Abstract
Background
Brain laser interstitial thermal therapy (LITT) under magnetic resonance imaging (MRI) guidance has recently gained US clinical approval for the ablation of soft, neurological tissue. LITT is a minimally invasive alternative to craniotomy.
Objective
While safety and efficacy are the focus of most current LITT studies, it is unclear how acute care costs (inpatient care ± aftercare) of LITT compare to craniotomy in an academic medical center. Therefore, the purpose of this analysis is to examine these costs of using brain LITT under MRI guidance compared to craniotomy in complex anatomies.
Methods
Consecutive patients treated at a single US center from 1 January 2010 to 21 October 2014 were retrospectively evaluated. Patients were included if they had a primary procedure for LITT or craniotomy (International Classification of Diseases, 9th revision, Clinical Modification [ICD-9-CM] procedure code 17.61 or ICD-9-CM procedure code 01.59, respectively) and were subgrouped according to their diagnosis of primary brain or metastatic brain cancer (ICD-9-CM 191.0–191.9 or ICD-9-CM 198.3, respectively). Patients were excluded if they had co-morbid conditions such as brain edema (ICD-9-CM 348.5). Patients were matched (LITT vs. craniotomy) based on diagnosis. Appropriate statistical analyses were undertaken to examine the year 2015 costs for care in all settings (acute hospital and post-hospital care, i.e., skilled nursing facility, rehabilitation, and home care) were examined.
Results
In patients treated for a primary brain cancer, there was no statistical difference in the acute and post-care costs of LITT and craniotomy (inverse variance, mean difference [MD], random effects model): MD = −US$1669; 95% confidence interval (CI) −$8192 to $4854; P = 0.62. When examining difficult to access primary malignancies, no difference was found: MD = −US$4719; 95% CI −$12,183 to $2745; P = 0.22. In metastatic brain cancer, LITT was found to be significantly less costly than craniotomy: MD = −US$6522; 95% CI −$11,911 to −$1133; P = 0.02.
Conclusions
In patients with metastatic brain cancer, LITT is less costly than craniotomy. Patients receiving LITT had a significantly shorter length of hospital stay, were significantly older, and were more likely to be discharged home. The use of LITT may be a reasonable option in bundled episodes of care for brain cancer and may fit into the Bundled Payment for Care Improvement (BPCI) program being evaluated by Medicare and providers.
Keywords: Skilled Nursing Facility, Home Healthcare, Magnetic Resonance Imaging Guidance, Inpatient Rehabilitation Facility, Barnes Jewish Hospital
Key Points for Decision Makers
| Minimally invasive brain cancer surgery, such as laser interstitial thermal therapy (LITT) may lessen the need for aftercare compared with that following more invasive surgeries. |
| Patients who are diagnosed with brain cancer generally have a poor prognosis and would likely prefer to spend the remainder of their lives at home. Minimally invasive surgery may offer this as a higher percentage of patients were discharged home versus craniotomy. |
| Minimally invasive brain surgery (LITT) may offer the opportunity to provide a bundle of care (hospital plus aftercare, e.g., comprehensive care for a 90-day period) and save the healthcare system money. These types of bundles are gaining acceptance under the Affordable Care Act initiatives for novel care delivery and payment models. |
Introduction
In the USA, there were 33,455 patients treated for primary brain cancer (International Classification of Diseases, 9th revision, Clinical Modification [ICD-9-CM] 191.0–191.9 [1]) in the year 2012 [2]. Using Medicare costs, the estimated inpatient acute care costs for treating these patients was US$24,290 [2]. Of these patients, approximately 25% were discharged to either a skilled nursing facility (SNF) or inpatient rehabilitation facility (IRF), with an additional 15% discharged to home healthcare [2]. Additionally, for the same year, there were 43,175 patients treated for metastatic brain cancer (ICD-9-CM 198.3) [2]. The estimated inpatient acute care costs for treating these patients was US$16,210 [2]. Similarly, approximately 25% were discharged to either an SNF or IRF, with an additional 22% discharged to home healthcare [2]. The average estimated reimbursement rates for an IRF approach US$23,000 [3],1 for an SNF they are US$4900,2 and for home healthcare they are US$159/day.3 Thus, these patients can cost the healthcare system significant amounts of money once acute inpatient and aftercare costs are combined. Additionally, patients who undergo complex craniotomy procedures (e.g., excisional surgery in or near sensory/motor areas [areas of eloquence] or deep-seated tumors) can incur complication rates of upwards of 15% [4–6], which commonly result in the need for aftercare in such settings as an SNF or IRF. It is thus important to identify therapies that can be used in treating complex anatomy, in order to reduce complications and associated care (and costs) peri- and post-procedure. A new technology, brain laser interstitial thermal therapy (LITT) under magnetic resonance imaging (MRI) guidance for treating these types of tumors has recently been introduced into the USA [7, 8]. In published data, the results have been found to minimize complications, most especially in complex anatomy [9]. The purpose of this current analysis is to examine the costs of using brain LITT under MRI guidance compared to craniotomy in these types of complex anatomies. US academic medical centers have incorporated LITT as an option in brain tumor surgery, especially in brain tumors where traditional surgeries such as craniotomy cannot access the tumor adequately due to its location in or near areas of eloquence or due to its difficult to access (DTA) and/or deep-seated nature. It has been found that LITT may reduce complications while at the same time resecting more of the tumor. Both of these factors are correlated to extending the lifespan of patients [10]. Medicare has recently introduced a Bundled Payment for Care Improvement (BPCI) program [11], which evaluates therapies over extended bundles of care (e.g., hospital care plus rehabilitation, nursing, and home care over a 90-day period) and pays for them as such. Thus, care provided and its associated costs post-hospital discharge will become an important component of the patient’s overall care. LITT may fit into this treatment paradigm based on shorter hospital stays [12].
Lastly, this analysis examines risk factors for complications such as post-operative hospital stay and its association with venous thromboembolism (VTE). It has been found that, on average, patients who develop VTE stay in the hospital for 7.7 days post-operatively compared with 6.1 days in those with no VTE diagnosed [13].
Methods
Consecutive patients treated at Barnes Jewish Hospital in St. Louis, MO, USA between 1 January 2010 and 21 October 2014 were retrospectively reviewed to identify those with a diagnosis code of either ICD-9-CM 191.0–191.9 (malignant neoplasm of the brain) or 198.3 (secondary/metastatic malignant neoplasm of the brain). Only patients with brain LITT (ICD-9-CM 17.61) or craniotomy (ICD-9-CM 01.59) were included in the analysis. The analysis was limited to only include patients with co-morbidities because this is the subset of patients we hypothesized were most likely to be treated with LITT. Health records were reviewed for diagnosis-related group (DRG) 25 (craniotomy and endovascular intracranial procedures with major complications) and DRG 26 (craniotomy and endovascular intracranial procedures with complications). However, the methods were revised as the analysis began to only include subjects assigned to DRG 26 due to the limited sample size of DRG 25 (n = 4) within the LITT cohort. After 2013, LITT as the principal procedure (ICD-9-CM 17.61) was used in the vast majority of patients assigned to DRG 26. Therefore, a before and after analysis could be performed on similar type patients in a craniotomy versus LITT analysis (with the craniotomy group largely being treated prior to 2013). The groups were then subgrouped according to their diagnosis of primary brain or metastatic brain cancer (ICD-9-CM 191.0–191.9 or 198.3, respectively). Subjects were further subgrouped by lesion location. If the lesion was located in or near areas of eloquence (sensory/motor) and deep-seated in nature they were determined to be ‘DTA.’ DTA lesions were physician-determined.
All costs were examined during the peri- and post-procedure period if they included inpatient surgery and stay and discharge to another site of care service (i.e., IRF, SNF, home healthcare, hospice, or readmittance due to complications resulting from the procedure). Costs for inpatient care were converted from charge to costs (using the institution-specific cost to charge ratio of 0.362). The institution-specific cost to charge ratio is calculated by Medicare for every hospital that is eligible to treat Medicare patients (i.e., the vast majority of US hospitals). As an example, for every US$1000 of charges submitted on a claim form by Barnes Jewish Hospital, it costs Barnes US$362 to deliver these services (US$1000 × 0.362 = US$362). These costs were reflective of the year in which they were incurred and were adjusted based on medical site-specific Consumer Price Index (CPI) inflation factors [14] to the year 2015. For additional site of service care, the specific 2015 Medicare reimbursement rate was adjusted for cost. It was assumed that patients were classified under Case Mix Group (CMG) 302 (Non-traumatic brain injury, due to surgery, Tier 1) for IRF care. For the year 2015 at Barnes Jewish Hospital, this reimbursement rate was estimated to be US$24,440 (after adjustments for wages, low-income patients, and teaching). This also assumes an average length of stay (ALOS) of 13 days for IRF care based on Medicare data [15]. It was further assumed that the costs for type of IRF setting were 99.7% of the reimbursement level based on Medicare data for IRFs, or a cost of US$24,367 [16]. Further, it was estimated that the reimbursement for SNF care was US$4284. This was calculated as follows: first, it was assumed that these patients would require ultra-high rehabilitation and would fall under resource utilization group (RUG) code RUC. The ALOS for this group in the St. Louis (MO, USA) area for 2014 was 26 days [17]. This 26-day ALOS was input into an SNF calculator, as well as St. Louis wage-specific indexes being used. Using these variables, the amount was calculated to be US$4930 for the 2015 calendar year [18]. This reimbursement rate was then adjusted for cost using a cost to reimbursement ratio of 86.9% [19], resulting in a cost of US$4284. Lastly, home healthcare was assumed to be at a full episode of care/payment. The patient discharged to home healthcare was classified as having high clinical, high functional, and high service resources, or C3F3S3 (CMS payment group 10333), with a case mix weight of 1.183. For the St. Louis area, at a non-routine add-on supply severity of ‘3’, the reimbursement level for the 2015 financial year is US$3471 [20]. This reimbursement rate was then adjusted for cost using a cost to reimbursement ratio of 87.3% [21], resulting in a cost of US$3030. Each of these adjusted costs were used as proxies for the overall cost for care of a patient, depending upon whether follow-on care was required.
Statistical Analysis
The analysis of costs were evaluated to determine whether the aggregate costs for acute care (inpatient stay ± aftercare) were statistically different from each other using the inverse variance, mean difference (MD), random effects with 95% confidence interval (CI) analysis method. Significant cost outliers were excluded from this analysis if they were determined to be outliers using Grubb’s test P < 0.05 for outlier identification [22]. Grubb’s test was used with the understanding that these data came from a normally distributed population. Ages of the patients were also evaluated at baseline to determine if there was a statistical difference. Further, an analysis of the incidence of the aftercare required (by site and in aggregate for 30-day readmissions, IRF, SNF, and home care) was also examined using a Mantel–Haenszel random effects risk ratio (RR) analysis with 95% CIs [23]. Summary statistics on length of stay (LOS) were also analyzed using the mentioned statistical methods. Lastly, a sensitivity analysis was performed on post-discharge total IRF costs of ± 25% of the amount used in the analysis (US$24,367; range of US$18,275 to US$30,459) as these costs were the largest cost driver of care outside of the hospital.
Results
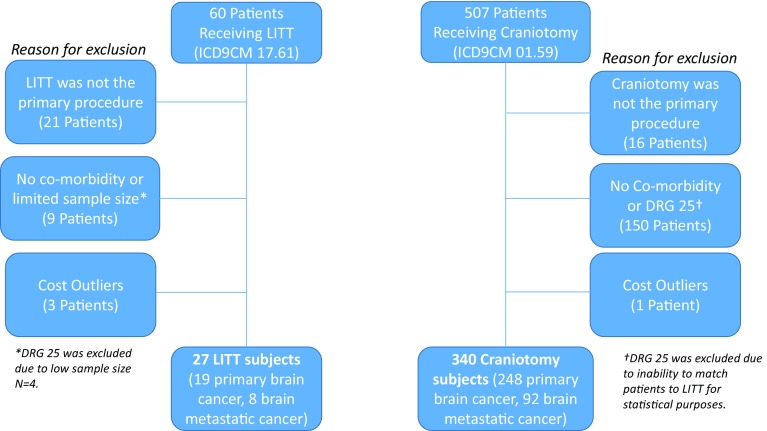
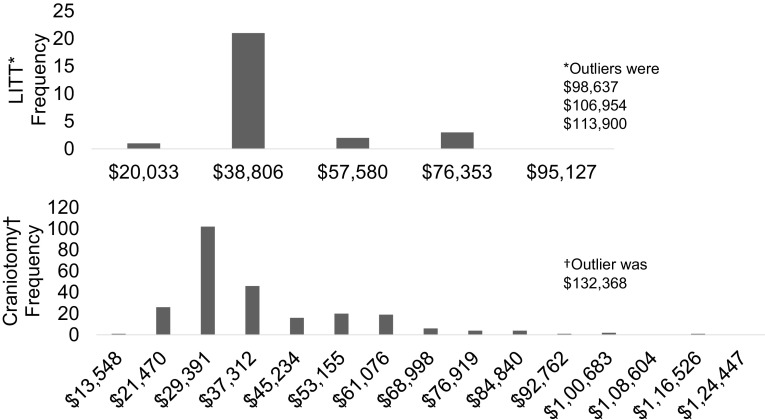
The dataset provided by Barnes Jewish Hospital originally contained 60 patients treated with LITT and 507 patients treated with craniotomy (Fig. 1); however, in order to make a side-by-side comparison with LITT and craniotomy, subjects were excluded based on the criteria described in Sect. 2. Within the LITT cohort, 33 patients were excluded. Twenty-one were excluded because LITT was not the principal or only procedure and nine LITT patients did not exhibit a co-morbidity (DRG 25 or DRG 26)4 or represented a very small number of patients with a major co-morbidity and/or complication [4]—because only four LITT patients reported DRG 25 (major complications), they were excluded from further subgrouping. Three LITT subjects were determined to be cost outliers5 (based on Grubbs test) (Fig. 2). Thus, 27 LITT patients remained, of whom 19 were diagnosed with primary brain cancer and co-morbidity (ICD-9-CM diagnosis 348.5) and eight with a diagnosis of metastatic brain cancer (ICD-9-CM 198.3). The baseline characteristics of the patients are shown in Table 1. In the vast majority of cases, these cancerous lesions, determined to be ‘DTA’ (for both LITT and craniotomy), were supratentorial in nature and were located in the frontal, parietal, and temporal lobes of the brain.
Fig. 1.
Subject inclusion/exclusion flow chart: consecutive patients treated at Barnes Jewish Hospital in St. Louis, MO, USA between 1 January 2010 and 21 October 2014 under ICD-9-CM 191.0–191.9 (malignant neoplasm of the brain) or 198.3 (secondary/metastatic malignant neoplasm of the brain). Subjects were reviewed for DRGs 25 and 26. Only subjects with DRG 26 were included in subgroup analyses due to a low sample size for DRG 25 within the LITT cohort. Cost outliers were excluded from the analysis. DRG diagnosis-related group, ICD-9-CM International classification of diseases, 9th revision, clinical modification, LITT laser interstitial thermal therapy
Fig. 2.
Distribution of procedure costs for LITT and craniotomy. Actual cost data were analyzed and clustered by frequency using Excel® data analysis ToolPak and Grubb’s test. Actual costs of outliers are presented. LITT laser interstitial thermal therapy
Table 1.
Baseline characteristics and discharge disposition
| Characteristic | LITT | Craniotomy |
|---|---|---|
| Primary brain cancers (ICD-9-CM diagnosis 191.0–191.9) | ||
| Number of patients | 19 | 248 |
| Age (years) [mean ± SD (range)] | 57.53 ± 12.05 (35–81) | 51.73 ± 15.47 (22–85) |
| M/F (n) | 14/5 | 148/100 |
| Diagnosis breakout [n (%)] | ||
| Malignant neoplasm of cerebrum (191) | 2 (10) | 3 (1) |
| Malignant neoplasm frontal lobe (191.1) | 9 (47) | 101 (41) |
| Malignant neoplasm of temporal lobe (191.2) | 2 (10) | 76 (31) |
| Malignant neoplasm of parietal lobe (191.3) | 1 (5) | 27 (11) |
| Malignant neoplasm of occipital lobe (191.4) | 1 (5) | 13 (5) |
| Malignant neoplasm of ventricles (191.5) | 1 (5) | 5 (2) |
| Malignant neoplasm of cerebellum NOS (191.6) | 0 | 5 (2) |
| Malignant neoplasm of brain stem (191.7) | 0 | 0 |
| Malignant neoplasm of other parts of brain (191.8) | 2 (10) | 14 (6) |
| Malignant neoplasm of brain, unspecified (191.9) | 1 (5) | 4 (2) |
| Number of 30-day readmissions [n (%)] | 0 | 31 (13) |
| Discharged to [n (%)] | ||
| Home | 15 (79) | 163 (66) |
| IRF | 3 (16) | 54 (22) |
| SNF | 0 | 3 (1) |
| Home healthcare | 1 (5) | 28 (11) |
| Metastatic brain cancer (ICD-9-CM diagnosis 198.3) | ||
| Number of patients | 8 | 92 |
| Age (years) [mean ± SD (range)] | 58.73 ± 9.65 (40–67) | 61.98 ± 10.23 (29–81) |
| M/F (n) | 5/3 | 40/52 |
| Number of 30-day readmissions [n (%)] | 0 | 17 (18) |
| Discharged to [n (%)] | ||
| Home | 8 (100) | 51 (55) |
| IRF | 0 | 25 (27) |
| SNF | 0 | 3 (3) |
| Home healthcare | 0 | 13 (14) |
F female, ICD-9-CM International classification of diseases, 9th revision, clinical modification, IRF inpatient rehabilitation facility, LITT laser interstitial thermal therapy, M male, NOS not otherwise specified, SD standard deviation, SNF skilled nursing facility
Costs
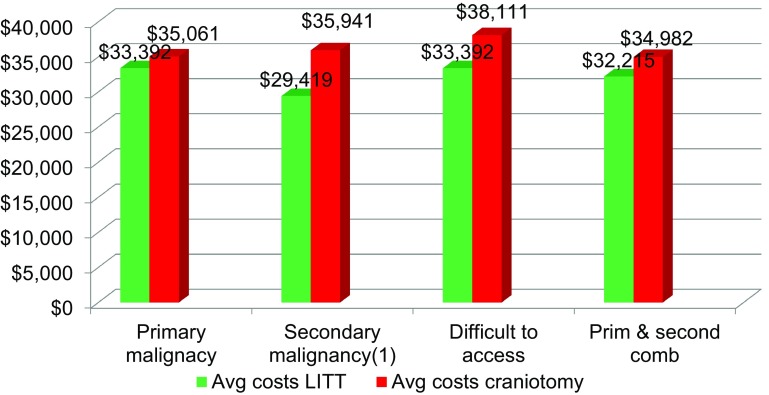
After removing outliers and aggregating patients by diagnosis and treatment method, the costs for treating patients using LITT versus craniotomy were not statistically different for primary (ICD-9-CM 191.0–191.9) plus secondary or metastatic brain tumors (ICD-9-CM 198.3) (see Table 2; Fig. 3). One caveat is that two outliers were removed for the ICD-9-CM 191–191.9 diagnoses with LITT. With the outliers included in these diagnoses the average/standard deviation for costs with LITT were US$40,729 ± 26,624, and with the outliers excluded the costs were US$33,392 ± 12,773.
Table 2.
Cost comparison by tumor type and procedure type
| Tumor typea | Procedure | Average costs (US$)b | Statistical findings | Average age (years) |
|---|---|---|---|---|
| Primary and metastatic (n = 27) | Brain LITT | 32,215 ± 11,891 | MD = –US$2767; 95% CI –7639 to 2105; P = 0.27 | 57.8 ± 11.2 |
| Primary and metastatic (n = 340) | Craniotomy | 34,982 ± 17,903 | 54.5 ± 14.9 | |
| Primary only (n = 19) | Brain LITT | 33,392 ± 13,773 | MD = –US$1669; 95% CI –8192 to 4854; P = 0.62 | 58.71 ± 12c |
| Primary only (n = 248) | Craniotomy | 35,061 ± 16,471 | 51 ± 15.5c | |
| Metastatic only (n = 8) | Brain LITT | 29,419 ± 4965 | MD = −US$6522; 95% CI −11,927 to −1117; P = 0.02 | 59 ± 9.6 |
| Metastatic only (n = 92) | Craniotomy | 35,941 ± 20,401 | 62 ± 10 | |
| DTA (n = 19) | Brain LITT | 33,392 ± 13,773 | MD = −US$4719; 95% CI −12,183 to 2745; P = 0.22 | 57 ± 12d |
| DTA (n = 65) | Craniotomy | 38,111 ± 17,139 | 49 ± 14d |
CI confidence interval, DTA difficult to access, ICD-9-CM International classification of diseases, 9th revision, clinical modification, LITT laser interstitial thermal therapy, MD mean difference
aPrimary tumors: ICD-9-CM diagnosis codes 191.0–191.9 (malignant neoplasm of the brain); secondary tumors: ICD-9-CM diagnosis code 198.3 (secondary malignant neoplasm, brain and spinal cord)
bAverage costs: average costs of procedure and post-acute care, which includes skilled nursing facility, inpatient rehabilitation facility, and/or home care
cSignificant at the P = 0.008 level
dSignificant at the P = 0.01 level
Fig. 3.
Average costs (in US dollars) of acute care by tumor and procedure type, including surgery and postoperative care. CI confidence interval, LITT laser interstitial thermal therapy
The ages of the patients with primary brain tumors were statistically different from the older patients in the LITT group versus craniotomy (58.7 ± 12 years vs. 51 ± 15.5 years, respectively; P = 0.008) (Table 2). In examining the costs in DTA primary tumors (ICD-9-CM 191.0–191.9), the costs for treating patients using LITT versus craniotomy were not statistically different (see Table 2; Fig. 3). The ages of these DTA patients were found to be statistically different (57 ± 12 years for LITT and 49 ± 14 years for craniotomy; P = 0.01). The costs were further separated by site of service (hospital, SNF, IRF, home care, readmissions) (Table 3). In treating metastatic brain cancer (ICD-9-CM 198.3) there was a statistical difference in costs favoring LITT (see Table 2; Fig. 3). However, when outliers were included in the metastatic brain cancer group, the costs were not statistically different: MD = −US$1169; 95% CI −14,757 to 17,095; P = 0.89. The ages of the patients in the metastatic brain cancer groups were not statistically different from each other.
Table 3.
Breakdown of average costs by site of service
| Tumor type | Procedure | Inpatient (US$) | 30-day readmittance (US$) | IRF and/or SNF (US$) | IRF and/or SNF readmittance (US$) | Home care (US$) | Total (US$) |
|---|---|---|---|---|---|---|---|
| Primary only (n = 19) | Brain LITT | 29,386 | 0 | 3847 | 0 | 159 | 33,392 |
| Primary only (n = 248) | Craniotomy | 27,726 | 1636 | 4964 | 466 | 269 | 35,061 |
| Metastatic only (n = 8) | Brain LITT | 29,419 | 0 | 0 | 0 | 0 | 29,419 |
| Metastatic only (n = 92) | Craniotomy | 25,349 | 3402 | 6403 | 358 | 428 | 35,941 |
| DTA (n = 19) | Brain LITT | 29,386 | 0 | 3847 | 0 | 159 | 33,392 |
| DTA (n = 65) | Craniotomy | 28,910 | 3251 | 4874 | 750 | 326 | 38,111 |
DTA difficult to access, IRF inpatient rehabilitation facility, LITT laser interstitial thermal therapy, SNF skilled nursing facility
A sensitivity analysis was performed on the costs for IRF with craniotomy assuming total IRF costs of ± 25% of the amount used in the analysis of US$24,367 (range of US$18,275 to US$30,459). We focused on this cost as it was the highest of the post-hospital site of care services costs. Specifically, there was a statistically significant difference identified earlier favoring LITT in ICD-9-CM 198.3. Using these IRF ranges lowered the overall costs for craniotomy to US$34,353 ± 18,661 (P = 0.06) (IRF at US$18,275 or 75% of the estimated costs used in the model) and increased overall costs for craniotomy to US$37,530 ± 22,147 (P = 0.002) (IRF at US$30,459 or 125% of the estimated costs used in the model).
Although there was a limited sample size within DRG 25 for the LITT cohort (n = 4) and this group was excluded from further subgroup analyses, we did look at average costs between craniotomy and LITT patients. Major complications were experienced by 150 craniotomy patients and brain edema was the complication reported in the majority of patients. The costs for craniotomy procedures were on average US$50,090 ± 26,967. Of these patients, 43% went to a SNF after the procedure. There were no outliers within the craniotomy cohort for DRG 25. Four LITT patients mapped to DRG 25 and there was high variability, with the average costs being US$85,375 ± 33,155.
Incidence of Aftercare and Readmissions
After removing all outliers, the incidence of discharge to other sites of service (IRF, SNF, and home healthcare) was significantly higher with craniotomy when examining all patients treated for primary and metastatic tumors: RR = 0.28; 95% CI 0.11–0.71; P = 0.007 (Fig. 4). These data indicate that patients were more likely to be discharged home with LITT than with craniotomy. For the most expensive site of service, IRF, there was no difference in the incidence of discharge to this care site for both primary and metastatic tumors: RR = 0.80; 95% CI 0.35–1.80; P = 0.59. Further, for the incidence of 30-day readmissions, there was no statistical difference between LITT and craniotomy: RR = 0.12; 95% CI 0.01–1.94; P = 0.14.
Fig. 4.
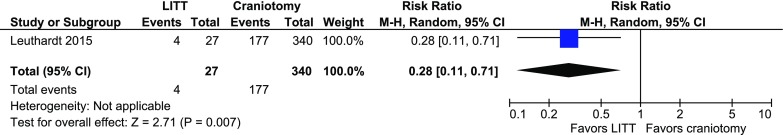
Forest plot: incidence of discharge to other sites of service, including inpatient rehabilitation facility, skilled nursing facility, and home healthcare. CI confidence interval, LITT laser interstitial thermal therapy, M-H Mantel–Haenszel
Twenty-five of 92 patients in the craniotomy group were readmitted for diagnosis of metastatic tumor versus zero of eight patients with LITT. These craniotomy readmissions added an average of US$3400 to the overall cost of care, with craniotomy averaging US$35,941 ± 20,301. Without these readmissions there would have been no statistically significant difference between craniotomy and LITT.
Length of Stay
The average length of stay (ALOS) for all diagnoses included within primary tumor and metastatic tumor was statistically different (P < 0.00001), favoring LITT (Table 4) with an ALOS of 2.33 ± 2.13 days versus an ALOS of 4.71 ± 3.16 days for craniotomy. This statistically meaningful difference remained when diagnoses were separated into the diagnoses of primary tumor and metastatic tumor. In an examination of each diagnosis by treatment type, the average/standard deviation for costs and LOS remained fairly consistent amongst each diagnosis (ICD-9-CM 191–191.9) for craniotomy. There were similar findings with LITT for each diagnosis.
Table 4.
Average length of stay for ICD-9-CM codes 191.0–191.9 and 198.3 (analysis method: inverse variance, mean difference, random effects)
| Primary procedure | Number of patients | ALOS (days) | ALOS (SD) | Findings | Average age (years) ± SD (P = 0.15) |
|---|---|---|---|---|---|
| LITT (17.61) | 27 | 2.33 | 2.13 | MD = −2.38; 95% CI −3.25 to −1.51; P < 0.00001 | 57.8 ± 11.2 |
| Craniotomy (01.59) | 340 | 4.71 | 3.16 | 54.5 ± 14.9 |
ALOS average length of stay, CI confidence interval, ICD-9-CM International classification of diseases, 9th revision, clinical modification, LITT laser interstitial thermal therapy, MD mean difference, SD standard deviation
Post-operative LOS is a risk factor for venous thromboembolism (VTE) [12]. Table 5 shows the number of VTE events along with the number of patients by diagnosis who had an ALOS of >7.7 days and those with an ALOS of <6.1 days. Two of 27 (7%) patients exceeded the 7.7-day ALOS in the LITT group and 43 of 340 (13%) exceeded it in the craniotomy group; this difference was not statistically different (Table 5). It should be noted that one of the four patients with primary/metastatic tumor and craniotomy where VTE was diagnosed (and required a readmission) had an ALOS exceeding 7.7 days.
Table 5.
Length of stay for ICD-9-CM codes 191.0–191.9 and 198.3 for those with a length of stay >7.7 and <6.1 days and the incidence of venous thrombosis post-procedure
| Primary procedure | Number of patients | ALOS (days) (mean ± SD) | Number of patients with an LOS >7.7 days [n (%)] | Number of patients with an LOS <6.1 days [n (%)] | Incidence of VT (in those with LOS >7.7 days) |
|---|---|---|---|---|---|
| LITT (17.61) | 27 | 2.33 ± 2.13 | 2 (7) | 25 (93) | 0 |
| Craniotomy (01.59) | 340 | 4.71 ± 3.16 | 43 (13) | 274 (81) | 1 |
ALOS average length of stay, ICD-9-CM International classification of diseases, 9th revision, clinical modification, LITT laser interstitial thermal therapy, LOS length of stay, SD standard deviation, VT venous thrombosis
Discussion
LITT is a relatively new technology and the majority of the current publications relating to LITT focus on the safety and efficacy of the device. Previous studies using cost modeling showed that LITT is cost effective compared to craniotomy [24]. This study attempted to decipher the early economic picture of LITT using actual cost data from a teaching hospital and aimed to understand patient outcomes as they relate to location of discharge.
In the comparison of LITT and craniotomy procedures performed in areas that were DTA or in areas of eloquence, the peri- and post-procedural costs are significantly less with LITT than with craniotomy for metastatic tumors but are not statistically different in primary tumors. When DTA tumors were examined in aggregate (metastatic plus primary), there was no statistical difference in the overall costs, despite costs being lower by US$4700 in the LITT group versus craniotomy. This non-statistically different finding was likely due to the small numbers of patients in the LITT group (n = 19). The older age of LITT patients may have also adversely affected the costs as increasing age is a risk factor for unfavorable post-operative outcomes (and costs associated with treating them) in patients with brain tumors [25]. Thus, the statistically significant finding of the older age of LITT patients may have increased the costs for this group. Lastly, DTA tumors have been found to have higher complication rates than non-DTA tumors [26–31] and there may be a major difference in the complication rate favoring lower complications with LITT [23]. The incidence of post-procedural discharge to other sites of care was also found to be significantly higher with craniotomy for primary and metastatic brain cancer. This is an important finding in that one might assume that since brain LITT is being utilized in more challenging anatomy (relative to craniotomy), the complication rates, and hence the incidence of post-procedural care, could potentially be higher, including from a cost standpoint; however, this was not the case. The minimally invasive nature of brain LITT (relative to an open craniotomy) likely reduces the collateral damage of the treatment of the tumor and reduces the global stress on the patient, which translates to a more rapid and functional discharge. Complication rates with craniotomy have been noted to be in the 11–21% range in large series of patients [4, 32–34], with most patients experiencing complications likely to require follow-on care. This higher complication rate was found despite intraoperative imaging (MRI and ultrasound) being used with craniotomy to help guide clinicians [4, 23, 32]. Complications seen with craniotomy can also affect any adjunctive therapy that might be needed to improve overall survival [32]. While there was no statistical difference in the incidence of 30-day readmissions between LITT and craniotomy in primary cancers (ICD-9-CM 191-191.9), it should be noted that none (out of 27) occurred in LITT while 44 (out of 340) occurred in craniotomy. In sensitivity analysis it was found that these additional costs had an effect on the statistically significant difference in costs seen between LITT and craniotomy for metastatic disease (in which 17 of the 44 thirty-day readmissions for craniotomy occurred), adding, on average, US$3400/patient for the patients evaluated for this condition. Thus, readmissions appear to be an issue that is more associated with craniotomy.
As can be seen from the data, patients in the LITT group had an ALOS of approximately 2.3 days versus 4.7 days for craniotomy; this difference was statistically different. The incidence of VTE in the diagnoses analyzed for primary and metastatic tumor was four of 340 patients in the craniotomy group versus no patients of 27 in the LITT group. It should be noted that LOS as a risk factor for VTE was minimized with LITT compared to craniotomy. Specifically, as it relates to VTE, three of the VTE patients in the craniotomy group had an LOS of 2–3 days. There are other risk factors that were present (other than an LOS >7.7 days) that may have caused these VTEs, such as a metastatic brain lesion (which one of these patients had) and high-grade glioma (which the other two had) [12]. One of the concerns with VTE in patients who have cancer is not only the additional costs associated with treating it but a significantly higher risk of death within 1 year of the VTE episode (as compared with those who have cancer but do not have a VTE episode) [35]. This risk of death in cancer patients experiencing a VTE may indicate the presence of advanced and aggressive disease, which also requires more aggressive therapies [34]. These likely cannot be initiated until the risk of a further VTE is abated. An advantage of using brain LITT is the ability to ambulate early, which is standard prophylaxis against VTE.
As it relates to how costs were examined, calculated, and evaluated (as identified in Sect. 2), we believe an appropriate methodology was used for doing so that is well-accepted in these types of analyses [36, 37].
These findings have relevance to recently introduced initiatives by Medicare to provide less costly, better quality care using ‘bundles of care.’ The BPCI program recently introduced by Medicare in October 2015 is being evaluated by thousands of providers across the country in various conditions and in various episodes of care [10]. This care entails acute hospital care and the associated aftercare post-discharge (commonly 90 days after hospital discharge). Since there appears to be a shortening of the hospital stay and the potential for less aftercare with LITT in patients with primary and metastatic brain cancers, LITT may hold promise; however, more economic studies are needed to validate these initial findings.
We believe this first look at actual cost data will encourage more research into resource utilization for craniotomy and LITT procedures. This research also supports the findings of prior published work [23]. However, because patients would likely choose a minimally invasive technology over an open procedure, there will probably never be a randomized study prospectively comparing LITT to craniotomy. Additionally, since this is surgery performed at the end of life, a randomized trial versus craniotomy may also be difficult to initiate. While additional research into this area is needed, the preliminary results of this study indicate trends that could guide the development of larger studies.
Limitations
Limitations of this analysis include its retrospective nature and the fact that it is a single-center study. It is unlikely that a prospective randomized trial would be performed on these patients, especially as the use of brain LITT in this institution (Barnes Jewish Hospital) is focused on very complex disease, in which the risk of complications resulting from craniotomy are very high. The fact that this is a single center at which brain LITT has been used regularly for several years demonstrates that good outcomes can result from routine experiential use of a novel technology. A further limitation is that reimbursement values converted to costs using national estimates of cost were used; since this is an estimate for institutions in the St. Louis area, it may not be reflective of the actual costs at other sites. However, Medicare reimbursement (payments) averages 5–7% below allowable Medicare costs for inpatient and outpatient services [38], 11.4% above costs for IRFs [39], and 13.1% above costs for SNFs [40]; thus, these cost estimates in aggregate are likely to be close to actual costs. In addition, since records are not available of the actual LOSs and care delivered in IRFs, SNFs, and home healthcare for these patients, estimates were used. The LOS estimate used in this analysis for SNFs (26 days) is likely close to the actual LOS, based on published data [41]. However, it is important to note that this analysis is not a comparison of efficacy. While LITT may have a cost advantage, assertions cannot be made at this time regarding which modality is more effective in prolonging the life of the patient.
It was assumed that patients discharged home and not receiving additional care (e.g., SNF, rehabilitation, home care) in both LITT and craniotomy did not have complications, but this may not have been the case. However, a recent systematic review and meta-analysis comparing LITT to craniotomy in patients with high-grade tumors in or near areas of eloquence found that there were significantly lower complications and significantly more of the tumor ‘excised’ with LITT [10]. As noted here, these factors relate strongly to overall survival. These LITT complication results also appear more favorable relative to other treatment options for the types of patients studied, such as stereotactic radiosurgery [42].
Another limitation was that the VTE analysis was not adjusted for known confounders of VTE and, therefore, the reported VTE results should be viewed with caution. In addition, the small sample size of the LITT metastatic cancer group and its lower cost findings (vs. similar type craniotomy patients) should be noted and viewed accordingly.
The number of exclusions in the LITT group was 33 patients. As mentioned, these patients were excluded based on the comparison of ‘like patients’ in each group, which may have led to an unintended selection bias.
Another limitation of this analysis is that in calculating the outliers, Grubb’s test was used with the assumption that the data came from a normally distributed population. Although it appears that the data had a normal distribution and that exclusion of outliers was justified, increasing the sample size in the LITT cohort may change the results.
There is heterogeneity in the data based on the use of LITT and craniotomy as the surgical procedure for the lesion location. In this particular practice, LITT is used for deep-seated, DTA (due to the lesion’s location in or near areas of eloquence) lesions. Conversely, lesions that are more superficial in nature, and not adjacent to areas of eloquence, are indicated for surgical incision via open craniotomy. Based on the fact that higher complication rates are commonly seen with deep-seated tumors (and LITT was used more often in these type of patients when taken as a percentage of all patients reported on in this study, i.e., 21/30 = 70% vs. 65/340 = 19%), it was surprising to discover that the incidence and costs for post-care (where these complications would be treated) was actually lower with LITT.
Conclusion
The use of brain LITT in very challenging anatomy demonstrates (via statistical analysis) at worst cost equivalency to craniotomy (with craniotomy being used in cases that are less challenging and potentially less costly) and at best cost savings in metastatic disease. This may be due in part to less care/lower costs for care post-discharge with LITT. These other (non-hospital) care sites cost the system significant additional monies and also delay the opportunity for these patients to go home—a significant consideration for patients with limited life expectancies. Lastly, based on the increase in bundled episodes of care (e.g., coordinated acute and post-discharge care over a period of time such as 90 days paid via a lump sum payment to all providers involved in the care) for many different types of care in the USA, LITT may be a viable alternative for this type of care, potentially saving the healthcare system money while delivering quality care.
Acknowledgements
The authors would like to acknowledge Nissa Mollema, PhD of Monteris Medical for editorial review.
Author contributions
EL collected the data on all patients, reviewed and made significant edits to the first draft of the manuscript, and made final edits to the manuscript. PS collected and analyzed the data and reviewed and made edits to the first draft of the manuscript. AK assisted in the collection of the data on all patients and reviewed and commented on the first draft of the manuscript. JV analyzed the data and provided appropriate statistical analysis and wrote the first draft of the manuscript.
Compliance with Ethical Standards
Funding
This study was funded by an unrestricted grant from Monteris Medical.
Conflict of interest
Eric Leuthardt is a medical consultant for the brain LITT product identified in the article. Jeff Voigt is a reimbursement consultant for the manufacturer of the brain LITT product identified in the article. Peter Sylvester has no conflicts of interest. Albert Kim has no conflicts of interest.
Footnotes
Case mix group 302 for non-traumatic brain injury incurred during neurosurgery procedure. Assumes a length of stay of 12–16 days. Derived from Federal Register. 2014 Aug 6;79(151):45888 [3].
Derived from 2015 Medicare rates in caring for a person post-brain surgery in an SNF.
Medicare daily rate for the 2015 financial year.
Medicare daily rate for the 2015 financial year.
Derived from 2015 Medicare rates in caring for a person post-brain surgery in an SNF.
References
- 1.International classification of diseases, 9th rev, clinical modification. Salt Lake City: Medicode; 1996.
- 2.Agency for Healthcare Research and Quality. HCUPnet. Query run on 22 July 2015. http://hcupnet.ahrq.gov/. Accessed 22 July 2015.
- 3.Inpatient rehabilitation facility prospective payment system for federal fiscal year 2015. Fed Regist. 2014;79(151):45872–45936. [PubMed]
- 4.Gulati S, Jakola AS, Nerland US, Weber C, Solheim O. The risk of getting worse: surgically acquired deficits, perioperative complications, and functional outcomes after primary resection of glioblastoma. World Neurosurg. 2011;76(6):572–579. doi: 10.1016/j.wneu.2011.06.014. [DOI] [PubMed] [Google Scholar]
- 5.Sawaya R, Maarouf H, Schoppa D, Hess K, Wu S, Shi W-M, et al. Neurosurgical outcomes in a modern series of 400 craniotomies for treatment of parenchymal tumors. Neurosurg. 1998;42(5):1044–1055. doi: 10.1097/00006123-199805000-00054. [DOI] [PubMed] [Google Scholar]
- 6.Jackson RJ, Fuller GN, Abi-Said D, Lang FF, Gokaslan ZL, Shi WM, et al. Limitations of stereotactic biopsy in the initial management of gliomas. Neuro-Oncol. 2001;3(3):193–200. doi: 10.1093/neuonc/3.3.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moteris Medical. MRI guided neurosurgical ablation. http://www.monteris.com/our-technology/neuroblate-system/. Accessed 17 Oct 2015.
- 8.Medtronic. MRI-guided laser ablation technology for minimally invasive neurosurgery. http://www.medtronic.com/for-healthcare-professionals/products-therapies/neurological/laser-ablation/visualase/. Accessed 17 Oct 2015.
- 9.Mohammadi AM, Hawasli AH, Rodriguez A, Schroeder JL, Laxton AW, Elson P, et al. The role of laser interstitial thermal therapy in enhancing progression free survival of difficult-to-access high-grad gliomas: a multicenter study. Cancer Med. 2014;3(4):971–979. doi: 10.1002/cam4.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barnett GH, Voigt JD, Alhuwalia MS. A systematic review and meta-analysis of studies examining the use of brain laser interstitial thermal therapy versus craniotomy for the treatment of high-grade tumors in or near areas of eloquence: an examination of the extent of resection and major complication rates associated with each type of surgery. Ster Func Neurosurg. 2016;94:164–173. doi: 10.1159/000446247. [DOI] [PubMed] [Google Scholar]
- 11.CMS.gov. Bundled Payments for Care Improvement (BPCI) initiative: general information. https://innovation.cms.gov/initiatives/bundled-payments/. Accessed 17 July 2016.
- 12.Hawasli AH, Bagade S, Shimony JS, Miller-Thomas M, Leuthardt EC. Magnetic resonance imaging-guided focused laser interstitial thermal therapy for intracranial lesions: single-institution series. Neurosurgery. 2013;73(6):1007–1017. doi: 10.1227/NEU.0000000000000144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith TR, Nanney AD, Lall RR, Graham RB, McClendon J, Jr, Lall RR, et al. Development of venous thromboembolism (VTE) in patients undergoing surgery for brain tumors: results from a single center over a 10 year period. J Clin Neurosci. 2015;22:519–525. doi: 10.1016/j.jocn.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 14.Bureau of Labor Statistics. Consumer Price Index. http://www.bls.gov/cpi/. Accessed 27 July 2015.
- 15.Department of Health and Human Services. Medicare Program; Inpatient Rehabilitation Facility Prospective Payment System for Federal Fiscal Year 2015; Final Rule. Center for Medicare and Medicaid Services. Fed Regist. 2014;79(151):45879. [PubMed]
- 16.Medicare Payment Advisory Committee (MEDPAC). Report to the Congress. Medicare Payment Policy. March 2015. p. 253. http://www.medpac.gov/, http://www.medpac.gov/-documents-/reports. Accessed 17 July 2015.
- 17.Inpatient rehabilitation facility data. http://www.pepperresources.org/Data. Accessed 27 July 2015.
- 18.WPS. Claim calculations/rates. http://www.wpsmedicare.com/j5macparta/departments/audit_reimbursement/arrates.shtml. Accessed 27 July 2015.
- 19.Medicare Payment Advisory Committee (MEDPAC). Report to the Congress. Medicare Payment Policy. March 2015. p. 195. http://www.medpac.gov/, http://www.medpac.gov/-documents-/reports. Accessed 27 July 2015.
- 20.Palmetto GBA. Home Health Prospective Payment System calculator. http://www.palmettogba.com/palmetto/hhapps.nsf/main?Openform&lob=J11HHH&tname=HHA%20PPS%20Claims%20Calculator. Accessed 27 July 2015.
- 21.Medicare Payment Advisory Committee (MEDPAC). Report to the Congress. Medicare Payment Policy. March 2015. http://www.medpac.gov/, http://www.medpac.gov/-documents-/reports. Accessed 27 July 2015.
- 22.GraphPad Software. QuickCalcs. Outlier calculator. http://www.graphpad.com/quickcalcs/grubbs2/. Accessed 28 July 2015.
- 23.Higgins J, Green S. Cochrane handbook for systematic reviews of interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. http://www.cochrane-handbook.org. Accessed 31 July 2015.
- 24.Voigt JD, Barnett GH. The value of using a brain laser interstitial thermal therapy (LITT) system in patients presenting with high grade gliomas where maximal safe resection may not be feasible. Cost Eff Resour Alloc. 2016;14:6. doi: 10.1186/s12962-016-0055-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bekelis K, Kalakoti P, Nanda A, Missios S. A predictive model of unfavorable outcomes after benign intracranial tumor resection. World Neurosurg. 2015;84:82–89. doi: 10.1016/j.wneu.2015.02.032. [DOI] [PubMed] [Google Scholar]
- 26.Lacroix M, Abi-Said D, Fourney DR, Gokaslan AL, Shu W, DeMonte F, et al. A multi-variate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival. J Neurosurg. 2001;95:190–198. doi: 10.3171/jns.2001.95.2.0190. [DOI] [PubMed] [Google Scholar]
- 27.McGirt MJ, Murkeejee D, Chaichana KL, Than KD, Quiones-Hinojosa A. Association of surgically acquired motor and language deficits on overall survival after resection of glioblastoma multiforme. Neurosurgery. 2009;65:463–470. doi: 10.1227/01.NEU.0000349763.42238.E9. [DOI] [PubMed] [Google Scholar]
- 28.Sanai N, Polley MY, McDermott MW, Parsa AT, Berger MS. An extent of resection threshold for newly diagnosed glioblastomas. J Neurosurg. 2011;155:3–8. doi: 10.3171/2011.2.JNS10998. [DOI] [PubMed] [Google Scholar]
- 29.Oszvald Á, Güresir E, Setzer M, Vatter H, Senft C, Seifert MS. An extent of resection threshold for newly diagnosed glioblastomas. J Neurosurg. 2012;116:357–364. doi: 10.3171/2011.8.JNS102114. [DOI] [PubMed] [Google Scholar]
- 30.Orringer D, Lau D, Khatri S, Zamora-Berridi GJ, Zhand K, Wu C, et al. Extent of resection in patients with glioblastoma: limiting factors, perception of resectability, and effect on survival. J Neurosurg. 2012;117:851–859. doi: 10.3171/2012.8.JNS12234. [DOI] [PubMed] [Google Scholar]
- 31.Hardesty DA, Sanai N. The value of glioma resection in the modern neurosurgical era. Front Neurol. 2012;2:140. doi: 10.3389/fneur.2012.00140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kuhnt D, Becker A, Ganslandt O, Bauer M, Buchfelder M, Nimsky C. Correlation of the extent of tumor volume resection and patient survival in surgery of glioblastoma multiforme with high-field intraoperative MRI guidance. Neuro Oncol. 2011;13(12):1339–1348. doi: 10.1093/neuonc/nor133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim SS, McCutcheon IE, Suki D, Weinberg JS, Sawaya R, Lang FF, et al. Awake craniotomy for brain tumors near eloquent cortex: correlation of intraoperative cortical mapping with neurological outcomes in 309 consecutive patients. Neurosurgery. 2009;64:836–846. doi: 10.1227/01.NEU.0000342405.80881.81. [DOI] [PubMed] [Google Scholar]
- 34.Jackson RJ, Fuller GN, Abi-Said D, Lang FF, Gokaslan ZL, Shi WM, et al. Limitation of stereotactic biopsy in the initial-management of gliomas. Neuro Oncol. 2001;3:193–200. doi: 10.1093/neuonc/3.3.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sørensen HT, Mellemkjaer L, Olsen JH, Baron JA. Prognosis of cancers associated with venous thromboembolism. N Engl J Med. 2000;343:1846–1850. doi: 10.1056/NEJM200012213432504. [DOI] [PubMed] [Google Scholar]
- 36.Shwartz M, Young DW, Siegrist R. The ratio of costs to charges: how good a basis for estimating costs? Inquiry. 1995;3294:476–481. [PubMed] [Google Scholar]
- 37.Taira DA, Seto TB, Siiegrist R, Cosgrove R, Berezin R, Cohen DJ. Comparison of analytic approaches for the economic evaluation of new technologies alongside multicenter clinical trials. Am Heart J. 2003;145(3):452–458. doi: 10.1067/mhj.2003.3. [DOI] [PubMed] [Google Scholar]
- 38.MedPAC 2015. Chapter 3: hospital inpatient and outpatient services: assessing payment adequacy and updating payments. http://www.medpac.gov/, http://www.medpac.gov/-documents-/reports. Accessed 2 Oct 2015.
- 39.MedPAC 2015. Chapter 10: inpatient rehabilitation facilities: assessing payment adequacy and updating payments. http://www.medpac.gov/, http://www.medpac.gov/-documents-/reports. Accessed 2 Oct 2015.
- 40.MedPAC 2014. Chapter 8: skilled nursing facilities: assessing payment adequacy and updating payments. http://www.medpac.gov/, http://www.medpac.gov/-documents-/reports. Accessed 2 Oct 2015.
- 41.Greenberg E, Treger I, Ring H. Rehabilitation outcomes in patients with brain tumors and acute stroke: comparative study of inpatient rehabilitation. Am J Phys Med Rehabil. 2006;85(7):568–573. doi: 10.1097/01.phm.0000223218.38152.53. [DOI] [PubMed] [Google Scholar]
- 42.Minniti G, Clarke E, Lanzetta G, Osti MF, Trasimeni G, Bozzzao A, et al. Stereotactic radiosurgery for brain metastases: analysis of outcome and risk of brain radionecrosis. Radiat Oncol. 2011;6:48. doi: 10.1186/1748-717X-6-48. [DOI] [PMC free article] [PubMed] [Google Scholar]