Abstract
Obesity is a global problem reaching epidemic proportions and can be explained by unhealthy eating and sedentary lifestyles. Understanding the psychological processes underlying unhealthy eating behaviour is crucial for the development of effective obesity prevention programmes. Dual-process models implicate the interplay between impaired cognitive control and enhanced automatic responsivity to rewarding food cues as key risk factors. The current study assessed the influence of four different components of trait impulsivity (reflecting impaired cognitive control) and automatic approach bias for food (reflecting automatic responsivity to food) on uncontrolled eating in a large sample (N = 504) of young adolescents. Of the four impulsivity factors, negative urgency was found to be the strongest predictor of uncontrolled eating. Interestingly, we found that lack of premeditation was a key risk factor for uncontrolled eating, but only when approach bias for food was high, supporting a dual-process model. Lack of perseverance showed a similar interactive pattern to a lesser degree and sensation-seeking did not predict uncontrolled eating. Together, our results show that distinct components of trait impulsivity are differentially associated with uncontrolled eating behaviour in adolescents, and that automatic processing of food cues may be an important factor in modulating this relationship.
Keywords: Uncontrolled-eating, Impulsivity, Food-bias, Dual-process, Adolescents, Obesity
Worldwide obesity is reaching epidemic proportions and has doubled since 1980. In 2014, 39% of adults were classified as being overweight and 13% as obese (World Health Organization (WHO), 2016). The future does not look any brighter, as current estimates indicate that 41 million children worldwide are overweight or obese (WHO, 2016). Within the UK, for instance, prevalence is steadily increasing with official figures for England and Wales suggesting that 20% of children are obese (National Child Measurement Programme, 2014/15) and if trends continue, it has been forecast to increase to 50% by the year 2030 (Wang, McPherson, Marsh, Gortmaker, & Brown, 2011). The WHO state that the fundamental causes of obesity are twofold: an increasing degree of sedentary lifestyles in combination with an increase in the consumption of a diet that contains too much sugar, fat and salt. The current western environment is especially obesogenic with the easy availability of high calorie appetitive food and the lack of physical activity (Berthoud, 2007).
Given the negative consequences of obesity on public health it is becoming increasingly important to understand the psychological processes that underlie the tendency to overeat unhealthy (high sugar, high fat) foods, especially in obesogenic environments. Uncontrolled eating refers to an eating style that is characterised by the over consumption of unhealthy food in response to external food cues – sometimes called external eating – and has been related to obesity and high calorie food consumption in adult populations (Cornelis et al., 2014, Karlsson et al., 2000, de Lauzon et al., 2004). Two psychological processes have been described in the literature, which may account for individual differences in uncontrolled eating. The first is (reduced) cognitive control, such as impulsive personality style, which has been found to be a key predictor of obesity in children (Thamotharan, Lange, Zale, Huffhines, & Fields, 2013). The second is automatic action tendencies to approach appetitive food cues in the environment, which is thought to be modulated by reward networks in the brain and be inflated in certain individuals, such as those at risk of obesity (Havermans et al., 2011, Mogg et al., 2012). The aim of the current study was to investigate the interaction between these two psychological processes in a large sample of adolescents, which is an under-researched population in this field, despite the growing prevalence of obesity in this age group.
Cognitive control refers to a collection of processes that enable individuals to act in a goal-directed manner, including inhibition, interference control, working memory and cognitive flexibility (Diamond, 2013). Disinhibition – or the propensity to act impulsively – has been implicated as a key risk factor in obesity with a recent meta-analysis reporting a moderate effect size in the relationship between general impulsivity and obesity in children (Thamotharan et al., 2013). However, impulsivity is itself a multi-factorial concept and it is not entirely clear which impulsivity factors are most associated with unhealthy eating. The current study focused on four factors of trait impulsivity that have been applied to obesity (Mobbs, Crepin, Thiery, Golay, & Van der Linden, 2010). The UPPS model of impulsivity (Whiteside & Lynam, 2001) differentiates between negative urgency, lack of perseverance, lack of premeditation and sensation-seeking. It has been hypothesised that the first three factors, related to self-control, are likely to predict obesity, while the last factor, sensation-seeking, is more of a motivational factor unrelated to obesity (Mobbs et al., 2010). This is supported in the literature, as negative urgency and lack of perseverance are the factors most often related to obesity (Becker et al., 2016, Delgado-Rico et al., 2012, Mobbs et al., 2010, Murphy et al., 2014). The UPPS model was later amended to include a fifth factor, namely positive urgency (Lynam, Smith, Cyders, Fischer, & Whiteside, 2007), which is similar to negative urgency as it measures emotion-driven impulsivity. However, for the current study we were only interested in assessing negative urgency based on previous research indicating a strong association between this factor and overeating, as well as controversy over whether positive and negative urgency explain overlapping pathways to psychopathology (Berg, Latzman, Bliwise, & Lilienfeld, 2015). We expected that negative urgency – describing impulsive behaviour in response to negative affective states – would most strongly predict uncontrolled eating, that lack of perseverance – describing a difficulty with focus and completing tasks – would moderately predict uncontrolled eating, that lack of premeditation – describing a general deficit in impulse control and failure to evaluate future consequences – would moderately predict uncontrolled eating, and that sensation-seeking – describing a motivation to engage in thrilling activities – would be unrelated to uncontrolled eating.
Automatic action-tendencies to food describe a natural cognitive mechanism to approach appetitive food cues in the environment, which are likely to be inflated when the salience of food is increased, such as when metabolic hunger levels are high in healthy populations (Seibt, Häfner, & Deutsch, 2007), or in the case of obesity when the overall rewarding properties of food are thought to be amplified (He et al., 2014). We measured approach bias for food with a Stimulus-Response Compatibility (SRC) task, in which participants are instructed to move a manikin towards or away from different stimulus features, e.g. in one block they might be instructed to approach food stimuli and avoid non-food stimuli and in another block would be instructed to avoid food stimuli and approach non-food stimuli. Faster reaction-times (RTs) in the approach food block compared to the avoid food block indicates greater reward sensitivity and an approach bias for food. Approach bias measured with this task has been shown to predict high levels of external eating (Brignell, Griffiths, Bradley, & Mogg, 2009) and obesity (Havermans et al., 2011, Mogg et al., 2012). However, it is considered an under-researched mechanism in comparison to other food-related cognitive biases, such as attention bias and implicit association (Brignell et al., 2009, Kemps and Tiggemann, 2015, Kemps et al., 2013, Popien et al., 2015, Schmitz et al., 2014). We were interested in using the SRC task, in order to assess the interaction between action-tendencies towards rewarding food cues and impulsive personality, to gain a deeper understanding of uncontrolled eating. Another way to assess action-tendencies is the approach-avoidance joystick task (AAT), which asks participants to push or pull a joystick towards or away from themselves in response to different stimulus features. In most versions of the AAT, participants respond to task-irrelevant features, e.g. the tilt of an image, rather than the content, and can therefore be said to measure implicit action-tendencies. At the moment it is unclear if implicit or explicit action-tendencies are more robust in predicting eating behaviour. For the current study we used an explicit SRC task for two reasons. Firstly, a recent study showed that explicit (rather than implicit) action tendencies to alcohol cues were stronger predictors of drinking behaviour (Kersbergen, Woud, & Field, 2015). Furthermore, as the data was collected in a school group testing setting, it was not feasible to use a joystick based task.
Dual-process models of overeating propose that the rewarding properties of food cues in the environment hyper-activate bottom-up automatic approach processes at the expense of top-down cognitive control processes (He et al., 2014, Kakoschke et al., 2015, Kemps and Tiggemann, 2015, Lawrence et al., 2012, Volkow et al., 2008, Wiers et al., 2007). According to this model, a strong approach bias for food coupled with a high degree of impulsivity would be a risky combination predicting unhealthy eating and obesity. This hypothesis is supported by a recent study in healthy adults, which found that individuals displaying both poor inhibitory control and a strong approach bias for food consumed the most high calorie snack food on a bogus taste-test. While the two processes failed to predict consumption independently, it was their interaction that was important (Kakoschke et al., 2015). More research is needed to investigate the implications of this risky combination on overeating, especially in adolescent populations. Dual-process models have been more widely applied in the addiction literature, and several studies have shown that individuals who are less able to exercise cognitive control over their impulses are more likely to develop problems with drugs and alcohol (Bechara, 2005, Houben and Wiers, 2009, Wiers et al., 2007). Dual process models are likely to apply to overeating, as unhealthy food activates the same neural substrates as other addictive substances, e.g. mesolimbic dopamine pathways (Volkow et al., 2008).
The current study is a cross-sectional investigation into automatic and controlled processes predicting uncontrolled eating in a large sample of young adolescents. The aim of the study was to advance current understanding of different trait impulsivity factors and how they relate to uncontrolled eating, as well as investigating whether approach bias for food is an important modulating factor. We tested four statistical models investigating the independent effects of four impulsivity traits on uncontrolled eating, as well as how each of these traits interacted with approach bias for food. We hypothesised that negative urgency would be the strongest predictor of higher uncontrolled eating, that lack of premeditation and lack of perseverance would moderately predict uncontrolled eating, and that sensation-seeking would not predict uncontrolled eating. We also hypothesised that approach bias for food would moderate these relationships, as individuals with a strong approach bias for food coupled with high impulsivity would report the highest levels of uncontrolled eating, as predicted by a dual-process model.
1. Method
1.1. Participants
Participants were 504 young adolescents taking part in a wider study on the development of cognitive biases – the CogBIAS longitudinal study – of which data from Wave 1 was completed in July 2016. Adolescents from years 7–9 (Age M = 12.91, SD = 0.87) were recruited from schools in the South England area (10 cohorts in total). Informed consent was received from parents and assent was received from children. Fifty-five percent of the sample was female. Body-mass-index (BMI: kg/m2) ranged from 13.91 to 36.72 and most of the participants measured a healthy weight (BMI M = 19.91, SD = 3.31), with only 11% measured as obese (using a crude cut-off of BMI ≥ 24 based on the Centres for Disease Control and Prevention recommendation for a girl aged 13).
1.2. Measures
Three-Factor Eating Questionnaire revised (TFEQ). The TFEQ (Karlsson et al., 2000) is an 18-item assessment of three separate eating styles – uncontrolled eating, emotional eating and cognitive restraint. Uncontrolled eating refers to extreme appetite and eating in response to external food cues, which was assessed with 9-items, including 7-items concerned with trait hunger and external eating (e.g. “When I see a real delicacy I often get so hungry that I have to eat it right away”), as well as 2-items on frequency of feeling hungry and frequency of binge eating episodes. Emotional eating was assessed with 3-items (e.g. “When I feel anxious I find myself eating”). Cognitive restraint was assessed with 6-items (e.g. “I do not eat some foods because they make me fat”). Most items from the questionnaire are rated on a 4-point scale, with high numbers reflecting unhealthy eating. Internal reliabilities were high for uncontrolled eating (Cronbach's α = 0.88), emotional eating (Cronbach's α = 0.87) and cognitive restraint (Cronbach's α = 0.80), which is very similar to previous research in a large adult cohort (Cornelis et al., 2014) and a study of older adolescents (de Lauzon et al., 2004), supporting its use in young adolescents. Twelve participants did not complete this questionnaire, resulting in missing data.
UPPS-R-Child version. The UPPS-R-C (Zapolski, Stairs, Settles, Combs, & Smith, 2010) is a 32-item measure of four impulsivity factors – (negative) urgency, lack of premeditation, lack of perseverance and sensation-seeking. Negative urgency refers to the tendency to act impulsively in response to negative emotional states (e.g. “When I feel bad, I often do things I later regret in order to feel better now”). Lack of premeditation refers to a difficulty in controlling impulses (e.g. “I tend to blurt things out without thinking”). Lack of perseverance refers to a difficulty in completing tasks (e.g. “I tend to get things done on time”- reverse scored). Sensation-seeking refers to the preference for doing exciting and thrilling activities (e.g. “I would enjoy water skiing”). Participants were asked to respond to each item using a 4-point scale (“Not at all like me” – “Not like me” – “Somewhat like me” – “Very much like me”) with high scores reflecting impulsivity. Internal reliabilities were high for negative urgency (Cronbach's α = 0.83), lack of premeditation (Cronbach's α = 0.82), lack of perseverance (Cronbach's α = 0.84) and sensation-seeking (Cronbach's α = 0.88), which was very similar to the original study (Zapolski et al., 2010). Three participants did not complete this questionnaire and an additional four participants failed to complete all items from the lack of perseverance subscale, resulting in missing data.
Grand's Hunger Scale (GHS). The GHS (Grand, 1968) was given prior to and after completion of the food bias task. Participants were asked to rate first how hungry they were using a 7-point scale and how much of their favourite food they could eat right now using a 6-point scale. The GHS at baseline was used as a covariate in our analyses and we report high internal reliability for these two items (Cronbach's α = 0.78) and no missing data.
Cognitive task. We administered a Stimulus-Response Compatibility (SRC) task in order to assess approach bias for food. Participants were instructed to approach or avoid different stimulus categories with a manikin using the up/down arrow keys. The task consisted of two blocks – a food approach/non-food avoid block and a food avoid/non-food approach block – which were counterbalanced in order of presentation. A trial began with a fixation cross in the centre of the screen (1000 ms), replaced by a stimulus (food or non-food picture) in the centre of the screen with a manikin (15 mm high) positioned 40 mm above or below the picture. There was a brief inter-trial interval (500 ms). Participants were instructed to either approach or avoid each stimulus type at the beginning of the task (i.e. stimulus type was task-relevant), and were instructed again after the end of the first block that the instructions had reversed. The task consisted of 112 experimental trials (approach food, avoid food, approach non-food, and avoid non-food trials in equal number). Approach and avoidance responses were made by pressing the up or down arrow keys. Responding caused the manikin to become animated and move in the direction of the arrow press. Each trial was completed when the participant had made three responses and the manikin either reached the picture (approach trials) or reached the top/bottom of the screen (avoid trials). Only the initial RT was used in later data analysis.
Pictures were chosen from the food-pics database (Blechert, Meule, Busch, & Ohla, 2014) which contains over 800 images of food and non-food items rated on perceptual characteristics and affective ratings. We chose 8 sweet snack food pictures (e.g. donut, ice-cream, grapes and blueberries) and 8 non-food miscellaneous household pictures (e.g. cushion, key, book and umbrella) that were matched for complexity, familiarity and valence. We designed our task based on an earlier study (Havermans et al., 2011), however due to time constraints in relation to the wider nature of the current study and needing to keep tasks short, we included less trials and less food pictures, which is why we focused only on sweet snack food items, rather than a combination of sweet, salty and fatty snacks. We chose food items that were likely to be available to the sample population as between meal snacks, in order to enhance detection of approach biases.
Data cleaning. Data for the SRC task was prepared by first removing error trials (12.7%) and extremely short RTs < 200 ms (0.7%) and long RTs > 3000 ms (0.9%) from the data-set. We also excluded trials that were 3 SDs from each participant's mean RT per trial type (1.4% trials). We then calculated a mean RT per stimulus (food, non-food) and response type (approach, avoid) for each participant in order to explore the data. Data from seven participants was removed for performing at near-chance level (>40% error rate). Food bias scores were calculated by collapsing RT information across blocks and subtracting mean RT in approach food/avoid non-food blocks from mean RT in avoid food/approach non-food blocks, in accordance with other studies (Brignell et al., 2009; Christiansen, Cole, Goudie & Field, 2012; Kersbergen et al., 2015). Higher scores indicate a stronger approach bias for food.
1.3. Procedure
Participants were tested in a group setting (M group size = 21.08, SD = 10.71) either at their school or at the Department of Experimental Psychology, University of Oxford. They completed a range of behavioural and questionnaire measures on Windows computers using Inquisit software delivered through the Internet. All participants completed two 60-min sessions consisting of three cognitive tasks and seven questionnaires – task order was always the same for each participant (Appendix A) and the assessments that are not relevant to the current study will be reported elsewhere. The two sessions were either completed back-to-back (e.g. period one and period two) or were completed on different days, depending on availability to book computer rooms. Each child also provided a saliva sample at the end of session two for prospective genetic analysis that will be reported elsewhere. The test session began with gaining informed assent, explaining the procedure and asking participants to remember to read all task instructions carefully without looking at their neighbour's computer screen. Two researchers were always present to provide help and support. Participants were individually invited into a separate room during the questionnaire section of the session to complete a height and weight assessment – 24 participants either refused or were unable to provide this measurement.
1.4. Statistical analysis
For our main analyses, we ran four separate regression models of uncontrolled eating, testing the independent and interactive effect of four separate impulsivity factors with approach bias for food. All predictor variables were mean centred prior to analysis and an interaction term was computed by multiplying each impulsivity factor with approach bias for food (Aiken, West, & Reno, 1991). We conducted four hierarchical regression models controlling for baseline hunger in step one. Additionally, an impulsivity factor and approach bias were entered in step one, and the interaction term was added in step two. Models with significant interactions were followed up with simple slopes analysis testing the effect of impulsivity on uncontrolled eating at high (+1 SD) and low (−1 SD) levels of approach bias for food.
2. Results
2.1. Correlations between variables
In order to explore the data, a correlation table with descriptive statistics is presented in Table 1. Most pertinent to the current study, we found that all of the impulsivity factors were positively related to uncontrolled eating, particularly negative urgency. Negative urgency was also highly correlated with emotional eating. Approach bias did not correlate with uncontrolled eating. Baseline hunger reported immediately before the SRC task did correlate with uncontrolled eating. Uncontrolled eating positively correlated with emotional eating and negatively with cognitive restraint. Uncontrolled eating did not correlate with BMI, however the other two eating styles did, as emotional eating and cognitive restraint were both related to higher BMI. In general, the impulsivity factors showed small inter-factor correlations supporting the notion that they are different constructs, however lack of premeditation and lack of perseverance showed a strong correlation.
Table 1.
Correlations and Descriptive Statistics between all variables (N = 504).
| Mean (SD) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1) hunger | 8.84 (2.73) | |||||||||
| 2) UE | 19.62 (5.83) | 0.21* | ||||||||
| 3) EE | 5.33 (2.51) | 0.02 | 0.54* | |||||||
| 4) CR | 13.51 (4.31) | -0.09 | -0.20* | 0.03 | ||||||
| 5) NU | 19.81 (4.84) | 0.07 | 0.34* | 0.34* | 0.15* | |||||
| 6) Lpre | 18.42 (4.44) | 0.07 | 0.18* | 0.05 | -0.03 | 0.31* | ||||
| 7) Lper | 17.31 (4.71) | 0.07 | 0.17* | 0.08 | -0.01 | 0.12* | 0.61* | |||
| 8) SS | 23.90 (5.91) | 0.08 | 0.09 | -0.04 | 0.09 | 0.14* | 0.21* | 0.01 | ||
| 9) AB-F | 48.41 (107.91) | -0.04 | 0.07 | 0.02 | -0.05 | 0.08 | -0.09 | -0.08 | -0.06 | |
| 10) BMI | 19.91 (3.31) | -0.03 | 0.01 | 0.21* | 0.21* | 0.01 | -0.11 | 0.05 | -0.06 | -0.01 |
Note: hunger = baseline hunger; UE = uncontrolled eating; EE = emotional eating; CR = cognitive restraint; NU = negative urgency; Lpre = lack of premeditation; Lper = lack of perseverance; SS = sensation-seeking; AB-F = approach bias for food; BMI = body-mass-index.
*significant at the p < 0.01 level.
2.2. Approach bias for food
Approach bias for food (measured with the SRC task) was calculated as the difference in RT between trials in the approach food block and trials in the avoid food block. Scores ranged from −294 to 466 (M = 48.41, SD = 107.91) with high positive numbers reflecting a strong approach bias for food. We conducted a paired samples t-test and found that overall participants were significantly faster in the approach food block (M = 743.21, SD = 149.31) compared to the avoid food block (M = 791.61, SD = 169.31), t (495) = −10.00, p < 0.001, d = 0.45.
2.3. Effect of impulsivity and approach bias on uncontrolled eating
An overview of the results from four regression models are presented in Table 2. Model one tested the independent and interactive effect of lack of premeditation and approach bias on uncontrolled eating. Step one tested the independent effects and was significant overall, F (3,480) = 12.01, p < 0.001, R2 = 0.07. Baseline hunger significantly predicted uncontrolled eating, as did lack of premeditation and approach bias for food, all in the predicted direction. Step two added the interaction term to the model and resulted in increased explained variance, ΔR2 = 0.01, p = 0.03, the overall model fit was significant, F (4,479) = 10.31, p < 0.001, R2 = 0.08, as the interaction between lack of premeditation and approach bias was significant. Model two tested the independent and interactive effect of negative urgency and approach bias on uncontrolled eating. Step one tested the independent effects and was significant overall, F (3,480) = 26.95, p < 0.001, R2 = 0.14, as baseline hunger significantly predicted uncontrolled eating, as did negative urgency, in the predicted direction, however approach bias for food was not a significant predictor. Step two added the interaction term to the model and resulted in no added variance explained, ΔR2 < 0.01, p = 0.30, the overall model fit was significant, F (4,479) = 20.51, p < 0.001, R2 = 0.15, but the interaction term was not significant. Model three tested the independent and interactive effect of lack of perseverance and approach bias on uncontrolled eating. Step one tested the independent effects and was significant overall, F (3,477) = 11.08, p < 0.001, R2 = 0.07, as baseline hunger significantly predicted uncontrolled eating, as did lack of perseverance and approach bias for food, in the predicted direction. Step two added the interaction term to the model and resulted in no added variance explained, ΔR2 < 0.01, p = 0.18, the overall model fit was significant, F (4,476) = 8.81, p < 0.001, R2 = 0.07, but the interaction term was not significant. Model four tested the independent and interactive effect of sensation-seeking and approach bias on uncontrolled eating. Step one tested the independent effects and was significant overall, F (3,480) = 7.93, p < 0.001, R2 = 0.05. Baseline hunger significantly predicted uncontrolled eating, but sensation-seeking was not significant and neither was approach bias for food. Step two added the interaction term and resulted in no added variance explained, ΔR2 < 0.01, p = 0.21, the overall model fit was significant, F (4,480) = 6.44, p < 0.001, R2 = 0.05, but the interaction term was not significant.
Table 2.
Regression models showing effects of impulsivity and approach bias for food on uncontrolled eating.
| Model 1 | b | SE b | β |
|---|---|---|---|
| Step 1 | |||
| Constant | 16.15 | 0.91 | |
| hunger | 0.41 | 0.11 | 0.21** |
| lack of premeditation | 0.22 | 0.06 | 0.21** |
| approach bias | 0.01 | 0.00 | 0.11* |
| Step 2 | |||
| Constant | 16.21 | 0.92 | |
| hunger | 0.41 | 0.11 | 0.21** |
| lack of premeditation | 0.22 | 0.06 | 0.21** |
| approach bias | 0.01 | 0.00 | 0.11* |
| interaction | 0.00 | 0.00 | 0.11* |
|
Note:N = 483: R2 = 0.07 for step 1: ΔR2 = 0.01 for step 2 (ps < 0.05): *p < 0.05, **p < 0.001 | |||
|
Model 2 |
b |
SE b |
β |
| Step 1 | |||
| Constant | 10.61 | 1.11 | |
| hunger | 0.41 | 0.11 | 0.21** |
| negative urgency | 0.41 | 0.11 | 0.32** |
| approach bias | 0.00 | 0.00 | 0.11 |
| Step 2 | |||
| Constant | 10.61 | 1.11 | |
| hunger | 0.41 | 0.11 | 0.21** |
| negative urgency | 0.41 | 0.11 | 0.32** |
| approach bias | -0.00 | 0.01 | -0.11 |
| interaction | 0.00 | 0.00 | 0.14 |
|
Note:N = 483: R2 = 0.14, p < 0.001 for step 1: ΔR2 < 0.01 (n.s.) for step 2: **p < 0.001 | |||
|
Model 3 |
b |
SE b |
β |
| Step 1 | |||
| Constant | 13.71 | 1.11 | |
| hunger | 0.41 | 0.11 | 0.21** |
| lack of perseverance | 0.21 | 0.11 | 0.21** |
| approach bias | 0.01 | 0.00 | 0.11* |
| Step 2 | |||
| Constant | 13.74 | 1.11 | |
| hunger | 0.41 | 0.11 | 0.21** |
| lack of perseverance | 0.21 | 0.11 | 0.21** |
| approach bias | -0.00 | 0.01 | -0.07 |
| interaction | 0.00 | 0.00 | 0.21 |
|
Note:N = 480: R2 = 0.07, p < 0.001 for step 1: ΔR2 < 0.01 (n.s.) for step 2: *p < 0.05, **p < 0.001 | |||
|
Model 4 |
b |
SE b |
β |
| Step 1 | |||
| Constant | 14.72 | 1.14 | |
| hunger | 0.41 | 0.11 | 0.21** |
| sensation-seeking | 0.08 | 0.04 | 0.11 |
| approach bias | 0.00 | 0.00 | 0.11 |
| Step 2 | |||
| Constant | 14.72 | 1.14 | |
| hunger | 0.40 | 0.11 | 0.21** |
| sensation-seeking | 0.11 | 0.04 | 0.08 |
| approach bias | -0.01 | 0.01 | -0.11 |
| interaction | 0.00 | 0.00 | 0.20 |
| Note:N = 483: R2 = 0.05, p < 0.001 for step 1: ΔR2 < 0.01 (n.s.) for step 2: **p < 0.001 | |||
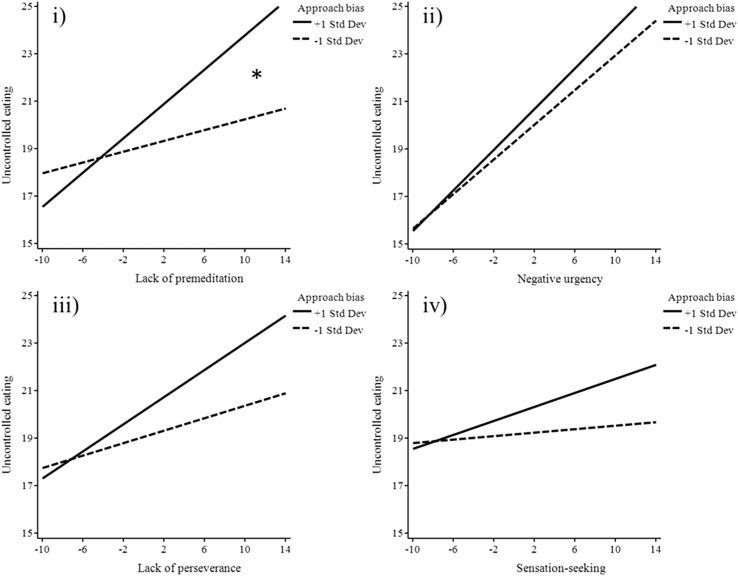
Simple slopes analysis was performed to follow up significant interactions (model one only). Lack of premeditation on uncontrolled eating was tested at high (+1 SD above the mean) and low (−1 SD below the mean) levels of approach bias for food. The analysis found that when approach bias was high, lack of premeditation was a strong predictor of uncontrolled eating, B = 0.41, t (480) = 4.43, p < 0.001, whereas when approach bias was low, lack of premeditation did not predict uncontrolled eating, B = 0.11, t (480) = 1.42, p = 0.21. This suggests that high automatic approach bias for food and high levels of lack of premeditation interact in explaining levels of uncontrolled eating. A graphical representation of all models is presented in Fig. 1, including the significant interaction from model one (Fig. 1(i)).
Fig. 1.
Graphical representation of separate impulsivity factors at high and low levels of approach bias for food predicting uncontrolled eating (i) lack of premeditation x food bias was the only significant interaction, (ii) negative urgency x food bias, (iii) lack of perseverance x food bias, (iv) sensation-seeking x food bias were non-significant interactions.
3. Discussion
The current study assessed the impact of trait impulsivity (reflecting impaired cognitive control) and approach bias for food (reflecting automatic responsivity to food) on uncontrolled eating behaviour in a large sample of adolescents. Four models were tested in order to assess the independent influence of four separate impulsivity factors on uncontrolled eating, and whether these relationships were modulated by approach bias for food. The results indicated that individuals scoring high on lack of premeditation were more likely to report high levels of uncontrolled eating when approach bias for food was also high. This pattern supports a dual-process model of overeating, as automatic processes related to reward sensitivity and controlled processes related to trait impulsivity interacted to explain uncontrolled eating. Individuals scoring high on negative urgency were also more likely to report high levels of uncontrolled eating but this was not moderated by approach bias, suggesting that this impulsivity factor is strongly related to uncontrolled eating regardless of level of approach bias for food. Likewise, individuals scoring high on lack of perseverance were more likely to report high levels of uncontrolled eating, and this was not moderated by approach bias. Finally, individuals scoring high on sensation-seeking were not more likely to report high levels of uncontrolled eating and this was not moderated by approach bias for food. In sum, we found that all impulsivity factors were related to high levels of uncontrolled eating, apart from sensation-seeking, and that approach bias for food was a significant moderator of this relationship only in the case of lack of premeditation.
The current results with a large sample of adolescents support the role of impulsivity in overeating (Delgado-Rico et al., 2012, Jasinska et al., 2012, Mobbs et al., 2010, Nederkoorn et al., 2015, Thamotharan et al., 2013). In addition to testing an adolescent sample, we assessed multiple factors of impulsivity providing important new data on the relations among trait impulsivity factors and uncontrolled eating. As predicted, we found that negative urgency was the factor most related to uncontrolled eating, in line with previous research (Becker et al., 2016, Delgado-Rico et al., 2012, Mobbs et al., 2010, Murphy et al., 2014). Our results extend previous findings to show that both lack of premeditation and lack of perseverance are moderately related to uncontrolled eating, while sensation-seeking is unrelated. Further, we found that uncontrolled eating is the maladaptive eating style most associated with trait impulsivity, as it was correlated with three impulsivity factors, while emotional eating and cognitive restraint only correlated with negative urgency. This highlights the need to address different individual risk factors for different unhealthy eating styles.
A strong dual-process model would predict an interaction between impulsivity and approach bias for food on uncontrolled eating. However, this pattern was only found for lack of premeditation. It is unclear why this impulsivity factor was the only one to interact with approach bias and this finding needs to be replicated before drawing any firm conclusions. Lack of premeditation reflects a general deficit in impulse control and a failure to evaluate future consequences, therefore it is reasonable to expect that those scoring high on this trait would engage in uncontrolled eating, especially when sensitive to appetitive food in the environment, which activates reward networks and approach motivated behaviour. The failure to support the interaction with negative urgency is likely to be explained by the fact that this impulsivity factor is strongly associated with uncontrolled eating, regardless of automatic processes. The failure to find an interaction with sensation-seeking could be explained by the lack of association between sensation-seeking and uncontrolled eating, e.g. research suggests it is more likely to predict risk-taking behaviour (Greene, Krcmar, Walters, Rubin, & Hale, 2000). The absence of an interaction with lack of perseverance is more puzzling, as this factor is closely related to lack of premeditation, but refers more to current task impulsivity. Future research may find evidence for an interaction between lack of perseverance and approach bias for food in explaining unhealthy eating, as the interaction did approach significance in the current study. One reason for the small interactive effects in our study could be due to measurement bias, as impulsivity and uncontrolled eating were both measured by self-report, which may have inflated their relationship, thus washing away an interactive effect with approach bias. For example, Kakoschke et al. (2015) measured impulsivity with a Go/No-go task and found that both impulsivity and high approach bias combined were necessary to explain unhealthy eating, while neither were predictive in isolation. Future research could benefit from measuring both behavioural and self-report impulsivity to understand these processes further.
There are some limitations to be noted regarding this study. Although we provide new information about the role of trait impulsivity factors, related to cognitive control, our findings do not directly address the role of cognitive control or response inhibition. Provided the heterogeneous nature of concepts like impulsivity and cognitive control, future research would benefit from including other measures, such as the Go/No-go task, in order to investigate whether results hold when including a more direct, task-based measure of response inhibition. Further, we only assessed the four-factor model of trait impulsivity (Whiteside & Lynam, 2001), while future research may benefit from using the adapted five-factor model (Lynam et al., 2007), in order to assess the relative contribution of positive urgency to uncontrolled eating. We also relied on self-report to assess uncontrolled eating, while other more objective measures, such as the bogus taste-test (Kakoschke et al., 2015, Nederkoorn et al., 2015), could be considered for future research. Some limitations with our SRC task should be noted, as the task was quite short and only included pictures of sweet snack foods. Thus, our findings may not generalise to savoury foods. Moreover, we did not measure subjective liking of the food items, which could be a potential confounding factor. We used an explicit approach-avoidance task in this research as food/non-food stimuli were task-relevant. Other measures that capture implicit processing biases, in which participants respond to task-irrelevant features, e.g. the tilt of an image, are also available. A potentially informative future research strategy would be to investigate the relative contribution of implicit and explicit action-tendencies on eating behaviours.
The cross-sectional nature of the current study, which does not allow for interpretation of the direction of effects, could be considered to be a further limitation. Future research would benefit from taking a longitudinal approach, or assessing whether modifying the cognitive processes of interest has a positive effect on unhealthy eating. The current data is from Wave 1 of a longitudinal study and we will follow-up on some of these questions over the years to come. All of our testing took place in groups in schools, which limited our ability to control certain variables, such as food intake prior to testing or number of other participants in the session. Finally, our sample was largely healthy and predominately from high socio-economic backgrounds, therefore may not be representative of the population at large, particularly those at highest risk of obesity.
Our findings provide new insights into the cognitive processes that are related to uncontrolled eating in a large sample of healthy adolescents. It is hoped that these results will inform future intervention strategies. For example, targeting inhibition in cognitive control training is likely to improve impulsive individuals approach motivated responding to appetitive food stimuli. In support of this, a recent randomised controlled trial using Go/No-go response inhibition training found encouraging results in a community sample of overweight adults, showing that those in the active condition reported less snack consumption and greater weight loss at one-week and six-month follow up (Lawrence et al., 2015). This study suggests that inhibition training can have real-world effects encouraging healthier eating, particularly when training is specific to food cues. Adolescents may be particularly responsive to inhibition training due to greater neural plasticity (Gogtay et al., 2004) and enhanced computer literacy.
In conclusion, the current results indicate that three separate impulsivity factors have an important influence on uncontrolled eating behaviour in a large sample of young adolescents. There was also evidence that automatic and controlled cognitive processes can sometimes interact to predict this unhealthy eating style. Critically, we found that distinct components of trait impulsivity were differentially associated with self-reported uncontrolled eating, and automatic processing of food cues was sometimes an important factor in modulating this relationship. Future research should be designed to further clarify the role of impulsivity and automatic approach bias for food on overeating – using a wider variety of measures including behavioural impulsivity and actual unhealthy food consumption. The results support the use of novel interventions of cognitive control training for those at risk of obesity, particularly those with high levels of impulsivity.
Acknowledgements
This research was funded by the European Research Council (ERC) under the European Union's Seventh Framework Programme (FP7/2007–2013)/ERC grant agreement no: [324176]. Funding sources had no involvement in study design, data collection, analysis and interpretation of data, writing of the report, nor in the decision making to submit the article for publication. We would like to acknowledge all of the research assistants who helped to collect data, including Annabel Songco, Lauren Heathcote and Sam Parsons. We are also extremely grateful to those who volunteered to participate in this study, including the adolescent participants, their parents for consenting to take part, and the teachers and IT support at each school who facilitated this research. Without them this research would not have been possible.
Appendix A. Procedure and testing session structure
| Session 1 = 60 min | Session 2 = 60 min |
|---|---|
| T1 = Flanker task | T1 = Memory bias task |
| T2 = Emotion dot-probe task | T2 = Balloon Analogue Risk Task (BART) |
| T3 = Adolescent Interpretation and Belief Questionnaire (AIBQ) | T3 = Food Stimulus Response Compatibility (SRC) taska |
| Q1 = Self-esteem scale | Q1 = Impulsivity UPPS scalea |
| Q2 = Worry scale | Q2 = Behavioural inhibition and activation scale |
| Q3 = Child Anxiety & Depression scale | Q3 = Risk evaluation scale |
| Q4 = Bully questionnaire | Q4 = Three Factor Eating questionnairea |
| Q5 = Child and Adolescent Survey of Experiences (CASE) | Q5 = Mental Health Continuum |
| Q6 = Rumination scale | Q6 = Connor-Davidson Resilience scale |
| Q7 = Pain questionnaire | Oragene saliva sample |
Relevant to current study.
References
- Aiken L.S., West S.G., Reno R.R. Sage; 1991. Multiple regression: Testing and interpreting interactions. [Google Scholar]
- Bechara A. Decision making, impulse control and loss of willpower to resist drugs: A neurocognitive perspective. Nature Neuroscience. 2005;8(11):1458–1463. doi: 10.1038/nn1584. [DOI] [PubMed] [Google Scholar]
- Becker K.D., Fischer S., Smith G.T., Miller J.D. The influence of negative urgency, attentional bias, and emotional dimensions on palatable food consumption. Appetite. 2016;100:236–243. doi: 10.1016/j.appet.2016.02.019. https://doi.org/10.1016/j.appet.2016.02.019 [DOI] [PubMed] [Google Scholar]
- Berg J.M., Latzman R.D., Bliwise N.G., Lilienfeld S.O. American Psychological Association; 2015. Parsing the heterogeneity of impulsivity: A meta-analytic review of the behavioral implications of the UPPS for psychopathology. [DOI] [PubMed] [Google Scholar]
- Berthoud H.R. Interactions between the “cognitive” and “metabolic” brain in the control of food intake. Physiology & Behavior. 2007;91(5):486–498. doi: 10.1016/j.physbeh.2006.12.016. [DOI] [PubMed] [Google Scholar]
- Blechert J., Meule A., Busch N.A., Ohla K. Food-pics: An image database for experimental research on eating and appetite. Frontiers in Psychology. 2014;5(617) doi: 10.3389/fpsyg.2014.00617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brignell C., Griffiths T., Bradley B.P., Mogg K. Attentional and approach biases for pictorial food cues. Influence of external eating. Appetite. 2009;52(2):299–306. doi: 10.1016/j.appet.2008.10.007. [DOI] [PubMed] [Google Scholar]
- Cornelis M.C., Rimm E.B., Curhan G.C., Kraft P., Hunter D.J., Hu F.B. Obesity susceptibility loci and uncontrolled eating, emotional eating and cognitive restraint behaviors in men and women. Obesity. 2014;22(5):E135–E141. doi: 10.1002/oby.20592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christiansen P., Cole J.C., Goudie A.J., Field M. Components of behavioural impulsivity and automatic cue approach predict unique variance in hazardous drinking. Psychopharmacology. 2012;219:501–510. doi: 10.1007/s00213-011-2396-z. [DOI] [PubMed] [Google Scholar]
- Delgado-Rico E., Rio-Valle J.S., Gonzalez-Jimenez E., Campoy C., Verdejo-Garcia A. BMI predicts emotion-driven impulsivity and cognitive inflexibility in adolescents with excess weight. Obesity. 2012;20(8):1604–1610. doi: 10.1038/oby.2012.47. [DOI] [PubMed] [Google Scholar]
- Diamond A. Executive functions. In: Fiske S.T., editor. Vol. 64. 2013. pp. 135–168. (Annual review of Psychology). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gogtay N., Giedd J.N., Lusk L., Hayashi K.M., Greenstein D., Vaituzis A.C.…Toga A.W. Dynamic mapping of human cortical development during childhood through early adulthood. Proceedings of the National Academy of Sciences of the United States of America. 2004;101(21):8174–8179. doi: 10.1073/pnas.0402680101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grand S. Color-word interference: An investigation of the role of vocal conflict and hunger in associative priming. Journal of Experimental Psychology. 1968;77(1):31–40. doi: 10.1037/h0025759. [DOI] [PubMed] [Google Scholar]
- Greene K., Krcmar M., Walters L.H., Rubin D.L., Hale L. Targeting adolescent risk-taking behaviors: The contributions of egocentrism and sensation-seeking. Journal of Adolescence. 2000;23(4):439–461. doi: 10.1006/jado.2000.0330. [DOI] [PubMed] [Google Scholar]
- Havermans R.C., Giesen J.C., Houben K., Jansen A. Weight, gender, and snack appeal. Eating Behaviors. 2011;12(2):126–130. doi: 10.1016/j.eatbeh.2011.01.010. [DOI] [PubMed] [Google Scholar]
- He Q., Xiao L., Xue G., Wong S., Ames S.L., Schembre S.M. Poor ability to resist tempting calorie rich food is linked to altered balance between neural systems involved in urge and self-control. Nutrition Journal. 2014;13(1):1. doi: 10.1186/1475-2891-13-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houben K., Wiers R.W. Response inhibition moderates the relationship between implicit associations and drinking behavior. Alcoholism: Clinical and Experimental Research. 2009;33(4):626–633. doi: 10.1111/j.1530-0277.2008.00877.x. [DOI] [PubMed] [Google Scholar]
- Jasinska A.J., Yasuda M., Burant C.F., Gregor N., Khatri S., Sweet M. Impulsivity and inhibitory control deficits are associated with unhealthy eating in young adults. Appetite. 2012;59(3):738–747. doi: 10.1016/j.appet.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kakoschke N., Kemps E., Tiggemann M. Combined effects of cognitive bias for food cues and poor inhibitory control on unhealthy food intake. Appetite. 2015;87:358–364. doi: 10.1016/j.appet.2015.01.004. [DOI] [PubMed] [Google Scholar]
- Karlsson J., Persson L.O., Sjostrom L., Sullivan M. Psychometric properties and factor structure of the Three-Factor Eating Questionnaire (TFEQ) in obese men and women. Results from the Swedish Obese Subjects (SOS) study. International Journal of Obesity. 2000;24(12):1715–1725. doi: 10.1038/sj.ijo.0801442. [DOI] [PubMed] [Google Scholar]
- Kemps E., Tiggemann M. Approach bias for food cues in obese individuals. Psychology & Health. 2015;30(3):370–380. doi: 10.1080/08870446.2014.974605. [DOI] [PubMed] [Google Scholar]
- Kemps E., Tiggemann M., Martin R., Elliott M. Implicit approach–avoidance associations for craved food cues. Journal of Experimental Psychology: Applied. 2013;19(1):30. doi: 10.1037/a0031626. [DOI] [PubMed] [Google Scholar]
- Kersbergen I., Woud M.L., Field M. The validity of different measures of automatic alcohol action tendencies. Psychology of Addictive Behaviors. 2015;29(1):225–230. doi: 10.1037/adb0000009. [DOI] [PubMed] [Google Scholar]
- de Lauzon B., Romon M., Deschamps V., Lafay L., Borys J.M., Karlsson J.…Grp F.S. The three-factor eating questionnaire-R18 is able to distinguish among different eating patterns in a general population. Journal of Nutrition. 2004;134(9):2372–2380. doi: 10.1093/jn/134.9.2372. [DOI] [PubMed] [Google Scholar]
- Lawrence N.S., Hinton E.C., Parkinson J.A., Lawrence A.D. Nucleus accumbens response to food cues predicts subsequent snack consumption in women and increased body mass index in those with reduced self-control. Neuroimage. 2012;63(1):415–422. doi: 10.1016/j.neuroimage.2012.06.070. https://doi.org/10.1016/j.neuroimage.2012.06.070 [DOI] [PubMed] [Google Scholar]
- Lawrence N.S., O'Sullivan J., Parslow D., Javaid M., Adams R.C., Chambers C.D.…Verbruggen F. Training response inhibition to food is associated with weight loss and reduced energy intake. Appetite. 2015;95:17–28. doi: 10.1016/j.appet.2015.06.009. https://doi.org/10.1016/j.appet.2015.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynam D., Smith G., Cyders M., Fischer S., Whiteside S. Purdue University; 2007. The UPPS-P questionnaire measure of five dispositions to rash action. Unpublished technical report. [Google Scholar]
- Mobbs O., Crepin C., Thiery C., Golay A., Van der Linden M. Obesity and the four facets of impulsivity. Patient Education and Counseling. 2010;79(3):372–377. doi: 10.1016/j.pec.2010.03.003. [DOI] [PubMed] [Google Scholar]
- Mogg K., Bradley B.P., O'Neill B., Bani M., Merlo-Pich E., Koch A.…Nathan P.J. Effect of dopamine D3 receptor antagonism on approach responses to food cues in overweight and obese individuals. Behavioural Pharmacology. 2012;23(5 and 6):603–608. doi: 10.1097/FBP.0b013e3283566a4a. [DOI] [PubMed] [Google Scholar]
- Murphy C.M., Stojek M.K., MacKillop J. Interrelationships among impulsive personality traits, food addiction, and body mass index. Appetite. 2014;73:45–50. doi: 10.1016/j.appet.2013.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nederkoorn C., Dassen F.C.M., Franken L., Resch C., Houben K. Impulsivity and overeating in children in the absence and presence of hunger. Appetite. 2015;93:57–61. doi: 10.1016/j.appet.2015.03.032. [DOI] [PubMed] [Google Scholar]
- Popien A., Frayn M., von Ranson K.M., Sears C.R. Eye gaze tracking reveals heightened attention to food in adults with binge eating when viewing images of real-world scenes. Appetite. 2015;91:233–240. doi: 10.1016/j.appet.2015.04.046. [DOI] [PubMed] [Google Scholar]
- Schmitz F., Naumann E., Trentowska M., Svaldi J. Attentional bias for food cues in binge eating disorder. Appetite. 2014;80:70–80. doi: 10.1016/j.appet.2014.04.023. [DOI] [PubMed] [Google Scholar]
- Seibt B., Häfner M., Deutsch R. Prepared to eat: How immediate affective and motivational responses to food cues are influenced by food deprivation. European Journal of Social Psychology. 2007;37(2):359–379. [Google Scholar]
- Thamotharan S., Lange K., Zale E.L., Huffhines L., Fields S. The role of impulsivity in pediatric obesity and weight status: A meta-analytic review. Clinical Psychology Review. 2013;33(2):253–262. doi: 10.1016/j.cpr.2012.12.001. [DOI] [PubMed] [Google Scholar]
- Volkow N.D., Wang G.J., Fowler J.S., Telang F. Overlapping neuronal circuits in addiction and obesity: Evidence of systems pathology. Philosophical Transactions of the Royal Society B-biological Sciences. 2008;363(1507):3191–3200. doi: 10.1098/rstb.2008.0107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y.C., McPherson K., Marsh T., Gortmaker S.L., Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. The Lancet. 2011;378(9793):815–825. doi: 10.1016/S0140-6736(11)60814-3. [DOI] [PubMed] [Google Scholar]
- Whiteside S.P., Lynam D.R. The five factor model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences. 2001;30(4):669–689. [Google Scholar]
- Wiers R.W., Bartholow B.D., van den Wildenberg E., Thush C., Engels R., Sher K.J.…Stacy A.W. Automatic and controlled processes and the development of addictive behaviors in adolescents: A review and a model. Pharmacology Biochemistry and Behavior. 2007;86(2):263–283. doi: 10.1016/j.pbb.2006.09.021. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) 2016. Obesity, data and statistics.http://www.euro.who.int/en/health-topics/noncommunicable-diseases/obesity/data-and-statistics/Accessed 23 October 2017 [Google Scholar]
- Zapolski T.C.B., Stairs A.M., Settles R.F., Combs J.L., Smith G.T. The measurement of dispositions to rash action in children. Assessment. 2010;17(1):116–125. doi: 10.1177/1073191109351372. [DOI] [PMC free article] [PubMed] [Google Scholar]