Abstract
Background
A rapidly aging society needs effective approaches to support frail older people who have a high risk of requiring long‐term care. We investigated the validity of the Basic Checklist (the “Kihon Checklist”) as a tool to select candidates for a program to prevent long‐term care.
Method
A survey with questions from the Basic Checklist was conducted with functionally independent older residents aged ≥65 years living in Takasaki City, Japan. Subjects who completed the questionnaire were followed over 3 years for the presence or absence of certification for long‐term care requirement. We used multiple logistic regression analysis to calculate the odds ratio (OR) and 95% confidence interval (95%CI) for long‐term care requirement certification.
Results
A total of 21 325 subjects were analyzed. The odds ratio was the highest when items number one‐20 had a total of ≥10 checked answers (OR, 2.71; 95%CI, 2.22‐3.32). Physical function (OR, 2.29; 95%CI, 2.05‐2.55), nutritional condition (OR, 1.85; 95%CI, 1.38‐2.48), oral function (OR, 1.40; 95%CI, 1.25‐1.57), whether patients were elected as a care prevention program candidate (OR, 1.90; 95%CI, 1.73‐2.08), Homebound state (OR, 1.91; 95%CI, 1.55‐2.37), the presence of dementia (OR, 1.97; 95%CI, 1.75‐2.20), and depression (OR, 1.96; 95%CI, 1.73‐2.22) were associated with a higher odds ratio.
Conclusion
Individuals who were selected as long‐term care prevention program candidates based on the Basic Checklist had a higher risk of requiring long‐term care. Older residents who corresponded to 10 or more of the 20 Basic Checklist items are at the highest risk of becoming certified as needing long‐term care.
Keywords: long‐term care, the Basic Checklist, community‐dwelling older people, screening
1. INTRODUCTION
A rapidly aging society needs effective approaches to support frail older people who have a high risk of requiring long‐term care. Municipalities in Japan are required to provide long‐term care requirement certification based on the results of care screening carried out by the long‐term care approval board.1 According to the severity of their medical conditions, older people can be certified as requiring support (levels 1 and 2) or long‐term care (levels 1‐5).2 In 2006, the long‐term care insurance system was revised to increase prevention of long‐term care, and since then municipalities have implemented long‐term care prevention programs for frail older people who are at risk of requiring support or long‐term care.2
The Ministry of Health, Labour, and Welfare of Japan developed the Basic Checklist (the “Kihon Checklist”) as a screening test to accurately and efficiently identify frail older people who are at risk of requiring support or long‐term care,3 and municipalities throughout Japan use the Basic Checklist to select older people as candidates for long‐term care prevention programs. The Basic Checklist comprises seven domains: the instrumental activities of daily living (IADL), physical function, nutritional condition, oral function, homebound state, dementia, and depression. Each negative, care‐requiring response equals one point, and persons with higher scores are more likely to be frail. Based on the scores, municipalities invite frail older people to participate in long‐term care prevention programs, and adopt appropriate approaches for each candidate.
The Basic Checklist has been used as a tool to determine the effects of exercise intervention in a physical function improvement program,4, 5 to evaluate frail older people's physical functions,6 and to screen for dementia.7 The association of the checklist with the ability to perform the IADL8 and with the homebound state9 has also been investigated. However, limited cohort studies have investigated whether the selection of care prevention program candidates based on the checklist can accurately predict which persons will be certified as requiring long‐term care. Although previous studies have suggested that such individuals can be predicted by the checklist, follow‐up of study participants was relatively short.10, 11 Long‐term care prevention programs are effective whether frail older people participate in these programs early and continue their participation for an extended period of time. Municipalities can efficiently implement such programs through the early selection of older people who are deemed likely to be certified as requiring long‐term care.
Therefore, to verify the predictive validity of the Basic Checklist, long‐term monitoring of the long‐term care requirement certification status of older people who have completed the checklist is needed. The purpose of this study was to investigate how well the selection of care prevention program candidates based on the Basic Checklist can predict those who will be certified as requiring long‐term care within 3 years after completing the checklist.
2. METHODS
2.1. Subjects
A survey with questions from the Basic Checklist was conducted among older people who had a health checkup provided by the municipality to prevent lifestyle‐related diseases between April 2010 and March 2011. The health checkup targeted 69,755 residents of Takasaki City, Gunma Prefecture, who were aged ≥65 years and did not require long‐term care or support. All older people who completed the questionnaire served as the study subjects, and they were followed from the day of questionnaire completion until March 2014 for the presence or absence of certification for long‐term care requirement. The presence or absence and timing of long‐term care requirement certification were investigated based on the long‐term care certification data recorded by Takasaki City government. The date of being certified as requiring long‐term care or support by the Review Board for Long‐term Care Certification was regarded as the time of requiring long‐term care. Older people who died or became exempt from the long‐term care insurance system of Takasaki City, for reasons such as moving out of the city, without being certified as requiring long‐term care, and people who were certified before March 2011 were excluded from the analyses.The Medical Ethics Committee of Gunma University approved this study (26‐19).
2.2. Summary of the basic checklist
The Basic Checklist comprises seven domains with 25 items (Table 1): (i) the IADL (five items [Number 1‐5]), (ii) physical function mainly to assess the risk of falls (five items [Number 6‐10]), (iii) nutritional condition (two items [Number 11‐12]), (iv) oral functions (three items [Number 13‐15]), mainly chewing and swallowing functions, (v) homebound state (two items [Number 16‐17]), (vi) dementia (three items [Number 18‐20]), and (vii) depression (five items [Number 21‐25]). Subjects answer was “yes” or “no” for each item, and each negative, care‐requiring response equals one point. Those with higher scores are more likely to be frail. If a subject meets any of the following four criteria; checked more than 10 of the items (Number 1‐20), checked ≥3 answers for the domain of physical function, checked answers for both items of the nutritional condition, or checked ≥2 answers for the oral function, they are selected as long‐term care prevention program candidates (Table 2). If a selected candidate meets the criteria for any of the following domains, they are also advised to attend additional programs; physical function improvement and dementia prevention programs: a checked answer for item Number 16 (homebound state), ≥1 checked answer for dementia, or checked ≥2 answers for depression (Table 2).
Table 1.
Items of the basic checklist
| No. | Itemsa | Answers | |
|---|---|---|---|
| 1 | I usually take the bus or train when going out. | 0. Yes | 1. No |
| 2 | I usually buy daily necessities myself. | 0. Yes | 1. No |
| 3 | I usually withdraw and deposit money myself. | 0. Yes | 1. No |
| 4 | I regularly visit my friends. | 0. Yes | 1. No |
| 5 | I sometimes give advice to my family members and friends. | 0. Yes | 1. No |
| 6 | I usually go upstairs without touching the handrail or wall. | 0. Yes | 1. No |
| 7 | I usually stand up from a sitting position without needing to hold onto anything. | 0. Yes | 1. No |
| 8 | I walk for about 15 min without stopping every day. | 0. Yes | 1. No |
| 9 | I fell over last year. | 1. Yes | 0. No |
| 10 | I am seriously concerned about falling. | 1. Yes | 0. No |
| 11 | I have experienced weight loss of 2‐3 kg over the last 6 mo. | 1. Yes | 0. No |
| 12 | Height (cm) weight (kg) *The answer “Yes” applies to the subject if his/her BMI is less than 18.5. | 1. Yes | 0. No |
| 13 | It is more difficult to eat solid food now compared to 6 mo ago. | 1. Yes | 0. No |
| 14 | I sometimes choke when drinking something, such as tea or soup. | 1. Yes | 0. No |
| 15 | I am concerned about my dry mouth. | 1. Yes | 0. No |
| 16 | I go out at least once a week. | 0. Yes | 1. No |
| 17 | I go out less this year than last year. | 1. Yes | 0. No |
| 18 | People I know say that I ask the same things repeatedly, or I am forgetful. | 1. Yes | 0. No |
| 19 | If I want to call someone, but do not know the person's phone number, I look up the number myself. | 0. Yes | 1. No |
| 20 | I sometimes lose track of the date. | 1. Yes | 0. No |
| 21 | My life has not been fulfilling over the past 2 wk. | 1. Yes | 0. No |
| 22 | For the past 2 wk, I have been unable to enjoy things that were enjoyable before. | 1. Yes | 0. No |
| 23 | For the past 2 wk, I have been reluctant to do things that I could do easily before. | 1. Yes | 0. No |
| 24 | For the past 2 wk, I have felt like I am a useless person. | 1. Yes | 0. No |
| 25 | For the past 2 wk, I have felt fatigue for no reason. | 1. Yes | 0. No |
Number 1‐5: instrumental activities of daily living, number 6‐10: physical function, number 11‐12: nutritional condition, number 13‐15: oral function, number 16‐17: homebound state, number 18‐20: dementia, and number 21‐25: depression.
Table 2.
Basic checklist's criteria to make selections in each domain
| Domains of the Basic Checklist | Criteria to make selections |
|---|---|
| (1) Items number 1‐20 | ≥10 checked answers |
| (2) Physical function (items number 6‐10) | ≥3 checked answers |
| (3) Nutritional condition (items number 11‐12) | Checked answers for both items |
| (4) Oral function (items number 13‐15) | ≥2 checked answers |
| (5) Selected as a care prevention program candidate | If the subject meets any of the criteria mentioned in (1)‐(4), he/she will be selected as a care prevention program candidate. |
| (6) Homebound state (items number 16‐17)a | (5) plus item number 16 applies to him/her. |
| (7) Dementia (items number 18‐20)a | (5) plus the subject has ≥1 checked answer for the domain of dementia. |
| (8) Depression (items number 21‐25)a | (5) plus the subject has ≥2 checked answers for the domain of depression. |
If the care prevention program candidate meets any of the criteria mentioned in (6)‐(8), he/she will be judged as requiring specialized support covering the domain.
2.3. Analyses
We divided subjects into those who were and were not classified as requiring long‐term care during study follow‐up to compare the variable distribution between the groups. Chi‐square tests were used to analyze the categorical variables, and Mann‐Whitney‘s U test was used for the ordinal and nonparametric variables.
We used multiple logistic regression to calculate the odds ratio (OR), 95% confidence interval (CI), chi‐square goodness of fit (χ2GF), and percentage of correct classifications (%CC) for long‐term care requirement certification between care prevention program candidates and noncandidates who were identified based on the Basic Checklist and between individuals who met the criteria for recommended participation in additional care prevention programs, and those who did not. The following factors were used for analyses: age; gender (male: 1, female: 0); the presence or absence of ≥10 checked answers for the first 20 items; [Items number. 1‐20, ≥10 checked answers] (Yes: 1, No: 0); the presence or absence of ≥3 checked answers for the domain of physical function [Physical function] (Yes: 1, No: 0); whether both items of nutritional condition apply to the subject [Nutritional condition] (Yes: 1, No: 0); whether ≥2 answers were checked for the domain of oral function [Oral function] (Yes: 1, No: 0); whether the subject has been selected as a care prevention program candidate based on the above‐mentioned criteria [Selected as a care prevention program candidate] (Yes: 1, No: 0); whether item number 16 (homebound state) applies to the subject [Homebound state] (Yes: 1, No: 0); whether ≥1 checked answer for dementia [Dementia] (Yes: 1, No: 0); and whether ≥2 checked answers for depression [Depression] (Yes: 1, No: 0).
To calculate the odds ratio, we created two models: Model 1 into which the covariates were entered one by one in a forward manner with age and gender, and Model 2 into which the six covariates other than [Items number 1‐20, ≥10 checked answers] and [Selected as a care prevention program candidate] were entered at the same time as the age and gender.Statistical analysis was performed using the Japanese version of SPSS v. 17.0 (IBM, Armonk, NY, USA). We regarded P<.05 as showing significance.
3. RESULTS
3.1. Selection of subjects
We collected completed questionnaires from a total of 22 513 older people between April 2010 and March 2011. The coverage rate of study population was 32.3%. Of these subjects, 644 were excluded from the analyses because they died or became exempt from the long‐term care insurance system of Takasaki City. An additional 544 people who were certified as requiring long‐term care before March 2011 were also excluded from the analyses. As a result, a total of 21 325 subjects were analyzed. Of these subjects, 2573 were certified as requiring long‐term care, and 18 752 were not certified between April 2011 and March 2014 (Figure 1). Table 3 shows the characteristics of the former and latter groups.
Figure 1.
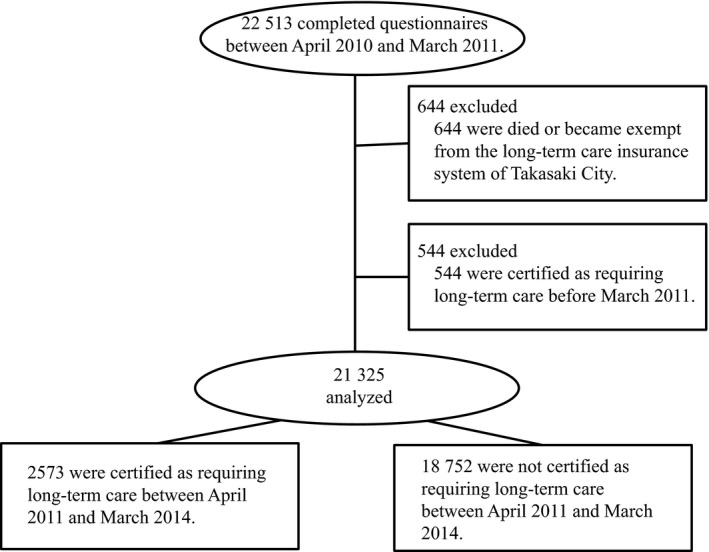
Flow of subjects through the study
Table 3.
Number and proportion of responses to Basic Checklist according to domain and whether the subject was certified as needing long‐term care
| Subjects not certified as requiring long‐term care (n=18 752) | Subjects certified as requiring long‐term care (n=2 573) | P‐valueb | |
|---|---|---|---|
| Gender (female) (%) | 11404 (60.8) | 1676 (65.1) | <.01 b |
| Age (years, mean ± standard deviation) | 74.0±5.5 | 80.0±5.8 | <.01 a |
| Domains of the Basic Checklist | |||
| Subjects with ≥10 checked answers for items number 1‐20 (%) | 307 (1.6) | 229 (8.9) | <.01 b |
| Subjects with ≥3 checked answers for the domain of physical function (%) | 1771 (9.4) | 731 (28.4) | <.01 b |
| Subjects to whom both items of nutritional condition apply (%) | 202 (1.1) | 76 (3.0) | <.01 b |
| Subjects with ≥2 checked answers for the domain of oral function (%) | 2352 (12.5) | 548 (21.3) | <.01 b |
| Subjects selected as care prevention program candidates (%) | 3753 (20.0) | 1082 (42.1) | <.01 b |
| Subjectsa with checked answer for item number 16 (homebound state) [%] | 325 (1.7) | 178 (6.9) | <.01 b |
| Subjectsa with ≥1 checked answer for the domain of dementia (%) | 1791 (9.6) | 611 (23.7) | <.01 b |
| Subjectsa with ≥2 checked answers for the domain of depression (%) | 1388 (7.4) | 500 (19.4) | <.01 b |
Subjects are selected as care prevention program candidates.
a, Mann‐Whitney tests; b, Chi‐square tests
3.2. Analyses
Table 4 shows the odds ratio of the need for long‐term care among those fulfilling the selection criteria in each domain.In Model 1, developed with each domain of the Basic Checklist plus age and gender as covariates, the fulfillment of the selection criteria in all domains of the Basic Checklist was highly associated with new long‐term care need certification (OR: 1.40‐2.71). The association between them was marked even when setting the significance level at P=.006 (P=.05/8) using the Bonferroni correction method in consideration of the eight domains of the criteria. Among the criteria of each domain of the Basic Checklist for care prevention program candidates, [Items number 1‐20, ≥10 checked answers] (OR: 2.71; 95% CI: 2.22‐3.32; χ2GF:<0.01; %CC: 88.1), [Physical function] (OR: 2.97; 95% CI: 2.05‐2.55; χ2GF:<0.01; %CC: 88.0), [Nutritional condition] (OR: 1.85; 95% CI: 1.38‐2.48; χ2GF:<0.01; %CC: 88.0), and [Oral function] (OR: 1.40; 95% CI: 1.25‐1.57; χ2GF:<0.01; %CC: 87.9) were associated with a higher odds ratio for requiring long‐term care. The criterion [Selected as a care prevention program candidate] was associated with a higher odds ratio for long‐term care requirement certification (OR: 1.90; 95% CI: 1.73‐2.08; χ2GF:<0.01; %CC: 88.0).
Table 4.
Association between long‐term care requirement certification and the criteria of each domain of the Basic Checklist for care prevention program participation
| Domains of the Basic Checklist | Model 1a | Model 2b | ||
|---|---|---|---|---|
| OR (95% CI) | P‐value | OR (95% CI) | P‐value | |
| [Items Number 1‐20, ≥10 checked answers] | 2.71 (2.22‐3.32) | <.01 | N.A. | N.A. |
| [Physical function] | 2.29 (2.05‐2.55) | <.01 | 1.87 (1.65‐2.13) | <.01 |
| [Nutritional condition] | 1.85 (1.38‐2.48) | <.01 | 1.60 (1.18‐2.16) | <.01 |
| [Oral function] | 1.40 (1.25‐1.57) | <.01 | 1.02 (0.89‐1.17) | .80 |
| [Selected as a care prevention program candidate] | 1.90 (1.73‐2.08) | <.01 | N.A. | N.A. |
| [Homebound state] | 1.91 (1.55‐2.37) | <.01 | 1.10 (0.88‐1.37) | .42 |
| [Dementia] | 1.97 (1.75‐2.20) | <.01 | 1.30 (1.11‐1.51) | <.01 |
| [Depression] | 1.96 (1.73‐2.22) | <.01 | 1.24 (1.06‐1.44) | <.01 |
OR, Odds ratio; CI, Confidence interval; N.A, Not applicable.
Model 1 into which the covariates were entered one by one along with the age and gender.
Model 2 into which the 6 covariates other than [Items Number 1‐20, ≥10 checked answers] and [Selected as a care prevention program candidate] were entered at the same time along with the age and gender.
Among the criteria for recommended participation in additional care prevention programs, [Homebound state] (OR: 1.91; 95% CI: 1.55‐2.37; χ2GF:<0.01; %CC: 88.0), [Dementia] (OR: 1.97; 95% CI: 1.75‐2.20; χ2GF:<0.01; %CC: 88.0), and [Depression] (OR: 1.96; 95% CI: 1.73‐2.22; χ2GF:<0.01; %CC: 87.9) were associated with a higher odds ratio (Table 4).
In Model 2—into which six domains of the Basic Checklist, excluding [Items number 1‐20, ≥10 checked answers] and [Selected as a care prevention program candidate], were simultaneously incorporated as covariates plus age and gender—the odds ratio of care needs significantly increased in the following domains: [Physical function] (OR: 1.87; 95% CI: 1.65‐2.13; χ2GF:<0.01; %CC:88.0); [Nutritional condition] (OR: 1.60; 95% CI: 1.18‐2.16; χ2GF:<0.01; %CC:88.0); [Dementia] (OR: 1.30; 95% CI: 1.11‐1.51; χ2GF:<0.01; %CC:88.0); and [Depression] (OR: 1.24; 95% CI: 1.06‐1.44; χ2GF:<0.01; %CC:88.0) (Table 4).
4. DISCUSSION
In multiple logistic regression analysis, to calculate the odds ratio of long‐term care needs at a 3 years follow‐up, the fulfillment of the selection criteria in all domains of the Basic Checklist was closely associated with new long‐term care need certification in Model 1, with each domain, age, and gender as covariates. In this model, the odds ratio was the highest for [Items number 1‐20, ≥10 checked answers], which is consistent with a previous study10 that monitored the status of long‐term care need certification 1 year after completion of the Basic Checklist. These findings highlight the importance of considering the fulfillment of [Items number 1‐20, ≥10 checked answers] as a comprehensive index based on the Basic Checklist when selecting care prevention program candidates. Our results also suggest that older residents who checked ≥10 of the 20 Basic Checklist items are at an increased risk of becoming certified as needing long‐term care, regardless of the domain and should therefore be high‐priority candidates for care prevention programs.
The odds ratio was the second highest for [Physical function]. The fulfillment of the selection criteria in this domain was also associated with an increased risk of becoming certified as needing long‐term care in previous studies.10, 11 [Physical function] showed the highest odds ratio in Model 2, which incorporated covariates from multiple domains simultaneously. Generally the leading causes of newly certified long‐term care needs are arthropathies (12.2%), fracture, and falls (9.3%) in Japan.12 Furthermore, decreased physical function is closely associated with new long‐term care need certification.12 Therefore, to promote care prevention for community‐dwelling older people, it may be useful to improve their physical function. Physical activity interventions for older people have been reported to promote physical function, which prevents falls,13, 14 and improves cognitive function.15, 16 Such approaches have been used by care prevention programs based on the long‐term care insurance system in a large number of intervention studies.17 The Basic Checklist has been used to select participants in some of them,18, 19, 20 in addition to being adopted as an index to measure the outcomes of physical activity interventions.20 It has also been used to select participants by investigators who examine other types of intervention.21, 22 The Basic Checklist is a useful instrument for multiple purposes, such as selecting care prevention program participants and measuring outcomes.
In both Models 1 and 2, new long‐term care need certification was closely associated with the fulfillment of the selection criteria in four domains: [Physical function], [Nutritional condition], [Dementia], and [Depression]. The association between the fulfillment of these selection criteria and risk was observed in previous studies.10, 11 The results of our study confirmed their findings by following a larger number of participants for a longer time.
This study included only the older people who completed the Basic Checklist. The health of persons who do not participate in health surveys of older people has frequently been reported to be poor.23, 24 Persons who did not complete the Basic Checklist were likely to be frail older residents in poor health, with an increased risk of becoming certified as individuals with long‐term care needs. By excluding them from this study, the proportion of persons at risk may have been underestimated. The low coverage rate of study population (32.3%) was a limitation of our study. Furthermore, information on diseases and a decreased functional ability to lead an independent life associated with long‐term care need certification was not available, and certified support or care grades were not classified. In consideration of these points, it may be necessary to conduct further research.
5. CONCLUSION
Individuals who were selected as long‐term care prevention program candidates based on the Basic Checklist had a higher risk of requiring long‐term care. Older residents corresponding to 10 or more of the 20 Basic Checklist items are at the highest risk of becoming certified as needing long‐term care.
CONFLICT OF INTEREST
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
ACKNOWLEDGMENTS
The authors thank Yuko Tsunoda at Gunma University, Maebashi, Japan, for her technical assistance. This study was conducted in cooperation with Takasaki City government according to the 2014, Takasaki City, Long‐Term Care Prevention Program Assessment Contract. Yamaguchi H was supported by a Grant‐in‐Aid for Scientific Research from the Ministry of Education, Science, Sports, Culture, and Technology, Japan (23300197 and 22650123).
Kamegaya T, Yamaguchi H, Hayashi K. Evaluation by the Basic Checklist and the risk of 3 years incident long‐term care insurance certification. J Gen Fam Med. 2017;18:230–236. https://doi.org/10.1002/jgf2.52
REFERENCES
- 1. Japanese Ministry of Health , Labour and Welfare . Long‐term Care Insurance in Japan. Available at: http://www.mhlw.go.jp/english/topics/elderly/care/index.html. accessed April 9, 2016.
- 2. Japanese Ministry of Health , Labour and Welfare . The current situation and the future direction of the Long‐term Care Insurance System in Japan ~With a Focus on the Housing for the Elderly. Available from: http://www.mhlw.go.jp/english/policy/care-welfare/care-welfare-elderly/dl/ri_130311-01.pdf. accessed April 9, 2016.
- 3. Japanese Ministry of Health , Labour and Welfare . The Basic Checklist. Available at: http://www.mhlw.go.jp/topics/kaigo/kaigi/051219/dl/2.pdf. accessed April 9, 2016 (in Japanese).
- 4. Arai T, Obuchi S, Sato M, Noro M. The relationships between the basic checklist score, physical function, and improvement in physical function. Nihon Ronen Igakkai Zasshi. 2010;47:585–91. (in Japanese). [DOI] [PubMed] [Google Scholar]
- 5. Kato C, Fujita R, Ida K. Participant characteristics and intervention effects of a program to improve the physical function in community‐dwelling frail elderly subjects. Nihon Ronen Igakkai Zasshi. 2013;50:804–11. (in Japanese). [DOI] [PubMed] [Google Scholar]
- 6. Nemoto M, Yabushita N, Seino S, et al. Identification of the physical function of frail older adults and effectivity of the health check‐up questionnaire (Kihon check‐list). J Phys Fitness Sports Med. 2011;60:413–22. (in Japanese). [Google Scholar]
- 7. Meguro K, Team KP. The validity of the Basic Checklist in the old‐old population: The Kurihara Project. Jpn J Geriat Psychiat. 2012;23:725–30. (in Japanese). [Google Scholar]
- 8. Suzuki N, Makigami K, Goto A, Yokokawa H, Yasumura S. Comparison of ability‐based and performance‐based IADL evaluation of community‐dwelling elderly using the Kihon Checklist and TMIG Index of Competence. Nihon Ronen Igakkai Zasshi. 2007;44:619–26. (in Japanese). [DOI] [PubMed] [Google Scholar]
- 9. Yamazaki S, Yasumura S, Goto A, et al. Factors associated with reducing the Tojikomori for potentially dependent elderly: the Kaigoyobou Keizokuteki Hyouka Bunseki Shien Jigyou of the health, labour and welfare ministry. Jpn J Gerontol. 2010;32:23–32. (in Japanese). [Google Scholar]
- 10. Tomata Y, Hozawa A, Ohmori‐Matsuda K, et al. Validation of the Kihon Checklist for predicting the risk of 1‐year incident long‐term care insurance certification: the Ohsaki Cohort 2006 Study. Nihon Koshu Eisei Zasshi. 2011;58:3–13. (in Japanese). [PubMed] [Google Scholar]
- 11. Hamazaki Y, Morikawa Y, Nakamura K, Morimoto S, Nakagawa H. Relationship between participation in a secondary screening test for the frail elderly and new onset of the need for long‐term care among the elderly in a rural town. Nihon Koshu Eisei Zasshi. 2012;59:801–9. (in Japanese). [PubMed] [Google Scholar]
- 12. Japanese Ministry of Health , Labour and Welfare . Graphical Review of Japanese Household. Available at: http://www.mhlw.go.jp/toukei/list/dl/20-21-h19.pdf. accessed April 9, 2016 (in Japanese).
- 13. Chang JT, Morton SC, Rubenstein LZ, et al. Interventions for the prevention of falls in older adults: systematic review and meta‐analysis of randomised clinical trials. BMJ 2004;328:680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Moncada LV. Management of falls in older persons: a prescription for prevention. Am Fam Physician 2011;84:1267–76. [PubMed] [Google Scholar]
- 15. Angevaren M, Aufdemkampe G, Verhaar HJ, Aleman A, Vanhees L. Physical activity and enhanced fitness to improve cognitive function in older people without known cognitive impairment. Cochrane Database Syst Rev. 2008;3: CD005381. [DOI] [PubMed] [Google Scholar]
- 16. Kamegaya T, Long‐Term‐Care Prevention Team of Maebashi City , Maki Y, Yamagami T, Yamaguchi T, Murai T, Yamaguchi H. Pleasant physical exercise program for prevention of cognitive decline in community‐dwelling elderly with subjective memory complaints. Geriatr Gerontol Int. 2012;12:673–9. [DOI] [PubMed] [Google Scholar]
- 17. Ukawa S, Tamakoshi A, Sakamoto A. A systematic review of intervention programs for frail elderly people enrolled in the Japanese social long‐term care insurance system. Nihon Koshu Eisei Zasshi. 2015;62:3–19. [DOI] [PubMed] [Google Scholar]
- 18. Maki Y, Ura C, Yamaguchi T, et al. Effects of intervention using a community‐based walking program for prevention of mental decline: a randomized controlled trial. J Am Geriatr Soc 2012;60:505–10. [DOI] [PubMed] [Google Scholar]
- 19. Hasegawa M, Yamazaki S, Kimura M, Nakano K, Yasumura S. Community‐based exercise program reduces chronic knee pain in elderly Japanese women at high risk of requiring long‐term care: a non‐randomized controlled trial. Geriatr Gerontol Int. 2013;13:167–74. [DOI] [PubMed] [Google Scholar]
- 20. Yamada M, Arai H, Sonoda T, Aoyama T. Community‐based exercise program is cost‐effective by preventing care and disability in Japanese frail older adults. J Am Med Dir Assoc. 2012;13:507–11. [DOI] [PubMed] [Google Scholar]
- 21. Ukawa S, Satoh H, Yuasa M, et al. A randomized controlled trial of a Functioning Improvement Tool home‐visit program and its effect on cognitive function in older persons. Int J Geriatr Psychiatry 2012;27:557–64. [DOI] [PubMed] [Google Scholar]
- 22. Sakayori T, Maki Y, Hirata S, Okada M, Ishii T. Evaluation of a Japanese “Prevention of long‐term care” project for the improvement in oral function in the high‐risk elderly. Geriatr Gerontol Int. 2013;13:451–7. [DOI] [PubMed] [Google Scholar]
- 23. Rockwood K, Stolee P, Robertson D, Shillington ER. Response bias in a health status survey of elderly people. Age Ageing 1989;18:177–82. [DOI] [PubMed] [Google Scholar]
- 24. Iwasa H, Yoshida H, Kim H, et al. A mortality comparison of participants and non‐participants in a comprehensive health examination among elderly people living in an urban Japanese community. Aging Clin Exp Res. 2007;19:240–5. [DOI] [PubMed] [Google Scholar]


