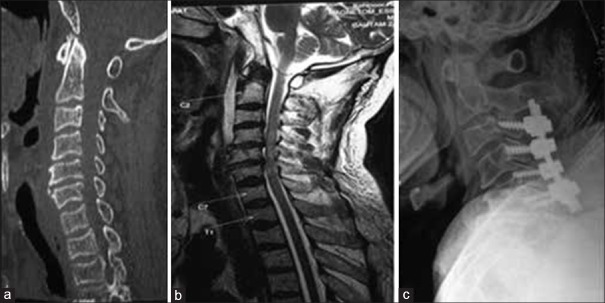
Figure 4.
X-ray cervical spine lateral view showing unifacet dislocation of C5/C6 (b) Sagittal T2W MRI cervical spine showing large prolapsed disc (c) Fluoroscopic view at same level showing primary anterior open reduction, corpectomy and fusion with instrumentation
Definitive treatment
The goals of management of cervical spine injury are to
Provide a stable well-aligned spine
Maximize neurological recovery
Obtain early functional recovery.
Indications for Surgery
The decision regarding surgery or nonoperative treatment is individualized. However, indications for surgery can be grouped as follows:
Neurological
The presence of a neurological deficit usually signifies mechanical instability. However, the mere presence of a neurological deficit should not be taken as an absolute indication for surgery. A classic example is a patient with a hyperextension injury and a central cord syndrome. Here, the spine is not unstable, but neither is surgical decompression usually indicated.
A complete neurological deficit by itself does not constitute an indication for surgery, as neuronal death cannot be expected to recover even after surgery. On the other hand, a progressive neurological deficit is a well accepted indication for surgery.
Surgery for a stable incomplete deficit with evidence of significant spinal canal compromise is controversial. While there is no unequivocal evidence that surgery improves neurological recovery, animal studies have shown that a contused cord is more susceptible to extrinsic compression than a normal spinal cord.52 Hence, the reduction in local tissue pressure by realignment of the spine or by direct surgical decompression of the spinal cord may promote neurological recovery by improving circulation/oxygenation.
The timing of spinal cord decompression is hotly debated. Animal studies have consistently shown improved spinal cord blood flow53 and better electrophysiological recovery following early decompression.52 Both La Rosa et al.54 and Fehlings and Perrin55 performed a meta-analysis to study the role of early decompression (<24 h) in acute SCI. They reported that there is no Class I data supporting the role and timing of decompression in acute SCI. However, there is reasonable evidence (Class II data) that early surgical intervention is safe and effective, and that even delayed decompression may promote neurological recovery. They recommend early spinal cord decompression, especially in patients with incomplete or progressive neurological deficit whenever safely possible.
Instability
This is the primary indication for surgery, as an unstable spine has the potential to cause deformity and neurological injury. However adequately defining instability is difficult, especially when attempting to extrapolate the definition to assist in surgical decision making.
Holdsworth described a two column classification for spinal instability.56 He suggested that the posterior column including the posterior bony structures and the posterior ligaments was the key to maintaining stability, especially the ability to resist kyphosis. This concept of instability is most commonly accepted today.57 Denis58 described a three column concept of spinal stability where the middle column consisting of the posterior longitudinal ligament (PLL), the posterior one-third of the vertebral body and the intervertebral disc was the key to stability. Injury to any two columns was deemed unstable. White and Punjabi developed a scoring system to assist in the estimation of spinal instability.59 Points are given based on the competence of the anterior and posterior spinal elements, the extent of static and dynamic displacement (including the stretch test), the presence of neurologic injury, and the anticipated physiologic loads to which the spine subsequently would be subjected. As a thumb rule, an injury is unstable if either all the anterior structures or all the posterior structures are injured. Injury to the disc and ligaments heal poorly and are prone to delayed instability.
The Holdsworth two-column concept of spinal stability forms the basis of two widely used classifications that help decision-making in cervical spine injuries namely; Allen's classification60 and the more recently described Subaxial Injury Classification.61 Allen described a comprehensive classification based on the injury mechanism as analyzed on plain radiographs. The criticism of this classification has been that it interprets injuries predominantly in one plane of motion and rotational injuries are not included. Although a spectrum of relatively more severe injuries is included in the classification, more subtle injuries like spinous process fractures and injuries in spondylotic spines, ankylosing spondylitis are not considered. In addition, it is very exhaustive, and there is a wide inter-observer variability.62 This classification is discussed in detail later in this article.
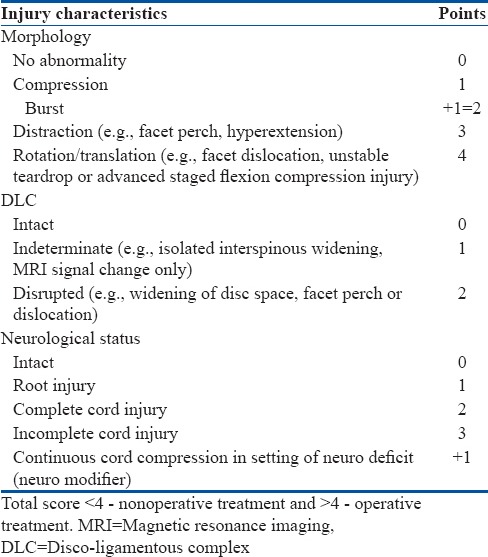
To provide a more objective method of decision making regarding the need for surgery and the surgical approach, the Spine Trauma Study Group has recently described a classification [Table 2] based on the injury morphology, the integrity of the PLC, and the severity of the neurological deficit. Each of these three categories is assigned a score which when summed up provides an injury severity score. Treatment decisions are then made based on the threshold values of the score. All three categories have shown good to excellent reliability and validity, except for the disco-ligamentous injury, which had lower inter and intra-observer agreement.
Table 2.
Subaxial cervical spine injury classification scale as described by the Spine Trauma Study Group
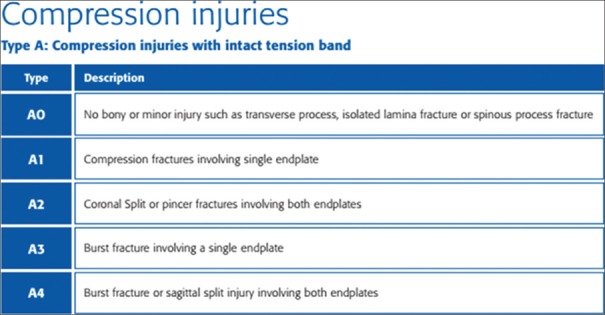
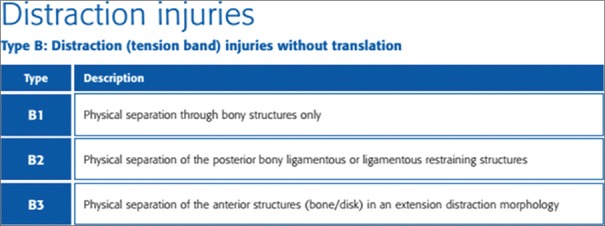
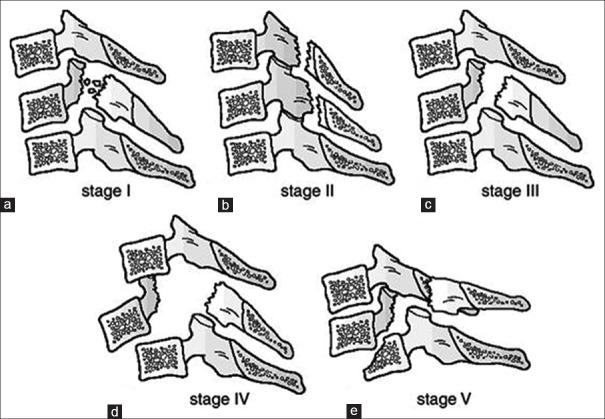
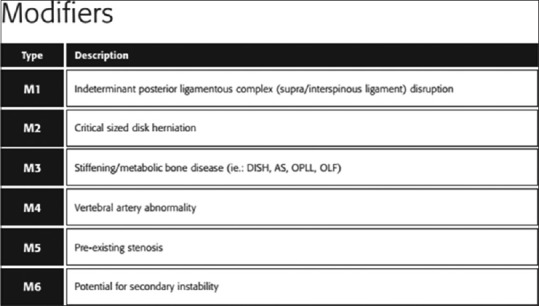
The AOSpine Knowledge Forum group has come up with a new classification system for cervical spine injuries.63 It has been broadly categorized into three groups [Figures 5–8] according to the nature/mechanism of injury. Additional modifiers (M1–M6) that were thought to be important enough for inclusion, but that may not be relevant to every case, are to be used on an as-needed basis to assist the physician in deciding treatment. Consideration has been given for various degrees of neurological impairment (N0–NX). It includes:
Figure 5.
AOSpine Knowledge Forum Cervical Spine Classification System. Compression injuries
Figure 8.
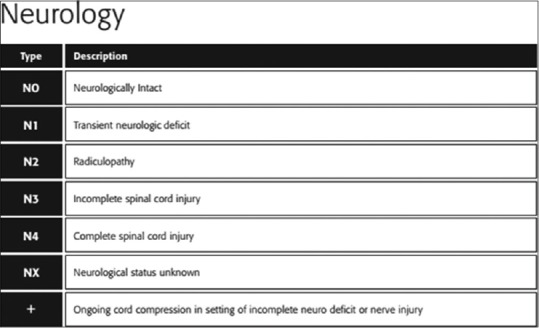
AOSpine Knowledge Forum Cervical Spine Classification System
Figure 6.
AOSpine Knowledge Forum Cervical Spine Classification System. Distraction injuries
Figure 7.
AOSpine Knowledge Forum Cervical Spine Classification System
Type A: COMPRESSION injuries (injuries with intact tension band)
Type B: DISTRACTION injuries (tension band injuries without translation)
Type C: TRANSLATIONAL injuries.
Spinal deformity
Most cervical injuries with a significant deformity would require surgery either for instability or for neurology. However, burst fractures due to axial compression could be stable because the posterior ligaments are intact and also present without neurological deficit. While some of these can be treated with a cervical orthosis, others may have significant kyphosis that merits surgery to limit adjacent segment degeneration and pain in the future.
Special situations
Patient factors to be considered include concomitant injuries, noncontiguous spinal injuries, smoking, co-morbidities, and the ability to realistically treat an injury non-surgically (e.g., the morbidly obese patient who cannot be fitted adequately for a halo brace).
Selection of Surgical Approach
The immediate aims of surgery are to realign the spine, decompress neural elements and provide mechanical stability. This can be achieved by an anterior decompression (discectomy/corpectomy) and instrumented fusion, a posterior stabilization with or without decompression and a combination of the two approaches. The decision regarding approach selection is based primarily on the morphology of the injury.
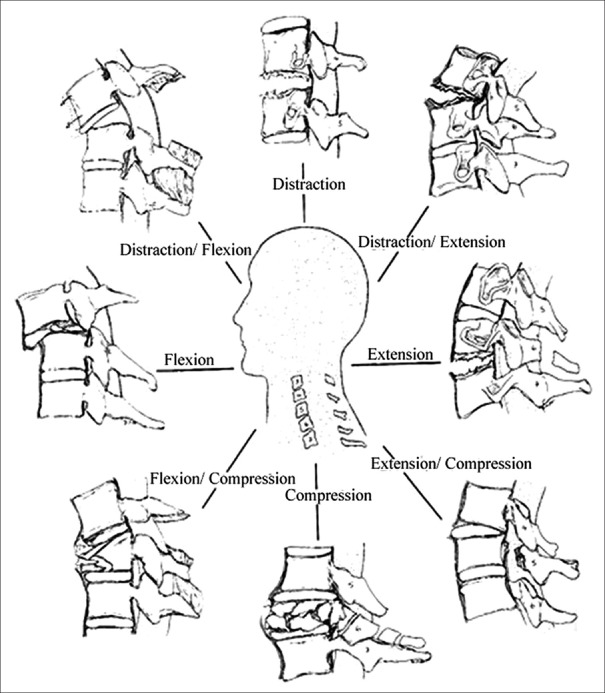
In 1982, Allen classifiied60 injuries based on the type of force causing the injury (compression/distraction), and the position of the head at the time of trauma (flexion/extension/neutral) [Figure 9]. Six different injury types are broadly described and based on the severity, a spectrum of injuries is described within each type to aid surgical decision making. The six types are flexion compression (21.8%), extension compression (24.2%), vertical compression (VC) (8.5%), flexion distraction (36.9%), extension distraction (5.6%), and lateral flexion (LF) (3%). The risk and severity of neurological injury increase with increasing stage within each type of injury. This classification has shown to be a good predictor of neurological outcome.
Figure 9.
A diagrammatic representation of the forces acting on the cervical spine
Vertical compression injuries
An axial load applied to the spine in the neutral position results in loading of the anterior column leading to failure of either the intervertebral disc, or the vertebral body. Failure of the disc may result in disc herniation. However, more commonly the end plates fail before the disc, and the disc material implodes into the body through the broken end plate. Depending on the severity of the injury, a variety of fracture patterns are seen within the vertebral body60 [Figure 10].
Figure 10.
Diagramatic representation of stages of a vertical compression injury- (a) Superior or inferior end plate fracture (b) Both end plates fractured, (c) Burst fracture with intact PLC
VC Stage 1 and 2 injuries represent a stable fracture of either the superior or inferior end plate or both end plates without any PLC injury. Both the anterior and posterior vertebral wall height is symmetrically reduced resulting in a cupping deformity of the vertebral body. There is no retropulsion or translation and only minimal local kyphosis. Neurologic deficits are rare. Most such injuries are treated with external immobilization for 8–12 weeks.
VC Stage 3 injuries are burst fracture of the vertebral body with variable comminution, loss of vertebral body height, and retropulsion of fracture fragments that may result in spinal cord compression and neurological deficit. Often the neurologic injury is much worse than the compression observed on imaging because the maximum retropulsion occurs at the time of impact.62,64 The PLC is usually intact. In neurologically intact patients, without posterior ligament injury or significant kyphosis, halo-vest immobilization for 12 weeks may be sufficient. However, Koivikko et al.65 reported better sagittal alignment, fusion rates, and neurological outcome following surgery compared to halo-vest immobilization for 69 patients with teardrop and burst fractures. The surgical procedure of choice is an anterior cervical corpectomy and instrumented fusion which allows decompression and provides mechanical stability66,67 [Figure 11]. In neurologically intact patients, posterior lateral mass/pedicle screw stabilization restricts the fusion to a single motion segment and hence may be preferred over an anterior fusion.
Figure 11.
(a) X-ray cervical spine lateral view showing vertical compression fracture stage 3 (b) Sagittal T2W MRI cervical spine showing vertical compression (c) X-ray cervical spine lateral view showing surgical management of vertical compression Stage 3 injury with quadriparesis
Compressive flexion injuries
These injuries are commonly seen following either a fall from height or due to the fall of a heavy object on the head. A compression force applied to a flexed cervical spine initially results in a compression failure of the vertebral body. More significant compression results in a posteriorly directed shear force that drives the posterior part of the Vertebral body into the spinal canal, disrupts the caudal disc and results in a tension failure of the PLC [Figure 12]. The anteroinferior portion of the vertebral body breaks off in this process and forms a triangular fragment, known as a teardrop fracture.68 Two-thirds of the patients will have an associated sagittal split of the vertebral body and a bilaminar fracture.69
Figure 12.
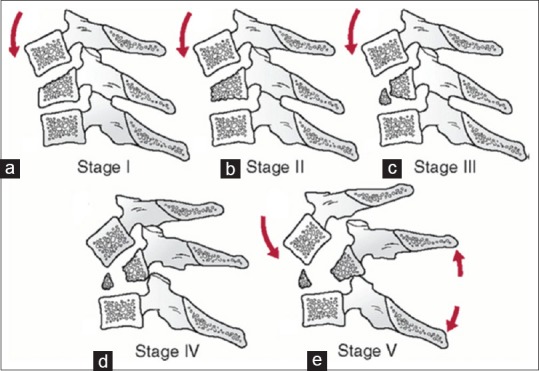
Line diagram showing stages of a compressive flexion injury (a) wedge compression, (b) anteroinferior beaking, (c) teardrop fracture, (d) Retrolisthesis of posterosuperior fragmet by <3 mm, (e) Retrolisthesis >3 mm
Compressive flexion (CF) Stage 1 is a wedge compression fracture. CF Stage 2 involves a more significant loss of anterior vertebral height with localized kyphosis, also called as “beaking” of the vertebral body. The PLC is intact and there is no retropulsion of bone into the spinal canal. Neurologic deficit is uncommon. Treatment is nonoperative with a cervical orthosis for 8–12 weeks. Serial radiographs are taken to look for progressive loss of vertebral height or a missed ligament injury. Dynamic X-rays must be done after orthosis removal to confirm stability.
CF Stage 3 represents a teardrop fracture with or without injury to the PLC. CF Stage 4 shows retrolisthesis of the posteroinferior edge of the vertebral body into the spinal canal by <3 mm, whereas CF Stage 5 shows retrolisthesis of >3 mm. There is almost always significant disruption of the PLC. A focal kyphosis is almost always present with circumferential soft tissue disruption. Quadrangular fractures70 are variants of CF Stage 5 with a large anteroinferior fracture fragment, significant posterior displacement of the vertebral body, angular kyphosis, disc disruption, and PLC disruption. This results in an apparent formation of two columns in the cervical spine with complete disruption of all discoligamentous attachments between them. The upper column consists of the posterosuperior body fragment with all the cephalad vertebrae, and the lower column consists of the anteroinferior fragment and all the caudal vertebrae. Neurological deficit is seen in 25% of CF Stage 3, 38% of CF Stage 4, and 91% of CF Stage 5 injuries due to retropulsion of bony fragments.60
Fisher et al.71 reported less kyphosis and instability at followup in teardrop fractures treated with surgery as compared to halo-vest. Most teardrop and quadrilateral fractures are unstable, and are best treated with anterior corpectomy and instrumented fusion.72,73 Additional posterior stabilization may be necessary to restore the tension band if there is severe posterior ligament injury (CF Stage 5), or if multilevel anterior corpectomy has been performed [Figure 13]. Toh et al.74 compared anterior versus posterior stabilization for burst and teardrop fractures and found that anterior decompression and fusion restored spinal canal diameter by 60%, as compared with only 6% with posterior stabilization. If the spine can be realigned easily with traction, then a posterior stabilization alone may be performed in neurologically intact patients.75,76
Figure 13.
(a) CT scan cervical spine showing compression fracture C7 vertebral body (b) Sagittal MRI T2WI of cervicodorsal spine junction showing compression flexion injury with disruption of posterior ligament. This case was treated by anterior corpectomy, fusion and stabilization
Distractive-flexion injuries
This is the most common injury pattern seen in the sub-axial cervical spine and commonly occurs in young males following motor vehicle accidents or after a fall. The most common level of injury is C6–C7, followed by C4–C5 and C5–C6.60,77 This hyperflexion injury involves a distraction force that travels from posterior to anterior with the center of rotation lying anterior to the vertebral body. Initially, the posterior ligamentous/osseous structures fail in tension. Sometimes, a compression fracture of the vertebral body may occur secondarily. Injuries may range from facet sprains and perched facets to unifacet or bifacet dislocations60 [Figure 14].
Figure 14.
Diagramatic representation of stages of distractive flexion injury: (a) flexion sprain, (b) unifacetal dislocation, (c) bifacetal dislocation with anterolisthesis <50%, (d) anterolisthesis >50%, (e) complete spondyloptosis
Facet sprains (distractive-flexion [DF] Stage 1) involve posterior ligament and facet capsule disruption, but are often dismissed as innocuous injuries when viewed on a lateral supine film where the spine is in a reduced position. MRI may show facet widening with increased T2-weighted signal intensity in the posterior ligaments. Later they may present with pain and instability78 [Figure 15]. These patients can be treated with rigid external immobilization for 8–12 weeks, with serial radiographs to look for sagittal malalignment, and dynamic radiographs at the end of treatment to rule out any instability. Alternatively, anterior cervical discectomy and fusion may be performed.
Figure 15.
(a) X-ray cervical spine lateral view showing flexion distraction injury missed at presentation, (b) X-ray cervical spine lateral view and (c) Sagittal MRI T2WI of cervical spine 7 days post injury showing disruption of posterior elements (d) x-ray cervical spine lateral view showing instrumented posterior stabilization
Unifacet (DF Stage 2)/bifacet dislocations (DF Stage 3 and 4) are more severe injuries involving a tear of the supraspinous and interspinous ligaments, the ligamentum flavum and the facet capsule.79 The PLL may be disrupted or stripped off the posterior surface of the vertebral body. Varying degrees of intervertebral disc disruption is seen in almost 60% of the patients.42,45 They are often associated with a facet fracture in the axial plane. The presence of a facet fracture reduces the probability of a successful closed reduction. Spinal cord or root injury is much more common with DF Stages 2, 3, and 4 (30%–90%).60,80 Occasionally, the inferior lip of the inferior facet of the cranial vertebra locks onto the tip of the superior lip of the superior facet of the caudal vertebra resulting in significant kyphosis and distraction. This condition is known as perched facets.
Emergency treatment includes obtaining realignment of the spine in the shortest possible time. Reduction of the dislocation reduces compression of the neural elements and the abnormal stretch of the ligaments and muscles. This in turn reduces the patient's severe pain and also produces a milieu that halts further neurologic injury and may promote neurological recovery. Closed reduction of the dislocation can be performed using either cervical traction or by manipulating the neck under sedation. In the case of a failed closed reduction, open reduction is performed either anteriorly or posteriorly.
Conventionally, the posterior open reduction has been preferred.40,81 Through a posterior midline incision, the spine is exposed subperiosteally up to the lateral gutter. Reduction can be achieved by manipulating the spinous processes with a towel clip or by applying a lamina distractor to obtain controlled distraction between the laminae and then extending the spine to obtain a reduction. However, the safest method is to excise the superior facet of the inferior vertebra which acts as a block to the reduction. Then, a pre inserted interspinous wire is gradually tightened to pull the dislocated vertebra back into alignment. Even a lateral mass screw-rod assembly can be used to restore alignment. The posterior approach is familiar to most surgeons and is almost certain to allow reduction of the dislocation in an acute setting. However, turning the patient into a prone position with an unstable spine can cause neurological worsening. The posterior reduction also carries a small risk of displacing a disc fragment that may result in postoperative neurological deterioration; hence, an MRI must be done before any posterior open reduction. If it shows a displaced disc fragment, then an anterior discectomy must be done before reducing the dislocation.
Anterior open reduction25,82 [Figure 16] involves an anterior retropharyngeal approach to the spine. The intervertebral disc at the dislocated level is then excised, and the neural elements are decompressed. In case the spine is kyphotic, it may be difficult to enter the disc space without excising the anteroinferior part of the vertebral body. Then by manipulation using a vertebral body distractor, the reduction can usually be achieved. In case the dislocation cannot be safely reduced, then it is advisable to turn the patient over and attempt a reduction from a posterior approach. The anterior open reduction is performed with visualization of the spinal cord, and hence, neurological deterioration due to displaced disc fragments is less likely.
Figure 16.
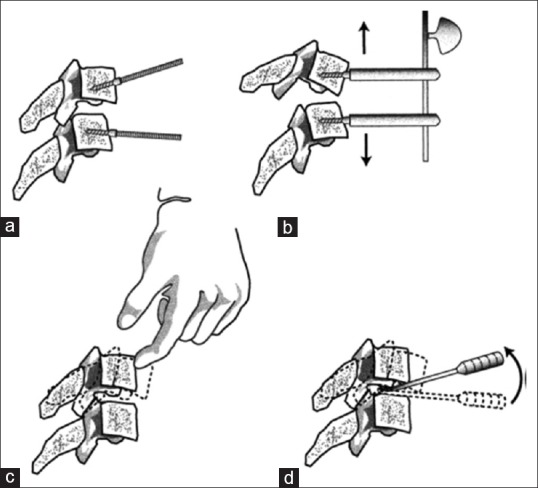
A diagramatic representation of a technique of anterior open reduction of facet dislocations. (a) insertion of distractor pins at a divergent angle to each other, (b) distractor pins made parallel to each other and distractor applied. Distraction done to unlock the facets, (c) gentle manual pressure is applied to push the cephalad vertebra back to obtain a reduction, (d) same maneuver can be performed using vertebral body spreaders or chisels in disc space. Adapted from: Ordonez BJ, Benzel EC, Naderi S, Weller SJ. Cervical facet dislocation: Techniques for ventral reduction and stabilization. J Neurosurg 2000;92 (1 Suppl):18-23
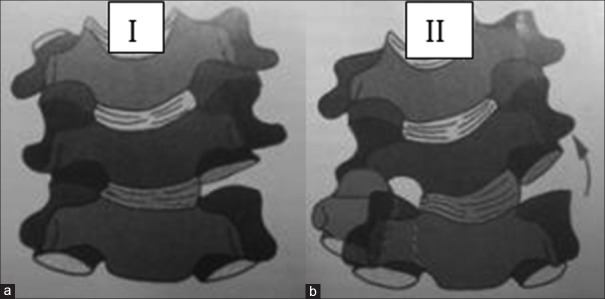
Surgical stabilization is the preferred definitive treatment, especially when the posterior disruption is ligamentous or when there are facet fractures involving >40% of the height of the lateral mass or with >1 mm diastasis.83,84 Both anterior and posterior approaches have shown good long term results.85 Conventionally, posterior stabilization has been preferred because it helps to restore the posterior tension band that is lost due to disruption of the posterior ligaments and muscles. Biomechanical studies have shown that posterior stabilization allows a more rigid fixation than anterior plates.86,87 Besides the posterior approach is familiar, the reduction is easy and instrumentation can be easily extended over multiple levels if required. In osteoporotic bone, posterior stabilization offers better fixation than anterior plating. Posterior stabilization can be achieved using either interspinous or sublaminar wire as well as with lateral mass screws and plates88 [Figure 17].
Figure 17.
A diagramatic representation of cervical spine showing different techniques of posterior stabilization - (a) Roger's interspinous wiring (b) Bohlman's triple wiring technique (c) lateral mass stabilization
Interspinous wiring techniques such as the Rogers technique and the Bohlman's triple wiring technique have been commonly used for posterior stabilization in patients with cervical trauma. They offer little stability in extension, lateral bending, and axial rotation and hence, the fixation needs to be protected in a brace or a halo-vest until fusion.89 Lateral mass fixation is the preferred method of stabilizing the spine.90,91 It offers more rigid fixation than wires in all planes, and it can be performed even when the posterior elements are fractured or excised. It allows a large central area for bone grafting. Unlike wires, lateral mass fixation can easily be extended cephalad and caudad. Besides lateral mass fixation has a much lesser chance of causing neurological injury than sublaminar wires.
Anterior stabilization92 is performed in the supine position so that there is less danger of loss of reduction when positioning the patient. The approach is through tissue planes and hence less bloody. Decompression is direct following which a large interbody graft can be inserted to restore continuity of the anterior column. However, the anterior plate is a buttress plate applied to the compression surface of the cervical vertebra. Hence, it fails to withstand significant shear forces resulting in loss of fixation with secondary instability [Figure 18] in up to 13% of patients.93 Loss of fixation is correlated with the presence of associated facet or vertebral body fracture, severe osteoporosis, and poor neuromuscular control.
Figure 18.
X-ray of cervical spine lateral view showing (a) flexion distraction injury C4 and C5 (b) anterior stabilization done (c) failure of anterior plates stabilization
Occasionally, it may be difficult to reduce bilateral facet subluxations. Special maneuvers may be needed to achieve a reduction in these cases. Casper distraction pins may be inserted into the vertebral bodies with the shaft positioned at a divergent angle of 10°–20°. Bringing the pins into parallel orientation and placing them in the distractor, followed by controlled distraction, often results in disengagement of the facets. The rostral level is then translated dorsally with the application of moderate pressure, to restore alignment.82
Unilateral subluxations are more difficult to reduce than bilateral subluxation.82 The distraction pins should be applied at a divergent angle in the coronal plane to allow the rotational deformity to be corrected after reduction. Alternatively, a vertebral body spreader may be inserted into the disc space. Distraction is done along with rotation of the spreader rostrally to achieve alignment.
Compressive-extension injuries
A fall from a height or even domestic falls may result in a direct blow to the forehead or the face resulting in a compression force being applied to an extended cervical spine [Figure 19]. The axial loading of the posterior spinal elements results in unilateral (compressive-extension [CE] Stage 1) or bilateral (CE Stage 2) fractures of the vertebral arch at one or more levels.60 These are stable injuries and are commonly treated nonoperatively with a rigid cervical orthosis for 12 weeks. Occasionally, unilateral fractures of both the pedicle and the lamina may occur resulting in a dissociation of the lateral mass, [Figure 20] and a rotary listhesis which requires stabilization.
Figure 19.
Diagramatic representation of stages of a compressive extension injury: (a) unilateral vertebral arch fracture (b) bilateral vertebral arch fractures, (c) bilateral vertebral arch fractures with anterior extension of the fracture, but spinal alignment maintained, (d and e) dissociation between anterior and posterior vertebral columns with progressive anterior translation
Figure 20.
(a and b) X-ray cervical spine anteroposterior and lateral views showing compressive extension Stage 1 injury- a lateral mass dissociation with rotary listhesis (c and d) CT scan showing a lateral mass dissociation with rotatory listhesis
With further extension or increased loads, the center of rotation of the extension moment shifts anteriorly and inferiorly resulting in a shear force that travels anteriorly, obliquely across the vertebral body or the disc rendering the spine unstable.94,95 The spinal alignment is maintained in CE Stage 3 but there is a progressive anterior translation of the cephalad spinal column in CE Stage 4 and 5. In Stage 4 and 5, there is the formation of a 2 column spine with the lack of continuity between the cephalad and caudad spine. This injury is most common in the lower cervical spine. In spite of the larger force required to cause the more severe injuries, the incidence of neurological deficit is low because of auto-decompression resulting from the separation of the anterior and posterior elements. While Stage 3 injuries can be managed nonoperatively in a halo-vest,96 Stage 4 and 5 injuries require surgical stabilization to restore spinal stability. Sagittal alignment can be restored with careful preoperative or intra-operative traction. Multilevel posterior lateral mass or pedicle screw fixation is the preferred option. In the case of significant vertebral body comminution, additional anterior reconstruction may be required to restore the load-bearing mechanics. Anterior stabilization alone is inadequate to neutralize the large shear forces involved.
When extension injuries occur in elderly patients with preexisting cervical spondylosis, there is a severe momentary compression of the spinal cord between the ligamentum flavum and the anterior osteophytes at the time of impact. This often result in a selective injury to the central spinal cord called the “central cord syndrome” [Figure 21], wherein the neurologic deficit is worse in the upper extremity as compared to the lower extremity.97 The prognosis for recovery is generally good although the patients may have significant residual hand dysfunction and variable spasticity.98,99 If there is any instability or malalignment, then surgical stabilization is indicated. The debate is whether a spinal canal decompression is necessary, and if so the timing of decompression is also controversial.100 Guest101 reported that decompression within 24 h of injury for traumatic central cord syndrome secondary to cervical fractures or acute disc prolapse is safe and promoted greater motor recovery than delayed decompression. However, if the central cord syndrome is associated with cervical spondylosis or stenosis, then the neurological recovery was not appreciable. However, Lenehan100 reported that early surgery (<24 h) is safe and produced better neurological recovery in patients with cervical spinal stenosis and traumatic central cord syndrome without instability.
Figure 21.
(a) CT scan cervical spine sagittal cut and (b) Sagittal MRI T2WI showing extension injury in spondylotic spine (c) X-ray cervical spine lateral view showing instrumented decompression. Central cord syndrome due to extension injury in spondylotic spine. Decompression done within 24 h
Distractive-extension injuries
These injuries occur following high-velocity vehicular accidents or following trivial falls in patients with pre-existing ankylosing spondylitis, diffuse idiopathic skeletal hyperostosis (DISH) or severe cervical spondylosis. Facial injuries are common. The spinal injury is often highly unstable and may be associated with a significant neurologic deficit.
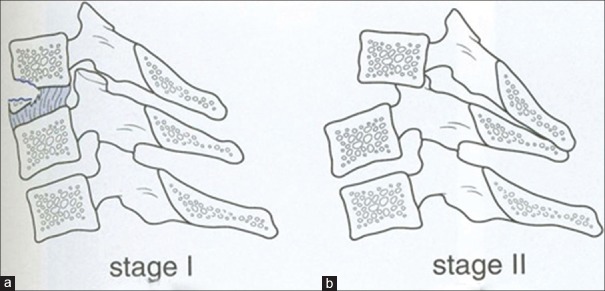
When a distraction force is applied to an extended cervical spine, the resultant injury progresses transversely from anterior to posterior resulting in sequential disruption of the ALL, the intervertebral disc, followed by the PLL, and in the end either a distraction failure of the PLC, or a fracture of the posterior bony elements,60,94,102,103 [Figure 22]. Distractive-extension (DE) Stage 1 signifies an injury where the PLL is intact, and the injury is confined to the anterior column without any retrolisthesis [Figure 23]. The transverse disruption of the anterior column may traverse through the disc, or may result in avulsion of the anteroinferior corner of the vertebra (extension teardrop fracture). A DE Stage 2 injury is extremely unstable due to the failure of the PLL with retrolisthesis of the cephalad vertebra which may result in spinal cord compression between the posteriorly displaced vertebra and the anterosuperior lamina of the next caudal vertebra. These injuries are stable in flexion and hence often missed when radiographs are obtained in a supine patient. Furthermore, the distorted anatomy in patients with ankylosing spondylitis or DISH makes radiographic interpretation difficult.
Figure 22.
A diagramatic representation of stages of distractive extension injury (a) Distraction injury of the anterior column but PLL intact, (b) Distraction injury involving both columns with PLL torn
Figure 23.
(a) X-ray cervical spine lateral view (b) CT scan sagittal cut (c) Sagittal MRI T2WI showing distractive extension Stage 1 injury with disruption of the anterior longitudinal ligament and intervertebral disc along with posterior element fractures. Was treated with anterior discectomy and fusion
When treating these injuries in patients with ankylosing spondylitis, the patient is propped up on pillows to recreate the pre-injury spinal alignment. Positioning the patient in hard collars may cause further extension and result in a worsening of the neurologic deficit.104 Application of traction for realignment of the spine can result in over distraction and worsening of the neurological deficit. The spine is best realigned in the flexed position.
Definitive treatment can be either a halo-vest immobilization or a surgical stabilization.105 In patients with significant preexisting deformity, elderly patients and patients with a neurologic deficit, a halo-vest is difficult to maintain. Hence, surgery is usually preferred.96 For DE Stage 1 injuries, anterior cervical fusion with plating is the treatment of choice, especially if the failure is purely discoligamentous. DE Stage 2 injuries are highly unstable and require posterior reduction with stabilization followed by an anterior fusion if necessary. In patients with ankylosing spondylitis, anterior stabilization alone is avoided because the osteoporotic vertebral bone affords poor fixation. If the spine gets realigned with gentle traction applied to the flexed neck, then multilevel posterior instrumentation may be adequate. However, if spinal realignment cannot be achieved, then posterior instrumentation is done along with an anterior decompression and instrumented fusion97 [Figure 24]. Some surgeons recommend using the fracture to achieve deformity correction.;106 However, this carries a significant risk of developing a neurologic deficit.107
Figure 24.
(a) Fluoroscopic view (b) Sagittal MRI T2WI (c) X-ray cervical spine lateral view showing distractive extension Stage 2 injury in a patient with ankylosing spondylitis-treated with circumferential stabilization
Lateral flexion injuries
With the head flexed to one side, any compression force applied would result in an asymmetric fracture of the vertebral body and a unilateral fracture of the posterior elements with the fracture line lying in the sagittal plane (LF1). Neurological injury is uncommon. Most LF1 injuries are treated nonoperatively. A more severe lateral bending injury (LF2) would result in avulsion of the contralateral posterior ligaments which is seen as facet joint widening on the AP X-ray [Figure 25]. LF2 injuries are frequently associated with avulsion of nerve roots or the brachial plexus.60 For LF2 injuries posterior stabilization can be done with the goal of fusing only one motion segment whenever possible.
Figure 25.
Diagramatic representation of stages of lateral flexion injuries (a) ipsilateral posterior elements involved, (b) contralateral posterior elements involved
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Lowery DW, Wald MM, Browne BJ, Tigges S, Hoffman JR, Mower WR NEXUS Group. Epidemiology of cervical spine injury victims. Ann Emerg Med. 2001;38:12–6. doi: 10.1067/mem.2001.116149. [DOI] [PubMed] [Google Scholar]
- 2.Goldberg W, Mueller C, Panacek E, Tigges S, Hoffman JR, Mower WR NEXUS Group. Distribution and patterns of blunt traumatic cervical spine injury. Ann Emerg Med. 2001;38:17–21. doi: 10.1067/mem.2001.116150. [DOI] [PubMed] [Google Scholar]
- 3.Burke DA, Linden RD, Zhang YP, Maiste AC, Shields CB. Incidence rates and populations at risk for spinal cord injury: A regional study. Spinal Cord. 2001;39:274–8. doi: 10.1038/sj.sc.3101158. [DOI] [PubMed] [Google Scholar]
- 4.Nobunaga AI, Go BK, Karunas RB. Recent demographic and injury trends in people served by the Model Spinal Cord Injury Care Systems. Arch Phys Med Rehabil. 1999;80:1372–82. doi: 10.1016/s0003-9993(99)90247-2. [DOI] [PubMed] [Google Scholar]
- 5.Tator CH, Duncan EG, Edmonds VE, Lapczak LI, Andrews DF. Changes in epidemiology of acute spinal cord injury from 1947 to 1981. Surg Neurol. 1993;40:207–15. doi: 10.1016/0090-3019(93)90069-d. [DOI] [PubMed] [Google Scholar]
- 6.National Spinal Cord injury Statistical Centre. Spinal cord injury facts and figures at a glance. Birmingham, AL: Publication of the National Spinal Cord Injury Statistical Center; 2011. [Google Scholar]
- 7.Baaj AA, Uribe JS, Nichols TA, Theodore N, Crawford NR, Sonntag VK, et al. Health care burden of cervical spine fractures in the United States: Analysis of a nationwide database over a 10-year period. J Neurosurg Spine. 2010;13:61–6. doi: 10.3171/2010.3.SPINE09530. [DOI] [PubMed] [Google Scholar]
- 8.Sokolowski MJ, Jackson AP, Haak MH, Meyer PR, Jr, Sokolowski MS. Acute mortality and complications of cervical spine injuries in the elderly at a single tertiary care center. J Spinal Disord Tech. 2007;20:352–6. doi: 10.1097/BSD.0b013e31802d0bc5. [DOI] [PubMed] [Google Scholar]
- 9.Prasad VS, Schwartz A, Bhutani R, Sharkey PW, Schwartz ML. Characteristics of injuries to the cervical spine and spinal cord in polytrauma patient population: Experience from a regional trauma unit. Spinal Cord. 1999;37:560–8. doi: 10.1038/sj.sc.3100878. [DOI] [PubMed] [Google Scholar]
- 10.McSwain NJ. Pre-hospital Trauma Life Support. 2nd ed. USA: Akron Educational; 1990. Spine management skills; pp. 225–6. [Google Scholar]
- 11.Trauma American College of Physicians. Advanced trauma life support program for physicians. 9th ed. Chicago, IL: Trauma American College of Physicians; 2004. [Google Scholar]
- 12.Saboe LA, Reid DC, Davis LA, Warren SA, Grace MG. Spine trauma and associated injuries. J Trauma. 1991;31:43–8. doi: 10.1097/00005373-199101000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Iida H, Tachibana S, Kitahara T, Horiike S, Ohwada T, Fujii K. Association of head trauma with cervical spine injury, spinal cord injury, or both. J Trauma. 1999;46:450–2. doi: 10.1097/00005373-199903000-00018. [DOI] [PubMed] [Google Scholar]
- 14.Wang CM, Chen Y, DeVivo MJ, Huang CT. Epidemiology of extraspinal fractures associated with acute spinal cord injury. Spinal Cord. 2001;39:589–94. doi: 10.1038/sj.sc.3101216. [DOI] [PubMed] [Google Scholar]
- 15.Cothren CC, Moore EE, Ray CE, Jr, Johnson JL, Moore JB, Burch JM. Cervical spine fracture patterns mandating screening to rule out blunt cerebrovascular injury. Surgery. 2007;141:76–82. doi: 10.1016/j.surg.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 16.Giacobetti FB, Vaccaro AR, Bos-Giacobetti MA, Deeley DM, Albert TJ, Farmer JC, et al. Vertebral artery occlusion associated with cervical spine trauma. A prospective analysis. Spine (Phila Pa 1976) 1997;22:188–92. doi: 10.1097/00007632-199701150-00011. [DOI] [PubMed] [Google Scholar]
- 17.Bula WI, Loes DJ. Trauma to the cerebrovascular system. Neuroimaging Clin N Am. 1994;4:753–72. [PubMed] [Google Scholar]
- 18.Cothren CC, Moore EE, Biffl WL, Ciesla DJ, Ray CE, Jr, Johnson JL, et al. Cervical spine fracture patterns predictive of blunt vertebral artery injury. J Trauma. 2003;55:811–3. doi: 10.1097/01.TA.0000092700.92587.32. [DOI] [PubMed] [Google Scholar]
- 19.Weller SJ, Rossitch E, Jr, Malek AM. Detection of vertebral artery injury after cervical spine trauma using magnetic resonance angiography. J Trauma. 1999;46:660–6. doi: 10.1097/00005373-199904000-00017. [DOI] [PubMed] [Google Scholar]
- 20.Blickenstaff KL, Weaver FA, Yellin AE, Stain SC, Finck E. Trends in the management of traumatic vertebral artery injuries. Am J Surg. 1989;158:101–5. doi: 10.1016/0002-9610(89)90355-3. [DOI] [PubMed] [Google Scholar]
- 21.Inamasu J, Guiot BH. Vertebral artery injury after blunt cervical trauma: An update. Surg Neurol. 2006;65:238–45. doi: 10.1016/j.surneu.2005.06.043. [DOI] [PubMed] [Google Scholar]
- 22.Duane TM, Dechert T, Wolfe LG, Aboutanos MB, Malhotra AK, Ivatury RR. Clinical examination and its reliability in identifying cervical spine fractures. J Trauma. 2007;62:1405–8. doi: 10.1097/TA.0b013e31804798d5. [DOI] [PubMed] [Google Scholar]
- 23.Gerrelts BD, Petersen EU, Mabry J, Petersen SR. Delayed diagnosis of cervical spine injuries. J Trauma. 1991;31:1622–6. doi: 10.1097/00005373-199112000-00010. [DOI] [PubMed] [Google Scholar]
- 24.Davis JW, Phreaner DL, Hoyt DB, Mackersie RC. The etiology of missed cervical spine injuries. J Trauma. 1993;34:342–6. doi: 10.1097/00005373-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med. 2000;343:94–9. doi: 10.1056/NEJM200007133430203. [DOI] [PubMed] [Google Scholar]
- 26.Sharma OP, Oswanski MF, Yazdi JS, Jindal S, Taylor M. Assessment for additional spinal trauma in patients with cervical spine injury. Am Surg. 2007;73:70–4. [PubMed] [Google Scholar]
- 27.Miller CP, Brubacher JW, Biswas D, Lawrence BD, Whang PG, Grauer JN. The incidence of noncontiguous spinal fractures and other traumatic injuries associated with cervical spine fractures: A 10-year experience at an academic medical center. Spine (Phila Pa 1976) 2011;36:1532–40. doi: 10.1097/BRS.0b013e3181f550a6. [DOI] [PubMed] [Google Scholar]
- 28.Bracken MB, Shepard MJ, Collins WF, Holford TR, Young W, Baskin DS, et al. A randomized, controlled trial of methylprednisolone or naloxone in the treatment of acute spinal-cord injury. Results of the Second National Acute Spinal Cord Injury Study. N Engl J Med. 1990;322:1405–11. doi: 10.1056/NEJM199005173222001. [DOI] [PubMed] [Google Scholar]
- 29.Bracken MB, Shepard MJ, Holford TR, Leo-Summers L, Aldrich EF, Fazl M, et al. Methylprednisolone or tirilazad mesylate administration after acute spinal cord injury: 1-year follow up. Results of the third National Acute Spinal Cord Injury randomized controlled trial. J Neurosurg. 1998;89:699–706. doi: 10.3171/jns.1998.89.5.0699. [DOI] [PubMed] [Google Scholar]
- 30.Hurlbert RJ. The role of steroids in acute spinal cord injury: An evidence-based analysis. Spine (Phila Pa 1976) 2001;26(24 Suppl):S39–46. doi: 10.1097/00007632-200112151-00009. [DOI] [PubMed] [Google Scholar]
- 31.Fehlings MG. Spine Focus Panel. Summary statement: The use of methylprednisolone in acute spinal cord injury. Spine (Phila Pa 1976) 2001;26(24 Suppl):S55. doi: 10.1097/00007632-200112151-00011. [DOI] [PubMed] [Google Scholar]
- 32.Pollack CV, Jr, Hendey GW, Martin DR, Hoffman JR, Mower WR NEXUS Group. Use of flexion extension radiographs of the cervical spine in blunt trauma. Ann Emerg Med. 2001;38:8–11. doi: 10.1067/mem.2001.116810. [DOI] [PubMed] [Google Scholar]
- 33.Wang JC, Hatch JD, Sandhu HS, Delamarter RB. Cervical flexion and extension radiographs in acutely injured patients. Clin Orthop Relat Res. 1999;365:111–6. doi: 10.1097/00003086-199908000-00015. [DOI] [PubMed] [Google Scholar]
- 34.Sanchez B, Waxman K, Jones T, Conner S, Chung R, Becerra S. Cervical spine clearance in blunt trauma: Evaluation of a computed tomography-based protocol. J Trauma. 2005;59:179–83. doi: 10.1097/01.ta.0000171449.94650.81. [DOI] [PubMed] [Google Scholar]
- 35.Antevil JL, Sise MJ, Sack DI, Kidder B, Hopper A, Brown CV. Spiral computed tomography for the initial evaluation of spine trauma: A new standard of care? J Trauma. 2006;61:382–7. doi: 10.1097/01.ta.0000226154.38852.e6. [DOI] [PubMed] [Google Scholar]
- 36.LeBlang SD, Nuñez DB., Jr Helical CT of cervical spine and soft tissue injuries of the neck. Radiol Clin North Am. 1999;37:515. doi: 10.1016/s0033-8389(05)70109-3. [DOI] [PubMed] [Google Scholar]
- 37.Goradia D, Linnau KF, Cohen WA, Mirza S, Hallam DK, Blackmore CC. Correlation of MR imaging findings with intraoperative findings after cervical spine trauma. AJNR Am J Neuroradiol. 2007;28:209–15. [PMC free article] [PubMed] [Google Scholar]
- 38.AANS. Management of vertebral artery injuries after non-penetrating cervical trauma. Neurosurgery. 2002;50(3 Suppl):S173–8. doi: 10.1097/00006123-200203001-00026. [DOI] [PubMed] [Google Scholar]
- 39.Biffl WL, Ray CE, Jr, Moore EE, Mestek M, Johnson JL, Burch JM. Noninvasive diagnosis of blunt cerebrovascular injuries: A preliminary report. J Trauma. 2002;53:850–6. doi: 10.1097/00005373-200211000-00008. [DOI] [PubMed] [Google Scholar]
- 40.Vital JM, Gille O, Sénégas J, Pointillart V. Reduction technique for uni- and biarticular dislocations of the lower cervical spine. Spine (Phila Pa 1976) 1998;23:949–54. doi: 10.1097/00007632-199804150-00021. [DOI] [PubMed] [Google Scholar]
- 41.Cotler HB, Miller LS, DeLucia FA, Cotler JM, Davne SH. Closed reduction of cervical spine dislocations. Clin Orthop Relat Res. 1987;214:185–99. [PubMed] [Google Scholar]
- 42.Grant GA, Mirza SK, Chapman JR, Winn HR, Newell DW, Jones DT, et al. Risk of early closed reduction in cervical spine subluxation injuries. J Neurosurg. 1999;90(1 Suppl):13–8. doi: 10.3171/spi.1999.90.1.0013. [DOI] [PubMed] [Google Scholar]
- 43.Star AM, Jones AA, Cotler JM, Balderston RA, Sinha R. Immediate closed reduction of cervical spine dislocations using traction. Spine (Phila Pa 1976) 1990;15:1068–72. doi: 10.1097/00007632-199015100-00016. [DOI] [PubMed] [Google Scholar]
- 44.Vaccaro AR, Falatyn SP, Flanders AE, Balderston RA, Northrup BE, Cotler JM. Magnetic resonance evaluation of the intervertebral disc, spinal ligaments, and spinal cord before and after closed traction reduction of cervical spine dislocations. Spine (Phila Pa 1976) 1999;24:1210–7. doi: 10.1097/00007632-199906150-00007. [DOI] [PubMed] [Google Scholar]
- 45.Rizzolo SJ, Piazza MR, Cotler JM, Balderston RA, Schaefer D, Flanders A. Intervertebral disc injury complicating cervical spine trauma. Spine (Phila Pa 1976) 1991;16(6 Suppl):S187–9. doi: 10.1097/00007632-199106001-00002. [DOI] [PubMed] [Google Scholar]
- 46.Eismont FJ, Arena MJ, Green BA. Extrusion of an intervertebral disc associated with traumatic subluxation or dislocation of cervical facets. Case report. J Bone Joint Surg Am. 1991;73:1555–60. [PubMed] [Google Scholar]
- 47.Kwon BK, Vaccaro AR, Grauer JN, Fisher CG, Dvorak MF. Subaxial cervical spine trauma. J Am Acad Orthop Surg. 2006;14:78–89. doi: 10.5435/00124635-200602000-00003. [DOI] [PubMed] [Google Scholar]
- 48.Burke DC, Berryman D. The place of closed manipulation in the management of flexion-rotation dislocations of the cervical spine. J Bone Joint Surg Br. 1971;53:165–82. [PubMed] [Google Scholar]
- 49.Lu K, Lee TC, Chen HJ. Closed reduction of bilateral locked facets of the cervical spine under general anaesthesia. Acta Neurochir (Wien) 1998;140:1055–61. doi: 10.1007/s007010050214. [DOI] [PubMed] [Google Scholar]
- 50.Ludwig SC, Vaccaro AR, Balderston RA, Cotler JM. Immediate quadriparesis after manipulation for bilateral cervical facet subluxation. A case report. J Bone Joint Surg Am. 1997;79:587–90. doi: 10.2106/00004623-199704000-00017. [DOI] [PubMed] [Google Scholar]
- 51.Payer M. Immediate open anterior reduction and antero-posterior fixation/fusion for bilateral cervical locked facets. Acta Neurochir (Wien) 2005;147:509–13. doi: 10.1007/s00701-004-0462-6. [DOI] [PubMed] [Google Scholar]
- 52.Dimar JR, 2nd, Glassman SD, Raque GH, Zhang YP, Shields CB. The influence of spinal canal narrowing and timing of decompression on neurologic recovery after spinal cord contusion in a rat model. Spine (Phila Pa 1976) 1999;24:1623–33. doi: 10.1097/00007632-199908150-00002. [DOI] [PubMed] [Google Scholar]
- 53.Carlson GD, Minato Y, Okada A, Gorden CD, Warden KE, Barbeau JM, et al. Early time-dependent decompression for spinal cord injury: Vascular mechanisms of recovery. J Neurotrauma. 1997;14:951–62. doi: 10.1089/neu.1997.14.951. [DOI] [PubMed] [Google Scholar]
- 54.La Rosa G, Conti A, Cardali S, Cacciola F, Tomasello F. Does early decompression improve neurological outcome of spinal cord injured patients? Appraisal of the literature using a meta-analytical approach. Spinal Cord. 2004;42:503–12. doi: 10.1038/sj.sc.3101627. [DOI] [PubMed] [Google Scholar]
- 55.Fehlings MG, Perrin RG. The role and timing of early decompression for cervical spinal cord injury: Update with a review of recent clinical evidence. Injury. 2005;36(Suppl 2):B13–26. doi: 10.1016/j.injury.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 56.Holdsworth F. Fractures, dislocations, and fracture-dislocations of the spine. J Bone Joint Surg Am. 1970;52:1534–51. [PubMed] [Google Scholar]
- 57.James KS, Wenger KH, Schlegel JD, Dunn HK. Biomechanical evaluation of the stability of thoracolumbar burst fractures. Spine (Phila Pa 1976) 1994;19:1731–40. doi: 10.1097/00007632-199408000-00013. [DOI] [PubMed] [Google Scholar]
- 58.Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976) 1983;8:817–31. doi: 10.1097/00007632-198311000-00003. [DOI] [PubMed] [Google Scholar]
- 59.White AA, 3rd, Panjabi MM. Clinical Biomechanics of the Spine. 2nd ed. Philadelphia, PA: JB Lippincott; 1990. [Google Scholar]
- 60.Allen BL, Jr, Ferguson RL, Lehmann TR, O’Brien RP. A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine (Phila Pa 1976) 1982;7:1–27. doi: 10.1097/00007632-198200710-00001. [DOI] [PubMed] [Google Scholar]
- 61.Vaccaro AR, Hulbert JR, Patel AA, Fisher C, Dvorak M, Lehman RA, Jr, et al. The subaxial cervical spine injury classification system (SLIC): A novel approach to recognize the importance of morphology, neurology and integrity of the disco-ligamentous complex. Spine. 2007;32:2365–74. doi: 10.1097/BRS.0b013e3181557b92. [DOI] [PubMed] [Google Scholar]
- 62.Carter JW, Mirza SK, Tencer AF, Ching RP. Canal geometry changes associated with axial compressive cervical spine fracture. Spine (Phila Pa 1976) 2000;25:46–54. doi: 10.1097/00007632-200001010-00010. [DOI] [PubMed] [Google Scholar]
- 63.Vaccaro AR, Koerner JD, Radcliff KE, Oner FC, Reinhold M, Schnake KJ, et al. AOSpine subaxial cervical spine injury classification system. Eur Spine J. 2016;25:2173–84. doi: 10.1007/s00586-015-3831-3. [DOI] [PubMed] [Google Scholar]
- 64.Chang DG, Tencer AF, Ching RP, Treece B, Senft D, Anderson PA. Geometric changes in the cervical spinal canal during impact. Spine (Phila Pa 1976) 1994;19:973–80. doi: 10.1097/00007632-199404150-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Koivikko MP, Myllynen P, Karjalainen M, Vornanen M, Santavirta S. Conservative and operative treatment in cervical burst fractures. Arch Orthop Trauma Surg. 2000;120:448–51. doi: 10.1007/s004029900129. [DOI] [PubMed] [Google Scholar]
- 66.Aebi M, Zuber K, Marchesi D. Treatment of cervical spine injuries with anterior plating. Indications, techniques, and results. Spine (Phila Pa 1976) 1991;16(3 Suppl):S38–45. doi: 10.1097/00007632-199103001-00008. [DOI] [PubMed] [Google Scholar]
- 67.Kiwerski JE. Early anterior decompression and fusion for crush fractures of cervical vertebrae. Int Orthop. 1993;17:166–8. doi: 10.1007/BF00186379. [DOI] [PubMed] [Google Scholar]
- 68.Torg JS, Pavlov H, O’Neill MJ, Nichols CE, Jr, Sennett B. The axial load teardrop fracture. A biomechanical, clinical and roentgenographic analysis. Am J Sports Med. 1991;19:355–64. doi: 10.1177/036354659101900406. [DOI] [PubMed] [Google Scholar]
- 69.Lee C, Kim KS, Rogers LF. Sagittal fracture of the cervical vertebral body. AJR Am J Roentgenol. 1982;139:55–60. doi: 10.2214/ajr.139.1.55. [DOI] [PubMed] [Google Scholar]
- 70.Favero KJ, Van Peteghem PK. The quadrangular fragment fracture. Roentgenographic features and treatment protocol. Clin Orthop Relat Res. 1989;239:40–6. [PubMed] [Google Scholar]
- 71.Fisher CG, Dvorak MF, Leith J, Wing PC. Comparison of outcomes for unstable lower cervical flexion teardrop fractures managed with halo thoracic vest versus anterior corpectomy and plating. Spine (Phila Pa 1976) 2002;27:160–6. doi: 10.1097/00007632-200201150-00008. [DOI] [PubMed] [Google Scholar]
- 72.Cabanela ME, Ebersold MJ. Anterior plate stabilization for bursting teardrop fractures of the cervical spine. Spine (Phila Pa 1976) 1988;13:888–91. doi: 10.1097/00007632-198808000-00002. [DOI] [PubMed] [Google Scholar]
- 73.Goffin J, van Loon J, Van Calenbergh F, Plets C. Long term results after anterior cervical fusion and osteosynthetic stabilization for fractures and/or dislocations of the cervical spine. J Spinal Disord. 1995;8:500–8. [PubMed] [Google Scholar]
- 74.Toh E, Nomura T, Watanabe M, Mochida J. Surgical treatment for injuries of the middle and lower cervical spine. Int Orthop. 2006;30:54–8. doi: 10.1007/s00264-005-0016-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nazarian SM, Louis RP. Posterior internal fixation with screw plates in traumatic lesions of the cervical spine. Spine (Phila Pa 1976) 1991;16(3 Suppl):S64–71. doi: 10.1097/00007632-199103001-00011. [DOI] [PubMed] [Google Scholar]
- 76.Fehlings MG, Cooper PR, Errico TJ. Posterior plates in the management of cervical instability: Long term results in 44 patients. J Neurosurg. 1994;81:341–9. doi: 10.3171/jns.1994.81.3.0341. [DOI] [PubMed] [Google Scholar]
- 77.Dvorak MF, Fisher CG, Arabi BB, Harris MB, Hurbert RJ, Rampersaud YR, et al. Clinical outcome of 90 isolated unilateral facet fractures, subluxations and dislocations treated surgically and nonoperatively. Spine. 2007;32:3007–13. doi: 10.1097/BRS.0b013e31815cd439. [DOI] [PubMed] [Google Scholar]
- 78.Harris JH, Jr, Edeiken-Monroe B, Kopaniky DR. A practical classification of acute cervical spine injuries. Orthop Clin North Am. 1986;17:15–30. [PubMed] [Google Scholar]
- 79.Sim E, Vaccaro AR, Berzlanovich A, Schwarz N, Sim B. In vitro genesis of subaxial cervical unilateral facet dislocations through sequential soft tissue ablation. Spine (Phila Pa 1976) 2001;26:1317–23. doi: 10.1097/00007632-200106150-00009. [DOI] [PubMed] [Google Scholar]
- 80.Nakashima H, Yukawa Y, Ito K, Machino M, Kato F. Mechanical patterns of cervical injury influence postoperative neurological outcome: A verification of the allen system. Spine (Phila Pa 1976) 2011;36:E441–6. doi: 10.1097/BRS.0b013e3181d99e8c. [DOI] [PubMed] [Google Scholar]
- 81.Fazl M, Pirouzmand F. Intraoperative reduction of locked facets in the cervical spine by use of a modified interlaminar spreader: Technical note. Neurosurgery. 2001;48:444–5. doi: 10.1097/00006123-200102000-00045. [DOI] [PubMed] [Google Scholar]
- 82.Ordonez BJ, Benzel EC, Naderi S, Weller SJ. Cervical facet dislocation: Techniques for ventral reduction and stabilization. J Neurosurg. 2000;92(1 Suppl):18–23. doi: 10.3171/spi.2000.92.1.0018. [DOI] [PubMed] [Google Scholar]
- 83.Hadley MN, Fitzpatrick BC, Sonntag VK, Browner CM. Facet fracture-dislocation injuries of the cervical spine. Neurosurgery. 1992;30:661–6. [PubMed] [Google Scholar]
- 84.Spector LR, Kim DH, Affonso J, Albert TJ, Hilibrand AS, Vaccaro AR. Use of computed tomography to predict failure of nonoperative treatment of unilateral facet fractures of the cervical spine. Spine (Phila Pa 1976) 2006;31:2827–35. doi: 10.1097/01.brs.0000245864.72372.8f. [DOI] [PubMed] [Google Scholar]
- 85.Wiseman DB, Bellabarba C, Mirza SK, Chapman J. Anterior versus posterior surgical treatment for traumatic cervical spine dislocation. Curr Opin Orthop. 2003;14:174–81. [Google Scholar]
- 86.Duggal N, Chamberlain RH, Park SC, Sonntag VK, Dickman CA, Crawford NR. Unilateral cervical facet dislocation: Biomechanics of fixation. Spine (Phila Pa 1976) 2005;30:E164–8. doi: 10.1097/01.brs.0000157418.20900.a1. [DOI] [PubMed] [Google Scholar]
- 87.Do Koh Y, Lim TH, Won You J, Eck J, An HS. A biomechanical comparison of modern anterior and posterior plate fixation of the cervical spine. Spine (Phila Pa 1976) 2001;26:15–21. doi: 10.1097/00007632-200101010-00005. [DOI] [PubMed] [Google Scholar]
- 88.Shapiro S, Snyder W, Kaufman K, Abel T. Outcome of 51 cases of unilateral locked cervical facets: Interspinous braided cable for lateral mass plate fusion compared with interspinous wire and facet wiring with iliac crest. J Neurosurg. 1999;91(1 Suppl):19–24. doi: 10.3171/spi.1999.91.1.0019. [DOI] [PubMed] [Google Scholar]
- 89.Mihara H, Cheng BC, David SM, Ohnari K, Zdeblick TA. Biomechanical comparison of posterior cervical fixation. Spine (Phila Pa 1976) 2001;26:1662–7. doi: 10.1097/00007632-200108010-00007. [DOI] [PubMed] [Google Scholar]
- 90.Kandziora F, Pflugmacher R, Scholz M, Schnake K, Putzier M, Khodadadyan-Klostermann C, et al. Posterior stabilization of subaxial cervical spine trauma: Indications and techniques. Injury. 2005;36(Suppl 2):B36–43. doi: 10.1016/j.injury.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 91.Pateder DB, Carbone JJ. Lateral mass screw fixation for cervical spine trauma: Associated complications and efficacy in maintaining alignment. Spine J. 2006;6:40–3. doi: 10.1016/j.spinee.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 92.Aebi M. Surgical treatment of upper, middle and lower cervical injuries and nonunions by anterior procedures. Eur Spine J. 2010;19(Suppl 1):S33–9. doi: 10.1007/s00586-009-1120-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Johnson MG, Fisher CG, Boyd M, Pitzen T, Oxland TR, Dvorak MF. The radiographic failure of single segment anterior cervical plate fixation in traumatic cervical flexion distraction injuries. Spine (Phila Pa 1976) 2004;29:2815–20. doi: 10.1097/01.brs.0000151088.80797.bd. [DOI] [PubMed] [Google Scholar]
- 94.Forsyth HF. Extension injuries of the cervical spine. J Bone Joint Surg Am. 1964;46:1792–7. [PubMed] [Google Scholar]
- 95.Lifeso RM, Colucci MA. Anterior fusion for rotationally unstable cervical spine fractures. Spine (Phila Pa 1976) 2000;25:2028–34. doi: 10.1097/00007632-200008150-00005. [DOI] [PubMed] [Google Scholar]
- 96.Vaccaro AR, Klein GR, Thaller JB, Rushton SA, Cotler JM, Albert TJ. Distraction extension injuries of the cervical spine. J Spinal Disord. 2001;14:193–200. doi: 10.1097/00002517-200106000-00002. [DOI] [PubMed] [Google Scholar]
- 97.Schneider RC, Cherry G, Pantek H. The syndrome of acute central cervical spinal cord injury; with special reference to the mechanisms involved in hyperextension injuries of cervical spine. J Neurosurg. 1954;11:546–77. doi: 10.3171/jns.1954.11.6.0546. [DOI] [PubMed] [Google Scholar]
- 98.Newey ML, Sen PK, Fraser RD. The long term outcome after central cord syndrome: A study of the natural history. J Bone Joint Surg Br. 2000;82:851–5. doi: 10.1302/0301-620x.82b6.9866. [DOI] [PubMed] [Google Scholar]
- 99.Harrop JS, Sharan A, Ratliff J. Central cord injury: Pathophysiology, management, and outcomes. Spine J. 2006;6(6 Suppl):198S–206S. doi: 10.1016/j.spinee.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 100.Lenehan B, Fisher CG, Vaccaro A, Fehlings M, Aarabi B, Dvorak MF. The urgency of surgical decompression in acute central cord injuries with spondylosis and without instability. Spine (Phila Pa 1976) 2010;35(21 Suppl):S180–6. doi: 10.1097/BRS.0b013e3181f32a44. [DOI] [PubMed] [Google Scholar]
- 101.Guest J, Eleraky MA, Apostolides PJ, Dickman CA, Sonntag VK. Traumatic central cord syndrome: Results of surgical management. J Neurosurg. 2002;97(1 Suppl):25–32. doi: 10.3171/spi.2002.97.1.0025. [DOI] [PubMed] [Google Scholar]
- 102.Kinoshita H, Hirakawa H. Pathological studies and pathological principles on the management of extension injuries of the cervical spine. Paraplegia. 1989;27:172–81. doi: 10.1038/sc.1989.26. [DOI] [PubMed] [Google Scholar]
- 103.Harris JH, Yeakley JW. Hyperextension-dislocation of the cervical spine. Ligament injuries demonstrated by magnetic resonance imaging. J Bone Joint Surg Br. 1992;74:567–70. doi: 10.1302/0301-620X.74B4.1624517. [DOI] [PubMed] [Google Scholar]
- 104.Thumbikat P, Hariharan RP, Ravichandran G, McClelland MR, Mathew KM. Spinal cord injury in patients with ankylosing spondylitis: A 10-year review. Spine (Phila Pa 1976) 2007;32:2989–95. doi: 10.1097/BRS.0b013e31815cddfc. [DOI] [PubMed] [Google Scholar]
- 105.Kanter AS, Wang MY, Mummaneni PV. A treatment algorithm for the management of cervical spine fractures and deformity in patients with ankylosing spondylitis. Neurosurg Focus. 2008;24:E11. doi: 10.3171/FOC/2008/24/1/E11. [DOI] [PubMed] [Google Scholar]
- 106.Hershman EB, Bercik RJ, Allen SC, Fielding JW. Correction of chin-on-chest deformity in ankylosing spondylitis through a fracture site. A case report. Clin Orthop Relat Res. 1985;201:201–4. [PubMed] [Google Scholar]
- 107.Kiwerski J, Wieclawek H, Garwacka I. Fractures of the cervical spine in ankylosing spondylitis. Int Orthop. 1985;8:243–6. doi: 10.1007/BF00266867. [DOI] [PubMed] [Google Scholar]