Abstract
Background
Singapore has been certified malaria-free by the World Health Organization since November 1982. However, sporadic autochthonous malaria outbreaks do occur. In one of the most recent outbreaks of vivax malaria, an entomological investigation identified Anopheles sinensis as the most probable vector. As metaphase karyotype studies divided An. sinensis into two forms, A and B, with different vector competence: the investigation of vector competence of An. sinensis found in Singapore was thus pursued using Plasmodium vivax field isolates from the Thailand–Myanmar border.
Methods
Adults and larvae An. sinensis were collected from Singapore from 14 different locations, using various trapping and collection methods between September 2013 and January 2016. Molecular identification of An. sinensis species were conducted by amplifying the ITS2 and CO1 region using PCR. Experimental infections of An. sinensis using blood from seven patients infected with P. vivax from the Thailand–Myanmar border were conducted with Anopheles cracens (An. dirus B) as control.
Results
Phylogenetic analysis showed that An. sinensis (F22, F2 and collected from outbreak areas) found in Singapore was entirely Form A, and closely related to An. sinensis Form A from Thailand. Artificial infection of these Singapore strain An. sinensis Form A resulted in the development of oocysts in four experiments, with the number of sporozoites produced by one An. sinensis ranging from 4301 to 14,538.
Conclusions
Infection experiments showed that An. sinensis Form A from Singapore was susceptible to Thai–Myanmar P. vivax strain, suggesting a potential role as a malaria vector in Singapore.
Keywords: Malaria vector, Infection, Anopheles sinensis Form A, An. cracens, Sporozoites
Background
Singapore was once rampant with malaria cases [1]. Outbreaks in mainland Singapore and off-shore islands of Singapore involving the known malaria vectors, i.e. Anopheles maculatus, Anopheles epiroticus (previously known as Anopheles sundaicus) and Anopheles letifer, were reported from 1960s to 1970s [2–4]. Singapore attained its malaria free status in November 1982 [2]. The total malaria annual incidence rate fluctuated between 2.9 and 3.9 cases per 100,000 people from 1998 to 2007, and 0.5 to 2.6 per 100,000 people from 2008 to 2015 [5]. The major causative parasite was P. vivax, followed by P. falciparum. While almost all cases were imported cases, there have been occasional sporadic malarial cases with no travel history (e.g. in 2010 and 2013) and 15 small sporadic localized transmissions with less than 50 cases in each outbreak [5–9]. As a tourist and business hub, with high reliance on foreign personnel from malaria endemic countries, Singapore remains vulnerable to malaria unless the vector population is well understood and remains well controlled.
The last outbreaks occurred in the middle of 2009, when three clusters with a total of 29 vivax malaria patients, with no recent travel history, were identified by the Ministry of Health. Relapse cases in vivax malaria amongst foreign workers from malaria endemic countries are common and defining if the cluster is due to local transmission is challenging. Therefore, molecular epidemiology was performed using the msp3a and msp1 genes of the parasite. It confirmed only two independent local transmissions in Mandai-Sungei Kadut and in Sembawang [8]. The predominant Anopheles found in the two areas was Anopheles sinensis, a mosquito that was not previously recognized as a vector in Singapore. Transmission in Jurong could not be confirmed as the infecting parasite from the cases showed no genetic link among them. Correspondingly, no potential Anopheles vectors, including An. sinensis, were found in the vicinity. Although An. sinensis has been implicated as the malaria vector in some parts of Asia, including Korea, China, Japan and Vietnam, it has never been reported as a vector in Singapore [10–23].
Anopheles sinensis is a member of the Hyrcanus group. Due to morphological complexity and similarity among the members of the group, the members have often been misidentified and their respective vector status is confusing [24, 25]. Furthermore, confirming An. sinensis as vector has been made more complicated by the existence of two forms, i.e. Form A and B, both of which are morphologically identical [26–28]. Yet, hybridization of these two forms showed they were genetically compatible, yielding viable progeny, complete synaptic polytene chromosomes and was said to exhibit cytological polymorphic races [29, 30].
The vector competence of these two forms of An. sinensis is not fully understood. To date, only a single study reported that An. sinensis Form B was able to produce sporozoites in the salivary glands, while Form A could not [31]. Based on the cytological polymorphism of An. sinensis and on previous vector competence studies [29–31], it was noteworthy that the two forms could have different vector abilities in malaria transmission depending on their geographic regions. This study aims to characterize Singapore’s strain of An. sinensis, including its vector competence.
Methods
Mosquito collection
In December 2013, larvae of the An. sinensis were collected from a grassy pool of a big field at Changi Coast Road, eastern Singapore and they were colonized in the laboratory. Following the first collection, 103 adults and larvae An. sinensis were collected from 13 different locations in Singapore between September 2013 and January 2016 (Fig. 1). Anopheles sinensis larvae were collected by the Environmental Health Officer (EHO) of National Environment Agency (NEA) during the routine malaria surveillance and were submitted to Environmental Health Institute (EHI) for identification. They were reared to adult for this study.
Fig. 1.
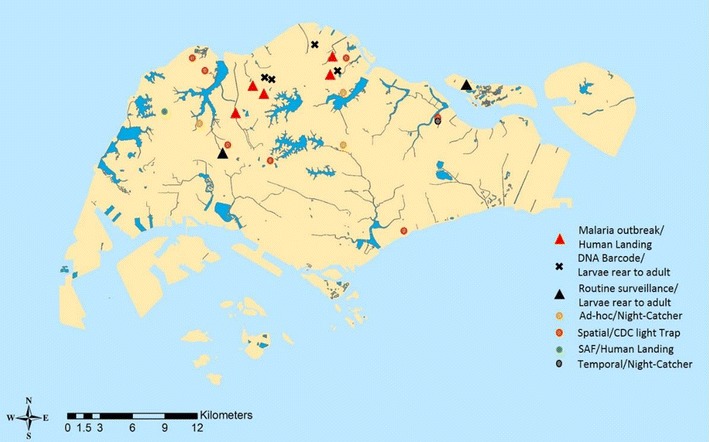
Spatial distribution of Anopheles sinensis collected from 13 locations throughout Singapore for determining the taxonomic forms of Singapore’s An. sinensis. Additionally, sequences of samples from four locations labelled “x” and five locations labelled as “∆” were extracted from Genbank as references. Note: Spatial/CDC light trap: Spatial distribution study conducted in 2013 using CDC light trap; Singapore Armed Forces/Human Landing: Mosquitoes collected from Singapore Military training grounds via Human Landing method; Ad hoc/Night-Catcher: Mosquitoes collected due to feedback on high Anopheles adult population using Night-Catcher; Temporal/Night-Catcher: An. sinensis collected from a 2 years temporal study using Night-Catcher; Routine surveillance/Larvae reared to adult: Larvae collected through routine surveillance were sent into EHI lab for identification and were reared to adult stage; DNA barcode/larvae reared to adult stage: Anopheles sinensis larvae were collected for DNA barcode project (DNA sequences were retrieved from Genbank and were used as reference in our current taxonomic study [32]); Malaria outbreaks/Human Landing: Adult An. sinensis were collected during 2009 malaria outbreak via Human Landing (DNA sequences were retrieved from Genbank for our current study [8])
For the An. sinensis adults, some were collected using modified CDC-light traps during spatial distribution study and ad-hoc collection in response to public feedback on high mosquito population. A portion of adult An. sinensis were collected through human landing catch during 2009 malaria outbreak in malaria cluster areas [8] and during surveillance by the Singapore Armed Forces in military training grounds [32]. The remaining adult An. sinensis were collected via Night-Catcher during temporal study and ad-hoc collection was conducted due to high mosquito population. Night-Catcher, an in-house mosquito trap, which was improvised from CDC light trap, enables hourly collection of mosquitoes using incandescent light and dry ice (CO2) as attractant (Fig. 2). All collections were conducted from 7 p.m. to the 10 a.m. the next morning.
Fig. 2.

Night Catcher is an in-house designed mosquito trap that enables trapping of mosquitoes at every hour. It was improvised from CDC light trap which uses incandescent light and dry ice (CO2) as attractants
Mosquito morphological identification
Larvae and adult mosquitoes were identified under compound microscope according to taxonomy keys [17, 33, 34]. Confirmed An. sinensis were reared in EHI’s insectary at 25 °C (± 2 °C) and 70% (± 10%) relative humidity. Upon emergence, the adults were then reconfirmed morphologically to the species level according to taxonomy keys [17, 33, 34]. Due to the absence of morphological trait differences between the two forms of An. sinensis, these mosquitoes were further determined using molecular taxonomic tools to ensure the accurate form determination as well as purity of the colony.
Molecular taxonomy
In order to identify the forms of An. sinensis in Singapore, regions of both the COI and rDNA internal transcribed spacer (ITS2) genes were sequenced. All 103 An. sinensis collected from 13 different locations were individually processed. Total DNA were extracted individually using DNeasy blood and tissue kit following the manufacturer’s procedures (Qiagen, Hilden, Germany) and stored at − 20 °C until analysis. Two regions flanking the mitochondrial COI gene and ITS2 gene were amplified by polymerase chain reaction (PCR) as described in previous studies [35–37]. Amplicons were then visualized on 2% agarose gel stained with GelRed (Biotium Inc., USA), and cleaned using Purelink PCR purification kit (Invitrogen Corp., USA) according to manufacturer’s instructions. Sequencing was carried out by a commercial laboratory using BigDye Terminator Cycle Sequencing kit (Applied Biosystems, USA). For the susceptible study, sixty adult mosquitoes that were used in the susceptible study were transferred individually into separate 2 ml vials and homogenized using a mixer mill (Retsch Mixer Mill MM301). The DNA extraction, PCR and gel visualization protocols were similar to what was described above. The sequences of the remaining 11 samples from nine different locations were extracted from EHI’s previously published data [8, 35].
Phylogenetic analysis and genetic distance calculation
Contiguous sequences of CO1 and ITS2 genes were created using Lasergene 9.0 software suite (DNASTAR Inc., USA). These sequences were then aligned using Clustal W algorithm [38] executed in BioEdit v7.05 software [39]. Neighbour joining algorithm was adopted during the construction of phylogenetic trees using MEGA 6.06 software suite [40]. Parameters selection included a Kimura-2 parameter substitution model with gamma distributed rates using the nearest neighbour interchange heuristic search method. Robustness of clustering was determined by bootstrap analysis with 1000 replicates. Reference DNA sequences were obtained from the GenBank database. The pairwise distances between each specimens was computed using MEGA 6.06 software package [40].
Colonization technique
Colonization was initiated by transferring wild-caught An. sinensis adults into 30 cm × 30 cm × 30 cm large cage made from acrylic plastic sheets. Ten percent sucrose was given as food source by soaking it with cotton wool in a glass bottle. Artificial insemination was conducted in earlier generations to propagate and establish a colony in the insectary. Subsequent generations were based on natural insemination, which was induced by exposing these mosquitoes to stroboscopic blue light from 7 p.m. to 9 p.m. for at least 5 days prior to blood feeding [41, 42]. Six days after emergence, females were transferred into 15 oz. transparent plastic container with plastic net affixed on top. Female mosquitoes were deprived from sugar overnight in these feeding containers with moistened cotton pad on top of the net. Specific Pathogen Free (SPF) mini-pig blood was offered to the mosquitoes via a Hemotek® feeding system. On the 3rd day post blood feeding, females were transferred into 15 oz. ovipots (transparent plastic containers) lined with moist filter paper for eggs collection. Eggs were collected on filter paper and hatched in Reversed Osmosis water (RO). Larvae food consisting of wheat germ, oats, dry yeast, casein or low fat milk powder, bubble rice, Vitamin B complex and Nestum were mixed and ground into fine powder. Approximately 0.1 g of larvae food was dispensed daily when the larvae grew from 1st to 2nd instars. Larvae food increased to 0.2 and 0.4 g during 3rd instars and 4th instars, respectively. The second generation (F2) of An. sinensis, collected from a country club in Singapore in July 2015, was also used in this study to compare the differential vector competence with the lab-bred (F22) strain. In order to produce sufficient mosquitoes for the comparison, artificial insemination of F0 and F1 An. sinensis were carried out. This strain was colonized following the above described protocol.
Transportation of Anopheles sinensis eggs
A colony of the twenty-second generation of An. sinensis (F22) and another of F2 were used for the competence study. An approval and an export permit were obtained from Director-General Public Health of National Environment Agency prior to sending the eggs of An. sinensis to SMRU. Eggs produced at the insectary of EHI, were transferred onto a clean piece of filter paper, packed and sealed in a sterile petri dish before transporting to Shoklo Malaria Research Unit (SMRU) laboratory, on the Thai-Myanmar border. Although An. sinensis Form A and B have previously been found in northern Thailand [28], every precaution was taken to ensure that Singapore’s strain An. sinensis used in this study were not released.
Preparation of patient blood for infection
Patients seeking consultation at SMRU migrant clinics located along the border (Wang Pha, Mawker Thai) where they were tested by blood smear microscopy, only gametocytes positive patients were selected for the study. After a written informed consent was obtained, five to 10 ml of venous blood were drawn into a heparin tube, and immediately placed in a water bath at 37–38 °C to prevent exflagellation of male microgametes [43]. Within an hour, blood samples were transported from the field clinics to the central SMRU laboratory for processing. Following centrifugation at 1800g for 5 min in an Eppendorf® centrifuge which was warmed at 38 °C, plasma was replaced with AB+ serum and within 10 min the blood was transported to the insectary.
Mosquito infection in secure insectary at Maesot
All experimental mosquito infections were carried out at the SMRU secured insectary in Mae Sot as described by Andolina et al. [44]. The secure insectary that is physically separated from open areas by four sealed and locked doors. Only authorized trained personnel can gain access and conduct infection studies. All infected/engorged mosquitoes were counted and placed in incubators (Sanyo®, MIR-254) were secured with netting material. Mosquitoes which fed insufficiently were killed in ethanol 70%. Anopheles cracens (An. dirus B), an efficient P. vivax vector [44] was used as a positive control and was fed with the same blood samples, in parallel with An. sinensis.
Microscopy detection of oocysts and sporozoites in mosquitoes
On seven to 8 days post infection, midguts of both mosquito species were dissected and stained with 1% mercurochrome. Oocyst positive midguts were placed in 100 µl of PBS and stored at − 80 °C until PCR was performed. Dissection of salivary glands for sporozoites detection was carried out 15 days post infection. Salivary glands were placed in an Eppendorf tube filled with 50 µl of Roswell Park Memorial Institute medium (RPMI) and kept on ice until the dissection of all mosquitoes was completed. The sample was spun down for 5 min in a micro centrifuge and salivary glands were pooled and crushed using a 100 µl pipette. 10 µl of salivary glands suspension was placed into a KOVA Glasstic slide with 10 grids. Sporozoites were counted and averaged on four grids, multiplied to the chamber factor and dilution factor in order to calculate the number of sporozoites per µl. Average sporozoites counts in a single mosquito was calculated by dividing the total sporozoites with the number of mosquitoes dissected.
Molecular detection of P. vivax in mosquitoes
To confirm P. vivax infection, DNA from dissected midguts was extracted in 100 µl PBS using a Qiagen Tissue Kit with minor modifications. Briefly, 180 µl of ATL buffer and 50 µl of proteinase K (Qiagen Tissue Kit) was added to the sample, mixed briefly by vortex and incubated overnight at 56 °C in a shaking incubator. Following digestion, DNA was bound to the silica membrane, washed then eluted in 200 µl water following manufacturer’s instructions. The sample was then concentrated by drying in a vacuum concentrator at 30 °C and re-eluted in 10 µl AE Buffer (Qiagen). Primers and probes described by Perandin et al. [45] were used to amplify and detect species specific regions of the 18S rRNA gene. Real-time PCR was done using QuantiTect Multiplex RT-PCR Kit and an ABI 7500 Fast Cycler.
Statistical analysis
R-3.1.1 software was used to conduct statistical analysis in this study [46]. Two-way Wilcoxon rank sum test was used when comparison of oocysts development was made between F2 and F22 An. sinensis Form A.
Ethics approval
The study was approved by Oxford Tropical Research Ethics Committee (Reference 28-09).
Results
Taxonomic status of Singapore strain Anopheles sinensis
A total of 103 mosquitoes collected from the various locations were confirmed to be An. sinensis through morphological identification. However, polymorphic wing variation at CuA was noted among the specimens from field collection (Fig. 3). Out of the 103 specimens, only 42 specimens had complete morphological characteristics where wing scales were still intact. Of the 42 specimens, 20 (47.6%) of them had pale CuA fringe spots, while the remaining 22 (52.4%) showed dark fringe spots. The locality and the proportion of the dark and pale CuA fringe spot are listed in Table 1. It was observed that each location could have both An. sinensis with pale and dark CuA fringe spots.
Fig. 3.
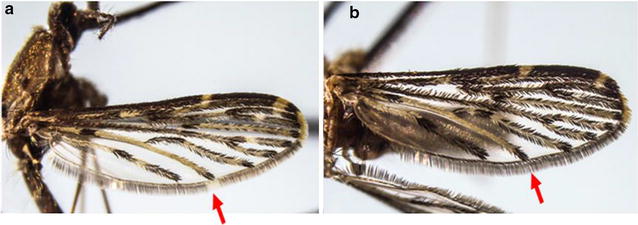
Anopheles sinensis’ wing vein CuA (indicated by red arrow) showed a pale fringe spot and b dark fringe spot [35]
Table 1.
The proportion of Anopheles sinensis with pale or dark CuA wing fringe spot and their respective locations
| Location | Pale CuA | Dark CuA |
|---|---|---|
| Bishan-AMK Park | 11 | 11 |
| Orchid Country Club | 2 | 1 |
| Lorong Halus | 2 | 2 |
| Lim Chu Kang | 4 | 4 |
| Western Training Plot | 0 | 1 |
| Lorong Semangka | 0 | 2 |
| Bukit Batok Rd | 1 | 2 |
| Total (%) | 20 (47.6%) | 22 (52.4%) |
Phylogenetic analysis based on ITS2 gene of 103 Singapore An. sinensis and 42 reference sequences from the NCBI database showed that all Singapore An. sinensis sequences, including those collected during 2009 outbreak, formed a monophyletic clade. Though the Singapore sequences were derived from mosquitoes with CuA pale or dark fringe spots, it is interesting to note the tight clustering despite the differences in wing fringe coloration. The phylogenetic tree also shows that the Singapore An. sinensis clustered together with Thailand’s An. sinensis Form A (bootstrap value = 85) (Fig. 4). On the other hand, An. sinensis Form B from Thailand (AY13047.1), Korea (AY130469.1), China (EU 931614) and Japan (EU 931613) formed a separate clade from our local An. sinensis with strong bootstrap support (bootstrap value = 100). None of the Singapore An. sinensis adults falls into the Form B clade. The data suggests that An. sinensis found in Singapore are Form A.
Fig. 4.
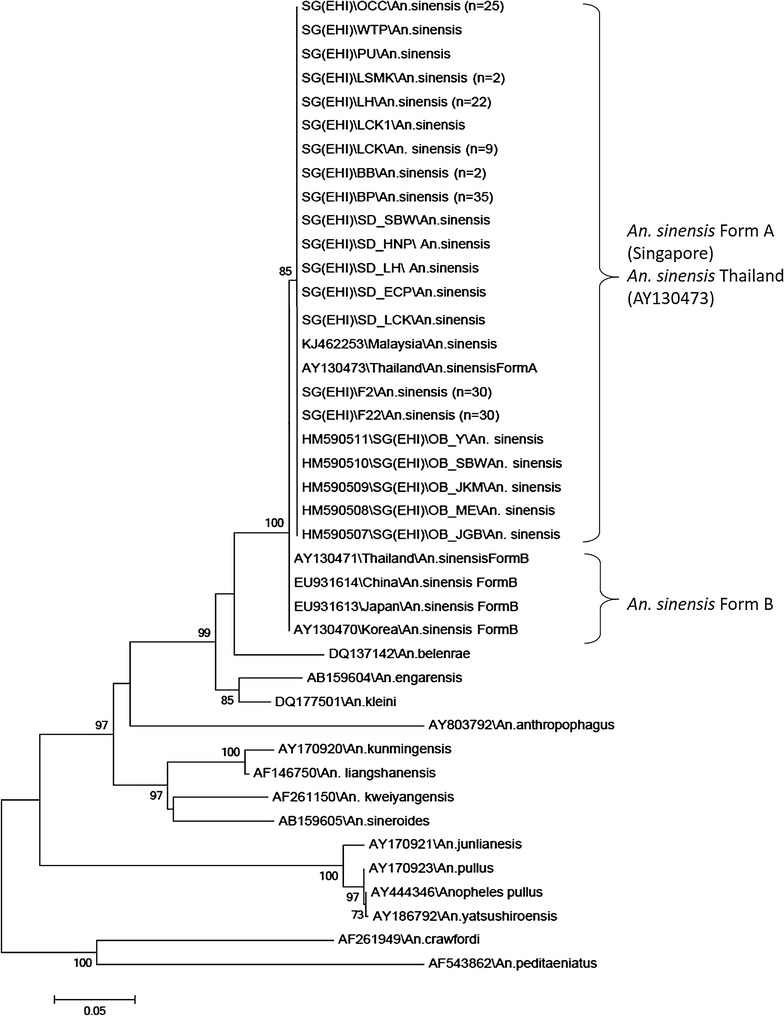
Phylogenetic tree of the ITS2 genes of Anopheles hyrcanus group, constructed using the neighbor-joining algorithm. The values next to the nodes are bootstrap percentages based on 1000 replicates, and only bootstrap percentages above 70% are shown
Similarly, the phylogenetic analysis of CO1 gene sequences using neighbor joining showed that Singapore An. sinensis clustered separately from An. sinensis Form B from Korea (AY444351) with bootstrap value of 73 (Fig. 5). There was no reference sequence of Form A CO1 gene in the NCBI database for comparison with Singapore An. sinensis sequences. Interestingly, unlike the ITS2 sequences, the COI gene sequences of local An. sinensis formed subgroups, though with weak bootstrap support, indicating subtle genetic changes at mitochondrial level.
Fig. 5.
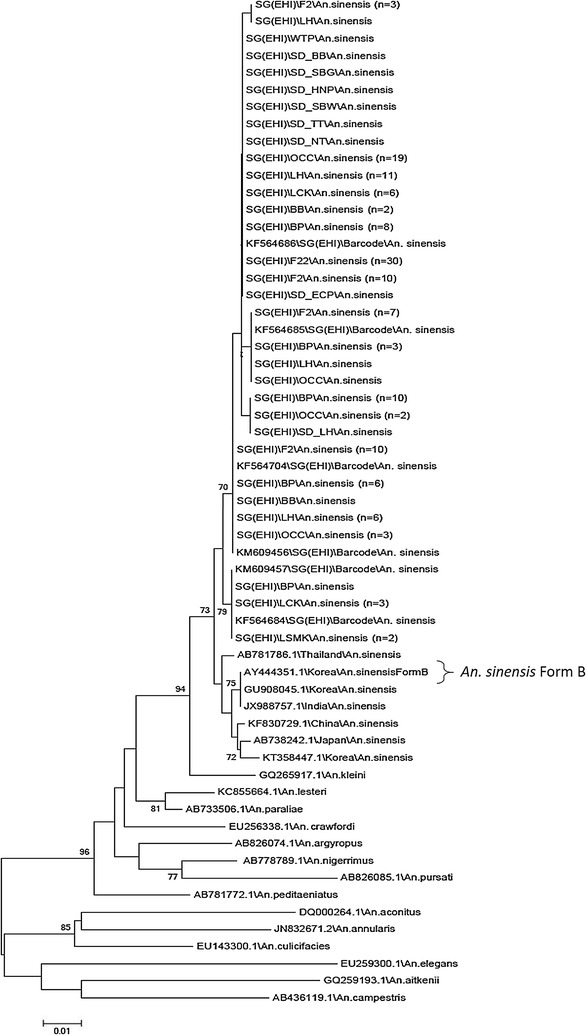
Phylogenetic tree of the CO1 genes of Anopheles hyrcanus group, constructed using the neighbor-joining algorithm. The values next to the nodes are bootstrap percentages based on 1000 replicates, and only bootstrap percentages above 70% are shown
Previously, it was reported that approximately 75% of An. sinensis in the Malaya region (including Singapore) and Borneo had dark fringe spot [34]. However, in this current study, it was interesting to note that 22 (52.4%) of the examined local An. sinensis has dark fringe spot at CuA (Table 1). When all 42 specimens with pale and dark CuA wing fringe spots were tallied with the CO1 phylogenetic tree, no specific clustering of pale or dark phenotype in subgroups. Both phenotypes randomly occurred within the CO1 phylogenetic tree.
To ensure that the laboratory mosquitoes used for infection is consistent with field caught mosquitoes, the CO1 and ITS2 genes of 30 F22 mosquitoes were also analysed. They were found to be the same as field caught ones (Figs. 4, 5).
Oocysts and sporozoites detection in An. sinensis
The bloods of seven patients with P. vivax were fed to F22 An. sinensis and An. cracens using Hemotek® feeding system membrane feeding. In total, 50–100% (Fig. 6) of dissected An. sinensis developed one to 92 oocysts (Table 2). Similar results were obtained with An. cracens where the infection rate was between 77.7 and 100%, with each mosquito developing one to 200 oocysts. These findings were further confirmed with real-time PCR.
Fig. 6.
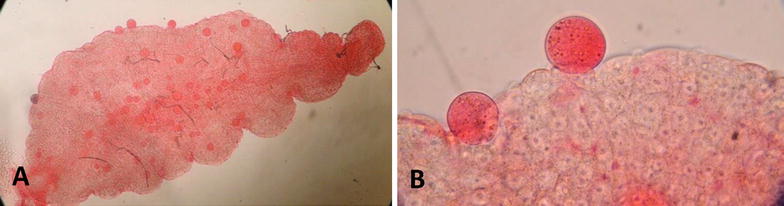
Photos of midguts of An. sinensis with growth of P. vivax oocysts (red globules). Visualizing midguts with oocysts growth at a ×4 magnification and b ×10 magnification
Table 2.
Detection of P. vivax oocysts in midguts and sporozoites in salivary glands of An. sinensis and An. cracens (control) on 6 Days Post Infection (DPI) and 15 DPI, respectively
| Gametocytaemia (gams/500WBC) | Mosquito species | No. of mosquitoes blood fed | Oocysts | Sporozoites | |||
|---|---|---|---|---|---|---|---|
| Number of mosquitoes with oocysts/dissected (%) | Average number of oocysts (SD) | Range of oocyst densities in each infected mosquito | Average no. of sporozoites in each mosquito | No. of mosquitoes dissected | |||
| 416 | An. sinensis (F22) | 17 | 9/14 (64.3) | 2.6 (± 2.7) | 1–8 | ND | ND |
| An. cracens | 17 | 14/17 (82.4) | 6.8 (± 6.2) | 1–18 | ND | ND | |
| 480 | An. sinensis (F22) | 10 | 7/7 (100.0) | 57 (± 17.4) | 27–82 | ND | ND |
| An. cracens | 10 | 7/9 (77.8) | 71 (± 42.6) | 60–100 | ND | ND | |
| 576 | An. sinensis (F22) | 10 | 5/5 (100.0) | 16 (± 7.7) | 3–22 | ND | ND |
| An. cracens | 10 | 5/5 (100.0) | 66 (± 26.2) | 12–90 | ND | ND | |
| 384 | An. sinensis (F22) | 24 | 5/7 * (71.4) | 6.4 (± 9.1) | 2–26 | 4435 | 7 |
| An. cracens | 20 | 7/7 (100.0) | 8.1 (± 19.9) | 2–18 | 9000 | 7 | |
| 768 | An. sinensis (F22) | 22 | 3/3 (100.0) | 7 (± 5.3) | 3–13 | 703 | 8 |
| An. cracens | 38 | 3/3 (100.0) | 26 (± 19.3) | 9–47 | 2812 | 7 | |
| 416 | An. sinensis (F22) | 48 | 3/3 (100.0) | 74 (± 21.6) | 50–92 | 4302 | 34 |
| An. cracens | 47 | 3/3 (100.0) | >200 (NA) | > 200 | 76,764 | 34 | |
| 304 | An. sinensis (F22) | 30 | 2/4 (50.0) | 18.8 (± 22.0) | 33–42 | 14,538 | 24 |
| An. cracens | 66 | 3/3 (100.0) | 18.7 (± 3.1) | 26–32 | 4687 | 24 | |
Data labelled (*) indicated the dissection performed on 15 DPI. ND indicated that dissection for sporozoites was not done
NA not available
Out of seven experiments, only the last four yielded enough blood fed mosquitoes for detection of parasite in salivary glands. Salivary glands from each experiment were pooled to ensure minimal loss of sporozoites during manipulation of examining. These four experiments showed that An. sinensis could produce 703–14,538 sporozoites per mosquito (Fig. 7), while An. cracens, produced 2812 sporozoites to 76,764 sporozoites per mosquito (Table 2).
Fig. 7.
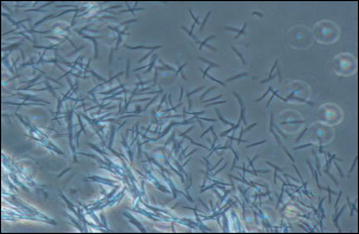
Microscopy image of sporozoites released from salivary glands of infected An. sinensis Form A (black arrows). Visualizing sporozoites on KOVA glass slides at ×40 magnification
Comparison between F22 and F2 mosquito strains
Comparison of infectivity between F22 and F2 strains of An. sinensis was conducted to determine if they were analogous. Both strains showed similar susceptibility to P. vivax infection (two-way Wilcoxon rank sum test, p = 0.935) with the F2 strain having 75–100% infection rate and F22 strain having a 50–100% at midguts (Table 3). Second generation of An. sinensis F2, had on average 25 and 51 oocysts in each midgut, while F22 had 11 and 74 oocysts on average.
Table 3.
Comparison of oocyst development between F2 strain and F22 Anopheles sinensis Form A
| Gametocytaemia (gams/500WBC) | Strains | Oocysts | Sporozoites | |||
|---|---|---|---|---|---|---|
| Positive/dissected (%) | Average no. of oocyst (± SD) | Oocyst range | Number of mosquitoes dissected | Average sporozoites per mosquito | ||
| 416 | F22 | 3/3 (100.0) | 74 (± 21.6) | 50–80 | 34 | 4302 |
| F2 | 3/3 (100.0) | 51.0 (± 9.0) | 50–60 | 35 | 10,928 | |
| 304 | F22 | 2/4 (50.0) | 11 (± 19.1) | 33–42 | 24 | 14,538 |
| F2 | 3/4 (75.0) | 25 (± 22.1) | 33–42 | 10 | 11,250 | |
Two-way Wilcoxon rank sum test showed no significant difference in the number of oocysts detected between F2 and F22 strains (p = 0.935). No statistical test was carried out on sporozoites since insufficient data was available.
The average numbers of sporozoites produced by F22 were 4302 and 14,538 sporozoites in each mosquito, while that produced by F2 strain were 10,928–11,250 sporozoites each. Statistical tests were not carried out on the average number of sporozoites produced due to insufficient data.
Discussion
In the 2009 malaria outbreaks in Singapore, An. sinensis, was the predominant Anopheles species found in local outbreak areas. Together with classical and molecular epidemiological data, it was suggested that An. sinensis was the probable malaria vector [8]. This study has now determined that An. sinensis in Singapore belongs to Form A of the species and more importantly, provided evidence that it is a potential malaria vector in Singapore. Due to limitation in transferring of Anopheles eggs and variation of rearing conditions, dissection of few mosquitoes in the initial four experiments could only be carried so as to confirm the successful development of vivax oocysts in An. sinensis Form A. Following that, minimal number of dissection for oocysts was needed, and infected An. sinensis Form A mosquitoes could be reserved for salivary glands dissection on 16 DPI, which is essentially crucial to determine the vector status of An. sinensis Form A.
Anopheles sinensis is classified under the Hyrcanus group. Under this group, it comprises of several species having minute differences in their morphology. From eight species [25], the total number of species within the Hyrcanus group increased to 27 [47, 48]. Using integrative taxonomy (the combination of morphological and molecular tools), Singapore’s An. sinensis was, for the first time, confirmed to be Form A. All An. sinensis collected from the field, including those collected from the 2009 local malaria outbreak [8] formed a clade with Form A of Thailand. No Form B was found. Although ITS2 showed homogeneity among the An. sinensis in Singapore, the COI analysis suggest some heterogeneity which probably could only be deciphered using techniques that provides better resolution e.g. Restriction-site Associated DNA sequencing (RADseq) [49] or whole genome sequencing [50].
Although there have been multiple reports of experimental infection that resulted in An. sinensis producing sporozoites [51–53], only two [18, 54] natural infections of An. sinensis have been recorded in the Southeast Asia. However, these findings were called into doubt [25]. Thailand has never implicated An. sinensis as an important malaria vector, with contrasting results in vector competencies being reported from two studies. One reported 61.5% of infected mosquitoes presenting with sporozoites; another showed only 5.88% in Form B and none in Form A [31, 52]. On the contrary, we have shown that Singapore’s strain of An. sinensis (Form A) is a potential vector of P. vivax, with competency level nearly equivalent to An. cracens. It could have been the vector of the 2009 local malaria outbreak. Together with the data from Korea, China and Thailand, the vector competencies of An. sinensis appears to be highly dependent on the taxonomic forms [31] and geographical areas of the mosquitoes, and the perhaps genetic diversity parasites [51], Difference due to experimental design also cannot be excluded. More work is needed to understand An. sinensis and its role in malaria transmission.
Although we are aware that experimental susceptibility tests do not necessarily reflect the role of malaria transmission in nature, such findings highlight the potential risk of An. sinensis if its population is left uncurbed. The habitats of An. sinensis in Singapore are not restricted to the rural, usually coastal, areas of Singapore, where typical malaria vectors were found. They appear to thrive well in urban freshwater bodies such as ponds and reservoirs that have become very integrated into the Singapore landscape. Being zoophilic, numerous reports classified An. sinensis as an inefficient or an unimportant vector even though infections were detected naturally and experimentally [13, 14, 51]. However, in an urbanized city like Singapore, where animals are scarce, An. sinensis could readily bite human since human density is considerably high [13, 15]. Thus, the risk of malaria transmission by An. sinensis could not be disregarded, and warrants monitoring and surveillance. During the investigation and mitigation of An. sinensis breeding, it was found that they can be controlled by removing algae that develop in these water bodies. More work is ongoing to determine the risk of An. sinensis breeding in urban Singapore.
Conclusions
Together, the data suggests that An. sinensis Form A could have been the vector of the 2009 local malaria outbreak and highlights a potential risk of malaria transmission in Singapore by An. sinensis. The local map of malaria receptive area for Anopheles surveillance and control has been reviewed to include the presence of An. sinensis.
Authors’ contributions
BM, NLC, LR and FN conceived the study. PSC, CA and MABAR were responsible of colonization of mosquitoes. CA, PSC, and LPSG were responsible of infection, detection and quantification of oocysts and sporozoites in mosquitoes. PSC was responsible in the preparation of manuscript. PSC conducted the DNA extraction, PCR and sequence alignment and analysis. PC was responsible of parasite DNA extraction and qPCR. CCS, CC and BR worked on implementing the study on a field level and reviewed the manuscript; CCS and LDQ provide advice in the experimental designs of this study. All authors read and approved the final manuscript.
Acknowledgements
We thank the support of staff from Vector-borne Programme of EHI for providing support in identification, field collection, infection and analysis of data. The valuable advice provided by Prof. Indra Vythilingam and Dr. David Lee Kim Sung is greatly appreciated. We also would like to thank Singapore Armed Forces for allowing us to conduct trapping in their territories for this study.
A special thanks to Prapan Kittiphanakun and Saw Nay Hsel for their support during the experiments and the mosquitoes rearing in the insectary at Shoklo Malaria Research Unit, Thailand.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
Not applicable.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Funding
FN, CA, CC were supported by the Wellcome Trust (Programme Grant 089179) and were part of the Wellcome Trust Mahidol University Oxford Tropical Medicine Research Programme funded by the Wellcome Trust Foundation (Grant No. OPP1023643); PC, BR, LR and BM were supported by funding from the Singapore Immunology Network (SIgN) and the Horizontal Programme on Infectious Diseases under the Agency for Science, Technology and Research (A*STAR, Singapore).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Sook-Cheng Pang and Chiara Andolina contributed equally to this work
Contributor Information
Sook-Cheng Pang, Email: Pang_Sook_Cheng@nea.gov.sg.
Chiara Andolina, Email: Chiara.Andolina@radboudumc.nl.
Benoit Malleret, Email: Benoit_Malleret@immunol.a-star.edu.sg.
Peter R. Christensen, Email: peter@shoklo-unit.com
Sai-Gek Lam-Phua, Email: Lam-Phua_Sai_Gek@nea.gov.sg.
Muhammad Aliff Bin Abdul Razak, Email: Muhammad_Aliff_ABDUL_RAZAK@nea.gov.sg.
Chee-Seng Chong, Email: Chong_Chee_Seng@nea.gov.sg.
Daiqin Li, Email: dbslidq@nus.edu.sg.
Cindy S. Chu, Email: Cindy@tropmedres.ac
Bruce Russell, Email: b.russell@otago.ac.nz.
Laurent Rénia, Email: renia_laurent@immunol.a-star.edu.sg.
Lee-Ching Ng, Email: ng_lee_ching@nea.gov.sg.
Francois Nosten, Email: francois@tropmedres.ac.
References
- 1.Brooke GE, Marckepeace WD, Braddel WD. One hundred years of Singapore. London; 1921.
- 2.Goh KT. Eradication of malaria from Singapore. Singap Med J. 1983;24:255–268. [PubMed] [Google Scholar]
- 3.Chew PK. The outbreak of malaria at Fuyong Estate in Singapore. Singap Med J. 1968;9:111–126. [PubMed] [Google Scholar]
- 4.Chan KL, Goh KT, Koh TS. The Whampoa–Kallang malaria outbreak, 1974-5. Singap Med J. 1976;17:124–132. [PubMed] [Google Scholar]
- 5.Lin Yj, Badaruddin H, Ooi P-LS. Badaruddin H, Ooi P-LS. Epidemiology of malaria in Singapore, 2008–15. Epidemiol News Bull. 2016;42(2):49–54. [Google Scholar]
- 6.Lee YCA, Tang CS, Ang LW, Han HK, James L, Goh KT. Epidemiological characteristics of imported and locally-acquired malaria in Singapore. Ann Acad Med Singap. 2009;38:840–849. [PubMed] [Google Scholar]
- 7.Ng LC, Lee KS, Tan CH, Ooi PL, Lam-Phua SG, Lin R, et al. Entomologic and molecular investigation into Plasmodium vivax transmission in Singapore, 2009. Malar J. 2010;9:305. doi: 10.1186/1475-2875-9-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ng OT, Ooi EE, Lee CC, Lee PJ, Ng LC, Pei SW, et al. Naturally acquired human Plasmodium knowlesi infection, Singapore. Emerg Infect Dis. 2008;14:814–816. doi: 10.3201/eid1405.070863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lim J, Han HK, Lim S, Ooi PL. An outbreak of vivax malaria in the off shore islands, July–Sept 2006. Commun Dis Div Minist Health. 2006;33:55–58. [Google Scholar]
- 10.Tanaka K, Mizusawa K, Saugstad ES. A revision of the adult and larval mosquitoes of Japan (including the Ryukyu Archipelago and the Ogasawara Islands) and Korea (Diptera: Culicidae) Contr Am Ent Inst. 1979;16:1–987. [Google Scholar]
- 11.Chow CY. Malaria vectors in China. Chin J Entomol Spec Pub. 1991;6:67–79. [Google Scholar]
- 12.Lu G, Zhou S, Horstick O, Wang X, Liu Y, Muller O. Malaria outbreaks in China (1990–2013): a systematic review. Malar J. 2014;13:269. doi: 10.1186/1475-2875-13-269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ree HI. Studies on Anopheles sinensis, the vector species of vivax malaria in Korea. Korean J Parasitol. 2005;43:75–92. doi: 10.3347/kjp.2005.43.3.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ree HI, Hong HK, Paik YH. Study on natural infection of Plasmodium vivax in Anopheles sinensis in Korea. Kisaengchunghak Chapchi. 1967;5:3–4. doi: 10.3347/kjp.1967.5.1.3. [DOI] [PubMed] [Google Scholar]
- 15.Pan JY, Zhou SS, Zheng X, Huang F, Wang DQ, Shen YZ, et al. Vector capacity of Anopheles sinensis in malaria outbreak areas of central China. Parasit Vectors. 2012;5:136. doi: 10.1186/1756-3305-5-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Otsuru M. Malaria studies in Japan after World War II. Part I. Epidemiological aspects of postwar malaria. Jpn J Exp Med. 1960;30:23–32. [PubMed] [Google Scholar]
- 17.Harrison BA, Scanlon JE. Medical entomology studies-II The subgenus Anopheles in Thailand (Diptera: Culicidae) Contrib Am Entomol Inst. 1975;12:1–307. [Google Scholar]
- 18.O’Connor CT. The Anopheles hyrcanus group in Indonesia. Mosq Syst. 1980;12:293–305. [Google Scholar]
- 19.Manh CD, Beebe NW, Van VNT, Quang TL, Lein CT, Nguyen DV. Vectors and malaria transmission in deforested, rural communities in north-central Vietnam. Malar J. 2010;9:259. doi: 10.1186/1475-2875-9-259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Van Hell JC. On the Anophelines of Southern Celbes, with reference to the vectors of malaria. Medisch Maandblad. 1950;3:379. [PubMed] [Google Scholar]
- 21.Lee HI, Lee JS, Shin EH, Lee WJ, Kim YY, Lee KR. Malaria transmission potential by Anopheles sinensis in the Republic of Korea. Korean J Parasitol. 2001;39:185–192. doi: 10.3347/kjp.2001.39.2.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee WJ, Klein TA, Kim HC, Choi YM, Yoon SH, Chang KS, et al. Anopheles kleini, Anopheles pullus, and Anopheles sinensis: potential vectors of Plasmodium vivax in the Republic of Korea. J Med Entomol. 2007;44:1086–1090. doi: 10.1093/jmedent/41.5.72. [DOI] [PubMed] [Google Scholar]
- 23.Sleigh AC, Liu XL, Jackson S, Li P, Shang LY. Resurgence of vivax malaria in Henan Province, China. Bull World Health Organ. 1998;76:265–270. [PMC free article] [PubMed] [Google Scholar]
- 24.Beales PF. A review of the taxonomic status of Anopheles sinensis and its bionomics in relation to malaria transmission. World Health Organization. 1984, WHO/MAL/84.1007.
- 25.Reid JA. The Anopheles hyrcanus group in South-East Asia (Diptera: Culicidae) Bull Entomol Res. 1953;44:5–77. doi: 10.1017/S0007485300022938. [DOI] [Google Scholar]
- 26.Harrison BA. A new interpretation of affinities within the Anopheles hyrcanus complex of Southeast Asia. Mosq Syst. 1972;4:73–83. [Google Scholar]
- 27.Harrison BA. A lectotype designation and description for Anopheles (An.) sinensis Wiedemann 1828, with a discussion of the classification and vector status of this and some other oriental anopheles. Mosq Syst. 1828;1973(5):1–13. [Google Scholar]
- 28.Baimai V, Rattanarithikul R, Kijchalao U. Metaphase karyotypes of Anopheles of Thailand and Southeast Asia: I. The Hyrcanus Group. J Am Mosq Control Assoc. 1993;9:59–67. [PubMed] [Google Scholar]
- 29.Choochote W, Jitpakdi A, Rongsriyam Y, Komalamisra N, Pitasawat B, Palakul K. Isoenzyme study and hybridization of two forms of Anopheles sinensis (Diptera: Culicidae) in northern Thailand. Southeast Asian J Trop Med Public Health. 1998;29:841–848. [PubMed] [Google Scholar]
- 30.Min GS, Choochote W, Jitpakdi A, Kim SJ, Kim W, Jung J, Junkum A. Intraspecific hybridization of Anopheles sinensis (Diptera: Culicidae) strains from Thailand and Korea. Mol Cell. 2002;14:198–204. [PubMed] [Google Scholar]
- 31.Rongsriyam Y, Jitpakdi A, Choochote W, Somboon P, Tookyang B, Suwonkerd W. Comparative susceptibility of two forms of Anopheles sinensis Wiedemann 1828 (Diptera: Culicidae) to infection with Plasmodium falciparum, P. vivax, P. yoelii and the determination of misleading factor for sporozoite identification. Southeast Asian J Trop Med Public Health. 1998;29:159–167. [PubMed] [Google Scholar]
- 32.Lee VJ, Ow S, Heah H, Tan MY, Lam P, Ng LC, et al. Elimination of malaria risk through integrated combination strategies in a tropical military training island. Am J Trop Med Hyg. 2010;82:1024–1029. doi: 10.4269/ajtmh.2010.09-0562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rattanarithikul R, Harrison BA, Harbach RE, Panthusiri P, Coleman RE. Illustrated keys to the mosquitoes of Thailand IV. Anopheles. Southeast Asian J Trop Med Public Health. 2006;37(Suppl 2):1–128. [PubMed] [Google Scholar]
- 34.Reid JA. Anopheline mosquitoes of Malaya and Borneo. Stud Inst Med Res Malays. 1968;31:1–520. [Google Scholar]
- 35.Chan A, Chiang LP, Hapuarachchi HC, Tan CH, Pang SC, Lee R, et al. DNA barcoding: complementing morphological identification of mosquito species in Singapore. Parasit Vectors. 2014;7:569. doi: 10.1186/s13071-014-0569-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kumar NP, Rajavel AR, Natarajan R, Jambulingam P. DNA barcodes can distinguish species of Indian mosquitoes (Diptera: Culicidae) J Med Entomol. 2007;44(1):1–7. doi: 10.1093/jmedent/41.5.01. [DOI] [PubMed] [Google Scholar]
- 37.Makhawi AM, Liu XB, Yang SR, Liu QY. Genetic variations of ND5 gene of mtDNA in populations of Anopheles sinensis (Diptera: Culicidae) malaria vector in China. Parasit Vectors. 2013;6:290. doi: 10.1186/1756-3305-6-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thompson DJ, Higgins DG, Gibson TI. CLUSTAL W: improving the sensitivity of progressive multiple sequence alignment through sequence weighting, position-specific gap penalties and weight matrix choice. Nucleic Acids Res. 1994;22:4673–4680. doi: 10.1093/nar/22.22.4673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hall TA. BioEdit: a user-friendly biological sequence alignment editor and analysis program for Windows 95/98/NT. Nucleic Acids Symp Ser. 1999;41:95–98. [Google Scholar]
- 40.Tamura K, Stecher G, Peterson D, Filipski A, Kumar S. MEGA6: molecular evolutionary genetics analysis version 6.0. Mol Biol Evol. 2013;30(12):2725–2729. doi: 10.1093/molbev/mst197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lardeux F, Quispe V, Tejerina R, Rodriguez R, Torrez L, Bouchite B, Chavez T. Laboratory colonization of Anopheles pseudopunctipennis (Diptera: Culicidae) without force mating. Comptes Rendus Biol. 2007;330:571–575. doi: 10.1016/j.crvi.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 42.Moreno M, Tong C, Guzman M, Chuquiyauri R, Llanos-Cuentas A, Rodriguez H, et al. Infection of laboratory-colonized Anopheles darlingi mosquitoes by Plasmodium vivax. Am J Trop Med Hyg. 2014;90(4):612–616. doi: 10.4269/ajtmh.13-0708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Billker O, Shaw MK, Margos G, Sinden RE. The roles of temperature, pH and mosquito factors as triggers of male and female gametogenesis of Plasmodium berghei in vitro. Parasitology. 1997;115:1–7. doi: 10.1017/S0031182097008895. [DOI] [PubMed] [Google Scholar]
- 44.Andolina C, Landier J, Carrara V, Chu SC, Franetich JF, Roth A, et al. The suitability of laboratory-bred Anopheles cracens for the production of Plasmodium vivax sporozoites. Malar J. 2015;14:312. doi: 10.1186/s12936-015-0830-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Perandin F, Manca N, Calderaro A, Piccolo G, Galati L, Ricci L, et al. Development of a real-time PCR assay for detection of Plasmodium falciparum, Plasmodium vivax, Plasmodium ovale for routine clinical diagnosis. J Clin Microbiol. 2004;42:1214. doi: 10.1128/JCM.42.3.1214-1219.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Team RDC. R: a language and environment for statistical computing. Vienna: R Found Stat Comput; 2011. [Google Scholar]
- 47.Harbach RE. The classification of genus Anopheles (Diptera: Culicidae): a working hypothesis of phylogenetic relationships. Bull Entomol Res. 2004;94(6):537–553. doi: 10.1079/BER2004321. [DOI] [PubMed] [Google Scholar]
- 48.Mosquito Taxonomy Inventory. http://mosquito-taxonomy-inventory.info/. Accessed 22 Sept 2017.
- 49.Rašić G, Filipović I, Callahan AG, Stamford D, Chan A, Lam-Phua SG, Tan CH, Hoffman AA. The queenslandensis and the type form of the dengue fever mosquito (Aedes aegypti L.) are genomically indistinguishable. PLoS Negl Trop Dis. 2016;10(11):e0005096. doi: 10.1371/journal.pntd.0005096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Turner TL, Hahn MW, Nuzhdin SV. Genomic islands of speciation in Anopheles gambiae. PLoS Biol. 2005;3(9):e285. doi: 10.1371/journal.pbio.0030285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhu G, Xia H, Zhou H, Li J, Lu F, Liu Y, Cao J, Gao Q, Sattabongkot J. Susceptibility of Anopheles sinensis to Plasmodium vivax in malarial outbreak areas of central China. Parasit Vectors. 2013;6:176. doi: 10.1186/1756-3305-6-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Somboon P, Suwonkerd W, Lines JD. Susceptibility of Thai zoophilic Anophelines and suspected malaria vectors to local strains of human malaria parasites. Southeast Asian J Trop Med Public Health. 1994;25(4):766–770. [PubMed] [Google Scholar]
- 53.Lee HW, Cho SH, Shin EH, Lee JS, Chai JY, Lee SH, Kim TS. Experimental infection of Anopheles sinensis with Korean isolates of Plasmodium vivax. Korean J Parasitol. 2001;39(2):177–183. doi: 10.3347/kjp.2001.39.2.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Covell G. A critical review of the data recorded regarding the transmission of malaria by the different species of Anopheles; with notes on distribution, habitats and breeding-places. Indian J Med Res. 1927;7:1–117. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


