Abstract
Objective:
Soluble suppression of tumorigenicity-2 (sST2), a member of the interleukin 1 receptor family, is increased in mechanical stress conditions and is produced by cardiomyocytes and cardiac fibroblasts. Elevated sST2 level is associated with the prognosis of acute coronary syndrome, pulmonary arterial hypertension, and acute and chronic heart failure (HF). In this study, we aimed to investigate the relationship between sST2 levels and cardiovascular mortality in outpatients with HF.
Methods:
This study used a prospective observational cohort design. A total of 130 consecutive outpatients with HF were prospectively evaluated. Clinical characteristics, laboratory results, cardiovascular risk factors, comorbidities, and medication use were recorded. The patients were followed up for a mean period of 12±4 months for the development of cardiovascular death. They were classified into two groups: those who survived and those who died.
Results:
Mean age of patients was 67±11 years (69% males). After follow-up, 23 of 130 patients (18%) experienced cardiovascular death. sST2 levels were higher among those who died compared with among those who survived [51 (21–162) vs. 27 (9–198) ng/mL, p<0.001]. Optimal cut-off sST2 level to predict cardiovascular mortality was found to be >30 ng/mL with a sensitivity of 87% and a specificity of 67% (AUC =0.808, 95% CI=0.730 to 0.872). sST2 levels were negatively correlated with left ventricular ejection fraction and triglyceride, total cholesterol, LDL cholesterol, and hemoglobin levels and were positively correlated with left atrium size and the presence of right ventricular dilatation. In multiple Cox regression analysis, sST2 level of >30 ng/mL (HR=6.756, p=0.002, 95% CI=1.983–23.018), hemoglobin level (HR=0.705, p<0.001, 95% CI=0.587–0.847), age (HR=1.050, p=0.013, 95% CI=1.010–1.091), and HDL cholesterol level (HR=0.936, p=0.010, 95% CI=0.889–0.984) remained to be associated with an increased risk of mortality.
Conclusion:
sST2 measurement could help risk stratification in outpatients with HF. Moreover, this is the first study describing the impact of sST2 protein in Turkish patients with HF.
Keywords: soluble suppression of tumorigenicity-2, heart failure, cardiovascular mortality
Introduction
Heart failure (HF) leads to frequent hospitalization and death worldwide (1, 2). The mortality and morbidity rates of HF have declined over the decades, but it still remains high despite new drugs and device therapies (3). Determining which patients may develop HF or which patients were followed up and treated with stabilized HF and are at a high risk for decompensation and cardiovascular (CV) death plays a key role in achieving the desired improvement in prognosis. The role of biomarkers in the risk classification of patients with HF is capital (4). Numerous studies have shown that new biomarkers, such as suppression of tumore-genicity 2 (ST2), galectin-3, and copeptin, can be used for risk stratification in patients with HF, along with previously found and useful ones, such as natriuretic peptides and troponin (4–8).
ST2 is a member of the interleukin (IL) 1 receptor family and is defined as a ligand for IL-33. Two main isoforms have been defined: transmembrane or cellular (ST2L) and soluble or circulating (sST2). IL-33 and its receptor are a part of the cardioprotective system that helps to prevent hypertrophy and apoptosis of cardiomyocytes. sST2 binds to IL-33 and inhibits its beneficial effects, resulting in increased concentrations of IL-33 in patients with CV stress and fibrosis (9–13). Recent studies have shown that increased sST2 levels are associated with higher mortality and morbidity in patients with coronary artery disease (CAD) (14), acute (15, 16) and chronic HF (17, 18), and pulmonary arterial hypertension (19). In the 2013 ACC/AHA guideline, the use of sST2 for risk classification in patients with chronic HF followed up on an outpatient basis is weakly recommended as class IIb and evidence level B (20). However, it is not recommended for use in clinical practice for risk estimation according to the ESC guidelines as there is no conclusive evidence (3).
In this study, the association between sST2 level and CV death in outpatients with HF was evaluated. Moreover, this is the first study describing the impact sST2 protein in Turkish patients with HF.
Methods
A total of 150 consecutive outpatients with HF were enrolled. Patients with cancer, sepsis, ongoing systemic inflammatory conditions, pregnancy, autoimmune disease, glucocorticoid therapy, acute myocardial ischemia, and cardiogenic shock were exclu-ded from the study. Finally, a total of 130 outpatients with HF were prospectively evaluated. Laboratory results, clinical characte-ristics, CV risk factors, comorbidities, and medication use were recorded. The patients were followed up for the development of CV death. CV death was defined as sudden death or death due to acute coronary syndrome, HF, or stroke. Following the index visit, CV death-related outcomes during follow-up were assessed by an independent investigator, who gathered and reviewed the patients’ medical records and made necessary phone calls for collecting data. Hypertension was defined as blood pressure of ≥140/90 mm Hg on more than two occasions during office measurements or receiving antihypertensive treatment. Diabetes mellitus was defined as fasting blood glucose level of ≥126 mg/dL or receiving antidiabetic treatment. The presence of CAD was defined as having abnormal stress test results with evidence of ischemia, documented coronary stenosis >50% on a coronary angiogram, or having a clinical history of CAD. The study was performed in accordance with the Declaration of Helsinki for Human Research and was approved by the Institutional Review Board.
Biomarker assays
Samples were collected via the peripheral vein into EDTA-containing tubes, centrifuged immediately, and then stored at –70°C for subsequent analysis. sST2 levels were assessed on baseline samples using a highly sensitive sandwich monoclonal immunoassay (Presage ST2 Assay, Critical Diagnostics, New York, NY), with a lower limit of detection of 2 ng/mL, an upper limit of detection of 200 ng/mL, an intra-assay coefficient of variation of <2.5%, and an interassay coefficient of variation of <4.6% (21).
Echocardiography
All patients underwent echocardiographic examinations with a cardiac ultrasound scanner (VIVID 7, General Electric-Vingmed Ultrasound, Horten, Norway) and a 2.5-MHz transducer in the left lateral decubitus position, with utilization of standard views and measurements by expert echocardiographers, according to guideline recommendations for chamber quantification within a defined protocol (22). Images were obtained using a 2.5-MHz broadband transducer at a depth of 16 cm in the parasternal and apical views (standard long-axis, two-and four-chamber images). LVEF was calculated from the conventional apical two-and four-chamber images using the biplane Simpson’s technique (22). Right ventricular (RV) dimensions were evaluated according to the most recent guidelines (22); hence, midcavity and/or basal RV diameter above and below the reference range in the apical four-chamber view at end-diastole were taken into consideration. The LA size was measured at the end of the ventricular systole by M-mode linear dimension, obtained from the parasternal long-axis view. Mitral, tricuspid, and aortic regurgitations were quantified according to recent guidelines and categorized as severe and non-severe (22). The systolic pulmonary artery pressure (SPAP) was calculated by peak velocity of tricuspid regurgitation and estimated right atrial pressure (23).
Statistical analysis
Continuous variables were presented as mean±SD and were stated median (min-max) in the asset of abnormal distribution. Categorical variables were presented as percentages. Comparisons between groups of patients were made as follows: categorical variables were compared using the chi-square test, normally distributed continuous variables were compared using the independent samples t test, and the Mann–Whitney U test was used if the distribution was skewed. Correlations were evaluated using Spearman’s correlation tests. Univariate regression analysis was used to quantify the association of variables with mortality. sST2 level of >30 ng/mL; age; creatinine, triglyceride, total cholesterol, HDL cholesterol, LDL cholesterol, and hemoglobin levels; LVEF; left atrium size; presence of hypertension; atrial fibrillation (AF); RV dilatation; and digoxin and aldosterone antagonist usage were entered into the multiple Cox regression analysis with forward stepwise method in order to determine the prognostic factors of CV death. All statistical procedures were performed using SPSS software version 14.0 (SPSS Inc., Chicago, IL, USA). A p value of 0.05 was considered as statistically significant.
Results
Mean age of the patients was 67±11 years (69% males, 31% females), with a mean follow-up period of 12±4 months. Mean ejection fraction was 33%±6%, and median sST2 level was 28 (9–198) ng/mL. Among 130 patients, 105 (81%) patients had ischemic HF and 25 (19%) had nonischemic HF. Patients were followed up for a mean period of 12±4 months, and 23 (18%) patients died. Among the 23 patients who died, 14 died due to HF, four due to sudden death, three due to acute coronary syndrome, and two dude to stroke. Among the patients who died, 96% were on antiplatelet therapy, 92% were on beta blockers, 83% were on furosemide, 56% were on RAS blockade, 38% had MRA, and 26% had digital therapy.
The optimal cut-off sST2 level for predicting mortality was >30 ng/mL, with a sensitivity of 87% and a specificity of 67% (AUC=0.808, 95% CI=0.730–0.872, Fig. 1).
Figure 1.
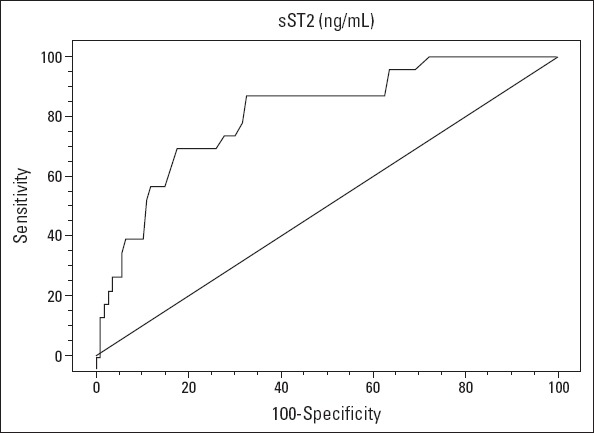
ROC curve for sST2 to predict mortality
The patients were classified into two groups: those who survived and those who died. sST2 levels were higher among those who died compared to among those who survived [51 (21–162) vs. 27 (9–198) ng/mL, p<0.001]. Hence, patients who died had above cut-off sST2 levels at baseline (>30 ng/mL) more frequently than those survived [20 (87%) vs. 35 (33%), p<0.001, Table 1].
Table 1.
Baseline characteristics of study patients
| Patients who survived | Patients who died | P | |
|---|---|---|---|
| n=107, 82% | n=23, 18% | ||
| Baseline characteristics | |||
| Age, years | 66±11 | 72±11 | 0.010 |
| Gender, male/female | 77/30 | 13/10 | 0.228 |
| Hypertension | 58 (54%) | 18 (78%) | 0.059 |
| Diabetes mellitus | 41 (38%) | 8 (35%) | 0.936 |
| Smoking | 13 (12%) | 3 (13%) | 1.000 |
| Atrial fibrillation | 14 (13%) | 7 (30%) | 0.058 |
| Coronary artery disease | 88 (82%) | 17 (6%) | 0.386 |
| COPD | 21 (20%) | 5 (22%) | 0.780 |
| Hyperlipidemia | 69 (65%) | 13 (57%) | 0.631 |
| ICD-CRT implantation | 33 (31%) | 5 (22%) | 0.537 |
| Echocardiography parameters | |||
| Left ventricular ejection fraction, % | 33±6 | 32±7 | 0.396 |
| Left ventricular diastolic diameter, cm | 5.5±0.7 | 5.7±0.8 | 0.279 |
| Severe mitral regurgitation | 6 (6%) | 4 (17%) | 0.076 |
| Severe aortic regurgitation | 1 (1%) | 0 (0%) | 1.000 |
| Left atrium size, cm | 4.2±0.6 | 4.6±0.5 | 0.002 |
| Severe tricuspid regurgitation | 9 (9%) | 5 (22%) | 0.074 |
| SPAP, mm Hg | 41±12 | 45±12 | 0.307 |
| Right ventricular dilatation | 31 (29%) | 12 (52%) | 0.057 |
| Laboratory analysis | |||
| sST2, ng/mL | 27 (9-198) | 51 (21-162) | <0.001 |
| sST2 >30 ng/mL | 35 (33%) | 20 (87%) | <0.001 |
| Fasting glucose, mg/dL | 138±66 | 147±63 | 0.554 |
| Creatinine, mg/dL | 1.1 (0.6-3.6) | 1.5 (0.7-5.1) | 0.049 |
| Alanine aminotransferase, IU/L | 29 (7-218) | 34 (5-112) | 0.475 |
| Triglyceride, mg/dL | 143±96 | 87±26 | <0.001 |
| Total cholesterol, mg/dL | 167±45 | 132±40 | 0.001 |
| HDL cholesterol, mg/dL | 42±10 | 36±12 | 0.011 |
| LDL cholesterol, mg/dL | 118±38 | 91±32 | 0.002 |
| Hemoglobin, gr/dL | 14±2 | 11±2 | <0.001 |
| Platelet counts, 103 | 218±59 | 217±63 | 0.745 |
| White blood cell | 8.2±2 | 7.9±2 | 0.595 |
| Medication | |||
| Antiplatelet agent | 103 (96%) | 22 (96%) | 1.000 |
| ACE inhibitors/ARB | 80 (74%) | 13 (56%) | 0.132 |
| Beta blocker | 99 (93%) | 21 (92%) | 1.000 |
| Digoxin | 11 (10%) | 6 (26%) | 0.080 |
| Furosemide | 71 (66%) | 19 (83%) | 0.199 |
| Aldosterone antagonist | 68 (64%) | 8 (38%) | 0.021 |
| Statin | 67 (63%) | 13 (57%) | 0.757 |
ACE - angiotensin converting enzyme; ARB - angiotensin receptor blocker; COPD - chronic obstructive pulmonary disease; CRT - cardiac resynchronization therapy; HDL - highdensity lipoprotein; ICD - intracardiac defibrillator; LDL - low-density lipoprotein; SPAPsystolic pulmonary artery pressure
A comparison of the baseline characteristics of the patients is presented in Table 1. The patients who died were older than those who survived. Aldosterone antagonist usage was more frequent among patients with survived HF relative to patients with died HF. Although statistically insignificant, the presence of hypertension (p=0.059), AF (p=0.058), and severe mitral and tricuspid regurgitation (p=0.076, p=0.074, respectively) was more frequent in patients who died compared with those who survived. Left atrium size was higher and hemoglobin and all cholesterol levels were lower in patients who died than in those who survived. There was no significant difference between the two groups in baseline characteristics and other laboratory parameters (Table 1).
In patients with HF, sST2 levels were negatively correlated with left ventricular ejection fraction and triglyceride, total cholesterol, LDL cholesterol, and hemoglobin levels and positively correlated with left atrium size and the presence of RV dilatation. There was no significant correlation between sST2 level and other laboratory findings (p>0.05, Table 2).
Table 2.
Spearman’s correlation coefficients for sST2 levels
| sST2 | P | |
|---|---|---|
| LVEF, % | -0.258 | 0.003 |
| Left atrium size, cm | 0.264 | 0.002 |
| LV diastolic diameter, cm | 0.268 | 0.002 |
| Right ventricular dilatation | 0.218 | 0.013 |
| Creatinine, mg/dL | 0.215 | 0.014 |
| Triglyceride, mg/dL | -0.379 | <0.001 |
| Total cholesterol, mg/dL | - 0.264 | 0.002 |
| LDL cholesterol, mg/dL | 0.275 | 0.002 |
| Hemoglobin, gr/dL | -0.370 | <0.001 |
LVEF - left ventricular ejection fraction
Results of the univariate and multivariate Cox proportional hazards analyses for mortality are listed in Table 3. sST2 level of >30 ng/mL; hemoglobin, total cholesterol, creatinine, triglyce-ride, LDL cholesterol, and HDL cholesterol levels; age; left atrium size; presence of hypertension, AF, and RV dilatation; and digoxin and aldosterone antagonist usage were found to have prognostic significance in univariate analysis. In multiple Cox regression analysis with forward stepwise method, sST2 level of >30 ng/mL (HR=6.756, p=0.002, 95% CI=1.983–23.018), hemoglobin level (HR=0.705, p<0.001, 95% CI=0.587–0.847), age (HR=1.050, p=0.013, 95% CI=1.010–1.091), and HDL cholesterol (HR=0.936, p=0.010, 95% CI=0.889–0.984) remained to be associated with an increased risk of CV death after adjustment for variables found to be statistically significant in univariate analysis and correlated with sST2 level (Table 3).
Table 3.
Univariate and multiple analyses of mortality
| Univariate | Multiple | |||||
|---|---|---|---|---|---|---|
| Variable | B | Exp beta (HR) | P | B | Exp beta (HR) | P |
| sST2 >30 ng/mL | 2.618 | 13.714 | <0.001 | 1.910 | 6.756 | 0.002 |
| Hemoglobin, g/dL | -0.543 | 0.581 | <0.001 | -0.350 | 0.705 | <0.001 |
| Total cholesterol, mg/dL | -0.020 | 0.980 | 0.002 | |||
| Age, years | 0.055 | 1.057 | 0.012 | 0.049 | 1.050 | 0.013 |
| Hypertension | 1.112 | 3.041 | 0.040 | |||
| Atrial fibrillation | 1.067 | 2.906 | 0.047 | |||
| Left atrium size, cm | 1.215 | 3.370 | 0.004 | |||
| Right ventricular dilatation | 0.984 | 2.674 | 0.036 | |||
| Creatinine, mg/dL | 0.833 | 2.300 | 0.020 | |||
| Triglyceride, mg/dL | -0.016 | 0.984 | 0.006 | |||
| HDL cholesterol, mg/dL | -0.060 | 0.942 | 0.015 | -0.067 | 0.936 | 0.010 |
| LDL cholesterol, mg/dL | -0.024 | 0.976 | 0.003 | |||
| Digoxin usage | 1.125 | 3.080 | 0.049 | |||
| Aldosterone antagonist usage | -1.185 | 0.306 | 0.014 | |||
| LV diastolic diameter, cm | 0.331 | 1.392 | 0.278 | |||
| LVEF, % | -0.032 | 0.696 | 0.393 | |||
All the variables from Table 1 were examined, and only those significant at a P<0.1 and those with a correlated sST2 level are shown in univariate analysis. The multiple Cox regression analysis included all univariate predictors and those correlated with sST2 levels. B - beta coefficient; HDL - high density lipoprotein; LDL - low density lipoprotein; LV - left ventricular; LVEF - left ventricular ejection fractions; HR - hazard ratio; Abbreviations in Table 1
Kaplan–Meier analysis yielded diverging survival curves for two previously defined subgroups of sST2 with a threshold of 30 ng/mL (p<0.001, Fig. 2).
Figure 2.
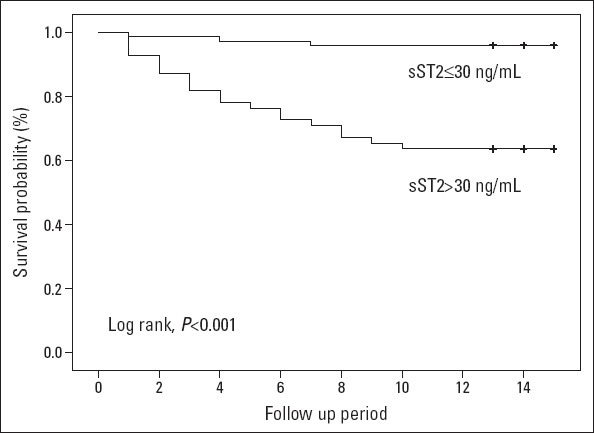
Kaplan–Meier curve for mortality
Discussion
The results of this study showed that elevated sST2 levels were independently associated with higher CV death rates in outpatients with HF. This study also showed that higher sST2 levels were associated with poor left and right ventricular function, poor kidney function, and anemia.
sST2 level is increased in mechanical stress conditions and is produced by cardiomyocytes and cardiac fibroblasts. In addition, sST2 levels also increase in collagen tissue diseases, cancer, sepsis, and ulcerative colitis, indicating that it is also associated with inflammation and immunological processes (9–13). Sabatine et al. have reported in their study published in 2008 that high baseline sST2 levels in STEMI patients are associated with CV death and HF (24). First, in the PRIDE study, patients with acute dyspnea were examined for sST2 levels, and it was observed that patients with acute decompensated HF had higher sST2 levels than those without HF. In addition, high sST2 levels with or without HF were associated with higher 1-year mortality (5). In the subgroup analysis of the PRIDE study (15), only patients diagnosed with HF were evaluated and an independent relationship with mortality was also determined. It has also been shown that sST2 levels in patients with HF are positively correlated with left heart and kidney functions and with NYHA class and levels of NT-pro BNP. However, there was no correlation between sST2 level and age and presence of AF and CAD. In this study, independent correlation with 1-year mortality was also found. In addition, negative correlation with LVEF, positive correlation with creatinine levels, and no correlation with age, and presence of AF and CAD were found. In another subgroup analysis (6), in which the echocardiography parameters of this study were examined in detail, it was observed that sST2 levels predicted 4-year mortality and that sST2 levels were related to LVEF, LV diastolic diameter, and RV systolic pressure. Moreover, in our study, it was determined that sST2 levels were similarly correlated with LV diastolic diameter and RV diameter and were not correlated with SPAP. Similar to previous studies, increased sST2 levels were found to be associated with short-and long-term mortalities, and correlations between sST2 levels and hemodynamic and biochemical parameters were also found in subsequent studies in patients with chronic HF (25–27). Felker et al. (18) have shown that sST2 levels are associated with functional capacity and poor outcomes in stable outpatients with HF. Unlike this and previous studies, they found that sST2 levels were correlated with age, sex, and ischemic etiology but not with LVEF. However, it is important to note that HFPEF patients were not included in their study. Finally, sST2 levels were studied in PAH patients and were documented to be associated with disease severity and clinical deterioration (19).
It is known that HF is associated with oxidative stress and neurohormonal activation. We demonstrated that sST2 levels were correlated with poor hemodynamic parameters, such as low LVEF, higher LV diastolic and left atrial diameters, higher creatinine levels, and lower cholesterol and hemoglobin levels. sST2 levels were correlated with left ventricular filling pressure in patients with HF. Moreover, sST2 was also found to be related to RV dilatation. Hence, we think that sST2 levels seem to reflect increasing severity of HF. Thereofore, this association of high sST2 levels with CV death suggests that CV stress, fibrosis, and inflammation may play a pathophysiological role in determining patients at a higher risk.
Study limitations
There are some limitations of the current study. Our study was limited by its monocentric nature; hence, the findings cannot be generalized to the overall population of patients with HF. The most important limitation was the relatively small sample size. Relatively small sample size might have influenced larger 95% CI for hazard ratios of sST2 levels. It might have been better to combine measurement of natriuretic peptides and other biomarkers, such as troponins. However, because of availability of echocardiography, natriuretic peptides are rarely utilized in our center (only in the emergency department). Finally, RV functions were assessed using RV size, SPAP, and tricuspid valve insufficiency, and no objective parameters such as tricuspid annular plane systolic excursion and RV fractional area change were used.
Conclusion
In the presence of the other clinical and laboratory para-meters, sST2 levels were shown to be an independent predictor of mortality in outpatients with HF. Furthermore, because sST2 levels have a high sensitivity of 87%, it is suggested that this level could be helpful in deciding the “rule out for mortality analysis.”
Footnotes
Conflict of interest: None declared.
Peer-review: Externally peer-reviewed.
Authorship contributions: Concept – İ.G., O.Y., A.Z., A.Zorlu., M.B.Y.; Design – İ.G., A.Z., A.Zorlu., M.B.Y.; Supervision – İ.G., A.Zorlu., M.B.Y.; Fundings – O.Y., Ö.D., H.Y.; Materials – O.Y., Ö.D., A.Zorlu.; Data collection and/or Processing – A.Z., Ö.D., H.Y., A. Zorlu.; Analysis &/or interpretation – İ.G., A.Zorlu., M.B.Y.; Literature search – İ.G., A.Zorlu., M.B.Y.; Writing – İ.G., A.Z., A.Zorlu.; Critical review – İ.G., H.Y., A.Zorlu., M.B.Y.
References
- 1.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Executive summary:heart disease and stroke statistics-2012 update:a report from the American Heart Association. Circulation. 2012;125:188–97. doi: 10.1161/CIR.0b013e3182456d46. [DOI] [PubMed] [Google Scholar]
- 2.McCullough PA, Philbin EF, Spertus JA, Kaatz S, Sandberg KR, Weaver WD. Resource Utilization Among Congestive Heart Failure (REACH) Study. Confirmation of a heart failure epidemic:findings from the Resource Utilization Among Congestive Heart Failure (REACH) study. J Am Coll Cardiol. 2002;39:60–9. doi: 10.1016/s0735-1097(01)01700-4. [DOI] [PubMed] [Google Scholar]
- 3.Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. Authors/Task Force Members. Document Reviewers. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure:The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016;18:891–975. doi: 10.1002/ejhf.592. [DOI] [PubMed] [Google Scholar]
- 4.Braunwald E. Biomarkers in heart failure. N Engl J Med. 2008;358:2148–59. doi: 10.1056/NEJMra0800239. [DOI] [PubMed] [Google Scholar]
- 5.Januzzi JL, Jr, Peacock WF, Maisel AS, Chae CU, Jesse RL, Baggish AL, et al. Measurement of the interleukin family member ST2 in patients with acute dyspnea:results from the PRIDE (Pro-Brain Natriuretic Peptide Investigation of Dyspnea in the Emergency Department) Study. J Am Coll Cardiol. 2007;50:607–13. doi: 10.1016/j.jacc.2007.05.014. [DOI] [PubMed] [Google Scholar]
- 6.Shah R, Chen-Tournoux A, Picard M, van Kimmenade R, Januzzi JL. Serum levels of the interleukin-1 receptor family member ST2, cardiac structure and function, and long-term mortality in patients with acute dyspnea. Circ Heart Fail. 2009;2:311–9. doi: 10.1161/CIRCHEARTFAILURE.108.833707. [DOI] [PubMed] [Google Scholar]
- 7.Felker GM, Fiuzat M, Shaw LK, Clare R, Whellan DJ, Bettari L, et al. Galectin-3 in ambulatory patients with heart failure:results from the HF-ACTION study. Circ Heart Fail. 2012;5:72–8. doi: 10.1161/CIRCHEARTFAILURE.111.963637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maisel A, Xue Y, Shah K, Mueller C, Nowak R, Peacock WF, et al. Increased 90- day mortality in patients with acute heart failure with elevated copeptin:secondary results from the Biomarkers in Acute Heart Failure (BACH) study. Circ Heart Fail. 2011;4:613–20. doi: 10.1161/CIRCHEARTFAILURE.110.960096. [DOI] [PubMed] [Google Scholar]
- 9.Liew FY, Pitman NI, McInnes IB. Disease-associated functions of IL-33:the new kid in the IL-1 family. Nat Rev Immunol. 2010;10:103–10. doi: 10.1038/nri2692. [DOI] [PubMed] [Google Scholar]
- 10.Villarreal DO, Weiner DB. Interleukin 33:a switch-hitting cytokine. Curr Opin Immunol. 2014;28:102–6. doi: 10.1016/j.coi.2014.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mueller T, Jaffe AS. Soluble ST2–analytical considerations. Am J Cardiol. 2015;115:8–21. doi: 10.1016/j.amjcard.2015.01.035. [DOI] [PubMed] [Google Scholar]
- 12.Dieplinger B, Mueller T. Soluble ST2 in heart failure. Clin Chim Acta. 2015;443:57–70. doi: 10.1016/j.cca.2014.09.021. [DOI] [PubMed] [Google Scholar]
- 13.Seki K, Sanada S, Kudinova AY, Steinhauser ML, Handa V, Gannon J, et al. Interleukin-33 prevents apoptosis and improves survival after experimental myocardial infarction through ST2 signaling. Circ Heart Fail. 2009;2:684–91. doi: 10.1161/CIRCHEARTFAILURE.109.873240. [DOI] [PubMed] [Google Scholar]
- 14.Shimpo M, Morrow DA, Weinberg EO, Sabatine MS, Murphy SA, Antman EM, et al. Serum levels of the interleukin-1 receptor family member ST2 predict mortality and clinical outcome in acute myocardial infarction. Circulation. 2004;109:2186–90. doi: 10.1161/01.CIR.0000127958.21003.5A. [DOI] [PubMed] [Google Scholar]
- 15.Mueller T, Dieplinger B, Gegenhuber A, Poelz W, Pacher R, Haltmayer M. Increased plasma concentrations of soluble ST2 are predictive for 1-year mortality in patients with acute destabilized heart failure. Clin Chem. 2008;54:752–6. doi: 10.1373/clinchem.2007.096560. [DOI] [PubMed] [Google Scholar]
- 16.Rehman S, Mueller T, JL J. Characteristics of the novel interleukin family biomarker ST2 in patients with acute heart failure. J Am Coll Cardiol. 2008;52:1458–65. doi: 10.1016/j.jacc.2008.07.042. [DOI] [PubMed] [Google Scholar]
- 17.Ky B, French B, Mccloskey K, Rame JE, McIntosh E, Shahi P, et al. High sensitivity ST2 for prediction of adverse outcomes in chronic heart failure. Circ Heart Fail. 2011;4:180–7. doi: 10.1161/CIRCHEARTFAILURE.110.958223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Felker GM, Fiuzat M, Thompson V, Shaw LK, Neely ML, Adams KF, et al. Soluble ST2 in ambulatory patients with heart failure:Association with functional capacity and long-term outcomes. Circ Heart Fail. 2013;6:1172–9. doi: 10.1161/CIRCHEARTFAILURE.113.000207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zheng YG, Yang T, He JG, Chen G, Liu ZH, Xiong CM, et al. Plasma soluble ST2 levels correlate with disease severity and predict clinical worsening in patients with pulmonary arterial hypertension. Clin Cardiol. 2014;37:365–70. doi: 10.1002/clc.22262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure:a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62:147–239. doi: 10.1016/j.jacc.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 21.Lu J, Snider JV, Grenache DG. Establishment of reference intervals for soluble ST2 from a United States population. Clin Chim Acta. 2010;411:1825–6. doi: 10.1016/j.cca.2010.07.014. [DOI] [PubMed] [Google Scholar]
- 22.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. American Society of Echocardiography's Nomenclature and Standards Committee;Task Force on Chamber Quantification;American College of Cardiology Echocardiography Committee;American Heart Association;European Association of Echocardiography, European Society of Cardiology. Recommendations for chamber quantification. Eur J Echocardiogr. 2006;7:79–108. doi: 10.1016/j.euje.2005.12.014. [DOI] [PubMed] [Google Scholar]
- 23.Yock PG, Popp RL. Noninvasive estimation of right ventricular systolic pressure by Doppler ultrasound in patients with tricuspid regurgitation. Circulation. 1984;70:657–62. doi: 10.1161/01.cir.70.4.657. [DOI] [PubMed] [Google Scholar]
- 24.Sabatine MS, Morrow DA, Higgins LJ, MacGillivray C, Guo W, Bode C, et al. Complementary roles for biomarkers of biomechanical strain ST2 and N-terminal prohormone B-type natriuretic peptide in patients with ST-elevation myocardial infarction. Circulation. 2008;117:1936–44. doi: 10.1161/CIRCULATIONAHA.107.728022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bayes-Genis A, Zhang Y, Ky B. ST2 and patient prognosis in chronic heart failure. Am J Cardiol. 2015;115:64B–9B. doi: 10.1016/j.amjcard.2015.01.043. [DOI] [PubMed] [Google Scholar]
- 26.Weinberg EO, Shimpo M, Hurwitz S, Tominaga S, Rouleau JL, Lee RT. Identification of serum soluble ST2 receptor as a novel heart failure biomarker. Circulation. 2003;107:721–6. doi: 10.1161/01.cir.0000047274.66749.fe. [DOI] [PubMed] [Google Scholar]
- 27.Bayes-Genis A, De Antonio M, Galan A, Sanz H, Urritia A, Cabanes R, et al. Combined use of high-sensitivity ST2 and NTproBNP to improve the prediction of death in heart failure. Eur J Heart Fail. 2012;14:32–8. doi: 10.1093/eurjhf/hfr156. [DOI] [PubMed] [Google Scholar]


