Abstract
Background
Several alternative mechanisms have been proposed to explain why some proteins are able to induce a TH2-biased and IgE-mediated immune response. These include specific interactions with receptors of the innate immune system, proteolytic activities, allergen-associated carbohydrate structures, and intrinsic structural determinants.
Objectives
Available data suggest that a fold-dependent allergy-promoting mechanism could be a driving force for the TH2-polarization activity of Bet v 1, the major birch pollen allergen.
Methods
Computer-aided sequence and fold analysis of the Bet v 1 family identified a short stretch susceptible for mutations inducing an altered fold of the entire molecule. With this knowledge, 7 consecutive amino acids of Bet v 1 were replaced with the homologous Mal d 1 sequence, creating the derivative BM4.
Results
The minimal changes of the sequence led to a loss of the Bet v 1–like fold and influenced the immunologic behavior. Compared to wild-type Bet v 1, BM4 induced elevated T-cell proliferation of human PBMCs. In the mouse model, immunization with Bet v 1 absorbed to aluminum hydroxide triggered strong TH2 polarization, whereas BM4 immunization additionally recruited TH1 cells. Furthermore, the fold variant BM4 showed enhanced uptake by dendritic cells and a decreased susceptibility to endo-/lysosomal proteolysis.
Conclusion
Modifications in the 3-dimensional structure of Bet v 1.0101 resulted in a change of its immunologic properties. We observed that the fold alteration led to a modified crosstalk with dendritic cells and a shift of the immune response polarization toward a mixed TH1/TH2 cytokine production.
Keywords: Protein remodeling, tree pollen allergens, Bet v 1 family, TH-cell polarization, IgE reactivity, allergenicity, antigen uptake, lysosomal degradation
Recently the search of inherent properties of allergens causing a TH2 immune polarization and the respective cytokine milieu led to the proposal of several alternative mechanisms of allergenicity. Interactions of allergens with receptors of the innate immune system, proteolytic activities, allergen-associated carbohydrate structures, and yet undefined intrinsic structural properties of allergens have been proposed as driving forces of allergenicity.1 In this context, the intrinsic structural properties of Bet v 1, the major birch pollen allergen, have been intensively investigated. The protein has been shown to be the main cause of spring pollinosis in the temperate climate zone of the northern hemisphere. In addition, a large panel of Bet v 1–homologous allergens has been identified and described in many Fagales pollens.2 Remarkably, only selected Bet v 1 isoforms seem to be accountable as main sensitizers and triggers of Fagales pollen allergies. Thus, recent studies focused on the comparison of immunogenicity as well as antigen uptake and processing of the high IgE-binding Bet v 1 isoform 0101 with the low IgE-binding isoform 0401. Despite an amino acid sequence identity of 95% and an almost identical tertiary structure, isoform Bet v 1.0401 was shown to induce a strong IgG but a moderate IgE immune response in a murine model, whereas Bet v 1.0101 induced high serum IgE titers and low IgG levels, a serologic status also reflected in patients with birch pollen allergy.3 With murine bone marrow–derived dendritic cells (BMDCs), Bet v 1.0401 was shown to be more efficiently taken up than isoform 0101, stimulated an increased activation of costimulatory molecules, and caused an increased activation of IFN-γ–producing T cells compared with Bet v 1.0101.4 Interestingly, the Bet v 1 homolog from celery, Api g 1, also showed this TH1 skewing of T cells cultured with antigen-loaded human monocyte-derived dendritic cells (DCs) isolated from patients with birch pollen allergy as well as healthy donors.5 Structural analysis of the Bet v 1 isoforms revealed that Bet v 1.0401 forms dimers via its single free cysteine, which is not present in isoform 0101. Therefore, the differences related to the decreased ability of Bet v 1.0401 to elicit an allergic immune response are probably a result of aggregate formation.4 Likewise, although not investigated in detail, a similar process of dimerization could be accountable for the TH1-polarizing mechanism of Api g 1, because the molecule also has a single free cysteine in its amino acid sequence. However, these observations do not explain the allergenic properties of Bet v 1.0101. Thus, we speculate that the fold of Bet v 1.0101 per se plays a role in the TH2 polarization. To test this hypothesis, we identified a sequence on the backbone of Bet v 1.0101 that is highly sensitive to mutations because amino acid exchanges lead to a change in fold stability of the entire protein. With this knowledge, a destabilizing sequence stretch from apple Mal d 1 was grafted onto the Bet v 1 backbone. The resulting mutant allergen, BM4, was unable to adopt the typical Bet v 1–like fold, as was demonstrated by the characterization of the molecule in terms of physicochemical properties, aggregation state, folding, and antibody binding. Furthermore, T-cell activation, interaction with antigen-presenting cells, and resistance to digestion by endo-/lysosomal proteases isolated from DCs revealed functional differences between the derivative and the wild-type (WT) molecule.
Methods
Patients and sera
Patients with Fagales pollen allergy were selected on the basis of case history, positive in vivo skin prick test, and in vitro IgE detection (CAP System; Phadia AB, Uppsala, Sweden). Patients with the IgE values greater than class 3 were selected. Experiments with blood samples from patients with pollen allergy were approved by the ethics committee of the Medical University and General Hospital of Vienna (no. EK028/2006). Informed written consent was obtained from all subjects included in the study.
Recombinant allergens
Recombinant Bet v 1.0101, termed Bet v 1 hereafter, was purchased from Biomay AG (Vienna, Austria). Endotoxin content was 1.09 ng/mg protein as determined by limulus amebocyte lysate (LAL) assay (Associates of Cape Cod, Inc, East Falmouth, Mass).
Cloning and expression of BM4
The Bet v 1 variant BM4 was generated by PCR amplification of mutated fragments of bet v 1.0101 (X15877) by using internal mismatch primers (see this article’s Table E1 in the Online Repository at www.jacionline.org) as described in the subsection on cloning of BM4 in this article’s Online Repository at www.jacionline.org. BM4 was cloned into a pET28b vector (Novagen; Merck KGaA, Darmstadt, Germany) by using NcoI and EcoRI restriction sites. Protein expression and purification was performed as described in the subsection on expression and purification of BM4 in this article’s Online Repository at www.jacionline.org. Endotoxin content was 1.18 ng/mg protein as determined by LAL assay (Associates of Cape Cod, Inc).
Physicochemical analysis of recombinant proteins
Purity of recombinant proteins was analyzed by SDS-PAGE, identity by amino acid analysis and mass spectrometry,6 secondary structure by circular dichroism, and homogeneity and aggregation behavior by dynamic light scattering (DLS) and online high-performance size exclusion chromatography light scattering.7 A brief description of these analyses is given in the subsection on physicochemical analysis of recombinant proteins in the Online Repository at www.jacionline.org. Shelf life and storage stability of recombinant allergens were tested in 5 mmol/L sodium phosphate pH 7.4 at 4°C and –20°C, respectively, for 30 days and analyzed by dynamic light scattering.
Fourier-transformed infrared spectroscopy
Infrared spectra of BM4 and Bet v 1 were recorded at 0.5 and 1.0 mg/mL, respectively, in 5 mmol/L sodium phosphate by using the Confocheck Fourier-transformed infrared (FTIR) system (Bruker Optics, Ettlingen, Germany) equipped with a mercury cadmium telluride detector.8 A description of the analysis is given in the subsection FTIR in the Online Repository at www.jacionline.org.
ELISA experiments
ELISA experiments using human serum samples in a 1:10 dilution were performed as described in the subsection ELISA experiments in this article’s Online Repository at www.jacionline.org.
Activation of basophils
The allergenic potential of BM4 was measured by rat basophilic leukemia (RBL) assay as previously described.9 Antigen-dependent β-hexosaminidase release into the supernatant was measured by enzymatic cleavage of the fluorogenic substrate 4-methyl umbelliferyl-N-acetyl-β-glucosaminide and expressed as a percentage of total enzyme content of Triton X-100–treated cells. Direct activation of human basophils from donors with birch pollen allergy was determined by upregulation of CD63 surface expression. Basophils from donors with allergy were stimulated with titrated concentrations of the proteins. Samples were stained with BD FastImmune CD63/CD123/anti–HLA-DR reagent (BD Biosciences, Franklin Lakes, NJ). Basophils were selected as CD123high, side scatterlow, and HLA-DRlow leukocytes, and CD63 upregulation was assessed in a minimum of 500 basophils per assay.10
T-cell proliferation assays
PBMCs obtained from donors with birch pollen allergy were stimulated with increasing concentrations of antigens as previously described.11 The stimulation index (SI) was calculated as a ratio between counts per minute obtained in cultures with T cells plus autologous antigen-presenting cells plus allergen and counts per minute obtained in cultures containing T cells and antigen-presenting cells.
Animal experiments
Female BALB/c mice (Charles River Laboratories, Wilmington, Mass) were purchased at 8 to 10 weeks of age and used for experiments 4 days after arrival. All experiments including immunizations, ELISAs, and ELISPOT assays were performed at the same time. Animals were injected subcutaneously with 5 μg antigen adsorbed to Alugel-S (Serva, Heidelberg, Germany) given as two 50-μL subcutaneous injections administered bilaterally in the lumbar region and boosted on days 14, 21, and 42. Sera were collected on days 0, 21, 49, and 180. Per group, 8 animals were tested. Serum IgG1, IgG2a, and IgE was analyzed by ELISA as described.4 Antigen-specific IL-2, IL-4, IL-5, IL-10, or IFN-γ–secreting splenic lymphocytes were analyzed by ELISPOT assay using matched-pair mAbs for IL-2, IL-4, IL-5, IL-10, or IFN-γ detection, respectively.12 All animal experiments were conducted according to national guidelines approved by the Austrian Ministry of Science (BMWF-66.012/0011-II/10b/2010).
In vitro antigen uptake
Bone-marrow derived DCs from BALB/c mice were harvested from culture at day 7. A total of 2 × 105 BMDCs were loaded with 1.5 μg/mL of Bet v 1–fluorescein isothiocyanate (FITC), Bet v 1–pHrodo (pHrodo succinimidyl ester; Invitrogen Corp, Carlsbad, Calif), BM4-FITC, or BM4-pHrodo. Cells were incubated in RPMI supplemented with 10% FBS (Gibco; Invitrogen Corp), 2 mmol/L L-glutamine, 100 U/mL penicillin, 0.1 mg/mL streptomycin (PAA Laboratories GmbH, Pasching, Austria), and 10 ng/mL GM-CSF (PeproTech GmbH, Hamburg, Germany) for the indicated time points at 37°C before labeling with specific antibodies against CD86 (clone: GL1), CD11c (clone: HL3) or matching isotype controls (all from BD Biosciences). Flow cytometric assays were performed on a FACS Canto II (BD Biosciences) and analyzed by using FlowJo software (FlowJo 8.8; Tree Star, Inc, Ashland, Ore).4
Endo-/lysosomal degradation assays
BMDCs were homogenized in 10 mmol/L TRIS acetate pH 7, 250 mmol/L sucrose, and microsomes were isolated by ultracentrifugation.13 Antigens (5 μg) were digested with microsomal/endo-/lysosomal enzymes (7 μg) in 100 mmol/L citrate buffer pH 4.8, 2 mmol/L dithiothreitol, at 37°C. Reactions were stopped by heat denaturation and analyzed by SDS-PAGE and mass spectrometry using an ESI-QTOF mass spectrometer fitted with a capillary reversed phase HPLC (Waters Corp, Milford, Mass).
Statistical analysis
Statistical evaluations were calculated with the Student t test. A value of P < .05 was considered statistically significant.
Results
Generation of the Bet v 1 variant BM4 by epitope grafting
In silico mutagenesis and calculation of z scores of Bet v 1 revealed that replacement of leucine 114 by lysine destabilizes the structure of the allergen.14 In addition, the amino acid position 112 has already been identified as susceptible for structural changes not only in Bet v 1 but also in homologous food allergens from apple, peach, cherry, and carrot.15–18 The side chains of the residues 112 and 114, respectively, are orientated toward the core of the hydrophobic cavity; thus, exchanges of these residues may interfere with the formation of this motif. However, the introduction of the point mutation L114K induced the formation of high-molecular-weight aggregates (data not shown). We speculated that this was in part a result of negative influences of adjacent residues present in Bet v 1. To amend this effect, we decided to embed the lysine residue in a naturally evolved environment, which we found in the Bet v 1 homolog from apple. Apple Mal d 1 is 1 amino acid shorter than Bet v 1, containing a gap located at position 118 of the Bet v 1 sequence, which results in a shift of K115 of Bet v 1 to position 114 of Mal d 1. Thus, we selected the Mal d 1 sequence 109 to 115 for the transplantation onto the Bet v 1 backbone. The resulting chimeric protein was designated BM4 (see this article’s Fig E1 in the Online Repository at www.jacionline.org). The recombinant allergen was cloned, expressed in Escherichia coli, and purified to homogeneity yielding 40 to 100 mg per liter of culture depending on the cell density at the time of harvest.
BM4 lacks the Bet v 1–like fold
Circular dichroism (Fig 1, A) and FTIR (Fig 1, B) spectroscopy were used to investigate the secondary structure of BM4. In contrast with Bet v 1, pronounced levels of unordered structural elements, indicated by the strong negative peak of the circular dichroism signal at 200 nm, were visible in the spectrum of BM4 at 20°C. On the basis of the FTIR spectra, we found that the content of 29.4% α-helices and 38.7% β-sheets in WT Bet v 1 was reduced to 9.9% α-helices and 17.7% β-sheets in BM4. These secondary structure changes directly affected the ligand-binding activity of BM4. The inner core of folded Bet v 1 is traversed by a solvent-accessible, hydrophobic cavity harboring binding sites for a wide variety of ligands.19 One of those is 8-anilino-1-naphtalene sulfonic acid (ANS), an essentially nonfluorescent compound displaying fluorescence when attached to hydrophobic areas of proteins. Fluorescence spectroscopy revealed that Bet v 1 but not BM4 was capable of binding ANS (see this article’s Fig E2 in the Online Repository at www. jacionline.org). Taken together, the results demonstrated that the Bet v 1 cavity—either blocked or collapsed—appears no longer accessible for small-molecular-weight ligands in BM4.
Fig 1.
A, Circular dichroism spectra of Bet v 1 and BM4 at 20°C. Spectra are baseline corrected and presented as mean residue molar ellipticity. deg, Degree; MRW, mean residue weight. B, The FTIR spectra of Bet v 1 and BM4 are presented as second derivatives. Typical regions of secondary structure elements are highlighted (α-helix, blue; intramolecular β-sheet, red; intermolecular β-sheet, green).
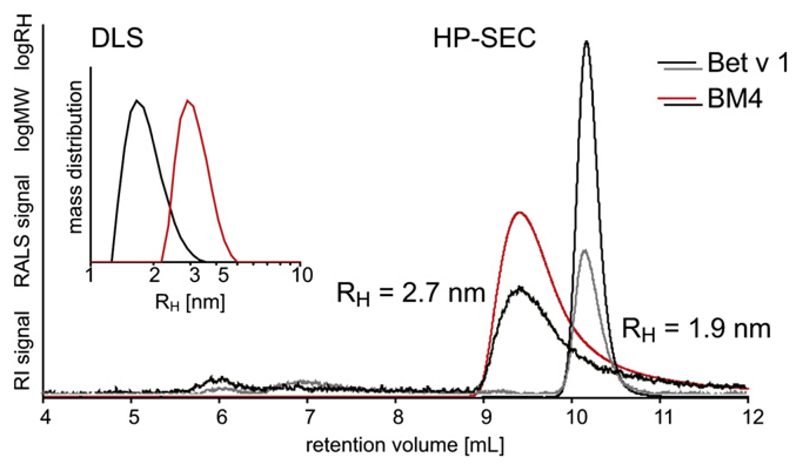
BM4 does not form oligomers or high-molecular-weight aggregates
To determine the aggregation behavior of BM4 in solution, DLS and High-Performance Size-Exclusion Chromatography (HPSEC) light scattering experiments were performed (Fig 2). The protein was analyzed in PBS at 24°C and in tissue culture medium at 37°C, and results were compared with Bet v 1. BM4 and Bet v 1 showed a hydrodynamic radius of 3.0 and 2.1 nm in DLS and 2.7 and 1.9 in HPSEC, respectively. Thus, both proteins were found to be monomeric to at least 99% at these measurement conditions. According to the crystal structure of Bet v 1 (1BV1), the protein has a globular shape, which was reflected by the hydrodynamic radius of approximately 2 nm. Therefore, the increased radius of BM4 might be interpreted as a more ellipsoid shape of the molecule. With the methods applied for structural characterization of BM4, it cannot be excluded that 0.1% to 1% of BM4 molecules show a Bet v 1–like fold, whereas the remaining 99% to 99.9% represent the fold variation. However, we were able to produce 3 structurally identical batches of BM4, which is considered a strong demonstration of the reproducibility and homogeneity of the recombinant protein.
Fig 2.
Aggregation behavior of Bet v 1 and BM4 were analyzed by DLS (small panel) and gel filtration (large panel). Hydrodynamic radius and molecular weight of both proteins were determined by light scattering. HP-SEC, High performance-size exclusion chromatography; MW, molecular weight; RALS, Right-angle light scattering; RH, hydrodynamic radius; RI, refractive index.
Fold changes of BM4 affect antibody binding
A reduction of IgE binding capacity of Bet v 1 from 1.16 ± 0.42 units to 0.02 ± 0.02 units (P <.001) for the fold variant BM4 was measured in direct ELISA. The reduced IgE binding of BM4 was verified by basophil activation by using either the RBL assay or freshly isolated human peripheral blood basophils from donors with Bet v 1 allergy (see this article’s Fig E3 in the Online Repository at www.jacionline.org). A total of 0.19 ± 0.19 ng/mL Bet v 1 compared with 6.46 ± 4.89 ng/mL BM4 (P <.05) was necessary to trigger 50% release of inflammatory mediators in RBL cells. In the basophil activation test, 0.06 ± 0.04 ng/mL Bet v 1 compared with 3.33 ± 2.13 ng/mL BM4 (P < .01) was required to obtain half-maximal activation.
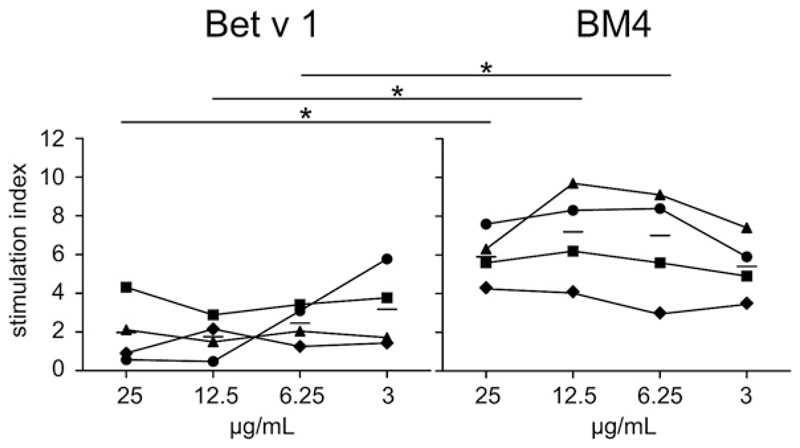
BM4 elicits strong T-cell proliferation
PBMCs isolated from donors with birch pollen allergy were stimulated with titrated concentrations of Bet v 1 and BM4. Proliferative responses were significantly more pronounced in response to BM4 (ie, mean SI at a concentration of 12.5 μg/mL = 7.1) than Bet v 1 (ie, mean SI at a concentration of 12.5 μg/mL = 1.8) at 3 of 4 concentrations determined (concentration range, 3-25 μg/mL; Fig 3).
Fig 3.
Proliferative responses of PBMCs from donors with birch pollen allergy stimulated with increasing amounts of Bet v 1 or BM4. Symbols represent individual patients, bars medians. P values were calculated by paired-sample t test (*P < .05).
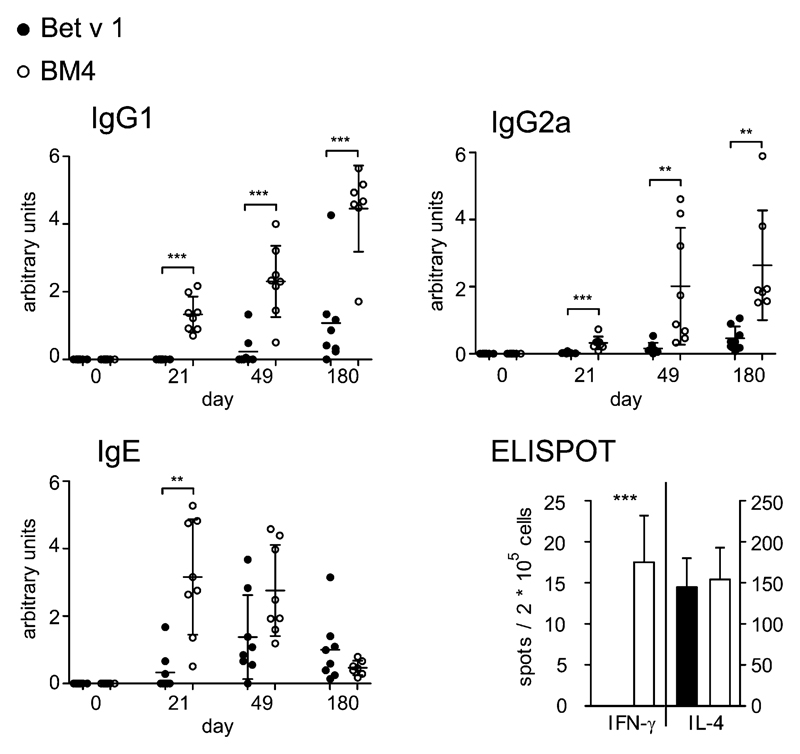
Immunization with BM4 recruits both TH2 and TH1 cells in BALB/c mice
To compare the immune responses induced by BM4 and Bet v 1, we first analyzed the Bet v 1–specific antibody responses of animals immunized with either antigen adsorbed to aluminum hydroxide (ALUM) at different time points (0, 21, 49, and 180 days). At all time points after sensitization, BM4 induced significantly higher levels of Bet v 1–specific IgG1 and IgG2a (Fig 4). Immunization with BM4 also induced Bet v 1–specific IgE antibodies. In contrast with Bet v 1, the BM4-induced IgG response exceeded the IgE response by several orders of magnitude. As proof that the altered fold of BM4 is responsible for the different immunologic behavior, a batch of the folded hypoallergenic Bet v 1.0101 derivative A1-620 was produced as recombinant protein as described in the subsection recombinant production of A1-6 in this article’s Online Repository at www.jacionline.org, characterized physico-chemically,21 and used for an animal study to investigate the humoral as well as cellular immune responses. The low IgE-binding molecule A1-6 showed the circular dichroism spectrum of folded Bet v 1, a hydrodynamic radius of 2.0 nm, which resembles the radius of WT Bet v 1, and was found to be monomeric to more than 99%. Similar to Bet v 1, A1-6 was not able to trigger increased production of IgG1, or IgG2a antibodies, but elicited high levels of IgE antibodies in mice (see this article’s Fig E4 in the Online Repository at www.jacionline.org). Evaluation of splenocytes from immunized animals in ELISPOT assays showed that immunization with Bet v 1, A1-6, and BM4 induced IL-2, IL-4, IL-5, and no IL-10–secreting T cells. The IL-4 immune response against the 3 antigens was comparable; however, IL-2 and IL-5 production was significantly elevated in A1-6–immunized mice compared with Bet v 1 and BM4, whereas Bet v 1 immunizations stimulated the lowest levels of both cytokine-secreting T-cell subpopulations. Of note, only BM4 immunizations induced IFN-γ–producing cells (Fig 4; see this article’s Fig E5 in the Online Repository at www.jacionline.org). These findings indicate that in mice, a mixed TH1/TH2 immune response is elicited against the fold variant BM4 compared with a clear TH2-driven response against Bet v 1 or the folded hypoallergenic mutant A1-6.
Fig 4.
A, BALB/c mice were immunized 4 times with either Bet v 1 (filled circles) or BM4 (open circles; n = 8 per group). Bet v 1–specific antibody levels were determined by ELISA. B, ELISPOT analysis of splenocytes from immunized animals expressed as mean cytokine-secreting cells per 105 spleen cells ± SEM. P values were calculated with t tests (**P < .01; ***P < .001).
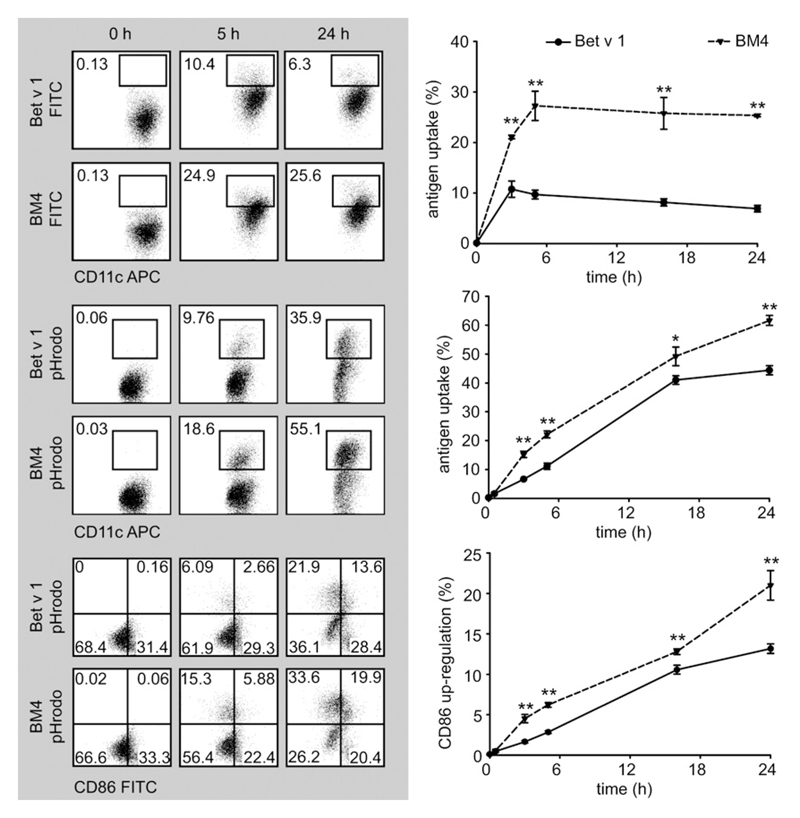
Pattern of BM4 uptake leads to efficient activation of DCs
To understand better the different T-cell and B-cell responses elicited by BM4, murine BMDCs were pulsed at defined time points with antigens labeled with either FITC or pHrodo. FITC is an indicator for attachment of antigens to the cell surface and antigen uptake. pHrodo, a pH-sensitive dye showing increased fluorescence at acidic pH, has been used to track antigen internalization. Uptake rates of CD11c+ cells and the upregulation of the costimulatory molecule CD86 were determined by flow cytometry (Fig 5). At early time points, Bet v 1–FITC and BM4-FITC were attached and taken up equally well into BMDCs. However, after 5 hours, 11% of Bet v 1 versus 21% of BM4 (P < .01) was bound or internalized by the cells. After 16 hours, this ratio was 8% Bet v 1 versus 26% BM4 (P < .01), and at 24 hours, the ratio was 7% Bet v 1 versus 25% BM4 (P < .01). Between 3 and 24 hours, significantly more (3 hours, 7% vs 15%, P < .01; 5 hours, 11% vs 22%, P < .01; 16 hours, 41% vs 49%, P < .05; 24 hours, 44% vs 62%, P < .01) BM4-pHrodo than Bet v 1–pHrodo was taken up by the DCs. Further, upregulation of CD86 was significantly increased for BM4-stimulated cells (Bet v 1 vs BM4 after 3 hours, 1.6% vs 4.5%, P < .01; 5 hours, 2.8% vs 6.2%, P < .01; 16 hours, 10.5% vs 12.8%, P < .05; 24 hours, 13.2% vs 24%, P < .01).
Fig 5.
BMDCs were pulsed with FITC or pHrodo-labeled Bet v 1 or BM4, stained for CD11c and CD86, and gated for CD11c expression. Representative fluorescence-activated cell-sorting profiles of 6 experiments per time point and antigen are shown. Numbers in the panels represent percentage values of analyzed cells (left panel). A time course analysis is presented as a line chart ± SEM (right panel). P values were calculated with t tests (*P < .05; **P < .01).
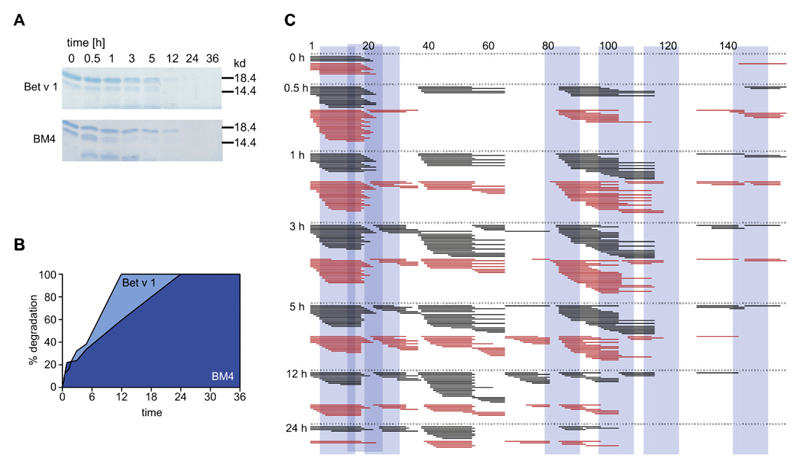
BM4 shows reduced susceptibility to endo-/lysosomal proteolysis
Previous studies demonstrated that antigens prone to rapid lysosomal degradation represent weak immunogens, whereas a certain resistance toward proteolysis enhances immunogenicity. Therefore, we subjected Bet v 1 and BM4 to degradation by microsomal proteases isolated from murine BMDCs. Proteolytic degradation monitored by gel electrophoresis at defined intervals revealed that 100% degradation of Bet v 1 occurred after 12 hours, compared with 24 hours for BM4, indicating an increased proteolytic resistance of the fold variant (Fig 6, A and B, respectively). Tandem mass spectrometry analysis of the peptides obtained by in vitro endo-/lysosomal degradation showed almost identical degradation patterns for BM4 and Bet v 1—for example, immunodominant peptide clusters in the regions aa 4-30, 79-123, and 142-153 are in accordance with published major T-cell epitopes of Bet v 122 (Fig 6, C).
Fig 6.
A, SDS-PAGE analysis of time-dependent endo-/lysosomal degradation of Bet v 1 and BM4. B, Percent degradation was determined densitometrically from SDS-PAGE bands and is presented as a line chart. C, Proteolytic fragments of Bet v 1 (black lines) or BM4 (red lines) were analyzed by mass spectrometry. Dominant T cell epitopes of Bet v 1 are indicated by vertical blue bars.
Discussion
Natural Bet v 1 is composed of a complex mixture of different isoforms showing high amino acid sequence identities (approximately 95%). However, striking differences were observed in their allergenic as well as immunogenic potentials. For example, Bet v 1.0101, formerly designated Bet v 1a, has been identified as the major component (more than 50%) of natural Bet v 1, whereas Bet v 1.0401, also known as Bet v 1d, accounts for approximately 10%.23 Because of their remarkably different allergenic behavior—strong IgE binding and weak T-cell reactivity for Bet v 1.0101 versus weaker IgE binding but elevated T-cell reactivity for Bet v 1.0401—both molecules have been extensively studied to understand the underlying mechanisms.24,25 For Bet v 1.0401, dimerization has been reported as a crucial mechanism for an altered crosstalk of the allergen, with the immune system leading to its weakened allergenic potential.4 However, this does not explain the high allergenicity of Bet v 1.0101. We speculate that the Bet v 1.0101 fold may be the crucial attribute causing the protein to become allergenic. To test the hypothesis, we generated the Bet v 1 derivative BM4, which is based on structural remodeling of Bet v 1.0101. The resulting molecule showed a reduction in both α-helical and β-sheet motifs compared with WT Bet v 1, accompanied by an increase in its hydrodynamic radius, suggesting a rodlike overall shape. This rendered the Bet v 1 cavity, present in-all folded members of the Bet v 1 family,19 inaccessible. Still, BM4 does not form aggregates. Three production batches of BM4 were analyzed concerning structural properties and aggregation behavior by using FTIR and DLS, respectively, and all batches showed identical behavior (data not shown), indicating the stability of the engineered Bet v 1 fold. The fold alteration also resulted in the loss of human IgE binding and mediator releasing capacity of BM4; however, the molecule retained the ability to stimulate Bet v 1–specific T cells.
Immunizations of BALB/c mice with ALUM-adsorbed BM4 resulted in significant production of IgG1, IgG2a, and IgE antibodies, which were cross-reactive with the WT molecule. Both kinetics and antibody concentrations were elevated compared with the immune response against Bet v 1. However, the BM4-induced IgG response exceeded the IgE response by several orders of magnitude, whereas in Bet v 1–immunized animals, this was not observed. Of note, BM4-induced IgG antibodies were even able to block human serum IgE binding to Bet v 1, as demonstrated in this article’s Fig E6 in the Online Repository at www.jacionline.org. Despite the TH2-polarizing effect of ALUM as adjuvant, analysis of murine splenocytes revealed the induction of TH1 cells producing IFN-γ in the BM4, but not Bet v 1 group. This TH1 component of the immune response to BM4 is reflected by the substantial amount of IgG2a in the serum and by a clearly increased IgG to IgE ratio. In addition, we were able to demonstrate that the observed in vivo immune response against BM4 was fold-dependent by using the hypoallergenic Bet v 1 derivative A1-6 as a control in our experiments. The mutant has a secondary structure similar to WT Bet v 1 and does not form aggregates. In fact, A1-6 elicited a strong TH2-biased immune response at the humoral as well as the cellular level, which was demonstrated by high levels of Bet v 1–specific IgE antibodies and a substantial amount of IL-2, IL-4, and IL-5–producing T cells accompanied by the absence of IFN-γ–producing cells.
To shed some light on the mechanisms of the BM4 interaction with the immune system, BMDCs were pulsed with labeled antigens to study antigen uptake. BM4 uptake into the dendritic endosomes was faster and more efficient and was accompanied by an increased upregulation of CD86 costimulatory molecules compared with the uptake of Bet v 1. Analysis of the endo-/lysosomal degradation pattern in vitro revealed a decreased susceptibility of BM4 toward proteolytic digestion, which has previously been shown to correlate positively with immunogenicity.13 No changes could be observed with respect to the peptide patterns generated by endo-/lysosomal degradation of BM4.
The data indicate that the altered structure of BM4 might be responsible for an increased uptake- as well as activation-rate of BMDCs. Obviously, changing of the Bet v 1 fold modified the communication of the molecule with DCs and induced a partial shift of the immune polarization by the recruitment of TH1 cells. At present, the nature of this polarizing stimulus remains speculative. It has been described that a weak MHC II signal at the immunologic synapse correlates with a TH2 immune response, which might explain the decreased TH2-polarizing capacity of the proteolytically more stable BM4.26 Given the fact that pollen allergens arrive at a very low dose via the airways (low microgram amounts per year),26,27 and that these allergens are delivered in combination with pollen-derived TH2 polarizing factors, such as lipid mediators, enzymes that can generate reactive oxygen intermediates, and proteases, which facilitate the allergen entry via tight junction degradation, the intrinsic weak interaction of allergens (low uptake rates, proteolytic instability) with DCs might be another driving factor in the development of an allergic disease.1,26,28
Beyond that, the fold-induced modified immunologic behavior of BM4 in combination with its excellent production yields, batch-to-batch reproducibility, good stability, and drastically reduced patient IgE binding shows the high potential of the molecule as a vaccine candidate. The data on the interplay of BM4 with DCs encourages clinical application and might serve as a milestone for designing new vaccine candidates, especially because it points out possibilities of how to address not only the B-cell but also the antigen-presenting cell and the T-cell compartments in rational vaccine design.
Supplementary Material
Clinical implications.
The rationally designed Bet v 1 fold variant BM4 evinces a modified interplay with DCs, resulting in a shifted TH1/TH2 polarization, thus opening new possibilities for allergy vaccine conception.
Acknowledgments
We thank Drs Rob Aalberse, Chrisof Ebner, Matthias Egger, Gabriele Gadermaier, Peter Hammerl, Peter Lackner, Adriano Mari, Rudolf Valenta, Nicole Wopfner, and Laurian Zuidmeer for their support in characterization and immunologic evaluation of BM4.
Supported by the Christian Doppler Research Association, Austria; Biomay AG, Vienna, Austria; Austrian Science Fund (FWF) Project L688; and Jubiläumsfondsproject 12533 of the Austrian National Bank, Austria.
Abbreviations used
- ALUM
Aluminum hydroxide
- ANS
8-Anilino-1-naphtalene sulfonic acid
- APC
Allophycocyanin
- BMDC
Bone marrow–derived dendritic cell
- DC
Dendritic cell
- DLS
Dynamic light scattering
- FITC
Fluorescein isothiocyanate
- FTIR
Fourier-transformed infrared
- LAL
Limulus amebocyte lysate
- RBL
Rat basophilic leukemia
- SI
Stimulation index
- WT
Wild-type
Footnotes
Disclosure of potential conflict of interest: M. Hauser receives research support from CK-Care AG, Switzerland. M. Himly receives research support from the Austrian Science Fund, Biomay AG, and the Austrian Research Promotion Agency. R. van Ree is a consultant for and receives research support from HAL Allergy BV. J. Thalhamer has consultant arrangements with Biomay AG and receives research support from Biomay AG, Christian Doppler Forschungsgesellschaft, and the Austrian Science Fund. B. Bohle receives research support from the Austrian Science Fund and Christian Doppler Forschungsgesellschaft. F. Ferreira receives research support from Biomay AG, the Austrian Science Fund, the Christian Doppler Research Association, and the European Union and has provided consultation for the AllergenOnline Database. The rest of the authors have declared that they have no conflict of interest.
References
- 1.Wills-Karp M, Nathan A, Page K, Karp CL. New insights into innate immune mechanisms underlying allergenicity. Mucosal Immunol. 2010;3:104–10. doi: 10.1038/mi.2009.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mothes N, Horak F, Valenta R. Transition from a botanical to a molecular classification in tree pollen allergy: implications for diagnosis and therapy. Int Arch Allergy Immunol. 2004;135:357–73. doi: 10.1159/000082332. [DOI] [PubMed] [Google Scholar]
- 3.Wagner S, Radauer C, Bublin M, Hoffmann-Sommergruber K, Kopp T, Greisenegger EK, et al. Naturally occurring hypoallergenic Bet v 1 isoforms fail to induce IgE responses in individuals with birch pollen allergy. J Allergy Clin Immunol. 2008;121:246–52. doi: 10.1016/j.jaci.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 4.Zaborsky N, Brunner M, Wallner M, Himly M, Karl T, Schwarzenbacher R, et al. Antigen aggregation decides the fate of the allergic immune response. J Immunol. 2010;184:725–35. doi: 10.4049/jimmunol.0902080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smole U, Wagner S, Balazs N, Radauer C, Bublin M, Allmaier G, et al. Bet v 1 and its homologous food allergen Api g 1 stimulate dendritic cells from birch pollen-allergic individuals to induce different Th-cell polarization. Allergy. 2010;65:1388–96. doi: 10.1111/j.1398-9995.2010.02407.x. [DOI] [PubMed] [Google Scholar]
- 6.van Ree R, Chapman MD, Ferreira F, Vieths S, Bryan D, Cromwell O, et al. The CREATE project: development of certified reference materials for allergenic products and validation of methods for their quantification. Allergy. 2008;63:310–26. doi: 10.1111/j.1398-9995.2007.01612.x. [DOI] [PubMed] [Google Scholar]
- 7.Himly M, Nony E, Chabre H, Van Overtvelt L, Neubauer A, van Ree R, et al. Standardization of allergen products, 1: detailed characterization of GMP-produced recombinant Bet v 1.0101 as biological reference preparation. Allergy. 2009;64:1038–45. doi: 10.1111/j.1398-9995.2009.01957.x. [DOI] [PubMed] [Google Scholar]
- 8.Oberg KA, Ruysschaert JM, Goormaghtigh E. The optimization of protein secondary structure determination with infrared and circular dichroism spectra. Eur J Biochem. 2004;271:2937–48. doi: 10.1111/j.1432-1033.2004.04220.x. [DOI] [PubMed] [Google Scholar]
- 9.Vogel L, Luttkopf D, Hatahet L, Haustein D, Vieths S. Development of a functional in vitro assay as a novel tool for the standardization of allergen extracts in the human system. Allergy. 2005;60:1021–8. doi: 10.1111/j.1398-9995.2005.00803.x. [DOI] [PubMed] [Google Scholar]
- 10.Gamboa PM, Sanz ML, Caballero MR, Antepara I, Urrutia I, Jauregui I, et al. Use of CD63 expression as a marker of in vitro basophil activation and leukotriene determination in metamizol allergic patients. Allergy. 2003;58:312–7. doi: 10.1034/j.1398-9995.2003.00096.x. [DOI] [PubMed] [Google Scholar]
- 11.Wallner M, Stocklinger A, Thalhamer T, Bohle B, Vogel L, Briza P, et al. Allergy multivaccines created by DNA shuffling of tree pollen allergens. J Allergy Clin Immunol. 2007;120:374–80. doi: 10.1016/j.jaci.2007.05.021. [DOI] [PubMed] [Google Scholar]
- 12.Bauer R, Scheiblhofer S, Kern K, Gruber C, Stepanoska T, Thalhamer T, et al. Generation of hypoallergenic DNA vaccines by forced ubiquitination: preventive and therapeutic effects in a mouse model of allergy. J Allergy Clin Immunol. 2006;118:269–76. doi: 10.1016/j.jaci.2006.03.033. [DOI] [PubMed] [Google Scholar]
- 13.Delamarre L, Pack M, Chang H, Mellman I, Trombetta ES. Differential lysosomal proteolysis in antigen-presenting cells determines antigen fate. Science. 2005;307:1630–4. doi: 10.1126/science.1108003. [DOI] [PubMed] [Google Scholar]
- 14.Thalhamer T, Dobias H, Stepanoska T, Proll M, Stutz H, Dissertori O, et al. Designing hypoallergenic derivatives for allergy treatment by means of in silico mutation and screening. J Allergy Clin Immunol. 2010;125:926–34. doi: 10.1016/j.jaci.2010.01.031. e10. [DOI] [PubMed] [Google Scholar]
- 15.Son DY, Scheurer S, Hoffmann A, Haustein D, Vieths S. Pollen-related food allergy: cloning and immunological analysis of isoforms and mutants of Mal d 1, the major apple allergen, and Bet v 1, the major birch pollen allergen. Eur J Nutr. 1999;38:201–15. doi: 10.1007/s003940050063. [DOI] [PubMed] [Google Scholar]
- 16.Scheurer S, Son DY, Boehm M, Karamloo F, Franke S, Hoffmann A, et al. Crossreactivity and epitope analysis of Pru a 1, the major cherry allergen. Mol Immunol. 1999;36:155–67. doi: 10.1016/s0161-5890(99)00033-4. [DOI] [PubMed] [Google Scholar]
- 17.Neudecker P, Lehmann K, Nerkamp J, Haase T, Wangorsch A, Fotisch K, et al. Mutational epitope analysis of Pru av 1 and Api g 1, the major allergens of cherry (Prunus avium) and celery (Apium graveolens): correlating IgE reactivity with three-dimensional structure. Biochem J. 2003;376:97–107. doi: 10.1042/BJ20031057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reese G, Ballmer-Weber BK, Wangorsch A, Randow S, Vieths S. Allergenicity and antigenicity of wild-type and mutant, monomeric, and dimeric carrot major allergen Dau c 1: destruction of conformation, not oligomerization, is the roadmap to save allergen vaccines. J Allergy Clin Immunol. 2007;119:944–51. doi: 10.1016/j.jaci.2006.11.699. [DOI] [PubMed] [Google Scholar]
- 19.Mogensen JE, Wimmer R, Larsen JN, Spangfort MD, Otzen DE. The major birch allergen, Bet v 1, shows affinity for a broad spectrum of physiological ligands. J Biol Chem. 2002;277:23684–92. doi: 10.1074/jbc.M202065200. [DOI] [PubMed] [Google Scholar]
- 20.Ferreira F, Ebner C, Kramer B, Casari G, Briza P, Kungl AJ. Modulation of IgE reactivity of allergens by site-directed mutagenesis: potential use of hypoallergenic variants for immunotherapy. FASEB J. 1998;12:231–42. doi: 10.1096/fasebj.12.2.231. [DOI] [PubMed] [Google Scholar]
- 21.Egger M, Hauser M, Himly M, Wopfner N, Wallner M, Ferreira F. Development of recombinant allergens for diagnosis and therapy. Front Biosci (Elite Ed) 2009;1:77–90. doi: 10.2741/E9. [DOI] [PubMed] [Google Scholar]
- 22.Mutschlechner S, Egger M, Briza P, Wallner M, Lackner P, Karle A, et al. Naturally processed T cell-activating peptides of the major birch pollen allergen. J Allergy Clin Immunol. 2010;125:711–8. doi: 10.1016/j.jaci.2009.10.052. 8 e1-8 e2. [DOI] [PubMed] [Google Scholar]
- 23.Swoboda I, Jilek A, Ferreira F, Engel E, Hoffmann-Sommergruber K, Scheiner O, et al. Isoforms of Bet v 1, the major birch pollen allergen, analyzed by liquid chromatography, mass spectrometry, and cDNA cloning. J Biol Chem. 1995;270:2607–13. doi: 10.1074/jbc.270.6.2607. [DOI] [PubMed] [Google Scholar]
- 24.Ferreira F, Hirtenlehner K, Jilek A, Godnik-Cvar J, Breiteneder H, Grimm R, et al. Dissection of immunoglobulin E and T lymphocyte reactivity of isoforms of the major birch pollen allergen Bet v 1: potential use of hypoallergenic isoforms for immunotherapy. J Exp Med. 1996;183:599–609. doi: 10.1084/jem.183.2.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wallner M, Himly M, Neubauer A, Erler A, Hauser M, Asam C, et al. The influence of recombinant production on the immunologic behavior of birch pollen isoallergens. PLoS One. 2009;4:e8457. doi: 10.1371/journal.pone.0008457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Constant S, Pfeiffer C, Woodard A, Pasqualini T, Bottomly K. Extent of T cell receptor ligation can determine the functional differentiation of naive CD4+ T cells. J Exp Med. 1995;182:1591–6. doi: 10.1084/jem.182.5.1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Martonen TB, Orourke MK. Deposition patterns of ragweed pollen in the human respiratory-tract. Grana. 1991;30:82–6. [Google Scholar]
- 28.Runswick S, Mitchell T, Davies P, Robinson C, Garrod DR. Pollen proteolytic enzymes degrade tight junctions. Respirology. 2007;12:834–42. doi: 10.1111/j.1440-1843.2007.01175.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.