Abstract
Background:
Management of nail injuries can often be a challenging experience, especially in presence of complex fingertips’ injuries that include soft tissue loss and distal phalanx injury. Most studies found in the literature focus on individual injuries and describe methods to tackle those injuries, notwithstanding the fact that the nail, nailbed, distal phalanx, soft tissue and skin of the finger tip form a complex and often more than one element of this complex is injured. This retrospective study therefore focuses on the management of nail bed injuries as a part of the complex finger tip injury and outlines the surgical principles and techniques that were used in their management.
Materials and Methods:
Two hundred and forty patients from a tertiary care center in different clinical settings where a wide variety of cases involving the nail bed injuries were included in this study. Patients comprised of 192 (80%) males and 48 (20%) females with the average male age of 37.3 years (range 1-66 years) and average female age of 29 years (range 1-59 years). 210 patients had single finger involment, 30 patients had two finger involvement (total fingers involved- 270). The middle finger was most commonly involved while the index finger was the second most commonest finger involved. In 198 (89.18%) patients local anaesthesia was used while in the rest: regional blocks [n = 10 (4.5%)] and general anaesthesia [n = 14 (6.3%)] were used.
Results:
In this retrospective study, out of the total of two hundred and forty patients, 222 (92.5%) patients underwent surgery, while the rest 18 (7.5%) were treated conservatively. Two hundred and ten patients who underwent surgery had complete healing over the course of treatment and followup, while four patients needed secondary interventional. Eight patients who had surgery were migrant workers were lost to follow up after surgery. Eight patients had postoperative complications that included infection, secondary necrosis, wound breakdown and non healing fractures.
Conclusion:
Accurate and timely diagnosis of nail bed injury and its meticulous repair is cardinal to the management of any nail bed injury. However all nail bed injuries must be seen in the context of associated injuries of the finger tip complex, namely skin, soft tissue and distal phalanx injuries. Fixation of associated bony injury which closely underlines the nail bed and provides physical support to the nail bed along with correction of soft tissue injuries in the form of flaps or grafts, compounded by the repair or replacement of nail plate in the first 24 hours.
Keywords: Fingertip injuries, nail bed injuries, trauma
MeSH terms: Nail disease, soft tissue injuries, trauma, wounds and injuries
Introduction
The human nail is a unique cutaneous structure that develops around the 10th week of intrauterine life from the sole plate and normally arises on the dorsal aspect of the tip of every finger or toe. While the nail provides stability and counter support to the soft tissue of the fingertip and functionally helps in lifting tiny objects and performing delicate movements, esthetically a finger without a nail looks deformed and unnatural to the human eye notwithstanding the occasional pleasurable scratch that is often missed in the literature. It is, therefore, imperative that every injury of the nail and nail bed complex is treated with the utmost care as the primary surgery is the best possible time to treat this injury. This paper reviews the causes and management of fingertip injuries with nail and nail bed injury and suggests possible strategies to reduce the incidence of such injuries along with a review of literature. Finger tip injuries can have multiple combinations of injuries involving the nail plate, nail bed, distal phalanx, and the soft tissue of the fingertip and therefore it is crucial that the management of all these injuries be considered in toto, thereby resulting in better patient outcomes.
Materials and Methods
240 consecutive patients with nail bed injuries referred to the plastic surgery department between April 2011 and April 2016 were included in this study. The nature of the injury along with the choice of available treatment options was explained in detail to all the patients, and they consented to undergo our management option preferred for their case. All patients were studied for the following parameters: age, sex, cause of injury, detail of injury, finger involved, operative treatment, postoperative pain, postoperative complications, antibiotic coverage, and wound infection. All injuries were photographed, X-rayed, and details of the wound injuries were documented before treatment. On discharge, all injuries were treated and followed up until they healed completely or lost to followup. All patients were operated within the first 24 h except severe crush injury cases where the vascularity was compromised and the patient was treated with venoactive drugs such as aspirin, pentoxifylline, and dipyridamole along with maintaining warmth and hydration to improve the microcirculation. All wounds were washed thoroughly with povidone-iodine solution and saline at first contact with the patient to reduce the chance of infection and remove all the contaminants and debris. Further, all patients received intravenous broad-spectrum antibiotics on admission and these were converted to oral antibiotics on discharge of the patient and continued for 7 days, and if infection persisted, cultures were taken and antibiotics changed according to sensitivity studies. Patients with comorbidities such as diabetes were managed by a diabetic specialist, and strict blood glucose control was maintained by insulin therapy when needed. For demographic data the total number of patients (n = 240) were included but for the analysis of results, 232 patients were selected as 8 patients were lost to followup.
Results
Out of a total of two hundred and forty patients with nail bed injuries, 192 (80%) were males and 48 (20%) females. The average age of male patients was 37.3 years (range 1-66 years) and an average age of female patients was 29 years (range 1-59 years). Of the 240 patients, 210 patients had single finger involment, 30 patients had two finger involvement (total fingers involved- 270) and eight patient had additional injuries. The most common finger involved was the middle finger, whereas the second most common finger involved was the index finger. The most common cause of injury was industrial trauma [(n = 123) (51.25%)], followed by road traffic accidents [(n = 49) (20.41)], Kitchen food grinder injury (n = 38) (15.83%) and door closure injuries [(n = 30) (12.5%)]. All patients on admission were as protocol administered a combination of intravenous antibiotics namely ceftriaxone, amikacin and metronidazole as per standard dosages based on body weight for 48 hours and then shifted to oral cefuroxime medication for 7 days. New antibiotics were started only on the basis of positive culture reports. In 222 (92.5%) patients, surgery was carried out while in 18 (7.5%) patients, conservative treatment was followed. Local anesthesia was used in 198 (89.18%) patients, whereas in the rest regional blocks [n = 10 (4.5%)] and general anesthesia [n = 14 (6.3%)] were used. Table 1 shows a list of all surgical procedures done in our patients. 65 (27%) patients had fractures of the distal phalanx in one form or other and 44 of these had fixation of these fractures. While 210 patients of the total patients who underwent surgery had complete healing, 4 patients needed secondary surgery. Of this, one patient had a severe crush injury and further necrosis was noticed postoperatively extending proximally in the nail bed and fingertip and therefore further debridement and wound repair was needed. In one patient, an infective granuloma appeared under the distal edge of the nail plate which needed to be removed. In two patients, infection and breakdown of wound occurred and secondary surgery was needed. In two patients, the distal phalanx fracture (which was present as the distal part of the distal phalanx and comminuted) failed to heal but was left alone as it did not functionally interfere with the function and patients were reluctant to undergo further interference. Five patients had wound infection[5/232, (2.15%)] in their postoperative follow up period and were successfully treated with antibiotics started as per the pus culture and sensitivity reports. Organisms isolated in the culture included staphylococcus aureus, klebseilla and pseudomonas. The average followup period was 1 years and 2 months (range 8-25 months). In 12 cases, the patients were unhappy with the quality of the new nail as it did not match the other finger nails though a new nail was formed on the repaired nail bed. The dominant hand was involved in153 (63.75%) patients while the nondominant hand was involved in 87 (36.25%) patients. All patients had some degree of postoperative pain which was treated with standard analgesics, and chronic pain (over 6 months) has not been reported by any of the patients. General anesthesia was preferred in pediatric cases and when other injuries in other body regions needing surgery were present or both hands were involved. Regional anesthesia was preferred when patients had multiple fingers involvement. Eight patients who were migrants were immediately lost to followup.
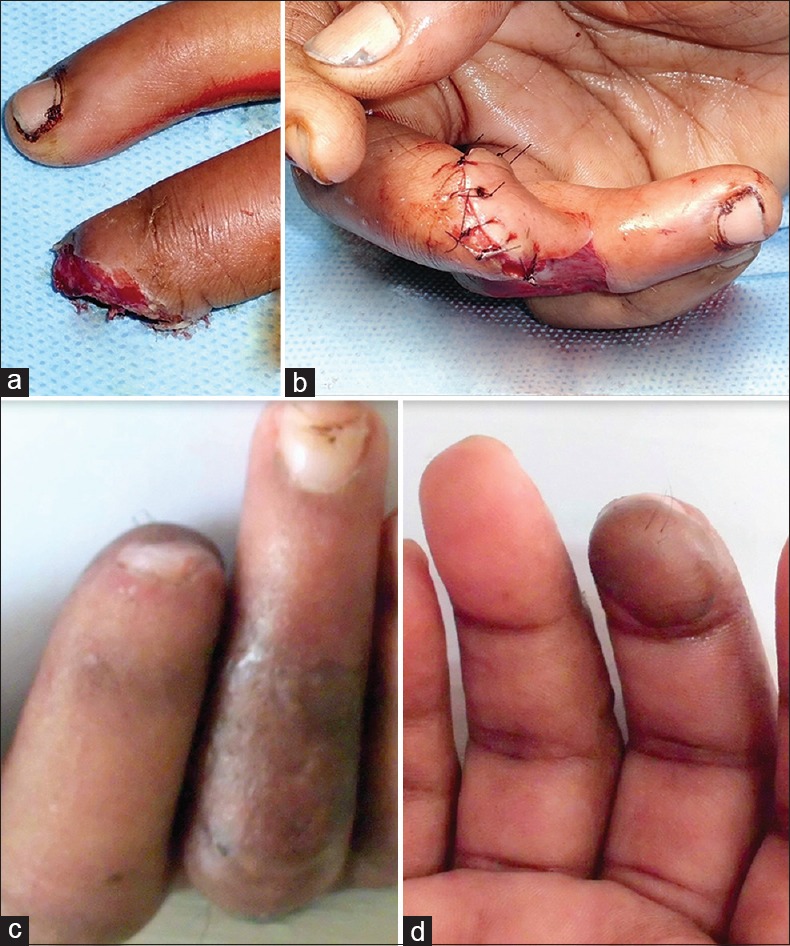
Table 1.
Surgical procedures
Representative cases
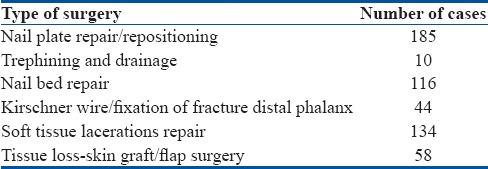
Case 1
A 44-year-old male was involved in an industrial accident which resulted in the partial avulsion of proximal part of nail and nail bed plate with soft tissue injury and fracture of the distal phalanx [Figure 1a]. Under local anesthesia, a Kirschner wire fixation of the distal phalanx fracture was done followed by debridement and repair of the nail bed with 6-0 Vicryl. The nail plate was repositioned and sutured to provide external support [Figure 1b and c]. Postoperatively, the wounds healed well, and acceptable nail growth was seen on followup [Figure 1d].
Figure 1.
(a) Clinical photograph showing industrial accident causing partial avulsion of proximal part of nail and nail plate with soft tissue injury. (b) X-ray picture showing Kirschner wire fixation of distal phalanx fracture. (c) Clinical photograph showing repair of nail bed, nail plate, and Kirschner wire in position. (d) Clinical photograph showing good healing with new nail growth at 9 months followup
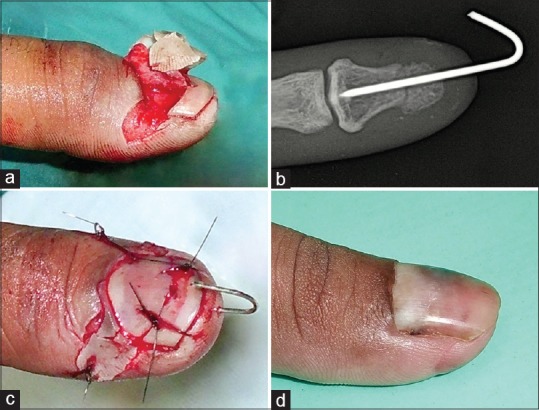
Case 2
A 23-year-old female was referred with a food processor blade injury that accidently occurred while grinding food spices in a food processor. The injury resulted in the amputation of the tip of the right middle finger with loss of most of the nail plate and nail bed along with partial loss of distal phalanx bone and soft tissue of the fingertip [Figure 2a]. To reconstruct the tip and save the nail bed remnant, a cross finger flap was done from the ring finger [Figure 2b]. The cross finger flap was then divided after 3 weeks, and a postoperative picture at 9 months shows good soft tissue healing with new nail growth from the preserved remnant of the nail bed matrix [Figure 2c and d].
Figure 2.
Clinical photograph showing (a) Food processor blade injury with loss of middle fingertip soft tissue, nail plate, nail bed, and part of distal phalanx. (b) Cross finger flap done to cover raw area with attempt to preserve remaining part of nail bed. (c and d) postoperative pictures showing good soft tissue healing with new nail growth of middle finger at 9 months
Discussion
The nail is an integument found exclusively in primates while modifications of this are seen in other mammals. The sterile matrix provides an ideal bed to which the nail plate can exclusively adhere and any disruption will eventually lead to nonadherence between the two.1 If the nail must grow, the germinal matrix needs to be preserved and if the nail must look normal, it must be well supported by the nail bed, the underlying bony distal phalanx, and the surrounding soft tissue. Injury to any of the structures that directly support the nail and nail bed complex will result in some abnormality, and therefore, it is essential that every fingertip injury is critically analyzed to chart out the elements injured, and a plan is promulgated to repair the same in the most prudent manner. It is believed that in most fingertip injuries, the middle finger and the thumb are most frequently injured as the middle finger is the longest one, and the thumb is the most common finger used to grip something when the injury happens.2 However, in our series, the most frequently injured finger was the middle finger and the second most common was the index finger.
Trauma remains the most common cause of nail bed injury and deformity. In our study [Table 2], the majority of the cases (n = 123; 51.25%) resulted from industrial accidents, and this could be explained by the fact that a large industrial belt with large and small scale industries neighbors the hospital. Following common well-established safety measures at construction sites, industrial and other work sites would have helped to reduce these injuries. The second most common cause of nail bed injuries in this series was road traffic accidents (n = 49; 20.41%). The most common cause of injury in patients using two-wheeler vehicles was from the handle bar being hit by an oncoming vehicle. The mere presence of a simple handguard would have helped prevent this injury. Kitchen food grinder injury (n = 38; 15.83%) accounted for the third most common cause of fingertip injury in our study. These injuries could be prevented by installing auto shut off features in the grinder when the lid is opened. The last group of fingertip injury causes was from accidental closure of doors. This is a preventable injury which can be avoided by simply attaching a “door closer:” a device that prevents the sudden and rapid closure of the door. Sporting injuries, iatrogenic, and self-inflicted injuries were conspicuous by their absence in our series.
Table 2.
Causes of nail bed injuries

Since the nail bed is so intimately associated with the nail plate, distal phalanx and soft tissue of the finger tip, the surgical management of nail bed injuries must address these other injuries as well. In contaminated wounds, immediate exploration and a thorough washout are essential as infection can be a serious issue leading to even flexor sheath infection and distal amputation.3 All our patients underwent surgical repair of all injuries in the first 24 hours and were covered comprehensively with antibiotics. This caused a low incidence of infection in this series (2.15%). In treating subungual hematomas with more than 50% surface area of the nail bed, we have routinely used wherever necessary a 10 no. surgical stab blade to cut a small triangular hole in the nail plate to drain the hematoma and give a saline washout under aseptic precautions, though the literature suggest the use of an 18 G needle, hot wire or drill.
In the presence of distal phalanx fractures, the possibility of concurrent significant nail bed injury is quite high and therefore removal of the nail plate, repair of the nail bed injury with fine 6-0 or 7-0 absorbable sutures, and replacing the nail plate as a protective cover to the nail bed is advisable and this has been our standard mode of therapy in patients suspected to have nail plate injury. Strauss et al.4 used 2-octyl cyanoacrylate (Dermabond) to repair nail bed wounds and found that the repair was faster than suture repair and in addition provided similar cosmetic and functional results. However, in all our cases, we have done a suture repair. Wherever possible, we have replaced the nail to cover the injured nail bed as it has provided great support to the nail bed and helped in its healing. It also helps prevent synechiae between the eponychial fold and the nail bed. When the nail plate has been lost or damaged beyond use a silastic sheet or a bit of plastic cut to nail shape can be used. Ogunro5 reported that when the residual nail bed is effectively covered to prevent drying and maintain a local environment suited for tissue regeneration, normal nail growth may be obtained. Many surgeons use a figure-of-eight stitch or its modifications to hold the nail plate in position.6 However, we have always used simple four quadrant sutures to pin the avulsed nail in position. Three of our patients had a significant area of nail bed loss. However, none of them consented to taking a nail bed graft from the adjoining finger or the big toe which is the procedure that is recommended under the circumstances. This was also due to the fact that these patients were all workers and they were worried to let a normal finger or toe tip be subjected to a surgical procedure while they already had an injured finger. The vascular and lymphatic channels are well developed into the nail bed, and the presence of multiple anastomoses permits the use of the nail bed and nail matrix as flaps with acceptable results.7 In all these cases, the remnant nail bed was repaired along with other injuries, and healing resulted in significant shortening of nail and deformity. In 4 patients who had minor loss of nail bed tissue, tiny local nail bed flaps were used to align and repair small defects in the nail bed. While the wounds may heal in 2–3 weeks, the nail plate will take around 3 months to grow completely. Splinting the finger for 3 weeks helps the healing process and causes less pain to the patient, and this has been a regular feature in managing our fingertip injuries.
All soft tissue injuries of the fingertip must be meticulously repaired as they form a supportive framework for the nail bed. In the presence of exposed distal phalanx coupled with the loss of tissue, a flap cover must be planned. A total of 58 flaps of various types were done in this series. Where the defect was central with exposure of distal phalanx, v-y flaps were done. When the defect was either ulnar or radial wards, a Kutler flap was the preferred mode of flap cover. In some of the cases where the crush laceration injury prevented us from planning any such flaps, a small rotation advancement flap of the remnant soft tissue was done to cover the defect. When the defect was large, cross finger flaps were used, and when multiple fingers needed soft tissue cover, abdominal flaps were preferred. In few patients, these flaps were sometimes combined with small skin grafts where the flap was mainly used to cover the exposed distal phalanx. While all attempts must be made to restore the fingertip pulp with volar innervated flaps from the same finger for functional purposes, in cases where only soft tissue loss of the pulp without any bony injury or exposure is present along with the nail bed injury, skin grafting may be the procedure of choice. Sometimes, the nail and nail bed complex may be completely avulsed from the distal phalanx with only a distal attachment to the soft tissue. Here, again one must access the viability of the avulsed tissue and debride and replace the entire complex back into its original position and suture it along the nail plate if available to enable maximum survival of the nail bed and subsequent nail growth. Small avulsed fragments can also be put back as composite-free grafts.
Fingertip injuries with nail bed injuries in children are often treated conservatively, and small wounds and lacerations may be left to heal spontaneously. Roser and Gellman8 reported in their study in children that the results of simple nail trephination were equivalent to or superior to the removal of the nail and nail bed repair with significantly lower cost when treating fingernail crush injuries with subungual hematoma. Small distal amputations of digits in infants have been known to survive as composite grafts, and this should be attempted after adequately cautioning the parents of the possible loss of the amputated part and need for reconstructive surgery.
The distal phalanx being closely related to the nail bed provides support and stability to the overlying nail bed from the volar side, and it is not surprising that distal phalanx fractures are found in about 50% of nail bed injuries. In fingertip crush injuries, distal phalangeal comminuted tuft fractures are quite common, but these do not need any specific treatment as the soft tissue around it gives adequate support along with the nail bed repair. In majority of our patients, these tuft fractures were supported by nail bed repair, soft tissue repair, and external splinting. However, with fractures of the middle and proximal part of the distal phalanx as well as with displaced fractures, Kirschner wire fixation will be needed to achieve and maintain reduction of the fractures as were carried out in 44 of our patients. In all our cases wherever possible, the nail plate was put back and sutured in place – the nail plate acted as a splint and also supported the distal phalanx fracture.
Even the most meticulous management of fingertip injuries may result in complications as predicting the eventual nail bed healing, and subsequent nail plate growth becomes difficult. In one of our patient who had a complex crush injury to the fingertip with bone and soft tissue loss, reconstruction with a v-y flap provided soft tissue cover to the exposed bone but resulted in a deformed nail growing over the tip of the finger in a curved fashion (parrot beak deformity) that caused severe pain and interfered with the patient finger function. Eponychial injuries must be meticulously repaired, but if there is a loss of eponychium which can lead to loss of nail shine then replacing the eponychium as a composite graft from the toe has been suggested in the literature.1 Twenty two cases had eponychial lacerations which were repaired primarily in our series. A large number of our patients were manual laborers and did not really bother nor complain about the loss of nail shine. In one of our cases, there was a nonadherence of the nail plate with the nail bed, and a granuloma appeared at the junction which was treated with antibiotics and curetting. Twelve of the patients had nail bed ridging possible from nail bed scarring on followup. However, none of them wished any correction as it did not bother them functionally. Three of our patients had bulbous fingertips on followup and all of these had severe crush injuries will comminute distal tuft fractures that were conservatively treated. Loss of bony distal phalanx support may sometimes need corrective bone grafting surgery after raising the nail bed complex as a flap. Healed fingertip injuries are often sensitive and sometimes painful, and therefore, rehabilitation of the fingertips must involve adapting the sensitive part to gradually increasing duration and frequency of stimulation as happened in three of our patients.9 In patients who had a total amputation proximal to the nail, reimplantation is a good technique if facilities are available.10 When the amputated part is crushed and unfit for reimplant then doing a v-y advancement flap and free grafting the nail bed has been reported.11 Abdominal flaps are usually not preferred in the reconstruction of fingertip injuries as they are often bulky and insensate, but they were done in our cases when multiple fingers were involved or there was a significant loss of bone and soft tissue support for the nail bed and adequate local flaps or cross finger flaps were not available.
Conclusion
Accurate and timely diagnosis of nail bed injury and its meticulous repair is cardinal to the management of any nail bed injury. However all nail bed injuries must be seen in the context of associated injuries of the finger tip complex, namely skin, soft tissue and distal phalanx injuries. Fixation of associated bony injury which closely underlines the nail bed and provides physical support to the nail bed along with correction of soft tissue injuries in the form of flaps or grafts, compounded by the repair or replacement of nail plate in the first 24 hours.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Bharathi RR, Bajantri B. Nail bed injuries and deformities of nail. Indian J Plast Surg. 2011;44:197–202. doi: 10.4103/0970-0358.85340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pearce S, Colville RJ. Nailbed repair and patient satisfaction in children. Ann R Coll Surg Engl. 2010;92:483–5. doi: 10.1308/003588410X12664192075891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fairbairn N. No such thing as “just” a nail bed injury. Pediatr Emerg Care. 2012;28:363–5. doi: 10.1097/PEC.0b013e31824d9d57. [DOI] [PubMed] [Google Scholar]
- 4.Strauss EJ, Weil WM, Jordan C, Paksima N. A prospective, randomized, controlled trial of 2-octylcyanoacrylate versus suture repair for nail bed injuries. J Hand Surg Am. 2008;33:250–3. doi: 10.1016/j.jhsa.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 5.Ogunro EO. External fixation of injured nail bed with the INRO surgical nail splint. J Hand Surg Am. 1989;14(2 Pt 1):236–41. doi: 10.1016/0363-5023(89)90012-9. [DOI] [PubMed] [Google Scholar]
- 6.Bindra RR. Management of nail-bed fracture-lacerations using a tension-band suture. J Hand Surg Am. 1996;21:1111–3. doi: 10.1016/S0363-5023(96)80329-7. [DOI] [PubMed] [Google Scholar]
- 7.Tos P, Titolo P, Chirila NL, Catalano F, Artiaco S. Surgical treatment of acute fingernail injuries. J Orthop Traumatol. 2012;13:57–62. doi: 10.1007/s10195-011-0161-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roser SE, Gellman H. Comparison of nail bed repair versus nail trephination for subungual hematomas in children. J Hand Surg Am. 1999;24:1166–70. doi: 10.1053/jhsu.1999.1166. [DOI] [PubMed] [Google Scholar]
- 9.Rosenthal EA. Treatment of fingertip and nail bed injuries. Orthop Clin North Am. 1983;14:675–97. [PubMed] [Google Scholar]
- 10.Endo T, Nakayama Y. Microtransfers for nail and fingertip replacement. Hand Clin. 2002;18:615–22. doi: 10.1016/s0749-0712(02)00077-x. [DOI] [PubMed] [Google Scholar]
- 11.Raja Sabapathy S, Venkatramani H, Bharathi R, Jayachandran S. Reconstruction of finger tip amputations with advancement flap and free nail bed graft. Hand Surg Br. 2002;27:134–8. doi: 10.1054/jhsb.2001.0695. [DOI] [PubMed] [Google Scholar]


